Abstract
Background
Chondrosarcoma is the second most frequent malignant bone tumor. Grade I chondrosarcoma (syn.: atypical cartilaginous tumor) is classified as an intermediately and locally aggressive neoplasm and typically is treated less aggressively (i.e., by intralesional curettage). Does the data regarding local recurrence (LR) and metastatic disease justify this?
Methods
From 1982 to 2014, 37 consecutive patients with G1 chondrosarcoma had been resected or curetted. The margin was defined as R0 (wide resection) or R1 (marginal resection). All patients were followed for evidence of local recurrence or metastatic disease. Overall and recurrence-free survival were calculated, and various potentially prognostic factors were evaluated.
Results
In 23 patients (62%), the tumor was widely (R0) resected, whereas in 14 patients, (38%) the resection was marginal (R1). Overall survival was 97% after 5 years, 92% after 10 years, and 67% after 20 years. Five-year local recurrence-free survival was 96%. Ten-year local recurrence-free survival was 83%. Local recurrence-free survival showed a significant correlation to margin status but no correlation to location or age. None of the patients with local recurrence died during the follow-up. One patient had metastatic disease at initial presentation, and a further five patients developed metastatic disease during follow-up. Metastatic disease proofed to be a highly significant factor for survival but was not correlated to local recurrence.
Conclusions
There was no significant correlation between the outcome and the primary tumor location. Marginal resection was a risk factor for LR, but there was no significant difference in the overall survival in patients with or without LR. Metastatic disease (16%) was more common than expected from the literature and a significant predictor for poor overall survival.
Similar content being viewed by others
Background
Representing more than 20% of all malignant tumors of the bone, chondrosarcoma (CS) is the third most common primary malignant bone tumor following osteosarcoma and multiple myeloma [1]. Chondrosarcomas are most often seen in adult age and are a very heterogenous group with a diverse behavior depending on the histological subtype. The most common subtype is conventional CS. Clear cell CS appears to have the best prognosis while dedifferentiated CS has the worst outcome [2]. For conventional CS, tumor grading and anatomic location are the main predictors of outcome [2,3,4].
Therapy consists mainly of surgical resection. In critical locations, radiotherapy in high dosage (if applicable) is effective as an adjuvant or as the sole therapy [5] while chemotherapy appears to be less effective [6, 7]. The definition of adequate surgical margins varies within the literature [4]. In high-grade chondrosarcomas, a wide resection is the standard to prevent local recurrence. In low-grade chondrosarcoma, intralesional curettage is commonly used although controversial [8,9,10]. In a large literature review in 2017, Chen et al. found only 1.2% metastatic disease and no difference in local recurrence with respect to surgical margins [11].
The WHO classification of grade I chondrosarcoma (atypical cartilaginous tumor) as an intermediately and locally aggressive neoplasm implies that there is no or only rarely metastatic disease with low-grade chondrosarcoma [12]. This definition comprises the benign clinical behavior of the lesions, but it is known that even grade I CS carries a risk of metastasis in up to 6% of cases [12].
With intralesional curettage becoming more and more common in low-grade chondrosarcoma, it appears important to take a closer look at the influence of less aggressive (intralesional) surgical margins and outcomes in grade I CS. Does a wider margin prevent metastases or local recurrence in low-grade CS? Is the location of the lesion a predictor of outcome in low-grade lesions as it is in high-grade CS [13, 14]?
The main aim of this retrospective study hence was to have a closer look at this very selective and homogenous group of patients with primary low-grade conventional CS treated at a single tumor center to determine prognostic factors for overall and recurrence-free survival. The secondary aim was a comparison of our data to the literature for quality-of-care reasons.
Materials and methods
Patients
From 1982 through 2014, 87 consecutive patients with central chondrosarcoma of the extremities, the pelvis, and the trunk wall were treated at our institution. All patients had a diagnosis of chondrosarcoma based on histological, radiological, and clinical features.
Preoperatively, mainly magnetic resonance imaging (MRI) and in some cases computed tomography (CT) were used to define size and location of the tumor. A CT scan of the chest was obtained to rule out or prove metastatic disease.
Margins and inclusion criteria
All patients underwent surgical resections. The margin was defined as R0 if a rim of healthy tissue around the lesion was present (wide resection) or R1 if the margins were contaminated as in close resections or curettages. From those 87 patients, 37 showed a low-grade (G1) histology and were classified as atypical cartilaginous tumors. Inclusion criteria for this study were therefore a histology-proven G1 grading in the resected specimen with or without proven metastatic disease.
Statistical analysis
All patients were followed for evidence of local recurrence or distant metastasis in general by MRI scans and chest x-rays. Due to the long investigation period with considerable changes in the ability to detect small metastases, especially in the lungs, and small local recurrences, the number of metastatic cases as also local recurrences might be underestimated. Subsequently, recurrence-free survival would be overestimated. Therefore, in addition, overall survival is calculated from the time of surgery to last follow-up or death in deceased patients. Overall and recurrence-free survival were calculated by the Kaplan-Meier method. Significance analysis was performed using the log-rank test or the chi-square test. The data analysis software used was SPSS 24®.
Results
The mean age of the 12 female and 25 male patients was 47.1 years (range 17–84 years). The upper extremity was involved in 4 cases (humerus 2, radius 1, hand 1), and the lower extremity in 23 cases (femur 15, tibia 4, fibula 2, feet 2). Five patients had the lesion in the trunk (scapula 4, ribs 1), and five in the pelvis (4 os ilium, 1 os pubis). Sixteen (43%) showed extraosseous tumor growth.
The median duration of symptoms was 19.8 months (range 0–153 months). Nineteen patients (51%) complained of pain, 3 (8%) complained about swelling, and 5 (11%) suffered from a pathological fracture, and in 6 cases (16%), the lesion was found as an incidental finding. Occasionally, there were neurological symptoms or a loss of the range of motion. Thirty-one patients (84%) had a biopsy taken before surgery. In four cases, the biopsies showed benign cartilaginous lesions, later classified as false negatives. Six patients had undergone intralesional surgery elsewhere with either intramedullary nails or endoprostheses prior to presenting to our institution, and the tumor had been overlooked or underestimated in these cases. One patient had metastatic disease at the time of diagnosis.
In 28 patients, the tumor was resected or curetted and the defect, as necessary, was filled with allogenic bone graft. A reconstruction with megaendoprostheses was performed in 8 (22%), and an amputation in 1 case (2%). In 23 patients (64%), the tumor was widely (R0) resected, whereas in 14 patients (38%), the resection was marginal (R1). There were no R2 resections. Histology showed a conventional low-grade chondrosarcoma in all patients. In pelvic lesions, 66% were marginal resections compared to 92% at the lower extremities and 33% at the upper extremities. There were no marginal resections at the trunk.
In five patients (14%), revisions due to complications had to be performed. The complications included loosening of an endoprosthesis in two, neurological impairment because of a malpositioned osteosynthesis screw, additional and more aggressive tumor resection, and deep wound infection in one case each.
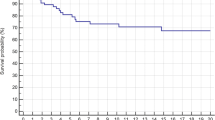
The mean follow-up in our series was 127.9 months (range 0–344 months). Only 3 patients had a follow-up time of less than 24 months, and 13 patients (35%) had a follow-up of less than 5 years. Five patients died during the follow-up: one within the first year, one after 7 years, and three after more than 15 years (Fig. 1).
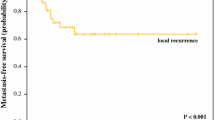
Overall survival was 97% after 5 years, 92% after 10 years, and 67% after 20 years (Fig. 1). Five-year local recurrence-free survival was 96%. Ten-year local recurrence-free survival was 83%. In total, 5 (14%) patients developed local recurrences: only 1 of them during the first 5 years and 4 after 10 years. In our patients, local recurrence-free survival showed a significant correlation with the margin status (Fig. 2; p = 0.035) but no correlation with the location or the patients’ age. This was confirmed by means of multivariate analysis (Table 1).
None of the patients with local recurrence (LR) died during the follow-up, and only one showed LR and metastatic disease (MD).
Six patients (16%) in our study developed metastases, whereas one patient had an initial spinal metastasis but remained free of disease after resection of that lesion. In five patients (14%), metastatic disease developed during follow-up (four pulmonary, one bone). Mean metastasis-free survival was 86% after 5 years and 75% after 20 years. Four of our patients deceased during the follow-up period (Fig. 3). In the multivariate analysis, there was no correlation between the surgical margins and the location in respect to metastatic disease.
Metastasis proved to be a significant predictive factor for survival (Fig. 3; p < 0.0001). Age over 50 showed a trend in respect to worse overall survival, but this failed significance testing (Fig. 4; p = 0.078). Only one of the patients (5%) without soft tissue extension died during the follow-up period compared to four patients (27%) with extraosseous infiltration (n.s.) (Fig. 5; p = 0.07). Local recurrence and lesion location showed no significance in predicting overall survival.
Discussion
Grade I chondrosarcoma is generally assumed to be an entity of low malignancy with 5-year survival rates of 90% and more and with little to no metastatic disease [12, 15]. There is, however, no consensus on prognostic factors (i.e., location of the lesion) or the influence of surgical margins (wide resection vs. curettage) and the clinical outcomes in grade I CS.
Although tumor location and patient age have been identified as being strong predictive factors for overall survival in patients with conventional chondrosarcoma in previous publications [16, 17], in our series of patients with low-grade CS, we observed no statistically significant correlation between overall survival and patient age at diagnosis (p = 0.078) or tumor location (p = 0.238).
A 14% LR rate in our group of patients is similar to previously published numbers of LR in low-grade CS, ranging between 0 and 26% [18,19,20,21]. Marginal resection was a significant predictor for LR (p = 0.037) in our series. It is known that local recurrence in high-grade chondrosarcoma is associated with poorer outcome, but there is still some debate about whether this is true for low-grade chondrosarcoma as well [22,23,24,25]. We were not able to demonstrate a significant correlation between local recurrence and overall survival in this group of patients (p = 0.6). Several authors have described a progression of the tumor and the occurrence of distant metastases in association with local recurrence [12, 22, 26, 27]. However, there also are studies that were unable to find such a correlation between LR and MD [23, 24]. In our patients, there was also no correlation between LR and MD with only one patient having both LR and MD. This discrepancy to some of the published literature might be due to the limited mean follow-up of the patients with LR in our group of only 77 months, especially since Schwab et al. described that poor outcomes in patients with LR become significant only beyond 10 years [22].
As mentioned above, there is no consensus on whether or not LR has any significance when it comes to overall survival in low-grade CS. However, many studies have shown that inadequate surgical margins lead to a higher rate of LR, necessitating further surgery with additional risks [10, 23, 24, 27]. Some studies suggest to combine intralesional curettage with adjuvant measures such as the application of poly-methyl-methacrylat (PMMA) or cryosurgery to reduce LR rates [20, 28, 29].
The metastatic potential of low-grade CS is controversially discussed in the literature with rates ranging between 0 and 6% [18, 24, 28, 30]. In our study, one patient already had MD at initial assessment and five patients developed MD during follow-up (16%). A possible reason for this observation could be the longer follow-up of our study with a mean metastasis-free survival of 76 months. Studies which did not describe any MD often report a much shorter follow-up period [31, 32]. However, there are also published studies with a long follow-up and little or no MD as well [9, 20]. This might reflect the difficulty in differentiating between atypical chondrogenic tumors and benign chondromas.
In this study, MD proved to be a significant predictor for a poor outcome (p < 0.0001) which is consistent with the findings of other authors. However, we found no significant correlation between the surgical procedure and MD. Interestingly, 2 out of 8 patients with intralesional curettage and 4 out of 16 patients with extraosseous tumor growth developed MD but there was no statistically significant correlation between surgical margins and MD (p = 0.45) or extraosseous growth and MD (p = 0.21).
Although not statistically significant, the high rate of MD and the higher mortality suggests that extraosseous tumor growth may be a different subtype of CS after all, since it appears to behave differently than regular low-grade CS.
Conclusion
While the location of the primary tumor is a strong prognostic factor for high-grade CS (i.e., pelvic lesions have a worse prognosis), in this study, there was no significant difference between patients’ outcomes and the tumor location. Marginal resection (R1) was a risk factor for LR, but compared to high-grade CS, there was no significant difference in the overall survival of patients with or without LR. Patients with soft tissue extension of the tumor showed a worse prognosis, but this failed significance testing. MD was more common (16%) than expected and a significant predictor for poor overall survival.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CS:
-
Chondrosarcoma
- CT:
-
Computed tomography
- G1, G2, G3:
-
Grading according to the French Federation of Cancer Centers’ grading system
- LR:
-
Local recurrence
- MD:
-
Metastatic disease
- MRI:
-
Magnetic resonance imaging
- n.s.:
-
Not significant
- PMMA:
-
Poly-methyl-methacrylate
- R0, R1, R2:
-
Resection margin
References
Doyle LA. Sarcoma classification: an update based on the 2013 World Health Organization classification of tumors of soft tissue and bone. Cancer. 2014;120:1763–74.
Bindiganavile S, Han I, Yun JY, Kim HS. Long-term outcome of chondrosarcoma: a single institutional experience. Cancer Res Treat. 2015;47:897–903.
Di Giorgio L, Touloupakis G, Vitullo F, Sodano L, Mastantuono M, Villani C. Intralesional curettage, with phenol and cement as adjuvants, for low-grade intramedullary chondrosarcoma of the long bones. Acta Orthop Belg. 2011;77:666–9.
Puri A, Shah M, Agarwal MG, Jambhekar NA, Basappa P. Chondrosarcoma of bone: does the size of the tumor, the presence of a pathologic fracture, or prior intervention have an impact on local control and survival? J Cancer Res Ther. 2009;5:14–9.
Outani H, Hamada K, Imura Y, Oshima K, Sotobori T, Demizu Y, Kakunaga S, Joyama S, Imai R, Okimoto T, et al. Comparison of clinical and functional outcome between surgical treatment and carbon ion radiotherapy for pelvic chondrosarcoma. Int J Clin Oncol. 2016;21:186–93.
van Maldegem AM, Gelderblom H, Palmerini E, Dijkstra SD, Gambarotti M, Ruggieri P, Nout RA, van de Sande MA, Ferrari C, Ferrari S, et al. Outcome of advanced, unresectable conventional central chondrosarcoma. Cancer. 2014;120:3159–64.
Gelderblom H, Hogendoorn PC, Dijkstra SD, van Rijswijk CS, Krol AD, Taminiau AH, Bovee JV. The clinical approach towards chondrosarcoma. Oncologist. 2008;13:320–9.
Donati D, Colangeli S, Colangeli M, Di Bella C, Bertoni F. Surgical treatment of grade I central chondrosarcoma. Clin Orthop Relat Res. 2010;468:581–9.
Chen YC, Wu PK, Chen CF, Chen WM. Intralesional curettage of central low-grade chondrosarcoma: a midterm follow-up study. J Chin Med Assoc. 2017;80:178–82.
Fiorenza F, Abudu A, Grimer RJ, Carter SR, Tillman RM, Ayoub K, Mangham DC, Davies AM. Risk factors for survival and local control in chondrosarcoma of bone. J Bone Joint Surg Br. 2002;84:93–9.
Chen X, Yu LJ, Peng HM, Jiang C, Ye CH, Zhu SB, Qian WW. Is intralesional resection suitable for central grade 1 chondrosarcoma: a systematic review and updated meta-analysis. Eur J Surg Oncol. 2017;43:1718–26.
Andreou D, Gilg MM, Gosheger G, Werner M, Hardes J, Pink D, Leithner A, Tunn PU, Streitburger A. Metastatic potential of grade I chondrosarcoma of bone: results of a multi-institutional study. Ann Surg Oncol. 2016;23:120–5.
Bergh P, Gunterberg B, Meis-Kindblom JM, Kindblom LG. Prognostic factors and outcome of pelvic, sacral, and spinal chondrosarcomas: a center-based study of 69 cases. Cancer. 2001;91:1201–12.
Jodi M, Carter CYI. Conventional chondrosarcoma: old controversies and new insights. Diagn Histopathol. 2014;20:181–90.
Funovics PT, Panotopoulos J, Sabeti-Aschraf M, Abdolvahab F, Funovics JM, Lang S, Kotz RI, Dominkus M. Low-grade chondrosarcoma of bone: experiences from the Vienna Bone and Soft Tissue Tumour Registry. Int Orthop. 2011;35:1049–56.
Bjornsson J, McLeod RA, Unni KK, Ilstrup DM, Pritchard DJ. Primary chondrosarcoma of long bones and limb girdles. Cancer. 1998;83:2105–19.
Giuffrida AY, Burgueno JE, Koniaris LG, Gutierrez JC, Duncan R, Scully SP. Chondrosarcoma in the United States (1973 to 2003): an analysis of 2890 cases from the SEER database. J Bone Joint Surg Am. 2009;91:1063–72.
de Camargo OP, Baptista AM, Atanasio MJ, Waisberg DR. Chondrosarcoma of bone: lessons from 46 operated cases in a single institution. Clin Orthop Relat Res. 2010;468:2969–75.
Hanna SA, Whittingham-Jones P, Sewell MD, Pollock RC, Skinner JA, Saifuddin A, Flanagan A, Cannon SR, Briggs TW. Outcome of intralesional curettage for low-grade chondrosarcoma of long bones. Eur J Surg Oncol. 2009;35:1343–7.
Meftah M, Schult P, Henshaw RM. Long-term results of intralesional curettage and cryosurgery for treatment of low-grade chondrosarcoma. J Bone Joint Surg Am. 2013;95:1358–64.
Kim W, Han I, Kim EJ, Kang S, Kim HS. Outcomes of curettage and anhydrous alcohol adjuvant for low-grade chondrosarcoma of long bone. Surg Oncol. 2015;24:89–94.
Schwab JH, Wenger D, Unni K, Sim FH. Does local recurrence impact survival in low-grade chondrosarcoma of the long bones? Clin Orthop Relat Res. 2007;462:175–80.
Lee FY, Mankin HJ, Fondren G, Gebhardt MC, Springfield DS, Rosenberg AE, Jennings LC. Chondrosarcoma of bone: an assessment of outcome. J Bone Joint Surg Am. 1999;81:326–38.
Donati D, El Ghoneimy A, Bertoni F, Di Bella C, Mercuri M. Surgical treatment and outcome of conventional pelvic chondrosarcoma. J Bone Joint Surg Br. 2005;87:1527–30.
Sheth DS, Yasko AW, Johnson ME, Ayala AG, Murray JA, Romsdahl MM. Chondrosarcoma of the pelvis. Prognostic factors for 67 patients treated with definitive surgery. Cancer. 1996;78:745–50.
Pant R, Yasko AW, Lewis VO, Raymond K, Lin PP. Chondrosarcoma of the scapula: long-term oncologic outcome. Cancer. 2005;104:149–58.
Weber KL, Pring ME, Sim FH. Treatment and outcome of recurrent pelvic chondrosarcoma. Clin Orthop Relat Res. 2002;397:19-28.
Streitburger A, Ahrens H, Balke M, Buerger H, Winkelmann W, Gosheger G, Hardes J. Grade I chondrosarcoma of bone: the Munster experience. J Cancer Res Clin Oncol. 2009;135:543–50.
Ahlmann ER, Menendez LR, Fedenko AN, Learch T. Influence of cryosurgery on treatment outcome of low-grade chondrosarcoma. Clin Orthop Relat Res. 2006;451:201–7.
Andreou D, Ruppin S, Fehlberg S, Pink D, Werner M, Tunn PU. Survival and prognostic factors in chondrosarcoma: results in 115 patients with long-term follow-up. Acta Orthop. 2011;82:749–55.
Mermerkaya MU, Bekmez S, Karaaslan F, Danisman M, Kosemehmetoglu K, Gedikoglu G, Ayvaz M, Tokgozoglu AM. Intralesional curettage and cementation for low-grade chondrosarcoma of long bones: retrospective study and literature review. World J Surg Oncol. 2014;12:336.
Campanacci DA, Scoccianti G, Franchi A, Roselli G, Beltrami G, Ippolito M, Caff G, Frenos F, Capanna R. Surgical treatment of central grade 1 chondrosarcoma of the appendicular skeleton. J Orthop Traumatol. 2013;14:101–7.
Acknowledgements
Not applicable.
Conflict of interest statement
All authors disclose no financial and personal relationships with other people or organizations that could inappropriately influence (bias) this work. This study did not have any grants or funding despite the academic setting of the institutions and authors.
Funding
This study did not have any grants or funding despite the academic setting of the institutions and authors.
Author information
Authors and Affiliations
Contributions
JF is a student doing his thesis on chondrosarcomas. He contacted the patients, acquired the data, and is involved in the drafting and revising of the manuscript. AK is a surgeon on many of the cases and is involved in the drafting and revising of the manuscript. AB-M is a radiologist reviewing the radiologic investigations and is involved in the drafting and revising of the manuscript. TK is a pathologist reviewing the pathologic investigations and is involved in the drafting and revising of the manuscript. LL is an oncologist and is involved in drafting and revising of the manuscript. Every patient was discussed in the interdisciplinary panel, and the final decision regarding chemotherapy was based on this. CB is a surgeon on many of the cases, is a reviewer of the manuscript, and is involved in the drafting and revising of the manuscript. FR reviewed the radiotherapy, decided which patient to treat or not to treat, and is involved in the drafting and revising of the manuscript. VJ is a surgeon on many of the cases, is a reviewer of the manuscript, and is involved in the drafting and revising of the manuscript. HRD is the corresponding author, developed the study concept, did the final data analysis, and provided the major clinical input in the writing of the manuscript. Each author has contributed significantly to and is willing to take public responsibility for this study: its design, data acquisition, and analysis and interpretation of data. All authors have been actively involved in the drafting and critical revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of the Medical Faculty, University of Munich. Written consent was obtained from all surviving patients included in this study. In accordance with the ethics committee, the data from non-surviving patients were irreversibly anonymized for statistical evaluation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Fromm, J., Klein, A., Baur-Melnyk, A. et al. Survival and prognostic factors in conventional G1 chondrosarcoma. World J Surg Onc 17, 155 (2019). https://doi.org/10.1186/s12957-019-1695-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-019-1695-4