Abstract
Background
Cancer survivors experience a decrement in health-related quality of life (HRQoL) resulting from the disease as well as adverse effects of therapy. We evaluated the HRQoL of cancer patients, stratified by primary cancer site, stage, treatment response and associated adverse events, along with its determinants.
Methods
Data were collected from 12,148 patients, sampled from seven purposively chosen leading cancer hospitals in India, to elicit HRQoL using the EuroQol questionnaire comprising of 5-dimensions and 5-levels (EQ-5D-5L). Multiple linear regression was used to determine the association between HRQoL and various socio-demographic as well as clinical characteristics.
Results
Majority outpatients (78.4%) and inpatients (81.2%) had solid cancers. The disease was found to be more prevalent among outpatients (37.5%) and inpatients (40.5%) aged 45–60 years and females (49.3–58.3%). Most patients were found to be in stage III (40–40.6%) or stage IV (29.4–37.3%) at the time of recruitment. The mean EQ-5D-5 L utility score was significantly higher among outpatients [0.630 (95% CI: 0.623, 0.637)] as compared to inpatients [0.553 (95% CI: 0.539, 0.567)]. The HRQoL decreased with advancing cancer stage among both inpatients and outpatients, respectively [stage IV: (0.516 & 0.557); stage III (0.609 & 0.689); stage II (0.677 & 0.713); stage I (0.638 & 0.748), p value < 0.001]. The outpatients on hormone therapy (B = 0.076) showed significantly better HRQoL in comparison to patients on chemotherapy. However, palliative care (B=-0.137) and surgery (B=-0.110) were found to be associated with significantly with poorer HRQoL paralleled to chemotherapy. The utility scores among outpatients ranged from 0.305 (bone cancer) to 0.782 (Leukemia). Among hospitalized cases, the utility score was lowest for multiple myeloma (0.255) and highest for testicular cancer (0.771).
Conclusion
Older age, lower educational status, chemotherapy, palliative care and surgery, advanced cancer stage and progressive disease were associated with poor HRQoL. Our study findings will be useful in optimising patient care, formulating individualized treatment plan, improving compliance and follow-up.
Similar content being viewed by others
Introduction
Cancer has been reported to be one of the leading causes of mortality and disability in several countries [1, 2]. Recently, 19.3 million annual incident cases, and 10 million cancer deaths were reported globally [3]. In India, cancer caused 813,000 deaths, which was over 8% of total mortality [4]. Despite one-fourth of the incidence rate, mortality rates due to cancer in India as are high as in the developed countries [5]. This is attributable to several demand and supply side barriers to accessing treatment, [6,7,8,9,10,11] as a result of which more than half of the cancer patients are diagnosed in an advanced stage during their initial consultation with physicians [11,12,13]. This often leads to a poor quality of life for patients with advanced cancer, need for multimodality treatment, treatment related adverse effects and poor prognosis [14].
With increasing advancements in cancer treatment modalities such as chemotherapy, targeted therapy, radiotherapy, surgery etc., overall and progression-free survival among cancer patients have significantly improved. Quality of life in these cancer patients with prolonged survival becomes even more paramount. However, these therapeutic interventions usually precipitate with severe adverse effects that impact the overall quality of life in physical, psychological, and social dimensions. Previous reports have identified that cancer patients have a poorer health-related quality of life (HRQoL), which is attributable to both the disease and adverse effects (AEs) associated with treatment [15, 16]. Additionally, HRQoL tends to diminish with progression of disease and subsequent treatments [16, 17]. Therefore, beyond focusing on clinical efficacy and safety endpoints, it is crucial to incorporate HRQoL into treatment decision-making. This inclusion helps provide a more comprehensive understanding of the potential value of new therapies [18,19,20,21,22,23,24].
There are several detailed disease-specific instruments to measure HRQoL among cancer patients [25,26,27]. In contrast, generic instruments to assess HRQoL such as the EuroQoL five-dimensions five-levels (EQ-5D-5L) is an easy to administer tool to generate utility scores in the range of 0 (death) to 1 (full health) [28]. Such utility scores are suitable for estimating quality-adjusted life years (QALYs) in health technology assessments [29]. Quantitative assessments of HRQoL offer a means to assess the health outcomes from the patient’s viewpoint. Such estimates are valuable for health service planning and the formulation of health policies [30].
Overall, there is scarce evidence on HRQoL for cancer. Previous research has primarily focused on assessing HRQoL post-treatment or comparing pre- and post-treatment HRQoL [31,32,33,34]. While these assessments are valuable for understanding the treatment impact on HRQoL, establishing baseline data related to HRQoL in cancer patients based on factors such as primary site, cancer stage, type of treatment and treatment response is crucial for effective treatment planning, service provision, and follow-up of these patients [35]. The previous studies have either focused on single cancer type, or have certain methodological limitations [36,37,38]. None of the studies have reported cancer-site specific utility scores so far. Considering the gap in literature, the present study has comprehensively ascertained the HRQoL (stratified by primary cancer site, stage, treatment, treatment response, associated adverse events) among the nationally representative sample of 12,148 patients enrolled across 7 cancer hospitals in six states of India, using the generic EQ-5D-5L instrument [39]. Additionally, the factors influencing HRQoL were analysed using a regression analyses.
Materials and methods
The cancer patients were recruited from seven leading cancer hospitals (Fig. 1). It is worthwhile to mention that two-thirds of the chosen hospitals are among the top 10 hospitals in India, having highest number of cancer claims under India’s national health insurance scheme, Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (ABPM-JAY) [40]. The detailed methodology has been documented in the protocol paper [39].
Patient selection
Sample size and sampling
Patients were enrolled in a prospective manner during the period from October 2020 to March 2022 at the outpatient department (OPD) and inpatient department (IPD) of the chosen hospitals. Patients were recruited using a systematic random sampling technique, with the sampling interval determined by the average volume of patients per day in each hospital to obtain the required sample size. In the context of site-specific disease management groups (DMGs) clinics, probability proportional to size (PPS) method was used to determine the number of days when data was collected from respective DMGs [39]. On a particular day, when data was collected from a given DMG, a minimum of 10 patients were recruited. This method has ensured a minimum number of patients for each cancer site/type.
We aimed to interview a minimum of 1690 patients at each healthcare facility, resulting in a total sample of 11,830 across 7 health-care facilities. However, we were able to recruit 12,148 patients (9,787 in OPD and 2,359 in IPD) in India for HRQoL assessment.
Inclusion criteria
All cancer patients, irrespective of age and gender, who sought treatment at OPD and IPD at chosen hospitals were recruited. The OPD patients included: newly diagnosed individuals (recently diagnosed with cancer), on-treatment patients (currently undergoing active cancer treatments such as chemotherapy or radiotherapy), and follow-up cases (patients who have completed their treatment and are on follow-up, with or without maintenance therapy).
All the inpatient admissions who had stayed overnight in the hospital were recruited. The HRQoL was assessed on the day of recruitment. The case definitions used for enrolment of patients in OPD and IPD are outlined in Annexure I.
Assessment for quality of life
The EQ-5D-5L questionnaire includes five domains: mobility, self-care, usual activity, pain/discomfort, and anxiety/depression [28]. Each domain is graded on a scale of five levels, ranging from no problems to extreme problems. The Indian value set was used to derive the utility scores [42]. A score of ‘1’ indicates perfect health, and ‘0’ indicates death, with a range of 1 to -0.549 [43]. Additionally, patients were asked to rate their present health state on a scale from 0 to 100 through the EuroQol visual analogue scale (EQ-VAS) [44].
Data analysis
We used Indian tariff value set to compute utility scores [45]. Mean utility scores according to primary cancer site, cancer stage, and type of treatment such as radiotherapy, chemotherapy, hormonal therapy, surgery, combination therapy etc. were calculated. We constructed the weights for different type of cancers using global disease burden data in the Indian context, in order to derive utility scores [46]. Sampling weights were calculated in order to correct for any discrepancies between the sample and the population. The sampling weights were computed for each stratum and were calculated as the ratio of the population count to the sample count within that stratum.
These analytical weights were then applied to give more or less weight to each observation according to their relative representativeness in the population. The weight for an individual in a particular stratum is equal to the total known population size in that stratum divided by the sample size in that stratum. The post-stratification weight, \( {w}_{i}\) for each respondent “i” in stratum “h” is calculated as:
where, \( {N}_{h}\) is known population size in stratum h and \( {n}_{h}\) is the sample size in stratum h.
Association between HRQoL and socio-demographic & clinical characteristics was assessed among cancer patients seeking outpatient as well as inpatient treatment.
Assessment of factors associated with HRQoL
ANOVA test was applied to evaluate the statistical significance of difference in quality of life scores among patients of different age groups, religion, marital status, area of residence, educational status, income status (based on consumption expenditure) and clinical characteristics. An independent samples t-test was specifically used to assess differences in HRQoL with gender stratification. Using the data for OPD and IPD patients separately, we used the multivariable linear regression. The multiple linear model was assumed to be
where Y is the outcome variable, \( {X}_{i}\) is the value of the ith predictor, and e is the error.
We used quality of life as a dependent variable, while remaining variables such as patient’s age, gender, area of residence, education level, marital status, wealth quintile, line of treatment, type of cancer and treatment, response to treatment, and occurrence of any adverse effect were considered as predictors. Normality of error term for both models (outpatient and inpatient) has been checked using “Kolmogorov Smirnov Test” with insignificant p-values as 0.253 (outpatients) and 0.185 (hospitalized cases). While the presence of homoscedasticity is checked using “Breusch-Pagan Test” with insignificance p-values as 0.098 (outpatients) and 0.188 (hospitalized cases), which fails to reject the null hypothesis of homoscedasticity. Hence, both models met the assumptions of a normal error term and homoscedasticity. There is no multicollinearity with variance inflation values ranging between 1.03 and 3.95 for outpatients, and from 1.06 to 2.03 for inpatients.
Ethical considerations
Ethical approval was obtained individually from the Institute Ethics Committee of all the participating centres. A written informed consent was obtained from all study participants. In case of participants aged 18 years and above, consent was obtained directly from them. However, for participants below the age of 18, parental or guardian consent was sought.
Results
The HRQoL of 9,787 cancer patients receiving outpatient care and 2,359 hospitalized cases was evaluated using the EQ-5D-5L and EQ-VAS tools. As shown in Table 1, Out of 9,787 outpatient cancer cases, majority were found to be diagnosed with solid cancers (78.4%) followed by haematological cancers (21.6%). At the time of recruitment, majority patients were in stage III (40.6%) and stage IV (29.4%) of cancer. Nearly 83.6% were on first line of treatment followed by 14.1% on second line treatment. The most common treatment modality at outpatient setting was chemotherapy and/or targeted therapy, given to approximately 50% cancer patients. The adverse effects were reported by 90% cancer patients.
As shown in Table 2, among hospitalized cases (N = 2,359), maximum patients fall within the 45–60 years age group, accounting for 37.5%, followed by the 31–45 years category (23.3%) and those above 60 years (21%). Majority patients were found to be hospitalized in semi-private hospitals (69.1%) while 30.9% were admitted in public health care facilities. The duration of hospitalization in most of the patients (29.6%) was more than 5 days. Majority hospitalized cancer cases presented in stage III (40%) and IV (37.3%) at the time of recruitment. Detailed sample characteristics of outpatient and hospitalized cases are outlined in Tables 1 and 2 respectively.
Cancer related HRQoL by socioeconomic factors
The mean utility score for outpatient and inpatient cancer patients across different socioeconomic and clinical groups are depicted in Tables 1 and 2 respectively. The mean utility score was significantly higher among cancer patients seeking outpatient care [0.630 (95% CI: 0.623, 0.637)] than those on inpatient treatment [0.553 (95% CI: 0.539, 0.567)]. Similarly, the mean EQ-VAS score [63.58 (95% CI: 63.25, 63.91)] was higher among outpatients than inpatients [56.03 (95% CI: 55.46, 56.6)].
Among outpatients, females had higher utility score (0.651) as compared to males (0.607). Similar trends were observed among hospitalized cancer patients, with an EQ-5D-5L index of 0.555 among females and 0.551 among males. Patients aged 16–30 years demonstrated the highest quality of life score, with a mean EQ-5D-5L score of 0.728 among outpatients and 0.619 among hospitalized cases. The utility scores among outpatients were found to be significantly lower among older age group i.e. 60 years & above (0.563). Similar findings were observed among hospitalized cases (0.540 among 45–60 years and 0.524 among patients aged above 60 years).
As shown in Tables 1 and 2, the utility scores were observed to increase with increase in level of education, ranging from 0.463 to 0.529 among illiterates to 0.630 to 0.724 among graduates and postgraduates. Moreover, HRQoL among outpatients was observed to be lowest among richer income groups (ranging from 0.548 to 0.587), and highest for poorest income groups (0.725). A similar pattern was observed among hospitalized cases.
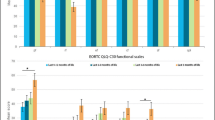
Cancer related HRQoL by clinical characteristics
As depicted in Tables 1 and 2, a significant decline in the HRQoL was observed with an increase in the severity of cancer stage (p value < 0.001). The poorest HRQoL was observed in stage IV cancer patients, ranging from 0.516 to 0.557, followed by stage III (0.609 to 0.689), stage II (0.677 to 0.713), and stage I (0.638 to 0.748) among inpatients and outpatients, respectively.
The outpatients who had undergone surgery were observed to have significantly poorer quality of life (0.529, p value < 0.001) than patients on other treatment modalities like palliative care (0.540), combination therapy (0.604), radiotherapy (0.611), chemotherapy (0.644), diagnostics (0.686), maintenance therapy (0.741) and hormone therapy (0.801). However, indoor cancer patients who were on maintenance therapy (-0.276) and palliative care reported poorer quality of life (0.247) in comparison to patients on other treatment modalities including combination therapy (0.413), diagnostics (0.451), hormone therapy (0.488), surgery (0.518), chemotherapy (0.587), radiotherapy (0.621) and immunotherapy (0.726) etc.
Further, cancer patients with adverse effects had lower quality of life (0.627 & 0.544) in comparison to patients with no adverse effects (0.835 & 0.637) among both outpatients and inpatients respectively. Also, patients who were disease free reported significantly better quality of life (0.691 among outpatients and 0.553 among inpatients) in contrast to patients with progressive disease (0.553 among outpatients and 0.420 among inpatients). Furthermore, patients who were hospitalized and on the first line of treatment reported a higher utility score of 0.572, in contrast to those on subsequent lines of treatment, with scores of 0.417, 0.444, and 0.416 for the second, third, and fourth lines of treatment, respectively.
Mean EQ-5D-5L utility scores showed significant differences across various categories, including education, marital status, treatment, stage of disease, treatment response, and the adverse effects among both outpatients and inpatients. In addition, mean EQ-5D-5L utility scores varied significantly across different age groups, gender, residential status and income quintile among outpatients. Significant differences were observed in EQ-5D-5 L scores based on the type of hospital, duration of hospitalization, and the line of treatment among inpatients.
Factors associated with HRQoL among outpatients
The utility score was found to decrease by 0.001 (B = -0.001) with every one unit increase in life year of the cancer patient (Table 3). The utility score increased significantly with level of education (B = 0.043 among patients having primary and middle level education versus B = 0.115 among graduates and postgraduates). In comparison to cancer patients in urban settings, individuals from slum areas reported a notably diminished quality of life (B = -0.098). The utility scores were observed to be significantly lower among richer income groups as compared to the poorest (B = -0.081 among rich and B = -0.058 among richest income groups). The patients on hormone therapy (B = 0.076) had better HRQoL as compared to patients on chemotherapy. However, palliative care (B=-0.137) and surgery (B=-0.110) were significantly associated with poorer HRQoL. Further, stage 4 cancer patients were observed to have significantly lower quality of life (B = -0.118) as compared to stage 1 cancer cases. As compared to first line therapy, cancer patients on third line of treatment were found to have significantly poorer quality of life (B = -0.146). Further, patients who were in progressive disease state were found to have significantly poorer quality of life (B = -0.0081) in comparison to disease-free survival patients. Absence of adverse effects was also significantly associated with higher quality of life (B = 0.113) in comparison to presence of adverse effects in cancer patients.
Factors associated with HRQoL among hospitalized patients
The utility score was observed to decrease by 0.002 (B = -0.002) with every one unit increase in life year of the cancer patient (Table 4). The patients having higher educational status (graduates & post graduates) reported significantly higher HRQoL (B = 0.075, p < 0.001) as compared to illiterate patients. As compared to first line therapy, cancer patients on second line therapy reported significantly lower HRQoL (B =- 0.065, p < 0.008). The utility scores were found to be significantly higher among cancer patients without adverse events (B = 0.085, p < 0.001). The patients hospitalized in semi-private hospitals had higher HRQoL (B = 0.231, p < 0.001), as against those admitted in public hospitals. The patients on surgery (B = -0.127), combination therapy (B = -0.133), diagnostic work up (B = -0.144), palliative care (B = -0.258) and maintenance therapy (B = -0.702) were observed to be significantly associated with poorer quality of life paralleled to chemotherapy. Further, patients who were in progressive disease state were found to experience significantly lower HRQoL (B = -0.149) relative to disease free survival patients.
Cancer site specific utility scores among patients seeking outpatient and indoor treatment
The stratified analysis was conducted to calculate utility scores based on primary cancer site for patients receiving both hospitalized and outpatient treatment, as presented in Tables 5 and 6. Significant differences (p value < 0.001) were noted between utility scores across various cancers. Among outpatients, utility scores ranged from 0.305 (bone cancer) to 0.782 (Leukemia). For hospitalized cases, the lowest utility score was observed for multiple myeloma (0.255), while the highest was for testicular cancer (0.771). Site-specific utility scores, using both EQ-5D-5L and EQ-VAS, stratified by the cancer site for patients who sought outpatient and hospitalized treatment, are detailed in Tables 5 and 6, respectively.
Discussion
Despite the advent of advanced therapeutic technologies which have significantly improved survival, achieving cancer-free status does not directly imply an improved quality of life [47]. The frequently considered efficacy criteria of cancer therapy often prove insufficient, lacking a comprehensive approach to the entire disease process, treatment, and overall well-being. As a result, it is imperative to account for the changes in HRQoL with the newer therapies, apart from their impact on survival [48, 49].
It is imperative to shift the objective of cancer treatment from solely achieving successful health outcomes to a more encompassing goal of enhancing the overall HRQoL for patients. A deeper comprehension of HRQoL in cancer patients is instrumental in enriching the lived experience of cancer survivors, emphasizing the importance of adding more life to the added years, rather than merely extending the years of life. Limited studies are available across the globe as well as from India that comprehensively assess HRQoL among cancer patients. None of the studies conducted so far have reported quality of life scores according to typer of cancer site, stage, treatment and response. Majority quality of life assessment studies conducted in India have focussed on single type of cancer with small sample sizes, thus cannot be generalizable to all cancer patients in India [50, 51, 52].
The findings of our study suggest that the HRQoL of cancer patients declines as their income level increases. A previous study conducted in India also revealed an escalating gradient in the self-reported morbidity with higher socioeconomic status [51, 53]. This suggests that individuals with higher income tend to report a diminished quality of life for a similar health condition—a phenomenon termed as positional objectivity [33]. It is plausible that wealthier individuals may be more health-conscious, leading them to assess their quality of life in relation to their health differently than those with lower incomes. Conversely, individuals with lower economic status may face unmet basic life needs, placing “health” lower in their priority ranking. Consequently, the wealthier individuals perceive themselves to have a poorer quality of life compared to their less affluent counterparts. Further, poorer HRQoL was observed among elderly patients among both outpatients and inpatients which indicate that these frail patients have poor tolerance to cancer treatment, slow recovery from adverse effects and hence attempts should be made for de-escalation of treatment in this elderly group to improve the HRQoL. The HRQoL was also found to be better among graduates and postgraduates (0.724 and 0.630 among outpatients and inpatients respectively). Higher education is associated with better awareness about the disease, treatment options and outcomes. The ability to make informed decisions improves the HRQoL in educated groups. Contrary to this ignorance breeds more fears and inability to make decisions. Thus, it is important to generate awareness about disease, treatment and outcomes in the illiterate cancer patients through social workers or Non-governmental organizations to improve their HRQoL.
Given the large sample size, our study is powered to provide valid estimates of HRQoL for 12 specific cancers in India, with a 5% margin of error; and top 20 cancers with a 10% margin of error and a 95% confidence interval.
Policy implications
Quality-adjusted life year (QALYs) has been recommended as a metric for valuation of health outcomes for economic evaluations in India [54]. In order to compute QALYs, the valuation of HRQoL for various health states is necessary. However, collecting primary data for estimating utility scores is a time-consuming and resource-intensive process. The HRQoL database developed in this study would be immensely beneficial for expediting HTA analyses. This is particularly crucial as HTA studies specifically require information on utility scores. Therefore, the current research makes a substantial contribution to the current body of evidence by providing separate utility scores specific to cancer site and cancer stage.
The clinical trials should not only assess the safety and survival end points but also incorporate the indicator of quality of life so as to choose best intervention for cancer care. Further, interventions causing minimal adverse effects should be explored as majority patients having adverse effects reported poorer quality of life. As financial constraints are major problem for the patients, financial toxicity and the impact on quality of life should be taken into account before recommending cost-intensive treatments to poor patients in palliative settings.
Strengths
We would like to highlight some of the methodological strengths of our study. Firstly, our patient cohort was sourced from seven healthcare facilities, encompassing the largest volume of oncology patients nationwide. Given that the HRQoL assessment is influenced by factors such as culture, ethnicity, region, and socio-demographic characteristics, the selected study hospitals provide a broad geographical representation. Therefore, the patient population, selected through systematic random sampling, is indicative of the diversity within the Indian population. Secondly, utility scores were computed using country-specific tariff values i.e. the Indian value-set [45]. Thirdly, it is the first study to ascertain HRQoL and its predictors in a substantially large sample of 12,148 cancer patients. Fourth, our study provides valuable information to identify determinants of HRQoL.
Limitations
We acknowledge certain limitations in our study. Firstly, as present study was a cross-sectional survey, therefore we could not assess the HRQoL of patients pre and post intervention. However, since the sample of patients was heterogeneous in nature, the data pertaining to HRQoL represented all types of cancer patients on different treatment modalities. Secondly, we have assessed the HRQoL among hospitalized cases at the time of recruitment and did not record the quality of life on each of day of hospitalization till discharge.
Conclusion
In conclusion, this study provides empirical evidence on HRQoL among cancer patients, as well as significant predictors of the HRQoL. Older age, lower educational status, chemotherapy, palliative care and surgery, stage of cancer, progressive disease were associated with poor HRQoL. The results of the present study should be used in devising individualized treatment plans, enhancing patient care, improving compliance and follow-up.
Data availability
The data underlying this article are available in the article and in its online supplementary material. The datasets and analysis will be available upon request. The study investigators retain ownership of their data. Any requests for access to data should be made directly to study investigator.
References
Bray F, Laversanne M, Weiderpass E, Soerjomataram I. The ever-increasing importance of cancer as a leading cause of premature death worldwide. Cancer. 2021;127(16):3029–30.
World Health Organization (WHO). (2020) Global Health Estimates 2020 deaths by cause, age, sex, by country and by region, 2000–2019. World Health Organization, Geneva. - references - scientific research publishing. 2022 [cited 2022 Aug 7]. Available from: https://www.scirp.org/reference/referencespapers.aspx?referenceid=3188789.
Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, Znaor A, Bray F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144(8):1941–53.
Sharma S. Fighting cancer with cheap treatment and screening. Hindustan Times, New Delhi. 2018 Sep 23 [cited 2022 August 7]. Available from: https://www.hindustantimes.com/health/fighting-cancer-with-cheap-treatment-and-screening/story-GbPF7x8Nb6Z15TWurEppNK.html.
Mallath MK, Taylor DG, Badwe RA, Rath GK, Shanta V, Pramesh CS, Digumarti R, Sebastian P, Borthakur BB, Kalwar A, Kapoor S. The growing burden of cancer in India: epidemiology and social context. Lancet Oncol. 2014;15(6):e205–12.
Gupta A, Shridhar K, Dhillon PK. A review of breast cancer awareness among women in India: Cancer literate or awareness deficit? Eur J Cancer. 2015;51(14):2058–66.
Tripathi N, Kadam YR, Dhobale RV, Gore AD. Barriers for early detection of cancer amongst Indian rural women. South Asian Journal of Cancer. 2014;3(02):122–7.
Nyblade L, Stockton M, Travasso S, Krishnan S. A qualitative exploration of cervical and breast cancer stigma in Karnataka, India. BMC Womens Health. 2017;17(1):1–5.
Palat G, Stenlander C, Jacob J, Sinha S, Rapelli V, Wiebe T, Brun E, Segerlantz M. Specialized palliative care and the quality of life for hospitalized cancer patients at a low-resource hospital in India. Indian J Palliat Care. 2018;24(3):289.
Pramesh CS, Badwe RA, Borthakur BB, Chandra M, Raj EH, Kannan T, Kalwar A, Kapoor S, Malhotra H, Nayak S, Rath GK. Delivery of affordable and equitable cancer care in India. Lancet Oncol. 2014;15(6):e223–33.
Rajpal S, Kumar A, Joe W. Economic burden of cancer in India: evidence from cross-sectional nationally representative household survey, 2014. PLoS ONE. 2018;13(2):e0193320.
Singh M, Prasad CP, Singh TD. Lalit,*. Cancer Research in India: challenges & opportunities. Indian J Medicl Res. October 2018;148(4):362–5. https://doi.org/10.4103/ijmr.IJMR_171_18.
Hebert JR, Ghumare SS, Gupta PC. Stage at diagnosis and relative differences in breast and prostate cancer incidence in India: comparison with the United States. Asian Pac J Cancer Prev. 2006;7(4):547.
Pakseresht S, Ingle GK, Garg S, Sarafraz N. Stage at diagnosis and delay in seeking medical care among women with breast cancer, Delhi, India. Iran Red Crescent Med J. 2014;16(12).
Smyth EN, Shen W, Bowman L, Peterson P, John W, Melemed A, Liepa AM. Patient-reported pain and other quality of life domains as prognostic factors for survival in a phase III clinical trial of patients with advanced breast cancer. Health Qual Life Outcomes. 2016;14(1):1–0.
Arboe B, Goerloev JS, Olsen MH, Dalton SO, Nielsen KF, Nielsen SR, Madsen C, de Nielsen R. Nully Brown P. Social outcomes after high dose chemotherapy with autologous stem cell transplant. Blood. 2016;128(22):1193.
Wang H, Manca A, Crouch S, Bagguley T, Yu G, Aas E, Howell D, Burton C, Patmore R, Roman E, Smith A. PCN351-HEALTH-STATE UTILITY VALUES IN DIFFUSE LARGE B-CELL LYMPHOMA. Value in Health. 2018;21:74.
Kelly JL, Pandya C, Friedberg JW, Mohile SG. Health-related quality of life in older patients following diffuse large B-cell lymphoma (DLBCL) diagnosis. Blood. 2012;120(21):4287.
Efficace F, Gaidano G, Lo-Coco F. Patient-reported outcomes in hematology: is it time to focus more on them in clinical trials and hematology practice? Blood the Journal of the American Society of Hematology. 2017;130(7):859–66.
Au HJ, Ringash J, Brundage M, Palmer M, Richardson H, Meyer RM. Added value of health-related quality of life measurement in cancer clinical trials: the experience of the NCIC CTG. Expert Rev PharmacoEcon Outcomes Res. 2010;10(2):119–28.
US Department of Health and Human Services FDA Center for Drug Evaluation and Research laurie. burke@ fda. hhs. gov, US Department of Health and Human Services FDA Center for Biologics Evaluation and Research toni. stifano@ fda. hhs. gov, US Department of Health and Human Services FDA Center for Devices. and Radiological Health SXD@ cdrh. fda. gov. Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health and Quality of Life Outcomes. 2006;4(1):79.
European Medicine Agency. The use of patient-reported outcome (PRO) measures in oncology studies. Appendix 2 to the guideline on the evaluation of anticancer medicinal products in man.
Kluetz PG, Slagle A, Papadopoulos EJ, Johnson LL, Donoghue M, Kwitkowski VE, Chen WH, Sridhara R, Farrell AT, Keegan P, Kim G. Focusing on core patient-reported outcomes in cancer clinical trials: symptomatic adverse events, physical function, and disease-related symptoms. Clin Cancer Res. 2016;22(7):1553–8.
Basch E, Geoghegan C, Coons SJ, Gnanasakthy A, Slagle AF, Papadopoulos EJ, Kluetz PG. Patient-reported outcomes in cancer drug development and US regulatory review: perspectives from industry, the Food and Drug Administration, and the patient. JAMA Oncol. 2015;1(3):375–9.
Cella D, Webster K, Cashy J, Kutikova L, Burgess MF, Lin BK, Bowman L, Liepa AM, Gauthier JE, Gregory SA, Johnson SA. Development of a measure of Health-Related Quality of Life for Non-hodgkin’s Lymphoma Clinical Research: The Functional Assessment of Cancer Therapy-Lymphoma (FACT-Lym).
Brucker PS, Yost K, Cashy J, Webster K, Cella D. General population and cancer patient norms for the Functional Assessment of Cancer Therapy-General (FACT-G). Eval Health Prof. 2005;28(2):192–211.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC, Kaasa S. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. JNCI: J Natl Cancer Inst. 1993;85(5):365–76.
Kind P. The EuroQol instrument. An index of health-related quality of life. Quality of life and pharmacoeconomics in clinical trials. 1996.
Department of Health Research. Health Technology Assessment in India– HTAIn. 2018. [cited August 7, 2022]. Available from: https://dhr.gov.in/sites/default/files/eNewsletter/img/HTAIn/HTAIn10-01-2017.pdf.
Pickard AS, Wilke CT, Lin HW, Lloyd A. Health utilities using the EQ-5D in studies of cancer. PharmacoEconomics. 2007;25(5):365–84.
Agarwal SK, Munjal M, Koul R, Agarwal R. Prospective evaluation of the quality of life of oral tongue cancer patients before and after the treatment. Ann Palliat Med. 2014;3(4):238–43.
Barrios R, Bravo M, Gil-Montoya JA, Martínez-Lara I, García-Medina B, Tsakos G. Oral and general health-related quality of life in patients treated for oral cancer compared to control group. Health Qual Life Outcomes. 2015;13(1):1–8.
Hassel AJ, Danner D, Freier K, Hofele C, Becker-Bikowski K, Engel M. Oral health-related quality of life and depression/anxiety in long-term recurrence-free patients after treatment for advanced oral squamous cell cancer. J Cranio-Maxillofacial Surg. 2012;40(4):e99–102.
Indrapriyadharshini K, Madankumar PD, Karthikeyan GR. Oral health-related quality of life in patients treated for oral malignancy at Kanchipuram district, India: a cross-sectional study. Indian J Cancer. 2017;54(1):11.
Rogers SN, Semple C, Babb M, Humphris G. Quality of life considerations in head and neck cancer: United Kingdom National Multidisciplinary guidelines. J Laryngology Otology. 2016;130(S2):49–52.
Borggreven PA, Verdonck-de Leeuw IM, Muller MJ, Heiligers ML, De Bree R, Aaronson NK, Leemans CR. Quality of life and functional status in patients with cancer of the oral cavity and oropharynx: pretreatment values of a prospective study. Eur Arch Otorhinolaryngol. 2007;264(6):651–7.
Infante-Cossio P, Torres-Carranza E, Cayuela A, Gutierrez-Perez JL, Gili-Miner M. Quality of life in patients with oral and oropharyngeal cancer. Int J Oral Maxillofac Surg. 2009;38(3):250–5.
Visacri MB, Ferrari GB, Pimentel R, Ambrósio RD, Lima CS, Mazzola PG, Moriel P. Evaluation of the quality of life of patients before treatment of squamous cell carcinoma of the head and neck by means of chemoradiotherapy. Contemp Oncology/Współczesna Onkologia. 2015;19(2):148–53.
Prinja S, Dixit J, Gupta N, Mehra N, Singh A, Krishnamurthy MN, Gupta D, Rajsekar K, Kalaiyarasi JP, Roy PS, Malik PS. Development of national cancer database for cost and quality of life (CaDCQoL) in India: a protocol. BMJ open. 2021;11(7):e048513.
Kaur S, Jain N, Bhatnagar PC. Early trends from Utilization of Oncology services: insights from Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (PM-JAY). Working Paper 004. https://www.pmjay.gov.in/sites/default/files/2019-11/Working 20paper-4% 20% 281% 29. pdf; 2021.
Ramasubbu SK, Pasricha RK, Nath UK, Rawat VS, Das B. Quality of life and factors affecting it in adult cancer patients undergoing cancer chemotherapy in a tertiary care hospital. Cancer Rep. 2021;4(2):e1312.
Jyani G, Sharma A, Prinja S, Kar SS, Trivedi M, Patro BK, Goyal A, Purba FD, Finch AP, Rajsekar K, Raman S. Development of an EQ-5D value set for India using an Extended Design (DEVINE) study: the Indian 5-Level version EQ-5D Value Set. Value in Health. 2022.
Prieto L, Sacristán JA. What is the value of social values? The uselessness of assessing health-related quality of life through preference measures. BMC Med Res Methodol. 2004;4(1):1–9.
Rabin R, Charro FD. EQ-SD: a measure of health status from the EuroQol Group. Ann Med. 2001;33(5):337–43.
Jyani G, Prinja S, Kar SS, Trivedi M, Patro B, Purba F, Pala S, Raman S, Sharma A, Jain S, Kaur M. Valuing health-related quality of life among the Indian population: a protocol for the development of an EQ-5D value set for India using an extended design (DEVINE) study. BMJ open. 2020;10(11):e039517.
Dhillon PK, Mathur P, Nandakumar A, Fitzmaurice C, Kumar GA, Mehrotra R, Shukla DK, Rath GK, Gupta PC, Swaminathan R, Thakur JS. The burden of cancers and their variations across the States of India: the global burden of Disease Study 1990–2016. Lancet Oncol. 2018;19(10):1289–306.
New Delhi Television Ltd. (NDTV). 1300 Die of Cancer Every Day in India. 2015. [cited 2022 August 7]. Available from: https://www.ndtv.com/india-news/1-300-die-of-cancer-every-day-in-india-763726.
Cdc.gov. CDC - Concept - HRQOL. 2011. [cited 2016 Apr 20]. Available from: https://www.cdc.gov/hrqol/concept.htm HRQoL concepts. Centers for Disease Control and Prevention. 2018 [cited 2022 Aug 7]. Available from: https://www.cdc.gov/hrqol/concept.htm.
Feeny D, Furlong W, Mulhern RK, Barr RD, Hudson M. A framework for assessing health-related quality of life among children with cancer. Int J Cancer. 1999;83(S12):2–9.
Jyani G, Chauhan AS, Rai B, Ghoshal S, Srinivasan R, Prinja S. Health-related quality of life among cervical cancer patients in India. Int J Gynecologic Cancer. 2020;30(12).
Prinja S, Jeyashree K, Rana S, Sharma A, Kumar R. Wealth related inequalities in self reported morbidity: positional objectivity or epidemiological transition? Indian J Med Res. 2015;141(4):438.
Gupta N, Pandey AK, Dimri K, Jyani G, Goyal A, Prinja S. Health-related quality of life among breast cancer patients in India. Support Care Cancer. 2022; 30(12):9983–9990. Doi10:1007/s00520-022-07395-7.Epub 2022 Oct 12. PMID: 36222977.
Goldie SJ, Kohli M, Grima D, Weinstein MC, Wright TC, Bosch FX, Franco E. Projected clinical benefits and cost-effectiveness of a human papillomavirus 16/18 vaccine. J Natl Cancer Inst. 2004;96(8):604–15.
Sharma D, Prinja S, Aggarwal AK, Rajsekar K, Bahuguna P. Development of the Indian reference case for undertaking economic evaluation for health technology assessment. Lancet Reg Health Southeast Asia. 2023;16:100241. https://doi.org/10.1016/j.lansea.2023.100241.
Funding
The study is funded by the Department of Health Research, Ministry of Health and Family Welfare, Government of India vide grant number F.No.T.11011/02/2017-HR/3100291. However, the funder did not play a role in the design of the study; the collection, analysis, and interpretation of the data; the writing of the manuscript; and the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Conceptualization: SP, NG, JD. Data curation: SP, JD, NG, ACK, PSR, NM, LK,PM, AS, DG, AG, KR, MNK, SG. Formal Analysis: SP, AG, JD, DG. Funding acquisition: SP. Investigation: SP, JD. Methodology: SP, JD, NG. Project administration: SP, JD. Resources: SP. Software: SP, JD. Supervision: SP. Validation: SP, JD, NG, DG, ACK, PSR, NM, LK, AS, PM, AG, KR, MNK, SG. Visualization: SP, JD, NG, DG, ACK, PSR, NM, LK, AS, PM, AG, KR, MNK, SG. Writing - original draft: JD, NG, SP. Writing - review & editing: SP, JD, NG, DG, ACK, PSR, NM, LK, AS, PM, AG, KR, MNK, SG.
Corresponding author
Ethics declarations
Ethical approval
The ethical approval was obtained from Institutional Ethics Committee of Post Graduate Institute of Medical Education and Research, India with reference number IEC-03/20202 − 1565.
Conflict of interest
All authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dixit, J., Gupta, N., Kataki, A. et al. Health-related quality of life and its determinants among cancer patients: evidence from 12,148 patients of Indian database. Health Qual Life Outcomes 22, 26 (2024). https://doi.org/10.1186/s12955-024-02227-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-024-02227-0