Abstract
Successful oral insulin administration can considerably enhance the quality of life (QOL) of diabetes patients who must frequently take insulin injections. Oral insulin administration, on the other hand, is seriously hampered by gastrointestinal enzymes, wide pH range, mucus and mucosal layers, which limit insulin oral bioavailability to ≤ 2%. Therefore, a large number of technological solutions have been proposed to increase the oral bioavailability of insulin, in which polymeric nanoparticles (PNPs) are highly promising for oral insulin delivery. The recently published research articles chosen for this review are based on applications of PNPs with strong future potential in oral insulin delivery, and do not cover all related work. In this review, we will summarize the controlled release mechanisms of oral insulin delivery, latest oral insulin delivery applications of PNPs nanocarrier, challenges and prospect. This review will serve as a guide to the future investigators who wish to engineer and study PNPs as oral insulin delivery systems.
Graphical Abstract

Similar content being viewed by others
Introduction
Insulin is a protein hormone commonly used for the treatment of diabetes, which is secreted by islet cells to regulate blood glucose. Insulin is essential for the treatment of type 2 diabetes. Diabetes mellitus is a metabolic disorder characterized by a reduction in insulin production by pancreatic islet cells, which consequently results in an elevated blood glucose level and abnormalities in the metabolism of carbohydrates, proteins, and lipids [1]. Diabetes mellitus is typically divided into two major types, type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM). T1DM requires insulin for treatment, whereas T2DM is treated with insulin secretagogues or insulin sensitizers. Insulin treatment is only used when other medications are ineffective [2]. Notwithstanding the oral administration route of drugs with minimum invasiveness has advantages over other forms, leading to higher patient compliance [3]. Nevertheless, oral administration of insulin faces various serious challenges, such as gastrointestinal enzymes, wide pH range, mucus, and mucosal layers that restrict the oral bioavailability of insulin to < 2% [4]. At the same time, there are a number of disadvantages associated with using oral insulin, such as unwanted side effects, poor pharmacokinetics, a short distribution half-life, and so on [5].
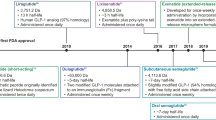
The novel intelligent nanocarrier delivery systems (NDS) offer an ideal solution to address issues such as low solubility, low bioavailability, undesired side effects, poor pharmacokinetics, short distribution half-life, and many others [6]. Nanocarriers can improve insulin loading capacity, stability, selectivity, and bioavailability and reduce the toxicity and side effects of oral insulin administration [7]. Furthermore, nanopcarriers protect insulin from gastrointestinal enzymes and slowly release insulin in the digestive tract, which then enters the liver via the portal vein, where it directly participates in the glucose metabolism of liver and lowers blood glucose levels [4, 8]. Recently, many nanocarriers, including lipid-based nanocarriers (liposomes, micelles) [9,10,11], dendrimers [12, 13], carbon nanotubes (CNTs) [14, 15], inorganic nanocarriers (quantum dots) [16, 17], gold nanoparticles [18, 19] and polymeric nanoparticles (PNPs) [20,21,22,23,24] have been reported. Nevertheless, because of low loading capacity, high-cost, lack of stability, inferior biocompatibility, or bio-safety, current NPs still show some disadvantages in oral insulin delivery [9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24]. Hence, PNPs have been the most researched materials for constructing nano-based drug-delivery systems due to their unique features such as simple craft, excellent stability, preferable biocompatibility, tailored medication administration, improved bioavailability, controlled drug release from a single dosage, and drug protection until delivery to the intended place [25,26,27] (Fig. 1). The amino and carboxyl groups present at the ends of insulin polypeptide chain can bind with PNPs through weak bonding interactions such as π–π, CH–π, hydrogen bonding, and van der Waals interactions or covalent bonding (Fig. 2) [28,29,30,31]. These interactions remarkably enhance the stability and number of insulin molecules loaded on the PNPs.
In this review, we summarize the most recent advances in employing PNPs as promising insulin nanocarriers in the oral insulin delivery system. First, we outline the classification and applications of PNPs as stimuli-responsive polymeric nanoparticles in oral insulin delivery system. Following that, insulin release strategies from PNPs nanocarriers are explored. Finally, we present a comprehensive overview of the progress, obstacles, and opportunities of using PNPs in oral insulin delivery systems so that future researchers can engineer and investigate them in these systems.
Drug release strategy
Nanocarrier system
A nanocarrier is a smart delivery system that depends on the breakdown or diffusion of NPs to release the drug at the target site. All nano-based targeted delivery vehicles are made up of three basic parts: (a) a physiologically inert nanocarrier, (b) a pharmaceutically active component, and (c) a targeting moiety attached to the surface [5]. The nanocarrier systems have demonstrated in vivo their potential to boost the drug stability and selectivity while decreasing toxicity and adverse effects.
Traditional drug delivery systems (TDDS) are non-specific targeting systems that rely on the systemic delivery route to distribute drugs throughout the body. Depending on the nature of the drug, this type of system may also have numerous adverse effects and inadequate drug delivery [4]. In recent years, intelligent drug delivery systems (IDDS) have outperformed traditional delivery systems in the context of drug delivery. The drug delivery systems (DDS) regulates the therapeutic effect of drugs by addressing issues related to their solubility, bioavailability, and toxicity [32]. The DDS are intelligently designed to deliver drugs to particular organs or tissues in a regulated manner in order to keep drug concentrations within the therapeutic range [33] or even to accomplish “programmed” or “on-demand” drug release [34].
Strategies for targeted drug release
The drug loading capacity of a nanomaterial is defined as the amount of drug docked per mass of the NPs [35], and drugs are loaded on the NP in two ways: (i) drug is combined during the NP manufacturing process, and (ii) drug is absorbed after the NPs preparation process [36]. The physical and chemical properties of a nanomaterial govern its drug loading capacity; hence, its structure must be kept intact for targeted drug delivery [37]. On the other hand, optimal size and surface charge of NPs increase their transport across the gastrointestinal epithelium. The optimized nanocarriers not only enhance the bioavailability of docked drugs but also their absorption, allowing for more effective insulin delivery [38]. The following factors largely influence drug release from NPs: pH, solubility, temperature, drug diffusion across the nanomaterial matrix, nanomaterial degradation, the drug incorporation process, and drug adsorption [39, 40]. In brief, targeted drug release relies mainly on the stimuli-responsive of the PNPs.
Takagi et al. [41] proposed the notion of stimuli-responsive material in 1990, which is about materials that respond optimally to changes in the environment while simultaneously performing their native function. According to the stimulus source, these materials may be classified as photo-responsive materials, thermal response materials, pH-responsive materials, electrically responsive materials, glucose-responsive materials, and so on. These materials have been widely employed in oil/water separation, biosensing, sustained-release drug delivery, "smart window," and so on in recent years. With each passing day, these materials are attracting the attention of an increasing number of scientists [42]. In addition, temperature-sensitive nanoparticles for insulin delivery were also of concern. Mahobia et al. [43] developed glucose and temperature-sensitive nanoparticles for insulin delivery. The released amount of insulin increased with increasing temperature from 18 to 37 ℃. However, once the drug has entered the body, it is difficult to control the temperature. The increased temperature can cause the degeneration of insulin, and somtimes, changes in temperature cannot lead to the release of oral insulin [44, 45].
pH-responsive insulin release
In fact, ionizable polymers (polyacids or polybases) are employed to produce the nanosystems, and their cargo is released because of changes in the ambient pH, which induce conformational and/or solubility changes in polymers, resulting in the decomposition or destabilization of these nanocarriers [23, 46, 47]. Since the gastrointestinal tract’s pH varies from highly acidic (1.2–3.0) to slightly alkaline (7.5–8.0) in the stomach and intestine, respectively, it might result in pH-induced insulin oxidation and deamination, which consequently disrupt its tertiary structure and therapeutic effect. Nanoparticles can safeguard pH-vulnerable drugs from the harsh ambient of the gastrointestinal tract and thereby improve the absorption of drugs inside the gut wall, facilitate cellular uptake by particular receptors, and regulate intracellular transport pathways [4].
The insulin-carrying nanovehicles must pass through the harsh environment of the gastrointestinal tract (GIT) to allow insulin to enter the bloodstream in the oral insulin delivery systems. As a result, nanocarriers employed in oral delivery systems to carry acid-labile insulin must be stable in gastric juice (pH = 1.2) and slowly discharge insulin in intestinal fluid (pH = 6.8). In the end, it permits insulin to enter the liver via the portal circulation and lower the blood glucose levels. There are several PNPs, including polysaccharides or protein-based NPs, COFs, and others, that have demonstrated pH-sensitive insulin release for diabetes therapy [31].
Asal et al. [24] manufactured and characterized the chitosan-based nanoparticles (ChNps) before using them to deliver insulin orally to diabetic patients. In an acidic medium, ChAuNps/PLGA demonstrated significant insulin retention (96 ± 0.08%). However, a large amount of insulin was released from ChAuNps/PLGA over an extended period at higher pH levels. Mukhopadhyay et al. [48] developed pH-sensitive chitosan-alginate core shell NPs for effective and safe oral insulin administration, which can encapsulate up to ∼ 85% insulin. The insulin pH sensitivity was illustrated through in-vitro release studies in which virtually all of the encapsulated insulin was retained in a simulated stomach buffer coupled with extended release in the model intestinal environment. An in-vivo investigation demonstrated the effectiveness of CS/ALG core–shell nanoparticles as nanocarriers in an oral insulin delivery system with a substantial hypoglycemic effect and an increase of 8.11% in insulin-relative bioavailability. There was no evidence of systemic toxicity following peroral administration, indicating that these NPs could be a promising device for potential oral insulin delivery. It’s worth noting that Yang et al. [49] developed ligand-switchable NPs (Pep/Gal-PNPs) in 2022. Once orally administered, the acidic environments trigger the extension of Pep from surface in a viruslike manner, enabling Pep/Gal-PNPs to traverse intestinal barriers efficiently. Subsequently, Gal is exposed by Pep folding at physiological pH, thereby allowing the specific targeting of Pep/Gal-PNPs to the liver.
pH and glucose dual responsive insulin release
It is critical to consider fluctuations in the pH of the GIT and the influence of blood glucose concentration on insulin release from NPs when developing oral insulin delivery systems for individuals with T1DM. Therefore, oral insulin delivery devices with dual sensitivity, like glucose and pH, would be extremely reliable. Generally, two approaches are employed to develop pH and glucose dual responsive devices: (i) either add glucose-sensitive substances (glucose oxidase (GOx), concanavalin-A, glucose binding proteins, and complex polymers of phenylboronic acid and polyol compounds) to the nanocarrier, or (ii) the nanocarrier itself has some glucose sensitivity.
Over the last few decades, many approaches for producing glucose-responsive stimuli-sensitive systems have been developed, including glucose oxidase (GOx) [50], concanavalin-A [51], glucose binding proteins [52] and complex polymers of phenylboronic acid and polyol compounds [53]. The glucose-responsive smart systems are particularly useful for patients with insulin-dependent diabetes mellitus since insulin discharge from them is controlled by blood glucose levels.
Jamwal et al. [54] developed a dextran-based glucose/pH-responsive insulin delivery system-glucose oxidase, which is clamped on acryloyl cross-aldehyde dextran NPs through the schiff base reaction, and enzymes on the NPs' surfaces hydrolyze glucose into gluconic acid, which resultantly decreases the pH of the medium and triggers the release of insulin by inducing degradation of the nanostructure. Xu et al. [55] fabricated a diabetes-specific oral delivery device by using ConA-INS-KGM NPs, which release insulin in response to different blood glucose levels. The NPs used in the development of this device were developed by cross linking konjac glucomannan (KGM) and concanavalin A (ConA).
Notably, Wei Tao et al. [56] developed an intelligent oral insulin platform based on glucose responsive polymeric nanoparticles (NPs). The NPs extended the therapeutic effect to up to 16 h in type I diabetic mice. This is the longest effective time among such types of oral insulin platforms reported to date and may reduce the frequency of insulin administration to once daily. This platform might be useful for the oral delivery of biologics in treating diabetes and related complications. In identical year, Benyettou et al. [22] manufactured imine-linked covalent organic framework (nCOF) nanostructures (TTA-DFP-nCOF) and exhibited a high bioavailability (24.1%) for oral delivery of insulin. The findings demonstrated that insulin release was minimal at pH = 2.0 and gradual at pH = 7.4. Notably, after 7.5 h of incubation, there was about 100% insulin release under hyperglycemic conditions displayed by diabetes patients (3 mg mL−1).
All in all, oral insulin release from NPs is mainly pH- and glucose-responsive. Table 1 shows the type of materials and their responsive conditions in different formulations.
PNPs for oral insulin delivery
The PNPs are oral drug delivery systems that are smaller than 100 nm in size, often ranging from 100 to 500 nm [65]. They are classified into two types: natural polymers and synthetic porous polymers.
Natural polymers
Natural polymers (polysaccharides, proteins, peptides, nucleic acids, and so on) offer several benefits, including biodegradability, biocompatibility, nontoxicity, and non-immunogenicity, for encapsulating and delivering active drug components [66, 67]. Natural polymer nanoparriers are biocompatible and biodegradable; therefore, they are regarded as the most promising material for setting up the novel oral insulin delivery systems [68, 69].
It has been discovered that approximately 800 different plant species have hypoglycemic potential, and that there are a variety of additional plant active compounds that can lower blood glucose levels. As a result, the employment of natural polymers with hypoglycemia potential in the production of nanovehicles will have a dual effect on the treatment of diabetic patients [70]. Among them, polysaccharide-based drug delivery systems (e.g. glucan, chitosan, pectin, alginate, hyaluronic acid (HA), starch, cellulose, pectin, etc.) and protein-based drug delivery systems (i.e. maize, keratin, whey protein, milk protein, albumin, casein, soy protein, histone, gelatin, pulse protein, etc.) have been extensively studied [37]. Until now, the FDA has licensed two oral insulin delivery systems (ORMD-0801 and HDV-I). They have not, however, been marketed due to the volatility of their toxicity and the various adverse effects of drugs in different clinical trials [71]. Hence, more research about the characterization of natural polymer nanoparticles is required.
Natural polysaccharide
Starch is a versatile, low-cost, and naturally occurring renewable biopolymer that contains amylose and amylopectin and may be employed in a variety of medical applications [72, 73]. Amylose is composed of α-D- (1–4) connected glucose units, whereas amylopectin is composed of the backbone of α-D- (1–4) joined glucose units and certain α-D- (1–6) linked branches [74] (Fig. 3a). Natural starch, on the other hand, has drawbacks like high digestibility and swelling index, high glycemic index, quick enzymatic breakdown in biological systems, and many others [75]. However, modified starch can alleviate some of the drawbacks associated with native starch. The modified starch derivatives (carboxymethyl short-chain amylose, cyclodextrin (CD), and others) have several potential therapeutic applications due to their low toxicity, high biocompatibility, and exceptional biodegradability [60]. Meneguin et al. [66] studied the employment of modified starch derivatives in oral insulin delivery systems. Yang et al. [61] on the other hand, produced carboxymethyl chitosan hydrogel-based carboxymethyl cyclodextrin-grafted microparticles for oral insulin delivery. The study's findings indicated that insulin was successfully retained by the hydrogel in the gastric environment and slowly released in the GIT. The smart polymeric hydrogel was created by EDC coupling NHS technique from precursor carboxymethyl chitosan (CMC) and carboxymethyl cyclodextrin (CMCD).
Chitosan (CS) is a non-toxic, cationic, linear, heteropolysaccharide derived from deacetylated chitin and composed of d-glucosamine and n-acetyl-d-glucosamine monomers linked by β-(1–4) glycosidic bonds [39, 76, 77]. The amino functional groups in CS play a vital role in regulating biochemistry and electrostatic interactions in nanodrug delivery systems, as well as offering solubility in slightly acidic solutions. [77, 78] (Fig. 3b). Chitosan's sticky properties and electrostatic attraction to negatively charged mucus are due to positively charged acetylglucosamine units [79]. CS is also biodegradable and cheap, making it an ideal polymer for oral drug delivery [80]. The current research has indicated that CS NPs are the best nanovehicles for oral administration of insulin to diabetic patients due to their perfect properties, such as biocompatibility, biodegradability, bioavailability, encapsulation rate, noncarcinogenicity, and nontoxicity.
Dextran is a branched chain homopolysachride composed of glucose monomers linked by α-1,6 glycosiside bonds and branched at positions α-1,2, α-1,3, and α-1,4 (Fig. 3c). The gluan-producing strains regulate the length and nature of branching units at positions 2, 3, and 4. Dextran is primarily synthesized from sucrose by numerous Lactobacillus species via glucan sucrase, which catalyzes the conversion of d-pyran glucose residues from sucrose to glucan [68]. Dextran, unlike other polysaccharides, is poorly degraded by regular amylases such as salivary amylase or malt amylase. Only dextranase in the lumen of the large intestine, liver, spleen, and kidney can depolymerize dextran [68, 81]. With these facts in mind, the dextran-based oral insulin delivery system will safeguard insulin against chemical and enzymatic degradation in the gastro-intestinal tract, as well as promote absorption by the intestinal epithelium, resulting in improved oral bioavailability [68]. The dextran ester, dextran ether, and dialdehyde dextran are the most prevalent dextran derivatives, with the latter being employed for oral insulin administration due to its exceptional properties.
Alibolandi et al. [59] developed an oral insulin delivery system based on the glucan-poly (propylene ester-hydroxyl-acetate copolymer) PLGA copolymer, which displayed sustained insulin release in a GIT simulation condition. Jamwal et al. recently developed a novel glucan-based glucose- and pH-responsive insulin delivery system [54], and its insulin release property as well as release kinetics under different pH mediums (AGF, pH 1.2, and AIF, pH 7.4) were studied using mathematical kinetic models. The insulin-loaded NPs were then tested in vitro for insulin release in response to various glucose concentrations.
Natural proteins
Proteins are one of the most significant natural biomaterials that are used to construct the novel nanovehicles because they display unique characteristics such as biodiversity, biodegradability, low immunogenicity, non-toxicity, and biocompatibility [82, 83]. Since protein-based nanovehicles possess a well-defined primary structure and can also be tailored by pre- or post-functionalization due to this property, different drugs, various components, and carriers can be integrated with hydrophobic or hydrophilic domains of proteins by using different reagents. Protein nanoparticles will also provide energy to the diabetic patient in addition to acting as insulin delivery vehicles [43]. Soy protein, albumin, transferrin, zein, keratin, and other proteins are exploited in the synthesis of nanopores, although transferrin, zein, and keratin have gained significant attention in the last decade as prospective multifunctional biopolymers [84].
Zein is a natural GRAS (Generally Recognized As Safe by the FDA) protein produced in maize that is not only extensively applied in the pharmaceutical industry but also in the production of polymer nanocarriers due to its safety, biodegradability, and nontoxicity. Furthermore, zein NPs have the potential to significantly enhance the oral bioavailability of small and large molecules. Inchaurraga et al. [62] developed naked zein NPs and polyethylene glycol-coated nanoparticles as oral insulin vehicles, which displayed bioavailability of 4.2% and 10.2%, respectively. The results of Inchaurraga et al. displayed that zein possess certain amount of insulin-carrying capacity. Bao et al. [63] developed insulin- and cholic acid-loaded zein NPs with dextran surfaces to increase insulin oral absorption in the GIT and the liver, the principal action organ of endogenous insulin. In type I diabetic mice, NPs showed an insulin loading efficiency of 74.6% and an oral pharmacological bioavailability of 12.5–20.5% [63].
Keratin is a structural protein present in mammals (hair, nails, skin, wool, hooves, and horns) and birds (bills and feathers) [83, 84]. Kunjiappan et al. [85] recently focused their research on the utilization of human hair keratin as carriers of indoloquinoxaline (INDX) derivatives for the treatment of type 2 diabetes mellitus. Indoloquinoxaline derivatives exhibited a variety of biological functions, including anti-diabetic potential, and the incorporation of keratin significantly increased their insulin encapsulation efficiency and substantially increased the release capacity. It has been demonstrated that keratin has the ability to load insulin. A large number of studies have shown that activation of adenosine monophosphate-activated protein kinase (AMPK) and suppression of the activity of protein tyrosine phosphatase 1B (PTP1B) are effective treatments for T2DM. Therefore, Ferroni et al. [83] formulated and manufactured INDX derivatives and incorporated keratin NPs using the dispersion method. The encapsulation efficiency and loading capacity of INDX into the keratin carrier were 89.9% and 11.9%, respectively. The results show that keratin is a promising choice for acting as a carrier for the oral insulin delivery system, but additional study is needed to validate it.
Transferrin (Tf) is a protein produced by the human body that regulates iron absorption and transportation by binding to TfR on epithelial cells. It is also resistant to chymotrypsin and tryptic digestion [23, 86]. Hence, when a large molecule of transferrin binds to a smaller molecule of insulin, it protects the insulin from digestive enzymes by preventing access to the insulin [87, 88]. Therefore, the use of Tf-modified NPs to guard insulin against GIT breakdown is crucial for oral insulin administration. Tf-coated polymeric NPs for oral insulin administration were developed by Zhu et al. and the surface-loaded Tf improved their transepithelial transport via receptor-mediated transcytosis.[89]. Nevertheless, these NPs showed poor release of insulin prior to transepithelial transport and limited their therapeutic bioavailability to ~ 7.8%. It is surprising that Wei Tao et al. [90] developed an oral hydrogel microbeads-mediated in situ synthesis of selenoproteins. We can start with the self-designed protein in vivo of PNPs that can survive the harsh environment of the gastrointestinal tract for oral insulin delivery. It can not only solve the disadvantage of natural protein that is easily degraded by gastrointestinal enzymes, but also solve the bio-safety of PNPs in vivo.
Synthetic porous polymers
The benefits of synthetic porous polymers (SPP) over natural polymers and other material types include the flexibility of producing polymeric materials and the potential of synthesizing this material according to pathology and patient demands [26]. The examples of SPP include charcoal activation, silica, porous coordination polymers (PCPs, including MOFs), porous organic polymers (POPs), and many others [91]. POPs are mostly composed of hyper-cross-linked polymers (HCPs), polymers with intrinsic microporosity (PIMs), conjugated microporous polymers (CMPs), porous aromatic frameworks (PAFs), covalent organic frameworks (COFs), and many more. POPs possess a distinct pore structure, variable pore size, tunable structure, and surface-modifiable characteristics [92].
The synthetic polymers MOFs [21] and COFs [22] have been shown to increase the bioavailability and delayed release of insulin in oral insulin administration systems [68, 93].
Activated charcoal
Activated charcoal has been shown in several studies that it prevents the obesity, metabolic syndrome, and a variety of other illnesses. Zhang et al. [93] discovered that combining acidic activated charcoal with an HFD reduced obesity in insulin resistance mice in a dose-dependent fashion However, because activated charcoal is often alkaline and can be influenced by gastric juice, it may not be able to protect insulin against pepsin breakdown. On the other hand, because activated charcoal is found in the form of powder, it is not digested and hence might affect the digestive tract [94].
Silica
Insulin can be administered orally using promising silica nanoparticles (SNs), particularly mesoporous silica nanoparticles (MSNs) due to their high biocompatibility, exceptional encapsulation efficiency, and controlled release, as well as appropriate loading processes [95]. Andreani et al. [64] synthesised SiNP and PEG-SiNP using the sol–gel technique and investigated them as insulin carriers. Later, Juère et al. [96] created dendritic mesopores of DMSNs in which insulin was effectively encapsulated, resulting in the prevention of insulin release in the stomach (pH = 1.2) and increased insulin transport to the intestine (pH = 7.4).
However, SNs have two major drawbacks: (i) poor epithelial membrane penetration, which has been greatly improved by necessary functionalization, and (ii) the complicated synthesis process involved in the production of SNs, which restricts their scale-up production. [95]. As a result, further research is required before using the silica nanoparticles in oral insulin administration.
PCPs
PCPs (including MOFs) are materials having an infinite network structure formed by the coordination bonding of metal nodes (metal ions or metal clusters) and organic linkers [97]. Contrary to traditional inorganic nanostructures, which are generally not biodegradable, many PCPs have intrinsic biodegradability and may be excreted by the kidneys without long-term retention in the body, reducing concerns about their possible long-term toxicity. It is evident that PCPs are a promising class of nanomaterials used in the field of nanomedicine [98], and some progress has already been made in employing MOFs in oral insulin delivery systems. It has been widely employed in major biomedical applications, including medication administration, biomedical imaging, and photodynamic therapy (PDT). It is important to mention here that ˃ 20,000 MOFs with various topologies have been registered [99,100,101]. These MOFs were produced using various synthetic techniques. Among these MOFs are IRMOFs (isoreticular metalorganic frameworks), ZIFs (zeolitic imidazolate frameworks), CPLs (coordination layered layers), MILs (materials of the Institute Lavoisier), UiOs (University of Oslo), and others [99,100,101,102].
Synthesis strategy and functionalization of MOFs
-
1.
Synthesis strategy of MOFs
MOFs are generally manufactured in a single step through the use of suitable metal salts, organic ligands, and solvents [103]. MOF synthesis was performed out at medium and low temperatures. In addition to solvothermal, reverse micro-emulsion, and template approaches, microwave, direct precipitation, and sonochemical (ultrasonic) technologies have recently been developed [104].
-
2.
Functionalization of MOFs
MOF functionalization can be divided into two types: pre-functionalization and post-synthetic modification (PSM) [105]. Pre-functionalization is the process of incorporating functional groups into the structure of MOFs prior to synthesis, which is accomplished by changing the organic ligand with specified substituents and then directly employing the changed ligand in the MOFs necessary for solvothermal synthesis (Fig. 4a). PSM is the method of adding new functional groups to a material after it has been synthesized, rather than on its molecular precursors (Fig. 4b). Hence, the compatibility between newly introduced functional group, reaction conditions, and final material produced through PSM is necessary. The incompatibility with the synthesis method must be avoided to generate the materials with distinct functionalization and structural stability. PSM offers an advantage over the pre-functionalization method due to better control over the type and number of functional groups added. As a result, when it is difficult to obtain MOFs of interest via the pre-functionalization method, this route is often taken for chemical modification. There are many kinds of post-synthetic modifications, including: covalent functionalization, coordinated covalent modification, surface functionalization, post-synthetic metalation, post-synthetic exchange, modification after coordination modification, dis-protection after synthesis, polymerization after synthesis, and cluster modification after synthesis.
Schematic diagrams of prefunctionalization and PSM of MOFs. a Pre-functionalization: Functional ligands are made by substituting the organic ligand with specified substituents and then directly incorporating the changed ligand into MOFs for functionalization. b PSM: Starting MOFs synthesized using unmodified organic ligands, which were then functionalized by adding new functional groups
Research progress in oral insulin delivery of MOFs
MOFs have many unique properties for drug delivery systems (DDS) when compared to traditional materials. MOFs, for example, not only have large porous surface areas that aid in drug or guest molecule loading efficiency, but they are also very easily functionalized due to their excellent biocompatibility, water solubility, and biodegradability, all of which improve drug bioavailability and efficiency in the body. Additionally, drugs may be chemically coupled or physically encapsulated within the carriers via a variety of interactions such as hydrogen bonds, Van der Waals forces, the π–π effect between aromatic rings, electrostatic interactions, coordination bonds, covalent bonds, and etc. The biomolecules are usually coupled to the MOFs via using different methods, such as surface attachment, covalent linkage, pore encapsulation, in situ encapsulation, forming bio-MOF (metal–biomolecule frameworks). The outstanding encapsulation capability of MOF makes it a one-of-a-kind platform for drug loading, therefore, several drugs, including DOX, 5-Fu (5-fluorouracil), β-estradiol, and insulin, have been delivered using this technique [106]. In recent years, the researchers have synthesized a variety of MOFs for of oral insulin delivery. Furthermore, several researchers conducted in vivo studies in mice and showed that MOFs have higher bioavailability in oral insulin administration.
Chen et al. [21] devised an acid-resistant Zr-based MOF (NU-1000) insulin delivery device with pores that interact well with insulin and disintegrate in the presence of phosphate ions (as in blood). In approximately 30 min, the NU-1000 was able to load 40% wt insulin via post-synthetic pore encapsulation process. In a simulated gastrointestinal environment, insulin-loaded NU-1000 was stable and rapidly released insulin under physiological settings (pH 7.0 in PBS). Zhou et al. created a polymer microsphere system that encapsulated insulin and SDS in MIL-100 [57]. The polymer coating of methoxy poly(ethylene glycol)-block poly(l-lactide) protected the MOF from degradation in the gastrointestinal environment, while SDS increased permeability through the intestinal membrane. The MIL-100 NP enhanced the endocytosis of insulin in monolayer Caco-2 cell culture and displayed excellent monolayer permeability. This oral delivery method, at 50 IU/kg, attained a maximal plasma insulin level (50 mIU/mL) at 4 h, and it remained higher for 8 h in a BALB/c mouse type I diabetes model. This system reduced glucose levels more slowly and for longer than subcutaneous injections. Moreover, the accumulation of insulin in the liver revealed that insulin discharged from the MOF moved through the portal veins to the liver and then to the cardiac tissue, closely resembling endogenous insulin circulation patterns. Rohra et al. demonstrated that the microfluidic synthesis of a metal–organic framework (MOF) (Ins-AuNPZIF-8) for insulin administration is based on the glucose stimulus response [58]. The insulin loading per unit weight of MOF was determined by using size exclusion chromatography and high-performance liquid chromatography, and the results were 77 and 88%, respectively, in the batch and microfluidic methods. The drug release experiments validated the MOFs’ response to glucose, which caused insulin release. This is the first work in which a SAR micromixer is used to synthesise MOFs, particularly ZIF-8, to encapsulate insulin and AuNPs. Simultaneously, Zou et al. encapsulated an adequate amount of insulin in acid-resistant metal–organic framework nanoparticles (UiO-68-NH2) and coated the exterior with targeting proteins (transferrin) to achieve very effective oral insulin administration [23]. The transferrin-coated nanoparticles efficiently crossed the intestinal epithelium and released the insulin under physiological settings, which resulted in a significant hypoglycemic response and 29.6% oral bioavailability.
The researchers have demonstrated that MOF nanoparticles can protect proteins from the degradative environment of the stomach and intestine, allowing them to be used in oral macromolecule delivery systems.
POPs
POPs offer higher surface areas and more controlled size distributions than traditional porous materials (such as charcoal activation, silica, and PCPs), making them appropriate for oral insulin administration systems.
The drug and the carrier are linked through weak interactions like van der Waals forces, hydrogen bonds, and hydrogen bond interactions [107,108,109]. POPs are mostly composed of hyper-cross-linked polymers (HCPs), polymers with intrinsic micro-porosity (PIMs), conjugated microporous polymers (CMPs), porous aromatic frameworks (PAFs), covalent organic frameworks (COFs), and other substances [91]. The COFs are very crystalline, whereas HCPs, PIMs, CMPs, and PAFs are amorphous [109]. The COFs, being a distinct class of porous materials with distinct properties, are regarded as having potential use in oral insulin delivery among POPs. The COFs are crystalline organic porous polymers made up of light elements such as C, H, O, N, and B that form covalent bond interactions via reversible reactions. COFs are low-density and high-surface-area nanomaterials that also have the following characteristics: customizable pore size, well-ordered internal structures, different topologies, and diverse monomer sources, which provide them with outstanding modifiability and a wide range of functions [110]. COFs materials have been extensively employed in adsorption and separation of biological macromolecules and gas [111,112,113,114,115,116,117,118], heterogeneous catalysis [119, 120], fluorescent sensing [121,122,123,124,125], proton / ion conduction [126, 127], accumulation energy [128, 129] and drug loading and release [130,131,132,133,134,135,136,137]. Côté et al. [138] designed and synthesized the first COFs from phenyl-di-borate [C6H4[B(OH)2]2 and hexa-hydroxyl-benzyl-benzene [C18H6(OH)6] with condensation reactions. Over the last decade, researchers have developed and synthesized a wide range of COFs and applied them to a variety of areas. COFs have gradually developed into an important class of POPs. On the basis of their topology, they are classified into two-dimensional (2D) and three-dimensional (3D) COFs, and based on different linking methods, they are divided into Boroxine, Boronate, Imine, Imide, Hydrazone, Azine, Triazine, Beta-ketoenamine, and so on.
Topological design of the COFs
Topological graphs are employed to design the COFs, which compress the knots and connectors of different geometries to form extended polygonal structures. However, different topological graphs are required for the designing of 2D and 3D COFs. The monomers can be classified into C1, C2, C3, C4, C6, and Td geometry based on their geometry, with Td geometry being required for the creation of 3D COFs [139].
Monomers having C1, C2, C3, C4, and C6 geometries are used to produce 2D COFs, whereas C2, C3, C4, and C6-symmetric monomers act as knots. The combination of [C2 + C2 + C2] (Fig. 5a) permits the construction of hexagonal 2D COFs in the self-condensation event, and this is mostly employed for the construction of boroxine and triazine-linked frameworks. The [C3 + C2] and [C3 + C3] (Fig. 5a) combinations yield hexagonal 2D COFs in two-component [1 + 1] poly-condensation systems with one knot and one linker, whereas [C4 + C2] and [C4 + C4] (Fig. 5b) pairings produce tetragonal 2D COFs. The [C2 + C2] (Fig. 5b) and [C6 + C2] (Fig. 5c) combinations yield rhombic and trigonal 2D COFs, while [C6 + C3] (Fig. 5c) produces multi-pore rhombic 2D COFs and [C2 + C2] (Fig. 5c) also form the dual-pore kagome-type 2D COFs. The knot unit with Td or orthogonal symmetry is essential to grow the backbones of 3D COFs in a 3D manner. However, various degrees of interpenetration are present in 3D COFs, including dia {[Td + C2] (Fig. 5d) and [Td + Td] (Fig. 5g)}, pts {[Td + C2] (Fig. 5e) and [Td + C4] (Fig. 5h)}, ctn {[Td + C3] (Fig. 5f)}, bor {[Td + C3] (Fig. 5f)}, srs {[Td + C3] (Fig. 5f)} and helical structures {[Td + C2] (Fig. 5i)}. The Figs. 5 and 6 describe the essential topological diagrams and building blocks for the construction of 2D and 3D COFs using Schiff-base chemistry.
Topology diagrams for designing 2D and 3D COFs to create skeletons and pores different. a) Hexagonal COFs formed either by self-condensation of C2-symmetric units or combination of C3-symmetric vertices and C2-/C3-symmetric units. b) Tetragonal COFs formed based on the C4+C2 topology or C4+C4 topology. Four-armed C2 vertices and linear C2 linkers lead to the single-pore rhombic shape. c) Trigonal COFs built by C6-symmetric knots and C2-symmetric linkers; multi-pore rhombic COFs constructed by C3-symmetric vertices and C6-symmetric units; dual-pore kagome topology constructed by four-armed C2 vertices and linear C2 linkers. The dia network formed by d) [Td + C2] or g) [Td + Td] diagrams. The pts network formed by e) [Td + C2] or h) [Td + C4] diagrams. The bor, ctn or srs network formed by f) [Td + C3] and the helix network formed by i) [Td + C2] diagrams
The topology diagram provides the principles for designing 2D and 3D COFs and provides a foundation for the COF field. A COF's structural diversity depends on its topology diagrams and building blocks.
Since the hexagonal topology diagram was developed, other shapes have been added, including tetragonal, rhombic, trigonal, and kagome. A large number of building blocks have been developed, ranging from simple arene to large π electron donors and acceptors, coordination sites, catalytic units, and spin systems. Linkages have also changed from non-conjugated to partially and fully conjugated. Moreover, the lattice was converted from isotropic to anisotropic. It is through these changes that the structural diversity of COFs is greatly enhanced, and the range of their properties, functions, and applications are greatly expanded [139].
Synthesis and functional regulation of COFs
-
1.
Synthesis of COFs
Solventothermal synthesis, microwave synthesis, interface synthesis, mechanical grinding synthesis, the sonochemical method, heating reflux synthesis, room-temperature synthesis (currently only for COFs with imine-linked -linked atoms), ionothermal synthesis, and other methods are used to create COFs. The solvent thermal approach is one of the most frequent and gentle procedures, although the synthesis period is lengthy, taking 2–7 days. As a result, developing moderate and short synthesis procedures is critical.
de la Peña Ruigómez et al. [140] developed a simple, quick, and efficient Schiff-base reaction through which RT-COF-1 was synthesized at room temperature from 1,3,5-Benzenetricarboxaldehyde (TFB) and 1,3,5-Tris(4-aminophenyl)benzene (TAPB) in the presence of acetic acid and inter-phenol, dimethyl sulfoxide (DMSO). Guan et al. [141] developed a technique for the synthesis of COFs that employed ionic liquids to produce 3D-IL-COF-1, 3D-IL-COF-2, and 3D-IL-COF-3. The 3D-IL-COF-1 was manufactured in ~ 3 min at ambient temperature and pressure, proving that COFs can be produced chemically.
-
2.
Functional regulation of COFs
The functions and features of COFs are generally lies in their pore structure and functional groups. The functionalization of materials may occur in three ways: bottom-up incorporation of functional moieties, in situ functionalization, and post-modification [142].
-
a.
Bottom-up incorporated functional moieties
This approach involves modifying the functional groups on the structural components prior to COF synthesis, because of which all functional groups are uniformly distributed in the COF framework and the number of active sites can be precisely regulated. When the modified functional groups on the structural units have a high steric hindrance then crystallization of the COFs decreases, but even it becomes difficult to perform.
-
b.
In situ functionalization
The in situ functionalization method is performed to incorporate the particular functional groups at specified locations on the structures of COFs during the condensation process. This method is relatively simple, but the applications of the COFs produced by it are limited.
-
c.
Postmodification
The post-modification process involves synthesising the initial framework of functional groups with reactivity as structural units and then grafting other types of functional groups into the pore tract. Although the synthesis of COFs by this method is simpler than that of bottom-up-incorporated functional moieties, the structure and porosity of these materials may be damaged during the modification process, and in addition, the quantity and distribution of active sites are difficult to manage.
As a result, it is critical that we develop moderate modification methods over the next decade.
Research progress in oral insulin delivery of COFs
COFs display a high drug loading capacity and high drug delivery efficiency, because of their unique characteristics, such as a high specific surface area, excellent crystallinity, a porous structure, and outstanding biocompatibility; consequently, they have extensive application possibilities in the field of drug delivery. The imine, imide, hydrazone, and triazine-type COFs are most commonly employed for drug delivery, but other types of COFs have also been used, such as phenazine linkage and olefin linkage. These COFs have a higher nitrogen content whose lone pair electrons are used to load drugs via hydrogen bonds or π−π bonds, and they significantly increase the drug-loading rate of COFs [143]. Fang et al. [130] developed two porous polyimide COFs (PI-COFs) in 2015 and used their large, uniform porosity and high stability to accomplish loading and controlled release of the model drug ibuprofen (IBU). This work is the first to demonstrate the use of COF materials in drug delivery. Their pioneering work has paved the way for the application of COFs to the field of drug delivery, and a number of additional functionalized COFs were developed to boost drug delivery efficiency in nanodrug delivery systems (NDDSs) [130,131,132,133,134,135,136,137, 144].
In 2016, two different nanoscale porous COFs were employed to load an anticancer drug (5-fluorouracil (5-FU)) by Bai et al. [145]. These drug loaded COFs showed good dispersibility in aqueous solution, high drug loading efficacy (the drug loading efficacy reached up to 30 wt%) and complete release in vitro. The same year, Vyas et al. [146] synthesised triazine COFs (TTI-COF) and used them for the quercetin uptake and release, highlighting the potential of COFs as nanocarriers. In 2017, Mitra et al. [147] modified TpASH by post-synthesis modification to yield folate conjugated CONs (TpASH-FA) for targeted drug delivery of anticancer drug 5-fluorouracil (5-FU) within the breast cancer cells MDA-MB-231. In 2018, Zhang et al. [148] developed a facile synthesis of a polymer-COF nanocomposite (denoted as PEG-CCM@APTES-COF-1) and targeted drug delivery of DOX. The results showed an enhanced tumor-inhibition effect was observed compared to the free DOX formulation. Wang et al. [149] prepared a style of pH-responsive COPs (THPP-BAE-PEG COPs), which can encapsulate anticancer drug doxorubicin (DOX) with the pH triggered drug release for chemotherapy. In 2020, Liu et al. [150] developed PEGylated redox-responsive nanoscale COFs (denoted F68@SS-COFs) for efficiently loading and delivering doxorubicin (DOX), showing a very high DOX-loading content (about 21%). In 2021, Anbazhagan et al. [151] designed a thioether-terminated triazole bridgecontaining COF (TCOF) for pH and glutathione S-transferase (GSH) dual-sensitive anticancer drug (DOX) delivery. Notably, almost 70%-80% of the loaded drug was released in 72 h of incubation.
Despite the fact that COFs have always been studied for drug delivery, it is probable that none of them have been used in oral insulin trials. Benyettou, et al. [22] presented an imine covalent organic framework (TTA-DFP-nCOF) that was first time used for the construction of oral insulin delivery systems in 2021. The triazine-based TTA-DFP-nCOF was chosen for its strong stability under harsh conditions, including acidic environments. This delivery system is distinguished by its excellent insulin-loading capacity (65 wt%), biocompatibility, bioavailability (24.1%), and insulin protection under severe circumstances, and hyperglycemia-induced drug release. The estimated pore size is roughly 1.7 nm, which is substantially smaller than insulin's molecular size (2.5–3 nm). As a result, it was concluded that insulin was intercalated between the layers of COF rather than deposited in the pores. The insulin orally delivered to the body is immediately absorbed by the intestinal epithelium and enters the liver via the portal vein, allowing glucose homeostasis to be maintained. Diabetes is known to induce damage to the liver and kidney, but no alterations were observed in these organs in TTA-DFP-nCOF/insulin-treated rats, demonstrating that the particles are harmless. Furthermore, it improved liver and kidney function, which suggested that COFs offer significant promise for oral insulin administration.
In conclusion, PNPs play a significant function as nanodrug carriers and show promising outcomes in the treatment of diabetes. Table 2 summarizes more important studies.
Conclusions and prospects
PNPs have significant potential for oral insulin administration. In recent years, many nanoparticle systems for oral insulin administration have been developed, including natural polymer nanocarriers and synthetic porous polymer nanocarriers. While some are promising, but their long-term efficacy in larger animals and humans must be proven. The majority of the better nanocarrier systems are made from natural small-molecular polymers, but their pore size cannot be controlled. As a result, future studies will focus on manufacturing methods for the synthesis of synthetic porous polymer nanoparticles. Prior to pre-clinical developments, oral insulin products have to be optimized in terms of encapsulation efficiency, loading capacity, gastrointestinal stability, bioavailability and bio-safety and intestinal permeation ability. However, no research has presently demonstrated that these barriers can be fully overcome and entered into clinical trials. This means that the clinical use of oral insulin is still a long way off.
In this review, we describe the controlled release techniques for oral insulin administration and explore the current oral insulin delivery applications of PNPs nanocarriers. Current PNPs production methods face various hurdles, including enhanced bioavailability and the biological stability of insulin in the GI tract. Few researchers have examined the bioavailability of MOFs for oral insulin administration among PNPs. As a result, future studies should explore the applicability of MOFs in humans by determining improvements in their bioavailability. MOF is a unique class of PNP, having porous materials with distinct properties and therefore being considered potential candidates for the construction of oral insulin delivery systems. COFs have a very good drug loading capacity and high drug delivery efficiency due to its unique properties, such as a wide surface area, easy crystallization, a porous structure, and outstanding biocompatibility. COFs as oral insulin carriers are currently being studied and have shown high loading capacity and bioavailability. We may start with the management of pore size design and interlayer space in COFs, then manufacture and precisely load 2.5–3.0 nm of insulin molecules in the pores or between layers to optimise oral insulin bioavailability in the future. We can begin by managing pore size and interlayer space in COFs, then produce and precisely load 2.5–3.0 nm of insulin molecules in the pores or between layers in the future to optimize the oral insulin delivery systems.
Availability of data and materials
Not applicable.
References
Sönmez M, Ficai D, Ficai A, Alexandrescu L, Georgescu M, Trusca R, Gurau D, Titu MA, Andronescu E. Applications of mesoporous silica in biosensing and controlled release of insulin. Int J Pharm. 2018;549(1–2):179–200.
Adler A, Bennett P, Colagiuri Chair S, Gregg E, Narayan KMV, Ines Schmidt M, Sobngwi E, Tajima N, Tandon N, Unwin N, et al. Reprint of: classification of diabetes mellitus. Diabetes Res Clin Pract. 2021;31:108972–108972.
Ouyang J, Zhang Z, Deng B, Liu J, Wang L, Liu H, Koo S, Chen S, Li Y, Yaremenko AV, et al. Oral drug delivery platforms for biomedical applications. Mater Today. 2023;62:296–326.
Zaiki Y, Lim LY, Wong TW. Critical material designs for mucus- and mucosa-penetrating oral insulin nanoparticle development. Int Mater. 2022;68(2):121–39.
Cao J, Li X, Tian H. Metal-organic framework (MOF)-based drug delivery. Curr Top Med Chem. 2020;27:5949–69.
Zhao S, Huang C, Yue X, Li X, Zhou P, Wu A, Chen C, Qu Y, Zhang C. Application advance of electrosprayed micro/nanoparticles based on natural or synthetic polymers for drug delivery system. Mater Des. 2022;220:110850.
Gedawy A, Martinez J, Al-Salami H, Dass CR. Oral insulin delivery: existing barriers and current counter-strategies. J Pharm Pharmacol. 2018;70(2):197–213.
Gowthamarajan K, Kulkarni GT. Oral insulin: fact or fiction? Resonance. 2003;8:38–46.
Jakoby J, Beuschlein F, Mentz S, Hantel C, Süss R. Liposomal doxorubicin for active targeting: surface modification of the nanocarrier evaluated in vitro and in vivo-challenges and prospects. Oncotarget. 2015;6(41):43698–711.
Mudassir J, Darwis Y, Muhamad S, Khan AA. Self-assembled insulin and nanogels polyelectrolyte complex (Ins/NGs-PEC) for oral insulin delivery: characterization, lyophilization and in-vivo evaluation. Int J Nanomed. 2019;14:4895–909.
Zhang Y, Xiong GM, Ali Y, Boehm BO, Huang YY, Venkatraman S. Layer-by-layer coated nanoliposomes for oral delivery of insulin. Nanoscale. 2021;13(2):776–89.
Vidal F, Guzman L. Dendrimer nanocarriers drug action: perspective for neuronal pharmacology. Neural Regen Res. 2015;10(7):1029–31.
da Silva SS, Igne Ferreira E, Giarolla J. Dendrimer prodrugs. Molecules. 2016;21(6):686.
Liu Z, Fan AC, Rakhra K, Sherlock S, Goodwin A, Chen X, Yang Q, Felsher DW, Dai H. Supramolecular stacking of doxorubicin on carbon nanotubes for in vivo cancer therapy. Angew Chem Int Edit. 2009;48(41):7668–72.
Peretz S, Regev O. Carbon nanotubes as nanocarriers in medicine. Curr Opin Colloid In. 2012;17(6):360–8.
Lim YT, Kim S, Nakayama A, Stott NE, Bawendi MG, Frangioni JV. Selection of quantum dot wavelengths for biomedical assays and imaging. Mol Imaging. 2003;2(1):50–64.
Zhao MX, Zeng EZ, Zhu BJ. The biological applications of inorganic nanoparticle drug carriers. Chemnanomat. 2015;1(2):82–91.
You J, Zhang G, Li C. Exceptionally high payload of doxorubicin in hollow gold nanospheres for near-infrared light-triggered drug release. ACS Nano. 2010;4(2):1033–41.
You J, Zhang R, Zhang G, Zhong M, Liu Y, Van Pelt CS, Liang D, Wei W, Sood AK, Li C. Photothermal-chemotherapy with doxorubicin-loaded hollow gold nanospheres: a platform for near-infrared light-trigged drug release. J Control Release. 2012;158(2):319–28.
Butterfield JT, Kim H, Knauer DJ, Nevala WK, Markovic SN. Identification of a peptide-peptide binding motif in the coating of nab-paclitaxel nanoparticles with clinical antibodies: bevacizumab, rituximab, and trastuzumab. Sci Rep. 2017;7:14476.
Chen Y, Li P, Modica JA, Drout RJ, Farha OK. Acid-resistant mesoporous metal-organic framework toward oral insulin delivery: protein encapsulation, protection, and release. J Am Chem Soc. 2018;140(17):5678–81.
Benyettou F, Kaddour N, Prakasam T, Das G, Sharma SK, Thomas SA, Bekhti-Sari F, Whelan J, Alkhalifah MA, Khair M, et al. In vivo oral insulin delivery via covalent organic frameworks. Chem Sci. 2021;12(17):6037–47.
Zou JJ, Wei G, Xiong C, Yu Y, Li S, Hu L, Ma S, Tian J. Efficient oral insulin delivery enabled by transferrin-coated acid-resistant metal-organic framework nanoparticles. Sci Adv. 2022;8(8):eabm4677.
Asal HA, Shoueir KR, El-Hagrasy MA, Toson EA. Controlled synthesis of in-situ gold nanoparticles onto chitosan functionalized PLGA nanoparticles for oral insulin delivery. Int J Biol Macromol. 2022;209:2188–96.
Mura S, Nicolas J, Couvreur P. Stimuli-responsive nanocarriers for drug delivery. Nat Mater. 2013;12(11):991–1003.
Rizvi SAA, Saleh AM. Applications of nanoparticle systems in drug delivery technology. Saudi Pharm J. 2018;26:64–70.
de Karine Cappuccio C, Josiel Martins C, Maria Gabriela C. Drug-loaded polymeric nanoparticles: a review. Int J Polym Mater. 2022;71:1–13.
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, Stein C, Basit A, Chan JCN, Mbanya JC, et al. IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;204:110945.
Yan HB, Zhang YQ, Ma YL, Zhou LX. Biosynthesis of insulin-silk fibroin nanoparticles conjugates and in vitro evaluation of a drug delivery system. J Nanopart Res. 2008;11(8):1937–46.
Fu Z, Gilbert ER, Liu D. Regulation of insulin synthesis and secretion and pancreatic beta-cell dysfunction in diabetes. Curr Diabetes Rev. 2013;9(1):25–53.
Singh N, Son S, An J, Kim I, Choi M, Kong N, Tao W, Kim JS. Nanoscale porous organic polymers for drug delivery and advanced cancer theranostics. Chem Soc Rev. 2021;50(23):12883–96.
Bochicchio S, Dalmoro A, Barba AA, d’Amore M, Lamberti G. New preparative approaches for micro and nano drug delivery carriers. Curr Drug Deliv. 2016;14(2):203–15.
Davoodi P, Lee LY, Xu Q, Sunil V, Sun Y, Soh S, Wang CH. Drug delivery systems for programmed and on-demand release. Adv Drug Deliver Rev. 2018;132:104–38.
Patra JK, Das G, Fraceto LF, Campos EVR, Rodriguez-Torres MDP, Acosta-Torres LS, Diaz-Torres LA, Grillo R, Swamy MK, Sharma S, et al. Nano based drug delivery systems: recent developments and future prospects. J Nanobiotechnol. 2018;16:71.
Singh R, Lillard JW. Nanoparticle-based targeted drug delivery. Exp Mol Pathol. 2009;86(3):215–23.
Roger E, Lagarce F, Garcion E, Benoit JP. Biopharmaceutical parameters to consider in order to alter the fate of nanocarriers after oral delivery. Nanomedicine. 2010;5(2):287–306.
Panigrahy SK, Kumar A. Biopolymeric nanocarrier: an auspicious system for oral delivery of insulin. J Biomat Sci-Polym E. 2022;33(16):2145–64.
Son GH, Lee BJ, Cho CW. Mechanisms of drug release from advanced drug formulations such as polymeric-based drug-delivery systems and lipid nanoparticles. J Pharm Investig. 2017;47(4):287–96.
Abdel-Moneim A, Ramadan H. Novel strategies to oral delivery of insulin: current progress of nanocarriers for diabetes management. Drug Develop Res. 2021;83(2):301–16.
Soppimath KS, Aminabhavi TM, Kulkarni AR, Rudzinski WE. Biodegradable polymeric nanoparticles as drug delivery devices. J Control Release. 2001;70(1–2):1–20.
Takagi T. A concept of intelligent materials. J Intel Mat Syst Str. 1990;1:149–56.
Alarcón CDH, Pennadam S, Alexander C. Stimuli responsive polymers for biomedical applications. Chem Soc Rev. 2005;34(3):276–85.
Mahobia S, Bajpai J, Bajpai AK. Soya protein as possible potential nanocarriers for in-vitro oral delivery of insulin in simulated gastric fluids (SGFs). Int J Polym Mater. 2017;67(6):340–50.
Torchilin VP. Multifunctional, stimuli-sensitive nanoparticulate systems for drug delivery. Nat Rev Drug Discov. 2014;13(11):813–27.
Danhier F, Feron O, Préat V. To exploit the tumor microenvironment: passive and active tumor targeting of nanocarriers for anti-cancer drug delivery. J Control Release. 2010;148(2):135–6.
Lee ES, Shin HJ, Na K, Bae YH. Poly(l-histidine)-PEG block copolymer micelles and pH-induced destabilization. J Control Release. 2003;90(3):363–74.
Lu C, Urban MW. Stimuli-responsive polymer nano-science: shape anisotropy, responsiveness, applications. Prog Polym Sci. 2018;78:24–46.
Mukhopadhyay P, Chakraborty S, Bhattacharya S, Mishra R, Kundu PP. pH-sensitive chitosan/alginate core-shell nanoparticles for efficient and safe oral insulin delivery. Int J Biol Macromol. 2015;72:640–8.
Yang T, Wang A, Nie D, Fan W, Jiang X, Yu M, Guo S, Zhu C, Wei G, Gan Y. Ligand-switchable nanoparticles resembling viral surface for sequential drug delivery and improved oral insulin therapy. Nat Commun. 2022;13(1):6649.
Qi W, Yan X, Duan L, Cui Y, Yang Y, Li J. Glucose-sensitive microcapsules from glutaraldehyde cross-linked hemoglobin and glucose oxidase. Biomacromol. 2009;10(5):1212–6.
Sahota T, Tomlins P, Taylor MJ. Long-term stability of glucose responsive dextran methacrylate-concanavalin a methacrylamide gels as part of an implantable artificial pancreas. Int J Polym Mater. 2015;64(18):946–54.
Ehrick JD, Luckett MR, Khatwani S, Wei Y, Deo SK, Bachas LG, Daunert S. Glucose responsive hydrogel networks based on protein recognition. Macromol Biosci. 2009;9(9):864–8.
Wu JZ, Williams GR, Li HY, Wang D, Wu H, Li SD, Zhu LM. Glucose- and temperature-sensitive nanoparticles for insulin delivery. Int J Nanomed. 2017;12:4037–57.
Jamwal S, Ram B, Ranote S, Dharela R, Chauhan GS. New glucose oxidase-immobilized stimuli-responsive dextran nanoparticles for insulin delivery. Int J Biol Macromol. 2018;123:968–78.
Xu M, Huang J, Jiang S, He J, Wang Z, Qin H, Guan YQ. Glucose sensitive konjac glucomannan/concanavalin A nanoparticles as oral insulin delivery system. Int J Biol Macromol. 2022;202:296–308.
Yufen X, Zhongmin T, Xiangang H, John J, Wei C, Chuang L, Jun Z, Na K, Nitin J, Jianzhong D, et al. Glucose-responsive oral insulin delivery platform for one treatment a day in diabetes. Matter. 2021;4(10):3269–85.
Wang Y, Yan J, Wen N, Xiong H, Cai S, He Q, Hu Y, Peng D, Liu Z, Liu Y. Metal-organic frameworks for stimuli-responsive drug delivery. Biomaterials. 2019;230:119619.
Zhou Y, Liu L, Cao Y, Yu S, He C, Chen X. A nanocomposite vehicle based on metal-organic framework nanoparticle incorporated biodegradable microspheres for enhanced oral insulin delivery. ACS Appl Mater Interfaces. 2020;12(20):22581–92.
Alibolandi M, Alabdollah F, Sadeghi F, Mohammadi M, Abnous K, Ramezani M, Hadizadeh F. Dextran-b-poly(lactide-co-glycolide) polymersome for oral delivery of insulin: in vitro and in vivo evaluation. J Control Release. 2016;227:58–70.
Mahkam M. Starch-based polymeric carriers for oral-insulin delivery. J Biomed Mater Res A. 2009;92A(4):1392–7.
Yang Y, Liu Y, Chen S, Cheong KL, Teng B. Carboxymethyl β-cyclodextrin grafted carboxymethyl chitosan hydrogel-based microparticles for oral insulin delivery. Carbohyd Polym. 2020;246:116617.
Inchaurraga L, Martínez-López AL, Martin-Arbella N, Irache JM. Zein-based nanoparticles for the oral delivery of insulin. Drug Deliv Transl Re. 2020;10(6):1601–11.
Bao X, Qian K, Yao P. Insulin- and cholic acid-loaded zein/casein-dextran nanoparticles enhance the oral absorption and hypoglycemic effect of insulin. J Mater Chem B. 2021;9(31):6234–45.
Andreani T, de Souza ALR, Kiill CP, Lorenzón EN, Fangueiro JF, Calpena AC, Chaud MV, Garcia ML, Gremião MPD, Silva AM, et al. Preparation and characterization of PEG-coated silica nanoparticles for oral insulin delivery. Int J Pharm. 2014;473(1–2):627–35.
Lohcharoenkal W, Wang L, Chen YC, Rojanasakul Y. Protein nanoparticles as drug delivery carriers for cancer therapy. Biomed Res Int. 2014;2014:180549.
Chowdhury A, Kunjiappan S, Panneerselvam T, Somasundaram B, Bhattacharjee C. Nanotechnology and nanocarrier-based approaches on treatment of degenerative diseases. Int Nano Lett. 2017;7(2):91–122.
Meneguin AB, Silvestre ALP, Sposito L, de Souza MPC, Sábio RM, Araújo VHS, Cury BSF, Chorilli M. The role of polysaccharides from natural resources to design oral insulin micro- and nanoparticles intended for the treatment of diabetes mellitus: a review. Carbohyd Polym. 2020;256:117504.
Hu Q, Lu Y, Luo Y. Recent advances in dextran-based drug delivery systems: from fabrication strategies to applications. Carbohyd Polym. 2021;264:117999.
Esrafili A, Wagner A, Inamdar S, Acharya AP. Covalent organic frameworks for biomedical applications. Adv Healthc Mater. 2021;10(6):2002090.
Li WL, Zheng HC, Bukuru J, De Kimpe N. Natural medicines used in the traditional Chinese medical system for therapy of diabetes mellitus. J Ethnopharmacol. 2004;92(1):1–21.
Moroz E, Matoori S, Leroux JC. Oral delivery of macromolecular drugs: where we are after almost 100 years of attempts. Adv Drug Deliv Rev. 2016;101:108–21.
Compart J, Li X, Fettke J. Starch-A complex and undeciphered biopolymer. J Plant Physiol. 2021;258:153389.
Garcia MAVT, Garcia CF, Faraco AAG. Pharmaceutical and biomedical applications of native and modified starch: a review. Starke. 2020;72(7–8):1900270.
Zhu F. Relationships between amylopectin internal molecular structure and physicochemical properties of starch. Trends Food Sci Tech. 2018;78:234–42.
Bhatt P, Kumar V, Goel R, Sharma SK, Kaushik S, Sharma S, Shrivastava A, Tesema M. Structural modifications and strategies for native starch for applications in advanced drug delivery. Biomed Res Int. 2022;2022:2188940.
Bhatt P, Kumar V, Goel R, Sharma SK, Kaushik S, Sharma S, Shrivastava A, Tesema M. Chitosan/iota-carrageenan and chitosan/pectin polyelectrolyte multilayer scaffolds with antiadhesive and bactericidal properties. Appl Surf Sci. 2020;502:144282.
Qiu A, Wang Y, Zhang G, Wang H. Natural polysaccharide-based nanodrug delivery systems for treatment of diabetes. Polymers. 2022;14(15):3217.
Simsek M, Asiyanbi-Hammed TT, Rasaq N, Hammed AM. Progress in bioactive polysaccharide-derivatives: a review. Food Rev Int. 2021;39(3):1612–27.
Mohammed MA, Syeda JTM, Wasan KM, Wasan EK. An overview of chitosan nanoparticles and its application in non-parenteral drug delivery. Pharmaceutics. 2017;9(4):53–79.
Ways TMM, Lau WM, Khutoryanskiy VV. Chitosan and its derivatives for application in mucoadhesive drug delivery systems. Polymers. 2018;10(3):267–304.
Shingel KI. Current knowledge on biosynthesis, biological activity, and chemical modification of the exopolysaccharide, pullulan. Carbohyd Res. 2004;339(3):447–60.
Varanko A, Saha S, Chilkoti A. Recent trends in protein and peptide-based biomaterials for advanced drug delivery. Adv Drug Deliv Rev. 2020;156:133–87.
Ferroni C, Varchi G. Keratin-based nanoparticles as drug delivery carriers. Appl Sci. 2021;11(20):9417.
Chaitanya Reddy C, Khilji IA, Gupta A, Bhuyar P, Mahmood S, Saeed Al-Japairai KA, Chua GK. Valorization of keratin waste biomass and its potential applications. J Water Process Eng. 2021;40:101707.
Kunjiappan S, Theivendren P, Pavadai P, Govindaraj S, Sankaranarayanan M, Somasundaram B, Arunachalam S, Ram Kumar Pandian S, Ammunje DN. Design and in silico modeling of indoloquinoxaline incorporated keratin nanoparticles for modulation of glucose metabolism in 3T3-L1 adipocytes. Biotechnol Progr. 2019;36(1):1–14.
Banerjee D, Flanagan PR, Cluett J, Valberg LS. Transferrin receptors in the human gastrointestinal-tract-relationship to body iron stores. Gastroenterology. 1986;91(4):861–9.
Xia CQ, Wang J, Shen WC. Hypoglycemic effect of insulin-transferrin conjugate in streptozotocin-induced diabetic rats. J Pharmacol Exp Ther. 2000;295(2):594–600.
Kavimandan NJ, Losi E, Peppas NA. Novel delivery system based on complexation hydrogels as delivery vehicles for insulin-transferrin conjugates. Biomaterials. 2006;27(20):3846–54.
Zhu X, Wu J, Shan W, Tao W, Zhao L, Lim J-M, D’Ortenzio M, Karnik R, Huang Y, Shi J, et al. Polymeric nanoparticles amenable to simultaneous installation of exterior targeting and interior therapeutic proteins. Angew Chemie. 2016;55(10):3309–12.
Ouyang J, Deng B, Zou B, Li Y, Bu Q, Tian Y, Chen M, Chen W, Kong N, Chen T, et al. Oral hydrogel microbeads-mediated in situ synthesis of selenoproteins for regulating intestinal immunity and microbiota. J Am Chem Soc. 2023;145(22):12193–205.
Wu D, Xu F, Sun B, Fu R, He H, Matyjaszewski K. Design and preparation of porous polymers. Chem Rev. 2012;112(7):3959–4015.
Kakkar A, Traverso G, Farokhzad OC, Weissleder R, Langer R. Evolution of macromolecular complexity in drug delivery systems. Nat Rev Chem. 2017;1(8):63–80.
Zhang X, Diao P, Yokoyama H, Inoue Y, Tanabe K, Wang X, Hayashi C, Yokoyama T, Zhang Z, Hu X, et al. Acidic activated charcoal prevents obesity and insulin resistance in high-fat diet-fed mice. Front Nutr. 2022;9:1–16.
Huber M, Pohl W, Reinisch G, Attems J, Pescosta S, Lintner F. Lung disease 35 years after aspiration of activated charcoal in combination with pulmonary lymphangioleiomyomatosis: a histological and clinicopathological study with scanning electron microscopic evaluation and element analysis. Virchows Arch. 2006;449(2):225–9.
Tan X, Liu X, Zhang Y, Zhang H, Lin X, Pu C, Gou J, He H, Yin T, Zhang Y, et al. Silica nanoparticles on the oral delivery of insulin. Expert Opin Drug Del. 2018;15(8):805–20.
Juere E, Caillard R, Marko D, Del Favero G, Kleitz F. Smart protein-based formulation of dendritic mesoporous silica nanoparticles: toward oral delivery of insulin. Chem-Eur J. 2020;26(23):5195–9.
Qian BB, et al. Porous coordination polymers: development and research progress. Sci China Chem. 2019;49:212837231.
Zhao J, Yang Y, Han X, Liang C, Liu J, Song X, Ge Z, Liu Z. Redox-sensitive nanoscale coordination polymers for drug delivery and cancer theranostics. ACS Appl Mater Interfaces. 2017;9(28):23555–63.
Zhao Y, Deng DS, Ma LF, Ji BM, Wang LY. A new copper-based metal-organic framework as a promising heterogeneous catalyst for chemo- and regio-selective enamination of beta-ketoesters. Chem Commun. 2013;49(87):10299–301.
Shen X, Pan Y, Sun Z, Liu D, Xu H, Yu Q, Trivedi M, Kumar A, Chen J, Liu J. Design of metal-organic frameworks for pH-responsive drug delivery application. Mini-Rev Med Chem. 2019;19(20):1644–65.
Cai H, Huang YL, Li D. Biological metal-organic frameworks: structures, host-guest chemistry and bio-applications. Coordin Chem Rev. 2017;378:207–21.
Fu HR, Wang N, Qin JH, Han ML, Ma LF, Wang F. Spatial confinement of a cationic MOF: a SC-SC approach for high capacity Cr (vi)-oxyanion capture in aqueous solution. Chem Commun. 2018;54(82):11645–8.
Yang X, Yuan S, Zou L, Drake H, Zhang Y, Qin J, Alsalme A, Zhou HC. One-step synthesis of hybrid core-shell metal-organic frameworks. Angew Chem Int Edit. 2018;57(15):3927–32.
Guan HY, LeBlanc RJ, Xie SY, Yue Y. Recent progress in the syntheses of mesoporous metal-organic framework materials. Coordin Chem Rev. 2018;369:76–90.
Sun Z, Wu S, Ma J, Shi H, Wang L, Sheng A, Yin T, Sun L, Li G. Colorimetric sensor array for human semen identification designed by coupling zirconium metal-organic frameworks with DNA-modified gold nanoparticles. ACS Appl Mater Interfaces. 2019;11(40):36316–23.
Rohra N, Gaikwad G, Dandekar P, Jain R. Microfluidic Synthesis of a bioactive metal-organic framework for glucose-responsive insulin delivery. ACS Appl Mater Interfaces. 2022;14(6):8251–65.
Mal A, Ding H, Li M, Li W, Wang C. Covalent organic frameworks with nanopores for biological applications: a review. ACS Appl Nano Mater. 2022;5(10):13972–84.
Wang H, Zhu W, Feng L, Chen Q, Chao Y, Dong Z, Liu Z. Nanoscale covalent organic polymers as a biodegradable nanomedicine for chemotherapy-enhanced photodynamic therapy of cancer. Nano Res. 2017;11(6):3244–57.
Tang Y, Varyambath A, Ding Y, Chen B, Huang X, Zhang Y, Yu DG, Kim I, Song W. Porous organic polymers for drug delivery: hierarchical pore structures, variable morphologies, and biological properties. Biomater Sci. 2022;10(19):5369–90.
Singh Y, Meher JG, Raval K, Khan FA, Chaurasia M, Jain NK, Chourasia MK. Nanoemulsion: concepts, development and applications in drug delivery. J Control Release. 2017;252:28–49.
Li H, Ding J, Guan X, Chen F, Li C, Zhu L, Xue M, Yuan D, Valtchev V, Yan Y, et al. Three-dimensional large-pore covalent organic framework with stp topology. J Am Chem Soc. 2020;142(31):13334–8.
Du Y, Yang H, Whiteley JM, Wan S, Jin Y, Lee SH, Zhang W. Ionic covalent organic frameworks with spiroborate linkage. Angew Chem. 2015;55(5):1737–41.
Park K, Lee K, Kim H, Ganesan V, Cho K, Jeong SK, Yoon S. Preparation of covalent triazine frameworks with imidazolium cations embedded in basic sites and their application for CO2 capture. J Mater Chem A. 2017;5(18):8576–82.
Cheng Y, Zhai L, Tong M, Kundu T, Liu G, Ying Y, Dong J, Wang Y, Zhao D. Selective gas permeation in mixed matrix membranes accelerated by hollow ionic covalent organic polymers. ACS Sustain Chem Eng. 2018;7(1):1564–73.
Maurya M, Singh JK. Effect of ionic liquid impregnation in highly water-stable metal-organic frameworks, covalent organic frameworks, and carbon-based adsorbents for post-combustion flue gas treatment. Energy Fuels. 2019;33:3421–8.
Ying Y, Tong M, Ning S, Ravi SK, Peh SB, Tan SC, Pennycook SJ, Zhao D. Ultrathin two-dimensional membranes assembled by ionic covalent organic nanosheets with reduced apertures for gas separation. J Am Chem Soc. 2020;142(9):4472–80.
van der Jagt R, Vasileiadis A, Veldhuizen H, Shao P, Feng X, Ganapathy S, Habisreutinger NC, van der Veen MA, Wang C, Wagemaker M, et al. Synthesis and structure-property relationships of polyimide covalent organic frameworks for carbon dioxide capture and (aqueous) sodium-ion batteries. Chem Mater. 2021;33(3):818–33.
Jin F, Lin E, Wang T, Geng S, Wang T, Liu W, Xiong F, Wang Z, Chen Y, Cheng P, et al. Bottom-up synthesis of 8-connected three-dimensional covalent organic frameworks for highly efficient ethylene/ethane separation. J Am Chem Soc. 2022;144(12):5643–52.
Wu Y, Xu H, Chen X, Gao J, Jiang D. A π-electronic covalent organic framework catalyst: π-walls as catalytic beds for Diels-Alder reactions under ambient conditions. Chem Commun. 2015;51(50):10096–8.
Liu M, Jiang K, Ding X, Wang S, Zhang C, Liu J, Zhan Z, Cheng G, Li B, Chen H, et al. Controlling monomer feeding rate to achieve highly crystalline covalent triazine frameworks. Adv Mater. 2019;31(19):1–7.
Mal A, Mishra RK, Praveen VK, Khayum MA, Banerjee R, Ajayaghosh A. Supramolecular reassembly of self-exfoliated ionic covalent organic nanosheets for label-free detection of double-stranded DNA. Angew Chem Int Edit. 2018;57(28):8443–7.
Zuo H, Li Y, Liao Y. Europium ionic liquid grafted covalent organic framework with dual luminescence emissions as sensitive and selective acetone sensor. ACS Appl Mater Interfaces. 2019;11(42):39201–8.
Singh H, Devi M, Jena N, Iqbal MM, Nailwal Y, De Sarkar A, Pal SK. Proton-triggered fluorescence switching in self-exfoliated ionic covalent organic nanosheets for applications in selective detection of anions. ACS Appl Mater Interfaces. 2020;12(11):13248–55.
Jiang W, Zhao Y, Zhang D, Zhu X, Liu H, Sun B. Efficient and robust dual modes of fluorescence sensing and smartphone readout for the detection of pyrethroids using artificial receptors bound inside a covalent organic framework. Biosens Bioelectron. 2021;194:113582.
Zhao L, Liang X, Ni Z, Zhao H, Ge B, Li W. Covalent organic framework modified polyacrylamide electrospun nanofiber membrane as a “turn-on” fluorescent sensor for primary aliphatic amine gas. Sensor Actuat B-Chem. 2022;366:131988.
Liu L, Yin L, Cheng D, Zhao S, Zang HY, Zhang N, Zhu G. Surface-mediated construction of an ultrathin free-standing covalent organic framework membrane for efficient proton conduction. Angew Chem Int Edit. 2021;60(27):14875–80.
Wang X, Shi B, Yang H, Guan J, Liang X, Fan C, You X, Wang Y, Zhang Z, Wu H, et al. Assembling covalent organic framework membranes with superior ion exchange capacity. Nat Commun. 2022;13(1):1020–9.
Liang X, Tian Y, Yuan Y, Kim Y. Ionic covalent organic frameworks for energy devices. Adv Mater. 2021;33(52):2105647.
Zou J, Fan K, Chen Y, Hu W, Wang C. Perspectives of ionic covalent organic frameworks for rechargeable batteries. Coordin Chem Rev. 2022;458:214431.
Fang Q, Wang J, Gu S, Kaspar RB, Zhuang Z, Zheng J, Guo H, Qiu S, Yan Y. 3D porous crystalline polyimide covalent organic frameworks for drug delivery. J Am Chem Soc. 2015;137(26):8352–5.
Zhang G, Ji Y, Li X, Wang X, Song M, Gou H, Gao S, Jia X. Polymer-covalent organic frameworks composites for glucose and pH dual-responsive insulin delivery in mice. Adv Healthc Mater. 2020;9(14):2000221.
Ghosh P, Banerjee P. Drug delivery using biocompatible covalent organic frameworks (COFs) towards a therapeutic approach. Chem Commun. 2023;59(84):12527–47.
Zhao Y, Das S, Sekine T, Mabuchi H, Irie T, Sakai J, Wen D, Zhu W, Ben T, Negishi Y. Record ultralarge-pores, low density three-dimensional covalent organic framework for controlled drug delivery. Angew Chem Int Edit. 2023;62(13):e202300172.
Ge L, Qiao C, Tang Y, Zhang X, Jiang X. Light-activated hypoxia-sensitive covalent organic framework for tandem-responsive drug delivery. Nano Lett. 2021;21(7):3218–24.
Das S, Sekine T, Mabuchi H, Irie T, Sakai J, Zhao Y, Fang Q, Negishi Y. Three-dimensional covalent organic framework with scu-c topology for drug delivery br. ACS Appl Mater Interfaces. 2022;14(42):48045–51.
Jia Y, Zhang L, He B, Lin Y, Wang J, Li M. 8-Hydroxyquinoline functionalized covalent organic framework as a pH sensitive carrier for drug delivery. Mat Sci Eng C-Mater. 2020;117:111243.
Zhao K, Gong P, Song S, Li J, Peng J, Wang Y, Qi C, Wang D, Liu Z. Size-controllable covalent organic frameworks with high NIR absorption for targeted delivery of glucose oxidase. J Mol Liq. 2022;346:117896.
Côté AP, Benin AI, Ockwig NW, O’Keeffe M, Matzger AJ, Yaghi OM. Porous, crystalline, covalent organic frameworks. Science. 2005;310(5751):1166–70.
Liu R, Tan KT, Gong Y, Chen Y, Li Z, Xie S, He T, Lu Z, Yang H, Jiang D. Covalent organic frameworks: an ideal platform for designing ordered materials and advanced applications. Chem Soc Rev. 2020;50(1):120–242.
de la Pena RA, Rodriguez-San-Miguel D, Stylianou KC, Cavallini M, Gentili D, Liscio F, Milita S, Maria Roscioni O, Luisa Ruiz-Gonzalez M, Carbonell C, et al. Direct on-surface patterning of a crystalline laminar covalent organic framework synthesized at room temperature. Chem-Eur J. 2015;21(30):10666–70.
Guan X, Ma Y, Li H, Yusran Y, Xue M, Fang Q, Yan Y, Valtchev V, Qiu S. Fast, ambient temperature and pressure ionothermal synthesis of three-dimensional covalent organic frameworks. J Am Chem Soc. 2018;140(13):4494–8.
Zhao W, Yu C, Zhao J, Chen F, Guan X, Li H, Tang B, Yu G, Valtchev V, Yan Y, et al. 3D Hydrazone-functionalized covalent organic frameworks as pH-triggered rotary switches. Small. 2021;17(41):202102630.
Zou J, Ren X, Tan L, Huang Z, Gou L, Meng X. Preparation and properties of covalent organic framework nanoparticles with high drug loading. Front Mater Sci. 2021;15(3):465–70.
Wang Y, Sun X, Wang Y. Synthesis of pH-responsive covalent organic frameworks nanocarrier for plumbagin delivery. Rsc Adv. 2022;12(25):16046–50.
Bai L, Phua SZF, Lim WQ, Jana A, Luo Z, Tham HP, Zhao L, Gao Q, Zhao Y. Nanoscale covalent organic frameworks as smart carriers for drug delivery. Chem Commun. 2016;52(22):4128–31.
Vyas VS, Vishwakarma M, Moudrakovski I, Haase F, Savasci G, Ochsenfeld C, Spatz JP, Lotsch BV. Exploiting noncovalent interactions in an imine-based covalent organic framework for quercetin delivery. Adv Mater. 2016;28(39):8749–54.
Mitra S, Sasmal HS, Kundu T, Kandambeth S, Illath K, Díaz Díaz D, Banerjee R. Targeted drug delivery in covalent organic nanosheets (CONs) via sequential postsynthesis. J Am Chem Soc. 2017;139(12):4513–20.
Zhang G, Li X, Liao Q, Liu Y, Xi K, Huang W, Jia X. Water-dispersible PEG-curcumin/amine-functionalized covalent organic framework nanocomposites as smart carriers for in vivo drug delivery. Nat Commun. 2018;9:2785.
Wang H, Zhu W, Liu J, Dong Z, Liu Z. pH-responsive nanoscale covalent organic polymers as a biodegradable drug carrier for combined photodynamic-chemotherapy of cancer. ACS Appl Mater Interfaces. 2018;10(17):14475–82.
Liu S, Yang J, Guo R, Deng L, Dong A, Zhang J. Facile fabrication of redox-responsive covalent organic framework nanocarriers for efficiently loading and delivering doxorubicin. Macromol Rapid Comm. 2020;41(4):1–6.
Anbazhagan R, Krishnamoorthi R, Kumaresan S, Tsai H-C. Thioether-terminated triazole-bridged covalent organic framework for dual-sensitive drug delivery application. Mater Sci Eng C. 2021;120:111704.
Ji N, Hong Y, Gu Z, Cheng L, Li Z, Li C. Preparation and characterization of insulin-loaded zein/carboxymethylated short-chain amylose complex nanoparticles. J Agric Food Chem. 2018;66(35):9335–43.
Chen Y, Song H, Huang K, Guan X. Novel porous starch/alginate hydrogels for controlled insulin release with dual response to pH and amylase. Food Funct. 2021;12(19):9165–77.
Li S, Liang N, Yan P, Kawashima Y, Sun S. Inclusion complex based on n-acetyl-l-cysteine and arginine modified hydroxypropyl-β-cyclodextrin for oral insulin delivery. Carbohyd Polym. 2020;252:117202.
Liu C, Xu H, Sun Y, Zhang X, Cheng H, Mao S. Design of virus-mimicking polyelectrolyte complexes for enhanced oral insulin delivery. J Pharm Sci. 2019;108(10):3408–15.
Zhou S, Deng H, Zhang Y, Wu P, He B, Dai W, Zhang H, Zhang Q, Zhao R, Wang X. Thiolated nanoparticles overcome the mucus barrier and epithelial barrier for oral delivery of insulin. Mol Pharm. 2019;17(1):239–50.
Shirzadian T, Nourbakhsh MS, Fattahi A, Bahrami G, Mohammadi G. Characterization and optimization of de-esterified tragacanth-chitosan nanocomposite as a potential carrier for oral delivery of insulin: in vitro and ex vivo studies. J Biomed Mater Res A. 2021;109(11):2164–72.
Wu J, Chen L, Zhang X, Xu C, Liu J, Gu J, Ji H, Feng X, Yan C, Song X. A core-shell insulin/CS-PLGA nanoparticle for enhancement of oral insulin bioavailability: in vitro and in vivo study. Int J Polym Mater. 2022;72(8):656–64.
Verma A, Sharma S, Gupta PK, Singh A, Teja BV, Dwivedi P, Gupta GK, Trivedi R, Mishra PR. Vitamin B12 functionalized layer by layer calcium phosphate nanoparticles: a mucoadhesive and pH responsive carrier for improved oral delivery of insulin. Acta Biomater. 2015;31:288–300.
Wu H, Guo T, Nan J, Yang L, Liao G, Park HJ, Li J. Hyaluronic-acid-coated chitosan nanoparticles for insulin oral delivery: fabrication, characterization, and hypoglycemic ability. Macromol Biosci. 2022;22(7):2100493.
Zhang YW, Tu LL, Tang Z, Wang Q, Zheng GL, Yin LN. pH-sensitive chitosan-deoxycholic acid/alginate nanoparticles for oral insulin delivery. Pharm Dev Technol. 2021;26(9):943–52.
Xu Z, Chen L, Duan X, Li X, Ren H. Microparticles based on alginate/chitosan/casein three-dimensional system for oral insulin delivery. Polym Advan Technol. 2021;32(11):4352–61.
Tian H, He Z, Sun C, Yang C, Zhao P, Liu L, Leong KW, Mao H-Q, Liu Z, Chen Y. Uniform core-shell nanoparticles with thiolated hyaluronic acid coating to enhance oral delivery of insulin. Adv Healthc Mater. 2018;7(17):1800285.
Xie Y, Jiang S, Xia F, Hu X, He H, Yin Z, Qi J, Lu Y, Wu W. Glucan microparticles thickened with thermosensitive gels as potential carriers for oral delivery of insulin. J Mater Chem B. 2016;4(22):4040–8.
Reboredo C, Gonzalez-Navarro CJ, Martinez-Lopez AL, Martinez-Oharriz C, Sarmento B, Irache JM. Zein-based nanoparticles as oral carriers for insulin delivery. Pharmaceutics. 2021;14(1):39.
Gao Y, He Y, Zhang H, Zhang Y, Gao T, Wang J-H, Wang S. Zwitterion-functionalized mesoporous silica nanoparticles for enhancing oral delivery of protein drugs by overcoming multiple gastrointestinal barriers. J Colloid Interf Sci. 2020;582:364–75.
Duan Y, Ye F, Huang Y, Qin Y, He C, Zhao S. One-pot synthesis of a metal-organic framework-based drug carrier for intelligent glucose-responsive insulin delivery. Chem Commun. 2018;54(42):5377–80.
He M, Yu P, Hu Y, Zhang J, He M, Nie C, Chu X. Erythrocyte-membrane-enveloped biomineralized metal-organic framework nanoparticles enable intravenous glucose-responsive insulin delivery. ACS Appl Mater Interfaces. 2021;13(17):19648–59.
Acknowledgements
Acknowledge Prof. Genlin Zhang for their fruitful discussion and suggestions during the preparation of this manuscript. We gratefully acknowledge the School of Chemistry and Chemical Engineering/State Key Laboratory Incubation Base for Green Processing of Chemical Engineering (Shihezi University) for providing the facilities to carry out this work.
Funding
This work was supported by National Natural Science Foundation of China (Grant No. 22178226, 51863018), Young Doctor Fund of Higher Education in Gansu Province, Grant Number 2021QB-105.
Author information
Authors and Affiliations
Contributions
GZ: initiated the work upon invitation, designed the proposal. Writing—reviewing and editing. YW: wrote the draft of the manuscript, designed and drew the graphs. AR: revised the manuscript. HW: revised the proposal. HL: revised the graphs. RM: revised the character.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors have reviewed the final version of the manuscript and approved it for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, Y., Li, H., Rasool, A. et al. Polymeric nanoparticles (PNPs) for oral delivery of insulin. J Nanobiotechnol 22, 1 (2024). https://doi.org/10.1186/s12951-023-02253-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12951-023-02253-y