Abstract
Objective
To analyze the clinical infection characteristics and genetic environments of resistance genes in carbapenem-resistant Citrobacter europaeus using whole-genome sequencing.
Methods
The susceptibility of two clinical isolates of C. europaeus (WF0003 and WF1643) to 24 antimicrobial agents was assessed using the BD Phoenix™ M50 System and Kirby-Bauer (K-B) disk-diffusion method. Whole-genome sequencing was performed on the Illumina and Nanopore platforms, and ABRicate software was used to predict resistance and virulence genes of carbapenem-resistant C. europaeus. The characteristics of plasmids carrying carbapenem-resistance genes and their genetic environments were analyzed. Single nucleotide polymorphisms were used to construct a phylogenetic tree to analyze the homology of these two C. europaeus strains with ten strains of C. europaeus in the NCBI database.
Results
The two strains of carbapenem-resistant C. europaeus are resistant to various antimicrobial agents, particularly carbapenems and β-lactams. WF0003 carries blaNDM− 1, which is located on an IncX3 plasmid that has high homology to the pNDM-HN380 plasmid. blaNDM− 1 is located on a truncated Tn125. It differs from Tn125 by the insertion of IS5 in the upstream ISAba125 and the deletion of the downstream ISAba125, which is replaced by IS26. WF1643 carries blaOXA− 48 in a Tn1999 transposon on the IncL/M plasmid, carrying only that single drug resistance gene. Homology analysis of these two strains of C. europaeus with ten C. europaeus strains in the NCBI database revealed that the 12 strains can be classified into three clades, with both WF0003 and WF1643 in the B clade.
Conclusion
To the best of our knowledge, this is the first study to report an IncX3 plasmid carrying blaNDM− 1 in C. europaeus in China. C. europaeus strains harboring carbapenem-resistance genes are concerning in relation to the spread of antimicrobial resistance, and the presence of carbapenem-resistance genes in C. europaeus should be continuously monitored.
Similar content being viewed by others
Introduction
Citrobacter spp. are gram-negative bacteria belonging to the Enterobacteriaceae family. They mostly act as opportunistic pathogens and can cause diarrhea, sepsis, meningitis, or respiratory and urinary tract infections in infants, young children, and immunocompromised patients [1, 2]. Currently, Citrobacter spp. are rapidly gaining clinical importance as multidrug-resistant pathogens causing opportunistic hospital- acquired and community-acquired infections.
In recent years, the excessive usage of antimicrobial agents, including carbapenems, has led to an increase in bacterial antimicrobial resistance [3]. In the first half of 2023, Enterobacteriaceae were still the primary pathogenic microorganisms causing hospital-acquired infections in China, according to data from CHINET (http://www.chinets.com/). Specifically, Citrobacter spp. showed resistance rates to meropenem, imipenem, ceftazidime, and cefoxitin of 6.1%, 5.4%, 25.9%, and 51.9%, respectively. At present, the emergence of carbapenem-resistant Citrobacter has increased the rate of hospital-acquired infections and mortality [4, 5]. Acquisition of carbapenem resistance by opportunistic pathogens poses a serious challenge to the treatment of infections. Moreover, it highlights the importance of monitoring antimicrobial-resistant bacteria along with investigation of resistance mechanisms.
Mechanisms of carbapenem resistance mainly include carbapenemase production and high production of AmpC enzymes or extended-spectrum β-lactamase, along with the deletion of outer-membrane pore proteins and/or high expression of efflux pumps [6]. The importance of carbapenemases is greater because most of their coding genes are carried on mobile genetic elements such as plasmids and transposons that can be transferred between bacteria [6]. The New Delhi metallo-β-lactamase blaNDM−1 is the most common carbapenem-resistance gene in Enterobacteriaceae, which is mainly located on plasmids. Plasmids carrying blaNDM−1 are diverse in the Enterobacteriaceae family, and the most common include IncX, IncA/C, IncF, and IncL/M incompatibility plasmids [7,8,9,10]. Mobile genetic elements—such as transposons, insertion sequences, integrons, and other movable genetic elements surrounding the structure of blaNDM−1 in Enterobacteriaceae—mediate the transmission of blaNDM−1 among bacteria [11]. blaOXA−48 is a globally prevalent carbapenem-resistance gene [12]. Tn1999 and efficient transfer of multiple plasmids (such as pOXA-48a, accession number JN626286) have accelerated the horizontal spread of blaOXA−48 among bacteria [13]. Therefore, the study of the structure of plasmids carrying carbapenem-resistance genes and their genetic environments can help in understanding the mechanism of widespread distribution of carbapenem-resistance genes in pathogens.
The aim of this study was to analyze the clinical infection characteristics and genetic environments of resistance genes in carbapenem-resistant Citrobacter europaeus in our hospital in China.
Methods
Bacterial isolation and identification
Two carbapenem-resistant C. europaeus strains (WF0003 and WF1643) were isolated from hospitalized patients at a tertiary hospital in northern China. WF0003 was isolated from ascites in 2011, and WF1643 was isolated from sputum in 2017. The strains were identified by Matrix Assisted Laser Destruction/Ionization Time of Flight Mass Spectrometry (MALDI-TOF MS) using Vitek MS (Sysmex bioMerieux, Marcy l’Etoole, France).
Antimicrobial susceptibility testing
The BD Phoenix™ M50 System (Becton, Dickinson and Company, New Jersey, USA) and K-B (K-B) disk-diffusion method (Oxoid, Hampshire, United Kingdom) was used to test the susceptibility of the strains to 24 antimicrobial agents commonly used in clinical practice. The susceptibility criteria were determined in accordance with the Clinical and Laboratory Standards Institute (CLSI) guidelines (2021) [14] (https://clsi.org/). Escherichia coli ATCC 25,922 served as the quality control strain.
Whole-genome sequencing and sequence assembly
The bacterial genomes were extracted using a bacterial DNA kit (OMEGA, GA, USA), and the purified DNA was subjected to whole-genome sequencing using a combination of the Illumina HiSeq X Ten (Illumina, CA, USA) and Nanopore PromethION (Oxford Nanopore Technologies, OX, UK) sequencing platforms. Paired-end DNA libraries were constructed with an average insert size of 350 bp for Illumina sequencing, and shotgun DNA libraries were generated with a 10 kb insert size for Nanopore sequencing. FastQC 0.11.8 (http://www.bioinformatics.babraham.ac.uk/projects/fastqc/) was used for quality control of raw reads. A hybrid assembly was then performed using Unicycler v0.4.9 [15], incorporating both the short paired-end Illumina reads and the long Nanopore reads.
Whole-genome sequencing analysis
Antimicrobial-resistance genes and virulence genes were identified using the NCBI and Virulence Factors of Pathogenic Bacteria (VFDB) databases with ABRicate 0.8 (https://github.com/tseemann/abricate) [16]. PlasmidFinder [17] was used to examine the type of plasmid replicon. The sequences of other strains were obtained using NCBI for the constructing of the phylogenetic tree (up to Sept 30, 2023). Then, the core single nucleotide polymorphisms (SNPs) were identified by Mummer 3.25 [18]. Maximum-likelihood phylogenetic trees were constructed using MEGAX 10.1.8 [19] based on the resulting core SNPs with a bootstrap iteration of 1000, and visualized by Interactive Tree Of Life (iTOL) [20]. Annotation of mobile elements, and other features utilized online databases, including ISfinder [21], and Tn Number Registry [22]. DANMEL was used for analyzing the sequenced mobile genetic elements in bacteria [23]. BLASTN was employed for the alignment and comparison of the plasmid sequences analyzed in this study with high homologous plasmid sequences publicly available in NCBI. Gene organization diagrams were drawn in Inkscape 0.48.1 software.
Nucleotide sequence accession numbers
The complete sequences of the two C. europaeus strains were submitted to GenBank under BioProject number PRJNA1088829.
Results
Patient background and clinical isolates of C. europaeus
Patient 1 was a 62-year-old female with chronic hepatitis B who was hospitalized in the infectious unit, and WF0003 was isolated from her ascites. The patient was treated with cefepime (for four days) and imipenem (for two days). The patient was discharged from the hospital in a poor state.
Patient 2 was an 87-year-old male with basal cell carcinoma of the face who was admitted from the healthcare setting, and WF1643 was isolated from his sputum. The patient received ceftazidime (for two days) before the WF1643 isolation, and was treated with moxifloxacin (for three days) and levofloxacin (for a day) after the WF1643 isolation. The patient was discharged from the hospital with an improvement in health. The hospital treatments of patients 1 and 2 are shown in Fig. 1.
Antimicrobial susceptibility testing
The results of the antimicrobial susceptibility testing revealed that the two strains of C. europaeus have high resistance rates to antimicrobial agents (Table 1). WF0003 and WF1643 are resistant to 13 and 10 antimicrobial agents, respectively. Both strains of C. europaeus exhibit high resistance to β-lactams and are susceptible to only three antimicrobial.
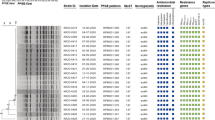
Resistance and virulence genes
WF0003 has 23 resistance genes, which are mainly against β-lactams and aminoglycosides, including the carbapenem-resistance gene blaNDM−1 and the polymyxin-resistance gene mcr-9. WF1643 has three resistance genes, including the carbapenem-resistance gene blaOXA−48 (Table 2).
Twenty-five and 27 virulence genes were identified in WF0003 and WF1643 isolates, respectively, which the most common were Vi-antigen-related, adhesion-related, nutrient/metabolism-related, and yersiniabactin-encoding genes (Table 2).
Genome features of the plasmids carried by C. europaeus
Three types of plasmids (IncHI2, IncX3, and RepA_1) were found in WF0003 (Table 3). pWF0003-1 is an IncHI2-type plasmid carrying multiple drug-resistance genes, including mcr-9. pWF0003-NDM plasmid is a 54-kb IncX3-type plasmid, carrying three resistance genes: blaNDM−1, blaSHV−12, and bleMBL. Furthermore, a 62-kb IncL/M-type plasmid (pWF1643-OXA) carrying blaOXA−48 was identified in WF1643.
Analysis of genetic environments of carbapenem-resistance genes
The pWF0003-NDM plasmid carrying blaSHV−12, bleMBL, and blaNDM−1 genes is 99% homologous to pNDM-HN380 (GenBank accession no. JX104760) (Fig. 2A). An inversion of the truncated IS26-blaSHV-12-IS26 unit in the blaNDM−1 region represents the only modular difference between pWF0003-NDM and pNDM-HN380. blaNDM−1 is located on ΔTn125. ΔTn125 on pWF0003-NDM differs from Tn125 in that the upstream ISAba125 has an IS5 insertion, and the downstream ISAba125 is missing and replaced by IS26. blaSHV−12 is located in the truncated IS26-blaSHV−12-IS26 sequence (Fig. 2B).
The pWF1643-OXA plasmid backbone region is highly homologous to pCP082157 (Fig. 3A). blaOXA−48 is located on an intact Tn1999 flanked by IS1999 (Fig. 3B). This transposon is inserted in the tir gene. The IS1R sequence is inserted in IS1999 upstream of Tn1999.2 in pCP082157. Compared with pCP082157, pWF1643-OXA (a part of the backbone region) is devoid of the Group-II intron reverse transcriptase/maturase functional gene ltrA.
Homology analysis
A phylogenetic tree was constructed using the two C. europaeus strains isolated in this study and ten strains of C. europaeus obtained from NCBI. This divided the 12 strains into three clades, with both strains isolated in this study in the B clade (Fig. 4). The 12 strains of C. europaeus were isolated from five different countries between 2011 and 2018. Two of them are from unknown sources, and the time of isolation was not reported. Four carbapenem-resistance genes (blaVIM−1, blaKPC−2, blaOXA−48, and blaNDM−1) were detected in seven of the 12 C. europaeus strains. WF0003 and WF1643 are closely related to C. europaeus strains from the USA and Germany, respectively.
Discussion
Citrobacter spp. are widespread in natural environments, including soil, water, air, and food. Normally, they do not cause disease in animals and humans, and therefore their clinical pathogenicity is often overlooked [24]. Despite the low prevalence of Citrobacter infections, invasive Citrobacter are associated with a high mortality rate [25]. In this study, two C. europaeus strains were isolated from elderly patients with underlying diseases. After being admitted to hospital, the patients were treated with antimicrobial agents, but patient 1 was in a poor condition and ceased treatment. The results are similar to Oyeka’s study [26], in which Citrobacter infections were associated with serious consequences in immunocompromised patients. C. europaeus was first reported in 2017 by Ribeiro et al. It was named C. europaeus with average nucleotide identity (ANI) values significantly below the 95% species threshold of C. freundii, C. werkmanii, and C. youngae [27]. Citrobacter is easily confused with E. coli and Salmonella because it exhibits great variability in its morphological and biochemical characteristics, antigenicity, and pathogenicity [28, 29]. Previously, the identification of Citrobacter spp. was mainly carried out through genotypic and phenotypic approaches. Nowadays, MALDI-TOF MS technology is widely used for bacterial identification, as it is faster and more accurate than traditional methods [30, 31]. Few complete genomes of C. europaeus are available at NCBI, and information about this bacterium is generally little; therefore, the incidence of infection with carbapenem-resistant C. europaeus is likely to be underestimated. To the best of our knowledge, this is the first study to investigate carbapenem-resistant C. europaeus clinical isolates in our hospital. We studied the resistance mechanisms and the plasmids carrying the resistance genes to understand the possible resistance and transmission mechanisms.
In Biez’s study, they isolated 1121 carbapenem non-susceptible Citrobacter spp. with high-level resistance to quinolones, β-lactams, and aminoglycosides [32]. Carbapenem-resistant C. europaeus exhibited resistance to multiple antimicrobial agents. This is consistent with our study, in which WF0003 and WF1643 exhibited resistance to 13 and 10 antimicrobial agents, respectively. Both strains were only sensitive to three antimicrobial agents, AMK, COL, and TGC. Such a high level of resistance is of concern and may lead to the ineffectiveness of available antimicrobial agents against this pathogen.
blaNDM-1 is the most prevalent carbapenem-resistance gene in Enterobacteriaceae in China [33], and the spread of blaNDM-1 between bacteria is mainly mediated by plasmids. In this study, we have shown that WF0003 carries blaNDM-1 on an IncX3 plasmid that is similar to pNDM-HN380 (GenBank accession no. JX104760), isolated from Klebsiella pneumonia in Hong Kong in 2011 [34]. The pNDM-HN380 plasmid has been reported in C. freundii, E. coli, and Enterobacter hormaechei [35,36,37], suggesting that plasmids harboring resistance genes are likely to be transmitted horizontally between different strains. Although IncX3 plasmids carrying blaNDM-1 have been frequently reported in other Citrobacter species [35, 38], this is the first report in C. europaeus in China.
In this study, blaNDM−1 in WF0003 isolate is located on ΔTn125, the major transposon responsible for the widespread dissemination of the blaNDM−1 gene. In Acinetobacter, Tn125 was identified in the pNDM-BJ01 plasmid as a composite transposon based on two identically oriented ISAba125 insertion sequences [39]. As per the sequencing data, Tn125 consists of ISAba125, blaNDM−1, bleMBL, trpF, dsbD, cutA, groES, groEL, ISCR21, and ISAba125, and is constrained at both ends by a 3-bp DR [37]. In Enterobacteriaceae, as a result of complex recombination events, Tn125 usually exists in various truncated forms [40]. These ΔTn125 forms are similar to the Tn125 variants found in several regions of China [41]. blaNDM−1 found in clinical or environmental isolates or isolates of animal origin, in China and abroad, exhibits various truncated forms of Tn125, although in different genetic environments [40, 42, 43]. This suggests that Tn125 plays an important role in the transmission of blaNDM−1.
In this study, we have shown that blaOXA−48 in the WF1643 isolate is located on an IncL/M plasmid on Tn1999. blaOXA−48 is the most prevalent carbapenem-resistance gene in Citrobacter spp [32], and was discovered and characterized in a carbapenem-resistant K. pneumonia isolate from a Turkish patient [44]. Subsequently, this gene has been identified and reported worldwide, including in China, the United States, and India [45]. In consistent with our study, blaOXA−48 is most commonly found in the 60–70 kb IncL/M plasmid, which has no other resistance genes. blaOXA−48 is found between two IS1999 insertion sequences on the Tn1999 complex transposon, upstream of lysR. blaOXA−48 transfer is mainly carried out through a 62-kb IncL/M plasmid (pOXA-48) [46], which is found in most blaOXA−48-positive Enterobacteriaceae members. The CP082157 reference plasmid harbors the blaOXA−48 gene, which is located on Tn1999.2, a variant of the Tn1999 transposon. A previous study [47] detected 91.8% Tn1999.2 and only 8.2% complete Tn1999, indicating that Tn1999.2 is more common than Tn1999. Potron et al. reported that IncL/M is an efficient carrier of resistance genes, and inactivation of the tir gene (encoding a transfer repressor protein) by the insertion of Tn1999 may contribute to the efficient transfer of pOXA-48a in various genetic backgrounds. Moreover, the current spread of blaOXA−48 is largely a result of the spread of a single prevalent plasmid [48].
WF0003 carries mcr-9 genes, but it is susceptible to colistin. This is consistent with Ju’s study, which isolated nine strains of Citrobacter carrying mcr-9, all of which were sensitive to colistin [49]. Kieffer’s study showed that the expression of mcr-9 could be induced by subinhibitory concentrations of colistin in the presence of qseB and qseC. Therefore, the minimal inhibitory concentration (MIC) levels of colistin were increased [50]. This suggests that the clinical use of colistin may induce colistin resistance in mcr-9-positive isolates and accelerate the dissemination of mcr-9 among potential pathogens. Therefore, the presence of mcr-9 in pathogens should be carefully monitored.
WF1643 is similar to a C. europaeus strain from Germany in that they both carry blaOXA−48. The prevalence of blaOXA−48 is geographically specific, mainly concentrated in the Middle East and Europe [51]. WF1643 shares high similarity with European strains. Therefore, great attention should be paid to the prevalence and evolution of blaOXA−48 to prevent large-scale epidemic outbreaks. WF0003 is similar to two strains of C. europaeus from the USA, although the two strains from the USA do not carry carbapenem-resistance genes and WF0003 is the only strain that carries blaNDM−1. However, because of the small number of clinical isolates of C. europaeus and small amount of data uploaded to the NCBI database, the estimation of the possession of carbapenem-resistance genes in C. europaeus may not be truly accurate. Future studies should focus on the identification of isolates and biological analysis of C. europaeus to better understand clinical infections and transmission of C. europaeus.
The limited number of samples in this study may not be representative of the overall diversity of C. europaeus in this region; however, this study still provides important clues for the classification and characterization of C. europaeus. This study reveals the predicted virulence and resistance genes of the C. europaeus strains isolated in our hospital, and the plasmids and genetic environments in which the carbapenem-resistance genes are located. Moreover, to the best of our knowledge, this is the first study to report an IncX3 plasmid carrying blaNDM−1 in C. europaeus in China. These results are of great importance for the in-depth understanding of carbapenem resistance in C. europaeus.
Data availability
The sequences of the two C. europaeus strains were submitted to GenBank under BioProject PRJNA1088829.
References
Babiker A, Evans DR, Griffith MP, et al. Clinical and genomic epidemiology of Carbapenem-Nonsusceptible Citrobacter spp. at a Tertiary Health Care Center over 2 decades. J Clin Microbiol. 2020;58(9):e00275–20.
Arana DM, Ortega A, González-Barberá E, et al. Carbapenem-resistant Citrobacter spp. isolated in Spain from 2013 to 2015 produced a variety of carbapenemases including VIM-1, OXA-48, KPC-2, NDM-1 and VIM-2. J Antimicrob Chemother. 2017;72(12):3283–7.
Grundmann H, Glasner C, Albiger B, et al. Occurrence of carbapenemase-producing Klebsiella pneumoniae and Escherichia coli in the European survey of carbapenemase-producing Enterobacteriaceae (EuSCAPE): a prospective, multinational study. Lancet Infect Dis. 2017;17(2):153–63.
Liu LH, Wang NY, Wu AY, et al. Citrobacter freundii bacteremia: risk factors of mortality and prevalence of resistance genes. J Microbiol Immunol Infect. 2018;51(4):565–72.
Qian C, Du Y, Li H, et al. Development of rapid and simple experimental and in silico serotyping systems for Citrobacter. Future Microbiol. 2018;13(13):1511–22.
Bush K, Bradford PA. Epidemiology of β-Lactamase-producing pathogens. Clin Microbiol Rev. 2020;33(2):e00047–19.
Du XX, Wang JF, Fu Y, et al. Genetic characteristics of blaNDM-1-positive plasmid in Citrobacter freundii isolate separated from a clinical infectious patient. J Med Microbiol. 2013;62(Pt 9):1332–7.
Hadziabdic S, Fischer J, Borowiak M, et al. The blaNDM-1-Carrying IncA/C2 plasmid underlies structural alterations and cointegrate formation in vivo. Antimicrob Agents Chemother. 2019;63(8):e00380–19.
Toledano-Tableros JE, Gayosso-Vázquez C, Jarillo-Quijada MD, et al. Dissemination of blaNDM-1 gene among several Klebsiella pneumoniae sequence types in Mexico Associated with horizontal transfer mediated by IncF-Like plasmids. Front Microbiol. 2021;12:611274.
Lopez-Diaz M, Ellaby N, Turton J, et al. NDM-1 carbapenemase resistance gene vehicles emergent on distinct plasmid backbones from the IncL/M family. J Antimicrob Chemother. 2022;77(3):620–4.
Wailan AM, Sartor AL, Zowawi HM, et al. Genetic contexts of blaNDM–1 in patients carrying multiple NDM-Producing strains. Antimicrob Agents Chemother. 2015;59(12):7405–10.
Poirel L, Castanheira M, Carrër A, et al. OXA-163, an OXA-48-related class D β-lactamase with extended activity toward expanded-spectrum cephalosporins. Antimicrob Agents Chemother. 2011;55(6):2546–51.
Kopotsa K, Osei Sekyere J, Mbelle NM. Plasmid evolution in carbapenemase-producing Enterobacteriaceae: a review. Ann N Y Acad Sci. 2019;1457(1):61–91.
CLSI. (2021). Performance Standards for Antimicrobial Susceptibility Testing. 31st ed. CLSI supplement M100. Wayne, PA: Clinical and Laboratory Standards Institute.
Wick RR, Judd LM, Gorrie CL, Holt KE, Unicycler. Resolving bacterial genome assemblies from short and long sequencing reads. PLoS Comput Biol. 2017;13(6):e1005595.
Feldgarden M, Brover V, Haft DH et al. Validating the AMRFinder Tool and Resistance Gene Database by using Antimicrobial Resistance genotype-phenotype correlations in a Collection of isolates. Antimicrob Agents Chemother. 2019;63(11).
Carattoli A, Zankari E, García-Fernández A, et al. In silico detection and typing of plasmids using PlasmidFinder and plasmid multilocus sequence typing. Antimicrob Agents Chemother. 2014;58(7):3895–903.
Delcher AL, Salzberg SL, Phillippy AM. Using MUMmer to identify similar regions in large sequence sets. Curr Protoc Bioinformatics. 2003(1):10.3.1-.3.8.
Kumar S, Stecher G, Li M, et al. MEGA X: Molecular Evolutionary Genetics Analysis across Computing platforms. Mol Biol Evol. 2018;35(6):1547–9.
Letunic I, Bork P. Interactive tree of life (iTOL) v4: recent updates and new developments. Nucleic Acids Res. 2019;47(W1):W256–9.
Siguier P, Perochon J, Lestrade L, et al. ISfinder: the reference centre for bacterial insertion sequences. Nucleic Acids Res. 2006;34(Database issue):D32–6.
Tansirichaiya S, Rahman MA, Roberts AP. Transposon Registry Mob DNA. 2019;10:40.
Wang P, Jiang X, Mu K, et al. DANMEL: a manually curated reference database for analyzing mobile genetic elements associated with bacterial drug resistance. mLife. 2022. https://doi.org/10.1002/mlf2.12046.
Lewicki M, Kozioł M, Lorenc K, et al. Citrobacter freundii and Acinetobacter baumanii infection in a patient with neoplastic lung disease-case report. Ann Agric Environ Med. 2021;28(4):724–8.
Shih CC, Chen YC, Chang SC, et al. Bacteremia due to Citrobacter species: significance of primary intraabdominal infection. Clin Infect Dis. 1996;23(3):543–9.
Oyeka M, Antony S. Citrobacter braakii Bacteremia: Case Report and Review of the literature. Infect Disord Drug Targets. 2017;17(1):59–63.
Ribeiro TG, Clermont D, Branquinho R, et al. Citrobacter europaeus sp. nov., isolated from water and human faecal samples. Int J Syst Evol Microbiol. 2017;67(1):170–3.
Pilar AVC, Petronella N, Dussault FM, et al. Similar yet different: phylogenomic analysis to delineate Salmonella and Citrobacter species boundaries. BMC Genomics. 2020;21(1):377.
Samuel G, Hogbin JP, Wang L, Reeves PR. Relationships of the Escherichia coli O157, O111, and O55 O-antigen gene clusters with those of Salmonella enterica and Citrobacter freundii, which express identical O antigens. J Bacteriol. 2004;186(19):6536–43.
Kwak HL, Han SK, Park S, et al. Development of a Rapid and Accurate Identification Method for Citrobacter species isolated from pork products using a matrix-assisted laser-desorption ionization time-of-flight Mass Spectrometry (MALDI-TOF MS). J Microbiol Biotechnol. 2015;25(9):1537–41.
Kolínská R, Spanělová P, Dřevínek M, et al. Species identification of strains belonging to Genus Citrobacter using the biochemical method and MALDI-TOF mass spectrometry. Folia Microbiol (Praha). 2015;60(1):53–9.
Biez L, Bonnin RA, Emeraud C, et al. Nationwide molecular epidemiology of carbapenemase-producing Citrobacter spp. in France in 2019 and 2020. mSphere. 2023;8(6):e0036623.
Qiao J, Chen Y, Ge H, et al. Coexistence of blaIMP-4, blaNDM-1 and blaOXA-1 in blaKPC-2-producing Citrobacter freundii of clinical origin in China. Front Microbiol. 2023;14:1074612.
Ho PL, Li Z, Lo WU, et al. Identification and characterization of a novel incompatibility group X3 plasmid carrying bla NDM-1 in Enterobacteriaceae isolates with epidemiological links to multiple geographical areas in China. Emerg Microbes Infect. 2012;1(11):e39.
Li Y, Fang C, Qiu Y, et al. Genomic characterization of a carbapenem-resistant Citrobacter freundii cocarrying blaKPC-2 and blaNDM-1. J Glob Antimicrob Resist. 2022;29:289–92.
Lv J, Qi X, Zhang D, Zheng Z, et al. First Report of Complete sequence of a blaNDM-13-Harboring plasmid from an Escherichia coli ST5138 clinical isolate. Front Cell Infect Microbiol. 2016;6:130.
Yuan Q, Xia P, Xiong L, et al. First report of coexistence of blaKPC-2-, blaNDM-1 and mcr-9-carrying plasmids in a clinical carbapenem-resistant Enterobacter hormaechei isolate. Front Microbiol. 2023;14:1153366.
Cao X, Xie H, Huang D, et al. Detection of a clinical carbapenem-resistant Citrobacter portucalensis strain and the dissemination of C. Portucalensis in clinical settings. J Glob Antimicrob Resist. 2021;27:79–81.
Poirel L, Bonnin RA, Boulanger A, et al. Tn125-related acquisition of blaNDM-like genes in Acinetobacter baumannii. Antimicrob Agents Chemother. 2012;56(2):1087–9.
Chen Z, Li H, Feng J, et al. NDM-1 encoded by a pNDM-BJ01-like plasmid p3SP-NDM in clinical Enterobacter aerogenes. Front Microbiol. 2015;6:294.
Hu K, Zhang J, Zou J, et al. Molecular characterization of NDM-1-producing carbapenem-resistant E. cloacae complex from a tertiary hospital in Chongqing, China. Front Cell Infect Microbiol. 2022;12:935165.
Lin D, Xie M, Li R, et al. IncFII Conjugative plasmid-mediated transmission of blaNDM-1 elements among animal-borne Escherichia coli strains. Antimicrob Agents Chemother. 2016;61(1):02285–02216.
Zhao Y, Wang L, Zhang Z, et al. Structural genomics of pNDM-BTR harboring In191 and Tn6360, and other blaNDM-carrying IncN1 plasmids. Future Microbiol. 2017;12:1271–81.
Poirel L, Héritier C, Tolün V, Nordmann P. Emergence of oxacillinase-mediated resistance to imipenem in Klebsiella pneumoniae. Antimicrob Agents Chemother. 2004;48(1):15–22.
Beyrouthy R, Robin F, Delmas J, et al. IS1R-mediated plasticity of IncL/M plasmids leads to the insertion of Bla OXA-48 into the Escherichia coli chromosome. Antimicrob Agents Chemother. 2014;58(7):3785–90.
Poirel L, Potron A, Nordmann P. OXA-48-like carbapenemases: the phantom menace. J Antimicrob Chemother. 2012;67(7):1597–606.
Argente M, Miró E, Martí C, et al. Molecular characterization of OXA-48 carbapenemase-producing Klebsiella pneumoniae strains after a carbapenem resistance increase in Catalonia. Enferm Infecc Microbiol Clin (Engl Ed). 2019;37(2):82–8.
Potron A, Poirel L, Nordmann P. Derepressed transfer properties leading to the efficient spread of the plasmid encoding carbapenemase OXA-48. Antimicrob Agents Chemother. 2014;58(1):467–71.
Ju X, Wang S, Yang X, et al. Epidemiology and molecular characteristics of mcr-9 in Citrobacter spp. from healthy individuals and patients in China. Microbiol Spectr. 2022;10(6):e0134622.
Kieffer N, Royer G, Decousser JW, et al. mcr-9, an Inducible Gene Encoding an Acquired Phosphoethanolamine Transferase in Escherichia coli, and its origin. Antimicrob Agents Chemother. 2019;63(9):e00965–19.
Pitout JDD, Peirano G, Kock MM, et al. The global ascendency of OXA-48-Type carbapenemases. Clin Microbiol Rev. 2019;33(1):e00102–19.
Acknowledgements
We thank Catherine Perfect, MA (Cantab), from Liwen Bianji (Edanz) (www.liwenbianji.cn), for editing the English text of a draft of this manuscript.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
X.D. designed the study. J.M., R.X., W.L., and M.L. conducted the study, collected the data, and prepared the article. J.M. provided valuable advice and edited the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Ethical approval
Given that all strains of this experiment were bacteria isolated from routine samples of the patients, and this study did not involve the patient’s private information or data on animal subjects, this study was exempted from the requirement of ethical approval by the Ethics Committee of Weifang People’s Hospital.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ma, J., Xu, R., Li, W. et al. Whole-genome sequencing of clinical isolates of Citrobacter Europaeus in China carrying blaOXA−48 and blaNDM−1. Ann Clin Microbiol Antimicrob 23, 38 (2024). https://doi.org/10.1186/s12941-024-00699-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12941-024-00699-y