Abstract
Introduction
Infections caused by Stenotrophomonas maltophilia are clinically important due to its intrinsic resistance to a broad range of antibiotics. Therefore, selecting the most appropriate antibiotic to treat S. maltophilia infection is a major challenge.
Aim
The current meta-analysis aimed to investigate the global prevalence of antibiotic resistance among S. maltophilia isolates to the develop more effective therapeutic strategies.
Method
A systematic literature search was performed using the appropriate search syntax after searching Pubmed, Embase, Web of Science and Scopus databases (May 2023). Statistical analysis was performed using Pooled and the random effects model in R and the metafor package. A total of 11,438 articles were retrieved. After a thorough evaluation, 289 studies were finally eligible for inclusion in this systematic review and meta-analysis.
Result
Present analysis indicated that the highest incidences of resistance were associated with doripenem (97%), cefoxitin (96%), imipenem and cefuroxime (95%), ampicillin (94%), ceftriaxone (92%), aztreonam (91%) and meropenem (90%) which resistance to Carbapenems is intrinsic. The lowest resistance rates were documented for minocycline (3%), cefiderocol (4%). The global resistance rate to TMP-SMX remained constant in two periods before and after 2010 (14.4% vs. 14.6%). A significant increase in resistance to tigecycline and ceftolozane/tazobactam was observed before and after 2010.
Conclusions
Minocycline and cefiderocol can be considered the preferred treatment options due to low resistance rates, although regional differences in resistance rates to other antibiotics should be considered. The low global prevalence of resistance to TMP-SMX as a first-line treatment for S. maltophilia suggests that it remains an effective treatment option.
Similar content being viewed by others
Introduction
Stenotrophomonas maltophilia (S. maltophilia) is commonly considered a microorganism with low virulence potential in humans. It is thus classified as an opportunistic pathogen, primarily affecting those with compromised immune systems. While S. maltophilia is infrequently detected within the oropharyngeal microbiota of healthy individuals, it is often found in the oropharynx of hospitalized individuals and those with cystic fibrosis [1]. In these two particular groups, it may cause persistent respiratory tract infection that may lead to inflammation, lung impairment, and sometimes even early death [2]. Stenotrophomonas spp. primarily cause hospital-acquired infections, with pneumonia being the most common manifestation. However, it can also lead to a variety of infections, including bloodstream, urinary, intra-abdominal, catheter and implanted device infections. In rare cases, it may cause heart-, bone-, soft tissue-, and nervous system infections [3]. S. maltophilia is a common pathogen in polymicrobial infections, and the rate of its isolation in the aforementioned infections ranges from 33 to 70%. In polymicrobial infections, the overall prognosis may be affected by interactions between different types of bacteria. For example, P. aeruginosa and S. maltophilia are able to form companion biofilms in the lungs, establishing an environment that is mutually beneficial to both of these bacterial species. This interaction has been associated with a higher mortality rate in pneumonia patients [4]. Effective management strategies for S. maltophilia infections are uncertain due to the limited number of treatment options available, supported by in vitro and clinical evidence. Furthermore, differentiating between colonization and invasive infections due to S. maltophilia can present a considerable challenge. Trimethoprim-sulfamethoxazole (TMP-SMX) is generally considered the preferred therapeutic option for the treatment of S. maltophilia infections based on promising in vitro activity and positive clinical outcomes [5]. Levofloxacin is generally considered an alternative antibiotic in case of resistance to TMP-SMX [6]. Other therapeutic alternatives, such as ceftazidime, ticarcillin-clavulanic acid, tigecycline, and colistin, have also been proposed. Infections caused by Stenotrophomonas spp. are clinically important due to their intrinsic resistance to a broad range of antibiotics, including most β-lactams [4, 5]. Antibiotic resistance is facilitated by different mechanisms involving plasmids, integrons, insertion sequence common region elements, antibiotic modifying enzymes, multidrug efflux pumps, and reduced outer membrane permeability to drugs [7]. Currently, beta-lactam antibiotics are not recommended for treating infections caused by S. maltophilia because two endogenous beta-lactamase genes are present intrinsically in all isolates of this bacterial species. The first one is a Class B zinc-dependent metallo-β-lactamase, identified as blaL1. This enzyme can hydrolyze all β-lactams, excluding aztreonam, and it is also unaffected by the β-lactamase inhibitors employed in clinical settings. The second is a class A serine-β-lactamase (blaL2) that is fortunately still susceptible to inhibition by presently available β-lactamase inhibitors but it can hydrolyze β-lactams, including cephalosporins and carbapenems [8, 9]. Efflux pumps of the Resistance Nodulation Division (RND) family, including SmeDEF and SmeYZ have an important role in conferring resistance to TMP-SMX and most antibiotics [10]. Moreover, animal strains significantly contribute to the genetic variation in the S. maltophilia complex, as they act as a source of mobile antibiotic resistance genes [11]. Hence, selecting the most appropriate antibiotic to treat S. maltophilia infection is a challenge. The main aim of the present study is to assess the global resistance rate of S. maltophilia to frequently prescribed antibiotics. Therefore, this meta-analysis of resistance rates may be useful in the development of innovative and robust therapeutic strategies.
Methods
Search strategy and study selection
Studies focused on S. maltophilia antimicrobial resistance were identified through a systematic search of online databases, including MEDLINE (PubMed), Web of Science, Embase, and Scopus (May 2023). The following search syntax was utilized for search in PubMed and other databases. The comprehensive search conducted using “Stenotrophomonas maltophilia”, “s. maltophilia” “antibiotic resistance” and all relevant keywords without any restriction during searching the databases. the search syntax is mentioned in supplementary file 1. We used Mesh Terms, Emtree, and the free text method to determine synonyms. This review was performed and documented in compliance with the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [12]. The records found through database searching were merged, and the duplicates were removed using EndNote 20 (Thomson Reuters, New York, NY, USA). To prevent bias, two reviewers independently screened the records by title/abstract and full text to exclude the irrelevant articles. The third author investigated any disparities.
Selection criteria and data extraction
All qualified studies were extracted and sorted into an Excel spreadsheet (Microsoft, Redmond, WA): first author’s name, publication year, country, continent, sample collection date, the total number of S. maltophilia strains collected, diagnostic methods, antibiotic susceptibility test methodology (disk diffusion, dilution method, automated system), interpretative guidelines used (CLSI, EUCAST, Other) and the number/fraction of resistant isolates to each antibiotic (Supplementary Table S1). To mitigate the possibility of any inaccuracies in the extraction of data, two authors (NBGH and LD) extracted the necessary data independently and reached an agreement on any discrepant data. Eligibility criteria for incorporating articles in the meta-analysis were a report on the proportion of antibiotic resistance, determined sample size and availability of a full-text English-published format of the article. The following factors determined exclusion: (1) S. maltophilia was not detected; (2) S. maltophilia was isolated from animals or the environment; (3) S. maltophilia antibiotic resistance was not presented or only superficially reported as MIC50/90; (4) evaluation of the combined effects of antibiotics only; (5) when the guideline used was not specified; (6) when there was no clear reporting of resistance rates; (7) data were from conference abstracts, editorials, prior meta-analyses, systematic reviews, narrative reviews;(8) when an article was not available, in case of articles without full-text availability; (9) failure to access full articles even after repeated attempts to establish contact with the corresponding author via electronic mail.
Quality assessment
Two blinded reviewers evaluated the research quality by utilizing a modified version of the assessment tool introduced by the Newcastle-Ottawa scale (NOS) adapted specifically for cross-sectional studies [13] (Supplementary Table S1). Each study was attributed scores of 0–4, 5–6, and 6–7, assigning low, moderate, and high quality, respectively. In instances where there was disagreement, a third reviewer was tasked with adjudication.
Publication bias
Publication bias was statistically assessed using Egger’s and Begg’s tests, Funnel plot, Fail and safe and Trim and Fill.
Definitions
Individuals were defined as being infected by S. maltophilia if they tested positive with appropriate phenotypical or molecular laboratory tests. The frequency of resistance was determined by a standard antimicrobial susceptibility test. Results from disk diffusion, dilution methods, and automated systems were accepted for the definition of resistance as well.
Statistical analysis
The main target of the present study was to determine the global prevalence of antibiotic resistance among clinical isolates of S. maltophilia to different classes of antibiotics. The resistance rates for all antimicrobial agents are depicted through a forest plot diagram its pertinent 95% confidence interval (CI). Subgroup analysis was performed to investigate differences in prevalence between antibiotics, to compare the resistance rates based on countries and continents, antimicrobial susceptibility testing (AST) methods used (disk diffusion, dilution methods, automated systems), year of publication (1958–2010 versus 2011–2023), quality assessment scores, and AST guidelines applied (CLSI, EUCAST, Other) (Supplementary Table S2). Meta-regression analysis conducted by moderator analysis for publication years is shown in the supplementary Figure file. The examination was executed employing proportions as the resultant measures. A random-effects model was applied to all information gathered. The level of heterogeneity (i.e., τ2) was estimated using the DerSimonian-Laird estimator [14]. In addition to the estimate of τ2, the Q-test for heterogeneity and the I2 statistic are reported. Studies with a studentized residual larger than the 100 × (1-0.05/(2×k))th percentile of a standard normal distribution were considered potential outliers and were excluded from the analyses. The rank correlation test [15] and the regression test [16] used the standard error of the observed outcomes as a predictor to check for funnel plot asymmetry. The analysis was carried out using R (version 4.2.1) and the metafor package (version 3.8.1) [17, 18]. P < 0.05 was considered statistically significant.
Results
Search results
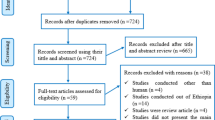
The process for the selection of articles is shown in Fig. 1. A total of 11,438 articles was identified by searching the four electronic databases mentioned above.
After removing duplicates (n = 7285), the titles and abstracts of 4664 articles were screened. Of these, 525 met the inclusion criteria and were retained for full-text review. Of the 525 studies, 236 were excluded because they were non-original studies, conference abstracts, reviews, articles without full text, studies with inappropriate data, or lacking susceptibility testing data or resistance data. A total of 289 studies were finally eligible for inclusion in the present systematic review and meta-analysis [19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171,172,173,174,175,176,177,178,179,180,181,182,183,184,185,186,187,188,189,190,191,192,193,194,195,196,197,198,199,200,201,202,203,204,205,206,207,208,209,210,211,212,213,214,215,216,217,218,219,220,221,222,223,224,225,226,227,228,229,230,231,232,233,234,235,236,237,238,239,240,241,242,243,244,245,246,247,248,249,250,251,252,253,254,255,256,257,258,259,260,261,262,263,264,265,266,267,268,269,270,271,272,273,274,275,276,277,278,279,280,281,282,283,284,285,286,287,288,289,290,291,292,293,294,295,296,297,298,299,300,301,302,303,304,305,306,307,308] (Supplementary Table S1).
Characteristics of the included studies
Overall, the analysis encompassed a total of 289 studies conducted between the years 1958 and 2023. These articles exhibited an extensive geographical reach, with studies executed in various regions across the globe. Most of the studies were sourced from Asia (n = 125, 42.95%), followed by the European region (n = 86, 29.55%), North America (n = 43, 14.77%), South America (n = 10, 3.43%), Africa (n = 9, 3.09%), and, finally, Australia (n = 1, 0.3%). A total of seventeen studies (5.8%) were conducted simultaneously on different continents and therefore classified as multi-continental. Utilization of standards in interpreting susceptibility outcomes with the application of dissimilar breakpoints displayed variation. Amongst the guidelines utilized in the interpretation of antimicrobial susceptibilities, those from Clinical & Laboratory Standards Institute (CLSI) were the most widely employed. The NOS critical appraisal checklist was utilized to evaluate the reviewed studies’ characteristics. Out of the 289 studies that were analysed, 72 (24.7%) received high-quality scores, 190 (65.3%) received moderate-quality scores, and 29 (10%) received low-quality scores. Resistance to trimethoprim-sulfamethoxazole and ceftazidime was detected in most studies (n = 225, 77.31%) included in the meta-analysis.
Meta-analysis results
The resistance rate to different antimicrobial agents and the subgroup analysis by continent, country, year of publication, method of susceptibility testing, quality score, and guideline were presented in supplementary Table S2 and Fig. 3-5. Furthermore, a more comprehensive examination has been conducted below regarding the dissemination of resistance towards certain crucial antibiotics highlighted in the CLSI, EUCAST, and FDA reports Fig. 6.
According to the results as shown in the forest plot diagram in Fig. 2, the highest resistance rate was documented for doripenem (97%), cefoxitin (96%), imipenem and cefuroxime (95%), ampicillin (94%), ceftriaxone (92%), aztreonam (91%) and meropenem (90%), respectively. The lowest resistance rates were found for minocycline (3%), cefiderocol (4%), doxycycline (7%) and gatifloxacin (9%).
Comparing the antibiotic resistance rates among S. maltophilia collections according to the continent of origin (Figs. 3 and 4) revealed that the highest resistance to imipenem was reported from South America (98%), Australia (98%), and Europe (97%). While the highest rate of resistance in other continents, such as North America, Africa, and Asia was found for ceftizoxime (99%), tigecycline (98%), and ampicillin (95%).
A subgroup meta-analysis examined antibiotic resistance rates before and after 2010. This revealed a considerable escalation in resistance toward certain antibiotics such as tigecycline, and ceftolozan/tazobactam in more recent times. In contrast, we found a decreased resistance rate against trimethoprim, tetracycline, imipenem, and amoxicillin/clavulanate (Fig. 5). Based on the results of Egger’s and Begg’s tests, there was a publication bias in the meta-analysis of imipenem, levofloxacin, minocycline. Due to this publication bias, the proportion of resistance to imipenem, levofloxacin, minocycline changed to 0.92, 0.20 and 0.06, respectively, after applying the fill and trim method (Table 1).
Prevalence of TMP-SMX resistance
A total of 33,188 isolates that were investigated in 225 studies were subjected to TMP-SMX resistance testing. The estimated average proportion through the employment of the random-effects model was µ = 0.147 (95%CI, 0.127, 0.169). The Q-test analysis presented evidence of heterogeneity among the actual outcomes Q (224) = 3955.963, I2 = 94.34%, P < 0.001. There was no significant difference in subgroup analysis (P > 0.05). According to the results of the meta-regression analysis, the prevalence of resistance was not correlated to the year of publication (r = 0.010, P = 0.394).
Prevalence of ceftazidime resistance
A total of 26,269 isolates that were investigated in 225 studies were subjected to ceftazidime resistance testing. The estimated average proportion by employing the random-effects model was µ = 0.500 (95% CI, 0.471, 0.529). The Q-test analysis presented evidence of heterogeneity among the actual outcomes Q (224) = 3422.047, I2 = 93.45%, P < 0.001. Due to the subgroup analysis, the difference between countries and AST guidelines was significant (P < 0.001). Hungary exhibited the highest resistance level among the countries that provided data on the prevalence of resistance to ceftazidime. At the same time, Poland demonstrated the lowest resistance level compared to the other countries (0.98 and 0.14, respectively). Most of the literature consulted the CLSI guidelines to determine the resistance level (Supplementary Table S2). According to the results of the meta-regression analysis, the prevalence of resistance was not correlated to the year of publication (r = -0.004, P = 0.572).
Prevalence of levofloxacin resistance
A total of 26,496 isolates that were investigated in 163 studies were subjected to levofloxacin resistance testing. The estimated average proportion by employing the random-effects model was µ = 0.160 (95%CI, 0.139, 0.184). The Q-test analysis presented evidence of heterogeneity among the actual outcomes Q (162) = 2580.510, I2 = 93.72%, P < 0.001. As a consequence of the subgroup analysis, a significant difference was found between continents and countries (P < 0.001). South America displayed the highest prevalence of resistance (0.21). Compared to the other countries that reported the prevalence of resistance, Malawi exhibited the highest resistance level (0.84). The automated system detected the highest number of resistant isolates. (Supplementary Table S2). The rank correlation and the regression test demonstrated potential funnel plot asymmetry (0.015 and < 0.001, respectively). Due to this publication bias, the implementation of the fill and trim method changed the proportion to 0.207 (95%CI, 0.181, 0.235). According to the results of the meta-regression analysis, the prevalence of resistance was not correlated to the year of publication (r = -0.023, P = 0.119).
Prevalence of chloramphenicol resistance
A total of 5815 isolates that were investigated in 56 studies were subjected to chloramphenicol resistance testing. The estimated average proportion through the employment of the random-effects model was µ = 0.292 (95%CI, 0.237, 0.353). The Q-test analysis presented evidence of heterogeneity among the actual outcomes Q (55) = 882.229, I2 = 93.77%, P < 0.001. As a consequence of the subgroup analysis, a significant difference was found between the AST method (P = 0.01). The automated system yielded the greatest quantity of resistant isolates. (0.51). According to the results of the meta-regression analysis, the prevalence of resistance was not correlated to the year of publication (r = 0.011, P = 0.629).
Prevalence of ticarcillin/clavulanic acid resistance
A total of 11,059 isolates that were investigated in 85 studies were subjected to ticarcillin/clavulanate resistance testing. The estimated average proportion through the employment of the random-effects model was µ = 0.313 (95% CI, 0.265, 0.364). The Q-test analysis presented evidence of heterogeneity among the actual outcomes (84) = 1649.878, I2 = 94.91%, P < 0.001. As a consequence of the subgroup analysis, the difference between countries and continents was significant (P < 0.001). Concerning the continents, North America and Europe displayed the highest prevalence of ticarcillin/clavulanic resistance (0.46 and 0.42, respectively). Furthermore, among the countries that reported the prevalence, Switzerland and Canada showed the most significant resistance level compared to other countries (0.87 and 0.73, respectively). (Supplementary Table S2). According to the results of the meta-regression analysis, the prevalence of resistance was not correlated to the year of publication (r = -0.001, P = 0.930).
Prevalence of tigecycline resistance
A total of 5892 isolates that were investigated in 45 studies were subjected to tigecycline resistance testing. The estimated average proportion through the employment of the random-effects model was µ = 0.214 (95%CI, 0.154, 0.291). The Q-test analysis presented evidence of heterogeneity among the actual outcomes Q (44) = 1017.756, I2 = 95.68%, P < 0.001. Due to the subgroup analysis, the difference between countries, continents, and the AST method was significant (P < 0.001). Concerning the continents, Africa displayed the highest prevalence of resistance (0.98). Furthermore, among the countries that reported the rate of resistance, Egypt showed the most significant resistance level compared to other countries (0.98). Most of the literature consulted the dilution method to determine the resistance (Supplementary Table S2). According to the results of the meta-regression analysis, the prevalence of resistance was weakly correlated to the year of publication (r = 0.212, P < 0.001).
Prevalence of minocycline resistance
A total of 11,507 isolates that were investigated in 71 studies were subjected to minocycline resistance testing. The estimated average proportion through the employment of the random-effects model was µ = 0.032 (95%CI, 0.020, 0.051). The Q-test analysis presented evidence of heterogeneity among the actual outcomes Q (70) = 919.005, I2 = 92.38%, P = < 0.001. Due to the subgroup analysis, the difference between the continent and AST methods was significant (P < 0.001). Concerning the continents, Africa displayed the highest prevalence of resistance (0.41). The dilution method was the predominant technique utilized in the literature to determine resistance. The majority of the literature consulted the CLSI guidelines to determine the resistance level (Supplementary Table S2). The rank correlation and the regression test indicated potential funnel plot asymmetry (0.003 and < 0.001, respectively). Due to this publication bias, the implementation of the fill and trim method resulted in a proportion change of 0.064 (95%CI, 0.042, 0.096). According to the results of the meta-regression analysis, the prevalence of resistance was not correlated to the year of publication (r = 0.050, P = 0.270).
Prevalence of colistin resistance
A total of 6807 isolates that were investigated in 57 studies were subjected to colistin resistance testing. The estimated average proportion through the employment of the random-effects model was µ = 0.446 (95%CI, 0.371, 0.525). The Q-test analysis presented evidence of heterogeneity among the actual outcomes Q (56) = 1364.348, I2 = 95.90%, P < 0.001. As a consequence of the subgroup analysis, a significant difference was found between countries and the AST method (P < 0.001). Somalia displayed the highest prevalence of resistance compared to the other countries (0.97). The most resistant isolates were detected by dilution methods (0.53). According to the results of the meta-regression analysis, the prevalence of resistance was not correlated to the year of publication (r = 0.017, P = 0.660).
Prevalence of cefiderocol resistance
A total of 1224 isolates that were investigated in 7 studies were subjected to cefiderocol resistance testing. The estimated average proportion through the employment of the random-effects model was µ = 0.047 (95% CI, 0.001, 0.785). The Q-test analysis presented evidence of heterogeneity among the actual outcomes Q (6) = 175.191, I2 = 96.58%, P < 0.001. There was no significant difference in subgroup analysis (P > 0.05). According to the results of the meta-regression analysis, the prevalence of resistance was not correlated to the year of publication (r = 2.312, P = 0.294).
Discussion
Several antimicrobial agents have been recommended for treating S. maltophilia infections and TMP-SMX, minocycline, tigecycline, levofloxacin, and cefiderocol are among these [8]. TMP-SMX and minocycline are recommended by the Infectious Diseases Society of America (IDSA) panel as the preferred drugs for monotherapy of mild infections and as part of combination therapy for moderate to severe infections. A second agent such as minocycline (preferred), tigecycline, levofloxacin, or cefiderocol can be added in case of a slow response to monotherapy [5]. The accurate performance of AST for S. maltophilia remains challenging due to the limited clinical data available regarding the relevance of in vitro assays. According to CLSI reviewed S. maltophilia breakpoints in 2019 because of this limitation, the CLSI S. maltophilia breakpoints have not been updated [309]. The lack of uniform breakpoints can be attributed to several unknown factors, including microbiological, clinical and pharmacokinetic/pharmacodynamic PK/PD data typically used to establish such breakpoints [310, 311]. The inadequate information available may have a considerable impact on the treatment of patients. Still, CLSI has established MIC interpretation criteria for seven antibiotics, including TMP-SMX, ticarcillin-clavulanate, ceftazidime, cefiderocol, levofloxacin, minocycline, and chloramphenicol. In contrast, The European Committee on Antimicrobial Susceptibility Testing (EUCAST) has defined MIC and disc breakpoints for only TMP-SMX. However, ticarcillin-clavulanate is no longer in production, and the utilization of chloramphenicol is infrequent in the United States due to its considerable toxicity. This leaves only five agents with interpretable antibiotic MIC data available to clinicians and for clinically relevant application in AST [4, 5]. Our comprehensive meta-analysis found that most studies were performed in the Asian continent (n = 125) and the highest and lowest global resistant rates were for doripenem and minocycline, respectively (Fig. 2). The general prevalence of resistance to TMP-SMX stands at a rather low 14.7%. Notably, South America has recorded the lowest rate of resistance. In investigating the global antibiotic resistance of S. maltophilia, two meta-analysis studies were conducted by Banar et al. [311] and Dadashi et al. [312]. The main advantage of our study compared to those is that we analyse antibiotic resistance rates over a wider time period (1958- May 2023) and accomplish a comprehensive investigation of resistance rates to further antibiotics. The aforementioned studies found that the resistance rate to TMP-SMX was lower than the rate observed in our study. These discrepancies can be explained due to their fewer studies than ours and the inclusion of studies that only used the CLSI guidelines to interpret antibiotic susceptibility data by Dadashi et al. [312]. Furthermore, the prevalence of resistance to this drug has not exhibited significant change (p > 0.01) during two distinct periods (14.4% from 1958 to 2010 vs. 14.6% from 2011 to 2023), thereby indicating the constant efficacy of this drug in managing S. maltophilia infections. Epidemiological studies have consistently demonstrated the efficacy of TMP-SMX, with a likelihood of activity exceeding 90% against S. maltophilia [5]. This antibiotic has nearly identical breakpoints for EUCAST (> 4 mg/L) and CLSI (≥ 4 mg/L). Therefore, a difference in resistance rates according to the breakpoint used was also observed in our study, so the prevalence was 12.8% (95% CI, 8.5–18.7%) using EUCAST, but 16.2% (95% CI, 13.4–19.3%) using CLSI.
In the tetracycline group, tetracycline exhibited the highest level of antibiotic resistance (73.7%), but resistance has decreased since 2010. However, there have been few reports on determining tetracycline susceptibility in this period. Resistance to minocycline and especially tigecycline has increased compared to previous decades and there are more reports of AST. Minocycline and tigecycline are used as second-line drugs to treat S. maltophilia infections. These drugs exhibit extensive penetration into lung tissue and have low MICs in surveillance studies against S. maltophilia, with activity against approximately 70–90% of isolates [5]. The guideline issued by the IDSA suggests using an elevated dosage regimen of minocycline as the primary monotherapy agent for mild infections. In cases of TMP-SMX and levofloxacin resistance, minocycline is also often used., as resistance to them is associated with multidrug efflux pumps but does not appear to impact minocycline susceptibility [313]. This antibiotic has minimal potential for interactions with other drugs and exhibits a relatively favorable tolerability profile [4]. Our meta-analysis found the lowest resistance rate for minocycline (3.2%). Similar to ours, Dadashi et al. [312] and Banar et al. also found minocycline as the best antibiotic against S. maltophilia isolates. On the other hand, tigecycline for treating community-acquired bacterial pneumonia was approved by the US Food and Drug Administration (FDA) in 2005 [9]. In our meta-analysis, the resistance rate to tigecycline was higher than minocycline (21.4). In our meta-analysis, the resistance rate to tigecycline was higher than minocycline (21.4). According to our meta-analysis data, a four-fold increase in resistance to tigecycline was seen during the two periods (8.2% in 1958–2010 and 30.2% in 2011–2023). Benar et al. also confirmed a 4-fold increase in resistance to this antibiotic during the years before 2010 compared to after 2010 [311]. In the past, S. maltophilia was effectively treated with β-lactam drugs. However, high rates of resistance are reported for almost all of them. In the penicillin group, all of them exhibited a high level of resistance. Of these, antibiotic susceptibility testing for ticarcillin and piperacillin has been lower from 2011 to 2023. Therefore, the therapeutic guidelines do not recommend using the penicillin group for managing S. maltophilia.
A noteworthy increase in antibiotic resistance has been observed in some members of the cephalosporin group. Specifically, ceftriaxone and cefazolin have exhibited consistent levels of resistance over two distinct periods. The resistance rate to cefotaxim has also decreased during the two periods (86.5% in 1958–2010 and 75.9% in 2011–2023)., which may be attributed to a limited number of reports during this interval. Contrarily, despite numerous reports of susceptibility to cefoperazone, a low level of susceptibility was noted during the same period. Carbapenem resistance poses a major obstacle for healthcare providers, with levels found to be at 90% or more. Among them, antibiotic susceptibility testing to meropenem and imipenem has been reported in most studies. Meropenem resistance has been consistently high two times, with rates of 92.2% from 1958 to 2010 and 88.2% from 2011 to 2023. Our meta-analysis found the lowest resistance rate for imipenem (95.8%), although due to publication bias, according to Trim and Fill analysis, the prevalence of resistance to this antibiotic is 92.1%. Nevertheless, it is noteworthy that resistance to imipenem has declined during the aforementioned chronological intervals. In the combination of β-lactam and inhibitor group, most studies have reported the antibiotic susceptibility testing to ticarcillin/clavulanate and piperacillin/tazobactam. The overall resistance rate to piperacillin/tazobactam was 2-fold compared to ticarcillin/clavulanate. However, it is noteworthy that the resistance rate has remained constant for ticarcillin/clavulanate and a slight increase for piperacillin/tazobactam throughout the period spanning from 1958 to 2010 and from 2011 to 2023. In addition, the number of reports evaluating the susceptibility of these two antibiotics was lower after 2010 rather than before 2010.
Only ticarcillin/clavulanate, ceftazidime, and cefiderocol have MIC interpretive criteria based on the CLSI guidelines among the β-lactam agents. Previously, ticarcillin/clavulanate and ceftazidime showed favorable efficacy in treating S. maltophilia. Susceptibility to these two antibiotics has decreased in recent studies [3]. Our study suggests that the resistance rate to ceftazidime was 50%, and the resistance rate remained constant during two periods. Benar et al. [311]. also reported the same rate of resistance to ceftazidime as ours. The IDSA panel does not recommend the prescription of ceftazidime for managing S. maltophilia infections due to its ineffectiveness against S. maltophilia isolates, even in cases where these isolates are susceptible in vitro [5]. Furthermore, an additional concern about inactivating β-lactamases is the potential for inaccuracy and non-reproducibility of ceftazidime [303, 314]. Furthermore, an additional issue that could be associated with the existence of inactivating β-lactamases is that the MIC of ceftazidime against S. maltophilia may not be precise and reproducible when utilizing AST that is typically utilized by clinical microbiology laboratories. Currently, the CLSI provides the breakpoint for ceftazidime in clinical settings; however, a few older reports (7 studies) have interpreted the breakpoint for ceftazidime based on previous versions of the EUCAST. Ticarcillin/clavulanic acid exhibited a resistance rate of 31.3%, which is similar to the results conducted by Banar et al. [311]. Like ceftazidime, the resistance rates to ticarcillin/clavulanic acid did not change during two periods (P > 0.01). Previous investigations have demonstrated that the susceptibility rates of S. maltophilia to the aforementioned antibiotic during 1997–1998 ranged from 71 to 90% but dropped to 27–46.1% during 2003–2008 [4]. In this meta-analysis, the antibiotic effectivity of cefiderocol as a novel siderophore cephalosporin was determined in a few studies (7 reports) with a low prevalence but a high heterogenicity (4.7%; 95% CI: 1-78.5%). All of them were performed after 2010 with the disk diffusion method. The majority of reports were in European countries. Cefiderocol exhibits favorable activity in vitro against S. maltophilia because of its stability against both serine and metallo-β-lactamases, as well as demonstrated MIC90 values that were as low as 0.12–0.5 mg/L, even if the isolates displayed resistance to TMP-SMX and/or levofloxacin [279, 315]. Despite the restricted accessibility of clinical data, it has been indicated through in vitro data and animal models that there is substantial potential for the utilization of cefiderocol in treating infections caused by S. maltophilia. The IDSA panel suggests that, although cefiderocol monotherapy may be effective for mild infections, combining cefiderocol with another agent should be used to treat moderate and severe S. maltophilia infections [5]. Using fluoroquinolones, particularly levofloxacin, as a second-line therapy is often implemented when resistance to TMP-SMX or where the administration is impossible due to a life-threatening allergy or other clinical factors [8]. There have been few reports of susceptibility testing for the fluoroquinolone group except for levofloxacin and ciprofloxacin. Amongst the class of quinolone and fluoroquinolone agents, ciprofloxacin had the highest resistance rate (46%), with a constant resistance trend over two periods. Although, few studies reported antibiotic susceptibility of ciprofloxacin in recent decades. Our study shows that the resistance rate to levofloxacin was relatively low (16%), although due to publication bias, the prevalence of resistance to this antibiotic is 20.7% according to trim and fill analysis. Banar et al. revealed a global resistance rate to levofloxacin exceeding our findings at 19.7% in contrast to our 17.7%. They showed a significant difference in the prevalence of resistance between the different regions [311]. On the other hand, Dadashi et al. highlighted a global prevalence of resistance to levofloxacin lower than ours (14.4% vs. 17.7%) due to the fewer included studies. The prevalence of resistance to this drug has decreased in two recent decades. The restricted application of this antibiotic in recent times can be attributed to the likelihood of resistance development during therapy [312]. This is particularly relevant for patients with cystic fibrosis or cirrhosis, who commonly experience frequent or chronic quinolone exposure [8]. Within the aminoglycoside group, every compound exhibited significant degrees of resistance. However, their use in antibiotic susceptibility testing declined during the 2011 to 2023 period due to their inefficiency. The overall resistance rate to chloramphenicol was relatively low (29.2). The frequency of resistance to this medication has experienced a decrease in recent years. The utilization of chloramphenicol in clinical settings is restricted due to its possible adverse effects, such as bone marrow suppression or induction of aplastic anemia [8].
In the present study, the overall resistance rate to colistin was relatively high (46.6%). Colistin treatment provides a rescue therapy for various multidrug-resistant (MDR) Gram-negative infections. However, its application is restricted by its notable nephrotoxicity and the emergence of more advanced, efficacious, and less toxic antimicrobial agents [8]. An increased incidence of colistin-resistant isolates has also been observed in recent years. (31.9% from 1958 to 2010 vs. 44% from 2011 to 2023). Similar to these results, Rodríguez et al. [316]. showed that colistin resistance elevated from 8% in 1996 to 45% in 2013 due to the significant increase (11.4-fold) of colistin usage during the study period. Drug susceptibility testing for Stenotrophomonas spp is obstructed by its diverse mechanisms of drug resistance [8]. Notably, no established CLSI susceptibility criteria exist for any of the polymyxins.
An increasingly common clinical challenge associated with this pathogen is heterogeneous resistance to colistin, whereby distinct subpopulations within a single isolate display different susceptibilities to the antibiotic [316]. There are also challenges with the accuracy and repeatability of polymyxin MICs. Therefore, the IDSA panel recommends avoiding polymyxins for S. maltophilia infections [5]. There are some limitations to our study. First, several studies did not use specific guidelines or report the exact resistance rate. Therefore, the rate of antibiotic resistance may have been affected by these studies not being included in the meta-analysis. Second, the full text of several published studies was not available despite communicating with the corresponding authors by sending several e-mails, and only a few of them responded. Third, certain studies assessed susceptibility rates solely based on MIC50/90 without reporting prevalence. Therefore, these studies, which may have influenced the pooled prevalence of antimicrobial resistance, were excluded from the meta-analysis.
Conclusion
According to our meta-analysis, due to the low rates of resistance to minocycline and cefiderocol, these two antibiotics can be suggested as the preferred therapeutic options for treating most if not all infections caused by S. maltophilia. TMP-SMX, as a first-choice drug of S. maltophilia, indicated the low rates of resistance worldwide. Hence, it seems that this drug is still an effective therapeutic option. Also, due to the high-frequency resistance to β-lactams (except cefiderocol), especially carbapenems and aminoglycosides, in the last two decades, these antibiotic groups should not be recommended in therapeutic guidelines, especially as monotherapy. On the other hand, the prevalence rates of antimicrobial resistance in S. maltophilia in the African continent are limited by the few numbers of studies. Hence, a regular monitoring and surveillance program should be carried out to determine the antibiotic sensitivity of this bacterium across this continent.
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Abbreviations
- TMP-SMX:
-
Trimethoprim-sulfamethoxazole
- RND:
-
Resistance Nodulation Division
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- NOS:
-
Newcastle-Ottawa scale
- CI:
-
confidence interval
- AST:
-
antimicrobial susceptibility testing
- CLSI:
-
Clinical & Laboratory Standards Institute
- EUCAST:
-
The European Committee on Antimicrobial Susceptibility Testing
- FDA:
-
US Food and Drug Administration
- MDR:
-
multidrug-resistant
- IDSA:
-
Infectious Diseases Society of America
References
Cerezer VG, Bando SY, Pasternak J, Franzolin MR, Moreira-Filho CA. Phylogenetic analysis of Stenotrophomonas spp. isolates contributes to the identification of nosocomial and community-acquired infections. Biomed Res Int. 2014;2014:151405.
Majumdar R, Karthikeyan H, Senthilnathan V, Sugumar S. Review on Stenotrophomonas maltophilia: an emerging Multidrug- resistant opportunistic Pathogen. Recent Pat Biotechnol. 2022;16(4):329–54.
Brooke JS. Stenotrophomonas maltophilia: an emerging global opportunistic pathogen. Clin Microbiol Rev. 2012;25(1):2–41.
Mojica MF, Humphries R, Lipuma JJ, Mathers AJ, Rao GG, Shelburne SA, Fouts DE, Van Duin D, Bonomo RA. Clinical challenges treating Stenotrophomonas maltophilia infections: an update. JAC Antimicrob Resist. 2022;4(3):dlac040.
Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ. Infectious Diseases Society of America Guidance on the treatment of AmpC beta-lactamase-producing enterobacterales, Carbapenem-Resistant Acinetobacter baumannii, and Stenotrophomonas maltophilia infections. Clin Infect Dis. 2022;74(12):2089–114.
Cho SY, Kang CI, Kim J, Ha YE, Chung DR, Lee NY, Peck KR, Song JH. Can levofloxacin be a useful alternative to trimethoprim-sulfamethoxazole for treating Stenotrophomonas maltophilia bacteremia? Antimicrob Agents Chemother. 2014;58(1):581–3.
Sánchez MB. Antibiotic resistance in the opportunistic pathogen Stenotrophomonas maltophilia. Front Microbiol. 2015;6:658.
Gibb J, Wong DW. Antimicrobial treatment strategies for Stenotrophomonas maltophilia: a focus on Novel therapies. Antibiot (Basel) 2021, 10(10).
Kullar R, Wenzler E, Alexander J, Goldstein EJC. Overcoming Stenotrophomonas maltophilia Resistance for a more rational Therapeutic Approach. Open Forum Infect Dis. 2022;9(5):ofac095.
Chang YT, Lin CY, Chen YH, Hsueh PR. Update on infections caused by Stenotrophomonas maltophilia with particular attention to resistance mechanisms and therapeutic options. Front Microbiol. 2015;6:893.
Mercier-Darty M, Royer G, Lamy B, Charron C, Lemenand O, Gomart C, Fourreau F, Madec JY, Jumas-Bilak E, Decousser JW. Comparative whole-genome phylogeny of animal, Environmental, and human strains confirms the Genogroup Organization and Diversity of the Stenotrophomonas maltophilia Complex. Appl Environ Microbiol 2020, 86(10).
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906.
Modesti PA, Reboldi G, Cappuccio FP, Agyemang C, Remuzzi G, Rapi S, Perruolo E, Parati G. Settings ESHWGoCRiLR: panethnic differences in blood pressure in Europe: a systematic review and Meta-analysis. PLoS ONE. 2016;11(1):e0147601.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Becker LM. The effects of exercise versus methylphenidate on attention and behavior in children with attention deficit hyperactivity disorder, predominantly inattentive type. The University of Alabama at Birmingham; 1997.
Sterne JA, Egger M. Regression methods to detect publication and other bias in meta-analysis. Publication bias meta‐analysis: Prev Assess Adjustments 2005:99–110.
Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36(3):1–48.
Team RC. R Core Team R: a language and environment for statistical computing. Foundation for Statistical Computing; 2020.
Hamdi AM, Fida M, Abu Saleh OM, Beam E. Stenotrophomonas bacteremia antibiotic susceptibility and prognostic determinants: Mayo Clinic 10-year experience. Open Forum Infectious diseases: 2020. Oxford University Press US; 2020. p. ofaa008.
Hanberger H, Erlandsson M, Burman LG, Cars O, Gill H, Lindgren S, Nilsson LE, Olsson-Liljequist B, Walther S. Group I-SS: high antibiotic susceptibility among bacterial pathogens in Swedish ICUs Report from a nation-wide surveillance program using TA90 as a novel index of susceptibility. Scand J Infect Dis. 2004;36(1):24–30.
Hanberger H, Nilsson LE, Group SS. High frequency of antibiotic resistance among Gram-negative isolates in intensive care units at 10 Swedish hospitals. Clin Microbiol Infect. 1997;3(2):208–15.
Hand E, Davis H, Kim T, Duhon B. Monotherapy with minocycline or trimethoprim/sulfamethoxazole for treatment of Stenotrophomonas maltophilia infections. J Antimicrob Chemother. 2016;71(4):1071–5.
Herrera-Heredia SA, Pezina-Cantu C, Garza-Gonzalez E, Bocanegra-Ibarias P, Mendoza-Olazaran S, Morfin-Otero R, Camacho-Ortiz A, Villarreal-Trevino L, Rodriguez-Noriega E, Palau-Davila L, et al. Risk factors and molecular mechanisms associated with trimethoprim-sulfamethoxazole resistance in Stenotrophomonas maltophilia in Mexico. J Med Microbiol. 2017;66(8):1102–9.
Ho MC, Hsiao CH, Sun MH, Hwang YS, Lai CC, Wu WC, Chen KJ. Antimicrobial susceptibility, minimum inhibitory concentrations, and clinical profiles of Stenotrophomonas maltophilia Endophthalmitis. Microorganisms. 2021;9(9):1840.
Hoban DJ, Bouchillon SK, Johnson JL, Zhanel GG, Butler DL, Miller LA, Poupard JA, Gemifloxacin Surveillance Study Research G. Comparative in vitro activity of gemifloxacin, ciprofloxacin, levofloxacin and ofloxacin in a north American surveillance study. Diagn Microbiol Infect Dis. 2001;40(1–2):51–7.
Hoban DJ, Bouchillon SK, Johnson JL, Zhanel GG, Butler DL, Saunders KA, Miller LA, Poupard JA, Surveillance Study Research G. Comparative in vitro potency of amoxycillin-clavulanic acid and four oral agents against recent north American clinical isolates from a global surveillance study. Int J Antimicrob Agents. 2003;21(5):425–33.
Hohl P, Frei R, Aubry P. In vitro susceptibility of 33 clinical case isolates of Xanthomonas maltophilia. Inconsistent correlation of agar dilution and of disk diffusion test results. Diagn Microbiol Infect Dis. 1991;14(5):447–50.
Hombach M, Bloemberg GV, Bottger EC. Effects of clinical breakpoint changes in CLSI guidelines 2010/2011 and EUCAST guidelines 2011 on antibiotic susceptibility test reporting of Gram-negative bacilli. J Antimicrob Chemother. 2012;67(3):622–32.
Hotta G, Matsumura Y, Kato K, Nakano S, Yunoki T, Yamamoto M, Nagao M, Ito Y, Takakura S, Ichiyama S. Risk factors and outcomes of Stenotrophomonas maltophilia bacteraemia: a comparison with bacteraemia caused by Pseudomonas aeruginosa and Acinetobacter species. PLoS ONE. 2014;9(11):e112208.
Hrbacek J, Cermak P, Zachoval R. Current antibiotic resistance patterns of rare uropathogens: survey from central European Urology Department 2011–2019. BMC Urol. 2021;21(1):61.
Hsueh P-R, Chen W-H, Luh K-T. Relationships between antimicrobial use and antimicrobial resistance in Gram-negative bacteria causing nosocomial infections from 1991–2003 at a university hospital in Taiwan. Int J Antimicrob Agents. 2005;26(6):463–72.
Hsueh S-C, Lee Y-J, Huang Y-T, Liao C-H, Tsuji M, Hsueh P-R. In vitro activities of cefiderocol, ceftolozane/tazobactam, ceftazidime/avibactam and other comparative drugs against imipenem-resistant Pseudomonas aeruginosa and Acinetobacter baumannii, and Stenotrophomonas maltophilia, all associated with bloodstream infections in Taiwan. J Antimicrob Chemother. 2019;74(2):380–6.
Hu LF, Chang X, Ye Y, Wang ZX, Shao YB, Shi W, Li X, Li JB. Stenotrophomonas maltophilia resistance to trimethoprim/sulfamethoxazole mediated by acquisition of Sul and dfrA genes in a plasmid-mediated class 1 integron. Int J Antimicrob Agents. 2011;37(3):230–4.
Hu LF, Chen GS, Kong QX, Gao LP, Chen X, Ye Y, Li JB. Increase in the prevalence of Resistance determinants to Trimethoprim/Sulfamethoxazole in Clinical Stenotrophomonas maltophilia isolates in China. PLoS ONE. 2016;11(6):e0157693.
Hu LF, Gao LP, Ye Y, Chen X, Zhou XT, Yang HF, Liiu YY, Mei Q, Li JB. Susceptibility of Stenotrophomonas maltophilia clinical strains in China to antimicrobial combinations. J Chemother. 2014;26(5):282–6.
Hu L-F, Xu X-H, Li H-R, Gao L-P, Chen X, Sun N, Liu Y-Y, Ying H-F, Li J-B. Surveillance of antimicrobial susceptibility patterns among Stenotrophomonas maltophilia isolated in China during the 10-year period of 2005–2014. J Chemother. 2018;30(1):25–30.
Huang CR, Chen SF, Tsai NW, Chang CC, Lu CH, Chuang YC, Chien CC, Chang WN. Clinical characteristics of Stenotrophomonas maltophilia meningitis in adults: a high incidence in patients with a postneurosurgical state, long hospital staying and antibiotic use. Clin Neurol Neurosurg. 2013;115(9):1709–15.
Hussain Qadri S, Ueno Y, Saldin H, Markley Burdette J, Lee GC. Comparative antibacterial activity of the new fluoroquinolone PD 131628. Drug Invest. 1992;4:409–15.
Saied WI, Merceron S, Schwebel C, Le Monnier A, Oziel J, Garrouste-Orgeas M, Marcotte G, Ruckly S, Souweine B, Darmon M. Ventilator-associated pneumonia due to Stenotrophomonas maltophilia: risk factors and outcome. J Infect. 2020;80(3):279–85.
Ince N, Yekenkurul D, Danis A, Caliskan E, Akkas I. An evaluation of six-year Stenotrophomonas maltophilia infections in a university hospital. Afr Health Sci. 2020;20(3):1118–23.
Insuwanno W, Kiratisin P, Jitmuang A. Stenotrophomonas maltophilia infections: clinical characteristics and Factors Associated with mortality of hospitalized patients. Infect Drug Resist. 2020;13:1559–66.
Isenberg HD, Alperstein P, France K. In vitro activity of ciprofloxacin, levofloxacin, and trovafloxacin, alone and in combination with beta-lactams, against clinical isolates of Pseudomonas aeruginosa, Stenotrophomonas maltophilia, and Burkholderia cepacia. Diagn Microbiol Infect Dis. 1999;33(2):81–6.
Ismail N, Zam Z, Hassan SA, Rahman ZA. A combination of trimethoprim-sulfamethoxazole and ceftazidime showed good in vitro activity against Stenotrophomonas maltophilia. Malaysian J Med Sciences: MJMS. 2017;24(2):21.
Jacquier H, Le Monnier A, Carbonnelle E, Corvec S, Illiaquer M, Bille E, Zahar JR, Jaureguy F, Fihman V, Tankovic J, et al. In vitro antimicrobial activity of last-resort antibiotics against unusual nonfermenting gram-negative bacilli clinical isolates. Microb Drug Resist. 2012;18(4):396–401.
Jean S-S, Lee Y-L, Liu P-Y, Lu M-C, Ko W-C, Hsueh P-R. Multicenter surveillance of antimicrobial susceptibilities and resistance mechanisms among Enterobacterales species and non-fermenting gram-negative bacteria from different infection sources in Taiwan from 2016 to 2018. J Microbiol Immunol Infect. 2022;55(3):463–73.
Ji Y, Jiang C, Ji J, Luo Y, Jiang Y, Lu Y. Post-cataract endophthalmitis caused by multidrug-resistant Stenotrophomonas maltophilia: clinical features and risk factors. BMC Ophthalmol. 2015;15(1):14.
Jia W, Wang J, Xu H, Li G. Resistance of Stenotrophomonas maltophilia to fluoroquinolones: Prevalence in a University Hospital and possible mechanisms. Int J Environ Res Public Health. 2015;12(5):5177–95.
Jian J, Xie Z, Chen L. Risk factors for mortality in hospitalized patients with Stenotrophomonas maltophilia bacteremia. Infect Drug Resist. 2022;15:3881–6.
Jitendranath A, Radhika R, Bhargavi L, Bhai G, Bai R. Current trend of nonfermenting Gram negative bacilli in a tertiary care hospital in Trivandrum. J Pure Appl Microbiol. 2016;10(1):425–9.
Johnson DM, Jones RN. CQ-397 and CQ-414: antimicrobial activity and spectrum of two fluoroquinolone—cephalosporin, dual-action compounds with carboxamido bonds. Clin Microbiol Infect. 1997;3(3):335–44.
Jones BM, Wagner JL, Chastain DB, Bookstaver PB, Stover K, Lin J, Matson H, White N, Motesh M, Bland CM. Real-world, multicentre evaluation of the incidence and risk factors for non-susceptible Stenotrophomonas maltophilia isolates. J Glob Antimicrob Resist. 2022;28:282–7.
Jones RN, Huynh HK, Biedenbach DJ, Fritsche TR, Sader HS. Doripenem (S-4661), a novel carbapenem: comparative activity against contemporary pathogens including bactericidal action and preliminary in vitro methods evaluations. J Antimicrob Chemother. 2004;54(1):144–54.
Jones RN, Pfaller MA, Marshall SA, Hollis RJ, Wilke WW. Antimicrobial activity of 12 broad-spectrum agents tested against 270 nosocomial blood stream infection isolates caused by non-enteric gram-negative bacilli: occurrence of resistance, molecular epidemiology, and screening for metallo-enzymes. Diagn Microbiol Infect Dis. 1997;29(3):187–92.
Jones RN, Sader HS, Beach ML. Contemporary in vitro spectrum of activity summary for antimicrobial agents tested against 18 569 strains non-fermentative gram-negative bacilli isolated in the SENTRY Antimicrobial Surveillance Program (1997–2001). Int J Antimicrob Agents. 2003;22(6):551–6.
Juhász E, Pongrácz J, Iván M, Kristóf K. Antibiotic susceptibility of sulfamethoxazole-trimethoprim resistant Stenotrophomonas maltophilia strains isolated at a tertiary care centre in Hungary. Acta Microbiol Immunol Hung. 2015;62(3):295–305.
Kanamori H, Yano H, Tanouchi A, Kakuta R, Endo S, Ichimura S, Ogawa M, Shimojima M, Inomata S, Ozawa D, et al. Prevalence of Smqnr and plasmid-mediated quinolone resistance determinants in clinical isolates of Stenotrophomonas maltophilia from Japan: novel variants of Smqnr. New Microbes New Infect. 2015;7:8–14.
Kanchanasuwan S, Rongmuang J, Siripaitoon P, Kositpantawong N, Charoenmak B, Hortiwakul T, Nwabor OF, Chusri S. Clinical characteristics, outcomes, and risk factors for mortality in patients with Stenotrophomonas maltophilia bacteremia. J Clin Med. 2022;11(11):3085.
Karamanlioglu D, Dizbay M. In vitro combination of tigecycline with other antibiotics in Stenotrophomonas maltophilia isolates. Turk J Med Sci. 2019;49(2):683–6.
Madi H, Lukic J, Vasiljevic Z, Biocanin M, Kojic M, Jovcic B, Lozo J. Genotypic and phenotypic characterization of Stenotrophomonas maltophilia strains from a Pediatric Tertiary Care Hospital in Serbia. PLoS ONE. 2016;11(10):e0165660.
Magrum B, Elefritz J, Murphy C, Stevenson K. 599: STENOTROPHOMONAS MALTOPHILIA TRIMETHOPRIM-SULFAMETHOXAZOLE RESISTANCE IN A CRITICALLY ILL POPULATION. Crit Care Med. 2020;48(1):280.
Malekan M, Tabaraie B, Akhoundtabar L, Afrough P, Behrouzi A. Distribution of class I integron and smqnr resistance gene among Stenotrophomonas maltophilia isolated from clinical samples in Iran. Avicenna J Med Biotechnol. 2017;9(3):138.
Malini A, Deepa E, Gokul B, Prasad S. Nonfermenting gram-negative bacilli infections in a tertiary care hospital in Kolar, Karnataka. J Lab Physicians. 2009;1(2):62–6.
Mansouri S, Razavi M, Norouzi F, GHOLAMHOSEINIAN NS. Prevalence of β-Lactamase production and antimicrobial susceptibility of multidrug resistant clinical isolates of non-fermenting Gram negative bacteria from hospitalized patients in Kerman/Iran. 2012.
McKnight AJ, Shaw A, Goldsmith CE, Clarke L, Millar BC, McCaughan J, Elborn JS, Reid A, Moore JE. Comparison of in vitro susceptibilities to levofloxacin and ciprofloxacin with Pseudomonas aeruginosa and Stenotrophomonas maltophilia isolated from cystic fibrosis patients in Northern Ireland. Br J Biomed Sci. 2005;62(1):30–2.
Thipperudraswamy T, Sudhindra K, Nadigar S, Kumar M. Prevalence of non-fermenting Gram negative Bacilli from clinical isolates and their Antibiogram Profile. J Biomedical Pharm Res. 2014;3:55–61.
Memish ZA, Shibl AM, Kambal AM, Ohaly YA, Ishaq A, Livermore DM. Antimicrobial resistance among non-fermenting gram-negative bacteria in Saudi Arabia. J Antimicrob Chemother. 2012;67(7):1701–5.
Mendes ET, Paez JIG, Ferraz JR, Marchi AP, Silva ILAF, Batista MV, Lima ALMd, Rossi F, Levin AS, Costa SF. Clinical and microbiological characteristics of patients colonized or infected by Stenotrophomonas maltophilia: is resistance to sulfamethoxazole/trimethoprim a problem? Revista do Instituto De Medicina Tropical De São Paulo 2020, 62.
Micozzi A, Venditti M, Monaco M, Friedrich A, Taglietti F, Santilli S, Martino P. Bacteremia due to Stenotrophomonas maltophilia in patients with hematologic malignancies. Clin Infect Dis. 2000;31(3):705–11.
Mohagheghzadeh N, Hashemizadeh Z, Khashei R, Kholdi S, Mohebi S, Motamedifar M. High occurrence of antibiotic resistance and biofilm-formation among Stenotrophomonas maltophilia isolated from a tertiary hospital in Southwest of Iran. Gene Rep. 2020;21:100827.
Mojica MF, Rutter JD, Taracila M, Abriata LA, Fouts DE, Papp-Wallace KM, Walsh TJ, LiPuma JJ, Vila AJ, Bonomo RA. Population structure, molecular epidemiology, and β-lactamase diversity among Stenotrophomonas maltophilia isolates in the United States. MBio. 2019;10(4):e00405–00419.
Alqahtani JM. Emergence of Stenotrophomonas maltophilia nosocomial isolates in a Saudi children’s hospital. Risk factors and clinical characteristics. Saudi Med J. 2017;38(5):521–7.
Morrison AJ Jr., Hoffmann KK, Wenzel RP. Associated mortality and clinical characteristics of nosocomial Pseudomonas maltophilia in a university hospital. J Clin Microbiol. 1986;24(1):52–5.
Morrissey I, Olesky M, Hawser S, Lob SH, Karlowsky JA, Corey GR, Bassetti M, Fyfe C. In Vitro Activity of Eravacycline against Gram-negative Bacilli isolated in Clinical Laboratories Worldwide from 2013 to 2017. Antimicrob Agents Chemother. 2020;64(3):e01699–01619.
Morsi S, Sharaf H, Gerges M. Association of Sul genes and class 1 integron with trimethoprimsulfamethoxazole resistance in Stenotrophomonas maltophilia clinical isolates in Zagazig University, Egypt. Afr J Clin Experimental Microbiol. 2016;17(3):158–65.
Mushtaq S, Vickers A, Doumith M, Ellington MJ, Woodford N, Livermore DM. Activity of beta-lactam/taniborbactam (VNRX-5133) combinations against carbapenem-resistant Gram-negative bacteria. J Antimicrob Chemother. 2021;76(1):160–70.
Mutlu M, Yilmaz G, Aslan Y, Bayramoglu G. Risk factors and clinical characteristics of Stenotrophomonas maltophilia infections in neonates. J Microbiol Immunol Infect. 2011;44(6):467–72.
Naas T, Lina G, Santerre Henriksen A, Longshaw C, Jehl F. In vitro activity of cefiderocol and comparators against isolates of Gram-negative pathogens from a range of infection sources: SIDERO-WT-2014–2018 studies in France. JAC-antimicrobial Resist. 2021;3(2):dlab081.
Naeem T, Absar M, Somily AM. Antibiotic resistance among clinical isolates of Stenotrophomonas maltophilia at a teaching hospital in Riyadh, Saudi Arabia. J Ayub Med Coll Abbottabad. 2012;24(2):30–3.
Nair AP, Sasi S, Al Maslamani M, Al-Khal A, Chacko K, Deshmukh A, Abukhattab M. Clinical and Epidemiological Characteristics of Stenotrophomonas maltophilia Associated Lower Respiratory Tract infections in Qatar: a retrospective study. Cureus. 2022;14(3):e23263.
Nayyar C, Thakur P, Tak V, Saigal K. Stenotrophomonas maltophilia: an Emerging Pathogen in Paediatric Population. J Clin Diagn Res. 2017;11(1):DC08–11.
Neela V, Rankouhi SZ, van Belkum A, Goering RV, Awang R. Stenotrophomonas maltophilia in Malaysia: molecular epidemiology and trimethoprim-sulfamethoxazole resistance. Int J Infect Dis. 2012;16(8):e603–607.
Nys C, Cherabuddi K, Venugopalan V, Klinker KP. Clinical and microbiologic outcomes in patients with Monomicrobial Stenotrophomonas maltophilia infections. Antimicrob Agents Chemother. 2019;63(11):e00788–00719.
Magni A, Giordano A, Mancini C, Pecoraro C, Varesi P, Quattrucci S, Trancassini M. Emerging cystic fibrosis pathogens: incidence and antimicrobial resistance. New Microbiol. 2007;30(1):59–62.
Tanimoto K. Stenotrophomonas maltophilia strains isolated from a university hospital in Japan: genomic variability and antibiotic resistance. J Med Microbiol. 2013;62(Pt 4):565–70.
ÇAYCI YT, BIYIK İ, YILMAZ G, BİLGİN K, BIRINCI A. Investigation of in vitro activity of colistin and tygecyclin against Stenotrophomonas maltophilia isolates. J Experimental Clin Med. 2021;38(4):529–32.
Taylor S, Margolick J, Abughosh Z, Goldenberg SL, Lange D, Bowie WR, Bell R, Roscoe D, Machan L, Black P. Ciprofloxacin resistance in the faecal carriage of patients undergoing transrectal ultrasound guided prostate biopsy. BJU Int. 2013;111(6):946–53.
Tebano G, Geneve C, Tanaka S, Grall N, Atchade E, Augustin P, Thabut G, Castier Y, Montravers P, Desmard M. Epidemiology and risk factors of multidrug-resistant bacteria in respiratory samples after lung transplantation. Transpl Infect Dis. 2016;18(1):22–30.
Tian L, Sun Z, Zhang Z. Antimicrobial resistance of pathogens causing nosocomial bloodstream infection in Hubei Province, China, from 2014 to 2016: a multicenter retrospective study. BMC Public Health. 2018;18(1):1121.
Toleman MA, Bennett PM, Bennett DM, Jones RN, Walsh TR. Global emergence of trimethoprim/sulfamethoxazole resistance in Stenotrophomonas maltophilia mediated by acquisition of Sul genes. Emerg Infect Dis. 2007;13(4):559–65.
Travassos LH, Pinheiro MN, Coelho FS, Sampaio JL, Merquior VL, Marques EA. Phenotypic properties, drug susceptibility and genetic relatedness of Stenotrophomonas maltophilia clinical strains from seven hospitals in Rio De Janeiro, Brazil. J Appl Microbiol. 2004;96(5):1143–50.
Tripodi MF, Andreana A, Sarnataro G, Ragone E, Adinolfi LE, Utili R. Comparative activities of isepamicin, amikacin, cefepime, and ciprofloxacin alone or in combination with other antibiotics against Stenotrophomonas maltophilia. Eur J Clin Microbiol Infect Dis. 2001;20(1):73–5.
Trupl J, Kunova A, Oravcova E, Pichňa P, Kukučková E, Grausova S, Grey E, Spanik S, Demitrovióvá A. Kral’ovičová K: resistance pattern of 2 816 isolates isolated from 17 631 blood cultures and etiology of bacteremia and fungemia in a single cancer institution. Acta Oncol. 1997;36(6):643–9.
Vartivarian S, Anaissie E, Bodey G, Sprigg H, Rolston K. A changing pattern of susceptibility of Xanthomonas maltophilia to antimicrobial agents: implications for therapy. Antimicrob Agents Chemother. 1994;38(3):624–7.
Vialichka A, Biagi M, Meyer K, Wu T, Shajee A, Tan X, Wenzler E. Activity of Delafloxacin and Levofloxacin against Stenotrophomonas maltophilia at simulated plasma and Intrapulmonary pH values. Microbiol Spectr. 2022;10(4):e02705–02721.
Vidigal PG, Dittmer S, Steinmann E, Buer J, Rath PM, Steinmann J. Adaptation of Stenotrophomonas maltophilia in cystic fibrosis: molecular diversity, mutation frequency and antibiotic resistance. Int J Med Microbiol. 2014;304(5–6):613–9.
Tsai WP, Chen CL, Ko WC, Pan SC. Stenotrophomonas maltophilia bacteremia in burn patients. Burns. 2006;32(2):155–8.
Tunger O, Vural S, Cetin CB, Keles G, Borand H, Gazi H. Clinical aspects and risk factors of nosocomial Stenotrophomonas maltophilia bacteremia episodes in a Turkish intensive care unit. J Chemother. 2007;19(6):658–64.
Valenza G, Tappe D, Turnwald D, Frosch M, Konig C, Hebestreit H, Abele-Horn M. Prevalence and antimicrobial susceptibility of microorganisms isolated from sputa of patients with cystic fibrosis. J Cyst Fibros. 2008;7(2):123–7.
Vonberg RP, Wolter A, Ziesing S, Gastmeier P. Surveillance of cystic fibrosis patients with multi-drug resistant gram-negative rods. Int J Hyg Environ Health. 2006;209(4):333–6.
Walkty A, Karlowsky JA, Baxter MR, Adam HJ, Zhanel GG. In vitro activity of plazomicin against gram-negative and gram-positive bacterial pathogens isolated from patients in Canadian hospitals from 2013 to 2017 as part of the CANWARD surveillance study. Antimicrob Agents Chemother. 2019;63(1):e02068–02018.
Wang H, Yu Y, Xie X, Wang C, Zhang Y, Yuan Y, Zhang X, Liu J, Wang P, Chen M. In-vitro antibacterial activities of cefpiramide and other broad-spectrum antibiotics against 440 clinical isolates in China. J Infect Chemother. 2000;6(2):81–5.
Wang L, Zhou W, Cao Y, Yang C, Liu H, Chen T, Chen L. Characteristics of Stenotrophomonas maltophilia infection in children in Sichuan, China, from 2010 to 2017. Med (Baltim). 2020;99(8):e19250.
Wang Y, Li Y, Zhao J, Guan J, Ni W, Gao Z. Susceptibility of cefiderocol and other antibiotics against carbapenem-resistant, Gram-negative bacteria. Ann Transl Med. 2022;10(5):261.
Watson L, Esterly J, Jensen AO, Postelnick M, Aguirre A, McLaughlin M. Sulfamethoxazole/trimethoprim versus fluoroquinolones for the treatment of Stenotrophomonas maltophilia bloodstream infections. J Glob Antimicrob Resist. 2018;12:104–6.
Wei C, Ni W, Cai X, Cui J. A Monte Carlo pharmacokinetic/pharmacodynamic simulation to evaluate the efficacy of minocycline, tigecycline, moxifloxacin, and levofloxacin in the treatment of hospital-acquired pneumonia caused by Stenotrophomonas maltophilia. Infect Dis (Lond). 2015;47(12):846–51.
Wei C, Ni W, Cai X, Zhao J, Cui J. Evaluation of Trimethoprim/Sulfamethoxazole (SXT), Minocycline, Tigecycline, Moxifloxacin, and Ceftazidime alone and in combinations for SXT-Susceptible and SXT-Resistant Stenotrophomonas maltophilia by in Vitro Time-kill experiments. PLoS ONE. 2016;11(3):e0152132.
Wu AL, Yeh LK, Ma DH, Chen PY, Lin HC, Sun CC, Tan HY, Chen HC, Chen SY, Hsiao CH. Clinical characteristics of Stenotrophomonas maltophilia Keratitis. Cornea. 2016;35(6):795–800.
Wu H, Wang JT, Shiau YR, Wang HY, Lauderdale TL, Chang SC, Hospitals T. A multicenter surveillance of antimicrobial resistance on Stenotrophomonas maltophilia in Taiwan. J Microbiol Immunol Infect. 2012;45(2):120–6.
Xia Q, Zhao R, Ren H, Fang H, Wang Y. Epidemiological investigation of non-fermentative bacterial infection in cirrhotic patients. Expert Rev Gastroenterol Hepatol. 2019;13(8):815–20.
Yang Y, Yan Q, Chen X, Liu W, Jian Z. Antibiotic Resistance Surveillance of clinical isolates of Stenotrophomonas maltophilia strains in the Central South of China from 2016 to 2019. Jundishapur J Microbiol 2019, 12(11).
Yeshurun M, Gafter-Gvili A, Thaler M, Keller N, Nagler A, Shimoni A. Clinical characteristics of Stenotrophomonas maltophilia infection in hematopoietic stem cell transplantation recipients: a single center experience. Infection. 2010;38(3):211–5.
Liu PY-F, Lau Y-J, Hu B-S, Shyr J-M, Shi Z-Y, Tsai W-S, Lin Y-H, Tseng C-Y. Comparison of susceptibility to extended-spectrum β-lactam antibiotics and ciprofloxacin among gram-negative bacilli isolated from intensive care units. Diagn Microbiol Infect Dis. 1995;22(3):285–91.
Zhanel GG, DeCorby M, Nichol KA, Wierzbowski A, Baudry PJ, Karlowsky JA, Lagace-Wiens P, Walkty A, Mulvey MR, Hoban DJ, et al. Antimicrobial susceptibility of 3931 organisms isolated from intensive care units in Canada: Canadian National Intensive Care Unit Study, 2005/2006. Diagn Microbiol Infect Dis. 2008;62(1):67–80.
Zhang R, Sun Q, Hu YJ, Yu H, Li Y, Shen Q, Li GX, Cao JM, Yang W, Wang Q, et al. Detection of the Smqnr quinolone protection gene and its prevalence in clinical isolates of Stenotrophomonas maltophilia in China. J Med Microbiol. 2012;61(Pt 4):535–9.
Zhang Y, Zhao C, Wang Q, Wang X, Chen H, Li H, Zhang F, Wang H. Evaluation of the in vitro activity of new polymyxin B analogue SPR206 against clinical MDR, colistin-resistant and tigecycline-resistant Gram-negative bacilli. J Antimicrob Chemother. 2020;75(9):2609–15.
Zhao J, Liu Y, Liu Y, Wang D, Ni W, Wang R, Liu Y, Zhang B. Frequency and genetic determinants of Tigecycline Resistance in clinically isolated Stenotrophomonas maltophilia in Beijing, China. Front Microbiol. 2018;9:549.
Zhao J, Xing Y, Liu W, Ni W, Wei C, Wang R, Liu Y, Liu Y. Surveillance of Dihydropteroate synthase genes in Stenotrophomonas maltophilia by LAMP: implications for infection control and initial therapy. Front Microbiol. 2016;7:1723.
Zhu L, Wang L, Zhang Y, Chen R, Li X, Sun J, Zhou D, Zhu M, Zheng X, Li L, et al. Fatal hemorrhagic pneumonia in patients with hematologic diseases and Stenotrophomonas maltophilia bacteremia: a retrospective study. BMC Infect Dis. 2021;21(1):723.
Abbas SM, Dhahi MAR. Evaluation of some virulence factors and drug resistance of bacteria isolated from the urine of patients with TCC-bladder cancer. Baghdad Sci J. 2022;19(3):0469.
Abbassi MS, Touati A, Achour W, Cherif A, Jabnoun S, Khrouf N, Ben Hassen A. Stenotrophomonas maltophilia responsible for respiratory infections in neonatal intensive care unit: antibiotic susceptibility and molecular typing. Pathol Biol (Paris). 2009;57(5):363–7.
Afsharipour M, Mahmoudi S, Raji H, Pourakbari B, Mamishi S. Three-year evaluation of the nosocomial infections in pediatrics: bacterial and fungal profile and antimicrobial resistance pattern. Ann Clin Microbiol Antimicrob. 2022;21(1):6.
Agarwal S, Kakati B, Khanduri S, Gupta S. Emergence of Carbapenem resistant non-fermenting gram-negative Bacilli isolated in an ICU of a Tertiary Care Hospital. J Clin Diagn Res. 2017;11(1):DC04–7.
Alcaraz E, Centrón D, Camicia G, Quiroga MP, Di Conza J, Passerini de Rossi B. Stenotrophomonas maltophilia phenotypic and genotypic features through 4-year cystic fibrosis lung colonization. J Med Microbiol. 2021;70(1):001281.
Bostanghadiri N, Ardebili A, Ghalavand Z, Teymouri S, Mirzarazi M, Goudarzi M, Ghasemi E, Hashemi A. Antibiotic resistance, biofilm formation, and biofilm-associated genes among Stenotrophomonas maltophilia clinical isolates. BMC Res Notes. 2021;14:1–6.
Cho SY, Lee DG, Choi SM, Park C, Chun HS, Park YJ, Choi JK, Lee HJ, Park SH, Choi JH, et al. Stenotrophomonas maltophilia bloodstream infection in patients with hematologic malignancies: a retrospective study and in vitro activities of antimicrobial combinations. BMC Infect Dis. 2015;15:69.
Alcaraz E, Garcia C, Papalia M, Vay C, Friedman L, Passerini de Rossi B. Stenotrophomonas maltophilia isolated from patients exposed to invasive devices in a university hospital in Argentina: molecular typing, susceptibility and detection of potential virulence factors. J Med Microbiol. 2018;67(7):992–1002.
Arega B, Woldeamanuel Y, Adane K, Sherif AA, Asrat D. Microbial spectrum and drug-resistance profile of isolates causing bloodstream infections in febrile cancer patients at a referral hospital in Addis Ababa, Ethiopia. Infect drug Resist. 2018;11:1511.
Arpi M, Victor MA, Mortensen I, Gottschau A, Bruun B. In vitro susceptibility of 124 Xanthomonas maltophilia (Stenotrophomonas maltophilia) isolates: comparison of the agar dilution method with the E-test and two agar diffusion methods. APMIS. 1996;104(2):108–14.
Asaad AM, Al-Ayed MS, Qureshi MA. Emergence of unusual nonfermenting gram-negative nosocomial pathogens in a Saudi hospital. Jpn J Infect Dis. 2013;66(6):507–11.
Averbuch D, Avaky C, Harit M, Stepensky P, Fried I, Ben-Ami T, Temper V, Peled Y, Troen H, Masarwa R, et al. Non-fermentative gram-negative rods bacteremia in children with cancer: a 14-year single-center experience. Infection. 2017;45(3):327–34.
Azimi A, Rezaei F, Yaseri M, Jafari S, Rahbar M, Douraghi M. Emergence of fluoroquinolone resistance and possible mechanisms in clinical isolates of Stenotrophomonas maltophilia from Iran. Sci Rep. 2021;11(1):9582.
Bao H, Qiao Y, Liu D, Chen J, Wu X, Hu X, Ma X, Wu D. The clinical impact of Stenotrophomonas maltophilia bacteremia on the 30-day mortality rate in patients with hematologic disorders: a single-institution experience. Infection. 2020;48(2):205–12.
Barbier-Frebour N, Boutiba-Boubake I, Nouvello M, Lemelan J-F. Molecular investigation of Stenotrophomonas maltophilia isolatesexhibiting rapid emergence of ticarcillin-clavulanate resistance. J Hosp Infect. 2000;45(1):35–41.
Behnia M, Logan SC, Fallen L, Catalano P. Nosocomial and ventilator-associated pneumonia in a community hospital intensive care unit: a retrospective review and analysis. BMC Res Notes. 2014;7:232.
Blondeau JM, Laskowski R, Borsos S. In-vitro activity of cefepime and seven other antimicrobial agents against 1518 non-fermentative gram-negative bacilli collected from 48 Canadian health care facilities. Canadian Afermenter Study Group. J Antimicrob Chemother. 1999;44(4):545–8.
Baseri Z, Dehghan A, Yaghoubi S, Razavi S. Prevalence of resistance genes and antibiotic resistance profile among Stenotrophomonas maltophilia isolates from hospitalized patients in Iran. New Microbes New Infections. 2021;44:100943.
Batra P, Mathur P, Misra MC. Clinical characteristics and prognostic factors of patients with Stenotrophomonas maltophilia infections. J Lab Physicians. 2017;9(2):132–5.
Biswas S, Dubus JC, Reynaud-Gaubert M, Stremler N, Rolain JM. Evaluation of colistin susceptibility in multidrug-resistant clinical isolates from cystic fibrosis, France. Eur J Clin Microbiol Infect Dis. 2013;32(11):1461–4.
Bodey GP, Ho DH, Linda E. Survey of antibiotic susceptibility among gram-negative bacilli at a cancer hospital. Am J Med. 1988;85(1):49–51.
Bohra R, Wadhwa R, Bala K. Isolation and characterization of lactose and non-lactose fermenting bacteria from tertiary care hospital and their antimicrobial susceptibility test. Asian J Pharm Clin Res 2017.
Caverly LJ, Spilker T, Kalikin LM, Stillwell T, Young C, Huang DB, LiPuma JJ. In Vitro activities of beta-lactam-beta-lactamase inhibitor Antimicrobial agents against cystic fibrosis respiratory pathogens. Antimicrob Agents Chemother. 2019;64(1):e01595–01519.
Bostanghadiri N, Ghalavand Z, Fallah F, Yadegar A, Ardebili A, Tarashi S, Pournajaf A, Mardaneh J, Shams S, Hashemi A. Characterization of phenotypic and genotypic diversity of Stenotrophomonas maltophilia strains isolated from selected hospitals in Iran. Front Microbiol. 2019;10:1191.
Jaidane N, Chaouech C, Naija W, Boujaafar N, Bouallegue O. Stenotrophomonas maltophilia bacteraemia: analysis of 33 episodes occurred in the ICU at the University Hospital in Sousse, Tunisia. OALib J. 2014;1:e954.
Burastero GJ, Orlando G, Santoro A, Menozzi M, Franceschini E, Bedini A, Cervo A, Faltoni M, Bacca E, Biagioni E. Ceftazidime/Avibactam in Ventilator-Associated Pneumonia due to difficult-to-treat Non-fermenter Gram-negative Bacteria in COVID-19 patients: a Case Series and Review of the literature. Antibiotics. 2022;11(8):1007.
Burns JL, Emerson J, Stapp JR, Yim DL, Krzewinski J, Louden L, Ramsey BW, Clausen CR. Microbiology of sputum from patients at cystic fibrosis centers in the United States. Clin Infect Dis. 1998;27(1):158–63.
Cai B, Tillotson G, Benjumea D, Callahan P, Echols R. The burden of bloodstream infections due to Stenotrophomonas maltophilia in the United States: a large, retrospective database study. Open forum infectious diseases: 2020. Oxford University Press US; 2020. p. ofaa141.
Candel FJ, Santerre Henriksen A, Longshaw C, Yamano Y, Oliver A. In vitro activity of the novel siderophore cephalosporin, cefiderocol, in Gram-negative pathogens in Europe by site of infection. Clin Microbiol Infect. 2022;28(3):447. e441-447 e446.
Canton R, Valdezate S, Vindel A, Sanchez Del Saz B, Maiz L, Baquero F. Antimicrobial susceptibility profile of molecular typed cystic fibrosis Stenotrophomonas maltophilia isolates and differences with noncystic fibrosis isolates. Pediatr Pulmonol. 2003;35(2):99–107.
Chen C-Y, Tang TSAYW, Tien J-L, Chen H-F, Chang Y-C, Hsueh S-C. Epidemiology of bloodstream infections in patients with haematological malignancies with and without neutropenia. Epidemiol Infect. 2010;138(7):1044–51.
Chen KJ, Sun MH, Hou CH, Chen HC, Chen YP, Wang NK, Liu L, Wu WC, Chou HD, Kang EY, et al. Susceptibility of bacterial endophthalmitis isolates to Vancomycin, ceftazidime, and amikacin. Sci Rep. 2021;11(1):15878.
Chang LL, Chen HF, Chang CY, Lee TM, Wu WJ. Contribution of integrons, and SmeABC and SmeDEF efflux pumps to multidrug resistance in clinical isolates of Stenotrophomonas maltophilia. J Antimicrob Chemother. 2004;53(3):518–21.
Chen S, Lin K, Li Q, Luo X, Xiao M, Chen M, Zhu H, Chen Y, Wu X, Zeng Y, et al. A practical update on the epidemiology and risk factors for the emergence and mortality of bloodstream infections from real-world data of 3014 hematological malignancy patients receiving chemotherapy. J Cancer. 2021;12(18):5494–505.
Cha MK, Kang CI, Kim SH, Cho SY, Ha YE, Chung DR, Peck KR, Song JH. Emergence of fluoroquinolone-resistant Stenotrophomonas maltophilia in blood isolates causing bacteremia: molecular epidemiology and microbiologic characteristics. Diagn Microbiol Infect Dis. 2016;85(2):210–2.
Chen Y, Suo J, Du M, Chen L, Liu Y, Wang L, Liang Z. Clinical features, outcomes, and risk factors of bloodstream infections due to Stenotrophomonas maltophilia in a tertiary-care hospital of China: a retrospective analysis. BioMed Research International 2019, 2019.
Cherif H, Kronvall G, Bjorkholm M, Kalin M. Bacteraemia in hospitalised patients with malignant blood disorders: a retrospective study of causative agents and their resistance profiles during a 14-year period without antibacterial prophylaxis. Hematol J. 2003;4(6):420–6.
Chhablani J, Sudhalkar A, Jindal A, Das T, Motukupally SR, Sharma S, Pathengay A, Flynn HW. Jr.: Stenotrophomonas maltophilia endogenous endophthalmitis: clinical presentation, antibiotic susceptibility, and outcomes. Clin Ophthalmol. 2014;8:1523–6.
Cho HH, Sung JY, Kwon KC, Koo SH. Expression of sme efflux pumps and multilocus sequence typing in clinical isolates of Stenotrophomonas maltophilia. Ann Lab Med. 2012;32(1):38–43.
Chong SY, Lee K, Chung HS, Hong SG, Suh Y, Chong Y. Levofloxacin Efflux and smeD in Clinical isolates of Stenotrophomonas maltophilia. Microb Drug Resist. 2017;23(2):163–8.
Chow JW, Satishchandran V, Snyder TA, Harvey CM, Friedland IR, Dinubile MJ. In vitro susceptibilities of aerobic and facultative gram-negative bacilli isolated from patients with intra-abdominal infections worldwide: the 2002 study for Monitoring Antimicrobial Resistance trends (SMART). Surg Infect (Larchmt). 2005;6(4):439–48.
Chung HS, Hong SG, Lee Y, Kim M, Yong D, Jeong SH, Lee K, Chong Y. Antimicrobial susceptibility of Stenotrophomonas maltophilia isolates from a Korean tertiary care hospital. Yonsei Med J. 2012;53(2):439–41.
Chung HS, Kim K, Hong SS, Hong SG, Lee K, Chong Y. The sul1 gene in Stenotrophomonas maltophilia with high-level resistance to trimethoprim/sulfamethoxazole. Ann Lab Med. 2015;35(2):246–9.
Çıkman A, Parlak M, Bayram Y, Güdücüoğlu H, Berktaş M. Antibiotics resistance of Stenotrophomonas maltophilia strains isolated from various clinical specimens. Afr Health Sci. 2016;16(1):149–52.
Cohn ML, Waites KB. Antimicrobial activities of gatifloxacin against nosocomial isolates of Stenotrophomonas maltophilia measured by MIC and time-kill studies. Antimicrob Agents Chemother. 2001;45(7):2126–8.
Corlouer C, Lamy B, Desroches M, Ramos-Vivas J, Mehiri-Zghal E, Lemenand O, Delarbre JM, Decousser JW. College De Bacteriologie-Virologie-Hygiene Des Hopitaux De F: Stenotrophomonas maltophilia healthcare-associated infections: identification of two main pathogenic genetic backgrounds. J Hosp Infect. 2017;96(2):183–8.
Crispino M, Boccia MC, Bagattini M, Villari P, Triassi M, Zarrilli R. Molecular epidemiology of Stenotrophomonas maltophilia in a university hospital. J Hosp Infect. 2002;52(2):88–92.
Cruz-Cordova A, Mancilla-Rojano J, Luna-Pineda VM, Escalona-Venegas G, Cazares-Dominguez V, Ormsby C, Franco-Hernandez I, Zavala-Vega S, Hernandez MA, Medina-Pelcastre M, et al. Molecular Epidemiology, Antibiotic Resistance, and virulence traits of Stenotrophomonas maltophilia strains Associated with an outbreak in a Mexican Tertiary Care Hospital. Front Cell Infect Microbiol. 2020;10:50.
ElBaradei A, Yakout MA. Stenotrophomonas maltophilia: genotypic characterization of virulence genes and the effect of ascorbic acid on Biofilm formation. Curr Microbiol. 2022;79(6):180.
Gulmez D, Hascelik G. Stenotrophomonas maltophilia: antimicrobial resistance and molecular typing of an emerging pathogen in a Turkish university hospital. Clin Microbiol Infect. 2005;11(11):880–6.
Eltahawy A, Khalaf R. Antibiotic resistance among gram-negative non-fermentative bacteria at a teaching hospital in Saudi Arabia. J Chemother. 2001;13(3):260–4.
Hajjej Z, Nasri M, Sellami W, Gharsallah H, Labben I, Ferjani M. Incidence, risk factors and microbiology of central vascular catheter-related bloodstream infection in an intensive care unit. J Infect Chemother. 2014;20(3):163–8.
de Rossi BP, García C, Calenda M, Vay C, Franco M. Activity of levofloxacin and ciprofloxacin on biofilms and planktonic cells of Stenotrophomonas maltophilia isolates from patients with device-associated infections. Int J Antimicrob Agents. 2009;34(3):260–4.
Delgado-Valverde M, Conejo MDC, Serrano L, Fernandez-Cuenca F, Pascual A. Activity of cefiderocol against high-risk clones of multidrug-resistant Enterobacterales, Acinetobacter baumannii, Pseudomonas aeruginosa and Stenotrophomonas maltophilia. J Antimicrob Chemother. 2020;75(7):1840–9.
Denisuik AJ, Garbutt LA, Golden AR, Adam HJ, Baxter M, Nichol KA, Lagace-Wiens P, Walkty AJ, Karlowsky JA, Hoban DJ, et al. Antimicrobial-resistant pathogens in Canadian ICUs: results of the CANWARD 2007 to 2016 study. J Antimicrob Chemother. 2019;74(3):645–53.
Di Bonaventura G, D’Antonio D, Catamo G, D’Ercole S, Piccolomini R. Comparative in vitro activity of levofloxacin and ciprofloxacin against bacterial isolates from neutropenic patients. Chemotherapy. 2002;48(3):134–7.
Di Bonaventura G, Spedicato I, D’Antonio D, Robuffo I, Piccolomini R. Biofilm formation by Stenotrophomonas maltophilia: modulation by quinolones, trimethoprim-sulfamethoxazole, and ceftazidime. Antimicrob Agents Chemother. 2004;48(1):151–60.
Diez-Aguilar M, Ekkelenkamp M, Morosini MI, Merino I, de Dios Caballero J, Jones M, van Westreenen M, Tunney MM, Canton R, Fluit AC. Antimicrobial susceptibility of non-fermenting gram-negative pathogens isolated from cystic fibrosis patients. Int J Antimicrob Agents. 2019;53(1):84–8.
Gupta P, Kale P, Khillan V. Resurgence of global opportunistic multidrug-resistant Stenotrophomonas maltophilia. Indian J Crit Care Med. 2018;22(7):503–8.
Duan Z, Qin J, Li C, Ying C. Clinical and molecular epidemiology of Stenotrophomonas maltophilia in Pediatric patients from a Chinese Teaching Hospital. Front Cell Infect Microbiol. 2020;10:411.
Duan Z, Qin J, Liu Y, Li C, Ying C. Molecular epidemiology and risk factors of Stenotrophomonas maltophilia infections in a Chinese teaching hospital. BMC Microbiol. 2020;20(1):294.
Duan T. Analysis of Microbiological and Clinical Characteristics of Bacterial Infection in Patients with Pulmonary Infection. Comput Intell Neurosci.2022:5607358.
Ejaz H. Determination of bacterial profile and spectrum of antimicrobial drug resistance in pediatric wound infections. J Pure Appl Microbiol. 2019;13(4):2097–104.
Wang C-H, Lin J-C, Lin H-A, Chang F-Y, Wang N-C, Chiu S-K, Lin T-Y, Yang Y-S, Kan L-P, Yang C-H. Comparisons between patients with trimethoprim–sulfamethoxazole-susceptible and trimethoprim–sulfamethoxazole-resistant Stenotrophomonas maltophilia monomicrobial bacteremia: a 10-year retrospective study. J Microbiol Immunol Infect. 2016;49(3):378–86.
Guzek A, Korzeniewski K, Tomaszewski D, Rybicki Z, Zwolinska E. Bacteriological Assessment of Pneumonia caused by Gram-negative Bacteria in patients hospitalized in Intensive Care Unit. Adv Exp Med Biol. 2017;955:39–46.
Guriz H, Ciftci E, Ayberkin E, Aysev D, Ince E, Arsan S, Yavuz G, Dogru U. Stenotrophomonas maltophilia bacteraemia in Turkish children. Ann Trop Paediatr. 2008;28(2):129–36.
Gomez-Garces JL, Aracil B, Gil Y, Burillo A. Susceptibility of 228 non-fermenting gram-negative rods to tigecycline and six other antimicrobial drugs. J Chemother. 2009;21(3):267–71.
Goncalves-Vidigal P, Grosse-Onnebrink J, Mellies U, Buer J, Rath PM, Steinmann J. Stenotrophomonas maltophilia in cystic fibrosis: improved detection by the use of selective agar and evaluation of antimicrobial resistance. J Cyst Fibros. 2011;10(6):422–7.
Gramegna A, Millar BC, Blasi F, Elborn JS, Downey DG, Moore JE. In vitro antimicrobial activity of ceftolozane/tazobactam against Pseudomonas aeruginosa and other non-fermenting gram-negative bacteria in adults with cystic fibrosis. J Glob Antimicrob Resist. 2018;14:224–7.
Grohs P, Taieb G, Morand P, Kaibi I, Podglajen I, Lavollay M, Mainardi JL, Compain F. In Vitro Activity of Ceftolozane-Tazobactam against Multidrug-Resistant Nonfermenting Gram-negative Bacilli isolated from patients with cystic fibrosis. Antimicrob Agents Chemother. 2017;61(4):e02688–02616.
de Microbiología S. Evolution of antimicrobial susceptibility patterns of aerobic and facultative gram-negative bacilli causing intra-abdominal infections: results from the SMART studies 2003–2007. Rev Esp Quimioter. 2008;21(3):166–73.
Guerci P, Bellut H, Mokhtari M, Gaudefroy J, Mongardon N, Charpentier C, Louis G, Tashk P, Dubost C, Ledochowski S, et al. Outcomes of Stenotrophomonas maltophilia hospital-acquired pneumonia in intensive care unit: a nationwide retrospective study. Crit Care. 2019;23(1):371.
Djordjevic ZM, Folic MM, Jankovic SM. Distribution and antibiotic susceptibility of pathogens isolated from adults with hospital-acquired and ventilator-associated pneumonia in intensive care unit. J Infect Public Health. 2017;10(6):740–4.
Ebrahim-Saraie HS, Heidari H, Soltani B, Mardaneh J, Motamedifar M. Prevalence of antibiotic resistance and integrons, Sul and Smqnr genes in clinical isolates of Stenotrophomonas maltophilia from a tertiary care hospital in Southwest Iran. Iran J Basic Med Sci. 2019;22(8):872–7.
Higgins C, Murtough S, Williamson E, Hiom S, Payne D, Russell A, Walsh T. Resistance to antibiotics and biocides among non-fermenting gram-negative bacteria. Clin Microbiol Infect. 2001;7(6):308–15.
Karlowsky JA, Adam HJ, Decorby MR, Lagace-Wiens PR, Hoban DJ, Zhanel GG. In vitro activity of ceftaroline against gram-positive and gram-negative pathogens isolated from patients in Canadian hospitals in 2009. Antimicrob Agents Chemother. 2011;55(6):2837–46.
Karlowsky JA, Kelly LJ, Thornsberry C, Jones ME, Evangelista AT, Critchley IA, Sahm DF. Susceptibility to fluoroquinolones among commonly isolated Gram-negative bacilli in 2000: TRUST and TSN data for the United States. Int J Antimicrob Agents. 2002;19(1):21–31.
Karunanidhi A, Thomas R, van Belkum A, Neela V. In vitro antibacterial and antibiofilm activities of chlorogenic acid against clinical isolates of Stenotrophomonas maltophilia including the trimethoprim/sulfamethoxazole resistant strain. Biomed Res Int. 2013;2013:392058.
Zhong L, Men T-Y, Li H, Peng Z-H, Gu Y, Ding X, Xing T-H, Fan J-W. Multidrug-resistant gram-negative bacterial infections after liver transplantation–spectrum and risk factors. J Infect. 2012;64(3):299–310.
Kataoka D, Fujiwara H, Kawakami T, Tanaka Y, Tanimoto A, Ikawa S, Tanaka Y. The indirect pathogenicity of Stenotrophomonas maltophilia. Int J Antimicrob Agents. 2003;22(6):601–6.
Kaur P, Gautam V, Tewari R. Distribution of class 1 integrons, sul1 and sul2 genes among clinical isolates of Stenotrophomonas maltophilia from a tertiary care hospital in North India. Microb Drug Resist. 2015;21(4):380–5.
Kawauchi R, Tada T, Sherchan JB, Shrestha S, Tohya M, Hishinuma T, Kirikae T, Sherchand JB. Stenotrophomonas maltophilia from Nepal Producing two Novel Antibiotic inactivating enzymes, a class A beta-lactamase KBL-1 and an Aminoglycoside 6’-N-Acetyltransferase AAC(6’)-Iap. Microbiol Spectr. 2022;10(4):e0114322.
Khan IU, Mirza IA, Ikram A, Ali S, Hussain A, Ghafoor T. In vitro activity of fosfomycin tromethamine against extended spectrum beta-lactamase producing urinary tract bacteria. J Coll Physicians Surg Pak. 2014;24(12):914–7.
Kim SH, Cho SY, Kang CI, Seok H, Huh K, Ha YE, Chung DR, Lee NY, Peck KR, Song JH. Clinical predictors of Stenotrophomonas maltophilia bacteremia in adult patients with hematologic malignancy. Ann Hematol. 2018;97(2):343–50.
Kim SY, Shin SY, Rhee J-Y, Ko KS. Imipenem-resistant Gram-negative bacterial isolates carried by persons upon medical examination in Korea. J Microbiol. 2017;55:612–8.
Knight T, Gupte A, Dulay K, Mitchell R, Salimnia H, Wang ZJ. Evaluation of an empiric antibiotic regimen in pediatric oncology patients presenting with fever does not reveal the emergence of antibiotic resistance over a 12-year period. Pediatr Hematol Oncol J. 2020;5(3):80–8.
Rhee JY, Choi JY, Choi MJ, Song JH, Peck KR, Ko KS. Distinct groups and antimicrobial resistance of clinical Stenotrophomonas maltophilia complex isolates from Korea. J Med Microbiol. 2013;62(Pt 5):748–53.
Kosai K, Yamagishi Y, Hashinaga K, Nakajima K, Mikamo H, Hiramatsu K, Takesue Y, Yanagihara K. Multicenter surveillance of the epidemiology of gram-negative bacteremia in Japan. J Infect Chemother. 2020;26(3):193–8.
Koseoglu O, Sener B, Gulmez D, Altun B, Gur D. Stenotrophomonas maltophilia as a nosocomial pathogen. Microbiologica-Quarterly J Microbiol Sci. 2004;27(3):273–80.
Kumwenda GP, Kasambara W, Chizani K, Phiri A, Banda A, Choonara F, Lichapa B. A multidrug-resistant Stenotrophomonas maltophilia clinical isolate from Kamuzu Central Hospital, Malawi. Malawi Med J. 2021;33(2):82–4.
Lambiase A, Raia V, Del Pezzo M, Sepe A, Carnovale V, Rossano F. Microbiology of airway disease in a cohort of patients with cystic fibrosis. BMC Infect Dis. 2006;6:4.
Lanzafame A, Bonfiglio G, Santini L, Mattina R. In vitro activity of levofloxacin against recent Gram-negative nosocomial pathogens. Chemotherapy. 2005;51(1):44–50.
Lecso-Bornet M, Bergogne-Berezin E. Susceptibility of 100 strains of Stenotrophomonas maltophilia to three beta-lactams and five beta-lactam-beta-lactamase inhibitor combinations. J Antimicrob Chemother. 1997;40(5):717–20.
Lee JY, Kang CI, Ko JH, Lee WJ, Seok HR, Park GE, Cho SY, Ha YE, Chung DR, Lee NY, et al. Clinical features and risk factors for development of breakthrough gram-negative bacteremia during Carbapenem Therapy. Antimicrob Agents Chemother. 2016;60(11):6673–8.
Lee M-R, Wang H-C, Yang C-Y, Lin C-K, Kuo H-Y, Ko J-C, Sheng W-H, Lee L-N, Yu C-J, Hsueh P-R. Clinical characteristics and outcomes of patients with pleural infections due to Stenotrophomonas maltophilia at a medical center in Taiwan, 2004–2012. Eur J Clin Microbiol Infect Dis. 2014;33:1143–8.
Leroy O, d’Escrivan T, Devos P, Dubreuil L, Kipnis E, Georges H. Hospital-acquired pneumonia in critically ill patients: factors associated with episodes due to imipenem-resistant organisms. Infection. 2005;33:129–35.
Liaw SJ, Lee YL, Hsueh PR. Multidrug resistance in clinical isolates of Stenotrophomonas maltophilia: roles of integrons, efflux pumps, phosphoglucomutase (SpgM), and melanin and biofilm formation. Int J Antimicrob Agents. 2010;35(2):126–30.
Liaw SJ, Teng LJ, Hsueh PR, Ho SW, Luh KT. In vitro activities of antimicrobial combinations against clinical isolates of Stenotrophomonas maltophilia. J Formos Med Assoc. 2002;101(7):495–501.
Lin Q, Zou H, Chen X, Wu M, Ma D, Yu H, Niu S, Huang S. Avibactam potentiated the activity of both ceftazidime and aztreonam against S. maltophilia clinical isolates in vitro. BMC Microbiol. 2021;21:1–6.
Ling TK, Xiong J, Yu Y, Lee CC, Ye H, Hawkey PM. Multicenter antimicrobial susceptibility survey of gram-negative bacteria isolated from patients with community-acquired infections in the people’s Republic of China. Antimicrob Agents Chemother. 2006;50(1):374–8.
Liu B, Tong S. An investigation of Stenotrophomonas maltophilia-positive culture caused by fiberoptic bronchoscope contamination. BMC Infect Dis. 2019;19(1):1072.
Liu JY, Wang FD, Ho MW, Lee CH, Liu JW, Wang JT, Sheng WH, Hseuh PR, Chang SC. In vitro activity of aminoglycosides against clinical isolates of Acinetobacter baumannii complex and other nonfermentative gram-negative bacilli causing healthcare-associated bloodstream infections in Taiwan. J Microbiol Immunol Infect. 2016;49(6):918–23.
Liu YM, Chen YS, Toh HS, Huang CC, Lee YL, Ho CM, Lu PL, Ko WC, Chen YH, Wang JH, et al. In vitro susceptibilities of non-enterobacteriaceae isolates from patients with intra-abdominal infections in the Asia-Pacific region from 2003 to 2010: results from the study for Monitoring Antimicrobial Resistance trends (SMART). Int J Antimicrob Agents. 2012;40(Suppl):S11–17.
Livermore DM, Mushtaq S, Warner M, Woodford N. Comparative in vitro activity of sulfametrole/trimethoprim and sulfamethoxazole/trimethoprim and other agents against multiresistant Gram-negative bacteria. J Antimicrob Chemother. 2014;69(4):1050–6.
Oliveira MEF, Araújo DG, Oliveira SR. Resistance of non-fermenting gram-negative bacilli isolated from blood cultures from an emergency hospital. Jornal Brasileiro De Patologia E Med Laboratorial. 2017;53:87–91.
Oncul O, Oksuz S, Acar A, Ulkur E, Turhan V, Uygur F, Ulcay A, Erdem H, Ozyurt M, Gorenek L. Nosocomial infection characteristics in a burn intensive care unit: analysis of an eleven-year active surveillance. Burns. 2014;40(5):835–41.
Osawa K, Shigemura K, Kitagawa K, Tokimatsu I, Fujisawa M. Risk factors for death from Stenotrophomonas maltophilia bacteremia. J Infect Chemother. 2018;24(8):632–6.
Palioura S, Gibbons A, Miller D, O’Brien TP, Alfonso EC, Spierer O. Clinical features, Antibiotic Susceptibility Profile, and outcomes of infectious keratitis caused by Stenotrophomonas maltophilia. Cornea. 2018;37(3):326–30.
Pankey GA, Ashcraft DS. In vitro synergistic/additive activity of levofloxacin with meropenem against Stenotrophomonas maltophilia. Diagn Microbiol Infect Dis. 2010;67(3):297–300.
Paopradit P, Srinitiwarawong K, Ingviya N, Singkhamanan K, Vuddhakul V. Distribution and characterization of Stenotrophomonas maltophilia isolates from environmental and clinical samples in Thailand. J Hosp Infect. 2017;97(2):185–91.
Papadimitriou-Olivgeris M, Kolonitsiou F, Militsopoulou M, Spiliopoulou I, Giormezis N. Clonal dissemination and resistance genes among Stenotrophomonas maltophilia in a Greek University Hospital during a four-year period. AIMS Microbiol. 2022;8(3):292.
Paprocka P, Mankowska A, Sklodowski K, Krol G, Wollny T, Lesiak A, Gluszek K, Savage PB, Durnas B, Bucki R. Bactericidal activity of Ceragenin in combination with Ceftazidime, Levofloxacin, Co-trimoxazole, and Colistin against the opportunistic Pathogen Stenotrophomonas maltophilia. Pathogens. 2022;11(6):621.
Park BC, Lim HR, Park SJ, Koh JW. Clinical features and management of Stenotrophomonas Maltophilia Keratitis. Ophthalmol Ther. 2021;10(3):525–33.
Patterson SB, Mende K, Li P, Lu D, Carson ML, Murray CK, Tribble DR, Blyth DM, Group IT. Stenotrophomonas maltophilia infections: clinical characteristics in a military trauma population. Diagn Microbiol Infect Dis. 2020;96(2):114953.
Pien CJ, Kuo HY, Chang SW, Chen PR, Yeh HW, Liu CC, Liou ML. Risk factors for levofloxacin resistance in Stenotrophomonas maltophilia from respiratory tract in a regional hospital. J Microbiol Immunol Infect. 2015;48(3):291–5.
Pompilio A, Savini V, Fiscarelli E, Gherardi G, Di Bonaventura G. Clonal diversity, biofilm formation, and antimicrobial resistance among Stenotrophomonas maltophilia strains from cystic fibrosis and non-cystic fibrosis patients. Antibiotics. 2020;9(1):15.
Poulos CD, Matsumura SO, Willey BM, Low DE, McGeer A. In vitro activities of antimicrobial combinations against Stenotrophomonas (Xanthomonas) maltophilia. Antimicrob Agents Chemother. 1995;39(10):2220–3.
Charles MP, Easow JM, Joseph NM, Ravishankar M, Kumar S, Sivaraman U. Aetiological agents of ventilator-associated pneumonia and its resistance pattern - a threat for treatment. Australas Med J. 2013;6(9):430–4.
Qin X, Razia Y, Johnson JR, Stapp JR, Boster DR, Tsosie T, Smith DL, Braden CR, Gay K, Angulo FJ, et al. Ciprofloxacin-resistant gram-negative bacilli in the fecal microflora of children. Antimicrob Agents Chemother. 2006;50(10):3325–9.
Qiu Y, Yang J, Chen Y, Yang J, Zhu Q, Zhu C, Li S, Liu J, Wan C, Zhu Y, et al. Microbiological profiles and antimicrobial resistance patterns of pediatric bloodstream pathogens in China, 2016–2018. Eur J Clin Microbiol Infect Dis. 2021;40(4):739–49.
Rajkumari N, Mathur P, Gupta AK, Sharma K, Misra MC. Epidemiology and outcomes of Stenotrophomonas maltophilia and Burkholderia cepacia infections among trauma patients of India: a five year experience. J Infect Prev. 2015;16(3):103–10.
Ramazanzadeh R, Chitsaz M, Bahmani N. Prevalence and antimicrobial susceptibility of extended-spectrum beta-lactamase-producing bacteria in intensive care units of Sanandaj general hospitals (Kurdistan, Iran). Chemotherapy. 2009;55(4):287–92.
Ratjen A, Yau Y, Wettlaufer J, Matukas L, Zlosnik JE, Speert DP, LiPuma JJ, Tullis E, Waters V. In vitro efficacy of high-dose tobramycin against Burkholderia cepacia complex and Stenotrophomonas maltophilia isolates from cystic fibrosis patients. Antimicrob Agents Chemother. 2015;59(1):711–3.
Renteria MI, Biedenbach DJ, Bouchillon SK, Hoban DJ, Raghubir N, Sajben P, Mokaddas E. In vitro activity of tigecycline against isolates collected from complicated skin and skin structure infections and intra-abdominal infections in Africa and Middle East countries: TEST 2007–2012. Diagn Microbiol Infect Dis. 2014;79(1):54–9.
Rhee JY, Song JH, Ko KS. Current Situation of Antimicrobial Resistance and genetic differences in Stenotrophomonas maltophilia Complex isolates by Multilocus Variable Number of Tandem Repeat Analysis. Infect Chemother. 2016;48(4):285–93.
Ribera A, Jurado A, Ruiz J, Marco F, Del Valle O, Mensa J, Chaves J, Hernandez G, Jimenez de Anta MT, Vila J. In vitro activity of clinafloxacin in comparison with other quinolones against Stenotrophomonas maltophilia clinical isolates in the presence and absence of reserpine. Diagn Microbiol Infect Dis. 2002;42(2):123–8.
Rizek C, Ferraz JR, van der Heijden IM, Giudice M, Mostachio AK, Paez J, Carrilho C, Levin AS, Costa SF. In vitro activity of potential old and new drugs against multidrug-resistant gram-negatives. J Infect Chemother. 2015;21(2):114–7.
Rodríguez CH, Nastro M, Calvo JL, Fariña ME, Dabos L, Famiglietti A. In vitro activity of colistin against Stenotrophomonas maltophilia. J Glob Antimicrob Resist. 2014;2(4):316–7.
Rolston KV, Frisbee-Hume S, LeBlanc B, Streeter H, Ho DH. In vitro antimicrobial activity of moxifloxacin compared to other quinolones against recent clinical bacterial isolates from hospitalized and community-based cancer patients. Diagn Microbiol Infect Dis. 2003;47(2):441–9.
Rolston KV, Kontoyiannis DP, Yadegarynia D, Raad II. Nonfermentative gram-negative bacilli in cancer patients: increasing frequency of infection and antimicrobial susceptibility of clinical isolates to fluoroquinolones. Diagn Microbiol Infect Dis. 2005;51(3):215–8.
Rolston KVI, Gerges B, Shelburne S, Aitken SL, Raad I, Prince RA. Activity of Cefiderocol and Comparators against isolates from Cancer patients. Antimicrob Agents Chemother. 2020;64(5):e01955–01919.
Romo-Ibanez A, Calatrava-Hernandez E, Gutierrez-Soto B, Perez-Ruiz M, Navarro-Mari JM, Gutierrez-Fernandez J. High clinical impact of rapid susceptibility testing on CHROMID ESBL((R)) medium directly from swabs. Ann Transl Med. 2020;8(9):604.
ÇAYCI YT, BIYIK İ. BİRİNCİ A: First Investigation of OqxAB and plasmid-mediated Quinolone Resistance determinant qnr genes in Stenotrophomonas maltophilia isolates. 2021.
Guclu AU, Kocak AA, Ok MA, Tutluoglu B, Basustaoglu A. Antibacterial resistance in lower respiratory tract bacterial pathogens: a multicenter analysis from Turkey. 2021.
Wan Q, Luo A, Ye Q, Liu S, Zhou J. Predictors of shock and mortality in solid organ transplant recipients with bacteremia caused by non-lactose-fermenting gram-negative bacilli. Infect Dis (Lond). 2016;48(1):32–9.
Wang CH, Yu CM, Hsu ST, Wu RX. Levofloxacin-resistant Stenotrophomonas maltophilia: risk factors and antibiotic susceptibility patterns in hospitalized patients. J Hosp Infect. 2020;104(1):46–52.
Ewig S, Soler N, Gonzalez J, Celis R, El-Ebiary M, Torres A. Evaluation of antimicrobial treatment in mechanically ventilated patients with severe chronic obstructive pulmonary disease exacerbations. Crit Care Med. 2000;28(3):692–7.
Fadda G, Spanu T, Ardito F, Taddei C, Santangelo R, Siddu A, Ciccaglione D, Observatory TIE. Antimicrobial resistance among non-fermentative gram-negative bacilli isolated from the respiratory tracts of Italian inpatients: a 3-year surveillance study by the Italian epidemiological survey. Int J Antimicrob Agents. 2004;23(3):254–61.
Farrell DJ, Sader HS, Flamm RK, Jones RN. Ceftolozane/tazobactam activity tested against Gram-negative bacterial isolates from hospitalised patients with pneumonia in US and European medical centres (2012). Int J Antimicrob Agents. 2014;43(6):533–9.
Fedler KA, Biedenbach DJ, Jones RN. Assessment of pathogen frequency and resistance patterns among pediatric patient isolates: report from the 2004 SENTRY Antimicrobial Surveillance Program on 3 continents. Diagn Microbiol Infect Dis. 2006;56(4):427–36.
Flamm RK, Castanheira M, Streit JM, Jones RN. Minocycline activity tested against Acinetobacter baumannii complex, Stenotrophomonas maltophilia, and Burkholderia cepacia species complex isolates from a global surveillance program (2013). Diagn Microbiol Infect Dis. 2016;85(3):352–5.
Flamm RK, Shortridge D, Castanheira M, Sader HS, Pfaller MA. In vitro activity of minocycline against US isolates of Acinetobacter baumannii-Acinetobacter calcoaceticus species complex, Stenotrophomonas maltophilia, and Burkholderia cepacia complex: results from the SENTRY Antimicrobial Surveillance Program, 2014 to 2018. Antimicrob Agents Chemother. 2019;63(11):e01154–01119.
Flores-Trevino S, Gutierrez-Ferman JL, Morfin-Otero R, Rodriguez-Noriega E, Estrada-Rivadeneyra D, Rivas-Morales C, Llaca-Diaz JM, Camacho-Ortiz A, Mendoza-Olazaran S, Garza-Gonzalez E. Stenotrophomonas maltophilia in Mexico: antimicrobial resistance, biofilm formation and clonal diversity. J Med Microbiol. 2014;63(Pt 11):1524–30.
Forrester JB, Steed LL, Santevecchi BA, Flume P, Palmer-Long GE, Bosso JA. In vitro activity of ceftolozane/tazobactam vs nonfermenting, Gram-negative cystic fibrosis isolates. Open Forum Infectious diseases: 2018. Oxford University Press US; 2018. p. ofy158.
Fritsche TR, Sader HS, Stilwell MG, Dowzicky MJ, Jones RN. Antimicrobial activity of tigecycline tested against organisms causing community-acquired respiratory tract infection and nosocomial pneumonia. Diagn Microbiol Infect Dis. 2005;52(3):187–93.
Fu W, Demei Z, Shi W, Fupin H, Yingyuan Z. The susceptibility of non-fermentative gram-negative bacilli to cefperazone and sulbactam compared with other antibacterial agents. Int J Antimicrob Agents. 2003;22(4):444–8.
Fuchs PC, Barry AL, Brown SD. Survey of antimicrobial activity of four commonly used third generation cephalosporins tested against recent bacterial isolates from ten American medical centers, and assessment of disk diffusion test performance. AST Surveillance Group. Diagn Microbiol Infect Dis. 1996;24(4):213–9.
Fuchs PC, Barry AL, Brown SD. In vitro activity of trovafloxacin against ciprofloxacin-susceptible and -resistant clinical bacterial isolates and assessment of the trovafloxacin disk test. Diagn Microbiol Infect Dis. 1999;33(1):33–8.
Fujita J, Yamadori I, Xu G, Hojo S, Negayama K, Miyawaki H, Yamaji Y, Takahara J. Clinical features of Stenotrophomonas maltophilia pneumonia in immunocompromised patients. Respir Med. 1996;90(1):35–8.
Gajdacs M, Urban E. A 10-year single-center experience on Stenotrophomonas maltophilia resistotyping in Szeged, Hungary. Eur J Microbiol Immunol (Bp). 2020;10(2):91–7.
Gales AC, Jones R, Forward K, Linares J, Sader HS, Verhoef J. Emerging importance of multidrug-resistant Acinetobacter species and Stenotrophomonas maltophilia as pathogens in seriously ill patients: geographic patterns, epidemiological features, and trends in the SENTRY Antimicrobial Surveillance Program (1997–1999). Clin Infect Dis. 2001;32(Supplement2):S104–13.
Gales AC, Jones RN, Sader HS. Global assessment of the antimicrobial activity of polymyxin B against 54 731 clinical isolates of Gram-negative bacilli: report from the SENTRY antimicrobial surveillance programme (2001–2004). Clin Microbiol Infect. 2006;12(4):315–21.
Gales AC, Jones R, Sader HS. Antimicrobial susceptibility profile of contemporary clinical strains of Stenotrophomonas maltophilia isolates: can moxifloxacin activity be predicted by levofloxacin MIC results? J Chemother. 2008;20(1):38–42.
Gallo SW, Figueiredo TP, Bessa MC, Pagnussatti VE, Ferreira CA, Oliveira SD. Isolation and characterization of Stenotrophomonas maltophilia isolates from a Brazilian hospital. Microb Drug Resist. 2016;22(8):688–95.
Garcia DO, Timenetsky J, Martinez MB, Francisco W, Sinto SI, Yanaguita RM. Proteases (caseinase and elastase), hemolysins, adhesion and susceptibility to antimicrobials of Stenotrophomonas maltophilia isolates obtained from clinical specimens. Brazilian J Microbiol. 2002;33:157–62.
Garcia-Rodriguez JA, Fresnadillo MJ, Garcia MI, Garcia-Sanchez E, Garcia-Sanchez JE, Trujillano I. Multicenter Spanish study of ciprofloxacin susceptibility in gram-negative bacteria. The Spanish Study Group on Quinolone Resistance. Eur J Clin Microbiol Infect Dis. 1995;14(5):456–9.
Garcia-Rodriguez J, Sanchez JG, Garcia MG, Sanchez EG, Bellido JM. Antibiotic susceptibility profile of Xanthomonas maltophilia in vitro activity of β-lactam/β-lactamase inhibitor combinations. Diagn Microbiol Infect Dis. 1991;14(3):239–43.
Garcia-Rodriguez JA, Garcia Sanchez JE, Munoz Bellido JL, Garcia Sanchez E, Garcia Garcia MI. In-vitro activity of meropenem, a new carbapenem, against imipenem-resistant Pseudomonas aeruginosa and Xanthomonas maltophilia. J Chemother. 1991;3(3):143–6.
Gesu GP, Marchetti F, Piccoli L, Cavallero A. Levofloxacin and ciprofloxacin in vitro activities against 4,003 clinical bacterial isolates collected in 24 Italian laboratories. Antimicrob Agents Chemother. 2003;47(2):816–9.
Biagi M, Tan X, Wu T, Jurkovic M, Vialichka A, Meyer K, Mendes RE, Wenzler E. Activity of potential alternative treatment agents for Stenotrophomonas maltophilia isolates Nonsusceptible to Levofloxacin and/or trimethoprim-sulfamethoxazole. J Clin Microbiol. 2020;58(2):e01603–01619.
Biagi M, Vialichka A, Jurkovic M, Wu T, Shajee A, Lee M, Patel S, Mendes RE, Wenzler E. Activity of Cefiderocol alone and in combination with levofloxacin, Minocycline, Polymyxin B, or Trimethoprim-Sulfamethoxazole against Multidrug-Resistant Stenotrophomonas maltophilia. Antimicrob Agents Chemother. 2020;64(9):e00559–00520.
Cercenado E, Cardenoso L, Penin R, Longshaw C, Henriksen AS, Pascual A. In vitro activity of cefiderocol and comparators against isolates of Gram-negative bacterial pathogens from a range of infection sources: SIDERO–WT–2014–2018 studies in Spain. J Glob Antimicrob Resist. 2021;26:292–300.
Cunha BA, Qadri SM, Ueno Y, Walters EA, Domenico P. Antibacterial activity of trovafloxacin against nosocomial gram-positive and Gram-negative isolates. J Antimicrob Chemother. 1997;39(Suppl Bsuppl2):29–34.
Juhász E, Krizsán G, Lengyel G, Grósz G, Pongrácz J, Kristóf K. Infection and colonization by Stenotrophomonas maltophilia: antimicrobial susceptibility and clinical background of strains isolated at a tertiary care centre in Hungary. Ann Clin Microbiol Antimicrob. 2014;13(1):1–7.
Nakamura R, Oota M, Matsumoto S, Sato T, Yamano Y. In Vitro Activity and in vivo efficacy of Cefiderocol against Stenotrophomonas maltophilia. Antimicrob Agents Chemother. 2021;65(4):e01436–01420.
Kampmeier S, Pillukat MH, Pettke A, Kossow A, Idelevich EA, Mellmann A. Evaluation of a Stenotrophomonas maltophilia bacteremia cluster in hematopoietic stem cell transplantation recipients using whole genome sequencing. Antimicrob Resist Infect Control. 2017;6:115.
Gajdacs M, Urban E. Epidemiological Trends and Resistance Associated with Stenotrophomonas maltophilia bacteremia: a 10-Year retrospective cohort study in a tertiary-care hospital in Hungary. Diseases. 2019;7(2):41.
Friedman N, Korman T, Fairley C, Franklin J, Spelman D. Bacteraemia due to Stenotrophomonas maltophilia: an analysis of 45 episodes. J Infect. 2002;45(1):47–53.
Glupczynski Y, Delmée M, Goossens H, Struelens M, Group BMIS. Distribution and prevalence of antimicrobial resistance among gram-negative isolates in intensive care units (ICU) in Belgian hospitals between 1996 and 1999. Acta Clin Belg. 2001;56(5):297–306.
Choi H, Ahn H, Lee R, Cho SY, Lee DG. Bloodstream infections in patients with hematologic diseases: causative organisms and factors Associated with Resistance. Infect Chemother. 2022;54(2):340–52.
Eryilmaz-Eren E, Izci F, Ture Z, Sagiroglu P, Kaynar L, Ulu-Kilic A. Bacteremia in hematopoietic stem cell recipients receiving fluoroquinolone Prophylaxis: incidence, resistance, and risk factors. Infect Chemother. 2022;54(3):446–55.
Mumcuoglu I, Caglar H, Erdem D, Aypak A, Gun P, Kursun S, Cakir EY, Aydogan S, Kirca F, Dinc B. Secondary bacterial infections of the respiratory tract in COVID-19 patients. J Infect Dev Ctries. 2022;16(7):1131–7.
Wu S, Yin D, Zhi P, Guo Y, Yang Y, Zhu D, Hu F. In Vitro Activity of MRX-8 and comparators against clinical isolated gram-negative Bacilli in China. Front Cell Infect Microbiol. 2022;12:829592.
AbuTaha SA, Al-Kharraz T, Belkebir S, Abu Taha A, Zyoud SH. Patterns of microbial resistance in bloodstream infections of hemodialysis patients: a cross-sectional study from Palestine. Sci Rep. 2022;12(1):18003.
Adan FN, Jeele MOO, Omar NMS. Epidemiology of Multidrug Resistant Non-fermentative Gram Negative Bacilli in patients with Hospital Acquired Pneumonia: an alarming report from Somalia. Infect Drug Resist. 2022;15:6297–305.
Chawla K, Berwal A, Hazra D, Kondalarao KM, Shenoy PA. Drug Resistance among Major non-fermenting Gram-negative pathogens isolated from respiratory tract infections in a Tertiary Care Hospital of South Karnataka. J Pure Appl Microbiol. 2022;16(3):2020–7.
Elsheredy A, Elsheikh A, Ghazal A, Shawky S. Prevalence of trimethoprim/sulfamethoxazole resistance genes among Stenotrophomonas maltophilia clinical isolates in Egypt. Acta Microbiol Immunol Hung. 2022;69(1):56–60.
Ho MM, Sun MH, Wu WC, Lai CC, Yeh LK, Hwang YS, Hsiao CH, Chen KJ. Antibiotic susceptibility and minimum inhibitory concentration for Stenotrophomonas maltophilia ocular infections. Antibiot (Basel). 2022;11(11):1457.
Khodashahi R, Naderi HR, Mohammadabadi M, Ataei R, Khodashahi M, Dadgarmoghaddam M, Elyasi S. Antimicrobial resistance patterns of bacterial and fungal isolates in COVID-19. Archives Clin Infect Dis 2022, 17(1).
Shortridge D, Streit JM, Mendes R, Castanheira M. In vitro activity of cefiderocol against US and European Gram-negative clinical isolates collected in 2020 as part of the SENTRY Antimicrobial Surveillance Program. Microbiol Spectr. 2022;10(2):e02712–02721.
Wu RX, Yu CM, Hsu ST, Wang CH. Emergence of concurrent levofloxacin- and trimethoprim/sulfamethoxazole-resistant Stenotrophomonas maltophilia: risk factors and antimicrobial sensitivity pattern analysis from a single medical center in Taiwan. J Microbiol Immunol Infect. 2022;55(1):107–13.
Zajac OM, Tyski S, Laudy AE. Phenotypic and molecular characteristics of the MDR Efflux Pump Gene-carrying Stenotrophomonas maltophilia strains isolated in Warsaw, Poland. Biology (Basel). 2022;11(1):105.
Zhou X, Wang L, Wu S, Yang Y, Guo Y, Shen S, Hu F, Yang F. Antimicrobial activities of sitafloxacin and comparators against the clinical isolates of less common nonfermenting gram-negative bacteria. J Glob Antimicrob Resist. 2022;30:123–6.
Hawser S, Kothari N, Monti F, Morrissey I, Siegert S, Hodges T. In vitro activity of eravacycline and comparators against Gram-negative and Gram-positive bacterial isolates collected from patients globally between 2017 and 2020. J Global Antimicrob Resist. 2023;33:304–20.
Khan A, Pettaway CH, Dien Bard J, Arias CA, Bhatti MM, Humphries RM. Evaluation of the performance of manual antimicrobial susceptibility testing methods and disk breakpoints for Stenotrophomonas maltophilia. Antimicrob Agents Chemother. 2021;65(5). https://doi.org/10.1128/aac. 02631 – 02620.
Ortiz-Gomez T, Toledano P, Gomez AC, Lopez M, Alonso CA, Ruiz J, Lagos J, Saenz Y. Phenotypic characteristics and Clonal relationships of Stenotrophomonas maltophilia isolates in hospitalized adults from a private Center in Lima, Peru. Infect Chemother. 2023;55(2):278–82.
Padovani M, Bertelli A, Corbellini S, Piccinelli G, Gurrieri F, De Francesco MA. In Vitro Activity of Cefiderocol on Multiresistant Bacterial Strains and Genomic Analysis of Two Cefiderocol Resistant Strains. Antibiot (Basel). 2023;12(4):785.
Song JE, Kim S, Kwak YG, Shin S, Um TH, Cho CR, Chang J. A 20-year trend of prevalence and susceptibility to trimethoprim/sulfamethoxazole of Stenotrophomonas maltophilia in a single secondary care hospital in Korea. Med (Baltim). 2023;102(4):e32704.
Srivastava S, Singh P, Sharad N, Kiro VV, Malhotra R, Mathur P. Infection trends, susceptibility pattern, and Treatment options for Stenotrophomonas maltophilia infections in Trauma patients: a retrospective study. J Lab Physicians. 2023;15(1):106–9.
Caliskan A, Copur Cicek A, Aydogan Ejder N, Karagoz A, Kirisci O, Kilic S. The antibiotic sensitivity of Stenotrophomonas maltophilia in a 5-year period and investigation of clonal outbreak with PFGE. J Infect Dev Ctries. 2019;13(7):634–9.
Mojica MF, Humphries R, Lipuma JJ, Mathers AJ, Rao GG, Shelburne SA, Fouts DE, Van Duin D, Bonomo RA. Clinical challenges treating Stenotrophomonas maltophilia infections: an update. JAC-Antimicrobial Resist. 2022;4(3):dlac040.
Rhoads DD. Stenotrophomonas maltophilia Susceptibility Testing challenges and strategies. J Clin Microbiol. 2021;59(9):e0109421.
Banar M, Sattari-Maraji A, Bayatinejad G, Ebrahimi E, Jabalameli L, Beigverdi R, Emaneini M, Jabalameli F. Global prevalence and antibiotic resistance in clinical isolates of Stenotrophomonas maltophilia: a systematic review and meta-analysis. Front Med (Lausanne). 2023;10:1163439.
Dadashi M, Hajikhani B, Nazarinejad N, Nourisepehr N, Yazdani S, Hashemi A, Hashemizadeh Z, Goudarzi M, Sameni F. Global prevalence and distribution of antibiotic resistance among clinical isolates of Stenotrophomonas maltophilia: a systematic review and meta-analysis. J Glob Antimicrob Resist 2023.
Chou CC, Shen CF, Chen SJ, Chen HM, Wang YC, Chang WS, Chang YT, Chen WY, Huang CY, Kuo CC, et al. Recommendations and guidelines for the treatment of pneumonia in Taiwan. J Microbiol Immunol Infect. 2019;52(1):172–99.
Khan A, Arias CA, Abbott A, Dien Bard J, Bhatti MM, Humphries RM. Evaluation of the Vitek 2, Phoenix, and MicroScan for Antimicrobial susceptibility testing of Stenotrophomonas maltophilia. J Clin Microbiol. 2021;59(9):e0065421.
Syed YY. Cefiderocol: a review in Serious Gram-negative bacterial infections. Drugs. 2021;81(13):1559–71.
Martínez-Servat S, Yero D, Huedo P, Marquez R, Molina G, Daura X, Gibert I. Heterogeneous colistin-resistance phenotypes coexisting in Stenotrophomonas maltophilia isolates influence Colistin susceptibility testing. Front Microbiol. 2018;9:2871.
Acknowledgements
Not applicable.
Funding
This research was supported by grant No: 1402-2-73-25892 from the Iran University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
DD-S conceptualized and designed the study and made revisions to the final manuscript. NBGH contributed to study design, identifying eligible studies, data extraction, design and production of figures, and wrote the manuscript. LD and ZE contributed to choosing eligible studies and data extraction. MSH contributed to the data and statistical analysis. TN contributed to manuscript writing and revisions. All authors were involved in the article and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Conflict of interest
The authors assert that the conducted investigation was devoid of any economic or monetary affiliations that could be perceived as a possible conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bostanghadiri, N., Sholeh, M., Navidifar, T. et al. Global mapping of antibiotic resistance rates among clinical isolates of Stenotrophomonas maltophilia: a systematic review and meta-analysis. Ann Clin Microbiol Antimicrob 23, 26 (2024). https://doi.org/10.1186/s12941-024-00685-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12941-024-00685-4