Abstract
Introduction
Stenotrophomonas maltophilia keratitis is an uncommon infectious disease of the cornea. The clinical features, antibiotic susceptibility, and clinical outcomes of S. maltophilia keratitis were investigated in this study.
Methods
Between January 2015 and February 2020, the medical records of 16 patients with culture-proven S. maltophilia-associated infectious keratitis were retrospectively reviewed. Clinical data were analyzed regarding risk factors, clinical presentation, antibiotic susceptibility, and clinical outcomes.
Results
The average age of the patients was 56.24 ± 24.84 years. The most common risk factors for S. maltophilia keratitis were trauma (6/16, 37.5%), use of contact lenses (6/16, 37.5%), and herpes simplex virus keratitis (3/16, 18.8%), which caused ocular instability. Regarding the antibiotic sensitivities, most isolates (15/16, 93.8%) were susceptible to fluoroquinolones, 87.5% (14/16) of them to aminoglycosides, and 81.3% (13/16) of them to beta-lactams. Patients were classified into two groups according to the initial antibiotic eye drops, and there were significant differences in the final visual acuity between two groups: mixed fluoroquinolone, beta-lactam, aminoglycoside group, and mixed beta-lactam and aminoglycoside groups (p = 0.039).
Conclusion
Ocular infection due to S. maltophilia is an opportunistic infection followed by instability of the ocular surface. In cases of S. maltophilia infection, mixed use of fluoroquinolone, beta-lactam, and aminoglycoside should be considered for treatment of choice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Stenotrophomonas maltophilia keratitis is an uncommon infectious disease of the cornea. |
Ocular infection due to S. maltophilia is an opportunistic infection followed by instability of the ocular surface. |
For S. maltophilia infection, mixed use of fluoroquinolone, beta-lactam, and aminoglycoside should be considered as treatment of choice. |
Multi-pathogenic infections in patients with S. maltophilia-associated ocular infection show poorer results than mono-pathogenic infections. |
Digital Features
This article is published with digital features, including a summary slide to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.14485314.
Introduction
Infectious keratitis is a severe disease that poses a threat to the cornea and visual acuity. The use of contact lens, ocular surface disease, diseases affecting the eyelids, eye surgery, human immunodeficiency virus infection, immunodeficiency, and steroid treatment may cause infectious keratitis [1,2,3,4]. The most important aspect of infectious keratitis is identifying the causal microbes based on cultures and treating patients on the basis of antibiotic sensitivities [5, 6]. Stenotrophomonas maltophilia is an opportunistic pathogen that is commonly detected in patients with immunodeficiencies and can cause pneumonia, bacteremia, endocarditis, meningitis, urinary tract infection, and skin or soft tissue infection. Infectious keratitis caused by S. maltophilia is uncommon [7, 8], and there are few sporadic case reports and case reviews on S. maltophilia keratitis [9,10,11,12,13,14,15,16]. In this study, we investigated the clinical features of S. maltophilia keratitis, the outcomes of its antibiotic susceptibility, and effective treatment solutions.
Compliance with Ethics Guidelines
The study protocol was reviewed by the Chosun University Hospital Institutional Review Board (Gwang-ju, South Korea), which granted a waiver of informed consent and exemption from ongoing IRB oversight. No patient identifying information was recorded or retained.
Methods
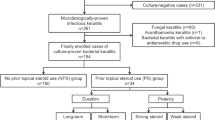
We retrospectively studied the medical records in our hospital, comprising culture data of 16 eyes from 16 patients with culture-proven S. maltophilia keratitis between January 2015 and February 2020. We excluded patients who had no culture data and whose follow-up period was < 1 month. This study was performed in accordance with guidelines of the Declaration of Helsinki and was approved by the Institutional Review Board of our hospital. Statistical analysis of the medical data was conducted for gender, age, general disease, history of ocular disease, operation record of ocular surgery, and predisposing factors. To evaluate the clinical process, we studied the size and position of corneal lesions at the first examination, existence of hypopyon, history of antibiotic use, surgical history, best-corrected visual acuity at the first and last visits, and epithelial regeneration period. The location of the infiltrate was defined as central if it was < 3 mm from the center and as peripheral if it was > 3 mm from the center. All patients underwent corneal scraping using a no. 15 Bard-Parker knife (Bard-Parker Co., Danbury, CT, USA) to obtain samples from the margins of infiltrates with transport medium and cultured on 5% sheep blood (blood agar plate). Sabouraud plates were incubated in CO [2] at 37 °C for up to 48 h. Isolates were identified using Vitek2 Gram Negative Identification cards (BioMerieux, Durham, NC), MALDI-TOF MS (ASTA, KOREA), or conventional microbiological procedures (aerobic/anaerobic growth, oxidase, motility, and nitrate) by experienced laboratory personnel. Antimicrobial susceptibility was evaluated using Vitek 2 g Negative Susceptibility cards. Results were interpreted according to the most current National Committee for Clinical Laboratory Standard guidelines.
We used a combination of 1.4% fortified tobramycin and 5% fortified cefazolin topical eye drops before obtaining the outcomes of the culture test. If the patients used topical fluoroquinolone eye drops (0.5% moxifloxacin, Vigamox®, Alcon, Fort Worth, TX, USA) before transfer to our hospital, we maintained the fluoroquinolone and added 1.4% fortified tobramycin and 5% fortified cefazolin eye drops. If the clinical symptoms and signs were improved, the antibiotics were maintained and tapered off; if the symptoms and signs worsened, we changed the antibiotics according to the results of antibiotic susceptibility. All statistical analyses were performed using SPSS version 20.0 (IBM Corp., Armonk, NY, USA). We compared the outcomes of treatment between the two groups. One group was treated with mixed fluoroquinolone, beta-lactam, and aminoglycoside, and the other group was treated with mixed beta-lactam and aminoglycoside antibiotics. We used Fisher’s exact test for categorical variables and Student’s t-test for continuous variables. P < 0.05 was considered statistically significant.
Results
We included 16 patients with S. maltophilia keratitis. The clinical data of the patients are shown in Table 1. The average age of the patients consisting of six men and ten women was 55.31 ± 17.27 years. Seven cases involved the right eye, and nine cases involved the left eye. The average follow-up period was 6.12 ± 4.19 months. Regarding the risk factors, 6/16 patients experienced ocular trauma (37.5%), 6/16 wore contact lenses (37.5%), 3/16 had a history of herpes simplex virus (HSV) keratitis (18.6%), and 1/16 had exposure keratitis (6.3%). Eight of these patients had systemic diseases, such as hypertension, diabetes mellitus, and brain infarction. The average surface area of ulcers was 16.63 ± 7.28 mm2. Regarding the locations of the ulcers, 11/16 were central and 5/16 were peripheral. Six of 16 patients showed hypopyon (37.5%). Fifteen patients responded well to antibiotic eye drops, but one patient underwent evisceration owing to severe ocular inflammation despite multiple anterior chamber irrigation and intracameral/intravitreal antibiotic injection. Among four patients who required surgical treatment, one underwent amniotic membrane transplantation, another underwent tarsorrhaphy, and corneal perforation was found in the other two patients who underwent corneal patch grafting. After remission, except for 1 patient who underwent evisceration, 15 patients underwent a visual acuity test; 13 patients showed better outcomes than the initial outcomes, and the visual acuity of 2 patients was unchanged.
Based on the results of the culture test, 3 of 16 patients had multi-pathogenic infections (Table 1). As shown in Table 2, there were 16 cases of antibiotic sensitivity. Almost all isolates (15/16, 93.8%) were susceptible to fluoroquinolones, 87.5% (14/16) to aminoglycosides, and 81.3% (13/16) to beta-lactams (Table 2). We classified the 16 cases based on the type of eye drops used: 8 cases used mixed fluoroquinolone, beta lactam, aminoglycoside, and 8 cases used beta lactam and aminoglycoside antibiotic eye drops. There were no statistically significant differences between the two groups in terms of sex and age, area and location of the ulcers, visual acuity before treatment, and epithelial regeneration period (p > 0.05). Visual acuities after treatment were significantly higher in the group using mixed fluoroquinolone, beta lactam, and aminoglycoside (p = 0.039) (Table 3).
Discussion
Cornea epithelial cells secrete IgA or surfactant proteins, e.g., surfactant protein, mucin glycoproteins, tight-junction/epithelial polarity, and epithelium-derived antimicrobial peptides (AMPs), which can inhibit or kill microbes. Unlike general infections, most ocular infections caused by S. maltophilia are preceded by ocular instability such as trauma and the use of contact lenses [9]. The barrier of corneal epithelial cells is destroyed, creating conditions that facilitate bacterial infection. Wiley et al. reported that S. maltophilia is one of the dominant bacteria of biofilms detected on patients’ contact lenses and is resistant to lens cleansers. In addition, the simultaneous use of corticosteroids in patients with corneal defects increases the risk of infection [17]. Another cause of S. maltophilia keratitis is ocular surface defects resulting from previous corneal surgeries or a patient’s corneal disease. It has been reported that patients with S. maltophilia keratitis have a higher incidence of ocular surface disease than those with other types of bacteria-induced keratitis [18, 19]. Similar to those reported previously, in the present study, the predominant causes in most cases were ocular trauma and the use of contact lenses. HSV keratitis and exposure keratitis, which can cause instability of the ocular surface, were also noted.
Infections due to S. maltophilia are less common than those due to Pseudomonas aeruginosa and have less toxic characteristics. Increased resistance of S. maltophilia to aminoglycosides, fluoroquinolones, and most beta-lactam antibiotics leads to poor treatment outcomes and is clinically important. A recent study showed that S. maltophilia is susceptible to the mixed use of ticarcillin and clavulanic acid [20]. It has been reported that S. maltophilia shows multidrug resistance to commonly used antibiotics and carbapenems [7, 8]; however, fluoroquinolone antibiotics may be the treatment of choice, based on a study by An-Lun et al. [21]. Another study has also shown that fluoroquinolones are also effective against S. maltophilia-associated endophthalmitis [22]. In the present study, most patients were susceptible to fluoroquinolones, beta-lactams, and aminoglycosides, except three patients who were resistant to multiple drugs. We compared the efficacy of antibiotics between the two groups. Visual acuities after treatment were significantly higher in the group using mixed fluoroquinolone, beta lactam, and aminoglycoside. Moreover, in the group using mixed beta lactams and aminoglycosides, two of eight patients did not show better outcomes than their initial visual acuities, and one patient underwent evisceration.
Multi-pathogenic infections in patients with S. maltophilia-associated ocular infection show poorer results than mono-pathogenic infections [23]. According to a previous study, the indirect pathogenicity of S. maltophilia plays an important role in the intervention between species [24]. In the present study, three cases had polymicrobial infections; two of these patients were classified as multidrug resistant, and one of them had culture-proven P. aeruginosa infection that did not respond to treatment. Eventually, this patient underwent evisceration. Accordingly, the results seem to be similar to those of other studies.
The limitations of this study were its retrospective design, involving a single center, and the small sample size. More accurate information regarding the response of S. maltophilia to antibiotics and treatment for polymicrobial infections requires extensive prospective research. Briefly, S. maltophilia is a relatively uncommon pathogen of keratitis, and S. maltophilia keratitis is related to several risk factors that cause instability of the ocular surface. Mixed use of fluoroquinolones, beta-lactams, and aminoglycosides is the treatment of choice for S. maltophilia infectious keratitis. In addition, in cases of polymicrobial infections, clinical attention is required because of resistance to antibiotics and poor outcomes.
Conclusion
Opportunistic ocular infection due to S. maltophilia is followed by instability of the ocular surface. In cases of S. maltophilia infection, mixed use of fluoroquinolone, beta-lactam, and aminoglycoside should be considered as treatment of choice.
References
Park MH, Yoo WS, Kim GN, et al. Clinical aspects of infectious keratitis in Western Gyeongsangnamdo, Republic of Korea. J Korean Ophthalmol Soc. 2019;60:731–9.
Ni N, Nam EM, Hammersmith KM, et al. Seasonal, geographic, and antimicrobial resistance patterns in microbial keratitis: 4-year experience in eastern Pennsylvania. Cornea. 2015;34:296–302.
Alipour F, Khaheshi S, Soleimanzadeh M. Contact lens-related complications: a review. J Ophthalmic Vis Res. 2017;12:193–204.
Sung MS, Choi W, You IC, et al. Factors affecting treatment outcome of graft infection following penetrating keratoplasty. Korean J Ophthalmol. 2015;29:301–8.
Solanki S, Rathi M, Khanduja S, et al. Recent trends: medical management of infectious keratitis. Oman J Ophthalmol. 2015;8:83–5.
Austin A, Lietman T, Rose-Nussbaumer J. Update on the management of infectious keratitis. Ophthalmology. 2017;124:1678–89.
Looney WJ, Narita M, Muhlemann K. Stenotrophomonasmaltophilia: an emerging opportunist human pathogen. Lancet Infect Dis. 2009;9:312–23.
Brooke JS. Stenotrophomonas maltophilia: an emerging global opportunistic pathogen. Clin Micro biol Rev. 2012;25:2–41.
Penland RL, Wilhelmus KR. Stenotrophomonas maltophilia ocular infections. Arch Ophthalmol. 1996;114:433–6.
Spraul CW, Lang GE, Lang GK. Xanthomonas maltophilia keratitis associated with contact lenses. CLAO J. 1996;22:158.
Richardson PR, Tappin MJ, Thickett KJ, et al. Temperature-dependent resistance to gentamicin in graft keratitis by Stenotrophomonas maltophilia. Eye (Lond). 1997;11(pt 1):124–6.
Cho BJ, Lee GJ, Ha SY, et al. Co-infection of the human cornea with Stenotrophomonas maltophilia and Aspergillus fumigatus. Cornea. 2002;21:628–31.
Fernandes M, Gangopadhyay N, Sharma S. Stenotrophomonas maltophilia keratitis after penetrating keratoplasty. Eye. 2005;19:921–3.
Kim JH, Shin HH, Song JS, et al. Infectious keratitis caused by Stenotrophomonas maltophilia and yeast simultaneously. Cornea. 2006;25:1234–6.
Mauger TF, Craig E. Combined acanthamoeba and Stenotrophomonas maltophilia keratitis treated with a conjunctival flap followed by penetrating keratoplasty. Cornea. 2006;25:631–3.
Holifield K, Lazzaro DR. Case report: spontaneous Stenotrophomonas maltophilia keratitis in a diabetic patient. Eye Contact Lens. 2011;37:326–7.
Wiley L, Bridge DR, Wiley LA, et al. Bacterial biofilm diversity in contact lens-related disease: emerging role of Achromobacter, Stenotrophomonas, and Delftia. Invest Ophthalmol Vis Sci. 2012;53:3896–905.
Green M, Apel A, Stapleton F. Risk factors and causative organisms in microbial keratitis. Cornea. 2008;27:22–7.
Keay L, Edwards K, Naduvilath T, et al. Microbial keratitis predisposing factors and morbidity. Ophthalmology. 2006;113:109–16.
Yao JDC, Louie M, Louie L, et al. Comparison of E test and agardilution for antimicrobial susceptibility testing of Stenotrophomonas-(Xanthomonas) maltophilia. J ClinMicrobiol. 1995;33:1428–30.
Wu AL, Yeh LK, Ma DH, et al. Clinical characteristics of Stenotrophomonas maltophilia keratitis. Cornea. 2016;35:795–800.
Ji Y, Jiang C, Ji J, et al. Post-cataract endophthalmitis caused by multidrug-resistant Stenotrophomonas maltophilia: clinical features and risk factors. BMC Ophthalmol. 2015;15:14.
Lim NC, Lim DK, Ray M. Polymicrobial versus monomicrobial keratitis: a retrospective comparative study. Eye Contact Lens. 2013;39:348–54.
Kataoka D, Fujiwara H, Kawakami T, et al. The indirect pathogenicity of Stenotrophomonas maltophilia. Int J Antimicrob Agents. 2003;22:601–6.
Acknowledgements
This study was supported by the research fund from Chosun University, 2015.
Funding
This study was supported by the research fund from Chosun University, 2015. The Rapid Service Fee was funded by the Authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship contributions
Beom-chan Park, Hwa-Rang Lim: statistical analysis, drafting the manuscript, editing. Jae-Woong Koh: concept and design, statistical analysis. Seon-Joo Park: concept and design.
Disclosures
Beom-chan Park, Hwa-Rang Lim, Jae-Woong Koh, and Seon-Joo Park have nothing to declare.
Compliance with Ethics Guidelines
The study protocol was reviewed by the Chosun University Hospital Institutional Review Board (Gwang-ju, South Korea), which granted a waiver of informed consent and exemption from ongoing IRB oversight. No patient identifying information was recorded or retained.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Park, BC., Lim, HR., Park, SJ. et al. Clinical Features and Management of Stenotrophomonas Maltophilia Keratitis. Ophthalmol Ther 10, 525–533 (2021). https://doi.org/10.1007/s40123-021-00348-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-021-00348-z