Abstract
Background
Knowledge of the population genetics and transmission dynamics of Plasmodium vivax is crucial in predicting the emergence of drug resistance, relapse pattern and novel parasite phenotypes, all of which are relevant to the control of vivax infections. The aim of this study was to analyse changes in the genetic diversity of P. vivax genes from field isolates collected at different times along the Thai–Myanmar border.
Methods
Two hundred and fifty-four P. vivax isolates collected during two periods 10 years apart along the Thai–Myanmar border were analysed. The parasites were genotyped by nested-PCR and PCR–RFLP targeting selected polymorphic loci of Pvmsp1, Pvmsp3α and Pvcsp genes.
Results
The total number of distinguishable allelic variants observed for Pvcsp, Pvmsp1, and Pvmsp3α was 17, 7 and 3, respectively. High genetic diversity was observed for Pvcsp (H E = 0.846) and Pvmsp1 (H E = 0.709). Of the 254 isolates, 4.3 and 14.6 % harboured mixed Pvmsp1 and Pvcsp genotypes with a mean multiplicity of infection (MOI) of 1.06 and 1.15, respectively. The overall frequency of multiple genotypes was 16.9 %. When the frequencies of allelic variants of each gene during the two distinct periods were analysed, significant differences were noted for Pvmsp1 (P = 0.018) and the Pvcsp (P = 0.033) allelic variants.
Conclusion
Despite the low malaria transmission levels in Thailand, P. vivax population exhibit a relatively high degree of genetic diversity along the Thai–Myanmar border of Thailand, in particular for Pvmsp1 and Pvcsp, with indication of geographic and temporal variation in frequencies for some variants. These results are of relevance to monitoring the emergence of drug resistance and to the elaboration of measures to control vivax malaria.
Similar content being viewed by others
Background
In Thailand, malaria is forest-related, with the highest prevalences recorded along regions bordering Myanmar, Laos and Cambodia. Forty-seven per cent of malaria cases in Thailand are due to Plasmodium vivax [1]. The control of P. vivax poses particular problems because of this parasite’s propensity to relapse. This is now compounded by the emergence of drug resistance; recently, one case of chloroquine-resistant vivax malaria has been reported in Thailand [2]. Approximately 6 % of Thai patients treated with a short acting anti-malarial drug followed by primaquine suffer a relapse of vivax malaria within 28 days [3]. To date, knowledge of the biology and epidemiology of P. vivax is relatively limited. Epidemiological and genetic studies of P. vivax population are essential for understanding the population dynamics and epidemiology of this parasite, and are relevant to monitoring responses to drug treatment.
Many polymorphic genetic markers are available for characterizing P. vivax populations [4–11]. Analyses of polymorphism and population diversity of P. vivax have focused on parasite molecules that are under selection by host immunity [12–15]. Most targeted polymorphic loci are found on single-copy P. vivax genes: msp1 coding for merozoite surface proteins (MSP1) (Pvmsp1), msp3alpha coding for another merozoite surface protein (Pvmsp3α), and csp coding for circumsporozoite protein (CSP)(Pvcsp). Pvmsp1 gene has a mosaic structure, with seven conserved blocks and six variable blocks [16]. Among these blocks, the variable block 10, previously designated as F3 fragment, is highly polymorphic and as such is a suitable genetic marker for population studies [5, 7, 17]. Pvmsp3α is characterized by a distinct alanine-rich central region [18] with a high degree of polymorphisms [11, 19, 20]. The Pvcsp harbours a central immunodominant region with a variable number of tandem repeats represented by two major variant types, VK210 and VK247 [21, 22] with a worldwide distribution [23]. The three loci above are considered to be under selective immune pressure.
The current genetic data on P. vivax population lags behind those on P. falciparum. This study aims to assess the genetic diversity using Pvmsp1F3, Pvmsp3α and Pvcsp loci in P. vivax isolates collected along the Thai–Myanmar border, and to investigate whether variations in frequencies occur geographically and temporally. This data is intended to help understand the dynamics of P. vivax populations, and to support the design of effective control measures.
Methods
Samples
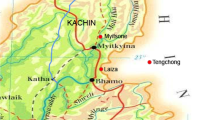
Two hundred and fifty-four stored anonymous frozen packed red cells collected during two periods: May 2003 to August 2004 (n = 173) and March 2012 to March 2013 (n = 81) were studied. DNA was extracted from the samples collected from patients presenting with P. vivax in Thai clinics along the Thai–Myanmar border in the west. The area is considered as having low and seasonal malaria transmission. The annual malaria incidence rates along Greater Mekong Subregion were 0.13–10.15 to 6/1000 populations in 2008 [24]. However, based on the record, some of the infections were probably acquired in the bordering countries. These isolates were from patients with the mean age (mean ± SD) of 25.28 ± 7.8 (range 14–57) and the mean % parasitaemia of 0.32 (range 0.1–1.19) during 2003–2004; and of 29.8 ± 11.5 (range 15–58) and the mean % parasitaemia of 0.401 (range 0.1–1.67) during 2012–2013. This cross sectional retrospective study was approved by the Ethics Committee of the Faculty of Tropical Medicine, Mahidol University (Approval number: MUTM 2013-034-01).
DNA template preparation
Plasmodium vivax genomic DNA was extracted from 200 µL of frozen-packed red cells using the commercially available DNA Blood kit according to the manufacturer’s instructions (QIAGEN, Germany). The volume of the template obtained was 100 µL, thus each 1 µL corresponds to the DNA present in 2 µL of whole blood. Confirmation of the microscopic diagnosis examination was achieved by a multiplex real-time PCR assay using both genus- and species-specific primers [25].
Genotyping of Pvmsp1F3 and Pvmsp3α by Nested PCR
Previously described primers for Pvmsp1F3 and Pvmsp3α [7] were used to amplify the polymorphic loci by nested PCR, with some modification. Briefly, amplification reactions were performed in a total volume of 25 µL containing 1X MyTag Red Mix (Bioline, UK) and 40 nM of each oligonucleotide primer. The amplification was initiated with 1 µL of the template genomic DNA, followed by the second amplification, in which 1 µL of diluted PCR products from the first amplification (at 1:1000 for Pvmsp1F3 and 1:100 for Pvmsp3α) were used. The cycling parameters were as follows: initial denaturation at 95 °C for 3 min; 30 cycles of denaturation at 95 °C for 1 min, followed by annealing at 60 °C for 1 min and extension at 72 °C for 1 min, and a final extension at 72 °C for 5 min. All PCR products were then analysed by electrophoresis on 3 % agarose gels and visualized under UV illumination after staining with ethidium bromide. The size of the amplified fragments was estimated by comparison to a 100 bp ladder marker. Each PCR product was screened for polymorphic banding by GeneTools analysis software (Syngene, UK). The genetic diversity of each marker was analysed by the number of alleles and the expected virtual heterozygosity (H E ), The expected virtual heterozygosity (HE), defining as the probability that a randomly chosen pair of alleles differed from each other can range between 0 and 1, with values close to 1, reflecting high genetic diversity levels in a population [7]. The formula of expected heterozygosity (HE) is [n/(n − 1)] × (1 − ∑pi2), where “n” is the number of samples analysed and Pi is the proportion of the parasite population having allele i. The mean multiplicity of infection (MOI) was calculated by dividing the total number of P. vivax clones by the number of PCR-positive isolates [7].
Genotyping of Pvcsp by PCR–RFLP
Pvcsp genotyping was based on restriction fragment length polymorphism analysis of the PCR products (PCR–RFLP) [5]. Briefly, Pvcsp was amplified by nested-PCR assay in a total of 25 µL and in presence of a reaction master mix containing 1X MyTag Red Mix (Bioline, UK) and 40 nM of each primer. One microlitres of template DNA was used to initiate amplification, followed by a second amplification, in which 1 µL of PCR products from the first amplification was used. The cycling conditions were as follows: 1 cycle of 95 °C for 5 min, 25 cycles (first amplification) and 30 cycles (second amplification) of denaturation at 94 °C for 1 min, followed by annealing at 62 °C for 2 min and extension at 72 °C for 2 min, and final extension at 72 °C for 5 min. Subsequently, 20 µL of the second PCR products were separately digested by restriction enzymes AluI and BstNI (New England Biolabs Inc., UK) according to the manufacture specification for 2 h in a total volume of 30 µL. The DNA fragments were separated by electrophoresis on 3 % agarose gel and visualized under UV illumination after ethidium bromide staining.
Statistical analysis
Statistical analyses were performed using SPSS software version 15.0. The frequencies of allelic variants in each marker between two different periods of sample collection were analysed using Chi square or Fisher’s exact test as appropriate. The P value was estimated by Monte Carlo based on the number of 10,000 randomly sampled data sets. P value of < 0.05 were considered as statistically significant.
Results
Genetic diversity and multiplicity of Pvmsp1F3, Pvmsp3α and Pvcsp
Amplification of the Pvmsp1F3 and Pvcsp fragments was achieved successfully for all the 254 P. vivax isolates, whereas the Pvmsp3α fragment could not be amplified in 45 isolates (18 %) despite repeated attempts (Table 1). The PCR fragments obtained were divided into bins that differed by 20 bp. Seven distinguishable Pvmsp1F3 size variants (designated A to G) with a size range of 220–360 bp (Fig. 1a) were observed with one variant (C, 251–270 bp) predominant at a frequency of 44 %. Three allelic size variants (designated A to C, 450–510 bp) were observed for the Pvmsp3α (Fig. 1b) at frequencies of 19, 34, and 47 %, respectively. Nine size variants (designated A to I, range 503–760 bp) were noted for Pvcsp (Fig. 1c) with the predominant variant (D, 641–660 bp) found at a frequency of 27 %. Pvcsp was further genotyped by RFLP [5] to distinguish between the two VK210 and VK247 repeat types (Fig. 2). When the PCR fragments are grouped by size and by repeat types, these could be divided into 17 different allelic forms, 9 PCR size variants for VK210 type and 8 for VK247 type (Fig. 3). The highest frequency was found for VK210D in both collection periods.
RFLP analysis of the Pvcsp fragments. In lanes with odd numbers, the fragments were digested with AluI (an enzyme that cuts repeatedly in the VK210 repeat region). In lanes with even numbers, the fragments were digested with BstNI (an enzyme that cuts repeatedly in the VK247 repeat region). Paired digestions from the fragments obtained from a single isolate are presented in lanes 1–2 (a VK210 variant), lanes 3–4 (a VK247 variant), and in lanes 5–6 and 7–8 in which mixed genotypes are present. A 100 bp ladder was used as molecular weight marker (M)
Frequency distribution of Pvcsp allelic variants from Thai P. vivax isolates collected over two periods. The number of isolates in the period of 2003–2004 (n = 173) and of 2012–2013 (n = 81) were analysed. Seventeen allelic variants were defined according to size (A to I) and repeat types (VK210 and VK247)
The multiplicity of infection (MOI) and the expected virtual heterozygosity (H E ) for Pvmsp1F3, Pvmsp3α and Pvcsp are shown in Table 1. High genetic diversity was observed in Pvmsp1F3 (H E = 0.709) and Pvcsp (H E = 0.846). Mixed genotype infections were observed in Pvmsp1F3 (n = 11, 7 MOI of 2 and 4 MOI of 3) and in Pvcsp (n = 37, 36 MOI of 2 and 1 MOI of 3) with a mean MOI of 1.06 and 1.15, respectively.
Distribution of allelic variants among P. vivax isolates along Thai–Myanmar border at different periods
The Pvmsp1F3 genotypes found in P. vivax isolates collected over two periods from the Thai–Myanmar border were compared (Fig. 4). Seven allelic Pvmsp1F3 variants were observed with low frequencies of the A and G variants. Infection with the C variant was predominant among isolates (44 %), and for both collection periods that were separated by ten years (38 % during 2002–2003 and 56 % during 2012–2013). A significant difference in the frequencies of the Pvmsp1F3 genotypes was found between the two collection periods (Fisher’s exact test, P = 0.018).
Distribution of Pvmsp1F3 allelic variants in P. vivax isolates collected along the Thai–Myanmar border during two periods. Distribution in 2003–2004 (black bars, n1 = number of isolates) and 2012–2013 (white bars, n2 = number of isolates) were shown. The allelic variants were designated A to G. Significant differences in allelic variant frequency between the two collection periods are indicated by asterisk (Fisher’s exact test, P = 0.018)
All three Pvmsp3α allelic variants were observed in the isolates from this area (Fig. 5). Infections with the C variant were predominant among the isolates (47 %), and for both collection periods (46 % for 2002–2003, and 48 % for 2012–2013). No significant differences in Pvmsp3α genotype frequencies were noted for the isolates collected during the two collection periods (X 2 = 0.701, degrees of freedom (df) = 2, P = 0.724).
Distribution of Pvmsp3α allelic variants in P. vivax isolates collected along the Thai–Myanmar border during two periods. Distribution in 2003–2004 (black bars, n1 = number of isolates) and 2012–2013 (white bars, n2 = number of isolates) were shown. The allelic variants were designated A to C. Chi square test did not detect any significant difference in allelic variant frequencies between the two collection periods (X 2 = 0.701, degrees of freedom (df) = 2, P = 0.724)
All 17 Pvcsp allelic variants (9 VK210 and 8 VK247) were found among the isolates collected. The distribution of single and mixed genotype infections of Pvcsp repeat types (VK210 and VK247) during two periods of 10 years different are shown in Fig. 6. Mixed Pvcsp genotype infections, either different allelic variants or different Pvcsp repeat types, were found among isolates with similar frequencies in both periods of sample collection (19 % during 2003–2004; 15 % during 2012–2013). VK210-only infections were predominant among isolates (66 %), and for both collection periods (69 % for 2002–2003, and 59 % for 2012–2013). Significant difference in frequencies of single and mixed Pvcsp genotype infections between the two periods was found (X 2 = 6.879, degree of freedom (df) = 2, P = 0.033). The frequency of VK210-single infection was slightly lower, but VK247-single infection was higher among isolates during 2012-2013 (VK210, 59 %; VK247, 26 %) than those during 2003–2004 (VK210, 69 %; VK247, 13 %).
Distribution of single and mixed genotype infections of the Pvcsp repeat types (VK210 and VK247) in P. vivax isolates collected along the Thai–Myanmar border. Distribution in the period of 2003–2004 (black bars, n1 = number of isolates) and of 2012–2013 (white bars, n2 = number of isolates) were shown. Significant differences in allelic variant frequencies between the two collection periods are indicated by asterisk (X 2 = 6.879, degrees of freedom (df) = 2, P = 0.033)
Discussion
It has long been known that the morphologically similar parasites of a Plasmodium species are in fact biologically and immunologically highly diverse. Until the advent of molecular genotyping through amplification, the study of this diversity for the parasites of humans was limited to experimental infections, enzyme typing, differential reactivity to specific antibodies, and, for P. falciparum, to in vitro cultured material. The advent of molecular genotyping based on genetic amplification has not only widened investigations to large numbers of field samples, but also to the all parasite species, including the hitherto neglected P. vivax.
The purpose of this study was to assess the genetic diversity of P. vivax collected from patients presenting in the Thai–Myanmar border of Thailand, for which a collection of samples obtained 10 years apart were available and based on the increasing evidence of drug resistance in this border area by the report in 2002–2003 of chloroquine resistance in P. vivax in Dawei (Mon State), Myanmar [26]. Given that P. vivax infections are generally treated with chloroquine, an emergence in 2008 of P. vivax resistance to chloroquine in this border area was reported and their spread has probably contributed to maintain a higher than expected level of genetic diversity [2].
Three polymorphic loci commonly used for the study of P. vivax were used for this study: the repeat region of Pvcsp, the F3 fragment of Pvmsp1F3 and a segment of Pvmsp3α, which were evaluated by the number of distinguishable size allelic variants found in P. vivax isolates. The data obtained for the Pvmsp1F3 and Pvcsp loci revealed that the parasites displayed a degree of genetic diversity with a high proportion of mixed genotype infections, which are in line with previous findings on the genetic diversity of P. vivax isolates collected from diverse endemic areas of Thailand [5, 9]. Recently, by using different sets of highly polymorphic microsatellite markers, a number of studies of genetic variability and transmission dynamics of P. vivax isolates from different malaria endemic areas have been observed with similar degree of diversity in Brazil (HE = 0.71) (H E = 0.71) [27]; Sri Lanka (H E = 0.86)/Myanmar (H E = 0.85)/Ethiopia (H E = 0.75) [28], and Vietnam (H E = 0.85) [29]. Moreover, some differences in the frequencies of Pvmsp1F3 variants and Pvcsp repeat types were noted among isolates in this border collected over the two distinct sample collection periods. Parasites with the Pvcsp VK210 repeat type dominated in all the samples sets analysed, a feature noted in other studies of isolates collected in Thailand [5, 9], Myanmar (98 %) [30], India (99 %) [6], Guyana (92 %) [31], Pakistan (96 %) and Iran (69 %) [8]. In the present study, VK247-single infection was higher among isolates collected during 2012–2013 (25 %) than those during 2003–2004 (13 %), with obviously higher in VK247G during 2012–2013 (14 %). This striking increasing incidence might cause by several selective constraints imposed by drug usage [32], as well as local vectors [33]. It is well documented from previous studies in different drug susceptibility between P. vivax VK247 subtype and VK210 subtype, in which the mean time to clear parasite DNA, as determined by quantitative PCR of P. vivax genotype-specific DNA during a treatment course, was significantly slower for VK210 parasites than for VK247 parasites [32]. Likewise, the differential susceptibility of mosquito vectors to P. vivax circumsporozoite phenotypes in southern Mexico was found, in which Anopheles albimanus is more susceptible to VK210 carrying parasites while Anopheles pseudopunctipennis is more susceptible to VK247 carrying parasites [33].
The Pvmsp3α fragment amplified in this study was relatively uninformative in that only three allelic variants were detected. In a previous study of P. vivax from Papua New Guinea employing the same amplification protocol, a high degree of diversity was observed, with 15 distinct allelic variants detected in 106 samples [7]. The contrast with the low diversity observed in this study is probably due to use of classical gel electrophoresis with a relatively low resolution (bin sizes of 20 bp) rather than capillary electrophoresis (bin sizes of 3 bp). This has also probably contributed to underestimate the diversity of Pvmsp1F3, since 28 distinct allelic variants were observed using capillary electrophoresis for the P. vivax isolates from Papua New Guinea [7]. It should be noted that genetic diversity is likely to be higher in Papua New Guinea where the malaria endemicity is higher than that on the Thai borders. Nonetheless, comparison of parasite genotyping data from different studies should be interpreted in the light of the resolution of the method used to distinguish between allelic variants. Sequencing of the allelic variants present in each would provide the most accurate data for genetic diversity studies; however, cost considerations preclude this for a number of researchers in endemic areas. Moreover, data from the standard protocols that are accessible to most is generally sufficient to provide a clear broad picture of parasite genetic diversity and to decide whether further more detailed studies would be warranted.
Whereas analyses of P. falciparum populations indicate that the MOI is broadly correlated with transmission levels [34–36], the observed MOI values for the Thai P. vivax isolates presented here were high despite the low levels of malaria transmission. This might indicate that the transmission levels are underestimated. It is probable that the presence of hypnozoites, which are the liver dormant forms that can activate at various times in the months and years following the infectious bite to initiate a blood infection, contributes significantly to this high level of diversity. P. vivax strains in Southeast Asia region are predicted to have a high relapse incidence (836 relapses per 100,000 person days) and a rapid mean time from primary episode to first relapse (41 days) [37]. Furthermore, analyses of relapse parasites clearly indicated that they are genetically diverse and often distinct from the parasites that appear during the primary infection [38, 39]. Another potential explanation is the geographical location of the site where the survey presented here was conducted. The proximity to the border of Myanmar where malaria endemicity is higher than in Thailand has probably contributed to increase diversity through the frequent movement of populations to and from Thailand, resulting in a steady introduction of strains. In the course of this study, a few P. vivax isolates were also collected at the Thai–Thai–Lao border (n = 1 during 2003–2004, and n = 10 during 2012–2013) and the Thai–Cambodia border (n = 3 during 2003–2004, and n = 10 during 2012–2013). Despite the limited number of isolates, they were found to harbour numerous distinct allelic variants for the three markers (five variants for Pvmsp1F3, threevariants for Pvmsp3α, and seven variants for Pvcsp, and three isolates had mixed Pvcsp genotype infections for the Thai–Lao boder; and six variants for Pvmsp1F3, three variants for Pvmsp3α, and 10 variants for Pvcsp and four isolates had mixed genotype infections at the Thai–Cambodia border). This might be due to the fact that P. vivax infections are generally treated with chloroquine, therefore, the emergence in 2008 of P. vivax resistance to chloroquine in areas of Myanmar bordering Thailand [26], and their spread has probably contributed to maintain a higher than expected level of genetic diversity [2].
Multiple genotype infections are common in malaria, and higher multiplicities of infections are likely to facilitate genetic recombination of parasites leading to the generation of novel strains [40], and could be an indicator of immune status [41]. Previous studies indicated that allelic recombination events are associated with the genetic diversity of Pvmsp1F3 [8, 16], Pvmsp3α [11, 20] and Pvcsp [10]. Mixed genotype Pvmsp1F3 or Pvcsp infections were found in 17 % of the isolates, a frequency similar to that observed in previous surveys in Thailand [5, 9], in India using Pvmsp3α [6], in Papua New Guinea using Pvmsp1F3 [42], or in Pakistan and Iran using Pvmsp1 [8]. Knowledge of the genetic diversity can be used to assess geographical differentiation and explain the spatial distribution of alleles at a given loci, and provide a baseline information for surveillance systems directed to identifying the origin of isolates in areas with occasional imported malaria cases [40].
The extensive polymorphism that characterize the loci targeted in this study are considered to be the result of selective constraints to which P. vivax is subjected [43], which include immune responses in the vertebrate host [39], drug pressure [32], as well as vector competence [33]. In this study, the degree of diversity recorded for the three markers did not vary between two collection that were separated by 10 years, though the frequencies of some Pvmsp1F3 and Pvcsp allelic variants altered significantly with time. Given the relatively limited number of isolates analysed and for each period, it is unclear whether these variations are sotchastic or due to selective pressure.
Conclusion
In summary, this study demonstrated that high genetic diversity and multiplicity of infection levels occur in the P. vivax parasites circulating along the Thai–Myanmar border despite the low level of malaria transmission to which the resident populations are subjected. The genotyping data presented will be useful to the selection of markers suitable for use in drug efficacy studies, and to an improved understanding of the epidemiology of P. vivax in Thailand, which can guide the design of measures to control and eventually eliminate this parasite.
Abbreviations
- Pvcsp :
-
circumsporozoite surface protein gene of Plasmodium vivax
- Pvmsp1 :
-
merozoite surface protein 1 gene of Plasmodium vivax
- Pvmsp3α:
-
merozoite surface protein 3 alpha gene of Plasmodium vivax
- PCR:
-
polymerase chain reaction
- RFLP:
-
restriction fragment length polymorphism
- bp:
-
base pair
- MOI:
-
multiplicity of infection
- H E :
-
expected virtual heterozygosity
References
WHO. World Malaria Report 2014. Geneva: World health Organization; 2014.
Rijken MJ, Boel ME, Russell B, Imwong M, Leimanis ML, Phyo AP, et al. Chloroquine resistant vivax malaria in a pregnant woman on the western border of Thailand. Malar J. 2011;10:113.
Krudsood S, Tangpukdee N, Wilairatana P, Phophak N, Baird JK, Brittenham GM, et al. High-dose primaquine regimens against relapse of Plasmodium vivax malaria. Am J Trop Med Hyg. 2008;78:736–40.
Cui L, Mascorro CN, Fan Q, Rzomp KA, Khuntirat B, Zhou G, et al. Genetic diversity and multiple infections of Plasmodium vivax malaria in Western Thailand. Am J Trop Med Hyg. 2003;68:613–9.
Imwong M, Pukrittayakamee S, Gruner AC, Renia L, Letourneur F, Looareesuwan S, et al. Practical PCR genotyping protocols for Plasmodium vivax using Pvcs and Pvmsp1. Malar J. 2005;4:20.
Kim JR, Imwong M, Nandy A, Chotivanich K, Nontprasert A, Tonomsing N, et al. Genetic diversity of Plasmodium vivax in Kolkata. Indian Malar J. 2006;5:71.
Koepfli C, Mueller I, Marfurt J, Goroti M, Sie A, Oa O, et al. Evaluation of Plasmodium vivax genotyping markers for molecular monitoring in clinical trials. J Infect Dis. 2009;199:1074–80.
Zakeri S, Raeisi A, Afsharpad M, Kakar Q, Ghasemi F, Atta H, et al. Molecular characterization of Plasmodium vivax clinical isolates in Pakistan and Iran using pvmsp-1, pvmsp-3alpha and pvcsp genes as molecular markers. Parasitol Int. 2010;59:15–21.
Kosaisavee V, Hastings I, Craig A, Lek-Uthai U. The genetic polymorphism of Plasmodium vivax genes in endemic regions of Thailand. Asian Pac J Trop Med. 2011;4:931–6.
Gonzalez-Ceron L, Martinez-Barnetche J, Montero-Solis C, Santillan F, Soto AM, Rodriguez MH, et al. Molecular epidemiology of Plasmodium vivax in Latin America: polymorphism and evolutionary relationships of the circumsporozoite gene. Malar J. 2013;12:243.
Rice BL, Acosta MM, Pacheco MA, Escalante AA. Merozoite surface protein-3 alpha as a genetic marker for epidemiologic studies in Plasmodium vivax: a cautionary note. Malar J. 2013;12:288.
Franke ED, Lucas CM, San Roman E. Antibody response of humans to the circumsporozoite protein of Plasmodium vivax. Infect Immun. 1991;59:2836–8.
Nogueira PA, Alves FP, Fernandez-Becerra C, Pein O, Santos NR, Pereira da Silva LH, et al. A reduced risk of infection with Plasmodium vivax and clinical protection against malaria are associated with antibodies against the N terminus but not the C terminus of merozoite surface protein 1. Infect Immun. 2006;74:2726–33.
Bitencourt AR, Vicentin EC, Jimenez MC, Ricci R, Leite JA, Costa FT, et al. Antigenicity and immunogenicity of Plasmodium vivax merozoite surface protein-3. PLoS ONE. 2013;8:e56061.
Stanisic DI, Javati S, Kiniboro B, Lin E, Jiang J, Singh B, et al. Naturally acquired immune responses to P. vivax merozoite surface protein 3α and merozoite surface protein 9 are associated with reduced risk of P. vivax malaria in young Papua New Guinean children. PLoS Negl Trop Dis. 2013;7:e2498.
Putaporntip C, Jongwutiwes S, Sakihama N, Ferreira MU, Kho WG, Kaneko A, et al. Mosaic organization and heterogeneity in frequency of allelic recombination of the Plasmodium vivax merozoite surface protein-1 locus. Proc Natl Acad Sci USA. 2002;99:16348–53.
Raza A, Ghanchi NK, Thaver AM, Jafri S, Beg MA. Genetic diversity of Plasmodium vivax clinical isolates from southern Pakistan using pvcsp and pvmsp1 genetic markers. Malar J. 2013;12:16.
Galinski MR, Corredor-Medina C, Povoa M, Crosby J, Ingravallo P, Barnwell JW. Plasmodium vivax merozoite surface protein-3 contains coiled-coil motifs in an alanine-rich central domain. Mol Biochem Parasitol. 1999;101:131–47.
Bruce MC, Galinski MR, Barnwell JW, Snounou G, Day KP. Polymorphism at the merozoite surface protein-3alpha locus of Plasmodium vivax: global and local diversity. Am J Trop Med Hyg. 1999;61:518–25.
Mascorro CN, Zhao K, Khuntirat B, Sattabongkot J, Yan G, Escalante AA, et al. Molecular evolution and intragenic recombination of the merozoite surface protein MSP-3alpha from the malaria parasite Plasmodium vivax in Thailand. Parasitology. 2005;131:25–35.
Arnot DE, Barnwell JW, Tam JP, Nussenzweig V, Nussenzweig RS, Enea V. Circumsporozoite protein of Plasmodium vivax: gene cloning and characterization of the immunodominant epitope. Science. 1985;230:815–8.
Rosenberg R, Wirtz RA, Lanar DE, Sattabongkot J, Hall T, Waters AP, et al. Circumsporozoite protein heterogeneity in the human malaria parasite Plasmodium vivax. Science. 1989;245:973–6.
Kain KC, Brown AE, Webster HK, Wirtz RA, Keystone JS, Rodriguez MH, et al. Circumsporozoite genotyping of global isolates of Plasmodium vivax from dried blood specimens. J Clin Microbiol. 1992;30:1863–6.
WHO. World Malaria Report 2008. Geneva: World Health Organization; 2008.
Kamau E, Tolbert LS, Kortepeter L, Pratt M, Nyakoe N, Muringo L, et al. Development of a highly sensitive genus-specific quantitative reverse transcriptase real-time PCR assay for detection and quantitation of Plasmodium by amplifying RNA and DNA of the 18S rRNA genes. J Clin Microbiol. 2011;49:2946–53.
Guthmann JP, Pittet A, Lesage A, Imwong M, Lindegardh N, Min Lwin M, et al. Plasmodium vivax resistance to chloroquine in Dawei, southern Myanmar. Trop Med Int Health. 2008;13:91–8.
Ferreira MU, Karunaweera ND, da Silva-Nunes M, da Silva NS, Wirth DF, Hartl DL. Population structure and transmission dynamics of Plasmodium vivax in rural Amazonia. J Infect Dis. 2007;195:1218–26.
Gunawardena S, Karunaweera ND, Ferreira MU, Phone-Kyaw M, Pollack RJ, Alifrangis M, et al. Geographic structure of Plasmodium vivax: microsatellite analysis of parasite populations from Sri Lanka, Myanmar, and Ethiopia. Am J Trop Med Hyg. 2010;82:235–42.
Van den Eede P, Erhart A, Van der Auwera G, Van Overmeir C, Thang ND, le Hung X, et al. High complexity of Plasmodium vivax infections in symptomatic patients from a rural community in central Vietnam detected by microsatellite genotyping. Am J Trop Med Hyg. 2010;82:223–7.
Moon SU, Lee HW, Kim JY, Na BK, Cho SH, Lin K, et al. High frequency of genetic diversity of Plasmodium vivax field isolates in Myanmar. Acta Trop. 2009;109:30–6.
Bonilla JA, Validum L, Cummings R, Palmer CJ. Genetic diversity of Plasmodium vivax Pvcsp and Pvmsp1 in Guyana, South America. Am J Trop Med Hyg. 2006;75:830–5.
Kain KC, Brown AE, Lanar DE, Ballou WR, Webster HK. Response of Plasmodium vivax variants to chloroquine as determined by microscopy and quantitative polymerase chain reaction. Am J Trop Med Hyg. 1993;49:478–84.
Gonzalez-Ceron L, Rodriguez MH, Nettel JC, Villarreal C, Kain KC, Hernandez JE. Differential susceptibilities of Anopheles albimanus and Anopheles pseudopunctipennis to infections with coindigenous Plasmodium vivax variants VK210 and VK247 in southern Mexico. Infect Immun. 1999;67:410–2.
Babiker HA, Ranford-Cartwright LC, Walliker D. Genetic structure and dynamics of Plasmodium falciparum infections in the Kilombero region of Tanzania. Trans R Soc Trop Med Hyg. 1999;93(Suppl 1):11–4.
Konate L, Zwetyenga J, Rogier C, Bischoff E, Fontenille D, Tall A, et al. Variation of Plasmodium falciparum msp1 block 2 and msp2 allele prevalence and of infection complexity in two neighbouring Senegalese villages with different transmission conditions. Trans R Soc Trop Med Hyg. 1999;93(Suppl 1):21–8.
Magesa SM, Mdira KY, Babiker HA, Alifrangis M, Farnert A, Simonsen PE, et al. Diversity of Plasmodium falciparum clones infecting children living in a holoendemic area in north-eastern Tanzania. Acta Trop. 2002;84:83–92.
Battle KE, Karhunen MS, Bhatt S, Gething PW, Howes RE, Golding N, et al. Geographical variation in Plasmodium vivax relapse. Malar J. 2014;13:144.
Imwong M, Snounou G, Pukrittayakamee S, Tanomsing N, Kim JR, Nandy A, et al. Relapses of Plasmodium vivax infection usually result from activation of heterologous hypnozoites. J Infect Dis. 2007;195:927–33.
Havryliuk T, Ferreira MU. A closer look at multiple-clone Plasmodium vivax infections: detection methods, prevalence and consequences. Mem Inst Oswaldo Cruz. 2009;104:67–73.
Cui L, Escalante AA, Imwong M, Snounou G. The genetic diversity of Plasmodium vivax populations. Trends Parasitol. 2003;19:220–6.
Vafa M, Troye-Blomberg M, Anchang J, Garcia A, Migot-Nabias F. Multiplicity of Plasmodium falciparum infection in asymptomatic children in Senegal: relation to transmission, age and erythrocyte variants. Malar J. 2008;7:17.
Koepfli C, Ross A, Kiniboro B, Smith TA, Zimmerman PA, Siba P, et al. Multiplicity and diversity of Plasmodium vivax infections in a highly endemic region in Papua New Guinea. PLoS Negl Trop Dis. 2011;5:e1424.
Escalante AA, Cornejo OE, Rojas A, Udhayakumar V, Lal AA. Assessing the effect of natural selection in malaria parasites. Trends Parasitol. 2004;20:388–95.
Authors’ contributions
SK designed the study; SM prepared DNA extraction, performed the genotyping and drafted the manuscript; PG supervised the genotyping techniques; SK provided P. vivax samples; JT prepared DNA extraction and data; CAL revised the manuscript; GS and SK supervised the work and revised the manuscript; SK financed the research. All authors read and approved the final manuscript.
Acknowledgements
We wish to thank Clinical Malaria Research Unit, Faculty of Tropical Medicine, Mahidol University for providing stored blood samples. We thank Somporn Krasaesub, Department of Administration, Armed Forces Research Institute of Medical Sciences (AFRIMS), Bangkok, Thailand for providing suggestions for data analysis. This study is supported by the Royal Golden Jubilee Ph.D. Program (RGJ) of the Thailand Research Fund, Grant No. PHD/0095/2554; the Office of Higher Education Commission, Ministry of Education, Thailand, Mahidol University under the National Research Universities Initiative; and the Faculty of Tropical Medicine, Mahidol University.
Competing interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Maneerattanasak, S., Gosi, P., Krudsood, S. et al. Genetic diversity among Plasmodium vivax isolates along the Thai–Myanmar border of Thailand. Malar J 15, 75 (2016). https://doi.org/10.1186/s12936-016-1136-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-016-1136-6