Abstract
Objective
Current literature is deficient in robust evidence delineating the correlation between the triglyceride glucose-body mass index (TyG-BMI) and the incidence of stroke. Consequently, this investigation seeks to elucidate the potential link between TyG-BMI and stroke risk in a cohort of middle-aged and senior Chinese individuals.
Methods
This study employs longitudinal data from four waves of the China Health and Retirement Longitudinal Study (CHARLS) conducted in 2011, 2013, 2015, and 2018, encompassing 8,698 participants. The CHARLS cohort was assembled using a multistage probability sampling technique. Participants underwent comprehensive evaluations through standardized questionnaires administered via face-to-face interviews. Our analytic strategy involved the application of Cox proportional hazards regression models to investigate the association between TyG-BMI and the risk of stroke. To discern potential non-linear relationships, we incorporated Cox proportional hazards regression with smooth curve fitting. Additionally, we executed a battery of sensitivity and subgroup analyses to validate the robustness of our findings.
Results
Our study utilized a multivariate Cox proportional hazards regression model and found a significant correlation between the TyG-BMI and the risk of stroke. Specifically, a 10-unit increase in TyG-BMI corresponded to a 4.9% heightened risk of stroke (HR = 1.049, 95% CI 1.029–1.069). The analysis also uncovered a non-linear pattern in this relationship, pinpointed by an inflection point at a TyG-BMI value of 174.63. To the left of this inflection point—meaning at lower TyG-BMI values—a 10-unit hike in TyG-BMI was linked to a more substantial 14.4% rise in stroke risk (HR 1.144; 95% CI 1.044–1.253). Conversely, to the right of the inflection point—at higher TyG-BMI values—each 10-unit increment was associated with a smaller, 3.8% increase in the risk of stroke (HR 1.038; 95% CI 1.016–1.061).
Conclusions
In the middle-aged and elderly Chinese population, elevated TyG-BMI was significantly and positively associated with stroke risk. In addition, there was also a specific non-linear association between TyG-BMI and stroke (inflection point 174.63). Further reduction of TyG-BMI below 174.63 through lifestyle changes and dietary control can significantly reduce the risk of stroke.
Similar content being viewed by others
Introduction
A stroke is medically characterized as an acute episode of neurological dysfunction, typically resulting from either a hemorrhage or an obstruction in blood flow, with symptoms persisting for more than 24 h or leading to death [1]. As a major health concern, stroke is associated with high rates of death, long-term disability, and limited effective treatments [2,3,4]. Data from the 2019 Global Burden of Disease study reveal that strokes have escalated from being the fifth to the third leading contributor to the global health burden since 1990 [5]. Projections indicate that, in the absence of effective preventive measures, annual stroke fatalities could reach between 7 and 8 million by the year 2030 [6]. The financial burden on families and society is enormous. Thus, the identification and management of stroke risk factors are crucial for prevention and for alleviating societal financial strains.
There is growing evidence that insulin resistance (IR) is recognized as a new risk factor for stroke and an early sign of type 2 diabetes, including not only diabetic but also nondiabetic individuals [7,8,9,10]. There are several methods to assess IR, and the Homeostasis Model Assessment of IR (HOMA-IR) has been widely used and shown its effectiveness in predicting cardiovascular disease [11]. Nevertheless, its requirement for fasting insulin levels limits its practicality in clinical settings. Studies have confirmed that the triglyceride-glycemic index (TyG), which consists of the product of fasting plasma glucose (FPG) levels and triglycerides (TG), is a simple, reproducible, and reliable index for assessing IR [12,13,14]. Many studies have confirmed the association of this index with stroke risk [15,16,17,18]. In addition, a study found that TyG is superior to HOMA-IR in predicting stroke risk [19]. Recently, there has been a surge of interest in a metric known as the triglyceride glucose-body mass index (TyG-BMI), which is the product of body mass index (BMI) and the TyG index. The TyG-BMI captures multiple clinical variables, such as BMI, glycemia, and lipid profiles simultaneously, and is more reflective of IR than the individual indices [20]. Studies have demonstrated that TyG-BMI is significantly associated with diabetes, hypertension, and nonalcoholic fatty liver disease (NAFLD) [21,22,23].
Since there is a significant association between IR and stroke, we hypothesized that TyG-BMI may be a valid predictor of stroke. Unfortunately, studies on the association between TyG-BMI and stroke are very limited, with only one cross-sectional study addressing this topic [24]. Besides, there are no studies investigating the non-linear relationship between them. In addition, studies differed in terms of implementation time, TyG-BMI range, sex ratio, and adjustment factors. Therefore, the relationship between TyG-BMI and stroke risk in the Chinese population remains unclear. To test this hypothesis, we embarked on a prospective cohort study using data from the China Health and Retirement Longitudinal Study (CHARLS) 2011–2018.
Methods
Study design
This cohort study used data from CHARLS from 2011 to 2018. TyG-BMI was considered the primary independent variable, and the incidence of stroke, coded as a binary variable (stroke = 1, no stroke = 0), served as the outcome of interest.
Data sources and study population
The data for this investigation were sourced from the China Health and Retirement Longitudinal Study (CHARLS), a comprehensive national cohort study designed to evaluate the economic, social, and health circumstances of the population [25]. The CHARLS cohort was established through a multistage probability sampling process, selecting participants from 450 communities across 150 counties in 28 provinces, resulting in 10,257 households included in the initial survey. The baseline survey included targeted individuals aged 45 and older as of the survey period, which spanned from June 2011 to March 2012. Data were collected via standardized questionnaires administered through personal interviews, with follow-up interviews conducted biennially. The study received ethical approval from the Biomedical Ethics Review Board of Peking University in China (IRB00001052-11015). All study participants provided written consent prior to their inclusion. The dataset and Additional file 1 pertinent to this study are publicly accessible on the CHARLS project’s website [25].
Our investigation drew upon data from waves of the CHARLS survey conducted in the years 2011, 2013, 2015, and 2018 [25]. The initial 2011–2012 baseline survey included 17,708 respondents. To refine our study group, we applied several exclusion criteria. Initially, we removed 1717 individuals who had been followed for less than two years. We also omitted 612 participants who had experienced a stroke prior to the baseline survey, 187 individuals for whom stroke data were incomplete, and 2 subjects who had received stroke treatment during the 2011 survey phase. Further exclusions were made for 4702 participants lacking blood glucose measurements and 1525 without recorded height or weight data. We also excluded 75 cases with TyG-BMI values exceeding three standard deviations from the mean. After applying these criteria, our final analysis encompassed 8698 participants. In addition, to further explore the relationship between changes in TyG-BMI (2011 to 2015) and stroke risk. We further included 5878 participants who had access to TyG-BMI values at both wave 1 and wave 3 surveys. The detailed methodology of our participant selection process is depicted in Fig. 1.
Variables
Calculation of triglyceride glucose-body mass index
The specific procedure for defining TyG-BMI in this study was as follows: TyG-BMI was calculated as TyG-BMI = BMI × TyG index, where TyG index = ln [FPG (mg/dL) × TG (mg/dL)/2], and BMI = weight/height2 (kg/m2) [14, 20].
Stroke diagnosis
Participants free of stroke at baseline who reported a stroke at subsequent follow-up were recorded as incident cases. Data on stroke occurrence were systematically gathered via a questionnaire inquiring if participants had been diagnosed with a stroke by a physician, the date of diagnosis or awareness of the condition, and whether they were undergoing treatment for their stroke [25, 26]. Affirmative responses during follow-up led to classification as first-time stroke diagnoses, with the reported date marking the onset. The interval between the stroke onset and baseline assessment was calculated to establish the timing of the stroke. For those without reported strokes during follow-up, we determined follow-up duration by the interval between the baseline assessment and their final survey date [25].
Covariates
Covariates were chosen based on prior studies and clinical expertise [26, 27]. The following covariates were included: (i) categorical variables: smoking status, sex, chronic kidney disease(CKD), chronic lung disease(CLD), malignant tumors, diabetes mellitus (DM), drinking status, hypertension; (ii) continuous variables: age, serum high-density lipoprotein cholesterol (HDL-c), BMI, Cystatin C, diastolic blood pressure(DBP), total serum cholesterol (TC), hemoglobin concentration (HGB), hemoglobin A1c (HBA1c), platelet (PLT), serum triglyceride (TG), fasting plasma glucose (FPG), serum low-density lipoproteins cholesterol (LDL-c), systolic blood pressure (SBP), blood urea nitrogen (BUN), Uric acid(UA), serum creatinine (Scr), Estimated glomerular filtration rate (eGFR).
Data collection
Interviewers trained by CHARLS staff at Peking University conducted in-home surveys using computer-assisted personal interviewing (CAPI) methods [25]. The core questionnaire of CHARLS included sections on demographics, health status, functioning, diagnosed chronic conditions, and health-related behaviors such as smoking, drinking, and exercise. These interviewers were also equipped to measure participants' physical health metrics, including height, weight, and blood pressure.
Participants were further requested to visit their nearest township hospital or local Centers for Disease Control and Prevention for comprehensive health evaluations. At these locations, trained nurses obtained an 8 mL fasting blood sample from each respondent. These samples underwent a complete blood count within one to two hours of collection. The samples were then prepared by separating plasma and red blood cells, followed by storage at − 20 °C for safe transportation. Finally, all collected blood samples were sent to Beijing for detailed analyses at the Chinese Center for Disease Control and Prevention [25].
To calculate the eGFR for “Asian origin” patients, the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula was employed [28]. This estimation takes into account variables such as sex, age, and Scr levels. The eGFR for female patients with Scr levels at or below 0.7 mg/dL is determined by the equation eGFR = 151 × (Scr/0.7)−0.328 × (0.993)age. For female patients with Scr levels above 0.7 mg/dL, the eGFR is calculated as eGFR = 151 × (Scr/0.7)−1.210 × (0.993)age. In male patients with Scr levels at or below 0.9 mg/dL, the eGFR is calculated using eGFR = 149 × (Scr/0.9)−0.415 × (0.993)age, and for those with Scr levels above 0.9 mg/dL, the eGFR formula is eGFR = 149 × (Scr/0.9)−1.210 × (0.993)age. The unit of age and Scr was year and mg/dL, respectively.
Missing data processing
In our study, there were missing data on BUN (1, 0.01%), smoking status (1, 0.01%), Scr (2, 0.02%), HDL-c (2, 0.02%), alcohol consumption (4, 0.05%), LDL-c (13, 0.15%), CLD (30, 0.34%), CKD (41, 0.47%), hypertension (46, 0.53%), DBP (61, 0.70%), HBA1c (62, 0.71%), DM (82, 0.94%), SBP (93, 1.06%), PLT (165, 1.90%), HGB (166, 1.91%), WBC (169, 1.94%), cystatin C (2090, 24.03%), and eGFR (2, 0.02%). In order to reduce bias due to missing variables, which prevented the modeling phase from accurately describing the statistical efficacy of the target sample, multiple imputations based on approaches reported by White and Groenwald for missing data [29, 30]. Age, LDL-c, drinking status, FPG, BUN, smoking status, HDL-c, CLD, eGFR, UA, malignancy, sex, TC, CKD, HBA1c, DM, PLT, and HGB were included in the estimation model (the number of iterations was 10, and the regression type was linear regression). The missing data analysis process used the missing at random (MAR) assumption [29].
Statistical analyses
Statistical analyses were conducted using R language software version 3.4.3 and Empower(R) software version 4.0. Statistical significance was defined as P values below 0.05 (two-sided). Baseline indicators were categorized based on the quartiles of TyG-BMI, and a comparison of the baseline characteristics was made for individuals in each group. Continuous variables were presented as median (interquartile range) or mean (SD: standard deviation), while categorical variables were described using percentages and frequencies. Differences between TyG-BMI groups were tested using the χ2 test, and differences in continuous variables were analyzed using analysis of variance (ANOVA) and the Kruskal–Wallis H test.
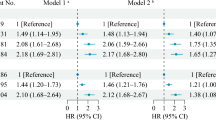
Univariate and multivariate Cox regression analyses were employed to evaluate the relationships between TG, FPG, TyG, BMI, and TyG-BMI with the risk of stroke. Three models were used: Model I (not adjusted for any covariates), Model II (adjusted for sex and age), Model III (adjusted for age, CRP, eGFR, sex; HDL-c, LDL-c, UA, CLD, PLT, Cystatin C; hypertension, HBA1C, diabetes; CKD, smoking, and drinking status variables). The TC was excluded from the final multivariate Cox proportional hazards model due to collinearity with other predictors, as detailed in Additional file 1: Table S1.
Besides, an unsupervised machine learning technique, the K-means algorithm with Euclidean distance, was utilized to group patients based on their TyG-BMI measurements in 2011 and 2015 [31]. Subsequently, the relationship between changes in TyG-BMI and the risk of stroke was investigated using a multivariate logistic regression model. Previous studies have shown a significant association between diabetes, obesity, CKD and stroke [32,33,34]. Several sensitivity analyses were performed to validate the findings. First, participants without diabetes (n = 8224) were analyzed. In addition, participants with a BMI ≥ 24 kg/m2 were excluded from the sensitivity analyses (n = 5208) [35]. Besides, the association between TyG-BMI and stroke risk in participants without CKD (n = 8120) was explored. In addition, continuous covariates were included in the equations using generalized additive modeling (GAM). The E-value was calculated to assess the possibility of unmeasured confounders between TyG-BMI and stroke risk [36].
To explore potential non-linear associations between the TyG-BMI index and stroke risk, we employed Cox proportional hazards models with smooth curve fitting. Where nonlinearity emerged, a recursive algorithm pinpointed the inflection point. We then formulated a piecewise Cox proportional hazards model on either side of these inflection points. The optimal model describing the TyG-BMI-stroke risk relationship was determined through a log-likelihood ratio test.
Subgroup analyses of different subgroups (age, sex, hypertension, smoking status, and alcohol consumption status) were performed using stratified Cox proportional hazards regression models. In addition to stratification factors, we adjusted for age, CRP, eGFR, sex, HDL-c, LDL-c, UA, CLD, PLT, Cystatin C, hypertension, HBA1C, DM, CKD, smoking, and drinking status. To assess the presence of an interaction term, we used likelihood ratio tests in models with and without an interaction term.
Results
Participant characteristics
A total of 8,698 participants, 4,008 males and 4,690 females, with a mean age of 59.36 (9.27) years, participated in the analysis. TyG-BMI was normally distributed, ranging from 88.45 to 331.39, with a mean (standard deviation) of 203.52 (38.66) (Fig. 2). Anthropometric and biochemical characteristics of patients stratified according to TyG-BMI quartiles are presented in Table 1. The results showed that various parameters such as FPG, BMI, TC, DBP, SBP, HBA1C, BMI, TyG, TG, UA, and HGB increased significantly with increasing TyG-BMI values. In contrast, age, HDL-c, BUN, and Scr showed opposite trends. In addition, the proportion of non-smokers, females, hypertensive disorders, and DM gradually increased with increasing TyG-BMI, whereas the proportion of males, CLD, and CKD gradually decreased.
The incidence rate of stroke
Table 2 showed that 1,001 participants had a stroke. The overall stroke incidence rate was 180 cases per 10,000 person-years. The stroke incidence rates for participants in the TyG-BMI quartiles were: Q1: 133.71/10000 person-years; Q2: 160.78/10000 person-years; Q3: 196.74/10000 person-years; Q4: 261.92/10000 person-years. The overall stroke incidence was 11.51%. The incidence for each TyG-BMI quartile was: Q1: 8.09%; Q2: 9.98%; Q3: 12.10%; Q4: 15.86% (Fig. 3). Participants with lower TyG-BMI had markedly lower stroke incidence compared to those with higher TyG-BMI.
Regardless of age group, women had a greater incidence of stroke among individuals in the age stratification based on age < 50, 50 to < 60, 60 to < 70, and ≥ 70. Additionally, it was shown that incidence rose with age in both men and women (Fig. 4).
Factors influencing the risk of stroke analyzed by univariate Cox proportional hazards regression
Based on univariate analyses, the risk of stroke was not related to BUN and HGB(P > 0.05), but was positively correlated with age, PLT, Scr, TC, TG, LDL-c, CRP, HBA1C, UA, Cystain C, FPG, hypertension, DM and current drinking, current smoking, whereas it was negatively associated with HDL-c and eGFR (all P < 0.05) (Additional fil 1: Table S2).
Relationship between TyG-BMI and the risk of stroke
To explore the association between TyG-BMI and stroke risk, we developed three Cox proportional hazards regression models, detailed in Table 3. A 10-unit increment in TyG-BMI was associated with a 7.1% elevation in stroke risk in Model I (HR = 1.071, 95% CI 1.055–1.087). Model II demonstrated an 8.4% increase in stroke risk per 10-unit increase in TyG-BMI (HR = 1.084, 95% CI 1.067–1.101). In Model III, each 10-unit rise in TyG-BMI was linked to a 4.9% increase in the risk of stroke (HR = 1.049, 95% CI 1.029–1.069).
Besides, we further converted TyG-BM from a continuous variable to a categorical variable based on quartiles. The multivariable-adjusted model revealed that, with the lowest quartile (Q1) as the reference, the hazard ratios (HRs) for the subsequent quartiles (Q2, Q3, and Q4) in relation to stroke risk were as follows: Q2 had an HR of 1.238 (95% CI 1.011, 1.517), Q3 had an HR of 1.387 (95% CI 1.128, 1.706), and Q4 had an HR of 1.611 (95% CI 1.292, 2.010). This indicates that, compared to participants in Q1, those in Q2 had a 23.8% increased risk of stroke, those in Q3 had a 38.7% increased risk, and those in Q4 had a 61.1% increased risk (Table 3).
Association of TG, FPG, TyG, and BMI with stroke risk based on multivariate Cox proportional hazards regression regression
The associations of TG, FPG, TyG, and BMI with stroke risk were further analyzed using multivariate Cox proportional hazards regression models (Additional file 1: Table S3). After adjusting for confounding variables, the results showed that there was no significant relationship between TG and FPG and stroke risk, with HR (95% CI, P) of 1.024 (95% CI 0.970–1.080, P = 0.389) and 1.015 (95% CI 0.987–1.044, P = 0.287), respectively. There was a significant positive relationship between BMI and the risk of stroke, with an increase in stroke risk of 4.5% for every 1 kg/m2 increase in BMI (HR = 1.045, 95% CI 1.025–1.064). In addition, TyG was significantly and positively associated with stroke risk, with each 1-unit increase in TyG increasing the risk of stroke by 16.5% (HR = 1.165, 95% CI 1.043–1.302).
Sensitivity analysis
To ensure the integrity of our findings, sensitivity analyses were systematically conducted. Initially, TyG-BMI was categorized into quartiles and subsequently reincorporated into the regression model in its modified categorical form. It was observed that the intervals between effect sizes were uniform across the groups, and this pattern of effect sizes remained congruent with those observed when TyG-BMI was assessed as a continuous variable, as indicated in Table 3.
Additionally, we introduced the continuity covariate as a curve into the equation using a GAM. Table 3 illustrated that the results obtained from Model IV closely paralleled those from the fully adjusted model, exhibiting an HR of 1.046 with a 95% CI of 1.026–1.067, achieving statistical significance (P < 0.001).
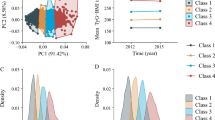
Besides, participants were categorized into two groups based on their TyG-BMI measurements in 2011 and 2015 using a K-means with Euclidean distance. These included a group in which a change in TyG-BMI between 2011 and 2015 was observed, with overall low TyG-BMI values (Class 1), and a group in which a change was observed alongside high TyG-BMI values (Class 2). As depicted in Additional file 1: Fig. S1, it was observed that participants in Class 1 exhibited overall low TyG-BMI levels (2011: 182.77 ± 22.56; 2015: 185.26 ± 24.08), whereas overall high TyG-BMI levels were exhibited by participants in Class 2 (2011: 245.52 ± 27.03; 2015: 250.24 ± 31.61). Multifactorial logistic regression analysis showed a 24.1% increased stroke risk in participants of Class 2 compared to participants of Class 1 (odds ratio OR = 1.241, 95CI% 1.012–1.523, P = 0.038) (Additional file 1: Table S4).
Furthermore, the study conducted additional analyses to verify the strength and consistency of the relationship between TyG-BMI and the risk of stroke by focusing on specific groups and adjusting for various health factors (Table 4). Firstly, in a group without DM, consisting of 8,224 participants, the analysis adjusted for factors such as age, CRP, eGFR, sex, HDL-c, LDL-c, UA, CLD, PLT, Cystatin C, hypertension, HBA1C, CKD, smoking, drinking status. This analysis still showed a significant positive link between TyG-BMI and stroke risk (per 10 units, HR = 1.052, 95%CI 1.030–1.073, P < 0.001). Secondly, when participants with CKD were excluded, the results were similar after adjusting for confounding variables (including age, CRP, eGFR, sex; HDL-c, LDL-c, UA, CLD, PLT, Cystatin C; Hypertension, HBA1C, diabetes, smoking, drinking status), the TyG-BMI association with stroke risk remained positively significant, with an HR(95% CI) of 1.048 (1.027–1.070, per 10 units of TyG-BMI). Lastly, the analysis was narrowed down to participants with a BMI under 24 kg/m2, adjusting for all the previously mentioned factors (included age, CRP, eGFR, sex; HDL-c, LDL-c, UA, CLD, PLT, Cystatin C, CKD, hypertension, HBA1C, DM, smoking, drinking status.). The findings showed a significant positive association between TyG-BMI (per 10 units) and stroke risk, with an HR (95%CI) of 1.062 (1.016, 1.110). Furthermore, the E-value (1.28) was found to be greater than the relative risk of TyG-BMI and unmeasured confounders (1.26), suggesting that unknown or unmeasured variables may have little effect on the relationship between TyG-BMI and stroke risk. Based on all sensitivity analyses, our findings were robust.
Cox proportional hazards regression model with smooth curve fitting to address nonlinearity
The nonlinearity of the association between TyG-BMI and stroke risk was discerned through the application of a Cox proportional hazards regression model with cubic spline functions, as depicted in Fig. 5. Subsequently, the most suitable model was ascertained via the log-likelihood ratio test, the results of which are detailed in Table 5, yielding a P-value of less than 0.05. An inflection point for the TyG-BMI was identified at 174.63 by employing a recursive algorithm. Post identification, a two-piecewise Cox proportional hazards regression model was utilized to ascertain the HRs and CIs on either side of this demarcation. It was observed that the HR stood at 1.144 (95% CI 1.044, 1.253) preceding the inflection point and 1.038 (95% CI 1.016–1.061) subsequent to it.
Results of subgroup analysis
The link between TyG-BMI and stroke risk was not affected by sex, age, smoking status, hypertension, and drinking status in any of the prespecified or exploratory subgroups examined (Table 6). That is to say, the interaction between these variables and TyG-BMI was not statistically significant (P > 0.05 for interaction).
Discussion
In this study, the connection between TyG-BMI and stroke incidence among middle-aged and senior individuals was evaluated. The findings revealed that a rise in TyG-BMI was associated with a significantly heightened risk of stroke. Additionally, an inflection point was identified, and different relationships between the TyG-BMI and stroke risk were detected on both sides.
The TyG index was first reported in 2008 and is considered a reliable, inexpensive, and simple surrogate for IR [37]. Many studies have confirmed that TyG is significantly associated with the incidence of atherosclerotic cardiovascular disease, including stroke [38,39,40,41,42,43]. A cohort study from the United States showed that after adjusting for potential confounders, each one-unit increase in the TyG index was associated with a 32.1% increase in the risk of stroke [43]. Another cohort study from China also showed a 34% increase in stroke risk for every 1-SD increase in the TyG index, with an adjusted HR of 1.34 (95% CI 1.11 to 1.61) [44]. In addition, the link between obesity and an elevated risk of stroke has been corroborated by numerous studies. BMI is frequently used as a measure of obesity, and a substantial positive correlation between BMI and the incidence of stroke has been documented in various research [34, 45, 46]. TyG-BMI is an obesity-related parameter that has been developed in recent years and has been strongly associated with NAFLD, cardiovascular events, prehypertension, and DM [21,22,23]. TyG-BMI is the product of BMI and TyG. This composite measure is believed to be a more accurate indicator of IR than individual indices. Given the known positive associations of both TyG and BMI with the risk of stroke and the critical role that IR is understood to play in stroke pathogenesis, we hypothesized that TyG-BMI might be positively correlated with stroke risk. Unfortunately, there is a scarcity of research investigating the connection between TyG-BMI and stroke risk, with only one study addressing this topic. A cross-sectional study from northeastern China showed that after multivariate adjustment, the risk of ischemic stroke increased by 20% for each standard deviation increase in TyG-BMI (OR = 1.20, 95% CI 1.10–1.32) [24]. Participants in the second and third tertiles of TyG-BMI had a significantly higher risk of ischemic stroke compared with those in the lowest tertile, with OR (95% CI) values of 1.39 (1.10–1.74) and 1.72 (1.37–2.17), respectively [24]. Our study expands on prior research supporting the hypothesis of a positive association between an elevated TyG-BMI index and stroke risk. Unlike previous studies, our investigation analyzed the TyG-BMI index as both categorical and continuous variables in relation to stroke risk, thus reducing information loss and quantifying their relationship. In addition, the K-means algorithm with Euclidean distance and logistic regression model were used to explore the association between changes in TyG-BMI and stroke risk, and it was found that those with consistently higher TyG-BMI had a similarly significant increase in stroke risk. Furthermore, sensitivity analyses specifically focused on participants who reported no CKD, no DM, and a BMI < 24 kg/m2. The results of the sensitivity analyses further confirmed that the relationships still existed in this group of participants. These results validate the stability of our findings. The identification of TyG-BMI as a risk factor for stroke and the elucidation of the relationship between the two provides a new perspective on stroke prevention and management, which is beneficial to patients' health outcomes and quality of life. In addition, it may lead clinicians and public health experts to revisit stroke risk assessment and prevention strategies.
The associations of TG, FPG, TyG, and BMI with stroke risk were further analyzed using multivariate Cox proportional hazards regression models. It was found that neither TG alone nor FPG was significantly associated with stroke risk, whereas the product of TG and FPG, the TyG index, was significantly and positively associated with stroke risk. Other possible reasons for this discrepancy include (1) the TyG index is considered a biomarker for metabolic syndrome [47]. Metabolic syndrome is an important factor in stroke risk and includes various metabolic abnormalities such as hypertension, abdominal obesity, and hyperlipidemia [48, 49]. Therefore, the TyG index provides a more comprehensive picture of the impact of these metabolic abnormalities on stroke risk than a single FPG or TG level. (2) Studies have confirmed that the TyG index is associated with IR, which is an independent risk factor for stroke [15]. IR may lead to a variety of pathologic changes, such as endothelial dysfunction, enhanced inflammatory response, and increased tendency to thrombosis, all of which may increase stroke risk [7, 15]. (3) FPG and TG can interact: Using FPG or TG levels alone to predict stroke risk may not be sensitive enough. However, if the two are combined into a single product, it may be possible to better reveal their interactions and synergistic effects in the metabolic process and thus more accurately predict stroke risk. In addition, BMI was also significantly and positively associated with stroke risk. Therefore, the tendency is to believe that the independent effect of TyG-BMI on stroke risk is based on the combined effect of TG, FPG, and BMI.
Although the precise mechanisms are not fully understood, the relationship between the TyG-BMI index and stroke risk is potentially linked to IR. The index is a composite measure that includes FPG, TG, and BMI, which serve as IR indicators. FPG levels reflect insulin sensitivity in the liver and insulin secretion in the pancreas [50]. In addition, the role of BMI and TG in recognizing IR has been demonstrated in previous studies [51,52,53]. TyG-BMI has been recommended as a marker for evaluating IR and IR-associated diseases [54, 55]. First, IR is implicated in the onset of atherosclerosis, fostering endothelial dysfunction, the emergence of foam cells, and the development of plaques prone to rupture [56,57,58]. Additionally, IR is often accompanied by a persistent state of mild inflammation, which can accelerate atherosclerotic processes and stimulate the release of pro-inflammatory markers [59, 60]. Moreover, IR can alter platelet function, leading to increased adhesion, activation, and aggregation, which may result in arterial narrowing or blockage, potentially leading to stroke [61, 62]. Therefore, the potential mechanism underlying the relationship between TyG-BMI and stroke incidence may be related to the association of three factors, FPG, TG, and BMI, with IR.
In addition, for the first time in our study, a non-linear relationship between TyG-BMI and stroke risk was observed. The inflection point of TyG-BMI was determined to be 174.63. When TyG-BMI was greater than 174.63, the risk of stroke decreased by 3.8% for every 10-unit decrease in TyG-BMI. On the other hand, when TyG-BMI was less than 174.63, the risk of stroke decreased by 14.4% for every 10-unit decrease in TyG-BMI. In other words, as the patient's TyG-BMI decreases, the risk of stroke gradually decreases. However, when TyG-BMI falls below 174.63, the stroke risk will fall more significantly. Further analysis showed that participants with TyG-BMI ≤ 174.63 had lower DBP, LDL-c, HB1AC, SBP, PLT, and UA, along with higher HDL-c, compared to those with TyG-BMI > 174.63. Additionally, those with TyG-BMI ≤ 174.63 had lower rates of CKD, DM, and hypertension (Additional file 1: Table S5). However, these indicators were strongly tied to stroke incidence [32,33,34, 63,64,65,66,67]. Due to these risk factors, the effect of TyG-BMI on stroke was relatively weak when TyG-BMI exceeded 174.63. In contrast, for those with TyG-BMI under 174.63, these stroke risk factors were lower and had less impact on stroke, and the role of TyG-BMI is relatively enhanced. This may explain the non-linear relationship between TyG-BMI and stroke risk. This finding of a curvilinear relationship between TyG-BMI and stroke has important clinical value. It facilitates clinical counseling and provides a basis for decision-making in stroke prevention. Combined reduction of BMI, TG, and FPG through dietary intervention and lifestyle changes can reduce the risk of stroke, and this risk will be significantly reduced by keeping TyG-BMI below 174.63. A previous cross-sectional study applied restricted cubic spline regression to analyze a possible non-linear relationship between TyG-BMI and ischemic stroke in the two cohorts included [24]. The results showed a linear relationship between TyG-BMI and ischemic stroke, with no threshold or saturation effect between the two. This is inconsistent with our findings of a non-linear relationship between TyG-BMI and stroke risk. The reasons may be as follows: first, the types of studies were different; the previous study was a cross-sectional study, whereas our study was a prospective cohort study. Second, the study populations were inconsistent; the previous study was a general population, whereas our study was a middle-aged and older population aged > 45 years. In addition, there were differences in the study methodology; the previous study used restricted cubic spline logistic regression to assess non-linear relationships. Whereas our study was a Cox proportional hazards model with cubic spline function. There were also differences in the covariates adjusted for, as we adjusted for more covariates, including UA, eGFR, DM, cystatin C, and CRP.
In the present study, several strengths have been identified. First, the application of both categorical and continuous TyG-BMI as independent variables was utilized to evaluate their association with stroke risk. This methodology was instrumental in diminishing information loss and in the precise quantification of the relationship under scrutiny. Second, the issue of missing data was addressed through the adoption of multiple imputation techniques. This strategy has been recognized for its capacity to enhance statistical power and for its role in minimizing bias that might arise from missing covariate data. Third, compared with previous studies, our study showed a significant improvement in the treatment of nonlinearity; for the first time, we found a non-linear relationship between TyG-BMI and stroke incidence. In addition, we performed a series of sensitivity analyses to ensure the stability of our findings. These analyses included exploring the relationship between changes in TyG-BMI (2011 to 2015) and stroke risk based on the K-means algorithm and multivariate logistic regression. The association between TyG-BMI and stroke incidence was reassessed after excluding subjects with DM, a BMI greater than 24 kg/m2, and CKD. Furthermore, the E-value was computed to assess the impact of potential unmeasured confounding factors, further affirming the study's findings.
The study in question presents certain limitations that warrant attention. Initially, the demographic focus on middle-aged and elderly individuals from China raises questions regarding the applicability of the findings to younger cohorts and different ethnic groups. To address this, future collaboration with international researchers is planned to explore these associations across varied genetic backgrounds. Additionally, the original dataset lacked certain stroke-related metrics, such as waist-to-hip ratio, medication usage, and familial stroke history. Third, as with all observational studies, residual confounding by unmeasured or uncontrolled confounders may remain despite adjustment for known potential confounders. However, we calculated E-values to assess the potential effect of unmeasured confounders, and the results suggested it was unlikely that these factors could entirely explain and influence our findings. Finally, this observational study could not ascertain causal relationships between TyG-BMI and stroke risk but only determine an association between them.
Conclusion
The study found a significant link between higher TyG-BMI levels and an increased risk of stroke among middle-aged and elderly individuals in China. Notably, the relationship between TyG-BMI and stroke risk was non-linear. When the TyG-BMI value was below 174.63, any further decrease in TyG-BMI was associated with a marked reduction in the risk of stroke. This study provides additional references to facilitate clinical consultation and optimize stroke prevention decisions.
Availability of data and materials
The data for this study can be accessed online at http://www.isss.pku.edu.cn/cfps/. To obtain the data, you will need to register as a user on the website. After your registration is reviewed and approved, you can follow the provided instructions to download the data set.
Abbreviations
- TyG-BMI:
-
Triglyceride glucose-body mass index
- HDL-c:
-
High-density lipoprotein cholesterol
- BMI:
-
Body mass index
- BUN:
-
Blood urea nitrogen
- LDL-c:
-
Low-density lipoproteins cholesterol
- FPG:
-
Fasting plasma glucose
- TG:
-
Triglyceride
- ALT:
-
Alanine aminotransferase
- SBP:
-
Systolic blood pressure
- TC:
-
Total cholesterol
- DBP:
-
Diastolic blood pressure
- GAM:
-
Generalized additive models
- Scr:
-
Serum creatinine
- OR:
-
Odds ratio
- eGFR:
-
Estimated glomerular filtration rate
- CKD:
-
Chronic kidney diseases
- UA:
-
Uric acid
- CLD:
-
Chronic lung diseases
- PLT:
-
Platelet
- DM:
-
Diabetes mellitus
- GAM:
-
Generalized additive model
- HBA1c:
-
Hemoglobin
- Ref:
-
Reference
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
References
Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, Elkind MS, George MG, Hamdan AD, Higashida RT, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(7):2064–89.
Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, Ford E, Furie K, Go A, Greenlund K, et al. Heart disease and stroke statistics–2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119(3):480–6.
Ishak B, Abdul-Jabbar A, Singla A, Yilmaz E, von Glinski A, Ramey WL, Blecher R, Tymchak Z, Oskouian R, Chapman JR. Intraoperative ischemic stroke in elective spine surgery: a retrospective study of incidence and risk. Spine. 2020;45(2):109–15.
Feigin VL, Nguyen G, Cercy K, Johnson CO, Alam T, Parmar PG, Abajobir AA, Abate KH, Abd-Allah F, Abejie AN, et al. Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. New Engl J Med. 2018;379(25):2429–37.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22.
Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurol. 2007;6(2):182–7.
Ding PF, Zhang HS, Wang J, Gao YY, Mao JN, Hang CH, Li W. Insulin resistance in ischemic stroke: mechanisms and therapeutic approaches. Front Endocrinol. 2022;13:1092431.
Zhao Y, Zhang J, Chen C, Qin P, Zhang M, Shi X, Yang Y, Lu J, Sun L, Hu D. Comparison of six surrogate insulin resistance indexes for predicting the risk of incident stroke: the Rural Chinese Cohort Study. Diabetes-Metab Res. 2022;38(7): e3567.
Chen W, Wang S, Lv W, Pan Y. Causal associations of insulin resistance with coronary artery disease and ischemic stroke: a Mendelian randomization analysis. BMJ Open Diab Res Care. 2020;8(1): e001217.
Wieberdink RG, Koudstaal PJ, Hofman A, Witteman JC, Breteler MM, Ikram MA. Insulin resistance and the risk of stroke and stroke subtypes in the nondiabetic elderly. Am J Epidemiol. 2012;176(8):699–707.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9.
Guerrero-Romero F, Simental-Mendía LE, González-Ortiz M, Martínez-Abundis E, Ramos-Zavala MG, Hernández-González SO, Jacques-Camarena O, Rodríguez-Morán M. The product of triglycerides and glucose, a simple measure of insulin sensitivity: comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocr Metab. 2010;95(7):3347–51.
Lee EY, Yang HK, Lee J, Kang B, Yang Y, Lee SH, Ko SH, Ahn YB, Cha BY, Yoon KH, et al. Triglyceride glucose index, a marker of insulin resistance, is associated with coronary artery stenosis in asymptomatic subjects with type 2 diabetes. Lipids Health Dis. 2016;15(1):155.
Han Y, Hu H, Li Q, Deng Z, Liu D. Triglyceride glucose-body mass index and the risk of progression to diabetes from prediabetes: a 5-year cohort study in Chinese adults. Front Public Health. 2023;11:1028461.
Yang Y, Huang X, Wang Y, Leng L, Xu J, Feng L, Jiang S, Wang J, Yang Y, Pan G, et al. The impact of triglyceride-glucose index on ischemic stroke: a systematic review and meta-analysis. Cardiovasc Diabetol. 2023;22(1):2.
Wang A, Wang G, Liu Q, Zuo Y, Chen S, Tao B, Tian X, Wang P, Meng X, Wu S, et al. Triglyceride-glucose index and the risk of stroke and its subtypes in the general population: an 11-year follow-up. Cardiovasc Diabetol. 2021;20(1):46.
Zhao Y, Sun H, Zhang W, Xi Y, Shi X, Yang Y, Lu J, Zhang M, Sun L, Hu D. Elevated triglyceride-glucose index predicts risk of incident ischaemic stroke: the Rural Chinese cohort study. Diabetes Metab. 2021;47(4):101246.
Wang X, Feng B, Huang Z, Cai Z, Yu X, Chen Z, Cai Z, Chen G, Wu S, Chen Y. Relationship of cumulative exposure to the triglyceride-glucose index with ischemic stroke: a 9-year prospective study in the Kailuan cohort. Cardiovasc Diabetol. 2022;21(1):66.
Pan Y, Jing J, Chen W, Zheng H, Jia Q, Mi D, Li H, Zhao X, Liu L, Wang C, et al. Post-glucose load measures of insulin resistance and prognosis of nondiabetic patients with ischemic stroke. J Am Heart Assoc. 2017;6(1): e004990.
Er LK, Wu S, Chou HH, Hsu LA, Teng MS, Sun YC, Ko YL. Triglyceride glucose-body mass index is a simple and clinically useful surrogate marker for insulin resistance in nondiabetic individuals. PLoS ONE. 2016;11(3): e149731.
Wang Y, Yang W, Jiang X. Association Between triglyceride-glucose index and hypertension: a meta-analysis. Front Cardiovasc Med. 2021;8:644035.
Wang X, Liu J, Cheng Z, Zhong Y, Chen X, Song W. Triglyceride glucose-body mass index and the risk of diabetes: a general population-based cohort study. Lipids Health Dis. 2021;20(1):99.
Wang R, Dai L, Zhong Y, Xie G. Usefulness of the triglyceride glucose-body mass index in evaluating nonalcoholic fatty liver disease: insights from a general population. Lipids Health Dis. 2021;20(1):77.
Du Z, Xing L, Lin M, Sun Y. Estimate of prevalent ischemic stroke from triglyceride glucose-body mass index in the general population. Bmc Cardiovasc Disor. 2020;20(1):483.
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 2014;43(1):61–8.
Wei G, Lin F, Cao C, Hu H, Han Y. Non-linear dose-response relationship between body mass index and stroke risk in middle-aged and elderly Chinese men: a nationwide Longitudinal Cohort Study from CHARLS. Front Endocrinol. 2023;14:1203896.
Chen X, Liu S, Chu J, Hu W, Sun N, Shen Y. Joint effect of elevated-c-reactive protein level and hypertension on new-onset stroke: a nationwide prospective cohort study of CHARLS. Front Public Health. 2022;10:919506.
Betzler BK, Sultana R, He F, Tham YC, Lim CC, Wang YX, Nangia V, Tai ES, Rim TH, Bikbov MM, et al. Impact of chronic kidney disease epidemiology collaboration (CKD-EPI) GFR estimating equations on CKD prevalence and classification among Asians. Front Med-Lausanne. 2022;9:957437.
White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30(4):377–99.
Groenwold RH, White IR, Donders AR, Carpenter JR, Altman DG, Moons KG. Missing covariate data in clinical research: when and when not to use the missing-indicator method for analysis. Can Med Assoc J. 2012;184(11):1265–9.
Timmerman ME, Ceulemans E, De Roover K, Van Leeuwen K. Subspace K-means clustering. Behav Res Methods. 2013;45(4):1011–23.
Mosenzon O, Cheng AY, Rabinstein AA, Sacco S. Diabetes and stroke: what are the connections? J Stroke. 2023;25(1):26–38.
Masson P, Webster AC, Hong M, Turner R, Lindley RI, Craig JC. Chronic kidney disease and the risk of stroke: a systematic review and meta-analysis. Nephrol Dial Transpl. 2015;30(7):1162–9.
Wang X, Huang Y, Chen Y, Yang T, Su W, Chen X, Yan F, Han L, Ma Y. The relationship between body mass index and stroke: a systemic review and meta-analysis. J Neurol. 2022;269(12):6279–89.
Zhou BF. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15(1):83–96.
VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268–74.
Ramdas NV, Satheesh P, Shenoy MT, Kalra S. Triglyceride Glucose (TyG) Index: a surrogate biomarker of insulin resistance. J Pak Med Assoc. 2022;72(5):986–8.
Ding X, Wang X, Wu J, Zhang M, Cui M. Triglyceride-glucose index and the incidence of atherosclerotic cardiovascular diseases: a meta-analysis of cohort studies. Cardiovasc Diabetol. 2021;20(1):76.
Tao LC, Xu JN, Wang TT, Hua F, Li JJ. Triglyceride-glucose index as a marker in cardiovascular diseases: landscape and limitations. Cardiovasc Diabetol. 2022;21(1):68.
Liu X, Tan Z, Huang Y, Zhao H, Liu M, Yu P, Ma J, Zhao Y, Zhu W, Wang J. Relationship between the triglyceride-glucose index and risk of cardiovascular diseases and mortality in the general population: a systematic review and meta-analysis. Cardiovasc Diabetol. 2022;21(1):124.
Liu Q, Cui H, Ma Y, Han X, Cao Z, Wu Y. Triglyceride-glucose index associated with the risk of cardiovascular disease: the Kailuan study. Endocrine. 2022;75(2):392–9.
Liao C, Xu H, Jin T, Xu K, Xu Z, Zhu L, Liu M. Triglyceride-glucose index and the incidence of stroke: a meta-analysis of cohort studies. Front Neurol. 2022;13:1033385.
Wang X, Liu Q, Wang T, Tian W, Chen X, Zhang J, Li Q, Ma D, Zhao L, Chen Z, et al. Triglyceride-glucose index and the risk of stroke in American adults: findings from the atherosclerosis risk in communities study. Diabetol Metab Syndr. 2023;15(1):187.
Huang Q, Yin L, Liu Z, Wei M, Feng J, Huang Q, Liu Y, Liu Z, Xia J. Association of novel lipid indicators with the risk of stroke among participants in Central China: a population-based prospective study. Front Endocrinol. 2023;14:1266552.
Bardugo A, Fishman B, Libruder C, Tanne D, Ram A, Hershkovitz Y, Zucker I, Furer A, Gilon R, Chodick G, et al. Body mass index in 1.9 million adolescents and stroke in young adulthood. Stroke. 2021;52(6):2043–52.
Gu H, Shao S, Liu J, Fan Z, Chen Y, Ni J, Wang C, Tu J, Ning X, Lou Y, et al. Age- and sex-associated impacts of body mass index on stroke type risk: a 27-year prospective cohort study in a low-income population in China. Front Neurol. 2019;10:456.
Kang SW, Kim SK, Kim YS, Park MS. Risk prediction of the metabolic syndrome using TyG Index and SNPs: a 10-year longitudinal prospective cohort study. Mol Cell Biochem. 2023;478(1):39–45.
Decker JJ, Norby FL, Rooney MR, Soliman EZ, Lutsey PL, Pankow JS, Alonso A, Chen LY. Metabolic syndrome and risk of ischemic stroke in atrial fibrillation: aric study. Stroke. 2019;50(11):3045–50.
Sheikh K. Metabolic syndrome and stroke. Stroke. 2008;39(11): e163 (Author reply e164).
Rizza RA. Pathogenesis of fasting and postprandial hyperglycemia in type 2 diabetes: implications for therapy. Diabetes. 2010;59(11):2697–707.
Stancáková A, Javorský M, Kuulasmaa T, Haffner SM, Kuusisto J, Laakso M. Changes in insulin sensitivity and insulin release in relation to glycemia and glucose tolerance in 6414 Finnish men. Diabetes. 2009;58(5):1212–21.
Watts GF, O’Brien SF, Silvester W, Millar JA. Impaired endothelium-dependent and independent dilatation of forearm resistance arteries in men with diet-treated non-insulin-dependent diabetes: role of dyslipidaemia. Clin Sci. 1996;91(5):567–73.
Tirosh A, Shai I, Bitzur R, Kochba I, Tekes-Manova D, Israeli E, Shochat T, Rudich A. Changes in triglyceride levels over time and risk of type 2 diabetes in young men. Diabetes Care. 2008;31(10):2032–7.
Tuo X, Yuan J, Wang XH, Xin Z. Identifying the insulin resistance index in nondiabetic Chinese subjects. Medicine. 2020;99(5): e19023.
Lim J, Kim J, Koo SH, Kwon GC. Comparison of triglyceride glucose index, and related parameters to predict insulin resistance in Korean adults: an analysis of the 2007–2010 Korean National Health and Nutrition Examination Survey. PLoS ONE. 2019;14(3): e212963.
Guo W, Zhu W, Wu J, Li X, Lu J, Qin P, Zhu C, Xu N, Zhang Q. Triglyceride glucose index is associated with arterial stiffness and 10-year cardiovascular disease risk in a chinese population. Front Cardiovasc Med. 2021;8:585776.
Wu S, Xu L, Wu M, Chen S, Wang Y, Tian Y. Association between triglyceride-glucose index and risk of arterial stiffness: a cohort study. Cardiovasc Diabetol. 2021;20(1):146.
Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C, Zuñiga FA. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. 2018;17(1):122.
Rohm TV, Meier DT, Olefsky JM, Donath MY. Inflammation in obesity, diabetes, and related disorders. Immunity. 2022;55(1):31–55.
Jin A, Wang S, Li J, Wang M, Lin J, Li H, Meng X, Wang Y, Pan Y. Mediation of systemic inflammation on insulin resistance and prognosis of nondiabetic patients with ischemic stroke. Stroke. 2023;54(3):759–69.
Du T, Yuan G, Zhang M, Zhou X, Sun X, Yu X. Clinical usefulness of lipid ratios, visceral adiposity indicators, and the triglycerides and glucose index as risk markers of insulin resistance. Cardiovasc Diabetol. 2014;13:146.
Santilli F, Vazzana N, Liani R, Guagnano MT, Davì G. Platelet activation in obesity and metabolic syndrome. Obes Rev. 2012;13(1):27–42.
Lindenstrøm E, Boysen G, Nyboe J. Influence of systolic and diastolic blood pressure on stroke risk: a prospective observational study. Am J Epidemiol. 1995;142(12):1279–90.
Ae R, Kanbay M, Kuwabara M. The causality between the serum uric acid level and stroke. Hypertens Res. 2020;43(4):354–6.
Robson R, Lacey AS, Luzio SD, Van Woerden H, Heaven ML, Wani M, Halcox JP, Castilla-Guerra L, Dawson J, Hewitt J. HbA1c measurement and relationship to incident stroke. Diabet Med. 2016;33(4):459–62.
Sadeghi F, Kovács S, Zsóri KS, Csiki Z, Bereczky Z, Shemirani AH. Platelet count and mean volume in acute stroke: a systematic review and meta-analysis. Platelets. 2020;31(6):731–9.
Amarenco P, Labreuche J, Touboul PJ. High-density lipoprotein-cholesterol and risk of stroke and carotid atherosclerosis: a systematic review. Atherosclerosis. 2008;196(2):489–96.
Acknowledgements
We would like to express our appreciation to the researchers and staff involved in the China Health and Retirement Longitudinal Study (CHARLS), as well as the study's participants. Their contributions have been essential in providing the data and methodological framework that underpin our study.
Funding
The study was conducted without any financial support; it did not receive funding from any grants, institutions, or other sources.
Author information
Authors and Affiliations
Contributions
The study was conceptualized by YS, HH, QL, and CC, who also drafted the initial manuscript and conducted the statistical analysis. DL and YH contributed to the manuscript revision and were instrumental in the study’s design. All authors involved in the study have read and given their approval to the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was ethically conducted and approved by the Biomedical Ethics Review Committee of Peking University in accordance with the principles of the Helsinki Declaration. Moreover, all participants provided written informed consent to take part in the study (IRB approval number IRB00001052–11015).
Consent for publication
Not applicable.
Competing interests
The authors affirm that they do not have any competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Table S1. Collinearity screening. Table S2. Factors influencing the risk of stroke were analyzed by univariate Cox proportional hazards regression. Table S3. Association of TG, FPG, TyG and BMI with stroke risk in different models. Table S4. Multivariate logistic regression analysis of the association between different TyG-BMI change groups (change from 2011 to 2015) and stroke risk. Table S5. The Baseline Characteristics of participants on both sides of the inflection point. Figure S1. showed the distribution of TyG-BMI across survey years after categorizing participants using the K-means algorithm. It was observed that participants in Class 1 exhibited overall low TyG-BMI levels (2011: 182.77 ± 22.56; 2015: 185.26 ± 24.08), whereas overall high TyG-BMI levels were exhibited by participants in Class 2 (2011: 245.52 ± 27.03; 2015: 250.24 ± 31.61).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shao, Y., Hu, H., Li, Q. et al. Link between triglyceride-glucose-body mass index and future stroke risk in middle-aged and elderly chinese: a nationwide prospective cohort study. Cardiovasc Diabetol 23, 81 (2024). https://doi.org/10.1186/s12933-024-02165-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-024-02165-7