Abstract
Background
The FIDELIO-DKD and FIGARO-DKD randomized clinical trials (RCTs) showed finerenone, a novel non-steroidal mineralocorticoid receptor antagonist (MRA), reduced the risk of renal and cardiovascular events in patients with type 2 diabetes mellitus (T2DM) and chronic kidney disease (CKD). Using RCT inclusion and exclusion criteria, we analyzed the RCT coverage for patients with T2DM and CKD in routine clinical practice in Germany.
Methods
German patients from the DPV/DIVE registries who were ≥ 18 years, had T2DM and CKD (an estimated glomerular filtration rate [eGFR] < 60 mL/min/1.73 m2 OR eGFR ≥ 60 mL/min/1.73m2 and albuminuria [≥ 30 mg/g]) were included. RCT inclusion and exclusion criteria were then applied, and the characteristics of the two populations compared.
Results
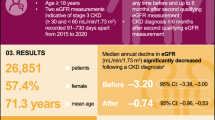
Overall, 65,168 patients with T2DM and CKD were identified from DPV/DIVE. Key findings were (1) Registry patients with CKD were older, less often male, and had a lower eGFR, but more were normoalbuminuric vs the RCTs. Cardiovascular disease burden was higher in the RCTs; diabetic neuropathy, lipid metabolism disorders, and peripheral arterial disease were more frequent in the registry. CKD-specific drugs (e.g., angiotensin-converting enzyme inhibitors [ACEi] and angiotensin receptor blocker [ARBs]) were used less often in clinical practice; (2) Due to the RCT’s albuminuric G1/2 to G4 CKD focus, they did not cover 28,147 (43.2%) normoalbuminuric registry patients, 4,519 (6.9%) albuminuric patients with eGFR < 25, and 6,565 (10.1%) patients with microalbuminuria but normal GFR (≥ 90 ml/min); 3) As RCTs required baseline ACEi or ARB treatment, the number of comparable registry patients was reduced to 28,359. Of these, only 12,322 (43.5%) registry patients fulfilled all trial inclusion and exclusion criteria. Registry patients that would have been eligible for the RCTs were more often male, had higher eGFR values, higher rates of albuminuria, more received metformin, and more SGLT-2 inhibitors than patients that would not be eligible.
Conclusions
Certain patient subgroups, especially non-albuminuric CKD-patients, were not included in the RCTs. Although recommended by guidelines, there was an undertreatment of CKD-patients with renin-angiotensin system (RAS) blockers. Further research into patients with normoalbuminuric CKD and a wider prescription of RAS blocking agents for CKD patients in clinical practice appears warranted.
Similar content being viewed by others
Background
The prevalence of chronic kidney disease (CKD) has increased in recent decades alongside an increase in diabetes and hypertension, the main drivers of CKD [1]. Kidney disease, attributable to diabetes mellitus (diabetic kidney disease; DKD), is one of the most common complications of diabetes and affects ~ 40% of patients with type 2 diabetes (T2DM) [2, 3]. The typical presentation of DKD includes a long-standing duration of diabetes, retinopathy, albuminuria without hematuria and gradually progressive kidney disease. However, reduced eGFR without albuminuria has been also frequently reported and is becoming increasingly more prevalent. DKD can ultimately lead to end-stage renal disease and is associated with an increased risk of cardiovascular (CV) disease and death [4,5,6]. Finally, people with diabetes can also develop CKD due to etiologies other than diabetes and some may have a combination of DKD and non-diabetic CKD [7].
Renin-angiotensin system (RAS) blockers, such as angiotensin converting enzyme inhibitors (ACEis) and angiotensin receptor blockers (ARBs), in the context of a multifactorial risk minimization strategy have been tested for their ability to revert CKD progression or at least prevent its further deterioration and were included in guidelines as a standard therapy for diabetic patients with CKD [8,9,10,11,12]. Furthermore, recent studies have shown that sodium-glucose co-transporter-2 (SGLT2) inhibitors improve renal outcomes [12,13,14]. However, despite the use of ACEIs, ARBs, and the concomitant use of SGLT2 inhibitors, the rate of renal deterioration remains high, with more than twice the normal decline in kidney function in patients with diabetes compared to patients without diabetes [13].
One of the potential reasons for the residual renal deterioration is an increase in aldosterone levels which are elevated in up to 50% of patients treated with RAS blockers within a year of initiating treatment, leading to increases in albuminuria and impairment of kidney function [15]. In line with this assumption, it has been shown that mineralocorticoid receptor antagonists (MRAs), even when added to ACEIs and ARBs, decrease proteinuria in patients with CKD [16]. As earlier MRAs, such as spironolactone and eplerenone, were effective but tended to show intolerable side effects, such as gynecomastia and hyperkalemia, a more tolerable but at least as effective and safe next-generation MRA was developed. Finerenone, a novel, non-steroidal, selective MRA was investigated in two large phase III clinical trials in patients with CKD [17, 18]. In FIDELIO-DKD, finerenone improved renal outcomes in T2DM patients with advanced CKD [19]. In FIGARO-DKD, finerenone improved CV outcomes in T2DM patients with early CKD [20]. The outcomes of the two studies were confirmed in the pooled FIDELITY analysis [21].
We were interested in the coverage of these two clinical trials for T2DM patients with CKD in Germany. As we recently published data on the prevalence of CKD [22] and the degree of guideline-conformant treatment [23], we now applied the inclusion and exclusion criteria used for the FIDELITY trial [21] to CKD patients in the registry. In our analysis, we explored:
-
A)
Differences between the CKD population documented in DPV/DIVE and the population that was part of the combined finerenone clinical trials (FIDELITY).
-
B)
The coverage of the FIDELITY CKD population focusing on albuminuric patients compared with CKD patients included in the registry (DPV and DIVE).
-
C)
The impact of the baseline requirement of the prescription of ACEi or ARBs for the study population to be in line with guideline-recommendations AND the coverage of the FIDELITY population for patients with CKD within DPV/DIVE when all the CKD criteria, the requirement for ACEi/ARB treatment at baseline, and all the further inclusion and exclusion criteria were applied.
Methods
Study design and data sources
This analysis used combined data from the DPV and DIVE registries [24,25,26]. In short, the DPV initiative collects data on patients with diabetes mellitus from centers predominantly in Germany. Data are collected using DPV software and the anonymized data are sent to the University of Ulm for aggregation into the database. The DPV initiative was established in 1995 and was approved by the ethics committee of the University of Ulm. Data collection was further approved by local review boards.
The DIVE registry was established in 2011 [27]. Consecutive patients with diabetes mellitus, regardless of their disease stage, were enrolled from specialized diabetes centers across the country, and continue to be followed up. Data are entered into the DPV online database using DPV software. The protocol was approved by the ethics committee of Hannover Medical School, and all patients provided written informed consent.
Patients and centers
A total of 216 specialized diabetes-centers from Germany were included in the present analysis. Patients were sampled in March 2022 and included in the current analysis if they had T2DM, were at least 18 years old, initially registered from 2015 to 2021, and had a clinical diagnosis of CKD [28, 29].
Documentation
For the current analysis, data regarding age, gender, body mass index (BMI), blood pressure, renal parameters, antidiabetic and antihypertensive drug treatment, and current comorbidities were considered. Data for the most recent treatment year per patient were aggregated and analyzed. For retinopathy, the two most recent treatment years were considered. eGFR was calculated according to the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula [30].
Statistics
Data from all patients documented at German sites in DPV and DIVE were combined and analyzed as a single data set. Patients were selected based on the availability of required clinical data, while patients with missing information on other values were excluded and the respective number of patients with missing information reported in the demographics table. CKD was defined as eGFR < 60 mL/min/1.73 m2 OR eGFR ≥ 60 mL/min/1.73m2 and albuminuria (≥ 30 mg/g) [28, 29]. Table 1 describes the patient selection based on the trials’ CKD criteria. Table 2 summarizes the selection criteria (inclusion and exclusion) used for the FIDELIO-DKD/FIGARO-DKD randomized clinical trials (RCTs) [17, 18]. In general, similar inclusion/exclusion criteria could be applied to the DPV/DIVE population, apart from a few minor discrepancies due to the type of information recorded in the registry database. It is important to note, however, that diabetic retinopathy and heart failure had specific definitions in the clinical trials that could not completely be reflected in the registry dataset.
Categorical variables are presented as percentages. Continuous variables are presented as means with standard deviations or medians with first and third quartiles (Q1, Q3). Unadjusted comparisons were conducted using a Chi-squared or Kruskal–Wallis test. The false discovery rate method was used to correct p-values for multiple testing. A two-sided p-value < 0.05 was considered statistically significant. Statistical analysis was performed using SAS version 9.4 (build TS1M7).
Results
A total of 65,168 adult patients with T2DM and CKD from Germany were included in the current analysis. Reasons for patient exclusion from the analysis are displayed in Fig. 1 and comprised patients residing outside of Germany, patients with forms of diabetes other than T2DM, patients aged < 18 years, patients included before 2015, missing data for GFR/albuminuria, and patients presenting without CKD.
Compliance and non-compliance with the RCT criteria were based on the inclusion and exclusion criteria as outlined in Table 2.
Comparison of patients in FIDELITY vs. DPV/DIVE
A comparison of patient characteristics between the 65,168 registry patients and the FIDELITY population is presented in Table 3 (columns 1 and 2). CKD patients in the registry were older (72.6 vs. 64.8 years), less often male (52.6 vs. 69.8%), had a shorter duration of diabetes (13.7 vs. 15.4 years), had a lower eGFR (54.2 vs. 57.6 mL/min/1.73 m2), and were more often normoalbuminuric (43.2 vs. 1.8% with UACR < 30 mg/g) compared with patients included in the RCTs.
In addition, there were several differences between the registry and the FIDELITY population with respect to their comorbid disease profile (Table 4): On the one hand, patients in the registry had lower rates of pre-existent CV disease, such as hypertension (78.0 vs. 96.5%), diabetic retinopathy (6.0 vs. 38.0%), coronary artery disease (CAD; 11.0 vs. 30.7%), myocardial infarction (10.2 vs. 15.5%), and ischemic stroke (9.0 vs. 11.9%). On the other hand, higher rates of diabetic neuropathy (45.9 vs. 26.9%), lipid metabolism disorders (87.4 vs. 45.6%), peripheral arterial disease (23.8 vs. 16.0%), and heart failure (12.3 vs. 7.5%) were observed in the registry population.
The proportion of patients in the registry receiving concomitant medication was substantially lower than the corresponding proportion in the FIDELITY population (Table 5), including statins (36.9 vs. 72.2%), platelet aggregation inhibitors (9.8 vs. 56.0%), antihypertensive drugs (ACEi 26.8 vs. 39.0%; ARBs 16.7 vs. 60.9%; beta-blockers 36.3 vs 49.9%; loop diuretics 14.1 vs. 21.5; thiazide diuretics 4.6 vs. 24.2%; and calcium antagonists 20.3 vs. 56.5%), and glucose-lowering drugs (metformin 38.0 vs 58.0% and sulfonylurea 5.2 vs. 26.0%).
Impact of the FIDELITY specific CKD criteria on patient selection
Based on the focus of albuminuric CKD patients in FIDELITY (Table 6), many of the 65,168 patients in DPV/DIVE were not represented by the RCTs because they were normoalbuminuric (urinary albumin-to-creatinine ratio [UACR] < 30 mg/g; 43.2%). In addition, patients with severely impaired kidney function (eGFR < 25 ml/min/1.73m2; 6.9%) and patients with only slight renal impairment (UACR 30–300 mg/g, normal eGFR [≥ 90 ml/min/1.73m2]; 10.1%) were not represented by the RCTs. This resulted in 59.2% of registry patients not being eligible for the RCTs based on the trials’ CKD definition alone, leaving 39.8% of the registry patients that had CKD compatible with the clinical trials’ CKD definition. As a consequence, a CKD severity shift was observed between patients in clinical practice versus patients considered for the RCTs (Fig. 2).
Patients’ CKD characteristics: comparison of DPV/DIVE population (n = 65,168) with FIDELITY clinical trial populations. The figure describes the proportion of patients in the FIDELITY and the DIVE/DPV analysis respectively by subgroups defined by albuminuria and eGFR. eFGR, estimated glomerular filtration rate
Impact of the trial‘s additional inclusion and exclusion criteria on patient selection
Considering the RCT’s requirement for baseline treatment with either ACEi or ARBs, the number of patients for analysis was reduced from 65,168 to 28,359. Overall, 56.5% of the registry patients were not treated with a RAS inhibitor although this is recommended by guidelines and, therefore, needs to be fulfilled by regulatory requirements during clinical trials. As this excluded patients based on clinical practice-specific decisions (e.g., prescription of RAS blockers) rather than on trial determined criteria, we further analyzed 28,359 of the 65,168 patients (43.5%) with ACEi/ARB pre-treatment to assess how all inclusion and exclusion criteria combined affected the representativeness of the trials for patients in clinical practice (Table 2). Overall, 12,322 patients fulfilled all the trials’ inclusion and exclusion criteria (43.5%), while 16,037 patients did not (56.5%).
The RCT-eligible patients were more often male (57.2 vs. 49.1%; p < 0.0001), had higher eGFR values (mean 60.1 vs. 48.6 mL/min/1.73 m2; p < 0.0001), and had higher rates of albuminuria (microalbuminuria [MAU] 75.1 vs. 19.9%; p < 0.0001) than patients not eligible for inclusion in the RCTs (Table 3, columns 3 to 6). Other differences were also mostly statistically significant, but likely of limited clinical relevancy. Furthermore, the comorbidity profile was quite consistent between RCT-eligible and non-eligible patients from clinical practice (Table 4, columns 3 to 6). Although some of the differences reached statistical significance, the absolute difference and, therefore, the potential clinical relevance, were small. Finally, the rates of statins (62.3 vs. 56.5%; p < 0.0001), calcium antagonists (40.3 vs. 35.5%; p < 0.0001), and the use of metformin (50.4 vs. 38.6%; p < 0.0001)/SGLT2-inihibitors (12.4 vs. 8.2%; p < 0.0001) was higher in RCT-eligible patients than in patients not eligible for the RCTs (columns 4 and 5).
To explore further potential differences in the risk profile between those eligible and non-eligible for the clinical trials, we computed the risk for cardiovascular mortality and progressive CKD as to Levey et al. [28] (Additional file 1: Table S1). We found that, while registry patients with low cardiovascular risk are not retained in the RCT ( +) or (−) population, patients in the RCT ( +) group had an increased cardiovascular risk as compared to the patients not eligible. The overall cardiovascular risk as determined by the SCORE-2 [31] was 9.8% in the RCT ( +) and 8.7% in the RCT (−) group (p < 0.0001) (Additional file 1: Table S2). This risk difference was mostly based on higher systolic blood pressure values, higher non-HDL cholesterol and slightly more smokers. A similar pattern was observed for the risk of progressive CKD (Additional file 1: Table S1). While RCT ( +) patients had a higher eGFR, more patients in the RCT (−) group had microalbuminuria more often (Table 3). Factors that perpetuate renal disease (Additional file 1: Table S3), were more common in the RCT ( +) group as exemplified by the rate of proteinuria (24.9 vs. 6.72%; p < 0.0001).
Discussion
The principal findings of this analysis are as follows:
-
1) As expected, there was a noteworthy difference between patients included into the combined RCTs and those seen and treated in clinical practice; in particular with respect to a higher age, more female patients being treated, the comorbid CV disease profile, the lower rate of albuminuria, and the rate of appropriate ACEi/ARB drug use, which was rather low in clinical practice.
-
2) More specifically, based on the focus on CKD grade 1/2 to 4 with albuminuria in the RCTs, more than half of the patients with CKD in clinical practice (59.2%), namely normoalbuminuric patients, patients with severely impaired kidney function (eGFR < 25 ml/min/1.73m2), and patients with only slight renal impairment (moderate albuminuria and normal eGFR) were not covered by the finerenone clinical trial population.
-
3) Many of the patients in clinical practice with CKD (56.5%) were not pre-treated with ACEi or ARBs, although guidelines clearly recommend such treatment. For the RCTs, a run-in phase was conducted to adjust all patients to the individually highest tolerated in-label dose of ACEi or ARB. At baseline, all RCT-patients were treated with either an ACEi or an ARB. Therefore, the registry patients without RAS-inhibition were not covered by the RCTs. The application of the full set of inclusion and exclusion criteria to patients actually receiving ACEi/ARBs at baseline left 43.5% of patients that would have been included in the finerenone RCTs. Patients that would have been excluded from the RCTs were more often female, had lower eGFR values, lower rates of albuminuria and received less metformin/less SGLT2-inhibitors than RCT-eligible patients.
-
4) As a side-result, there was a clear undertreatment of CKD patients in clinical practice compared to the guideline recommendations.
Comparison of CKD patients in the trials vs. clinical practice
As patients in RCTs need, by authority request, to fulfil all guideline requirements to investigate the effect of the new drug on top of optimized standard of care treatment, a clear difference has been expected for the comparison between RCT-patients and clinical practice. It is well known that patients in clinical trials tend to be younger and represent a higher proportion of male patients, as was observed in the present analysis [33,34,35]. In recent RCTs, more high-risk patients are included to show a relevant clinical benefit and to shorten study duration. Nonetheless, some differences were noteworthy and require further discussion: (1) Diabetic retinopathy as a comorbid condition was diagnosed more often in the clinical trial population. Diabetic retinopathy was low and comparable in DPV/DIVE patients with or without RAS blocking agents and after applying the RCTs’ inclusion and exclusion criteria to these patients. Because retinopathy was part of the inclusion criteria of FIDELIO-DKD, it can be assumed that its investigation was mandated by the study protocol at or prior to baseline, resulting in more patients being diagnosed and less patients overlooked. Furthermore, it appears that retinopathy is less well investigated and documented in clinical practice, especially in its early stages [36]. (2) On the contrary, diabetic neuropathy was more often diagnosed in the registry population than in the RCT patients. Although there was no specific exclusion criterion for patients with neuropathy, these patients may only rarely have been considered candidates for inclusion in the finerenone RCTs by the trial physicians based on reasons not documented. (3) For the RCTs, patients with a clinical diagnosis of chronic heart failure with reduced ejection fraction and persistent symptoms (New York Heart Association class II–IV) were excluded, as there is a clear guideline recommendation for an MRA-treatment; hence inclusion in a placebo-controlled MRA study is ethically unacceptable. The 7.5% of the patients with heart failure in the RCT are likely to represent patients with preserved ejection fraction, which makes up about half of all patients with heart failure [37]. In the registry we were not able to discriminate heart failure patients with preserved or reduced ejection fraction and, therefore, it appears reasonable to expect a higher rate of heart failure (12.3%) in the registry population than in the RCTs. (4) The use of CV and anti-diabetic drug therapy was increased in the RCT-patients compared to clinical practice, where a clear undertreatment was seen. The increased rate of treatment in the RCT population on the one hand results from the specification of the optimized guideline-conformant background therapy and, on the other hand, it reflects the increased attention and optimization efforts seen in RCTs [38]. A potential further contributor to the apparent discrepancy is a potential underreporting of CV drug therapy in the treatment of diabetes specialists, as the drugs may be prescribed by the treating cardiologist and not fully recorded in the diabetologist’s file. (5) Finally, patients in the registry had a lower eGFR and were more likely to be normoalbuminuric, which is a result of the focus on CKD patients with albuminuria in the RCTs as already outlined and will be discussed below.
Exclusion of CKD patients based on the focus on CKD patients with albuminuria
The CKD definition commonly used today includes patients with a reduced eGFR (eGFR < 60 ml/min/1.73m2) with or without albuminuria. In comparison, the FILEDITY-population includes albuminuric patients only, as did most other RCTs in CKD-patients that have been published (DAPA-CKD, CREDENCE). The RCTs focus on albuminuric high-risk CKD patients for kidney and CV events [12, 39, 40] and a recent comparison of the trial population with finerenone eligible patients from the US [41] based on the NHANES data exactly described this picture: the US population had fewer individuals with severe albuminuria (> 300 mg/g) and more individuals with moderately elevated albuminuria (30–300 mg/g). In addition, it follows a classic diagnosis of diabetic nephropathy, which is based on the presence of persistent proteinuria, slowly evolving from a stage of MAU. Macroalbuminuria is then followed by a progressive decline in kidney function [42, 43]. While this so-called Mogensen sequence is still an important reference in type 1 diabetes, non-albuminuric renal impairment and progressive renal decline have more recently received increasing attention [44]. Pugliese et al. estimated that, among patients with T2DM, 50–65% have no CKD, 20–30% have albuminuria alone (but without a decline in the eGFR), and 15–25% have reduced eGFR. Of the latter subgroup with a reduced eGFR, about half of the patients present without relevant albuminuria, meaning that the other half of patients have reduced eGFR, but albuminuria [44]. This is in line with our own data; adding up eGFR stages 3 to 5 (n = 45,279) and putting these numbers into relation to those with eGFR stages 3 to 5 but without albuminuria (n = 28,147), we report a rate of 62.2%.
Similar to the present finding, patients with normoalbuminuric kidney disease were also excluded in the SGLT-2 inhibitor clinical trials CREDENCE [13, 45] and DAPA-CKD [46]. CREDENCE (Canagliflozin 100 mg/day) included patients with an eGFR 30 to 90 ml/min/1.73m2 and urinary albumin excretion of between 300–5000 mg/g [13, 45]. DAPA-CKD documented the effect of 5 or 10 mg/day of dapagliflozin in patients with an eGFR 25–75 ml/min/1.73m2 and urinary albumin excretion of between 200–5000 mg/g [46]. The latest SGLT-2 inhibitor trial, EMPA-KIDNEY (Empagliflozin 10 mg/day), considered patients with eGFR 20–45 OR eGFR 45–90 ml/min/1.73m2 with at least 200 mg/g of albuminuria [47]. Further to the above-mentioned CREDENCE and DAPA-CKD trials, normoalbuminuric patients with a severe decline of the eGFR (20–45 ml/min/1.73m2) were also documented in EMPA-KIDNEY. While the trial also included patients without diabetes and, therefore, cannot be directly compared to the results of our registry, it is the first to cover patients with normoalbuminuric CKD.
Given that normoalbuminuric CKD appears to be frequent with 43.2% of the patients in our clinical practice cohort with an eGFR below 60 ml/min/1.73m2, clinical trials studying the effects of drug treatment in this patient population, either with finerenone or SGLT2 inhibitors, are strongly desired.
Exclusion of patients based on the lack of ACEi/ARBs use
When selecting patients for the present analysis, we arrived at a number of 65,168 patients with CKD in the DPV/DIVE cohort. Of these, only 28,359 patients were prescribed either ACEi or ARBs, leaving 56.5% without any blockade of RAS despite CKD although guidelines recommend their use [12]. This probably is due to the inclusion of patients with either early or normoalbuminuric CKD. The rate is higher than reported rates of 36% non-prescription in moderate to severe CKD [48]. It further agrees with a previously published study from the US which looked into the use of antihypertensive drugs in patients with CKD [49]. Less than one half of the participants with CKD in the NHANES were using antihypertensive drugs. While beta-blockers were the most commonly used, ARBs were the least used antihypertensive agents among participants with CKD. Age (≥ 70 years), awareness of hypertension or diabetes, and higher stage of CKD were associated with an increased likelihood of antihypertensive drug use among participants with CKD. In our cohort, patients had a mean age of 73 years, 22.0% were not hypertensive based on a threshold of 140/90 mmHg, 31.3% had an eGFR of ≥ 60 mL/min/1.73 m2, and 43.2% of the patient had albuminuria not reaching 30 mg/g. Taken together the potential lack of coverage of the finerenone trials for clinical practice patients was mostly based on the lack of ACEi/ARB prescription in the registry patient population.
Exclusion of patients based on further trial specific criteria
The application of the full set of inclusion and exclusion criteria to patients actually receiving ACEi/ARBs at baseline left 43.5% of patients who would have been included in the finerenone RCTs. While the selection criteria ensure guideline-consistency, comparability of patients and patients’ safety in the clinical trials, they also exclude many patients that need further treatment in clinical practice. Patients that would have been excluded from the RCTs were slightly older, more often female, had lower eGFR values, substantially lower rates of albuminuria and received less SGLT2-inhibitors than eligible patients. As older people with CKD are also less likely to have albuminuria than younger people [50], it is possible that the lower frequency of albuminuria in the RCT-ineligible population compared with the RCT-eligible population could in part relate to these criteria.
Moreover, we observed and increased cardiovascular and renal risk in the registry population eligible for the clinical trials than in patients not eligible. This was based on a variety of specific risk factors such as systolic blood pressure values, non-HDL cholesterol levels and smoking. Also, the level of proteinuria was, as already outlined above, increased in RCT eligible patients.
The pattern of CV and diabetes-related drug therapy differed substantially between the finerenone RCTs and clinical practice, mainly based on the undertreatment with RAS blockers of the registry patients. However, if patients not treated with RAS blockers are excluded from the comparison, treatment patterns did not differ much. Furthermore, there was an apparent undertreatment with SGLT-2i and GLP-1RA despite the available evidence to support their use. It was higher though in the RCT eligible registry patients than in the clinical trials: GLP-1RA 9.7% vs. 7.2% and SGLT-2i 12.4% vs. 6.7%. Several potential factors may contribute to the low prescription rate, including prescriber hesitancy, treatment inertia and increased drug costs [51]. A lower use of statins, platelet aggregation inhibitors, ARBs, and calcium channel blockers were the most prominent differences. While the lack of platelet aggregation inhibitor use may be related to a lower prevalence of CAD in the clinical practice setting, all other treatments were intensified in the finerenone RCTs, due to guideline and authority recommendation and by a closer surveillance and optimized treatment when entering the trial.
Strengths and limitations
Major strengths of the current analysis are the large number of patients and the good quality of the data recorded in the DPV/DIVE databases. Nonetheless, not all information pertinent to the RCT selection criteria were available for all patients. For example, during the initial search in the entire DPV/DIVE database (n = 718,138), 102,439 patients did not have an eGFR value available (vs. 51,540 who were recorded as having no CKD), and it is possible that some of these patients might have been suitable for inclusion in the analysis if these data had been available. Furthermore, we were not able to discriminate heart failure with or without preserved ejection fraction and, as such, we were not able to fully resemble the trial inclusion and exclusion criteria in this regard. Finally, the clinical effectiveness of finerenone and its safety in clinical practice could not be evaluated as it was not registered at the time of the analysis. It should be kept in mind that p-values are based on large patient numbers and not all significant differences may have clinical relevancy.
Conclusions
The main findings of the present analysis are that certain patient subgroups, especially non-albuminuric CKD-patients, a common group in clinical practice, were not included in the finerenone RCTs. Furthermore, the registry data showed an undertreatment of CKD patients with RAS blockers in clinical practice, although guidelines clearly recommend such treatment. These limitations result in the study population being only partially comparable to clinical practice as data on finerenone are, therefore, not available for certain common patient groups. Further research into patients with normoalbuminuric CKD and a wider prescription of RAS blocking agents for patients with CKD in clinical practice appears warranted.
Availability of data and materials
The datasets generated and analyzed during the current study are not publicly available due to data privacy but aggregated data may be available from the corresponding author on reasonable request.
References
Xie Y, Bowe B, Mokdad AH, Xian H, Yan Y, Li T, Maddukuri G, Tsai CY, Floyd T, Al-Aly Z. Analysis of the global burden of disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int. 2018;94(3):567–81.
Gheith O, Farouk N, Nampoory N, Halim MA, Al-Otaibi T. Diabetic kidney disease: world wide difference of prevalence and risk factors. J Nephropharmacol. 2016;5(1):49–56.
Bailey RA, Wang Y, Zhu V, Rupnow MF. Chronic kidney disease in US adults with type 2 diabetes: an updated national estimate of prevalence based on kidney disease: improving global outcomes (KDIGO) staging. BMC Res Notes. 2014;7:415.
Alicic RZ, Rooney MT, Tuttle KR. Diabetic kidney disease: challenges, progress, and possibilities. Clin J Am Soc Nephrol. 2017;12(12):2032–45.
Narres M, Claessen H, Droste S, Kvitkina T, Koch M, Kuss O, Icks A. The incidence of end-stage renal disease in the diabetic (compared to the non-diabetic) population: a systematic review. PLoS ONE. 2016;11(1):e0147329.
Nichols GA, Deruaz-Luyet A, Hauske SJ, Brodovicz KG. The association between estimated glomerular filtration rate, albuminuria, and risk of cardiovascular hospitalizations and all-cause mortality among patients with type 2 diabetes. J Diabetes Complicat. 2018;32(3):291–7.
Anders HJ, Huber TB, Isermann B, Schiffer M. CKD in diabetes: diabetic kidney disease versus nondiabetic kidney disease. Nat Rev Nephrol. 2018;14(6):361–77.
Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, Remuzzi G, Snapinn SM, Zhang Z, Shahinfar S, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345(12):861–9.
Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB, Ritz E, Atkins RC, Rohde R, Raz I, et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med. 2001;345(12):851–60.
Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008;358(6):580–91.
Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The collaborative study group. N Engl J Med. 1993;329(20):1456–62.
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, Federici M, Filippatos G, Grobbee DE, Hansen TB, et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41(2):255–323.
Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, Edwards R, Agarwal R, Bakris G, Bull S, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380(24):2295–306.
Heerspink HJL, Stefansson BV, Correa-Rotter R, Chertow GM, Greene T, Hou FF, Mann JFE, McMurray JJV, Lindberg M, Rossing P, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383(15):1436–46.
Bomback AS, Klemmer PJ. The incidence and implications of aldosterone breakthrough. Nat Clin Pract Nephrol. 2007;3(9):486–92.
Bomback AS, Kshirsagar AV, Amamoo MA, Klemmer PJ. Change in proteinuria after adding aldosterone blockers to ACE inhibitors or angiotensin receptor blockers in CKD: a systematic review. Am J Kidney Dis. 2008;51(2):199–211.
Bakris GL, Agarwal R, Anker SD, Pitt B, Ruilope LM, Nowack C, Kolkhof P, Ferreira AC, Schloemer P, Filippatos G, et al. Design and baseline characteristics of the finerenone in reducing kidney failure and disease progression in diabetic kidney disease trial. Am J Nephrol. 2019;50:1–12.
Ruilope LM, Agarwal R, Anker SD, Bakris GL, Filippatos G, Nowack C, Kolkhof P, Joseph A, Mentenich N, Pitt B, et al. Design and baseline characteristics of the finerenone in reducing cardiovascular mortality and morbidity in diabetic kidney disease trial. Am J Nephrol. 2019;50:1–12.
Bakris GL, Agarwal R, Anker SD, Pitt B, Ruilope LM, Rossing P, Kolkhof P, Nowack C, Schloemer P, Joseph A, et al. Effect of finerenone on chronic kidney disease outcomes in type 2 diabetes. N Engl J Med. 2020;383(23):2219–29.
Pitt B, Filippatos G, Agarwal R, Anker SD, Bakris GL, Rossing P, Joseph A, Kolkhof P, Nowack C, Schloemer P, et al. Cardiovascular events with finerenone in kidney disease and type 2 diabetes. N Engl J Med. 2021;385(24):2252–63.
Agarwal R, Filippatos G, Pitt B, Anker SD, Rossing P, Joseph A, Kolkhof P, Nowack C, Gebel M, Ruilope LM, et al. Cardiovascular and kidney outcomes with finerenone in patients with type 2 diabetes and chronic kidney disease: the FIDELITY pooled analysis. Eur Heart J. 2021;00:1–12.
Bramlage P, Lanzinger S, van Mark G, Hess E, Fahrner S, Heyer CHJ, Friebe M, Seufert J, Danne T, Holl RW. Patient and disease characteristics of type-2 diabetes patients with or without chronic kidney disease: an analysis of the German DPV and DIVE databases. Cardiovasc Diabetol. 2019;18(1):33.
Bramlage P, Lanzinger S, Tittel SR, Hess E, Fahrner S, Heyer CHJ, Friebe M, Buschmann I, Danne T, Seufert J, et al. Guidelines adherence in the prevention and management of chronic kidney disease in patients with diabetes mellitus on the background of recent European recommendations—a registry-based analysis. BMC Nephrol. 2021;22(1):184.
Diabetes-Patienten-Verlaufsdokumentation (DPV) [http://buster.zibmt.uni-ulm.de/dpv/index.php/en/].
Schwab KO, Doerfer J, Hungele A, Scheuing N, Krebs A, Dost A, Rohrer TR, Hofer S, Holl RW. Non-high-density lipoprotein cholesterol in children with diabetes: proposed treatment recommendations based on glycemic control, body mass index, age, sex, and generally accepted cut points. J Pediatr. 2015;167(6):1436–9.
Bohn B, Schofl C, Zimmer V, Hummel M, Heise N, Siegel E, Karges W, Riedl M, Holl RW, initiative DPV. Achievement of treatment goals for secondary prevention of myocardial infarction or stroke in 29,325 patients with type 2 diabetes: a German/Austrian DPV-multicenter analysis. Cardiovasc Diabetol. 2016;15(1):72.
Danne T, Kaltheuner M, Koch A, Ernst S, Rathmann W, Russmann HJ, Bramlage P, Studiengruppe D. “DIabetes Versorgungs-evaluation” (DIVE)–a national quality assurance initiative at physicians providing care for patients with diabetes. Dtsch Med Wochenschr. 2013;138(18):934–9.
Levey AS, de Jong PE, Coresh J, El Nahas M, Astor BC, Matsushita K, Gansevoort RT, Kasiske BL, Eckardt KU. The definition, classification, and prognosis of chronic kidney disease: a KDIGO controversies conference report. Kidney Int. 2011;80(1):17–28.
KDIGO 2012. Clinical practice guideline for the evaluation and management of chronic kidney disease: chapter 1: definition and classification of CKD. Kidney Int Suppl. 2013;3:19–62.
Schwandt A, Denkinger M, Fasching P, Pfeifer M, Wagner C, Weiland J, Zeyfang A, Holl RW. Comparison of MDRD, CKD-EPI, and Cockcroft-Gault equation in relation to measured glomerular filtration rate among a large cohort with diabetes. J Diabetes Complicat. 2017;31(9):1376–83.
group Sw, collaboration ESCCr. SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J. 2021;42(25):2439–54.
Taal MW, Brenner BM. Predicting initiation and progression of chronic kidney disease: developing renal risk scores. Kidney Int. 2006;70(10):1694–705.
Martin K, Begaud B, Latry P, Miremont-Salame G, Fourrier A, Moore N. Differences between clinical trials and postmarketing use. Br J Clin Pharmacol. 2004;57(1):86–92.
Bourgeois FT, Orenstein L, Ballakur S, Mandl KD, Ioannidis JPA. Exclusion of elderly people from randomized clinical trials of drugs for ischemic heart disease. J Am Geriatr Soc. 2017;65(11):2354–61.
Cruz-Jentoft AJ, Carpena-Ruiz M, Montero-Errasquin B, Sanchez-Castellano C, Sanchez-Garcia E. Exclusion of older adults from ongoing clinical trials about type 2 diabetes mellitus. J Am Geriatr Soc. 2013;61(5):734–8.
Li YT, Wang Y, Hu XJ, Chen JH, Li YY, Zhong QY, Cheng H, Mohammed BH, Liang XL, Hernandez J, et al. Association between systolic blood pressure and diabetic retinopathy in both hypertensive and normotensive patients with type 2 diabetes: risk factors and healthcare implications. Healthcar. 2021;9(5):580.
Shah KS, Xu H, Matsouaka RA, Bhatt DL, Heidenreich PA, Hernandez AF, Devore AD, Yancy CW, Fonarow GC. Heart failure with preserved, borderline, and reduced ejection fraction: 5-year outcomes. J Am Coll Cardiol. 2017;70(20):2476–86.
Lenfant C. Shattuck lecture–clinical research to clinical practice–lost in translation? N Engl J Med. 2003;349(9):868–74.
Stevens PE, Levin A, Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group M. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158(11):825–30.
Ninomiya T, Perkovic V, de Galan BE, Zoungas S, Pillai A, Jardine M, Patel A, Cass A, Neal B, Poulter N, et al. Albuminuria and kidney function independently predict cardiovascular and renal outcomes in diabetes. J Am Soc Nephrol. 2009;20(8):1813–21.
Chiu N, Aggarwal R, Bakris GL, Pitt B, Bhatt DL. Generalizability of FIGARO-DKD and FIDELIO-DKD trial criteria to the US population eligible for finerenone. J Am Heart Assoc. 2022;11(7):e025079.
Santoro D, Torreggiani M, Pellicano V, Cernaro V, Messina RM, Longhitano E, Siligato R, Gembillo G, Esposito C, Piccoli GB. Kidney biopsy in type 2 diabetic patients: critical reflections on present indications and diagnostic alternatives. Int J Mol Sci. 2021;22(11):5425.
Mogensen CE, Christensen CK, Vittinghus E. The stages in diabetic renal disease. With emphasis on the stage of incipient diabetic nephropathy. Diabetes. 1983;32(Suppl 2):64–78.
Pugliese G, Penno G, Natali A, Barutta F, Di Paolo S, Reboldi G, Gesualdo L, De Nicola L, Italian Diabetes S, the Italian Society of N. Diabetic kidney disease: new clinical and therapeutic issues. Joint position statement of the Italian diabetes society and the Italian Society of Nephrology on “The natural history of diabetic kidney disease and treatment of hyperglycemia in patients with type 2 diabetes and impaired renal function.” J Nephrol. 2020;33(1):9–35.
Jardine MJ, Mahaffey KW, Neal B, Agarwal R, Bakris GL, Brenner BM, Bull S, Cannon CP, Charytan DM, de Zeeuw D, et al. The canagliflozin and renal endpoints in diabetes with established nephropathy clinical evaluation (CREDENCE) study rationale, design, and baseline characteristics. Am J Nephrol. 2017;46(6):462–72.
Wheeler DC, Stefansson BV, Batiushin M, Bilchenko O, Cherney DZI, Chertow GM, Douthat W, Dwyer JP, Escudero E, Pecoits-Filho R, et al. The dapagliflozin and prevention of adverse outcomes in chronic kidney disease (DAPA-CKD) trial: baseline characteristics. Nephrol Dial Transplant. 2020;35(10):1700–11.
Group E-KC. Design, recruitment, and baseline characteristics of the EMPA-KIDNEY trial. Nephrol Dial Transplant. 2022;37:1317.
Shirazian S, Grant CD, Mujeeb S, Sharif S, Kumari P, Bhagat M, Mattana J. Underprescription of renin-angiotensin system blockers in moderate to severe chronic kidney disease. Am J Med Sci. 2015;349(6):510–5.
Sonawane KB, Qian J, Hansen RA. Utilization patterns of antihypertensive drugs among the chronic kidney disease population in the United States: a cross-sectional analysis of the national health and nutrition examination survey. Clin Ther. 2015;37(1):188–96.
O’Hare AM. The management of older adults with a low eGFR: moving toward an individualized approach. Am J Kidney Dis. 2009;53(6):925–7.
Lam D, Shaikh A. Real-life prescribing of sglt2 inhibitors: how to handle the other medications including glucose-lowering drugs and diuretics. Kidney 360. 2021;2(4):742–6.
Acknowledgements
We thank all participating centers of the DPV and DIVE initiatives. In addition, we thank Ramona Ranz and Andreas Hungele for data management and development of the DPV documentation software (both clinical data managers, Ulm University).
Funding
The DPV registry was supported by the German Diabetes Society (DDG) and the German Centre for Diabetes Research (DZD, grant number 82DZD14E03). The DIVE registry received funding from Abbott, AstraZeneca, Bayer Vital, Boehringer, and Sanofi. Funders were not involved in the analysis and interpretation of data, the writing of the report or the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
SM, KM, AG, RV, TO, and TD contributed to the data collection. PB and SL designed the analysis, drafted the manuscript and created figures. SL was responsible for the statistical analyses. SM, KM, AG, RV, TO, and TD and RWH contributed to the discussion and reviewed/edited the manuscript. SL had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. RWH coordinates the DPV initiative. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The DPV initiative, which was established in 1995, was approved by the ethics committee of the University of Ulm, and data collection was approved by local review boards. The DIVE registry was established in Germany in 2011. The protocol was approved by the ethics committee of the Medical School of Hannover, and all patients included in the DIVE registry provided written informed consent.
Consent for publication
Not applicable.
Competing interests
JS and TD report Grants and personal fees from Abbott, AstraZeneca, and Sanofi, outside the submitted work. PB reports to have received research support from the funders of DIVE. SL, SM, KM, AG, RV, TO and RWH have no competing interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1
. Cardiovascular and renal risk [28]. Table S2. Determinants of cardiovascular risk [31]. Table S3. Renal disease—perpetuating factors* [32].
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bramlage, P., Lanzinger, S., Mühldorfer, S. et al. An analysis of DPV and DIVE registry patients with chronic kidney disease according to the finerenone phase III clinical trial selection criteria. Cardiovasc Diabetol 22, 108 (2023). https://doi.org/10.1186/s12933-023-01840-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-023-01840-5