Abstract
Background
To analyze whether medical care is in accordance with guidelines for secondary prevention of myocardial infarction (MI), or stroke in patients with type 2 diabetes from Germany and Austria.
Methods
29,325 patients (≥20 years of age) with type 2 diabetes and MI, or stroke, documented between 2006 and 2015 were selected from the Diabetes-Patienten-Verlaufsdokumentation database. We analyzed medication, clinical characteristics, and lifestyle factors according to national secondary prevention guidelines in patients with MI, or stroke, separately.
Results
HbA1C <7.5 % was achieved in 64.9 % (MI), and in 61.1 % (stroke) of patients. LDL <100 mg/dl was documented in 56.2 % (MI), and in 42.2 % (stroke). Non-smoking was reported in 92.0 % (MI), and in 93.1 % (stroke), physical activity in 9.6 % (MI), and 5.5 % (stroke). Target values of blood pressure (<130/80 mmHg in MI, 120/70–140/90 in stroke) were reached in 67.0 % (MI), and in 89.9 % (stroke). Prescription prevalence of inhibitors of platelet aggregation (IPA) was 50.7 % (MI), and 31.7 % (stroke). 57.0 % (MI), and 40.1 % (stroke) used statins, 65.1 % (MI), and 65.8 % (stroke) used any type of antihypertensives, and ACE inhibitors were prescribed in 49.7 % (MI), and 41.3 % (stroke). A body mass index (BMI) <27 kg/m2 and the use of beta blockers were only recommended in subjects with MI. Of the patients with MI, 32.0 % had a BMI <27 kg/m2, and 59.5 % used beta blockers.
Conclusions
Achievement of treatment goals in secondary prevention of MI, or stroke in subjects with type 2 diabetes needs improvement. Target goals were met more frequently in patients with MI compared to subjects with stroke. Especially the use of IPA was very low in patients with stroke. There remains great potential to reduce the risk of repeated macrovascular events and premature death, as well as to increase patients’ quality of life.
Similar content being viewed by others
Background
The prevalence of type 2 diabetes is increasing worldwide [1–3]. Moreover, studies indicate an earlier onset of type 2 diabetes and a longer life-expectancy with diabetes [2, 4]. A prolonged exposure to an adverse diabetic milieu and a high prevalence of cardiovascular risk factors (as obesity, hypertension, or dyslipidemia) [5], contribute to a high risk for macrovascular complications (MVCs) as myocardial infarction (MI), or stroke. In patients with diabetes, cardiovascular disease (CVD) is two to eight folds higher compared to the general population and is the leading cause of death [6–8]. Additionally, disease progression in patients with type 2 diabetes seems to be more severe with a worse long-term prognosis compared to subjects without diabetes [5, 9]. MVCs have an adverse effect on patients’ quality of life and are also a huge public health problem due to high economic costs [10–12].
German and international guidelines (from e.g. the American Heart Association) for secondary prevention of MI and stroke aim to reduce cardiovascular morbidity and mortality and to improve patient’s quality of life [8, 13–15]. These guidelines address pharmacological and lifestyle interventions, and provide target values amongst others for serum glucose, blood pressure, or serum lipids [8, 13–15]. However, data of previous studies indicate a suboptimal implementation of guidelines in medical care [16–21]. Although there are studies analyzing primary prevention of CVD risk factors in patients with diabetes [21–25], or adherence to secondary prevention guidelines in the general population [26–29] no studies exist investigating the achievement of current guideline targets for secondary prevention of MVCs in subjects with type 2 diabetes.
Our objective was to examine whether medical care in patients with type 2 diabetes who already experienced a MI or stroke meets current guideline recommendations for secondary prevention. We also analyzed sociodemographic and clinical differences between patients with and without MVCs.
Methods
Data source and subjects
Data were provided by the German/Austrian DPV (Diabetes-Patienten-Verlaufsdokumentation) registry. The DPV software is used for standardized, prospective documentation of diabetes care and outcome and is currently used by 428 centers from Germany (n = 398) and Austria (n = 30). Twice a year, data are anonymized and transmitted from the participating health care facilities to Ulm, Germany, and aggregated into a cumulative database for clinical research and quality assurance [16]. Implausible and inconsistent data are reported back to the centers for verification or correction. The DPV initiative is approved by the Ethics Committee of the University of Ulm, Germany and data collection by the local review boards.
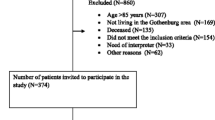
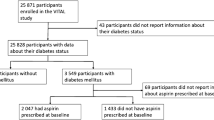
As of March 2015, 404,609 patients were registered in DPV. Adult patients (≥20 years of age) with type 2 diabetes documented during the year 2006 or thereafter were included; leaving 221,943 subjects from 178 participating centers (Fig. 1). If a macrovascular complication (stroke, or MI) was documented in the DPV software by the physician, the patient was assigned to the respective patient group (“MI only”, “stroke only”, “MI and stroke”). The diabetic foot syndrome (DFS) is a result of macrovascular and polyneuropathic complications. Additionally, guidelines for DFS contain recommendations primarily for wound management [30]. Hence, patients with DFS were excluded from the present analysis (n = 19,784; Fig. 1).
Due to heterogeneity on medical possibilities, and available drugs, data before the year 2006 were excluded. The recommendations considered did not differ between the year 2006 and 2015. For each patient, the last year of treatment was analyzed.
Outcomes
Sociodemographic characteristics (as e.g. sex, age, and age at diagnosis), clinical data (HbA1C, BMI, serum lipids, systolic and diastolic blood pressure), and lifestyle factors (smoking, physical activity) were compared between patients with at least one MVC (MI, stroke, or both) or patients without MVCs.
We considered variables according to national guidelines. In patients with MI, we analyzed HbA1C (<7.5 %), blood pressure (<130/80 mmHg), LDL-cholesterol (<100 mg/dl), body mass index (BMI) (<27 kg/m2), medical treatment (inhibitors of platelet aggregation (IPA), statins, beta blockers, ACE inhibitors, and any type of antihypertensives), smoking (yes/no), and physical activity (yes/no) [13].
In patients with stroke, we analyzed HbA1C (<7.5 %), blood pressure (systolic 120–<140 mmHg/diastolic 70–<90 mmHg), LDL-cholesterol (<100 mg/dl), medical treatment (IPA, statins, ACE inhibitors, and any type of antihypertensives), smoking (yes/no), and physical activity (yes/no) [14, 15].
HbA1C was mathematically standardized to the reference range of 20–42 mmol/mol (diabetes control and complication trial: 4.05–6.05 %) by applying the multiple-of-the-mean transformation method [31]. Systolic and diastolic blood pressure as well as serum lipids were measured in local laboratories compliant with national guidelines [32]. Information on smoking behavior and physical activity in supervised sports groups were based on patient self-reports to their diabetes-care teams.
Statistical analysis
Sociodemographic characteristics and clinical data were presented as median (Q1;Q3), or as percentage. To compare groups, Chi square (χ2) test was used for dichotomous variables, and Kruskal–Wallis test for continuous variables. The false discovery rate (FDR) was applied to correct p-values for multiple comparisons [33]. To analyze potential gender-differences in drug use, clinical characteristics, and recommended lifestyle, logistic regression models were applied in “MI only” and “stroke only” groups. Due to differences in age distribution among men and women, data were adjusted for age-groups (20–<65, 65–<75, >75 years of age).
Due to the large number of subjects studied, a two-sided p value <0.01 was considered significant. All statistical analyses were implemented with SAS 9.4 (Statistical Analysis Software, SAS Institute, Cary, NC, USA).
Results
Differences between patients with or without MVCs
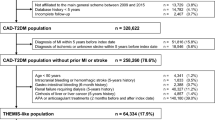
We included a total of 202,159 type 2 diabetes subjects (male: 51.4 %) with a median age of 70.6 (Q1;Q3: 60.6;77.9) years and a median diabetes duration of 8.1 (2.7;14.1) years. Of the patients included, 29,325 had at least one MVC. In subjects with MVCs, there was a male preponderance (57.6 vs. 50.3 %; p < 0.0001), their median age was higher (73.6 vs. 69.9 years; p < 0.0001) and the diabetes duration was longer (9.8 vs. 7.8 years; p < 0.0001) compared to patients without MVCs (Table 1). Total cholesterol as well as LDL-cholesterol were higher in patients without MVCs (both p < 0.0001). Differences between patient groups are described in detail in Table 1.
Differences within patients with MVCs
We also analyzed differences in sociodemographic and clinical characteristics between type 2 diabetes patients with MI only (n = 15,015), stroke only (n = 11,738), or both MVCs (MI and stroke) (n = 2572) (Table 2). The lowest percentage of women was present in patients with MI only (37.0 %), and the highest in patients with stroke only (49.9 %). Age at diabetes diagnosis was earlier in patients with MI (60.9 years) compared to the other groups (e.g. 63.9 years in patients with stroke). Diabetes duration was longest in patients with both MVCs (11.0 years) (Table 2). Diastolic and systolic blood pressure were higher in patients with stroke (135/80 mmHg) compared to patients with MI (130/74 mmHg) or both MVCs (130/75 mmHg). Total- and LDL-cholesterol were highest in patients with stroke. A comprehensive description of patient characteristics can be found in Table 2.
Achievement of target goals and medication in patients with type 2 diabetes and MI
Approximately two-thirds of the patients with type 2 diabetes and MI achieved target values of HbA1C (64.9 %) and blood pressure (67.0 %) (Fig. 2a). More than half of the patients (56.2 %) reached target value of LDL-cholesterol. Guidelines also recommend weight loss in subjects with a BMI over 27 kg/m2. In our patients with MI, only one-third (32.2 %) had a BMI of less than 27 kg/m2. Physical activity was self-reported by 9.6 % and non-smoking by 92.0 % of the patients (Fig. 2a). Use of different pharmaceutical agent classes as per recommendation was documented in 50 % (use of IPA) to 65 % (use of any type of antihypertensives) of patients (Fig. 2b). Of those patients treated with antihypertensives (n = 9773), 66.6 % reached target values of blood pressure. In subjects treated with statins (n = 8556), 62.8 % achieved LDL <100 mg/dl.
Achievement of target goals and medication in patients with type 2 diabetes and stroke
In most patients with stroke (89.9 %), target values of blood pressure were reached. Less than two-thirds had an HbA1C of <7.5 % (Fig. 3a). LDL-cholesterol under 100 mg/dl was only documented in 42.2 %. 5.5 % of the patients reported to be physically active, 93.1 % were documented as non-smokers (Fig. 3a). About two-thirds of the patients were treated with any type of antihypertensive drugs, whereas the use of IPA, statins or ACE inhibitors was only documented in 30 % to 40 % of the subjects with stroke (Fig. 3b). In patients treated with antihypertensives (n = 7726), 89.3 % met a blood pressure between 120/70 and 140/90 mmHg. 49.8 % of statin-treated patients (n = 4710) reached target value of LDL <100 mg/dl.
Gender differences in the attainment of guideline recommendations
Logistic regression analysis revealed a slightly, but significantly better achievement of recommended treatment goals in men compared to women (Table 3). The biggest difference was observed in LDL-cholesterol. In subjects with MI, 60.1 % of men and 49.2 % of women reached the target value of <100 mg/dl (p < 0.0001). In patients with stroke, 46.1 % of men and 38.3 % of women met the goal. Only the proportion of non-smokers was higher in women compared to men (MI: 94.0 vs. 92.0 %; stroke: 95.3 vs. 92.4 %; both p < 0.0001). Table 3 summarizes all gender-differences.
Discussion
Our aim was to analyze the adherence to guidelines for secondary prevention of MI or stroke in patients with type 2 diabetes who already experienced a MI, or stroke. Overall, concordance with recommendations is rather mixed. Achievement of target values was best for glycaemic control and blood pressure. Almost all patients reported to be a non-smoker. Hardly anyone was physically active in supervised sport groups. Even use of medication according to guidelines was quite poor, except for the use of antihypertensives. Treatment goals were met more often in subjects with MI compared to subjects with stroke. Particularly the use of IPA was very low in patients with stroke. We further investigated sociodemographic and clinical characteristics in patients with and without MVCs.
Differences between patients with or without MVCs
Our analysis revealed lower rates of CVD risk factors in patients with MVCs (Table 1). Especially blood lipids and diastolic blood pressure were lower in patients with MI, or stroke. One explanation for the differences found is that in our analysis, patients with MVCs more frequently receive lipid-lowering drugs (45.1 vs. 23.8 %) or antihypertensives (65.8 vs. 48.7 %) compared to subjects without MVCs. It can be also assumed that patients with a history of at least one MVC are more concerned about their health. Furthermore it is possible that medical care is more intensive in subjects with MVCs and physicians might be more focused on CVD risk factors. This assumption can be supported by results of the German DETECT study, indicating that prescription rates of guideline recommended medication in subjects with CVD correlate with the number of comorbidities [28].
Meeting target goals in patients with MI or stroke
The best achievement was present for blood pressure. In patients with MI, about two-thirds had a blood pressure below 130/80 mmHg (Fig. 2a). In patients with stroke, over 90 % reached recommended values (Fig. 3a). Differences in achievement may be explained by higher target values for stroke patients (70–90 mmHg for diastolic; 120–140 mmHg for systolic blood pressure). In German type 2 diabetes guidelines, target value for blood pressure is 140/80 mmHg [34]. This objective was achieved in 68.6 % of our study population without MVCs.
Studies investigating secondary prevention of MI or stroke in patients with type 2 diabetes are lacking. However, there are studies analyzing the prevalence of CVD risk factors in patients with diabetes, irrespective of previous MVC events [22, 24, 25]. Compared to results of the ESTHER-study, a German cohort study from Saarland (population-based data on primary care; patients with diabetes, n = 1375), achievement of recommended blood pressure targets in the DPV study population is high. In the ESTHER-study, only 8.7 % reached a blood pressure below 130/80 mmHg [24]. Findings from the German DIAB-CORE project (pooled data from six population-based studies; patients with type 2 diabetes, n = 1287), reported in 36.4 % of the subjects a blood pressure below 140/90 mmHg [25]. In an analysis of the National Health and Nutrition Examination Survey (NHANES) from the USA, in the years 2007–2010 (n = 1376), blood pressure of <130/80 mmHg was achieved in 51.1 % of the patients, and values <140/90 mmHg in 72.0 % [22]. Results of the EUROASPIRE IV (European Action on Secondary and Primary Prevention by Intervention to Reduce Events) study, including patients of 24 European countries, reported in 32 % of the patients with newly diagnosed diabetes and in 26 % of the patients with known diabetes a blood pressure <130/80 mmHg [35].
In guidelines for secondary prevention of MI/stroke, normoglycemia is recommended without a specific cut off value [13–15]. According to general national type 2 diabetes guidelines, HbA1C should be between 6.5 and 7.5 % depending on patients’ needs and preferences [34]. We therefore set a threshold of <7.5 %. An HbA1c <7.5 % was documented in approximately two-thirds of the patients with stroke (61.6 %), or MI (64.9 %). This is comparable to subjects without MVCs (60.1 %). A recently published study from Wales analyzed changes in HbA1C levels in patients with diabetes before and 1 year after stroke [36]. The authors reported a significant improvement in HbA1C levels from 7.7 to 7.3 %. They also compared the achievement of HbA1C levels ≤7.5 % in diabetes patients with and without stroke. One year after the incident stroke, an HbA1C ≤7.5 % was documented in 62.5 % of patients who experienced stroke and in 65.3 % of the controls [36]. Our findings are also in line with results of the NHANES study. These authors reported an HbA1C of <7.0 % in 52.5 % of the patients, and an HbA1C of <8.0 % in 77.9 % [22].
In our study population, achievement of LDL targets was worst. Values below 100 mg/dl were present in only 42.2 % of the patients with stroke (Fig. 3a), and in 56.2 % of the patients with MI (Fig. 2a). LDL <100 mg/dl is also recommended in type 2 diabetes without MVCs [34]. Even in these subjects, only 38.8 % met the goal. Hence, high values of LDL might be an overall problem in type 2 diabetes. However, in a direct comparison with other studies from Germany, clinical characteristics of DPV-patients are better. For example in the ESTHER-study, only in 13.3 % of the patients, LDL <100 mg/dl was reported [24]. In the DIAB-CORE study, only information on the mean LDL was available. The mean LDL-value of 137 mg/dl is much higher compared to our study population (105 mg/dl in patients with MVCs, 115 mg/dl in patients without MVCs) [25]. In the US, 56.2 % achieved LDL <100 mg/dl [22]. The EUROASPIRE IV study indicated in 56 % of the patients with newly diagnosed diabetes and in 66 % with known diabetes LDL values <97 mg/dl [35]. Overall, patients included in the current DPV study seem to have better control of CVD risk compared to subjects of other German cohorts [24, 25, 37]. Patients in DPV are mainly treated in specialized diabetes centers, whereas participants of the ESTHER study or the DIAB-CORE project are predominantly treated by general practitioners [24, 25]. This could be one explanation for better treatment. Additionally, benchmarking with other centers participating in the DPV initiative might further encourage the diabetes team to improve clinical care in their patients [38].
Lifestyle factors
In the DPV database, the documentation of smoking was missing in 19.8 % (n = 2966) with MI, and in 21.7 % (n = 2549) with stroke. Most patients (>90 %) reported to be a non-smoker. This roughly correspondents to the prevalence in the general population. According to the German census, smoking prevalence ranges from 22.0 % in the 60 to <65 year olds to 5.2 % in subjects over 75 years of age [39]. The low smoking prevalence reported in diabetes subjects should be assessed positively, however, under-reporting cannot be completely excluded.
Physical activity is also recommended in the secondary prevention of MI and stroke. In the present analysis, 5 to 10 % of patients with MI or stroke reported to be physically active (Figs. 2a, 3a). In the ESTHER-study, physical activity was reported in 43.6 % [24]. However, in DPV, only physical activity in guided sport-groups is documented by the diabetes team. This could be one explanation for the lower percentage. Physical activity in guided sport-groups is important directly after the first episode after MI/stroke. Since we analyze the last treatment year of the patients, it is possible, that the MI/stroke already dates back several years. Hence, guided sport-groups are no longer required and it is possible that patients exercise privately. Furthermore, physical immobility due to stroke could be a limiting factor in physical activity. Moreover, in the DPV database, information on physical activity is available in only 34.7 % (MI) and 41.5 % (stroke) of patients.
Recommendations on BMI are present only in guidelines for MI. According to national guidelines [13], body weight should be reduced if the BMI is over 27 kg/m2. In our analysis, 32.2 % had a BMI <27 kg/m2. In patients without MVCs, the proportion is slightly lower (29.9 %). A study from Sweden demonstrated the importance of successful weight management in newly diagnosed patients with type 2 diabetes [40]. The authors stated that overweight and obese subjects had a substantially increased risk of incident atrial fibrillation compared to normal weight subjects. Even modest weight gain during the first 1.5 years after diabetes diagnosis seemed to be associated with increased atrial fibrillation risk [40].
Medication
Except for antihypertensive drugs (MI: 65.1 %; stroke: 65.8 %), concordance with recommendations is very low in our study population (Figs. 2b, 3b). Treatment goals are met more frequently in patients with MI compared to subjects with stroke. The use of IPA (31.7 %) is especially low in patients with stroke. As already mentioned, we analyzed the last year of treatment. It is therefore possible that recommendations were observed initially, but treatment was discontinued over time. In a large analysis of a German sickness fund (n = 30.028), initial prescription prevalence after myocardial infarction and treatment after 5 years were evaluated [29]. Initial prescription was higher compared to our analysis. Beta blockers were prescribed in 82 % of the patients, statins in 73 %, and ACE inhibitors in 69 % [29]. However, 5 years after a MI, only few of the subjects were still treated according to recommendations with 36 % of the patients prescribed beta-blockers, 31 % ACE inhibitors, and in 17 % statins [29]. A very large study with over half a million subjects from the UK Biobank highlighted that medication was in many people not according to secondary prevention recommendations [26]. A study from the USA analyzed treatment in 364 subjects who survived coronary heart disease [41]. Best adherence to recommendations was present for lipid lowering drugs (60 %), followed by beta blockers (58 %) and ACE inhibitors (38 %) [41]. Other European countries, such as the Netherlands [27], and Denmark [42] have reported a low proportion of subjects meeting guideline-defined treatment goals. To improve secondary prevention of CVD, the introduction of the “polypill” (fixed-dose combination pill) is discussed [43]. The polypill concept was recently implemented in a number of European countries and in the USA [43].
Subgroup analysis
In almost all cases, treatment goals were met more often in men compared to women (Table 3). Some studies confirm our findings [28, 44, 45], while others do not [23, 24, 46]. For example, the analysis of Xin Song and colleagues indicated in all categories of anthropometric measures of obesity a higher CVD mortality in men compared to women [46]. A suboptimal achievement of target values was also present in those patients treated with antihypertensives or statins—except of blood pressure in patients with stroke. Only half of the statin-treated subjects with MI (49.8 %) and less than two-thirds with stroke (62.8 %) achieved LDL <100 mg/dl. In patients with MI treated with antihypertensives, only about two-thirds (66.6 %) achieved recommended blood pressure values of <130/80 mmHg. This gives rise to the assumption that medication is underdosed in clinical practice. Underdose in CVD medication was confirmed by other studies [47, 48]. Steinberg et al. stated that less than half of the subjects with acute coronary heart syndrome reached target values of LDL <100 mg/dl and that the recorded statin doses were lower than those with an evidence-based effect [48]. This was also reported by a study from the Euro Heart Survey on Diabetes and the heart [47]. The authors indicated that neither dosage of antihypertensive drugs nor dosages of statins were increased despite blood pressure and serum lipids exceeding recommended targets [47]. Although there are many studies indicating an improvement in survival and quality of life in patients who received medical treatment according to guidelines [21, 49, 50], a significant discrepancy between recommendations and actual care is present. There are many potential reasons for this gap. Aside from a lack of knowledge of current guidelines, physician inexperience, lack of physician time, or patients’ non-adherence, clinical reasons such as comorbidities or adverse effects of medications might also be present [18, 21, 51]. Furthermore, external constraints for example the type of health insurance (private vs. statutory health insurances), access to medical care (including distance to the medical practice, or availability of specialists), or financial aspects may also be implicated [18, 21, 51]. Another reason could be a lack of resources available to implement secondary prevention measures [21].
Strengths and limitations
The main strength of the current observational study is its large number of patients. Since we solely consider subjects from centers participating in the DPV initiative, a selection bias cannot be completely excluded and the generalizability of our results might be therefore limited. Another shortcoming is that we could only assess the proportion of patients meeting treatment goals and not the reasons for non-adherence. A further limitation is that clinical characteristics and medical treatment were not completely documented in all patients with MI, or stroke. However, up to now, there seems to be no comparable study investigating adherence to current secondary prevention guidelines of MI, or stroke in the high-risk group of type 2 diabetes subjects. Despite these limitations, analyses as the present one are urgently needed to reveal weaknesses in medical care providing an evidence basis for improvement.
Conclusion
This cross-sectional study indicates that medication and lifestyle changes for secondary prevention in subjects with type 2 diabetes who already experienced MI, or stroke are not in line with guideline recommendations. Overall, patients with stroke less frequently met treatment goals compared to subjects with MI. Especially the use of IPA was low. This analysis also confirms the need to improve secondary prevention of CVD risk factors. Aside from greater efforts by physicians to implement current guidelines, new strategies need to be developed to further increase patient motivation and compliance to hopefully result in sustainable behavior changes, including increased physical activity and healthy food choices.
Abbreviations
- BMI:
-
body mass index
- CVD:
-
cardiovascular disease
- DPV:
-
diabetes patienten verlaufsdokumentation
- DSF:
-
diabetic foot syndrome
- EUROASPIRE:
-
European Action on Secondary and Primary Prevention by Intervention to Reduce Events
- FDR:
-
false discovery rate
- IPA:
-
inhibitors of platelet aggregation
- MI:
-
myocardial infarction
- MVC:
-
macrovascular complication
- NHANES:
-
National Health and Nutrition Examination Survey
References
Danaei G, Finucane MM, Lu Y, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378:31–40.
Chen L, Magliano DJ, Zimmet PZ. The worldwide epidemiology of type 2 diabetes mellitus–present and future perspectives. Nat Rev Endocrinol. 2012;8:228–36.
Heidemann C, Du Y, Schubert I, Rathmann W, Scheidt-Nave C. Prevalence and temporal trend of known diabetes mellitus: results of the German Health Interview and Examination Survey for Adults (DEGS1). Bundesgesundhbl Gesundheitsforsch Gesundheitsschutz. 2013;56:668–77.
Constantino MI, Molyneaux L, Limacher-Gisler F, et al. Long-term complications and mortality in young-onset diabetes: type 2 diabetes is more hazardous and lethal than type 1 diabetes. Diab Care. 2013;36:3863–9.
Kalofoutis C, Piperi C, Kalofoutis A, Harris F, Phoenix D, Singh J. Type II diabetes mellitus and cardiovascular risk factors: current therapeutic approaches. Exp Clin Cardiol. 2007;12:17–28.
Buyken AE, von Eckardstein A, Schulte H, Cullen P, Assmann G. Type 2 diabetes mellitus and risk of coronary heart disease: results of the 10-year follow-up of the PROCAM study. Eur J Cardiovasc Prev Rehabil. 2007;14:230–6.
International Diabetes Federation (IDF). IDF DIABETES ATLAS: 7th ed. 2015. https://www.idf.org/diabetesatlas. Accessed 19 April 2016.
American Diabetes Association (ADA). 8. Cardiovascular disease and risk management. Diab Care. 2016;39(Suppl 1):S60–71.
Mukamal KJ, Nesto RW, Cohen MC, et al. Impact of diabetes on long-term survival after acute myocardial infarction: comparability of risk with prior myocardial infarction. Diab Care. 2001;24:1422–7.
Pscherer S, Dippel FW, Lauterbach S, Kostev K. Amputation rate and risk factors in type 2 patients with diabetic foot syndrome under real-life conditions in Germany. Prim Care Diab. 2012;6:241–6.
de Visser CL, Bilo HJG, Groenier KH, de Visser W, de Jong Meyboom B. The influence of cardiovascular disease on quality of life in type 2 diabetics. Qual Life Res. 2002;11:249–61.
Nichols GA, Brown JB. The impact of cardiovascular disease on medical care costs in subjects with and without type 2 diabetes. Diab Care. 2002;25:482–6.
Bundesärztekammer (BÄK), Kassenärztliche Bundesvereinigung (KBV), Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF). Nationale VersorgungsLeitlinie Chronische KHK—Langfassung. 3rd ed. 2014. Accessed 19 April 2016.
Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin (DEGAM). Schlaganfall. DEGAM-Leitlinie Nr. 8. 2012. http://www.degam.de/degam-leitlinien-379.html Accessed 19 April 2016.
Deutsche Schlaganfall-Gesellschaft (DSG), Deutsche Gesellschaft für Neurologie (DGN). Sekundärprophylaxe ischämischer Schlaganfall und transitorische ischämische Attacke (Teil 1). 2015. http://www.dgn.org/leitlinien/11-leitlinien-der-dgn/3024-ll-23-ll-sekundaerprophylaxe-ischaemischer-schlaganfall-und-transitorische-ischaemische-attacke. Accessed 19 April 2016.
Scheuing N, Berger G, Bergis D, et al. Adherence to clinical care guidelines for cystic fibrosis-related diabetes in 659 German/Austrian patients. J Cyst Fibros. 2014;13:730–6.
Steel N, Bachmann M, Maisey S. Self reported receipt of care consistent with 32 quality indicators: national population survey of adults aged 50 or more in England. BMJ. 2008;337:a957.
Karbach U, Schubert I, Hagemeister J, Ernstmann N, Pfaff H, Höpp HW. Physicians’ knowledge of and compliance with guidelines: an exploratory study in cardiovascular diseases. Dtsch Arztebl Int. 2011;108:61–9.
Cleland JGF, Cohen-Solal A, Aguilar JC, et al. Management of heart failure in primary care (the improvement of Heart Failure Programme): an international survey. Lancet. 2002;360:1631–9.
Hagemeister J, Schneider CA, Barabas S, et al. Hypertension guidelines and their limitations–the impact of physicians’ compliance as evaluated by guideline awareness. J Hypertens. 2001;19:2079–86.
Organisation for Economic Cooperation and Development (OECD). Cardiovascular disease and diabetes: policies for better health and quality of care. OECD Health Policy Studies. Paris: OECD Publishing; 2015.
Casagrande SS, Fradkin JE, Saydah SH, Rust KF, Cowie CC. The prevalence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988–2010. Diab Care. 2013;36:2271–9.
Malik S, Lopez V, Chen R, Wu W, Wong ND. Undertreatment of cardiovascular risk factors among persons with diabetes in the United States. Diab Res Clin Pract. 2007;77:126–33.
Raum E, Lietzau S, Stegmaier C, Brenner H, Rothenbacher D. For the majority of patients with diabetes blood pressure and lipid management is not in line with recommendations. Results from a large population-based cohort in Germany. Pharmacoepidemiol Drug Saf. 2008;17:485–94.
Rückert IM, Schunk M, Holle R, et al. Blood pressure and lipid management fall far short in persons with type 2 diabetes: results from the DIAB-CORE Consortium including six German population-based studies. Cardiovasc Diabetol. 2012;11:50.
Hewitt J, Walters M, Padmanabhan S, Dawson J. Cohort profile of the UK Biobank: diagnosis and characteristics of cerebrovascular disease. BMJ Open. 2016;6:e009161.
van der Elst ME, Bouvy ML, de Blaey CJ, de Boer A. Preventive drug use in patients with a history of nonfatal myocardial infarction during 12-year follow-up in The Netherlands: a retrospective analysis. Clin Ther. 2005;27:1806–14.
Bischoff B, Silber S, Richartz BM, Pieper L, Klotsche J, Wittchen HU. Inadequate medical treatment of patients with coronary artery disease by primary care physicians in Germany. Clin Res Cardiol. 2006;95:405–12.
Mangiapane S, Busse R. Prescription prevalence and continuing medication use for secondary prevention after myocardial infarction: the reality of care revealed by claims data analysis. Dtsch Arztebl Int. 2011;108:856–62.
Bundesärztekammer (BÄK) Arbeitsgemeinschaft der Deutschen Ärztekammern, Kassenärztliche Bundesvereinigung (KBV), Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF). Nationale VersorgungsLeitlinie Typ-2-Diabetes. Präventions- und Behandlungsstrategien für Fußkomplikationen (Langfassung). 2nd ed. 2010. http://www.bundesaerztekammer.de/richtlinien/leitlinien/. Accessed 19 April 2016.
Rosenbauer J, Dost A, Karges B, et al. Improved metabolic control in children and adolescents with type 1 diabetes: a trend analysis using prospective multicenter data from Germany and Austria. Diab Care. 2011;35:80–6.
Bundesärztekammer (BÄK) Arbeitsgemeinschaft der Deutschen Ärztekammern. Richtlinie der Bundesärztekammer zur Qualitätssicherung laboratoriumsmedizinischer Untersuchungen (Rili-BÄK). Dtsch Arztebl. 2014;111:A1583–618.
Westfall PH, Tobias RD, Wolfinger RD. Multiple comparisons and multiple tests using SAS. 2nd ed. Cary: SAS Institute; 2011.
Bundesärztekammer (BÄK), Kassenärztliche Bundesvereinigung (KBV), Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF). Nationale VersorgungsLeitlinie Therapie des Typ-2-Diabetes—Langfassung, 1. Auflage. Version 3. 2013, zuletzt geändert: April 2014. 2013. http://www.versorgungsleitlinien.de/themen/diabetes2/dm2_therapie. Accessed 19 April 2016.
Gyberg V, de Bacquer D, de Backer G, et al. Patients with coronary artery disease and diabetes need improved management: a report from the EUROASPIRE IV survey: a registry from the EuroObservational Research Programme of the European Society of Cardiology. Cardiovasc Diabetol. 2015;14:133.
Robson R, Lacey AS, Luzio SD, et al. HbA1c measurement and relationship to incident stroke. Diab Med. 2016;33:459–62.
Geller JC, Cassens S, Brosz M, et al. Achievement of guideline-defined treatment goals in primary care: the German Coronary Risk Management (CoRiMa) study. Eur Heart J. 2007;28:3051–8.
Grabert M, Schweiggert F, Holl RW. A framework for diabetes documentation and quality management in Germany: 10 years of experience with DPV. Comput Methods Programs Biomed. 2002;69:115–21.
Gesundheitsberichterstattung des Bundes. Gesundheitsverhalten und -gefährdungen. Tabak/Rauchen. Rauchen, Rauchverhalten der Bevölkerung. 2015. http://www.gbe-bund.de/gbe10/trecherche.prc_them_rech2?tk=5800&tk2=6200&ut_string=%28Gesamtes_Unterthema%29&ber=1&tab=1&gra=1&def=1&link=1&son=1&anz_ber=11&anz_tab=13&anz_gra=6&anz_def=5&anz_link=2&anz_son=15&p_sprache=D&x=&p_news=&button=1&p_uid=gast&p_aid=54803767&cb_wk=dummy&p_th_id=6200&p_bread_fid=&p_fund_old=0&p_item_news=&next_tr=1&erg_art=TAB#TAB. Accessed 19 April 2016.
Grundvold I, Bodegard J, Nilsson PM, et al. Body weight and risk of atrial fibrillation in 7,169 patients with newly diagnosed type 2 diabetes; an observational study. Cardiovasc Diabetol. 2015;14:5.
Vulic D, Lee BT, Dede J, Lopez VA, Wong ND. Extent of control of cardiovascular risk factors and adherence to recommended therapies in US multiethnic adults with coronary heart disease: from a 2005–2006 national survey. Am J Cardiovasc Drugs. 2010;10:109–14.
Gasse C, Jacobsen J, Larsen AC, et al. Secondary medical prevention among Danish patients hospitalised with either peripheral arterial disease or myocardial infarction. Eur J Vasc Endovasc Surg. 2008;35:51–8.
Hedner T, Kjeldsen SE, Narkiewicz K, Oparil S. The polypill: an emerging treatment alternative for secondary prevention of cardiovascular disease. Blood Press. 2016:1–4.
Manteuffel M, Williams S, Chen W, Verbrugge RR, Pittman DG, Steinkellner A. Influence of patient sex and gender on medication use, adherence, and prescribing alignment with guidelines. J Womens Health (Larchmt). 2014;23:112–9.
Chen SL, Lee WL, Liang T, Liao IC. Factors associated with gender differences in medication adherence: a longitudinal study. J Adv Nurs. 2014;70:2031–40.
Song X, Tabák AG, Zethelius B, et al. Obesity attenuates gender differences in cardiovascular mortality. Cardiovasc Diabetol. 2014;13:144.
Anselmino M, Bartnik M, Malmberg K. Management of coronary artery disease in patients with and without diabetes mellitus. Acute management reasonable but secondary prevention unacceptably poor: a report from the Euro Heart Survey on Diabetes and the heart. Eur J Cardiovasc Prev Rehabil. 2007;14:28–36.
Steinberg BA, Braganza AJM, Eminowicz G, et al. Are statins being underdosed in clinical practice? data from TACTICS-TIMI 18. Crit Pathw Cardiol. 2005;4:169–73.
Bittner V, Bertolet M, Barraza FR, et al. Comprehensive cardiovascular risk factor control improves survival: the BARI 2D Trial. J Am Coll Cardiol. 2015;66:765–73.
Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the task force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J. 2008;29:2388–442.
Maggioni AP, Anker SD, Dahlström U, et al. Are hospitalized or ambulatory patients with heart failure treated in accordance with European Society of Cardiology guidelines? Evidence from 12,440 patients of the ESC Heart Failure Long-Term Registry. Eur J Heart Fail. 2013;15:1173–84.
Authors’ contributions
BB wrote/edited the manuscript and created figures. CS, VZ, MH, NH, ES, WK, MR, and RWH contributed to the discussion and reviewed/edited the manuscript. RWH conceptualized the study. RWH is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors read and approved the final manuscript.
Acknowledgements
We thank E. Bollow (Institute of Epidemiology and Medical Biometry, ZIBMT, University of Ulm) for statistical analysis. Furthermore, we thank all participating centers of the DPV initiative, especially the collaborating centers in this investigation: Aachen—Innere RWTH, Aachen—Uni-Kinderklinik RWTH, Aidlingen Praxisgemeinschaft, Altötting-Burghausen Innere Medizin, Asbach Kamillus-Klinik Innere, Augsburg IV. Med. Klinik, Bad Aibling Internist. Praxis, Bad Driburg/Bad Hermannsborn Innere, Bad Hersfeld Innere, Bad Krozingen Klinik Lazariterhof Park-Klinikum, Bad Kösen Kinder-Rehaklinik, Bad Mergentheim—Gemeinschaftspraxis DM-dorf Althausen, Bad Orb Spessart Klinik Reha, Bad Reichenhall Kreisklinik Innere Med., Bad Säckingen Hochrheinklinik Innere, Bayreuth Innere Medizin, Berchtesgaden MVZ Innere Med, Berlin Endokrinologikum, Berlin Evang. Krankenhaus Königin Elisabeth, Berlin Klinik St. Hedwig Innere, Berlin Oskar Zieten Krankenhaus Innere, Berlin Parkklinik Weissensee, Berlin Schlosspark-Klinik Innere, Berlin St. Josephskrankenhaus Innere, Berlin Vivantes Hellersdorf Innere, Bottrop Knappschaftskrankenhaus Innere, Braunfels-Wetzlar Innere, Bremen—Mitte Innere, Bremerhaven Kinderklinik, Castrop-Rauxel Rochus-Hospital, Chemnitz-Hartmannsdorf Innere Medizin—DIAKOMED-1, Coesfeld/Dülmen Innere Med., Darmstadt Innere Medizin, Datteln Vestische Kinderklinik, Deggendorf Medizinische Klinik II, Dornbirn Kinderklinik, Dortmund Knappschaftskrankenhaus Innere, Dortmund Medizinische Kliniken Nord, Dortmund-Hombruch Marienhospital, Dortmund-St. Josefshospital Innere, Dortmund-West Innere, Dresden Uni-Kinderklinik, Duisburg Evang. und Johanniter Krhs Innere, Duisburg Malteser Rhein-Ruhr St. Anna Innere, Duisburg Malteser St. Johannes, Duisburg-Huckingen, Duisburg-Huckingen Malteser Rhein-Ruhr ST. Johannes, Duisburg-St.Johannes Helios, Eberswalde Klinikum Barnim Werner Forßmann—Innere, Eisleben Lutherstadt Helios-Klinik, Erfurt Kinderklinik, Erlangen Uni Innere Medizin, Essen Diabetes-Schwerpunktpraxis, Forchheim Diabeteszentrum SPP, Frankfurt Diabeteszentrum Rhein-Main-Erwachsenendiabetologie (Bürgerhospital), Frankfurt Uni-Klinik Innere, Freiburg Uni Innere, Friedberg Innere Klinik, Fulda Innere Medizin, Geislingen Klinik Helfenstein Innere, Gelnhausen Innere, Gelsenkirchen Kinderklinik Marienhospital, Gießen Ev. Krankenhaus Mittelhessen, Graz Universitäts-Kinderklinik, Göppingen Innere Medizin, Güstrow Innere, Halberstadt Innere Med. St. Salvator AMEOS Klinik, Halberstadt Kinderklinik St. Salvator, Hamburg Endokrinologikum, Hanau St. Vincenz—Innere, Hannover Kinderklinik auf der Bult, Heidelberg St. Josefskrankenhaus, Heidelberg Uni-Kinderklinik, Heidelberg Uniklinik Innere, Heidenheim Arztpraxis Allgemeinmed, Heilbronn Innere Klinik, Herdecke Kinderklinik, Herford Innere Med I, Heringsdorf Inselklinik, Herne Evan. Krankenhaus Innere, Herten St. Elisabeth Innere Medizin, Hildesheim GmbH—Innere, Idar Oberstein Innere, Ingolstadt Klinikum Innere, Innsbruck Universitätsklinik Innere, Iserlohn Innere Medizin, Jena Uni-Kinderklinik, Kamen Klinikum Westfalen Hellmig Krankenhaus, Karlsburg Klinik für Diabetes & Stoffwechsel, Kassel Rot-Kreuz-Krankenhaus Innere, Kaufbeuren Innere Medizin, Kempen Heilig Geist—Innere, Kempen Heilig Geist-KHS—Innere, Kirchen DRK Krankenhaus Kinderklinik, Kirchheim-Nürtingen Innere, Kleve Innere Medizin, Koblenz Kemperhof 1. Med. Klinik, Konstanz Innere Klinik, Krefeld Alexianer Innere, Krefeld Innere Klinik, Krefeld-Uerdingen St. Josef Innere, Landau/Annweiler Innere, Lilienthal Diabeteszentrum, Limburg Innere Medizin, Lindenfels Luisenkrankenhaus Innere, Lindenfels Luisenkrankenhaus Innere 2, Linz AKH—2. Med, Linz Krankenhaus Barmherzige Schwestern Kardiologie Abt. Int. II, Ludwigshafen diabetol. SPP, Luxembourg—Centre Hospitalier, Lübeck Uni-Klinik Innere Medizin, Lünen Klinik am Park, Magdeburg Städtisches Klinikum Innere, Magdeburg Uni-Kinderklinik, Mannheim Uniklinik Innere Medizin, Marburg—UKGM Endokrinologie & Diabetes, Marktredwitz Innere Medizin, Marpingen-SPP, Moers—St. Josefskrankenhaus Innere, Murnau am Staffelsee—diabetol. SPP, Mühlacker Enzkreiskliniken Innere, München Diabetes-Zentrum Süd, München Schwerpunktpraxis, Münster Clemens-Hospital Innere, Münster Herz Jesu Innere, Neuburg Kinderklinik, Neumarkt Innere, Neunkirchen Innere Medizin, Neuwied Marienhaus Klinikum St. Elisabeth Innere, Nidda Bad Salzhausen Klinik Rabenstein/Innere-1 Reha, Nidda Bad Salzhausen Klinik Rabenstein/Innere-2 Reha, Oberhausen Innere, Oberhausen Kinderklinik, Offenbach/Main Innere Medizin, Oschersleben MEDIGREIF Bördekrankenhaus, Osterkappeln Innere, Ottobeuren Kreiskrankenhaus, Oy-Mittelberg Hochgebirgsklinik Kinder-Reha, Passau Kinderklinik, Pfullendorf Innere Medizin, Pirmasens Städtisches Krankenhaus Innere, Plauen Vogtlandklinikum, Prenzlau Krankenhaus Innere, Rastatt Kreiskrankenhaus Innere, Reutlingen Kinderklinik, Reutlingen Klinikum Steinenberg Innere, Rosenheim Innere Medizin, Rosenheim Schwerpunktpraxis, Rostock Universität Innere Medizin, Saaldorf-Surheim Diabetespraxis, Schwerin Innere Medizin, Schwäbisch Hall Diakonie Innere Medizin, Spaichingen Innere, St. Pölten Innere, Stolberg Kinderklinik, Stuttgart Bethesda Agaplesion, Tettnang Innere Medizin, Timmendorfer Strand, Traunstein diabetol. Schwerpunktpraxis, Trostberg Innere, Ulm Schwerpunktpraxis Bahnhofsplatz, Ulm Uni Innere Medizin, Villingen-Schwenningen SPP, Villingen-Schwenningen Schwarzwald-Baar-Klinikum Innere, Wangen Oberschwabenklinik Innere Medizin, Weisswasser Kreiskrankenhaus, Wels Klinikum Pädiatrie, Wernberg-Köblitz SPP, Wetzlar Schwerpunkt-Praxis, Wien 3. Med. Hietzing Innere, Wien Uni Innere Med III, Wien Uni-Kinderklinik, Wien Wilhelminenspital 5. Med. Abteilung, Wiesbaden Horst-Schmidt-Kinderkliniken, Wittenberg Innere Medizin, Wolgast Innere Medizin, Zweibrücken Ev. KH. Innere.
Availability of data and materials
All data relevant to the given manuscript have been stored in a separate file which can be made freely available to external investigators upon request.
Competing interests
The authors declare that they have no competing interests.
Funding
The study was supported by the European Foundation for the Study of Diabetes (EFSD). Further financial support was provided by the German Competence Network Diabetes mellitus (diabetes meta-database) funded by the Federal Ministry of Education and Research (FKZ 01GI1106), now integrated into the German Center for Diabetes Research (DZD). Sponsors were not involved in data acquisition or analysis.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Bohn, B., Schöfl, C., Zimmer, V. et al. Achievement of treatment goals for secondary prevention of myocardial infarction or stroke in 29,325 patients with type 2 diabetes: a German/Austrian DPV-multicenter analysis. Cardiovasc Diabetol 15, 72 (2016). https://doi.org/10.1186/s12933-016-0391-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-016-0391-8