Abstract
Background
The intake of nutrients with antioxidant properties is hypothesized to augment antioxidant defenses, decrease oxidant damage to tissues, and attenuate age-related rate of decline in lung function. The objective was to determine whether long-term intervention with selenium and/or vitamin E supplements attenuates the annual rate of decline in lung function, particularly in cigarette smokers.
Methods
The Respiratory Ancillary Study (RAS) tested the single and joint effects of selenium (200 μg/d L-selenomethionine) and vitamin E (400 IU/day all rac-α-tocopheryl acetate) in a randomized double-blind placebo-controlled trial. At the end of the intervention, 1,641 men had repeated pulmonary function tests separated by an average of 3 years. Linear mixed-effects regression models estimated the effect of intervention on annual rate of decline in lung function.
Results
Compared to placebo, intervention had no main effect on either forced expiratory volume in the first second (FEV1) or forced expiratory flow (FEF25–75). There was no evidence for a smoking by treatment interaction for FEV1, but selenium attenuated rate of decline in FEF25–75 in current smokers (P = 0.0219). For current smokers randomized to selenium, annual rate of decline in FEF25–75 was similar to the annual decline experienced by never smokers randomized to placebo, with consistent effects for selenium alone and combined with vitamin E.
Conclusions
Among all men, there was no effect of selenium and/or vitamin E supplementation on rate of lung function decline. However, current smokers randomized to selenium had an attenuated rate of decline in FEF25–75, a marker of airflow.
Trial registration
Clinicaltrials.gov identifier: NCT00241865.
Similar content being viewed by others
Background
Pulmonary function, which is reliably measured by spirometry, is central to the diagnosis and staging of chronic obstructive pulmonary disease (COPD). COPD, the third most common cause of death in the US, led to $29.5B in direct costs and $20B in lost productivity costs in 2010 [1]. The age-related rate of decline in the forced expiratory volume in the first second (FEV1) is a marker of mortality risk in the general population [2] and in healthy smokers [3], the rate of decline is steeper in smokers [4] and in COPD patients, although the latter association varies by disease attributes [5,6]. The forced expiratory flow at the mid-portion of forced vital capacity (FEF25–75) reflects the state of small airways, and offers a measure of lung function reflecting airflow rather than volume [7]. Attenuating lung function decline may reduce morbidity and mortality, both in healthy persons and in COPD patients. The identification of factors that affect lung function decline is important to the development of clinical or public health interventions.
Both smoking and aging accelerate the annual rate of decline in FEV1 [4,8]; the effect of other factors, including diet, is less clear [9]. Observational studies of nutrients (whole foods, micronutrients, dietary patterns, biomarkers) and lung outcomes (COPD, lung function) support the broad hypothesis that nutrients with antioxidant properties improve lung health [10-13], presumably by altering the oxidant/antioxidant balance in lung tissue. A recent critical review of the evidence for a causal relation between nutrition and lung outcomes [9] concluded there was a “limited/suggestive” role for diet, reflecting that the majority of studies are cross-sectional. However, most existing longitudinal studies report protective associations of antioxidant nutrients and lung outcomes, and there is strong evidence that the beneficial effects of diet may be limited to smokers [14]. Given that observational studies are limited by potential confounding due to lifestyle factors associated with healthful diets, and given that measures of diet based on self-report are subject to bias and have poor precision, experimental studies are needed to fully understand whether nutrition affects lung function and its decline with age, particularly in cigarette smokers.
The few randomized controlled trials considering respiratory endpoints other than lung cancer used post-hoc, secondary analyses [15-17] mainly in special populations (all heavy smokers, all with vascular disease), did not study lung function decline, and did not test selenium. Using the infrastructure of the Selenium and Vitamin E Cancer Prevention Trial (SELECT) [18], we conducted an ancillary study nested within SELECT to investigate the a priori hypothesis that supplementation with selenium and/or vitamin E, two nutrients with antioxidant potential, would attenuate the annual decline in lung function; we hypothesized a stronger effect in cigarette smokers given their higher exposure to inhaled oxidants.
Methods
Study design
The Respiratory Ancillary Study (RAS) was nested within SELECT [18], a phase 3 randomized, placebo-controlled double-blind trial of 35,533 men testing whether selenium (200 μg/d L-selenomethionine) and vitamin E (400 IU/d all rac-α-tocopheryl acetate) alone and/or in combination would prevent prostate cancer. SELECT eligibility included age ≥55 y (≥50 y in African-Americans), serum prostate-specific antigen ≤ 4 ng/mL, and no clinical evidence of prostate cancer. SELECT enrolled men in the United States and Canada between 2001–2004; use of study supplements stopped on 10/23/2008, after an interim analysis determined that there was no effect and that further intervention was unlikely to show significant reduction in prostate cancer incidence [18]. RAS used a post-randomization design, due to rapid enrollment in SELECT relative to the start of RAS; thus, we did not measure pre-randomization lung function, but we captured the rate of decline over the intervention period through repeated measurements of lung function. This design assumed that the intervention effect is reached early in the study, and is stable over time. To test the hypothesis that current smokers benefit more from intervention, RAS enrolled men from the 16 SELECT sites with the greatest number of current cigarette smokers (Additional file 1: Table S1). Based on the predicted effect of intervention on annual FEV1 decline, assuming a 7–10 year follow-up, the target sample size in RAS was 3000 men.
Participants
Eligibility requirements for registration to RAS included SELECT registration at one of the 16 SELECT sites with a high proportion of smokers and adherence to supplements (either active or placebo) at the time of RAS registration. Each SELECT site invited all eligible current smokers to RAS and, depending on the number of participants at the site, either a random sample or all eligible former and never smokers. Ultimately, men were registered at their first (5%), second (17%), third (38%) or fourth (40%) annual SELECT visit. The RAS was approved by local IRBs at each of the 16 study sites, and by the Cornell University IRB.
End point assessment
The primary endpoint was annual decline in FEV1; the secondary endpoint was annual decline in FEF25–75. Spirometry was assessed at three out of four annual visits spanning three years. Due to early termination of SELECT, not all RAS participants completed all scheduled pulmonary function tests (PFTs); the endpoint (the third and final PFT) was available for 57% of participants. We assume this is an unbiased sample given the timing of supplementation withdrawal relative to the timing of a participant’s annual visit is expected to be random and thus equal across arms.
Pulmonary function testing followed American Thoracic Society guidelines [19] and used the EasyOne handheld, flow-sensing spirometer, which has excellent validity and reliability, and significantly simpler field implementation in comparison to desktop devices [20]. Only PFTs meeting criteria for acceptable start and end of test and for reliability were included in analyses; further details are provided in Additional file 1: Table S2).
Statistical analysis
There were three pre-specified main effect comparisons between each active treatment arm and placebo, with a P-value threshold of 0.018 to account for the three tests with a common placebo group. All analyses were intent-to-treat, and effects were estimated using a linear mixed-effects regression model incorporating the repeated measurements of pulmonary function (either FEV1 or FEF25–75) as the outcome. The model included random intercept and slope, and the following fixed effects: time (time between each PFT and baseline), treatment arm and its interaction with time (treatment-by-time), age, height, race and smoking. The treatment-by-time coefficient estimated the effect of treatment on annual rate of decline in lung function. All RAS men with ≥1 (n = 2920) PFT were included in the model and contributed to estimates of effects of age, height, race and smoking, but only men with ≥2 PFTs (n = 1677) were informative for the estimate of the time-by-treatment coefficient. Missing data were assumed to be missing at random, given very low drop-out rates. To test whether treatment effects differed by smoking status, models were extended to include the treatment-by-time-by-smoking interaction terms, and the significance threshold for the interaction effects was a nominal P-value of 0.05.
Results
Participants
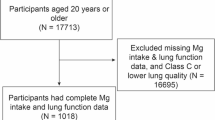
RAS enrolled 2,920 men (Figure 1) at 16 SELECT sites between 7/2/2004 and 4/30/2007. RAS eligibility and enrollment were blind to intervention arm, and indeed the number of participants across the four arms was balanced (Figure 1). RAS experienced minimal attrition, with only 2-3% of men in each intervention group refusing further RAS and/or SELECT follow-up at some time point after registration. All participants studied herein had at least one acceptable PFT, and 56 to 60% of participants in each arm had repeated PFTs, confirming that repeated measurements for the endpoint assessment were similar by arm. The mean number of PFTs per participant was 2.3 (SD 1.1; median 3) with a mean of 36.1 months (SD 4.2) between first and last PFT (median 35.8 months; range 24 to 52). Spirometry quality control scores ranged from 3.2 to 3.7 out of maximum score of 4 (Additional file 1: Table S2).
Flow of participants included in FEV 1 analysis by intervention group. 1Participants lost to follow-up defined as deaths and participants not in contact for 2 years prior to the end of supplemented time period (March 1, 2009 was used in analyses to proxy the end of supplement). 2Refusals defined as withdrawals from SELECT and/or RAS.
RAS participants had similar distributions of age, race/ethnicity, education, smoking history and height across intervention arms (Table 1), confirming that the post-randomization design yielded four groups balanced on characteristics. The participants with one PFT were similar on all baseline characteristics to participants with repeated PFTs (data not shown); this is consistent with our expectation because the lack of repeated PFT data was a function of the date the intervention was withdrawn, and was not driven by participant choice or participant characteristics. Thus, we expect the estimate of the effect of treatment on lung function decline to be unbiased. Among participants who completed the final PFT, the mean time from SELECT registration to a participant’s last PFT was 60.4 months (SD 10.8; median 59.8), thus results reflect intervention effects of about 5 years duration.
Adherence among RAS participants (Table 2), determined using pill count, compares well to all SELECT participants [18]. Across the four arms, 87 to 92% of RAS men were adherent to the selenium supplement (or matching placebo) in year 1, and 80 to 84% were adherent in year 5. Similarly, 87 to 92% of RAS men were adherent to the vitamin E supplement (or matching placebo) in year 1, and 79 to 81% were adherent in year 5. Across all arms, for the full study period, self-supplementation with non-study vitamin E and selenium (drop-in rate, assessed by self-reported use of either supplement) was reported by ≤2.3% and ≤1.2% of participants, respectively.
Rate of decline in pulmonary function
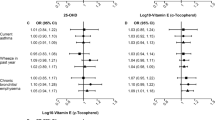
Overall, the distribution of rate of decline in FEV1 was consistent with expectations of decline, and the mean annual change in FEV1 was −37.5 mL (SD 12.5; Additional file 1: Figure S1). Compared to never smokers, FEV1 was 363 mL lower in current smokers and annual decline in FEV1 was 6.9 mL/y steeper. In unadjusted analyses of raw data, compared with the placebo group (Table 3), participants randomized to intervention experienced an attenuation of between 3 and 6 mL/y in rate of change in FEV1, but there were no statistically significant differences between arms. Similarly, for rate of decline in FEF25–75 (mL/second/y), there were no statistically significant differences between arms (Table 4).
In linear mixed-effects regression models adjusted for covariates, the main effect of intervention on rate of decline in lung function was similar to the estimates based on raw data, considering markers of both volume (FEV1; Table 3) and flow (FEF25–75; Table 4). Thus, in intervention groups the annual rate of decline in FEV1 was lower by between 1 and 6 mL/y versus placebo, but effects were not statistically significant (Table 3). Similarly, there were no statistically significant main effects of any intervention on the annual rate of decline in FEF25–75 (Table 4). Sensitivity analyses that considered study site or the registration contact at which men started RAS (reflecting the length of time on study intervention) showed similar results.
Effect modification by cigarette smoking
The hypothesis that smoking modifies the effect of supplementation was pre-specified, and models were extended to estimate intervention effects within categories of cigarette smoking; categories included current, former (quit prior to trial), and never (lifetime never smoker). In the placebo arm, expected differences in rate of decline in FEV1 were confirmed such that the annual decline in current smokers was 11 to 16 mL/y steeper compared to former and never smokers (Table 3). Similarly, the annual rate of decline in FEF25–75 in current smokers on placebo was more than two-fold that in never smokers (P = 0.0189; Table 4).
There was no evidence that smoking modified the effect of intervention on rate of decline in FEV1, and all P values exceeded the threshold of 0.05. However, for the FEF25–75 outcome, compared to placebo the annual rate of decline in FEF25–75 was attenuated in current cigarette smokers in the selenium arm (P = 0.0219) and in the combined arm (P = 0.0236). Further models testing any selenium (selenium alone and selenium + vitamin E, combined) vs. placebo showed that FEF25–75 rate of decline was decreased by more than half in current smokers on any selenium compared to current smokers in the placebo group (P = 0.0095).
Discussion
This is the first randomized trial of selenium and/or vitamin E intervention that studies the rate of decline in pulmonary function as the endpoint. This study is important because it contributes new information about whether interventions that presumably affect the antioxidant/oxidant balance in lung tissue can ameliorate or attenuate a functional outcome reflecting lung health. Neither supplementation with selenium nor vitamin E had statistically significant main effects on rate of decline in FEV1 or FEF25–75. Following our a priori hypothesis that effects are stronger in and/or limited to current cigarette smokers, there was evidence for a differential effect of selenium in current smokers for the flow-related endpoint such that smokers supplemented with any selenium, either alone or in combination with vitamin E, had an attenuated rate of decline in FEF25–75.
This randomized trial evidence for an effect of selenium on annual rate of decline in lung function in smokers is consistent with prior cross-sectional studies that reported strong positive associations of serum selenium with lung function [14]. An analysis of baseline bloods collected on a subset of SELECT participants [18] found that men were rarely low on serum selenium, where low selenium was defined as ≤ 121.6 ng/mL consistent with prior studies of cancer outcomes [21]. While this suggests the potential-to-benefit from selenium intervention in the overall study may be low, the potential to benefit in smokers is likely to be greater given prior evidence that selenium concentrations are lower in smokers [22], and, indeed, this is supported by our findings.
The pattern of the RAS findings, including the effect of selenium on flow (FEF25–75) but not volume parameters and the magnitude of the effect sizes, are similar to the effects of air pollution on lung function reported in the SAPALDIA study. Based on 11 years of follow-up, SAPALDIA reported mean annual rate of decline in FEV1 and FEF25–75 of 35 mL/y (SD 30) and 71 mL/second/y (SD 65), respectively [23]. In the RAS placebo arm, average annual rates of decline were very similar, although the RAS estimates are more variable given the shorter duration of follow-up and more closely spaced PFTs. SAPALDIA reported that reductions in particulate matter ≤ 10 microns in diameter (PM10) were associated with the rate of change in both FEV1 and FEF25–75, but the strength of the association and the level of statistical significance were greater for the FEF25–75 outcome [23], similar to the findings reported herein for supplement effects in RAS. In current smokers the selenium intervention effect size for annual decline in FEV1 was similar to the effect size for reducing PM10 exposure by 10 μ/m3 in SAPALDIA (attenuated FEV1 decline by 4 mL/y). Greater effect sizes were seen for FEF25–75 in both studies: in SAPALDIA, reducing PM10 attenuated FEF25–75 decline by 11 mL/second/y, in RAS selenium supplementation attenuated FEF25–75 decline by 59 mL/second/y. While FEV1 is less variable than FEF25–75 in cross-sectional studies [19], longitudinal declines in both endpoints are of interest and FEF25–75 findings may be salient in smokers given that changes in flow rates may signal early changes in small airways function [24]. Although such changes may not be predictive at the individual level, they may be informative in the comparison of treatment groups. In addition, a longitudinal endpoint, which leverages repeated measurements per participant, and uses all available spirometry data on each participant (an approach that is consistent with two prior studies of longitudinal change [5,25]), is less affected by variability in comparison to cross-sectional studies.
Although the vitamin E effect sizes were clinically meaningful and consistent in effect direction (attenuated rate of decline) across two pulmonary function measures, with stronger effects of intervention in current smokers, the effects did not meet pre-set criteria for statistical significance. These findings reflect either a true lack of effect of vitamin E on rate of decline in lung function, the possibility that baseline vitamin E levels were high (or at minimum, not deficient) and thus there was limited potential to benefit from supplementation, or the possibility that attenuation in decline might occur only with a longer period of supplementation. While several past observational studies reported that associations of vitamin E were limited to smokers [26], such studies are more likely to be affected by confounding than the randomized trial findings reported herein.
The Respiratory Ancillary Study (RAS) to SELECT used a post-randomization design, and participants were registered to the RAS after active supplementation began. The primary endpoint was rate of decline in lung function; absolute differences in lung function due to the supplements over a fixed period of time were not calculated because first measurements were obtained after the participants started taking their supplements. The design assumes that effects are achieved quickly and are stable over the supplemented period, which is reasonable given the hypothesis of support for antioxidant function provided by the supplements.
This study measured pre-bronchodilator spirometry, but the lack of post-bronchodilator spirometry is not a serious weakness given the primary outcome is rate of decline, which relies on within-person repeated measurements. A recent study shows similar associations of pre- and post-bronchodilator spirometry with mortality [3], which is welcome news given the added participant burden of conducting post-bronchodilator spirometry in healthy population studies.
The strengths of RAS include the enrichment of the study sample with current cigarette smokers, which was part of the a priori intent to test effect modification, and the inclusion of a diverse sample (24% African Americans), which supports inference to broader population groups. An additional strength was the extensive infrastructure provided by SELECT, which allowed RAS to be conducted with efficiencies of cost and effort. SELECT infrastructure included an online data collection tool, which allowed incorporation of web-based uploading of spirometry data on a weekly basis, and bi-annual meetings of study personnel, which allowed for optimal training and refresher courses on spirometry methodology.
A few limitations are worth noting. In the post-randomization design, we cannot directly estimate whether the intervention increased FEV1 early in the supplementation period in smokers on the active study supplements. This question is important given that prior studies among individuals with COPD show that some clinical treatments increase FEV1, but have no effect on FEV1 rate of decline [27], and in light of the Lung Health Study, which showed that smoking cessation led to a small but significant initial rebound in FEV1, followed by an attenuation in the rate of decline [28]. Our study was conducted in male participants in the SELECT prostate cancer prevention trial, thus whether findings apply to women requires further study. In addition, the design of SELECT did not vary dose and/or formulation, and did not consider whether genetic variation might influence nutrient requirements for optimal health. Finally, the premature termination of supplements meant that final pulmonary function test on some participants was collected well after supplements had been discontinued, and thus analyses were based on fewer participants than originally planned.
Conclusions
While smoking cessation is the key public health intervention to prevent smoking-related health effects, about 20% of the population continues to smoke [1]. This study investigated the role of nutritional supplementation in lung function decline to identify possible intervention strategies to mitigate lung effects in continuing smokers. This randomized controlled trial found statistically significant protective effects of selenium, specifically 200 μg/d L-selenomethionine, on rate of decline in FEF25–75 in current cigarette smokers. Supplementation with selenium attenuated the annual rate of decline in FEF25–75 in current cigarette smokers, but neither vitamin E nor selenium had effects on rate of decline in FEV1. Further studies are needed to understand whether intervention effects are modified by baseline selenium nutriture and/or selenium-related genetic variation [29].
Abbreviations
- FEV1 :
-
Forced expiratory volume in the first second
- FEF25–75 :
-
Forced expiratory flow
- COPD:
-
Chronic obstructive pulmonary disease
- SELECT:
-
Selenium and Vitamin E Cancer Prevention Trial
- RAS:
-
The Respiratory Ancillary Study to SELECT
References
American Lung Association. Trends in COPD (Chronic Brochitis and Emphysema): Morbidity and Mortality. Epidemiology and Statistics Unit, Research and Health Education Division, March 2013. [http://www.lung.org/finding-cures/our-research/trend-reports/copd-trend-report.pdf]
Sabia S, Shipley M, Elbaz A, Marmot M, Kivimaki M, Kauffmann F, et al. Why does lung function predict mortality? Results from the Whitehall II Cohort Study. Am J Epidemiol. 2010;172:1415–23.
Mannino DM, Diaz-Guzman E, Buist S. Pre- and post-bronchodilator lung function as predictors of mortality in the Lung Health Study. Respir Res. 2011;12:136.
Anthonisen NR, Connett JE, Kiley JP, Altose MD, Bailey WC, Buist AS, et al. Effects of smoking intervention and the use of an inhaled anticholinergic bronchodilator on the rate of decline of FEV1. The Lung Health Study. JAMA. 1994;272:1497–505.
Vestbo J, Edwards LD, Scanlon PD, Yates JC, Agusti A, Bakke P, et al. Changes in forced expiratory volume in 1 second over time in COPD. N Engl J Med. 2011;365:1184–92.
Washko GR. Rate of decline in FEV1: is emphysema the culprit? Am J Respir Crit Care Med. 2012;185:2–3.
DeMeo DL, Carey VJ, Chapman HA, Reilly JJ, Ginns LC, Speizer FE, et al. Familial aggregation of FEF(25–75) and FEF(25–75)/FVC in families with severe, early onset COPD. Thorax. 2004;59:396–400.
Lee PN, Fry JS. Systematic review of the evidence relating FEV1 decline to giving up smoking. BMC Med. 2010;8:84.
Eisner MD, Anthonisen N, Coultas D, Kuenzli N, Perez-Padilla R, Postma D, et al. An official American Thoracic Society public policy statement: Novel risk factors and the global burden of Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2010;182:693–718.
Fogarty A, Britton J. The role of diet in the aetiology of asthma. Clin Exp Allergy. 2000;30:615–27.
Romieu I, Trenga C. Diet and obstructive lung diseases. Epidemiol Rev. 2001;23:268–87.
Schunemann HJ, Freudenheim JL, Grant BJ. Epidemiologic evidence linking antioxidant vitamins to pulmonary function and airway obstruction. Epidemiol Rev. 2001;23:248–67.
McKeever TM, Britton J. Diet and asthma. Am J Respir Crit Care Med. 2004;170:725–9.
Hu G, Cassano PA. Antioxidant nutrients and pulmonary function: the Third National Health and Nutrition Examination Survey (NHANES III). Am J Epidemiol. 2000;151:975–81.
Rautalahti M, Virtamo J, Haukka J, Heinonen OP, Sundvall J, Albanes D, et al. The effect of alpha-tocopherol and beta-carotene supplementation on COPD symptoms. Am J Respir Crit Care Med. 1997;156:1447–52.
Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of antioxidant vitamin supplementation in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:23–33.
Agler AH, Kurth T, Gaziano JM, Buring JE, Cassano PA. Randomised vitamin E supplementation and risk of chronic lung disease in the Women’s Health Study. Thorax. 2011;66:320–5.
Lippman SM, Klein EA, Goodman PJ, Lucia MS, Thompson IM, Ford LG, et al. Effect of selenium and vitamin E on risk of prostate cancer and other cancers: the Selenium and Vitamin E Cancer Prevention Trial (SELECT). JAMA. 2009;301:39–51.
American Thoracic Society. Standardization of Spirometry, 1994 Update. American Thoracic Society. Am J Respir Crit Care Med. 1995;152:1107–36.
Barr RG, Stemple KJ, Mesia-Vela S, Basner RC, Derk SJ, Henneberger PK, et al. Reproducibility and validity of a handheld spirometer. Respir Care. 2008;53:433–41.
Duffield-Lillico AJ, Dalkin BL, Reid ME, Turnbull BW, Slate EH, Jacobs ET, et al. Selenium supplementation, baseline plasma selenium status and incidence of prostate cancer: an analysis of the complete treatment period of the Nutritional Prevention of Cancer Trial. BJU Int. 2003;91:608–12.
Arnaud J, Bertrais S, Roussel AM, Arnault N, Ruffieux D, Favier A, et al. Serum selenium determinants in French adults: the SU.VI.M.AX study. Br J Nutr. 2006;95:313–20.
Downs SH, Schindler C, Liu LJ, Keidel D, Bayer-Oglesby L, Brutsche MH, et al. Reduced exposure to PM10 and attenuated age-related decline in lung function. N Engl J Med. 2007;357:2338–47.
Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26:948–68.
Tang W, Kowgier M, Loth DW, Soler Artigas M, Joubert BR, Hodge E, et al. Large-scale genome-wide association studies and meta-analyses of longitudinal change in adult lung function. PLoS One. 2014;9:e100776.
Guenegou A, Leynaert B, Pin I, Le Moel G, Zureik M, Neukirch F. Serum carotenoids, vitamins A and E, and 8 year lung function decline in a general population. Thorax. 2006;61:320–6.
Soriano JB, Sin DD, Zhang X, Camp PG, Anderson JA, Anthonisen NR, et al. A pooled analysis of FEV1 decline in COPD patients randomized to inhaled corticosteroids or placebo. Chest. 2007;131:682–9.
Anthonisen NR, Connett JE, Murray RP. Smoking and lung function of Lung Health Study participants after 11 years. Am J Respir Crit Care Med. 2002;166:675–9.
Davis CD, Tsuji PA, Milner JA. Selenoproteins and cancer prevention. Annu Rev Nutr. 2012;32:73–95.
Acknowledgements
SELECT principal investigators at each SELECT site implemented this study, together with clinical research associates at each site, and the cooperation of these investigators was critical to the successful completion of RAS. The clinical research associates collected data for RAS, and participated in bi-annual review session on study protocol and spirometry methods. The first spirometry training for RAS was conducted in collaboration with Drs. Robert Jensen and Robert Crapo and a review session was conducted in collaboration with Dr. Paul Enright; the assistance of these experts was key to assuring the quality of measurement in the study, and we gratefully acknowledge this important role. RAS acknowledges these dedicated professionals for their hard work and contributions to the collection of spirometry and questionnaire data, as follows: Altamira Family Medicine, San Juan PR: Jaime Claudio, MD and Migdalia Arce; Le Centre de Recherché, Quebec Canada: Louis LaCombe, MD and Sylvie Comeau; Harbor Medical Center, UCLA, Los Angeles CA: Rowan T. Chlebowski, MD, PhD and Qi Yuan, Ebonie McDaniel and Joseph Quinsay; London Regional Cancer Center and Health Sciences Center, London Canada: Joseph L. Chin, MD and Eric Winquist, MD, and Julie Duncan, Carolyn Pollack, Juanita Will, Ann-Marie Waschenko, Deb Bruckshwaiger, Joanne Ouelette, Nancy Pus; MD Anderson, Houston TX: Elise D. Cook, MD and Gwen Corrigan, Alma Garcia, Sandy Black, Karen Davin, Patti Reed; Rush University Medical Center, Chicago IL: Steven Rothschild, MD and Walter Washington, Rolanda J. Flynn, Jennifer Patwardhan, Joe Harrington; SUNY Stonybrook, Stonybrook NY: Iris A. Granek, MD and Pushpa Talanki; Swedish Medical Center, Seattle WA: Gary E. Goodman, MD and Sarah Fanizzi, Kris Huget; University of California, San Diego and Chula Vista Hospital: Kellog Parsons, MD and Pat Junquera, Kyle York, Sue Stockton; Upstate Carolina Medical Center, Spartanburg SC: James D. Bearden III, MD and Penny Horne, Darlene Mullins, Jonaka Hunter-Young; VA Medical Center Jesse Brown, Chicago IL: Thomas E. Lad, MD and Bharathi Reddivari, Rubina Salar; VA Medical Center Kansas City, Kansas City KS: Peter J. Van Valdhuizen, Jr., MD and Tracina Renaud, Sara Spencer; VA Medical Center Minneapolis, Minneapolis MN: Timothy J. Wilt, MD, MPH and Lori Sorensen; VA Medical Center Puget Sound, Seattle WA: Daniel W. Lin, MD and Crystal Kimmie, Alma MacAraeg, Judy Stenstrom; VA Medical Center Washington DC: Steven H. Krasnow, MD and Theresa Schaefer; Wichita Community Clinical Oncology Program, Wichita KS: Shaker Dakhil, MD and ZoeAnna Buckner, Marta Guerrero. Finally, the authors wish to thank the participants in the study: the research would not have been possible without their generous contributions of time and effort.
Funding
Supported by the NHLBI (R01HL071022), and SELECT was funded by Public Health Service grants CA37429 and 5UM1CA182883 from the National Cancer Institute.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
PC, AK, CT designed RAS; SL, EK, CT and PG designed SELECT; PC, KG, MB, KR, JH collected data; PC, KG, KA, AK, PG, CT analyzed and interpreted data; PC drafted manuscript and all authors contributed to critical revision in preparation for publication. All authors read and approved the final manuscript.
Scott M Lippman and Eric Klein contributed equally to this work.
Additional file
Additional file 1:
Supplemental Methods. Table S1. The geographic location and number of participants in the Respiratory Ancillary Study (RAS), by SELECT study site, April 2004 through October 2008. Table S2. Spirometry Testing: Description of Pulmonary Function Test Measurements and Quality Control Indicators in the Respiratory Ancillary Study to SELECT, April 2004 to October 2008. Table S3. Linear mixed-effects regression model for main effects of treatment on FEV1 and FEF25–75 for model testing each treatment arm vs. placebo. Table S4. Linear mixed-effects regression model for effects of treatment on FEV1 and FEF25–75 including test of smoking by treatment interaction. Figure S1. Distribution of Annual Change in Forced Expiratory Volume in the First Second (FEV1)1 for Participants in the Respiratory Ancillary Study (RAS) to SELECT.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Cassano, P.A., Guertin, K.A., Kristal, A.R. et al. A randomized controlled trial of vitamin E and selenium on rate of decline in lung function. Respir Res 16, 35 (2015). https://doi.org/10.1186/s12931-015-0195-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-015-0195-5