Abstract
Background
The rate of forced expiratory volume in 1 second (FEV1) decline ("beta") is a marker of chronic obstructive pulmonary disease risk. The reduction in beta after quitting smoking is an upper limit for the reduction achievable from switching to novel nicotine delivery products. We review available evidence to estimate this reduction and quantify the relationship of smoking to beta.
Methods
Studies were identified, in healthy individuals or patients with respiratory disease, that provided data on beta over at least 2 years of follow-up, separately for those who gave up smoking and other smoking groups. Publications to June 2010 were considered. Independent beta estimates were derived for four main smoking groups: never smokers, ex-smokers (before baseline), quitters (during follow-up) and continuing smokers. Unweighted and inverse variance-weighted regression analyses compared betas in the smoking groups, and in continuing smokers by amount smoked, and estimated whether beta or beta differences between smoking groups varied by age, sex and other factors.
Results
Forty-seven studies had relevant data, 28 for both sexes and 19 for males. Sixteen studies started before 1970. Mean follow-up was 11 years. On the basis of weighted analysis of 303 betas for the four smoking groups, never smokers had a beta 10.8 mL/yr (95% confidence interval (CI), 8.9 to 12.8) less than continuing smokers. Betas for ex-smokers were 12.4 mL/yr (95% CI, 10.1 to 14.7) less than for continuing smokers, and for quitters, 8.5 mL/yr (95% CI, 5.6 to 11.4) less. These betas were similar to that for never smokers. In continuing smokers, beta increased 0.33 mL/yr per cigarette/day. Beta differences between continuing smokers and those who gave up were greater in patients with respiratory disease or with reduced baseline lung function, but were not clearly related to age or sex.
Conclusion
The available data have numerous limitations, but clearly show that continuing smokers have a beta that is dose-related and over 10 mL/yr greater than in never smokers, ex-smokers or quitters. The greater decline in those with respiratory disease or reduced lung function is consistent with some smokers having a more rapid rate of FEV1 decline. These results help in designing studies comparing continuing smokers of conventional cigarettes and switchers to novel products.
Similar content being viewed by others
Background
It is generally believed that 15% to 20% of all long-term regular smokers will develop clinically overt chronic obstructive pulmonary disease (COPD) and that most COPD cases worldwide are attributable to cigarette smoking [1]. COPD, along with ischaemic heart disease and lung cancer, is a major contributor to the number of deaths caused by smoking [2]. In this paper, we attempt to provide information relevant to determining the maximum reduction in risk of COPD that might be achieved from the introduction of new-generation nicotine delivery products that are currently being developed with the aim of substantially reducing the risks of tobacco-related disease. There are two underlying assumptions: that any benefits from the introduction of these products cannot exceed those of giving up smoking and that the rate of decline over time in forced expiratory volume in 1 second (FEV1) is a reliable marker of the risk of COPD. FEV1 is also a marker of other respiratory diseases such as asthma, pulmonary fibrosis or cystic fibrosis. The information we provide should also be relevant in a wider context, such as research into the use of non-nicotine-containing drugs in the area of smoking cessation and more generally in accurately conveying the hazards of smoking.
We present a systematic review of the epidemiological evidence on the relationship of smoking status to the rate of FEV1 decline. While our major interest is in the comparison of rates in continuing smokers and those who gave up, we also summarize information on the rate of FEV1 decline in never smokers and on the relationship of FEV1 decline to amount smoked. We also investigate how differences in the rate of FEV1 decline by smoking status are affected by other factors, with the aim of identifying those subgroups that show the largest differences between continuing smokers and those who give up smoking.
It is well known that continuing smokers have an average rate of decline in FEV1 that is substantially greater than that of people who have never smoked [2], and a recent review by Willemse et al. [3] summarizes some data demonstrating that giving up smoking reduces the rate of decline in smokers without chronic symptoms, in smokers with nonobstructive chronic bronchitis and in smokers with COPD. However, summary estimates, based on all available data, of the extent of the decline in those who give up smoking relative to those who continue to smoke is not available in the literature, and a major aim of our paper is to provide this information.
We restrict attention to studies providing data on FEV1 in the same individuals at more than one time point and also data for those who give up smoking. Four smoking groups are particularly relevant to the analyses, and, to avoid confusion, we henceforward consistently describe them as "never smokers", "ex-smokers", "quitters" and "continuing smokers". We define "quitters" as subjects smoking at the start of the follow-up period but not still smoking at the end, and "ex-smokers" as those who had given up smoking by the start of the follow-up period and did not resume smoking during it. "Continuing smokers" are those reporting current smoking at the start and end of the period, and "never smokers" are those reporting never having smoked at both time points. For convenience, we also routinely use the term "beta" to mean the estimated rate of decline of FEV1 in millilitres per year over the follow-up period, with a positive beta implying a lower FEV1 at the end of the period. Beta is often used in statistical contexts to describe the slope of a line.
Methods
Selection of studies
Studies selected had to satisfy five conditions: (1) FEV1 must be measured in the same individuals at least twice over a period of at least 2 years; (2) data must be reported separately for those who give up smoking, with randomized studies reporting results only by advice to quit smoking being excluded; (3) results for a quantitative index of FEV1 decline over a period must be available directly or calculable from the data presented; (4) subjects studied must be adults (or present results for an age group, such as 15+ years, consisting predominantly of adults); and (5) subjects studied may be healthy individuals or patients with COPD, chronic bronchitis or emphysema, but not patients with other specific conditions (for example, α1-antitrypsin deficiency) or workers in occupations with a high risk of disease (for example, miners).
Relevant publications were initially sought from a MedLine search conducted on 6 April 2009, on "(Lung function or FEV1 or decline in FEV1) and (ex-smokers or smoking cessation)" limited to "Humans" and to "All adults: 19+ years", from publications cited in Table 2 and 3 of a review by Willemse et al. in 2004 [3], from the relevant chapter of an International Agency for Research on Cancer handbook in 2007 [1], from an earlier unpublished collection of literature on smoking and FEV1 (Alison Thornton, personal communication, 28 October 2004) and from reference lists of papers identified. Subsequently, on 6 July 2010, the search was updated to 30 June 2010, with new publications being identified from this search and from reference lists of papers identified. Fuller details of the search strategy are given in Additional file 1 FEV1 search strategy.doc.
Data entry
For each study, relevant data were entered into a study database and a beta database. The study database contains a single record for each study describing various study attributes, including relevant publications, sexes considered, age range, location, timing, length of follow-up, study design (prospective or intervention study, study of the general population or of patients with specified respiratory diseases, nature of the population, exclusions, study size and use of bronchodilators for measuring FEV1), availability of FEV1 results (beta, beta relative to never smokers, beta relative to continuing smokers and other indices such as beta divided by height cubed or FEV1 change as a percentage of predicted), potential confounding variables used for one or more betas, availability of results for different aspects of smoking, availability of betas stratified by sex, age and other stratifying variables, and the number of beta records in the beta database.
The beta database contains a record for each beta for each study. This record is divided into four parts. The first part gives the smoking habits at the start and end of the follow-up period classified by smoking status (never smoker, ex-smoker, current smoker, ever smoked and nonsmoker), smoking product (any, cigarettes ± other products, cigarettes only, pipes or cigars only or pipe only), cigarette type (any, manufactured only or hand-rolled only) and, where relevant, details of dose-response variables (measure of exposure and range of values, for example, 10-19 cigarettes/day). The second part of the beta record gives the sex and age of the individuals to whom the beta relates and, where applicable, details of other stratifying variables (such as baseline FEV1 level or whether histamine-responsive or not). The third part gives details of potential confounding variables taken into account when estimating the beta. The final part contains the beta data, giving the type of beta (direct, relative to never smokers or relative to continuing smokers), the value itself expressed as the decline in millilitres per year (with negative values indicating an increase) and available information relevant to the variability of the beta (the lower and upper 95% confidence interval (CI), standard deviation (SD), standard error (SE) and number of subjects the beta is based on (N)). It also contains information on how the beta was derived and the length of the period studied. Details are also entered for the reference group for betas relative to never smokers (never anything, never cigarettes) and for betas relative to continuing smokers (any product, cigarettes). Commentary also provides further detail relating to the beta where necessary.
It should be noted that the beta database contains only data relevant to betas estimated directly relative to never smokers or relative to continuing smokers. Data for indices such as FEV1 decline per year divided by height cubed or percentage change from baseline are available for very few studies, and data on FEV1 change as a percentage of predicted, though available for rather more studies, would have been difficult to use in meta-analysis because of the varying definition of the predicted value.
In some studies, the estimate of beta is given directly, but in others it was estimated by dividing the difference between FEV1 values given at the start and end of follow-up by the length of follow-up. The length of follow-up itself was not always provided precisely and sometimes had to be estimated from information given on the timing of the relevant surveys. Where necessary, betas and their SDs or SEs were estimated from data given graphically or by individual subject.
Fuller details of the variables recorded in the databases are given in Additional file 2 Data recorded.doc.
Statistical analysis
Most analyses were carried out on the basis of unweighted and inverse variance-weighted linear multiple regression analysis. For the weighted analysis, an estimate of SE was required. For some betas, the SE was given directly, and in others it could be calculated directly using standard formulae from available information on the 95% CI or on N and SD combined. For some betas, information was available on N, but not on variability (SD, SE or CI). For those betas, SE was estimated from the age-specific mean SD for those other betas where the SD was directly available. For some betas, none of N, SD, SE or CI was provided, so the SE could not be estimated, the beta not being included in the weighted analysis. In principle, the SE could have been estimated from the beta and its associated P value. However, P values were rarely available, and where provided they were not given to sufficient accuracy (for example, only as P < 0.05) to allow reasonable estimation of the SE.
The main analyses were conducted on the four smoking groups already described: never smokers, ex-smokers, quitters and continuing smokers. Estimates of beta were not included in the analysis if information on smoking habits was lacking at the start or end of follow-up if the betas related to other smoking groups (for example, never smokers at the start who smoked during follow-up) or were for smokers of pipes and/or cigars only. While multiple betas for the same smoking group and the same study could be included, provided they were independent (for example, estimates for different sexes, age groups or levels of other stratifying variables), only one beta was chosen from nonindependent alternatives. Where there was a choice, preference was given to betas based on the longest follow-up time, betas given separately by age, betas adjusted for the most variables, betas where the SE was available or could be calculated, betas based on FEV1 measurements taken without bronchodilator and for other study-specific reasons described in the Results.
Analyses were carried out using fixed-effects linear regression models to compare the four smoking groups, without adjustment for other variables, with adjustment for both sex (males, females, and sexes combined) and age (midpoint of age interval in the ranges <40, 40-49, 50-69, and 70+), and with adjustment for "block", a block being a set of betas from the same study and for the same levels of stratifying variables. Data within a block are presented on the same row in the tables presenting the beta data used in the analyses. The fixed-effects block-adjusted analyses fit a separate term for each block. The results of an alternative analysis using a random effects model in which block effects were assumed to be normally distributed are also shown.
The relationship of beta to sex, age and various other factors (length of follow-up period, continental location of the study, final follow-up year, publication year, population type and study type) was also studied using weighted and unweighted fixed-effects linear multiple regression analysis based on models including sex, age, smoking group and the factor of interest. Estimates of beta with 95% CI are presented by level of smoking group and factor. Differences between betas for smoking groups are also presented, with the significance of the difference presented as P < 0.001, P < 0.01, P < 0.05 or P ≥ 0.05. For differences between levels of the factors, only the significance level is presented.
Similar unweighted and inverse variance-weighted linear multiple regression analyses were also carried out based on differences in betas within the same block between (1) continuing smokers and quitters and (2) continuing smokers and ex-smokers. Whereas the analyses involving data from all four smoking groups test whether beta varies by other factors, such as age and sex, these analyses test whether the specified differences in beta between smoking groups varies by these factors. For the purpose of the analysis of differences, the SE of a difference was estimated as the root mean square of the SEs of the two betas concerned.
Analyses were also carried out comparing betas by amount smoked. These were restricted to betas which concerned continuing smokers, where the unit of exposure was cigarettes/day, where the subject stayed in the same exposure group between the start and end of follow-up and where preference was given to estimates adjusted for the most variables. Unweighted and inverse variance-weighted linear regression analyses related beta to cigarettes/day after adjustment for block using fixed-effects modelling. As the data for a given beta were available only for a range of cigarettes/day smoked, the value used in the regression analyses was the mean of the lower and upper limits (for example, mean 19.5 cigarettes/day for 15-24 cigarettes/day). For the highest consumption groups, which are open-ended, the mean was estimated assuming that the upper limit was 50 cigarettes/day (for example, mean 37.5 cigarettes/day for 25+ cigarettes/day).
In interpreting the analyses described above, the most importance was given to the results from the inverse variance-weighted analyses adjusted for block where relevant using fixed-effects modelling. The unadjusted analyses and those adjusted for age and sex may be somewhat biased by the fact that the results for the different smoking groups come from different sets of studies.
Some studies reported betas separately by level of other factors, each as baseline FEV1, bronchodilator responsiveness or occupational exposure. To assess whether beta was associated with the factor, the unweighted and inverse variance-weighted trends in beta (increase per level) and their SEs were estimated separately for continuing smokers, quitters, ex-smokers, for the difference between quitters and continuing smokers and for the difference between ex-smokers and continuing smokers.
The heterogeneity of beta estimates was assessed separately for the four smoking groups by an F-test comparing the between-study variance in betas with the within-study variance. To avoid complications due to the SE of beta for some studies having to be calculated indirectly, this assessment was limited to those studies where the SE was provided or could be calculated from the SD and N and where N was known.
Software
ROELEE version 3.1 software (available from P.N. Lee Statistics and Computing Ltd., Sutton, Surrey, UK) was used for entry of the data into the study and beta databases and for virtually all the statistical analyses. The data were then transferred to SAS version 9.1 software (SAS Institute Inc., Cary, NC, USA), and the analyses run on ROELEE were rerun as a cross-check. The analyses treating block as a random effect were run only in SAS.
Results
The studies
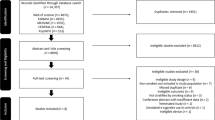
From the abstracts of the publications identified in the initial search in 2009 and the update in 2010, it was often possible to tell that no relevant data were available, and after excluding these publications, a total of 260 were examined in detail, with 96 publications finally accepted. These publications related to 47 studies. Additional file 1 FEV1 search strategy.doc, gives fuller details of the progress of the search, summarized as a flow diagram in Figure 1. Of the 47 studies finally identified, only 20 were identified directly from the initial MedLine search in 2009, with a further 11 identified from other reviews and 15 from secondary references. The updated search identified only one additional study.
Flow diagram for literature search. The diagram shows the number of papers and studies identified, examined, accepted and rejected at the different stages of the literature search. Reasons for rejection of papers are coded as follows. R1, paper unobtainable; R2, study of patients with specified conditions that are not chronic obstructive pulmonary disease; R3, study of workers in high-risk occupations; R4, study of children; R5, review paper with no new studies mentioned; R6, not a prospective study; R7, follow-up period too short (< 2 yr); R8, no follow-up data; R9, data only for FEV0.75; R10, no relevant data on FEV1 decline in those who gave up smoking. Fuller details are given in Additional file 1 FEV1 search strategy.doc.
Table 1 summarizes the details of the baseline population, exclusions, location and follow-up period of the 47 studies identified, with studies identified in 2009 numbered 1 to 46 and the study identified in 2010 numbered 47. Table 2 gives a distribution of various study characteristics. Thirty-seven studies can be broadly classified as relating to the general population (though a number of the studies excluded subjects with specified diseases), with six relating to subjects with specified respiratory diseases (or, in the case of study 37, to men with some potential risk factors for FEV1 decline). Four were intervention studies, with the presence of a specified respiratory disease being a requirement for three of these (studies 43, 44 and 46). Twenty-eight studies involved both sexes, and the remainder involved males only. Fifteen studies were restricted to relatively young people, with a maximum age at baseline of 59 years, while three studies were restricted to relatively older adults, with a minimum age at baseline of at least 60 years. Of the 44 single-country studies, 13 were conducted in the USA, 2 in Canada, 6 in the UK, 7 in Western Europe, 7 in Scandinavia, 2 in Eastern Europe, 6 in Asia and 1 in Australia. There were also three multicountry studies (studies 7, 43 and 44). Many of the studies started many years ago: 16 began in 1960-1969 and 15 began in 1970-1979. On the basis of the difference between the year of start at baseline and the year of the end of follow-up, the mean length of follow-up is estimated as 11 years, with seven studies taking at least 20 years. An attempt was made to determine, for each study, the number of individuals entering the follow-up period. This ranged from a minimum of 13 individuals in study 38 to 9,317 individuals in study 1. Twenty-one studies included at least 1,000 individuals.
Estimates of FEV1decline by smoking habit ("betas")
From the 47 selected studies, 951 beta estimates were derived. A total of 849 are direct estimates for specified smoking groups, 12 are estimates expressed relative to continuing smokers and 90 are estimates expressed relative to never smokers. For the purposes of this publication, attention is restricted to the direct estimates. This is partly because the number of direct estimates is much larger and partly because both the studies providing data relative to continuing smokers and 8 of 10 studies providing data relative to never smokers also provide direct estimates of betas. Also, though the estimates relative to never smokers can be used to estimate differences in betas between continuing smokers and those who gave up smoking (our major interest), it was not possible to estimate SDs because of the nonindependence of the betas for the two smoking groups arising from the common comparison group.
The analyses conducted are either unweighted or inverse variance-weighted. For a beta to be included in the weighted analyses, an estimate of its SE is required. This information is available directly for 173 of the 849 betas and can readily be calculated from SD and N for 205 and from the 95% CI for 44. While it was not possible to derive an estimate for 154 betas, an estimate of SE was imputed for 273 betas where only N was available using age-specific estimates of SD (52.75 for age <40, 52.11 for age 40-49, 48.97 for age 50-69 and 26.61 for age 70+) derived from those studies which did provide an estimate of SD.
Selection of betas for the main analyses comparing the four smoking groups
Of the 849 direct estimates, 97 were not considered for further analysis, as information on smoking habits was unavailable at baseline for 4 betas and at the end of follow-up for 93. Of the remaining 752 estimates, 684 relate to the major smoking groups: never smokers, ex-smokers, quitters and continuing smokers, with the remaining 68 relating to rarer or less clearly defined combinations of smoking habits, such as those who were never smokers at baseline and current smokers at follow-up or those who were current smokers at baseline and ever smokers at follow-up.
A further 173 betas were also rejected from the main analysis: 166 because they were dose-response estimates (considered separately) and 7 because the smokers were smokers of pipes and/or cigars only. This left 511 potentially useful estimates.
To avoid double-counting of nonindependent data, there was a need in certain studies for a decision to be made regarding which estimates to include in our main analysis and which to exclude. In studies 41 and 43, preference is given to betas on the basis of measurements taken without use of a bronchodilator, as this applies to most of the available data. Preference is also given to betas based on the longest available follow-up time (relevant to studies 1, 4 and 23), betas given separately by age (studies 4 and 25), betas that are adjusted for the most variables (studies 3, 13 and 46), betas from publications that provide information for all four smoking groups (studies 5, 23, 29, 31 and 45) and betas with information on N, SD or SE (study 7). Also, for study 32, preference is given to the unstratified data from the 1994 paper [4] for quitters and to the data stratified by airway responsiveness from the 1995 paper [5] for the other smoking groups, as the later source did not give data for quitters. For study 47, preference is given to the data unstratified for healthy versus unhealthy status, as stratified results were available only for current smokers.
The betas and SEs used in the main analyses are shown in Table 3. These relate to only 39 of the 47 studies, with two studies (8 and 33) providing only estimates relative to never smokers and six studies (11, 14-16, 24 and 40) having incomplete information on smoking habits. For some studies, data are not available for all four smoking groups, notably for study 25, where only data for never smokers are available, data for continuing smokers being classified by amount smoked and for those who gave up being for ex-smokers and quitters combined. Studies 37, 46 and 47 also have data only for ex-smokers and quitters combined. It should be noted that for study 29, the age-specific data which have no SEs are used in the unweighted analyses, but the ages combined data, which do have SEs, are used in the weighted analyses. SEs are available for all other estimates except for those for never smokers and ex-smokers in study 45. There are a total of 303 estimates of beta in Table 3 with 295 being available for unweighted analyses (all except the eight estimates for ages 25-74 for study 29) and 261 being available for weighted analyses (all except the 40 estimates in study 29 and the 2 estimates in study 45 without SEs).
Comparison of betas in the four smoking groups
Table 4 compares betas in the four smoking groups based on unweighted and inverse variance-weighted analysis. The results are shown without adjustment, with adjustment for age and sex and with adjustment for block. Each row of data in Table 3 is a block, and the block-adjusted analysis attempts to adjust simultaneously for all the factors fixed in the study design and by the choice of subgroup for analysis. Adjustment for age and sex reduces the residual variance by 27.4% in the unweighted analysis and by 30.6% in the weighted analysis, while adjustment for block reduced it by 76.9% in the unweighted analysis and by 78.1% in the weighted analysis.
The results consistently show a lower beta in never smokers than in continuing smokers (P < 0.001) with the difference estimated as 10.8 mL/yr (95% CI, 8.9 to 12.8) in the weighted, block-adjusted analysis and over 10 mL/yr in all the other analyses. Ex-smokers also show a beta that is consistently less than that in continuing smokers (P < 0.001 in all analyses), with the estimated difference (12.4 mL/yr; 95% CI, 10.1 to 14.7, in the weighted, block-adjusted analysis) again always over 10 mL/yr. Betas for ex-smokers and never smokers do not vary significantly in any of the analyses. Betas for quitters lie between those for continuing smokers and never smokers in all the analyses, consistent with the quitters' having smoked for only part of the follow-up period. In the weighted, block-adjusted analysis, beta is estimated to be 8.5 mL/yr (95% CI, 5.6 to 11.4) less in quitters than in continuing smokers (P < 0.001) and 2.4 mL/yr (95% CI, -0.4 to 5.1) more in quitters than in never smokers.
In the text above, the block-adjusted results cited are those based on fixed-effects modelling. As is evident from Table 4 the alternative analyses using random-effects modelling produced virtually identical beta estimates to those using fixed-effects modelling. Though the CIs using random-effects modelling are somewhat wider, the interpretation of the data is unaffected, with betas for continuing smokers clearly greater (P < 0.001) than those in the other three groups, which do not differ significantly.
Similar conclusions were also reached using block-adjusted analyses (fixed effects or random effects) which were run excluding those betas where only beta and N were available, and the SE was imputed from age-specific estimates of SD derived from other studies (data not shown).
Two sets of additional analyses corresponding to those in Table 4 but differing in the betas included, were also conducted. The additional weighted analyses were based on those 253 betas used in the unweighted analyses presented in Table 4 that had SEs, and the additional unweighted analyses were based on the 261 betas used in the weighted analyses in Table 4. The results (not shown) were very similar to those shown in Table 4 with mean betas lowest (and similar) in never smokers and ex-smokers, highest in continuing smokers and intermediate in quitters.
Heterogeneity of betas
The ratio of between-study to within-study variance in betas was estimated as 11.94 for never smokers (P < 0.001), 15.51 for continuing smokers (P < 0.001), 9.84 for quitters (P < 0.01) and 1.32 (NS) for ex-smokers. These ratios were based on, respectively, those 28, 30, 27 and 24 beta estimates considered in the main analyses for which information was available on N and also either SE or SD.
Relationship of beta to age, sex and study characteristics
Table 5 gives the results of analyses relating beta to age, sex and various study characteristics. Note that as some betas were for the sexes combined, the parameter of sex has three levels (males, females, and both). In the inverse variance-weighted analysis, betas are clearly lower in females (compared to both males and the sexes combined) and are lower at age <40 years and age 70+ years than at ages 40-49 and 50-59 years. After adjustment for age, sex and smoking group, no significant association is seen with population type or study type. There is evidence that betas are somewhat greater in studies in Europe than in North America and in studies where the final follow-up year and publication year were 1980 or later. In the unweighted analyses, there are again associations with age, sex, continental location of study and final follow-up year, but the association with publication year is no longer significant.
Although Table 5 provides evidence of variation in beta by sex, age and other study characteristics, it was clear from inspection of the SDs in the various regression models that none of these characteristics could explain more than a small part of the between-study heterogeneity noted above (data not shown).
Differences in betas between continuing smokers and those who gave up smoking
The data in Table 3 allow the calculation of 63 within-block differences in beta between continuing smokers and quitters and 60 within-block differences between continuing smokers and ex-smokers. Of the 123 differences, 21 have no SE (20 in study 29 and 1 in study 45), so these data could not be used in weighted analyses. The mean difference between continuing smokers and quitters is estimated as 11.2 mL/yr (95% CI, 7.0 to 15.3), based on unweighted analysis of 61 betas, and 7.1 mL/yr (95% CI, 4.7 to 9.6) based on weighted analysis of 53 betas, while the difference between continuing smokers and ex-smokers is estimated as 14.9 mL/yr (95% CI, 11.5 to 18.3) based on unweighted analysis of 58 betas and as 12.3 mL/yr (95% CI, 8.7 to 16.0) based on weighted analyses of 49 betas.
Variation by age, sex and study characteristics in differences in beta between continuing smokers and those who gave up smoking
There is little consistent evidence that differences in beta between continuing smokers and those who gave up smoking vary meaningfully by age (adjusted for sex) or sex (adjusted for age). There is significant variation by sex (P < 0.001) in the differences in betas between continuing smokers and ex-smokers in both the unweighted and inverse variance-weighted analyses, but these differences are due to larger differences where estimates are for the sexes combined, with five of the seven estimates deriving from one study (43). No significant variation is seen by sex in the difference in beta between continuing smokers and quitters. Variation by age (P < 0.001) in the difference in beta between continuing smokers and ex-smokers is seen in the weighted analyses, but this does not follow any trend, with the differences being larger for ages 40-49 (18.7 mL/yr, based on n = 12 betas) and ages 50-69 (14.5 mL/yr, n = 23) than for ages <40 (6.3 mL/yr, n = 6) and ages 70+ (9.9 mL/yr, n = 8), and is not evident in the unweighted analyses. Variation by age is also evident for the difference between continuing smokers and quitters, but this is evident only in the unweighted analyses (P < 0.001), with differences being larger for ages <40 (28.2 mL/yr, n = 10) than for ages 40-49 (7.8 mL/yr, n = 17), ages 50-69 (10.2 mL/yr, n = 25) or ages 70+ (1.1 mL/yr, n = 9).
After adjustment for age and sex, there is little evidence of variation in either difference by length of follow-up period, continental location of study, final follow-up year, year of publication or study type. There is, however, a consistent tendency for the difference to be greater where the estimates relate to patients with specific respiratory diseases than where they relate to the general population. For the difference between continuing smokers and quitters, the excess difference associated with having respiratory disease is 21.6 mL/yr (P < 0.05) in unweighted analyses (using 61 betas, with 3 relating to subjects with respiratory disease) and 31.3 mL/yr (P < 0.05) in inverse variance-weighted analyses (using 53 betas, 3 for subjects with respiratory disease). For the difference between continuing smokers and ex-smokers, the excess is 12.3 mL/yr (P < 0.05) in unweighted analyses (using 58 betas, 8 for subjects with respiratory disease) and 4.8 mL/yr (not significant) in weighted analyses (using 49 betas, 8 for subjects with respiratory disease).
Relationship of beta to amount smoked in continuing smokers
As noted above, 166 of the estimates of beta relate to dose-response relationships. Table 6 presents the data for those 74 estimates which concern continuing smokers, where the unit of exposure is cigarettes per day and where the subjects stayed in the same exposure group between the start and end of follow-up. Eighteen estimates were excluded because they concerned quitters, and 44 were excluded because the unit of exposure was not cigarettes per day or the level of exposure was undefined at follow-up. Of the remaining 104 estimates, 30 were excluded and of those, 12 were excluded because the level of exposure differed between start and follow-up and 18 were excluded (in studies 13 and 31) as preference was given to estimates adjusted for the most variables. Of the 74 betas shown, 36 are from study 29, with 30 individual age betas without CI and 6 combined age estimates with CI. CIs are available for all the other 38 estimates derived from 6 studies. There are 26 "blocks" of independent dose-response relationships.
Some dose relationships are evident from inspection, with the betas being higher for the highest consumption than for the lowest consumption in every block, except for one block where the betas are the same. After adjustment for block, the estimated increase in beta per cigarette per day is 0.33 (95% CI, 0.22 to 0.44) in unweighted analysis based on 68 betas and 0.33 (95% CI, 0.20 to 0.45) in inverse variance-weighted analysis based on 44 betas.
Relationship of some other factors to beta and differences in betas between smoking groups
A number of the studies present betas separately by level of factors other than age, sex or study characteristics. Table 7 summarizes trends in beta by level for those factors for which data were available for continuing smokers and also for quitters and/or ex-smokers. With the notable exception of study 4, which reports a strong tendency for beta to decline with reducing FEV1, both in continuing smokers and quitters, the results from studies 5, 13 and 45 are consistent in demonstrating a strong tendency for betas in all three smoking groups to be greater where there is evidence of reduced lung function as determined by low FEV1, forced vital capacity (FVC) or presence of mild obstruction. The trend in betas is generally greater in continuing smokers than in quitters or ex-smokers, though the difference in trends between continuing smokers and either quitters or ex-smokers is significant in only one case: study 5, in which a marked trend is seen in continuing smokers, but no trend is seen in ex-smokers.
There is also evidence from study 43 that, in continuing smokers, beta increases with increasing number of doctor visits for lower respiratory infection. Though no such increase is seen in ex-smokers, the difference in trends is not statistically significant.
No clear evidence of an association with betas within or between smoking groups is evident in respect of respiratory symptoms at baseline (study 29), bronchodilator responsiveness (studies 34 and 35) or histamine responsiveness (study 32). The results from study 7 also do not suggest any marked relationship of beta to occupational exposure, though lack of SEs limits detailed interpretation.
Discussion
A major objective of our review is to quantify and compare the rate of FEV1 decline (beta) in those who continue to smoke (continuing smokers) and those who give up smoking (quitters and ex-smokers). In an ideal world, this review would involve a number of large studies in which smoking habits, FEV1 levels and relevant confounding variables were measured at regular intervals and in which betas could be assessed separately for continuing smokers and for those who gave up, by time quit, on the basis of recently recorded smoking data. One could then distinguish between alternative possible models for FEV1 decline. For example, it might be that, following giving up smoking (and not subsequently restarting), the rate of decline in FEV1 drops immediately to a lower level than that of continuing smokers and continues at this level. Alternatively, it might be that, on giving up smoking, the rate of decline drops only slightly at first but then increases over time until it reaches a fixed level. The theory suggested by Fletcher and Peto [6] implies that the first situation may obtain, but there are few studies which present data in enough detail to distinguish such alternatives.
Anthonisen et al. [7], on the basis of a randomized clinical trial of smoking intervention (The Lung Health Study, study 43), did present a figure that suggests that giving up smoking leads to a reduced (and constant) beta quite quickly, though their study also suggests that in the first year or so after giving up, FEV1 levels may actually increase slightly. However, such data seem extremely rare, and the studies considered here include many in which FEV1 was recorded at only two time points, and some where, despite FEV1 being recorded at multiple time points, the data presented relate only to the average beta over the whole follow-up period. Studies where results are presented for more than one time period are relatively rare, and some of these studies do not adequately characterize smoking status at the beginning and end of each period studied. To allow assessment of FEV1 decline from a reasonable number of studies, therefore, we have summarized the data relating to the experience of a smoking group over a defined period, with the key information recorded being the smoking habits of that group at the beginning and end of the period and the beta estimated over the period studied. While the limitations of the available data mean that we cannot estimate the exact shape of the decline in FEV1 over time, our approach (which implicitly assumes a linear decline) is supported by the lack of relationship noted between beta and length of follow-up period (see Table 5).
Before discussing the results obtained, some other limitations of the data should be noted. Many of the 47 studies with relevant data are old, with 16 starting before 1970 and 42 beginning before 1990, and almost half of the studies provided data only for men. A number of the studies are quite small, with nine involving less than 100 individuals, implying very limited numbers in some of the smoking groups. In many of the studies, there was no adjustment for any variables, not even age or height. Smoking habits were not always defined at both the beginning and end of the time interval studied. FEV1 results were virtually never recorded after bronchodilator therapy as recommended for the diagnosis of COPD [8, 9]. For many of the studies, estimates of the variability of the betas are not available, though for some estimates, the variability could be derived on the basis of SD estimates for other studies and knowledge of sample size. There are very limited data on how betas for a given smoking group vary by other factors of interest, as is evident from Table 7. It should also be pointed out that although there is a reasonable amount of information on how beta varies by amount smoked per day in continuing smokers (see Table 6), there are no such data for those who give up smoking. Also, comparisons of continuing smokers with quitters or ex-smokers are very often unadjusted for the amount smoked per day at the time when the quitters or ex-smokers were still smoking. We have not attempted to assess the individual studies for quality and susceptibility to bias, partly because there are no generally recognized methods for doing so for observational epidemiological studies, partly because a one-dimensional score for a study cannot really adequately summarize the multiple facets of its quality, and partly as differentially weighting (or rejecting) results from different studies based on an inevitably subjective score is always contentious, perhaps especially so when the study was supported by the tobacco industry.
Another possible limitation of our work concerns the completeness of our database, given the difficulty of being certain that all the relevant literature has been obtained, particularly when studies have been conducted over such a long period and given that some studies which clearly have the ability to provide relevant results seem never to have published findings in an appropriate format.
Despite all these limitations, we believe that the database assembled is of value in assessing the relationship of smoking habits, and particularly giving up smoking, to the magnitude of beta. A number of main conclusions can be drawn from our analyses.
First, beta in never smokers is clearly less than that in continuing smokers. The results summarized in Table 4 suggest that, whereas beta in continuing smokers is over 40 mL/yr, it is less than 30 mL/yr in never smokers. The difference exceeds 10 mL/yr and is highly significant (P < 0.001) in all the analyses shown. Though there is variation between blocks (that is, rows of Table 3) in the level of betas, the higher betas in continuing smokers is evident in virtually every block.
It is also clear that betas in ex-smokers, who gave up before the start of the period over which the FEV1 was measured, are quite similar to those in never smokers. In the inverse variance-weighted analyses adjusted for block, beta was estimated as 27.6 mL/yr, a nonsignificant 1.6 mL/yr lower than the estimate of 29.2 mL/yr for never smokers. Estimates for quitters (31.6 mL/yr for the same analyses) tend to be somewhat higher than for never smokers or ex-smokers, but are clearly lower than those in continuing smokers. Though variability in the estimates does not make the intermediate position of quitters well-defined, the results can plausibly be explained by the quitters having smoked for part of the period during which the betas were estimated. Data were not available to relate time of quitting to beta.
Our analyses also show that, in continuing smokers, there is a clear dose relationship with amount smoked, with an increase in beta of 0.33 mL/yr per cigarette/day. Though the data are relatively limited, they are consistent in showing a beta greater in the heaviest smokers than in the lightest smokers.
Four of the studies (4, 5, 13 and 45) provide information relating beta to smoking group by level of lung function, as determined by FEV1, FEV1/FVC or presence of mild obstruction. Studies 5, 13 and 45 present results which seem consistent with what has been termed the "horse-racing effect" [6, 10], whereby reduced lung function predicts a rapid rate of decline simply because the rapid decline produced the reduced level of lung function in the first place. However, study 4 presents results which seem totally inconsistent with this finding, particularly in comparison with study 13. The results shown in Table 7 for this study are for the first 2 years follow-up, as SEs could not be derived for the full 6 years of follow-up. Though the strong tendency for betas to be higher in continuous smokers and quitters with a high baseline FEV1 seen in the first 2 years of follow-up seems not so marked for the full 6 years follow-up (see Table 5 of the source paper [11]), there is still no evidence of the horse-racing effect, as the authors note. Why this inconsistency is seen is not clear.
In all four studies, the trend in beta in relation to reduced lung function is weaker in quitters and ex-smokers than in continuing smokers. However, only in study 5, where a tendency for low baseline FEV1/FVC to predict an increased beta is clearly evident in continuing smokers but not evident in ex-smokers, is the difference from continuing smokers significant at P < 0.05.
The other factors considered in Table 7 (doctor visits for lower respiratory infection, bronchodilator responsiveness, histamine responsiveness and various aspects of occupational exposure) generally show no relationship with beta in continuing smokers, quitters or ex-smokers or with the difference in beta between continuing smokers and the other two smoking groups. The only exception was the significant tendency for beta in continuing smokers to increase with doctor visits. The evidence for each of these factors is very limited, each coming from a single study. While there do not appear to be other studies that allow assessment of differences in trends between continuing smokers and quitters or ex-smokers, it is possible that additional studies may provide evidence for the association in smokers or in the whole population, regardless of smoking habits. Because this review is mainly concerned with the study of effects of giving up smoking, we did not consider studies which did not report results for quitters or ex-smokers.
The same applies to the study characteristics considered in Table 5. Had we been specifically trying to answer the question whether beta varies by age or sex, much additional literature would have been considered. Of more interest is whether these study characteristics are related to the difference in betas between continuing smokers and quitters or ex-smokers. The main finding here is that the difference in betas between continuing smokers and quitters is greater where the estimates relate to individuals with specific respiratory diseases than when they relate to the general population. This is consistent with the theory that a susceptible proportion of smokers suffer a more rapid decline in lung function than do other smokers or those who have given up smoking. This susceptible proportion would be more likely both to have reduced lung function and be diagnosed with respiratory disease [6]. Other than having a greater beta, having reduced lung function, and being more likely to be diagnosed as having COPD, our review does not cast any light on characteristics linked to susceptibility in smokers.
For the purposes of designing a study comparing smokers and users of new-generation nicotine delivery products, it would be useful to know the level of decline in FEV1 one would expect over a defined time period in continuing smokers and those who give up smoking. Our analyses, presenting the results in terms of average FEV1 decline per year (beta) assume that the rate of decline is approximately constant over time, an assumption which is supported by the analyses presented in Table 5. Though this analysis is uncertain, being ecological in nature (as the relationship of beta to length of follow-up is evaluated only between studies), the strength of the association is clearly not strong. This suggests that our estimates of beta, based on 39 studies with an average follow-up period of 9 years, can be taken to apply both to short-term studies of say 5 years and to longer-term studies of, say, 15 years. It would seem reasonable to design a study comparing FEV1 declines in continuing smokers of conventional cigarettes and switchers to new products, assuming that beta reduces a somewhat conservative 10 mL/yr on quitting and that it reduces by perhaps 8 or 9 mL/yr in the switchers, provided that there is good toxicological evidence that these new products have little or no respiratory effect. For a 5-year study, we estimate that a comparison of continuing smokers and switchers would require about 120 smokers per group to have 80% power to detect a difference of 8 mL/yr at the P < 0.05 significance level, assuming participants do not change their smoking habits and ignoring dropouts. To detect a difference of 9 mL/yr would require about 95 smokers per group.
Conclusions
While the available data have a number of limitations, it is possible to draw a number of conclusions relating to the annual rate of FEV1 loss (beta) in continuing smokers, quitters, ex-smokers and never smokers. Continuing smokers have a beta that is clearly greater, by more than 10 mL/yr, than in never smokers and is positively related to the number of cigarettes smoked per day. Betas in ex-smokers are similar to those in never smokers, and betas in quitters are only slightly greater. There is no clear evidence that differences in betas between continuing smokers and those who have given up smoking depend on age or sex, but differences are greater in studies of populations with respiratory disease than in general population studies. Some, but not all, studies suggest that betas are greater in those with reduced lung function, particularly in continuing smokers.
Abbreviations
- CI:
-
confidence interval
- COPD:
-
chronic obstructive pulmonary disease
- FEV1 :
-
forced expiratory volume in 1 second (mL/yr)
- FVC:
-
forced vital capacity
- N :
-
number of subjects
- SD:
-
standard deviation
- SE:
-
standard error.
References
International Agency for Research on Cancer (IARC): IARC Handbooks of Cancer Prevention, Tobacco Control, Reversal of Risk After Quitting Smoking. 2007, Lyon, France: IARC, 11.
US Surgeon General: The Health Consequences of Smoking: A Report of the Surgeon General. 2004, Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, Accessed 22 November 2010, [http://www.surgeongeneral.gov/library/reports/index.html]
Willemse BWM, Postma DS, Timens W, Ten Hacken NHT: The impact of smoking cessation on respiratory symptoms, lung function, airway hyperresponsiveness and inflammation. Eur Respir J. 2004, 23: 464-476. 10.1183/09031936.04.00012704.
Xu X, Weiss ST, Rijcken B, Schouten JP: Smoking, changes in smoking habits, and rate of decline in FEV1: new insight into gender differences. Eur Respir J. 1994, 7: 1056-1061. 10.1183/09031936.94.07030477.
Rijcken B, Schouten JP, Xu X, Rosner B, Weiss ST: Airway hyperresponsiveness to histamine associated with accelerated decline in FEV1. Am J Respir Crit Care Med. 1995, 151: 1377-1382.
Fletcher C, Peto R, Tinker C, Speizer FE: The Natural History of Chronic Bronchitis and Emphysema: An Eight-Year Study of Early Chronic Obstructive Lung Disease in Working Men in London. 1976, Oxford, UK, New York, and Toronto: Oxford Univ. Press
Anthonisen NR, Connett JE, Kiley JP, Altose MD, Bailey WC, Buist AS, Conway WA, Enright PL, Kanner RE, O'Hara P, et al: Effects of smoking intervention and the use of an inhaled anticholinergic bronchodilator on the rate of decline of FEV1. The Lung Health Study. JAMA. 1994, 272: 1497-1505. 10.1001/jama.272.19.1497.
Pauwels R, Buist A, Calverley P, Kenkins C, Hurd S: Global strategy for the diagnosis, management, and prevention of global initiative for chronic obstructive lung disease. NHLBI/WHO global initiative for chronic obstructive lung disease (GOLD) workshop summary. Am J Respir Crit Care Med. 2001, 163: 1256-1276.
Global Initiative for Chronic Obstructive Disease: Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. 2006. Executive Summary. 2006, Medical Communications Resources Inc., Gig Harbor, WA, USA, (Revised 2006). Accessed 22 November 2010, [http://www.goldcopd.org/]
Burrows B, Knudson RJ, Camilli AE, Lyle SK, Lebowitz MD: The "horse-racing effect" and predicting decline in forced expiratory volume in one second from screening spirometry. Am Rev Respir Dis. 1987, 135: 788-793.
Burchfiel CM, Marcus EB, Curb JD, MacLean CJ, Vollmer WM, Johnson LR, Fong KO, Rodriguez BL, Masaki KH, Buist AS: Effects of smoking and smoking cessation on longitudinal decline in pulmonary function. Am J Respir Crit Care Med. 1995, 151: 1778-1785.
Bartholomew HC, Knuiman MW: Longitudinal analysis of the effect of smoking cessation on cardiovascular risk factors in a community sample: the Busselton Study. J Cardiovasc Risk. 1998, 5: 263-271. 10.1097/00043798-199808000-00009.
James AL, Palmer LJ, Kicic E, Maxwell PS, Lagan SE, Ryan GF, Musk AW: Decline in lung function in the Busselton Health Study: the effects of asthma and cigarette smoking. Am J Respir Crit Care Med. 2005, 171: 109-114. 10.1164/rccm.200402-230OC.
Beck GJ, Doyle CA, Schachter EN: A longitudinal study of respiratory health in a rural community. Am Rev Respir Dis. 1982, 125: 375-381.
Bossé R, Sparrow D, Garvey AJ, Costa PT, Weiss ST, Rowe JW: Cigarette smoking, aging, and decline in pulmonary function: a longitudinal study. Arch Environ Health. 1980, 35: 247-252.
Bossé R, Sparrow D, Rose CL, Weiss ST: Longitudinal effect of age and smoking cessation on pulmonary function. Am Rev Respir Dis. 1981, 123: 378-381.
Gottlieb DJ, Sparrow D, O'Connor GT, Weiss ST: Skin test reactivity to common aerollergens and decline of lung function. The Normative Aging Study. Am J Respir Crit Care Med. 1996, 153: 561-566.
Sparrow D, Rosner B, Cohen M, Weiss ST: Alcohol consumption and pulmonary function: a cross-sectional and longitudinal study. Am Rev Respir Dis. 1983, 127: 735-738.
Sparrow D, Glynn RJ, Cohen M, Weiss ST: The relationship of the peripheral leukocyte count and cigarette smoking to pulmonary function among adult men. Chest. 1984, 86: 383-386. 10.1378/chest.86.3.383.
Sparrow D, O'Connor GT, Rosner B, Demolles D, Weiss ST: A longitudinal study of plasma cortisol concentration and pulmonary function decline in men. The Normative Aging Study. Am Rev Respir Dis. 1993, 147: 1345-1348.
Camilli AE, Burrows B, Knudson RJ, Lyle SK, Lebowitz MD: Longitudinal changes in forced expiratory volume in one second in adults: effects of smoking and smoking cessation. Am Rev Respir Dis. 1987, 135: 794-799.
Chambers DC, Boldy DAR, Ayres JG: Chronic respiratory symptoms, von Willebrand factor and longitudinal decline in FEV1. Respir Med. 1999, 93: 726-733. 10.1016/S0954-6111(99)90040-9.
Chinn S, Jarvis D, Melotti R, Luczynska C, Ackermann-Liebrich U, Antó JM, Cerveri I, de Marco R, Gislason T, Heinrich J, Janson C, Künzli N, Leynaert B, Neukirch F, Schouten J, Sunyer J, Svanes C, Vermeire P, Wjst M, Burney P: Smoking cessation, lung function, and weight gain: a follow-up study. Lancet. 2005, 365: 1629-1635. 10.1016/S0140-6736(05)66511-7.
Sunyer J, Zock JP, Kromhout H, Garcia-Esteban R, Radon K, Jarvis D, Toren K, Künzli N, Norbäck D, d'Errico A, Urrutia I, Payo F, Olivieri M, Villani S, Van Sprundel M, Antó JM, Kogevinas M, Occupational Group of the European Community Respiratory Health Survey: Lung function decline, chronic bronchitis, and occupational exposures in young adults. Am J Respir Crit Care Med. 2005, 172: 1139-1145. 10.1164/rccm.200504-648OC.
Clément J, van de Woestijne KP: Rapidly decreasing forced expiratory volume in one second or vital capacity and development of chronic airflow obstruction. Am Rev Respir Dis. 1982, 125: 553-558.
Comstock GW, Brownlow WJ, Stone RW, Sartwell PE: Cigarette smoking and changes in respiratory findings. Arch Environ Health. 1970, 21: 50-57.
Corbin RP, Loveland M, Martin RR, Macklem PT: A four-year follow-up study of lung mechanics in smokers. Am Rev Respir Dis. 1979, 120: 293-304.
Eriksson S, Lindell SE, Wiberg R: Effects of smoking and intermediate α1-antitrypsin deficiency (PiMZ) on lung function. Eur J Respir Dis. 1985, 67: 279-285.
Ferris BG, Chen H, Puleo S, Murphy RLH: Chronic nonspecific respiratory disease in Berlin, New Hampshire, 1967 to 1973: a further follow-up study. Am Rev Respir Dis. 1976, 113: 475-485.
Fletcher CM, Peto R, Speizer FS, Tinker CM: A follow-up study of the natural history of obstructive bronchitis. Bronchitis III, Proceedings of the Third International Symposium on Bronchitis at Groningen, The Netherlands, 23-26 September 1969. Edited by: Orie NGM, van der Lende R. 1970, Royal Vangorcum, Assen, The Netherlands, and Charles C Thomas, Springfield, IL, USA, 103-116.
Fletcher C, Peto R: The natural history of chronic airflow obstruction. Br Med J. 1977, 1: 1645-1648. 10.1136/bmj.1.6077.1645.
Frew AJ, Kennedy SM, Chan-Yeung M: Methacholine responsiveness, smoking, and atopy as risk factors for accelerated FEV1 decline in male working populations. Am Rev Respir Dis. 1992, 146: 878-883.
Górecka D, Czernicka-Cierpisz E: Wpływ palenia tytoniu na czynnoś#263; płuc u pracowników Instytutu Grużlicy i Chorób Płuc w Warszawie (Effect of smoking or respiratory function of employees of the Institute of Tuberculosis and Lung diseases in Warsaw). Pneumonol Alergol Pol. 1992, 60: 47-53.
Griffith KA, Sherrill DL, Siegel EM, Manolio TA, Bonekat HW, Enright PL: Predictors of loss of lung function in the elderly. The Cardiovascular Health Study. Am J Respir Crit Care Med. 2001, 163: 61-68.
Huhti E, Ikkala J: A 10-year follow-up study of respiratory symptoms and ventilatory function in a middle-aged rural population. Eur J Respir Dis. 1980, 61: 33-45.
Humerfelt S, Gulsvik A, Skjaerven R, Nilssen S, Kvåle G, Sulheim O, Ramm E, Eilertsen E, Humerfelt SB: Decline in FEV1 and airflow limitation related to occupational exposures in men of an urban community. Eur Respir J. 1993, 6: 1095-1103.
Katoh T, Ohmori H, Nakao H, Kuroda Y, Imai H, Maehara M, Kai M, Tsunetoshi Y: Effects of smoking on pulmonary function: a cross-sectional and longitudinal study. J UOEH. 2001, 23: 403-409.
Kauffmann F, Drouet D, Lellouch J, Brille D: Twelve years spirometric changes among Paris area workers. Int J Epidemiol. 1979, 8: 201-212. 10.1093/ije/8.3.201.
Kauffmann F, Querleux E, Drouet D, Lellouch J, Brille D: Évolution du VEMS en 12 ans et tabagisme chez 556 travailleurs de la régionne parisienne (Twelve year FEV1 changes and smoking habits among 556 workers in the Paris area). Bull Euop Physiopath Respir. 1979, 15: 723-737.
Kauffmann F, Annesi I, Chwalow J: Validity of subjective assessment of changes in respiratory health status: a 30 year epidemiological study of workers in Paris. Eur Respir J. 1997, 10: 2508-2514. 10.1183/09031936.97.10112508.
Krzyzanowski M, Jedrychowski W, Wysocki M: Factors associated with change in ventilatory function and the development of chronic obstructive pulmonary disease in a 13-year follow-up of the Cracow study. Risk of chronic obstructive pulmonary disease. Am Rev Respir Dis. 1986, 134: 1011-1019.
Lange P, Groth S, Nyboe J, Mortensen J, Appleyard M, Jensen G, Schnohr P: Effects of smoking and changes in smoking habits on the decline of FEV1. Eur Respir J. 1989, 2: 811-816.
Vestbo J, Lange P: The effect of smoking cessation on FEV1 is modified by the presence of chronic mucus hypersecretion [Abstract]. Am J Respir Crit Care Med. 1994, 149: A394.
Taylor RG, Joyce H, Gross E, Holland F, Pride NB: Bronchial reactivity to inhaled histamine and annual rate of decline in FEV1 in male smokers and ex-smokers. Thorax. 1985, 40: 9-16. 10.1136/thx.40.1.9.
Lim TK, Taylor RG, Watson A, Joyce H, Pride NB: Changes in bronchial responsiveness to inhaled histamine over four years in middle aged male smokers and ex-smokers. Thorax. 1988, 43: 599-604. 10.1136/thx.43.8.599.
Watson A, Joyce H, Hopper L, Pride NB: Influence of smoking habits on change in carbon monoxide transfer factor over 10 years in middle aged men. Thorax. 1993, 48: 119-124. 10.1136/thx.48.2.119.
Watson A, Joyce H, Pride NB: Changes in carbon monoxide transfer over 22 years in middle-aged men. Respir Med. 2000, 94: 1103-1108. 10.1053/rmed.2000.0920.
Liu C, Wang D: Follow-up study of lung function changes for 10 years in healthy elder of ex-smokers. Zhonghua Jie He He Hu Xi Za Zhi (Chinese Journal of Tuberculosis and Respiratory Diseases). 1999, 22: 677-679.
Olofsson J, Bake B, Svärdsudd K, Skoogh BE: The single breath N2-test predicts the rate of decline in FEV1. The study of men born in 1913 and 1923. Eur J Respir Dis. 1986, 69: 46-56.
Omori H, Nonami Y, Morimoto Y: Effect of smoking on FEV1 decline in a cross-sectional and longitudinal study of a large cohort of Japanese males. Respirology. 2005, 10: 464-469. 10.1111/j.1440-1843.2005.00727.x.
Sandvik L, Erikssen G, Thaulow E: Long term effects of smoking on physical fitness and lung function: a longitudinal study of 1393 middle aged Norwegian men for seven years. BMJ. 1995, 311: 715-718.
Sato K, Kioi S, Arakawa M: Effect of smoking on the decline in forced expiratory volume in one second. Nihon Kyobu Shikkan Gakkai Zasshi. 1997, 35: 288-293.
Sherman CB, Xu X, Speizer FE, Ferris BG, Weiss ST, Dockery DW: Longitudinal lung function decline in subjects with respiratory symptoms. Am Rev Respir Dis. 1992, 146: 855-859.
Xu X, Dockery DW, Ware JH, Speizer FE, Ferris BG: Effects of cigarette smoking on rate of loss of pulmonary function in adults: A longitudinal assessment. Am Rev Respir Dis. 1992, 146: 1345-1348.
Soejima K, Yamaguchi K, Kohda E, Takeshita K, Ito Y, Mastubara H, Oguma T, Inoue T, Okubo Y, Amakawa K, Tateno H, Shiomi T: Longitudinal follow-up study of smoking-induced lung density changes by high-resolution computed tomography. Am J Respir Crit Care Med. 2000, 161: 1264-1273.
Tashkin DP, Clark VA, Coulson AH, Simmons M, Bourque LB, Reems C, Detels R, Sayre JW, Rokaw SN: The UCLA population studies of chronic obstructive respiratory disease. VIII. Effects of smoking cessation on lung function: a prospective study of a free-living population. Am Rev Respir Dis. 1984, 130: 707-715.
Tashkin DP, Detels R, Simmons M, Liu H, Coulson AH, Sayre J, Rokaw S: The UCLA population studies of chronic obstructive respiratory disease. XI: Impact of air pollution and smoking on annual change in forced expiratory volume in one second. Am J Respir Crit Care Med. 1994, 149: 1209-1217.
Van der Lende R, Kok TJ, Peset Reig R, Quanjer PH, Schouten JP, Orie NGM: Decreases in VC and FEV1 with time: indicators for effects of smoking and air pollution. Bull Eur Physiopath Respir. 1981, 17: 775-792.
Villar MTA, Dow L, Coggon D, Lampe FC, Holgate ST: The influence of increased bronchial responsiveness, atopy, and serum IgE on decline in FEV1: a longitudinal study in the elderly. Am J Respir Crit Care Med. 1995, 151: 656-662.
Vollmer WM, Johnson LR, Buist AS: Relationship of response to a bronchodilator and decline in forced expiratory volume in one second in population studies. Am Rev Respir Dis. 1985, 132: 1186-1193.
Wilhelmsen L, Orha I, Tibblin G: Decrease in ventilatory capacity between ages of 50 and 54 in representative samples of Swedish men. Br Med J. 1969, 3: 553-556. 10.1136/bmj.3.5670.553.
Kohansal R, Martinez-Camblor P, Agusti A, Buist AS, Mannino DM, Soriano JB: The natural history of chronic airflow obstruction revisited: an analysis of the Framingham offspring cohort. Am J Respir Crit Care Med. 2009, 180: 3-10. 10.1164/rccm.200901-0047OC.
Annesi I, Oryszczyn MP, Frette C, Neukirch F, Orvoen-Frija E, Kauffmann F: Total circulating IgE and FEV1 in adult men. An epidemiologic longitudinal study. Chest. 1992, 101: 642-648. 10.1378/chest.101.3.642.
Demedts M: Early emphysema. Ten years' evolution. Chest. 1988, 94: 337-342. 10.1378/chest.94.2.337.
Grol MH, Gerritsen J, Vonk JM, Schouten JP, Koëter GH, Rijeken B, Postma DS: Risk factors for growth and decline of lung function in asthmatic individuals up to age 42 years. Am J Respir Crit Care Med. 1999, 160: 1830-1837.
Howard P: The changing face of chronic bronchitis with airways obstruction. Br Med J. 1974, 2: 89-93. 10.1136/bmj.2.5910.89.
Hughes JA, Hutchison DCS, Bellamy D, Dowd DE, Ryan KC, Hugh-Jones P: The influence of cigarette smoking and its withdrawal on the annual change of lung function in pulmonary emphysema. Q J Med. 1982, 51: 115-124.
Postma DS, de Vries K, Koëter GH, Sluiter HJ: Independent influence of reversibility of air-flow obstruction and nonspecific hyperreactivity on the long-term course of lung function in chronic air-flow obstruction. Am Rev Respir Dis. 1986, 134: 276-280.
Scanlon PD, Connett JE, Waller LA, Altose MD, Bailey WC, Buist AS, Tashkin DP: Smoking cessation and lung function in mild-to-moderate chronic obstructive pulmonary disease. The Lung Health Study. Am J Respir Crit Care Med. 2000, 161: 381-390.
Kanner RE, Anthonisen NR, Connett JE: Lower respiratory illnesses promote FEV1 decline in current smokers but not ex-smokers with mild chronic obstructive pulmonary disease. Results from the Lung Health Study. Am J Respir Crit Care Med. 2001, 164: 358-364.
Anthonisen NR, Connett JE, Murray RP: Smoking and lung function of Lung Health Study participants after 11 years. Am J Respir Crit Care Med. 2002, 166: 675-679. 10.1164/rccm.2112096.
Soriano JB, Sin DD, Zhang X, Camp PG, Anderson JA, Anthonisen NR, Buist AS, Burge PS, Calverley PM, Connett JE, Petersson S, Postma DS, Szafranski W, Vestbo J: A pooled analysis of FEV1 decline in COPD patients randomized to inhaled corticosteroids or placebo. Chest. 2007, 131: 682-689. 10.1378/chest.06-1696.
Townsend MC: Effects of smoking and smoking cessation on FEV1 decline at three MRFIT centers [Abstract]. Am Rev Respir Dis. 1987, 135 (Suppl): A342..
Townsend MC, DuChene AG, Morgan J, Browner WS: Pulmonary function in relation to cigarette smoking and smoking cessation. Prev Med. 1991, 20: 621-637. 10.1016/0091-7435(91)90059-D.
Xie G, Cheng X, Xu X: (Risk factors of chronic obstructive pulmonary disease in patients with chronic bronchitis). Zhonghua Yi Xue Za Zhi. 2001, 81: 1356-1359.
Huhti E, Sutinen S, Reinilä A, Poukkula A, Saloheimo M: Lung cancer in a defined geographical area: history and histological types. Thorax. 1980, 35: 660-667. 10.1136/thx.35.9.660.
Czajkowska-Malinowska M, Nowiński A, Górecka D, Zieliński J: Wpływ wczesnego środowiskowego wykrywania POCHP na ograniczenie nałogu palenia tytoniu (Effects of spirometric screening in the community on smoking cessation). Pneumonol Alergol Pol. 2001, 69: 524-529.
Godtfredsen NS, Lange P, Prescott E, Osler M, Vestbo J: Changes in smoking habits and risk of asthma: a longitudinal population based study. Eur Respir J. 2001, 18: 549-554. 10.1183/09031936.01.00100801.
Rose G, Hamilton PJS: A randomised controlled trial of the effect on middle-aged men of advice to stop smoking. J Epidemiol Community Health. 1978, 32: 275-281. 10.1136/jech.32.4.275.
Sherrill DL, Holberg CJ, Enright PL, Lebowitz MD, Burrows B: Longitudinal analysis of the effects of smoking onset and cessation on pulmonary function. Am J Respir Crit Care Med. 1994, 149: 591-597.
Sherrill DL, Enright P, Cline M, Burrows B, Lebowitz MD: Rates of decline in lung function among subjects who restart cigarette smoking. Chest. 1996, 109: 1001-1005. 10.1378/chest.109.4.1001.
Omori H, Morimoto Y: (Effects of smoking habits on pulmonary function. Cross-sectional and longitudinal studies in male subjects on medical check-up). Nihon Kokyuki Gakkai Zasshi. 2004, 42: 306-312.
Connett JE, Murray RP, Buist AS, Wise RA, Bailey WC, Lindgren PG, Owens GR: Changes in smoking status affect women more than men: results of the Lung Health Study. Am J Epidemiol. 2003, 157 (Suppl): 973-979. 10.1093/aje/kwg083.
Harber P, Tashkin DP, Simmons M, Crawford L, Hnizdo E, Connett J: Effect of occupational exposures on decline of lung function in early chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2007, 176: 994-1000. 10.1164/rccm.200605-730OC.
Murray RP, Anthonisen NR, Connett JE, Wise RA, Lindgren PG, Greene PG, Nides MA: Effects of multiple attempts to quit smoking and relapses to smoking on pulmonary function. J Clin Epidemiol. 1998, 51: 1317-1326. 10.1016/S0895-4356(98)00120-6.
Simmons MS, Connett JE, Nides MA, Lindgren PG, Kleerup EC, Murray RP, Bjornson WM, Tashkin DP: Smoking reduction and the rate of decline in FEV1: results from the Lung Health Study. Eur Respir J. 2005, 25: 1011-1017. 10.1183/09031936.05.00086804.
Wise RA, Enright PL, Connett JE, Anthonisen NR, Kanner RE, Lindgren P, O'Hara P, Owens GR, Rand CS, Tashkin DP: Effect of weight gain on pulmonary function after smoking cessation in the Lung Health Study. Am J Respir Crit Care Med. 1998, 157: 866-872.
Wise RA, Kanner RE, Lindgren P, Connett JE, Altose MD, Enright PL, Tashkin DP: The effect of smoking intervention and an inhaled bronchodilator on airways reactivity in COPD: the Lung Health Study. Chest. 2003, 124: 449-458. 10.1378/chest.124.2.449.
Eberly LE, Ockene J, Sherwin R, Yang L, Kuller L: Pulmonary function as a predictor of lung cancer mortality in continuing cigarette smokers and in quitters. Int J Epidemiol. 2003, 32: 592-599. 10.1093/ije/dyg177.
Piitulainen E, Eriksson S: Decline in FEV1 related to smoking status in individuals with severe α1-antitrypsin deficiency (PiZZ). Eur Respir J. 1999, 13: 247-251. 10.1183/09031936.99.13224799.
Pelkonen M, Tukiainen H, Tervahauta M, Notkola IL, Nissinen A, Salorinne Y, Nissinen A: Pulmonary function, smoking cessation and 30 year mortality in middle aged Finnish men. Thorax. 2000, 55: 746-750. 10.1136/thorax.55.9.746.
Pelkonen M, Notkola IL, Tukiainen H, Tervahauta M, Tuomilehto J, Nissinen A: Smoking cessation, decline in pulmonary function and total mortality: a 30 year follow up study among the Finnish cohorts of the Seven Countries Study. Thorax. 2001, 56: 703-707. 10.1136/thorax.56.9.703.
Pelkonen M, Notkola IL, Nissinen A, Tukiainen H, Koskela H: Thirty-year cumulative incidence of chronic bronchitis and COPD in relation to 30-year pulmonary function and 40-year mortality: a follow-up in middle-aged rural men. Chest. 2006, 130: 1129-1137. 10.1378/chest.130.4.1129.
Stolzmann KL, Gagnon DR, Brown R, Tun CG, Garshick E: Longitudinal change in FEV1 and FVC in chronic spinal cord injury. Am J Respir Crit Care Med. 2008, 177: 781-786. 10.1164/rccm.200709-1332OC.
Bake B, Oxhøj H, Sixt R, Wilhelmsen L: Ventilatory lung function following two years of tobacco abstinence. Scand J Respir Dis. 1977, 58: 311-318.
Bednarek M, Gorecka D, Wielgomas J, Czajkowska-Malinowska M, Regula J, Mieszko-Filipczyk G, Jasionowicz M, Bijata-Bronisz R, Lempicka-Jastrzebska M, Czajkowski M, Przybylski G, Zielinski J: Smokers with airway obstruction are more likely to quit smoking. Thorax. 2006, 61: 869-873. 10.1136/thx.2006.059071.
Bohadana AB, Nilsson F, Westin A, Martinet N, Martinet Y: Smoking cessation - but not smoking reduction - improves the annual decline in FEV1 in occupationally exposed workers. Respir Med. 2006, 100: 1423-1430. 10.1016/j.rmed.2005.11.005.
Buist AS, Sexton GJ, Nagy JM, Ross BB: The effect of smoking cessation and modification on lung function. Am Rev Respir Dis. 1976, 114: 115-122.
Emmons KM, Weidner G, Foster WM, Collins RL: Improvement in pulmonary function following smoking cessation. Addict Behav. 1992, 17: 301-306. 10.1016/0306-4603(92)90036-U.
Górecka D, Bednarek M, Nowiński A, Kamiński D, Bieleń P, Kołakowski J, Pływaczewski R, Goljan A, Puścińska E, Zieliński J: Czynniki określające sukces w porzucaniu palenia u osób uczestniczących w środowiskowych badaniach spirometrycznych (Predictors of success in smoking cessation among participants of spirometric screening for COPD). Pneumonol Alergol Pol. 2001, 69: 611-616.
Jensen EJ, Pedersen B, Frederiksen R, Dahl R: Prospective study on the effect of smoking and nicotine substitution on leucocyte blood counts and relation between blood leucocytes and lung function. Thorax. 1998, 53: 784-789. 10.1136/thx.53.9.784.
McCarthy DS, Craig DB, Cherniack RM: Effect of modification of the smoking habit on lung function. Am Rev Respir Dis. 1976, 114: 103-113.
Parkes G, Greenhalgh T, Griffin M, Dent R: Effect on smoking quit rate of telling patients their lung age: the Step2quit randomised controlled trial. BMJ. 2008, 336: 598-600. 10.1136/bmj.39503.582396.25.
Willemse BWM, ten Hacken NH, Rutgers B, Lesman-Leegte IGAT, Postma DS, Timens W: Effect of 1-year smoking cessation on airway inflammation in COPD and asymptomatic smokers. Eur Respir J. 2005, 26: 835-845. 10.1183/09031936.05.00108904.
Brown LC, Powell JT: Risk factors for aneurysm rupture in patients kept under ultrasound surveillance. UK Small Aneurysm Trial Participants. Ann Surg. 1999, 230: 289-296. 10.1097/00000658-199909000-00002.
Buffels J, Degryse J, Decramer M, Heyrman J: Spirometry and smoking cessation advice in general practice: a randomised clinical trial. Respir Med. 2006, 100: 2012-2017. 10.1016/j.rmed.2006.02.014.
Annesi I, Neukirch F, Orvoen-Frija E, Oryszczyn MP, Korobaeff M, Doré MF, Kauffmann F: The relevance of hyperresponsiveness but not of atopy to FEV1 decline. Preliminary results in a working population. Bull Eur Physiopathol Respir. 1987, 23: 397-400.
Anthonisen NR: Lessons from the Lung Health Study. Proc Am Thorac Soc. 2004, 1: 143-145. 10.1513/pats.2306033.
Anthonisen NR, Lindgren PG, Tashkin DP, Kanner RE, Scanlon PD, Connett JE: Bronchodilator response in the lung health study over 11 yrs. Eur Respir J. 2005, 26: 45-51. 10.1183/09031936.05.00102604.
Boggia B, Farinaro E, Grieco L, Lucariello A, Carbone U: Burden of smoking and occupational exposure on etiology of chronic obstructive pulmonary disease in workers of Southern Italy. J Occup Environ Med. 2008, 50: 366-370. 10.1097/JOM.0b013e318162f601.
Browner WS, Du Chene AG, Hulley SB: Effects of the multiple risk factor intervention trial smoking cessation program on pulmonary function. A randomized controlled trial. West J Med. 1992, 157: 534-538.
Buist AS, Nagy JM, Sexton GJ: The effect of smoking cessation on pulmonary function: a 30-month follow-up of two smoking cessation clinics. Am Rev Respir Dis. 1979, 120: 953-957.
Carey IM, Cook DG, Strachan DP: The effects of adiposity and weight change on forced expiratory volume decline in a longitudinal study of adults. Int J Obes. 1999, 23: 979-985. 10.1038/sj.ijo.0801029.
Chinn DJ, Cotes JE, Reed JW: Longitudinal effects of change in body mass on measurements of ventilatory capacity. Thorax. 1996, 51: 699-704. 10.1136/thx.51.7.699.
Clotet J, Gómez-Arbonés X, Ciria C, Albalad JM: La espirometría es un buen método para la detección y el seguimiento de la EPOC en fumadores de alto riesgo en atención primaria (Spirometry is a good method for detecting and monitoring chronic obstructive pulmonary disease in high-risk smokers in primary health care). Arch Bronconeumol. 2004, 40: 155-159.
Colditz GA, Stein C: Smoking cessation, weight gain, and lung function. Lancet. 2005, 365: 1600-1601. 10.1016/S0140-6736(05)66486-0.
Engström G, Wollmer P, Valind S, Hedblad B, Janzon L: Blood pressure increase between 55 and 68 years of age is inversely related to lung function: longitudinal results from the cohort study 'Men born in 1914'. J Hypertens. 2001, 19: 1203-1208. 10.1097/00004872-200107000-00004.
Enright PL, Connett JE, Bailey WC: The FEV1/FEV6 predicts lung function decline in adult smokers. Respir Med. 2002, 96: 444-449. 10.1053/rmed.2001.1270.
Evers H, Herrmann H, Ohme G: Due wertigkeit des maximalen exspiratorischen fluß-volumen-diagramms in einer longitudinalstudie 2. mitteilung: ergebnisse bei jungen erwachsenen) Valuation of the maximal expiratory flow-volume curve in a follow-up study. 2nd paper: results in young adults. Z Erkr Atmungsorgane. 1986, 167: 79-86.
Godtfredsen NS, Prescott E, Osler M, Vestbo J: Predictors of smoking reduction and cessation in a cohort of Danish moderate and heavy smokers. Prev Med. 2001, 33: 46-52. 10.1006/pmed.2001.0852.
Godtfredsen NS, Vestbo J, Osler M, Prescott E: Risk of hospital admission for COPD following smoking cessation and reduction: a Danish population study. Thorax. 2002, 57: 967-972. 10.1136/thorax.57.11.967.
Hoogendoorn M, Rutten-van Mölken MP, Hoogenveen RT, van Genugten MLL, Buist AS, Wouters EFM, Feenstra TL: A dynamic population model of disease progression in COPD. Eur Respir J. 2005, 26: 223-233. 10.1183/09031936.05.00122004.
Kanner RE: Early intervention in chronic obstructive pulmonary disease. A review of the Lung Health Study results. Med Clin North Am. 1996, 80: 523-547.
Kuller LH, Ockene JK, Townsend M, Browner W, Meilahn E, Wentworth DN: The epidemiology of pulmonary function and COPD mortality in the multiple risk factor intervention trial. Am Rev Respir Dis. 1989, 140 (3 Pt 2): S76-S81.
Labrecque M, Khemici E, Cartier A, Malo JL, Turcot J: Impairment in workers with isocyanate-induced occupational asthma and removed from exposure in the province of Québec between 1985 and 2002. J Occup Environ Med. 2006, 48: 1093-1098. 10.1097/01.jom.0000243399.81329.d0.
Løkke A, Lange P, Scharling H, Fabricius P, Vestbo J: Developing COPD: a 25 year follow up study of the general population. Thorax. 2006, 61: 935-939. 10.1136/thx.2006.062802.
Makris D, Moschandreas J, Damianaki A, Ntaoukakis E, Siafakas NM, Milic Emili J, Tzanakis N: Exacerbations and lung function decline in COPD: new insights in current and ex-smokers. Respir Med. 2007, 101: 1305-1312. 10.1016/j.rmed.2006.10.012.
O'Hara P, Connett JE, Lee WW, Nides M, Murray R, Wise R: Early and late weight gain following smoking cessation in the Lung Health Study. Am J Epidemiol. 1998, 148: 821-830.
Peach H, Hayward DM, Ellard DR, Morris RW, Shah D: Phlegm production and lung function among cigarette smokers changing tar groups during 1970s. J Epidemiol Community Health. 1986, 40: 110-116. 10.1136/jech.40.2.110.
Peters-Golden M, Wise RA, Schneider P, Hochberg M, Stevens MB, Wigley F: Clinical and demographic predictors of loss of pulmonary function in systemic sclerosis. Medicine. 1984, 43: 221-231.
Pletcher MJ, Hulley BJ, Houston T, Kiefe CI, Benowitz N, Sidney S: Menthol cigarettes, smoking cessation, atherosclerosis, and pulmonary function: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Arch Intern Med. 2006, 166: 1915-1922. 10.1001/archinte.166.17.1915.
Postma DS, Sluiter HJ: Prognosis of chronic obstructive pulmonary disease: the Dutch experience. Am Rev Respir Dis. 1989, 140: S100-S105.
Pride NB, Tattersall SF, Benson MK, Hunter D, Mansell A, Fletcher CM, Peto R: Peripheral function and spirometry in male smokers and exsmokers. Chest. 1980, 77: 289-290.
Remy-Jardin M, Edme JL, Boulenguez C, Remy J, Mastora I, Sobaszek A: Longitudinal follow-up study of smoker's lung with thin-section CT in correlation with pulmonary function tests. Radiology. 2002, 222: 261-270. 10.1148/radiol.2221001154.
Ryu JH, Myers JL, Capizzi SA, Douglas WW, Vassallo R, Decker PA: Desquamative interstitial pneumonia and respiratory bronchiolitis-associated interstitial lung disease. Chest. 2005, 127: 178-184. 10.1378/chest.127.1.178.
Siracusa A, Forcina A, Volpi R, Mollichella E, Cicioni C, Fiordi T: An 11-year longitudinal study of the occupational dust exposure and lung function of polyvinyl chloride, cement and asbestos cement factory workers. Scand J Work Environ Health. 1988, 14: 181-188.
Snow WM, Connett JE, Sharma S, Murray RP: Predictors of attendance and dropout at the Lung Health Study 11-year follow-up. Contemp Clin Trials. 2007, 28: 25-32. 10.1016/j.cct.2006.08.010.
Stratelis G, Mölstad S, Jakobsson P, Zetterström O: The impact of repeated spirometry and smoking cessation advice on smokers with mild COPD. Scand J Prim Health Care. 2006, 24: 133-139. 10.1080/02813430600819751.
Tetzlaff K, Theysohn J, Stahl C, Schlegel S, Koch A, Muth CM: Decline of FEV1 in scuba divers. Chest. 2006, 130: 238-243. 10.1378/chest.130.1.238.
Tollerud DJ, Weiss ST, Elting E, Speizer FE, Ferris B: The health effects of automobile exhaust. VI. Relationship of respiratory symptoms and pulmonary function in tunnel and turnpike workers. Arch Environ Health. 1983, 38: 334-340.
Twisk JWR, Staal BJ, Brinkman MN, Kemper HCG, van Mechelen W: Tracking of lung function parameters and the longitudinal relationship with lifestyle. Eur Respir J. 1998, 12: 627-634. 10.1183/09031936.98.12030627.
Zimmermann H, Brandli O: Der Verlauf der chronischen obstruktiven Lungenkrankheit unter Therapie (The course of treated chronic obstructive lung disease). Schweiz Med Wochenschr. 1980, 110: 232-236.
Dockery DW, Speizer FE, Ferris BG, Ware JH, Louis TA, Spiro A: Cumulative and reversible effects of lifetime smoking on simple tests of lung function in adults. Am Rev Respir Dis. 1988, 137: 286-292.
Nemery B, Moavero NE, Brasseur L, Stanescu DC: Changes in lung function after smoking cessation: an assessment from a cross-sectional survey. Am Rev Respir Dis. 1982, 125: 122-124.
Yang SC, Yang SP: Bronchial responsiveness and lung function related to cigarette smoking and smoking cessation. Chang Gung Med J. 2002, 25: 645-655.
Young RP, Hopkins R, Eaton TE: Forced expiratory volume in one second: not just a lung function test but a marker of premature death from all causes. Eur Respir J. 2007, 30: 616-622. 10.1183/09031936.00021707.
Waage HP, Vatten LJ, Opedal E, Hilt B: Lung function and respiratory symptoms related to changes in smoking habits in asbestos-exposed subjects. J Occup Environ Med. 1996, 38: 178-183. 10.1097/00043764-199602000-00015.
StĂnescu D, Sanna A, Veriter C, Kostianev S, Calcagni PG, Fabbri LM, Maestrelli P: Airways obstruction, chronic expectoration, and rapid decline of FEV1 in smokers are associated with increased levels of sputum neutrophils. Thorax. 1996, 51: 267-271. 10.1136/thx.51.3.267.
StĂnescu D, Veriter C, Sanna A: In long-term smokers and former smokers the bronchodilator response is not related to the fall in FEV. Respiration. 1999, 66: 501-505. 10.1159/000029448.
Lebowitz MD, Holberg CJ, Knudson RJ, Burrows B: Longitudinal study of pulmonary function development in childhood, adolescence and early adulthood. Am Rev Respir Dis. 1987, 136: 69-75.
Krzyzanowski M, Camilli AE, Lebowitz MD: Relationships between pulmonary function and changes in chronic respiratory symptoms. Comparison of Tucson and Cracow longitudinal studies. Chest. 1990, 98: 62-70. 10.1378/chest.98.1.62.
Anthonisen NR: Epidemiology and the lung health study. Eur Respir Rev. 1997, 7: 202-205.
Barter CE, Campbell AH: Relationship of constitutional factors and cigarette smoking to decrease in 1-second forced expiratory volume. Am Rev Respir Dis. 1976, 113: 305-314.
Leader WG, Wolf KM, Cooper TM, Chandler MHH: Symptomatology, pulmonary function and response, and T lymphocyte β2-receptors during smoking cessation in patients with chronic obstructive pulmonary disease. Pharmacotherapy. 1994, 14: 162-172.
Sherrill DL, Lebowitz MD, Knudson RJ, Burrows B: Longitudinal methods for describing the relationship between pulmonary function, respiratory symptoms and smoking in elderly subjects: the Tucson Study. Eur Respir J. 1993, 6: 342-348.
Bode FR, Dosman J, Martin RR, Macklem PT: Reversibility of pulmonary function abnormalities in smokers. Am J Med. 1975, 59: 43-52. 10.1016/0002-9343(75)90320-4.
Friedman GD, Siegelaub AB: Changes after quitting cigarette smoking. Circulation. 1980, 61: 716-723.
Michaels R, Sigurdson M, Thurlbeck S, Cherniack R: Elastic recoil of the lung in cigarette smokers: the effect of nebulized bronchodilator and cessation of smoking. Am Rev Respir Dis. 1979, 119: 707-716.
Yang F: A survey on the damages of small airway function by smoking. Acta Academiae Medicine Suzhou. 1999, 19: 648.
Rose G, Hamilton PJS, Colwell L, Shipley MJ: A randomised controlled trial of anti-smoking advice: 10-year results. J Epidemiol Community Health. 1982, 36: 102-108. 10.1136/jech.36.2.102.
Higgins MW, Enright PL, Kronmal RA, Schenker MB, Anton-Culver H, Lyles M: Smoking and lung function in elderly men and women. The cardiovascular health study. JAMA. 1993, 269: 2741-2748. 10.1001/jama.269.21.2741.
Jiang J, Tang Z, Tao S, et al: A 7 year follow-up survey of ventilation function in 38 male adult smokers. Prev Med J Chin PLA. 1994, 12: 372-374.
Wang P, Lei Q, Li Y, et al: The relationship between dynamic changes of pulmonary function in 13 years and smoking in 150 elderly people. Health Med J Chin PLA. 1999, 3: 22-23.
Wang M, Wang B: A survey of health status and ex-smokers before and after quitting smoking. J Baotou Med Coll. 2000, 16: 16-17.
Wang L, Zhang X, Li Y, et al: Effect of etiological therapy to pulmonary function recovery of the patient with small airway disease. J Shandong University (Health Sciences). 2002, 40: 135-137.
Kerstjens HAM, Brand PLP, Postma DS: Risk factors for accelerated decline among patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1996, 154: S266-S272.
Bande J, Clément J, van de Woestijne KP: The influence of smoking habits and body weight on vital capacity and FEV1 in male Air Force personnel: a longitudinal and cross-sectional analysis. Am Rev Respir Dis. 1980, 122: 781-790.
Barter CE, Campbell AH, Tandon MK: Factors affecting the decline of FEV1 in chronic bronchitis. Aust N Z J Med. 1974, 4: 339-345.
Beaty TH, Menkes HA, Cohen BH, Newill CA: Risk factors associated with longitudinal change in pulmonary function. Am Rev Respir Dis. 1984, 129: 660-667.
Betsuyaku T, Nishimura M, Takeyabu K, Tanino M, Miyamoto K, Kawakami Y: Decline in FEV1 in community-based older volunteers with higher levels of neutrophil elastase in bronchoalveolar lavage fluid. Respiration. 2000, 67: 261-267. 10.1159/000029508.
Burchfiel CM, Marcus EB, Sharp DS, Enright PL, Rodriguez BL, Masaki KH, Hwang LJ, Curb JD: Characteristics associated with rapid decline in forced expiratory volume. Ann Epidemiol. 1996, 6: 217-227. 10.1016/1047-2797(96)00007-5.
Alessandri C, Basili S, Violi F, Ferroni P, Gazzaniga PP, Cordova C: Hypercoagulability state in patients with chronic obstructive pulmonary disease. Thromb Haemost. 1994, 72: 343-346.
Edelman NH, Mittman C, Norris AH, Cohen BH, Shock NW: The effects of smoking upon spirometric performance of community dwelling men. Am Rev Respir Dis. 1966, 94: 421-429.
Berry G, McKerrow CB, Molyneux MKB, Rossiter CE, Tombleson JBL: A study of the acute and chronic changes in ventilatory capacity of workers in Lancashire cotton mills. Br J Industr Med. 1973, 30: 25-36.
Diem JE, Liukkonen JR: A comparative study of three methods for analysing longitudinal pulmonary function data. Stat Med. 1988, 7: 19-28. 10.1002/sim.4780070107.
Buist AS, Vollmer WM, Johnson LR, Bernstein RS, McCamant LE: A four-year prospective study of the respiratory effects of volcanic ash from Mt St Helens. Am Rev Respir Dis. 1986, 133: 526-534.
Parker DR, O'Connor GT, Sparrow D, Segal MR, Weiss ST: The relationship of nonspecific airway responsiveness and atopy to the rate of decline of lung function. The Normative Aging Study. Am Rev Respir Dis. 1990, 141: 589-594.
Sparrow D, Stefos T, Bossé R, Weiss ST: The relationship of tar content to decline in pulmonary function in cigarette smokers. Am Rev Respir Dis. 1983, 127: 56-58.
Habib MP, Klink ME, Knudson DE, Bloom JW, Kaltenborn WT, Knudson RJ: Physiologic characteristics of subjects exhibiting accelerated deterioration of ventilatory function. Am Rev Respir Dis. 1987, 136: 638-645.
Lebowitz MD, Postma DS, Burrows B: Adverse effects of eosinophilia and smoking on the natural history of newly diagnosed chronic bronchitis. Chest. 1995, 108: 55-61. 10.1378/chest.108.1.55.
Sherrill DL, Lebowitz MD, Knudson RJ, Burrows B: Smoking and symptom effects on the curves of lung function growth and decline. Am Rev Respir Dis. 1991, 144: 17-22.
Ferris BG, Higgins ITT, Higgins MW, Peters JM, Van Ganse WF, Goldman MD: Chronic nonspecific respiratory disease, Berlin, New Hampshire, 1961-1967: A cross-sectional study. Am Rev Respir Dis. 1971, 104: 232-244.
Jedrychowski W: Biological meaning of the prospective epidemiological study on chronic obstructive lung disease and aging. Arch Gerontol Geriatr. 1983, 2: 237-248. 10.1016/0167-4943(83)90027-4.
Jedrychowski W, Krzyzanowski M, Wysocki M: Are chronic wheezing and asthma-like attacks related to FEV1 decline? The Cracow study. Eur J Epidemiol. 1988, 4: 335-342. 10.1007/BF00148921.
Krzyzanowski M: Changes of ventilatory capacity in an adult population during a five year period. Bull Eur Physiopathol Respir. 1980, 16: 155-170.
Lange P: Development and prognosis of chronic obstructive pulmonary disease with special reference to the role of tobacco smoking. An epidemiologic study. Dan Med Bull. 1992, 39: 30-48.
Tattersall SF, Benson MK, Hunter D, Mansell A, Pride NB, Fletcher CM, Peto R, Gray R, Humphreys PRR: The use of tests of peripheral lung function for predicting future disability from airflow obstruction in middle-aged smokers. Am Rev Respir Dis. 1978, 118: 1035-1050.
Tashkin DP, Altose MD, Connett JE, Kanner RE, Lee WW, Wise RA: Methacholine reactivity predicts changes in lung function over time in smokers with early chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1996, 153: 1802-1811.
Townsend MC, DuChene AG, Morgan J, Browner W: Pulmonary function in relation to smoking and smoking cessation in the Multiple Risk Factor Intervention Trial (MRFIT) [Abstract]. Am Rev Respir Dis. 1986, 133 (Suppl): A158..
Evald T, Dirksen A, Keittelmann S, Viskum K, Kok-Jensen A: Decline in pulmonary function in patients with α1-antitrypsin deficiency. Lung. 1990, 579-585. 10.1007/BF02718180. Suppl
Horton FO, Mackenthun AV, Anderson PS, Patterson CD, Hammarsten JF: α1 antitrypsin heterozygotes (Pi type MZ). Chest. 1980, 77 (Suppl): 261-264. 10.1378/chest.77.2_Supplement.261-a.
Janus ED, Phillips NT, Carrell RW: Smoking, lung function, and α1-antitrypsin deficiency. Lancet. 1985, 152-154. 10.1016/S0140-6736(85)91916-6.
Seersholm N, Kok-Jensen A, Dirksen A: Decline in FEV1 among patients with severe hereditary α1-antitrypsin deficiency type PiZ. Am J Respir Crit Care Med. 1995, 152 (6 Pt 1): 1922-1925.
Wu MC, Eriksson S: Lung function, smoking and survival in severe α1-antitrypsin deficiency, PiZZ. J Clin Epidemiol. 1988, 41: 1157-1165. 10.1016/0895-4356(88)90019-4.
Higgins ITT, Gilson JC, Ferris BG, Waters ME, Campbell H, Higgins MW: Environmental epidemiology. IV Chronic respiratory disease in an industrial town: a nine-year follow-up study. Preliminary report. Am J Public Health. 1968, 58: 1667-1676. 10.2105/AJPH.58.9.1667.
Higgins ITT: The epidemiology of chronic respiratory disease. Prev Med. 2: 14-33. 10.1016/0091-7435(73)90005-4.
Thenault D, Friemel F, Cannet G, Larger C: Qu'implique la découverte d'une valeur de compliance pulmonaire élevée? (What are the implications of a high pulmonary compliance?). Respiration. 1986, 49: 170-180. 10.1159/000194876.
Kashiwabara K, Nakamura H, Yokoi T: Chronological change of serum carcinoembryonic antigen (CEA) concentrations and pulmonary function data after cessation of smoking in subjects with smoking-associated CEA abnormality. Clin Chim Acta. 2001, 303: 25-32. 10.1016/S0009-8981(00)00341-7.
Johansen D, Larsen V, Landfrits U, Døssing M: Rygestop hos patienter med svær grad af irreversibel kronisk obstruktiv lungesygdom rygerlunger (Smoking cessation in patients with severe irreversible chronic obstructive pulmonary disease, smoker's lung). Ugeskr Laeger. 1999, 161: 3655-3658.
Peterson DI, Lonergan LH, Hardinge MG: Smoking and pulmonary function. Arch Environ Health. 1968, 16: 215-218.
Stolz D, Anderson SD, Gysin C, Miedinger D, Surber C, Tamm M, Leuppi JD: Airway reactivity to inhaled mannitol in cigarette smokers: a longitudinal study. Respir Med. 2007, 101: 1470-1476. 10.1016/j.rmed.2007.01.008.
Marcus EB, Buist AS, Curb JD, MacLean CJ, Reed DM, Johnson LR, Yano K: Correlates of FEV1 and prevalence of pulmonary conditions in Japanese-American men. Am Rev Respir Dis. 1988, 138: 1398-1404.
Morse JO, Lebowitz MD, Knudson RJ, Burrows B: Relation of protease inhibitor phenotypes to obstructive lung diseases in a community. N Engl J Med. 1977, 296: 1190-1194. 10.1056/NEJM197705262962102.
Albers M, Schermer T, Heijdra Y, Molema J, Akkermans R, van Weel C: Predictive value of lung function below the normal range and respiratory symptoms for progression of chronic obstructive pulmonary disease. Thorax. 2008, 63: 201-207. 10.1136/thx.2006.068007.
Ashley F, Kannel WB, Sorlie PD, Masson R: Pulmonary function: relation to aging, cigarette habit, and mortality. Ann Intern Med. 1975, 82: 739-745.
Bolliger CT, Zellweger JP, Danielsson T, van Biljon X, Robidou A, Westin A, Perruchoud AP, Säwe U: Influence of long-term smoking reduction on health risk markers and quality of life. Nicotine Tob Res. 2002, 4: 433-439. 10.1080/1462220021000018380.
Brantly ML, Paul LD, Miller BH, Falk RT, Wu M, Crystal RG: Clinical features and history of the destructive lung disease associated with α-1-antitrypsin deficiency of adults with pulmonary symptoms. Am Rev Respir Dis. 1988, 138: 327-336.
Eriksson S, Wu MC: Aspects of treatment in α1-antitrypsin deficiency: insights derived from a Swedish PiZZ series. Eur Respir J. 1990, 3 (Suppl 9): 39s-43s.
Ferris BG, Higgins ITT, Higgins MW, Peters JM: Chronic nonspecific respiratory disease in Berlin, New Hampshire, 1961 to 1967. Am Rev Respir Dis. 1973, 107: 110-122.
Frette C, Annesi I, Korobaeff M, Neukirch F, Dore MF, Kauffmann F: Blood eosinophilia and FEV1. Cross-sectional and longitudinal analyses. Am Rev Respir Dis. 1991, 143: 987-992.
Garvey AJ, Bosse R, Seltzer CC: Smoking, weight change, and age: a longitudinal analysis. Arch Environ Health. 1974, 28: 327-329.
Grol MH, Postma DS, Vonk JM, Schouten JP, Rijcken B, Koëter GH, Gerritsen J: Risk factors from childhood to adulthood for bronchial responsiveness at age 32-42 yr. Am J Respir Crit Care Med. 1999, 160: 150-156.
Herrmann H: Die Bedeutung kommunaler Umweltfaktoren für die Entstehung chronischer Atemwegserkrankungen (The importance of environmental factors on the development of chronic lung diseases). Z Erkr Atmungsorgane. 1983, 161: 163-176.
Higgins ITT, Higgins MW, Gilson JC, Campbell H, Waters WE, Ferris BG: Smoking and chronic respiratory disease: finding in surveys carried out in 1957 and 1966 in Staveley in Derbyshire, England. Chest. 1971, 59 (Suppl): 34s-35s.
Hjalmarsson A, Svärdsudd K: Health consequences of giving up smoking in a prospective population study of middle-aged Swedish men. The study of men born in 1913. Acta Med Scand. 1981, 210: 93-96. 10.1111/j.0954-6820.1981.tb09781.x.
Hutchison DCS: Natural history of α1-protease inhibitor deficiency. Am J Med. 1988, 84 (Suppl 6A): 3-12.
Jaakkola MS, Ernst P, Jaakkola JJK, N'gan'ga LW, Becklake MR: Effect of cigarette smoking on evolution of ventilatory lung function in young adults: an eight year longitudinal study. Thorax. 1991, 46: 907-913. 10.1136/thx.46.12.907.
Jedrychowski W, Krzyzanowski M: Ventilatory lung function and chronic chest symptoms among the inhabitants of urban areas with various levels of acid aerosols: prospective study in Cracow. Environ Health Perspect. 1989, 79: 101-107. 10.2307/3430535.
Johnston RN, McNeill RS, Smith DH, Legge JS, Fletcher F: Chronic bronchitis: measurements and observations over 10 years. Thorax. 1976, 31: 25-29. 10.1136/thx.31.1.25.
Kanner RE, Connett JE, Williams DE, Buist AS: Effects of randomized assignment to a smoking cessation intervention and changes in smoking habits on respiratory symptoms in smokers with early chronic obstructive pulmonary disease: the Lung Health Study. Am J Med. 1999, 106: 410-416. 10.1016/S0002-9343(99)00056-X.
Madison R, Mittman C, Afifi AA, Zelman R: Risk factors for obstructive lung disease. Am Rev Respir Dis. 1981, 124: 149-153.
Ohlson CG, Bodin L, Rydman T, Hogstedt C: Ventilatory decrements in former asbestos cement workers: a four year follow up. Br J Ind Med. 1985, 42: 612-616.
Peat JK, Woolcock AJ, Cullen K: Decline of lung function and development of chronic airflow limitation: a longitudinal study of non-smokers and smokers in Busselton, Western Australia. Thorax. 1990, 45: 32-37. 10.1136/thx.45.1.32.
Petty TL, Pierson DJ, Dick NP, Hudson LD, Walker SH: Follow-up evaluation of a prevalence study for chronic bronchitis and chronic airway obstruction. Am Rev Respir Dis. 1976, 114: 881-890.
Postma DS, Gimeno F, van der Weele LT, Sluiter HJ: Assessment of ventilatory variables in survival prediction of patients with chronic airflow obstruction: the importance of reversibility. Eur J Respir Dis. 1985, 67: 360-368.
Poukkula A, Huhti E, Mäkaräinen M: Chronic respiratory disease among workers in a pulp mill. A ten-year follow-up study. Chest. 1982, 81: 285-289. 10.1378/chest.81.3.285.
Seersholm N, Wencker M, Banik N, Viskum K, Dirksen A, Kok-Jensen A, Konietzko N: Does α1-antitrypsin augmentation therapy slow the annual decline in FEV1 patients with severe hereditary α1-antitrypsin deficiency?. Eur Respir J. 1997, 10: 2260-2263. 10.1183/09031936.97.10102260.
Sharp JT, Paul O, McKean H, Best WR: A longitudinal study of bronchitic symptoms and spirometry in a middle-aged, male, industrial population. Am Rev Respir Dis. 1973, 108: 1066-1077.
Sorlie P, Lakatos E, Kannel WB, Celli B: Influence of cigarette smoking on lung function at baseline and at follow-up in 14 years: the Framingham study. J Chronic Dis. 1987, 40: 849-856. 10.1016/0021-9681(87)90184-6.
Sparrow D, O'Connor GT, Basner RC, Rosner B, Weiss ST: Predictors of the new onset of wheezing among middle-aged and older men. Am Rev Respir Dis. 1993, 147: 367-371.
Tager IB, Segal MR, Speizer FE, Weiss ST: The natural history of forced expiratory volumes. Effect of cigarette smoking and respiratory symptoms. Am Rev Respir Dis. 1988, 138: 837-849.
Vikgren J, Boijsen M, Andelid K, Ekberg-Jansson A, Larsson S, Bake B, Tylén U: High-resolution computed tomography in healthy smokers and never-smokers: a 6-year follow-up study of men born in 1933. Acta Radiol. 2004, 45: 44-52. 10.1080/02841850310002970.
Woolf CR, Zamel N: The respiratory effects of regular cigarette smoking in women. A five year prospective study. Chest. 1980, 78: 707-713. 10.1378/chest.78.5.707.
Berglund DJ, Abbey DE, Lebowitz MD, Knutsen SF, McDonnell WF: Respiratory symptoms and pulmonary function in an elderly nonsmoking population. Chest. 1999, 115: 49-59. 10.1378/chest.115.1.49.
Burrows B, Knudson RJ, Cline MG, Lebowitz MD: Quantitative relationship between cigarette smoking and ventilatory function. Am Rev Respir Dis. 1977, 115: 195-205.
Frette C, Barrett-Connor E, Clausen JL: Effect of active and passive smoking on ventilatory function in elderly men and women. Am J Epidemiol. 1996, 143: 757-765.
Grimes CA, Hanes B: Influence of cigarette smoking on the spirometric evaluation of employees of a large insurance company. Am Rev Respir Dis. 1973, 108: 273-282.
Higgins ITT: Tobacco smoking, respiratory symptoms, and ventilatory capacity. Studies in random samples of the population. Br Med J. 1959, i: 325-329. 10.1136/bmj.1.5118.325.
Higgins MW, Keller JB: Seven measures of ventilatory lung function. Am Rev Respir Dis. 1973, 108: 258-272.
Kuperman AS, Riker JB: The variable effect of smoking on pulmonary function. Chest. 1973, 63: 655-660. 10.1378/chest.63.5.655.
Wilhelmsen L: Effects on broncho-pulmonary symptoms, ventilation and lung mechanics of abstinence from tobacco smoking. Scand J Respir Dis. 1967, 48: 407-414.
Kuller L, Meilahn E, Townsend M, Weinberg G: Control of cigarette smoking from a medical perspective. Annu Rev Public Health. 1982, 3: 153-178. 10.1146/annurev.pu.03.050182.001101.
Lebowitz MD, Burrows B: Risk factors in induction of lung disease: an epidemiologic approach. Mechanisms of lung injury. Edited by: Stein RP, Weinbaum G. 1986, Philadelphia: Stickley Publishing, 208-222.
Vollmer WM, Johnson LR, McCamant LE, Buist AS: Longitudinal versus cross-sectional estimation of lung function decline: further insights. Stat Med. 1988, 7: 685-696. 10.1002/sim.4780070607.
Tabona M, Chan-Yeung M, Enarson D, MacLean L, Dorken E, Schulzer M: Host factors affecting longitudinal decline in lung spirometry among grain elevator workers. Chest. 1984, 85: 782-786. 10.1378/chest.85.6.782.
Pham QT, Mur JM, Chau N, Teculescu DB, Henquel JC: A longitudinal study of respiratory symptoms and lung function in French iron miners. Bull Eur Physiopathol Respir. 1985, 21 (Suppl): 11A.
Pham QT, Teculescu D, Bruant A, Chau N, Viaggi MN, Rebstock E: Iron miners: a ten year follow-up. Eur J Epidemiol. 1992, 8: 594-600. 10.1007/BF00146382.
StĂnescu D, Sanna A, Veriter C, Robert A: Identification of smokers susceptible to development of chronic airflow limitation. A 13-year follow-up. Chest. 1998, 114: 416-425. 10.1378/chest.114.2.416.
Au DH, Bryson CL, Chien JW, Sun H, Udris EM, Evans LE, Bradley KA: The effects of smoking cessation on the risk of chronic obstructive pulmonary disease exacerbations. J Gen Intern Med. 2009, 24: 457-463. 10.1007/s11606-009-0907-y.
Chavannes NH, Schermer TR, Wouters EF, Akkermans RP, Dekhuijzen RP, Muris JW, van Weel C, van Schayck OC: Predictive value and utility of oral steroid testing for treatment of COPD in primary care: the COOPT study. Int J Chron Obstruct Pulmon Dis. 2009, 4: 431-436.
Løkke A, Christensen LB, Fuglsang C: Walk-in-spirometri-pilotundersøgelse til tidlig opsporing af kronisk obstruktiv (Walk-in spirometry pilot project for discovering of early chronic obstructive pulmonary disease). Ugeskr Laeger. 2009, 171: 3083-3088.
Shavelle RM, Paculdo DR, Kush SJ, Mannino DM, Strauss DJ: Life expectancy and years of life lost in chronic obstructive pulmonary disease: findings from the NHANES III Follow-up Study. Int J Chron Obstruct Pulmon Dis. 2009, 4: 137-148.
Toljamo T, Kaukonen M, Nieminen P, Kinnula VL: Early detection of COPD combined with individualized counselling for smoking cessation: a two-year prospective study. Scand J Prim Health Care. 2010, 28: 41-46. 10.3109/02813431003630105.
Yamane T, Hattori N, Kitahara Y, Haruta Y, Sasaki H, Yokoyama A, Kohno N: Productive cough is an independent risk factor for the development of COPD in former smokers. Respirology. 2010, 15: 313-318. 10.1111/j.1440-1843.2009.01682.x.
Godtfredsen NS, Lam TH, Hansel TT, Leon ME, Gray N, Dresler C, Burns DM, Prescott E, Vestbo J: COPD-related morbidity and mortality after smoking cessation: status of the evidence. Eur Respir J. 2008, 32: 844-853. 10.1183/09031936.00160007.
Downs SH, Brändli O, Zellweger JP, Schindler C, Künzli N, Gerbase MW, Burdet L, Bettschart R, Zemp E, Frey M, Keller R, Tschopp JM, Leuenberger P, Ackermann-Liebrich U, SAPALDIA team: Accelerated decline in lung function in smoking women with airway obstruction: SAPALDIA 2 cohort study. Respir Res. 2005, 6: 45-10.1186/1465-9921-6-45.
Mannino DM, Davis KJ: Lung function decline and outcomes in an elderly population. Thorax. 2006, 61: 472-477. 10.1136/thx.2005.052449.
Mannino DM, Reichert MM, Davis KJ: Lung function decline and outcomes in an adult population. Am J Respir Crit Care Med. 2006, 173: 985-990. 10.1164/rccm.200508-1344OC.
Prescott E, Bjerg AM, Andersen PK, Lange P, Vestbo J: Gender difference in smoking effects on lung function and risk of hospitalization for COPD: results from a Danish longitudinal population study. Eur Respir J. 1997, 10: 822-827.
Robbins DR, Enright PL, Sherrill DL: Lung function development in young adults: is there a plateau phase?. Eur Respir J. 1995, 8: 768-772.
Sherrill DL, Camilli A, Lebowitz MD: On the temporal relationships between lung function and somatic growth. Am Rev Respir Dis. 1989, 140: 638-644.
Van Pelt W, Borsboom GJJM, Rijcken B, Schouten JP, van Zomeren BC, Quanjer PH: Discrepancies between longitudinal and cross-sectional change in ventilatory function in 12 years of follow-up. Am J Respir Crit Care Med. 1994, 149: 1218-1226.
Wang X, Mensinga TT, Schouten JP, Rijcken B, Weiss ST: Determinants of maximally attained level of pulmonary function. Am J Respir Crit Care Med. 2004, 169: 941-949. 10.1164/rccm.2201011.
Kerstjens HAM, Rijcken B, Schouten JP, Postma DS: Decline of FEV1 by age and smoking status: facts, figures, and fallacies. Thorax. 1997, 52: 820-827. 10.1136/thx.52.9.820.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1741-7015/8/84/prepub
Acknowledgements
This research was funded by Philip Morris International, Inc. However, the opinions and conclusions of the researchers are their own and do not necessarily reflect the position of Philip Morris International, Inc. We thank Pauline Wassell and Diane Morris for typing the various drafts of the paper and Yvonne Cooper for assistance in obtaining the relevant literature. We also thank the referees for helpful comments which led to improvement of the paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
PNL, founder of P.N. Lee Statistics and Computing Ltd., is an independent consultant in statistics and an adviser in the fields of epidemiology and toxicology to a number of tobacco, pharmaceutical and chemical companies. JSF works for P.N. Lee Statistics and Computing Ltd.
Authors' contributions
PNL carried out the literature search and, with JSF's assistance, extracted the relevant data, carried out the statistical analyses, prepared a detailed report and drafted the manuscript for publication.
Electronic supplementary material
12916_2010_343_MOESM1_ESM.DOC
Additional file 1: Detailed search strategy. Fuller details of the search, summarized in Figure 1 in the paper, including the stages at which each of the examined papers was accepted and rejected. Note that the reference list of the paper itself includes not only those references cited in the paper but also those cited in this additional file. (DOC 266 KB)
12916_2010_343_MOESM2_ESM.DOC
Additional file 2: Data recorded on the study and beta databases. Fuller details of the variables recorded on the databases as summarized in Methods: Data entry. (DOC 158 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Lee, P.N., Fry, J.S. Systematic review of the evidence relating FEV1decline to giving up smoking. BMC Med 8, 84 (2010). https://doi.org/10.1186/1741-7015-8-84
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1741-7015-8-84