Abstract
Background
Maternal and neonatal health services are life-saving interventions for neonatal health outcomes. As Rwanda endeavors to accomplish sustainable development goals, adequate ANC is essential to lessen of neonatal mortality. The utilization of ANC continues to be inadequate and high neonatal mortality rate persevere in Rwanda. Understanding the direct and indirect factors that affect newborn health outcomes is necessary for well-targeted interventions. However, few studies had been conducted in Rwanda to evaluate the importance of ANC in improving neonatal health. This study therefore assessed the association between ANC and neonatal outcomes.
Methods
The Demographic and Health Surveys (DHS) are household surveys that are cross-sectional, nationally representative, and used to collect data on population, health, and nutrition. Data from the 2010,2015 and 2020 Rwanda Demographic and Health Surveys (RDHS) were used. The study involved 17,747 women between the ages of 15 and 49 who had a single live birth and at least one ANC visit in five years prior to each survey. Bivariate and multivariable logistic regression, a survey adjusted for clusters at multiple level, and the estimation of adjusted odds ratios (aOR) and 95% confidence intervals were used to evaluate the relationship between the outcome and independent variables.
Results
Out of 17,747 women ;7638(42.91%) of the mothers had adequate ANC visits and low birth weight (LBW) was found among 833(4.63%) neonates. The birth of a LBW baby (aOR:4.64;95%CI:3.19,6.74) was directly related to increased odds of neonatal death. Mothers aged 20–34 years (aOR:0.40; 95%CI:0.20,0.81), a preceding birth interval of 24months or greater (aOR:0.41:95%CI:0.28,0.60), baby being female (aOR:0.72; 95%CI:0.54,0.96), having adequate ANC visits (aOR:0.64;95% CI:0.46,0.89) and the birth order of the newborn being ranked second or third (aOR:0.60; 95%CI:0.38,0.95) were negatively associated with neonatal death.
Conclusion
Health education programs targeting teen and primigravida mothers should be encouraged. Among the newborn survival interventions, addressing short birth intervals and the effective management of LBW cases should be explored. The findings confirm the fundamental importance of adequate ANC in the neonatal survival.
Similar content being viewed by others
Introduction
Antenatal care (ANC) refers to the treatment given to pregnant women and adolescent girls by skilled health-care professionals in order to maximise the health of both mother and child throughout pregnancy [1]. Neonatal death, defined as death within the first 28 days of life, is one of the most pressing public health issues in low and middle-income countries (LMICs) [2,3,4]. In 2020, an estimated 2.4 million neonatal deaths were reported, reflecting a global burden of 17 neonatal deaths per 1000 live births, and the majority of these neonatal deaths took place in LMICs [2,3,4]. More than three-quarters (80%) of all newborn mortality occur in Central, South Asia, and Sub-Saharan Africa (SSA) [5]. With one in every 38 neonates dying before the age of one month, SSA has the highest rate of neonatal mortality [5].
Rwanda’s neonatal mortality rate is estimated to be 18 per 1000 live births, far higher than the UN Sustainable Development Goal (SDG) 3.2, which is to reduce neonatal mortality to less than 12 per 1000 live births [5,6,7].
The utilization of maternal health care services in Rwanda is below average except for the health facility delivery which is nearly 90% [8]. The adequacy of ANC and the utilization of postnatal care services within seven days following delivery is 47.2% and 12.8% respectively [8]. Nonetheless, these services are essential for identifying the fetus and maternal risk indications during pregnancy, labor, and postpartum [9, 10]. According to a study done in 57 LMICs, both adequate ANC visits and timing of first ANC were linked to lower odds of neonatal mortality [11]. A study done in Kenya, a country in the region revealed that missing any ANC was linked to neonatal mortality [12]. The 2016 World Health Organization (WHO) guidelines on ANC recommend at least 8 contacts for every pregnant woman; however, Rwanda still implements the 2001 policy which only recommended 4 visits [8]. The utilization of these services in Rwanda is challenged by individual, socioeconomic and community level factors [13,14,15]. Women’s unenlightenment on pregnancy complications [16] and the perceived barriers to utilizing health care [15] were found to be hindering ANC attendance in Rwanda.
Other challenges to the use of the maternal healthcare services include unskilled and poor attitude of health providers [17, 18]. A recent study found that the COVID-19 in Rwanda dramatically reduced the use of maternal and child health services [19].
The determinants of neonatal outcomes and maternal health-care utilization are always based on methods that assume direct rather than indirect relationships [20, 21]. Given that ANC is linked to better maternal and foetal health indicators and that Rwanda continues to have a high neonatal mortality rate, our study’s exposure is ANC and its outcome is neonatal death (death within 28 days of birth). We also studied other health services factors such as iron supplementation and tetanus injections during pregnancy to examine their association with neonatal outcomes in Rwanda settings. Few studies had been conducted at Rwanda country level to examine the associations between adequate ANC on neonatal death. We sought to breach this gap by exploring the associations between adequacy of ANC, various confounders and neonatal outcomes. This study adds on the scant evidence already available to help devise retention strategies for ANC attendance in the continuum of care and assess ANC services and their links to neonatal survival.
Methods
Study settings
Rwanda is landlocked country in the central eastern Africa. Its landscape is characterized by hills and with its 503 persons per kilometer square is ranked in the top 3 most densely populated countries in Africa [22]. The health system in Rwanda is organized as a three-level pyramid consisting of central, intermediate, and peripheral levels [23]. The central level includes the directorates of the Ministry of Health and the national reference hospitals. The intermediate level is represented by health districts and district hospitals. The peripheral level is represented by health centers and health posts, which include community health workers [23].
The central level, based in the capital city of Kigali, is responsible for the development of health policy, strategy, monitoring &evaluation as well as to coordinate resources at the national level. The intermediate, or district, level is represented by health district administration and the referral district hospitals. The district hospital is responsible for managing all health problems for a well-defined population, supervises health centres and communities and reports to the health district administration. The peripheral level located at the sector and cell levels is the operational unit represented by the health centres and the community-based organizations. It is comprised of first-level health facilities, particularly health centres and health posts. With participation from the community, the health facility plans, coordinates, and carries out health activities in its catchment area [23].
Most of women receive ANC at health centres, with the clinic and referral hospital only being utilized for particular tests like ultrasounds [24]. Health centers are understaffed and rural women have difficulties accessing them due to poor road networks in a hilly landscape, this negatively impact the ANC attendance as well as referral systems [25]. Inadequate ANC visits, poor attitude of health workers and a weak referral system in place might be contributing to a high neonatal mortality.
Study design and data source
This study is a cross-sectional study design that used secondary data from three waves of Rwanda Demographic and Health Survey (RDHS). The three waves are the RDHS 2010, RDHS 2015 and RDHS 2020.The RDHS is a cross-sectional survey that employs a two-stage sampling design to get a nationally representative household sample. In the first step, clusters (villages) are chosen from a list of all clusters in the country. Selecting households within each cluster is done in the second stage. Over the three waves, the women’s response has been high, exceeding 99%. The RDHS gathers information on mother and child health services during a time frame within the five years prior to the survey. More specifics to sampling design, sample size, study instruments, data collection, how informed consent was obtained, and other related procedure are described elsewhere [8]. The RDHS data are available at Measure DHS website at https://dhsprogram.com/data/available-datasets.cfm.
Analytic sample
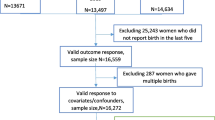
The 2010, 2015, and 2020 RDHS birth recode (BR) datasets were merged for the purposes of this study using accepted standards for handling DHS data. Women aged 15 to 49 years’ old who had a single live birth in the five years prior to each survey and had at least one ANC visit answered questions about ANC were included in this sample. Women with missing values or invalid responses to the main exposure, outcome, and possible confounders, such as “don’t know”, were drawn out. 17,747 of the 41,802 women who participated in the survey met the criteria for inclusion. More information is shown in Fig. 1.
Study variables
Outcome and exposure
The study had one dependent variable which is neonatal death, which was defined as the death of a newborn 28 days following birth. Neonatal death was dichotomous and coded 0 and 1 for no and yes respectively.
The main exposure variable was adequacy of ANC. Four ANC visits are considered adequate (coded 1) according to the policy in use in Rwanda during the time of the study. The visits were considered inadequate when they were less than four (coded 0).
We considered as control variables several socioeconomic, demographic and health service factors for their relevance in the uptake of ANC and the effect on neonatal death. These factors were adapted from Andersen’s behavioral model, Mosley and Chen [26]. Many studies have made use of the Andersen’s behavioral model and the analytical framework by Mosley and Chen to study the determinants of the maternal health services utilization and birth outcomes [26,27,28].
Categories were created for numerical values like age and birth order. Maternal age in years was tabulated into groups (15–19 years, 20–34 years, 35–49 years); the birth order of the baby was into three categories (1st, 2nd -3rd ,4th and above). Using principal component analysis, the household wealth index was created from data on the ownership of long-lasting assets, access to infrastructure and utilities, and dwelling features. Each woman was into five categories (poorest, poorer, middle, richer, and richest) depending on a household asset score, comprising 20% of the population. Later, these five categories were translated into three categories (poor, middle, and rich).
Statistical analyses
Stata v17.0 [29] was used for all of the statistical analysis. Descriptive statistics for the sociodemographic characteristics of the study participants by survey year were generated using the frequency and percentage as indicated in Table 1. We used chi-square tests to establish demographic and socio-economic factors associated with the outcome variable. Potential factors with p < 0.20 were retained for multivariable logistic regression in the final model. To assess the goodness of fit of the model we used AIC (Akaike’s information criterion). When covariates were found to be collinear, utilising the variance inflation factor (VIF > 4), the variable most correlated with the outcome variable was retained. We carried out all analyses utilizing the survey module “svyset” stata commands, taking into account clustering, stratification, and sample weight.
Results
From the results in Table 1, it can be observed that adequate utilization of ANC increased over the three survey waves. Adequate utilization of ANC increased from 36.10% in 2010 through 44.17% in 2015 to 48.58% in 2020. Majority of the respondents were young women of 20–34 years (67.97%) and they were ranked poor (43.51%). Most of the interviewed women (84.20%) resided in rural areas and had a primary school education (69.33%). Almost a half of the newborns were males (50.87%).
Table 2 shows the distribution of adequacy of ANC by background characteristics and the results of the bivariable analysis for the relationship between the factors and neonatal death are shown in the rightest column. In bivariable analysis, variables significantly associated with neonatal death are maternal age, the preceding birth interval, birth order, and low birthweight.
The interrelationship between adequate utilization of ANC and neonatal outcomes
Figure 2 shows the details of the interrelationship between adequacy of ANC utilization and neonatal death. The predictors of neonatal death were having adequate ANC, young age of mother, the preceding birth interval, the birth order and low birthweight. Young mothers had 60% decreased odds of neonatal death (aOR:0.40; 95%CI:0.20,0.81) compared to the adolescent mothers. Having adequate ANC visits decreased the odds of neonatal death by 36%(aOR:0.64;95% CI:0.46,0.89) compared to inadequate use of ANC.A preceding birth interval greater or equal to 24months reduced the odds of neonatal death by 59%(aOR:0.41; 95%CI:0.28,0.60) compared to a preceding birth interval of less than 24months. A second or third birth order reduced the odds of neonatal death by 40%(OR:0.60;95%CI:0.38,0.95) compared to the 1st birth order. Sex of newborn being female reduced the odds of neonatal death by 28%(aOR:0.72; 95%CI:0.54,0.96) compared to male newborns. Low birthweight increased the odds of neonatal death by almost five times (aOR:4.64; 95%CI:3.19,6.74) compared to normal birthweight newborns.
Discussion
The current study investigated the relationship between the adequate utilization of ANC and neonatal death in Rwanda. We found that the adequate utilization of ANC reduced by 41% the odds of neonatal death compared to the inadequate utilization of ANC.
The predictors of neonatal death were the adequate utilization of ANC, the age of the mother, the preceding birth interval, the birth order of the newborn, the sex of the newborn and low birthweight. When compared to inadequate ANC visits, adequate ANC visits had a lower risk of neonatal death. A recent hospital-based study in Rwanda discovered that women who received four or more ANC visits had a decreased incidence of LBW [30]. Several research have shown similar conclusions [20, 31,32,33]. A case-control study conducted in Brazil by Kassar S.B et al. in 2013 [20] and a case control study conducted in Ethiopia by Desta S.A et al. in 2020 [32] ound that four or more ANC visits were associated with a decreased risk in LBW. A cross-sectional study conducted in Bangladesh by Selina K et al. in 2008 [31] and a cross-sectional study in northern Uganda by Kananura et al. in 2017 [33] revealed that the increase in ANC visits were associated with normal birth weight. The World Health Organization (WHO) recommends at least four ANC checkups throughout pregnancy since this is a time when babies are vulnerable to issues such as preterm birth, restricted fetal growth, and congenital infections, all of which increase the likelihood of neonatal death [34]. In addition, attending ANC has been suggested as a possible avenue for mothers and their families to receive information and advice on obstetric care as well as the identification and management of infections such as Malaria, HIV/AIDS, syphilis, and other sexually transmitted diseases that affect the fetus [34]. This emphasizes the necessity of implementing population-based interventions that promote early ANC attendance [35].
In comparison to mothers aged 15–19, mothers aged 20–34 have a lower risk of newborn death. Studies in Ethiopia [36], Bangladesh, and Nepal have all reported similar results [37, 38]. Preterm birth or small-for-gestational-age are plausible mediating factors, according to a study conducted in Nepal [38], although neither of these variables were examined in our study. It’s also likely that a young mother’s perceived lack of childcare expertise is detrimental to their children’s health and survival [39]. The only way to effectively provide ANC for vulnerable populations is to integrate it with community-based public health programmes that target socioeconomic and lifestyle issues, such as youth care and social services [40].
In our research, preceding birth intervals of two years or more were found to less likely result in neonatal death than birth intervals of less than two years. This conclusion is in line with what has been discovered in Ethiopia and other developing Asian countries [36, 41,42,43]. The shorter birth interval impact could be linked to maternal depletion syndrome and resource sharing among siblings, as well as lower levels of care and attention for high-ranking infants [44, 45].
Our study revealed that LBW newborns were more likely to die during the neonatal period. Several studies have found that LBW babies are more likely to die [20, 46, 47]. According to these research, LBW babies are at a higher risk of a variety of health issues, which increases their chances of dying if proper care is not provided. Furthermore, the inadequate capacity of health services in LMICS to prevent, screen, and manage the issues associated with LBW babies makes it difficult for newborns to survive. As a result, interventions aiming at increasing health workers’ capacity to detect and care for LBW babies at health facilities are critical. LBW a leading cause of neonatal death could be due to small for gestational age, a variable that we were not able to capture in this study. perinatal and later adult health are significantly impacted by ANC. Maternal health and pregnancy outcomes could be significantly enhanced by health education aimed at adolescent girls, women, and their partners regarding ANC.
Strengths and limitations
The study’s use of a nationally representative population-based, combined dataset is a notable strength. We were able to generate a large sample size by merging the three surveys, which allowed us to assess the impact of various factors on neonatal outcomes with acceptable precision. Another feature of the study is that the DHS 5-year birth history data provide good to excellent information for estimating child mortality [48, 49]; this has been proven to lessen recall bias in the interview mothers’ reporting of birth and death dates [50, 51]. Decision-makers can benefit from the evidence-based information this study offered for implementing public health policies pertaining to ANC evaluations and improvement. Our study, on the other hand, contains a number of limitations. In the DHS, only surviving mothers were interviewed, and there could be an association between maternal death and newborn mortality, resulting in an underestimating of neonatal deaths. Data on key major determinants of maternal health-care consumption, such as health insurance, was only gathered for the most recent delivery, which limited our ability to assess the impact of such variables. Variables such as facility readiness, interpersonal relationships between clinicians and women, transportation, and other cultural norms and beliefs that could have influenced the uptake of antenatal care were not included in this study. Due to the cross-sectional nature of the data, we were only able to investigate relationships rather than causality.
Conclusion
Our findings demonstrate that the uptake of ANC has increased, which has improved newborn survival. Among the newborn survival interventions, addressing short birth intervals and the effective management of LBW cases should be explored. Addressing the coverage but also the quality of the content in ANC but also the skilling of the healthcare workers in dealing with risky obstetric conditions and equipping the health facilities with the essential tools for delivery care can potentially contribute to Rwanda’s achievement of the SDG goal 3.2 by 2030. Future research would carry out a longitudinal study examining the effect of several mediator variables from the ANC utilization to neonatal survival.
Data Availability
The datasets used during the current study are available from the DHS program website http://dhsprogram.com/data/available-datasets.cfm. but registration and application is required before access to data is granted.
Abbreviations
- ANC:
-
Antenatal Care
- RDHS:
-
Rwanda Demographic and Health Survey
- WHO:
-
World Health Organization
- LBW:
-
Low birth weight
- SDGs:
-
Sustainable Development Goals
References
Organization WH. WHO recommendations on antenatal care for a positive pregnancy experience. Geneva PP - Geneva: World Health Organization. https://apps.who.int/iris/handle/10665/250796.
Wang H, Bhutta ZA, Coates MM et al. Global,regional, national,and selected subnational levels of stillbirths, neonatal,infant, and under-5 mortality, 1980–2015: a systematic analysis for the global burden of Disease Study 2015. Lancet. 2016;388:1725–74.
WHO, UNICEF, UNFPA, World Bank Group UNPD. Trends in matrnal mortality:1990–2015. Geneva,Switzerland; 2015.
Hug L, Alexander M, You D et al. National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: a systematic analysis. Lancet Glob Heal. 2019;7:e710-20.
UNICEF, WHO, World Bank UD. mortality rate, neonatal. world bank group. 2020. https://data.worldbank.org/indicator/SH.DYN.NMRT?locations=RW. Accessed 2 Feb 2022.
UNICEF. Monitoring the situation of children and women. UNICEF. 2021. https://data.unicef.org/country/rwa/. Accessed 23 Feb 2023.
World Health Organization. World health statistics 2020:monitoring health for the SDGs,sustainable development goals. Geneva,Switzerland; 2020.
National Institute of Statistics of Rwanda(NISR) M of H (MOH)[Rwanda] and I. Rwanda Demographic and Health Survey 2019-20 final report. Kigali,Rwanda and Rockville,Maryland,USA; 2021.
Marsh DR, Darmstadt GL, Moore J, Daly P OD. Advancing newborn health and survival in developing countries:a conceptual framework. J Perinatol. 2002;22:572–6.
Zelalem Ayele D, Belayihun B, Teji K AAD. Factors Affecting Utilization of Maternal Health Care Services in Kombolcha District, Eastern Hararghe Zone, Oromia Regional State, Eastern Ethiopia. Int Sch Res Not. 2014;29.
Doku D, Neupane S. Survival analysis of the association between antenatal care attendance and neonatal mortality in 57 low- and middle-income countries. Int J Epidemiol. 2017;46.
Arunda M, Emmelin A AB. Effectiveness of antenatal care services in reducing neonatal mortality in Kenya: analysis of national survey data. Glob Heal Action. 2017;10.
Rwabufigili BN, Mukamurigo J, Thomson DR, Hedt-Gauthier BL SJ. Factors associated with postnatal care utilisation in Rwanda:a secondary analysis of 2010 demographic and Health Survey data. BMC Pregnancy Childbirth. 2016;16:122.
Hategeka C, Arsenault C KM. Temporal trends in coverage,quality and equity of maternal and child health services in Rwanda,2000–2015. BMJ Glob Heal. 2020.
Nisingizwe MP, Tuyisenge G, Hategeka C, Karim ME. Are perceived barriers to accessing health care associated with inadequate antenatal care visits among women of reproductive age in Rwanda? BMC Pregnancy Childbirth. 2020;20:1–10.
Kpienbaareh D, Kofinti RE, Konkor I, Amoak D, Kansanga MM LI. Knowledge of pregnancy Complications and utilization of antenatal care services in Rwanda. Int J Heal Plann Manag. 37:1680–93.
Doyle K, Kazimbaya S, Levtov R, Banerjee J, Betron M, Sethi R, et al. The relationship between inequitable gender norms and provider attitudes and quality of care in maternal health services in Rwanda: a mixed methods study. BMC Pregnancy Childbirth. 2021;21:156. doi:https://doi.org/10.1186/s12884-021-03592-0.
Ntigurirwa P, Mellor K, Langer D, Evans M, Robertson E, Tuyisenge L, Groves A LT. A health partnership to reduce neonatal mortality in four hospitals in Rwanda. Glob Heal. 2017;13:28.
Wanyana D,Wong R HD. Rapid assessment on the utilization of maternal and child health services during COVID-19 in Rwanda. Public Heal Action. 2021;11:12–21.
Kassar SB, Melo AM, Coutinho SB, Lima MC LP. Determinants of neonatal death with emphasis on health care during pregnancy, Childbirth and reproductive history. J Pediatr(Rio J). 2013;89:269–77.
Titaley CR, Dibley MJ, Agho K, Roberts CL, Hall J. Determinants of neonatal mortality in Indonesia. BMC Public Health. 2008;8:232. doi:https://doi.org/10.1186/1471-2458-8-232.
National Institute of Statistics of Rwanda(NISR). The fifth Rwanda Population and Housing Census,Main indicators Report. Kigali,Rwanda.
Rwanda M of H. Health Service Packages for Public Health Facilities [Internet]. 2017. Available from: www.moh.gov.rw, accessed August 2020). Kigali; 2017. www.moh.gov.rw.
Holmlund S, Ntaganira J, Edvardsson K, Lan PT, Semasaka Sengoma JP LKH et al. Health professionals’ experiences and views on obstetric ultrasound in Rwanda: a cross sectional study. PLoS One. 2018;13.
Uwimana G, Elhoumed M, Gebremedhin MA, Nan L, Zeng L. Determinants of timing, adequacy and quality of antenatal care in Rwanda: a cross-sectional study using demographic and health surveys data. BMC Health Serv Res. 2023;23:217. doi:https://doi.org/10.1186/s12913-023-09231-y.
Babitsch B, Gohl D LT. Re-visiting Andersen’s behavioral model of health services use:a systematic review of studies from 1998–2011. Psychosoc Med. 2012;9.
Beeckman K, Louckx F, Putman K. Determinants of the number of antenatal visits in a metropolitan region. BMC Public Health. 2010;10:1–9.
Guliani H, Sepehri A, Serieux J. Determinants of prenatal care use: evidence from 32 low-income countries across Asia, Sub-saharan Africa and Latin America. Health Policy Plan. 2014;29:589–602.
StataCorp. Stata Statistical Software: Release 17. 2021.
Akintije CS, Yorifuji T, Wada T, Mukakarake MG, Mutesa L YT. Antenatal Care visits and adverse pregnancy outcomes at a hospital in Rural Western Province,Rwanda. Acta Med Okayama. 2020;74:495–503.
Khatun S RM. Socio-economic determinants of low birth weight in Bangladesh: a multivariate approach. Bangladesh Med Res Counc Bull. 2008;34:81–6.
Desta SA, Damte A, Hailu T. Maternal factors associated with low birth weight in public hospitals of Mekelle city, Ethiopia: a case-control study. Ital J Pediatr. 2020;46:124. doi:https://doi.org/10.1186/s13052-020-00890-9.
Kananura RM, Wamala R, Ekirapa-Kiracho E, Tetui M, Kiwanuka SN, Waiswa P, et al. A structural equation analysis on the relationship between maternal health services utilization and newborn health outcomes: a cross-sectional study in Eastern Uganda. BMC Pregnancy Childbirth. 2017;17:98. doi:https://doi.org/10.1186/s12884-017-1289-5.
Lincetto O, Mothebesoane-anoh S, Gomez P MS. Antenatal Care:opportunities for Africa’s newborns. Int J Sci Technol Res. 2013;2:51–62.
Allemseged A, Mektie W SB. Maternal risk factors associated with low birth weight. J Coll Physicians Surg Pak. 2003;13:25–8.
Mekonnen Y, Tensou B, Telake DS, Degefie T BA. Neonatal mortality in Ethiopia:trends and determinants. BMC Public Health. 2013;17:483.
Kamal SM. What is the association between maternal age and neonatal mortality?An analysis of the 2007 Bangladesh demographic and Health Survey. Asia Pac J Public Heal. 2015;27:NP1106-17.
Sharma V, Katz J, Mullany LC, Khatry SK, LeClerq SC, Shrestha SR, Darmstadt GL TJ. Young maternal age and the risk of neonatal mortality in rural Nepal. Arch Pediatr Adolesc Med. 2008;162:828–35.
Obungu W, Kizito P, Bicego GT, Macro International I for RD. Trends, age patterns, and determinants of early childhood mortality in Kenya.DHS further analysis No. 12. Calverton, Maryland; 1994.
Denktaş S, Poeran J, van Voorst SF, Vos AA, de Jong-Potjer LC, Waelput AJM, et al. Design and outline of the healthy pregnancy 4 all study. BMC Pregnancy Childbirth. 2014;14:253. doi:https://doi.org/10.1186/1471-2393-14-253.
Shakya K MC. Neonatal mortality and maternal health care in Nepal:searching for patterns of association. J Biosoc Sci. 2001;33:87–105.
Arokiasamy P GA. Neonatal mortality in the empowered action group states of India:trends and determinants. J Biosoc Sci. 2008;40:183–201.
DaVanzo J, Hale L,Razzaque A RM. The effects of pregnancy spacing on infant and child mortality in Matlab, Bangladesh:how they vary by the type of pregnancy outcome that began the interval. Popul Stud(Camb). 2008;62:131–54.
Rutstein SO. Effects of preceding birth intervals on neonatal,infant and under-five years mortality and nutritional status in developing countries:evidence from the demographic and health surveys. Int J Gynaecol Obs. 2005;89 Suppl 1:S7-24.
Zenger E. Siblings’ neonatal mortality risks and birth spacing in Bangladesh. Demography. 1993;30:477–88.
Kananura RM, Tetui M,Mutebi A, Bua JN, Waiswa P, Kiwanuka SN et al. The neonatal mortality and its determinants in rural communities of Eastern Uganda. Reprod Health. 2016;16:13.
Oji S OC. Do place of delivery and delivery assistants matter? Open Demogr J. 2011;4:1–10.
Curtis SL. Assessment of the quality of data used for Direct Estimation of Infant and child mortality in DHS-II Surveys.Occasional Papers No.3. Calverton,Maryland; 1995.
Hill K. Approaches to the measurement of childhood mortality:a comparative review. Popul Index. 57:368–82.
Hall S. Neonatal mortality in Developing Countries:What can we learn from DHS data?(S3RI Applications and Policy Working Papers,A05/02. University of Southampton; 2005.
Mahy M. Childhood mortality in the developing world: A review of evidence for the Demographic and Health Surveys. DHS Comparative Reports No. 4. 2003. http://dhsprogram.com/pubs/pdf/CR4/CR4.pdf.
Acknowledgements
Not applicable.
Funding
The authors received a grant from Shaanxi Open Sharing Platform of Critical Disease Prevention and Big Health Data Science (Grant No.2023-CX-PT-47), which had no role in the study design, conceptualization of the study, analysis and interpretation of the data or the preparation and review of the manuscript.
Author information
Authors and Affiliations
Contributions
G.U conceptualized the study idea, obtained and cleaned data, performed data analysis, interpreted results and prepared the manuscripts. E.M and M.A.G contributed to the study design and analysis. Q.Q and M.M.A Wrote original draft and contributed to the study design, L.W contributed in the review and editing of the final manuscript. L.Z provided direct supervision, technical support in all aspects of this paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study is a secondary analysis of the 2010,2014-15 and 2019-20 RDHS data; approval to access and download data files from the online DHS archive was granted by worldwide DHS program.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1:
Crude and adjusted odds ratios for the relationship between adequate ANC and neonatal outcome.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Uwimana, G., Elhoumed, M., Gebremedhin, M.A. et al. Association between adequacy of antenatal care and neonatal outcomes in Rwanda: a cross-sectional study design using the Rwanda demographic and health surveys. BMC Health Serv Res 23, 1379 (2023). https://doi.org/10.1186/s12913-023-10345-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-10345-6