Abstract
Introduction
Proton pump inhibitor (PPI) abuse poses an overwhelming threat to the allocation of medical resources and places a heavy burden on global medical expenses. In this study, we put forward our prospective prescription review system and evaluated the effects of this system on clinical outcomes, rational medication use and costs related to PPIs.
Methods
A retrospective cohort study was conducted in which the included patients were divided into a preintervention group (2019.10–2020.09) and a postintervention group (2020.10–2021.09). To reduce the bias of patients’ baseline characteristics, the propensity score matching (PSM) method was employed. The primary endpoints were the incidence of stress ulcers (SUs), the improvement and cure rates of gastrointestinal haemorrhage, the defined daily dose (DDD), the drug utilization index (DUI) and the DDD/100 patient-days. The secondary endpoints included the types of unreasonable medication orders for PPIs, the PPI utilization rate and PPI costs.
Results
A total of 53,870 patients were included to evaluate the secondary endpoints, and 46,922 patients were paired by PSM and assessed to evaluate the primary endpoints. The number of PPIs used and PPI costs were significantly lower in the postintervention group than in the preintervention group (P < 0.001). The rationality evaluation results showed that the frequency of PPI use and the number of drug interactions were significantly higher in the preintervention group than in the postintervention group (P < 0.01). The proportion of patients taking oral PPIs was significantly increased in the postintervention group (29.30% vs. 34.56%, p < 0.01). For the utilization of PPIs both for prevention and treatment, the DUI and DDD/100 patient-days were substantially decreased in the postintervention group (P < 0.001 and P < 0.05, respectively). The incidence of SUs in the postintervention group was 44.95%, and that in the preintervention group was 51.93% (p < 0.05).
Conclusion
The implementation of the prospective prescription review system on rational PPI use correlated with reduced PPI costs, more rational PPI medication use and better clinical outcomes, and this system is worthy of long-term implementation for further improvement of rational drug use.
Similar content being viewed by others
Introduction
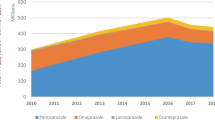
Critically ill patients are at high risk for experiencing stress ulcers (SUs). When using a positive faecal occult blood test or unexplained haemoglobin decline as the diagnostic criteria, the incidence of SUs in critically ill patients ranges from 15 to 50% [1]. To prevent the occurrence of SUs, proton pump inhibitors (PPIs) are considered effective and rank as the most commonly prescribed drugs worldwide [2]. However, with the surge in PPI expenditures, the irrational use of PPIs without evidence has increased rapidly [3], resulting in unreasonable financial expenditures. Forgacs I et al. [4] indicated that almost £2 billion are being spent on PPIs with unnecessary medication purposes each year worldwide. In addition to the economic waste of PPIs, adverse effects of long-term use and potential disadvantages in health issues have been identified and attracted the attention of researchers. The adverse effects of long-term use included increased risks of infections (lungs and gastrointestinal tract), bone fractures, liver and kidney damage, as well as a decrease in absorption of vitamins and minerals from the intestine [5,6,7,8,9]. In terms of potential harms, drug-drug interactions (DDIs) may occur when PPIs are added to polytherapy, which could result in unpredictable outcomes and threaten patients’ health [10].
In recent years, various measures have been taken to improve the abuse of PPIs globally. Clinical pharmacists, as the initiators of rational drug use, have been actively involved in this work and have achieved satisfactory results. Khalili H et al. [11] reported that clinical pharmacists introduced a treatment guideline for stress ulcer prophylaxis (SUP) based on a warranted evidenced protocol and assisted physicians in prescribing acid-suppressive therapy (AST) for SUP, which obtained reductions in the overall use of AST and the use of AST for patients without reasonable indications. Masood U et al. [12] showed that their clinical pharmacist team reviewed SUP patients during medical rounds, made appropriate changes according to the guidelines and educated residents and fellows on the implemented initiative of SUP, which caused a substantial reduction in the costs related to inappropriate SUP use. Moreover, Mitchell S et al. [13] described that their team owned prescriptive authority on decreasing inappropriate stress ulcer prophylaxis rates instead of recommendations, which could be more time-efficient and cost-saving. As in China, the “Consensus Review for SUP and Treatment” and “Prevention and Treatment of Stress Related Mucosal Disease” were released in 2015 and to some extent promoted the rational drug use of PPIs and the prevention of SUs [14]. Under the guidance, Chinese clinical pharmacists have been taking interventions to control PPI overuse on the premise of reducing the incidence of SUs in hospitals. The majority of the interventions are focused on daily rounds with physicians and educative group activities about the rational use of PPIs [15, 16]. Some pharmacists have explored classic management methods for improving rational PPI use. Yun H et al. [17] studied the application of the plan-do-check-act (PDCA) method in promoting rational prophylactic injectable proton pump inhibitor use (PIPU), while clinical pharmacists led a guidance team in providing pharmaceutical care.
In China, the prospective prescription review system is a real-time prescription monitoring system that requires clinical pharmacists to set rules for intercepting prescriptions with drug-related problems (DRPs) according to clinical guidelines, medical insurance policy, drug descriptions, etc. Since the National Health Commission issued a prescription review of medical institutions in July 2018, approximately 42.7% of hospitals have successively carried out a prospective prescription review system and achieved remarkable results [18]. Xie H et al. [19] reported that the introduction of the prescription review system was associated with safer prescribing of analgesics. However, to date, few studies have examined prospective prescription review systems regarding the promotion of rational PPI use.
Therefore, the clinical pharmacists in our hospital developed a prospective prescription review system correlating PPI prescriptions to the fasting state and all the related diagnoses of stressors. This system attempts to improve clinical outcomes associated with gastrointestinal bleeding while controlling unreasonable PPI use and reducing unnecessary PPI expenses.
Methods
Study setting
This was a retrospective preintervention/postintervention study conducted in Tongji University affiliated East Hospital. Tongji University affiliated East Hospital is a tertiary teaching hospital with 1800 beds in Shanghai. This hospital of two districts owns 9 ICUs and a wide range of general wards, including the Department of Cardiology, Department of Obstetrics and Gynecology, Department of Oncology, etc. In October 2018, the clinical pharmacists in the Department of Pharmacy launched a prescription review system, which provided a real-time prescription review for all outpatients and inpatients. The study protocol was approved by the Tongji University affiliated East Hospital Review Board (2020-092). The need for written informed consent was waived by the Research Ethics Committee of Tongji University affiliated East Hospital due to the retrospective nature of the study. All methods were conducted following relevant guidelines and regulations.
Risk assessment and prevention system of stress ulcers
The establishment of risk assessment and prevention of SUs was based on a prospective prescription audit system, which intends to remind doctors of prescriptions that may lead to DRPs. When there is DRP in the prescription issued by the doctor, the warning message will automatically pop up in the doctor’s work interface. If the doctor does not modify the prescription according to the warning message, he or she can select “request dispensing”. Then, the clinical pharmacist will receive this prescription in his or her work interface and will write recommendations according to the patient’s condition, and the clinical pharmacist will send the recommendations back to the doctor’s work interface for interaction. The doctor can choose to modify the prescription according to the pharmacist’s recommendations or reject the recommendations. On the premise of continuing the workflow above, the risk assessment and prevention system of stress ulcers aims to dynamically monitor and evaluate stressors and risk factors and promote the timely adjustment of the dosage and course of PPI treatment. It realizes the connection between PPIs and fasting state and all the related diagnoses of stressors. The details are as follows: (1) When doctors prescribe PPIs for patients without stressors or risk factors, the system will give timely warnings to intercept the prescriptions. (2) When doctors prescribe oral PPIs for patients at risk of gastrointestinal bleeding (stressor ≥ 1, or risk factors ≥ 2), the system will judge whether there are DRPs, and the warning message will automatically pop up in the doctor’s work interface. (3) When doctors prescribe intravenous PPIs for patients at risk of gastrointestinal bleeding (stressor ≥ 1, or risk factors ≥ 2), based on the process above, whether one more step to determine if intravenous administration is needed should be judged by the system. [Fig. 1].
Subject
The study patients were divided into two cohorts according to the implementation of the system: a preintervention cohort (2019.10-2020.9) and a postintervention cohort (2020.10-2021.9). We reviewed all the in-hospital prescriptions during this period. Two clinical pharmacists collected medical information on the patients’ demographics (sex, age, inpatient department, purpose of PPI use and length of hospital stay), diagnoses, drug information (drug name, dosage form, usage dates, specification, usage and dosage, and expenditures) and detailed in-hospital expenses from the Electronic Medical Record System (EMR). Data on intravenous PPI review points and irrational PPI evaluation results were collected from the prospective prescription system. Then, the collected data were cross-checked by two senior pharmacists. The inclusion criteria were as follows: (1) Patients with in-hospital prescriptions including PPIs (both the oral and intravenous administration forms); (2) Patients aged ≥ 18 years; and (3) Patients with admission and discharge diagnoses related to Zollinger-Ellison syndrome, peptic ulcer, gastroesophageal reflux, upper gastrointestinal bleeding, Helicobacter pylori infection and SUs. The exclusion criteria included the following: (1) Patients who were not discharged during the data extraction period; (2) Patients with incomplete in-hospital data; (3) Patients with histamine-2 receptor antagonist (H2RA) prescriptions during the in-hospital period; and (4) Patients with an admission time less than 48 h.
Variables and outcomes
Stressors were defined as underlying diseases that induced SUs, which mainly included the following [20]: (1) Mechanical ventilation duration > 48 h; (2) Coagulation mechanism disorder (an internal normalised ratio (INR) > 1.5, a platelet level < 50 × 109/L or a partial prothrombin time > 2); (3) History of peptic ulcer or upper gastrointestinal bleeding within 1 year; (4) Severe head injury and cervical spinal cord injury, with a Glasgow Coma Score ≤ 10 points(or cannot execute simple commands); (5) Severe burns (burn area>30%); (6) Severe trauma and multiple injuries; (7) Various difficult and complicated operations (operation time > 3 h, operation grade ≥ 3); (8) Kidney dysfunction or renal replacement therapy; (9) Acute liver dysfunction or chronic liver disease; (10) Acute respiratory distress syndrome (ARDS); 11) Shock or persistent low blood pressure (persistent low blood pressure duration>30 min; shock refers to a systolic blood pressure < 90 mmHg or lower than a basal blood pressure > 40 mmHg); 12) Sepsis; 13) Cardiovascular accident; and 14) Severe psychological stress, due to mental trauma or excessive stress.
The risk factors for Sus included [20, 21]: (1) An ICU hospital stay > 1 week; (2) A positive faecal occult blood duration > 3 days; (3) High-dose corticosteroid administration (250 mg/day of steroids or equivalent hydrocortisone); and (4) Nonsteroidal anti-inflammatory drug (NSAID) administration.
SUs were defined as no diagnosis related to gastrointestinal bleeding that was present in the admission diagnosis, but a diagnosis related to gastrointestinal bleeding or stress ulcer was demonstrated in the discharge diagnosis. SUs occurred in patients who were previously given preventive PPIs based on risk factors and stressors, related medical history, etc. PPI medications then replaced preventive PPI medications for treatment once upper gastrointestinal haemorrhage symptoms, signs and laboratory examination abnormalities appeared.
The defined daily dose (DDD) of PPIs was defined as “the average maintenance dose of a drug when used for its major indication in adults” and was calculated according to the recommendations in the WHO ATC/DDD Index 2019, the “Pharmacopeia of the People’s Republic of China-Clinical Medication Instructions” (2015 edition), the “Chinese Pharmacist and Physician Clinical Medication Guide”, etc.
The DDDs was calculated as follows: total PPI consumption/DDD. The higher the DDDs value was, the higher the frequency of use of the drug.
The drug utilization index (DUI) was calculated as follows: the sum of the DDDs of all PPIs for patients in each group/the total number of days the medication was used by the patients. The DUI can be used to evaluate the rationality of clinical medication use. A DUI greater than 1.0 means that the doctor’s daily dose is greater than the DDD, demonstrating unreasonable medication use.
The DDDs/100 patient-days was calculated as follows: the average DDDs of PPIs consumed per 100 patient-beds per day.
The SU incidence (%) was calculated as follows: the number of patients with SUs/the number of all patients with preventive PPI use ×100%.
Improvement and cure of gastrointestinal haemorrhage refer to the evaluation of improvement or cure added in the diagnosis related to gastrointestinal bleeding in the discharge diagnosis. Evaluation of the improvement rate and cure rate of gastrointestinal haemorrhage was performed for the patients who experienced PPI treatment medications.
The improvement and cure rates of gastrointestinal haemorrhage (%) was calculated as follows: the number of patients with improved or cured gastrointestinal haemorrhage/the number of all patients with PPI use ×100%.
PPI costs were calculated as follows: the number of patients with PPI drug costs in each group/the total number of patients in each group.
The Charlson Comorbidity Index (CCI) [22] is a weighted index that considers the number and seriousness of comorbid diseases according to a point system based on 19 comorbidities. Every comorbidity was assigned a weight of 1, 2, 3 or 6, and the CCI score was calculated by summing the weight of comorbidities. A CCI score of 0 indicated no comorbidities; a CCI score of 1 indicated one comorbidity; a CCI score of 2 indicated two comorbidities weighted as 1 or one comorbidity weighted as 2; a CCI score of 3 indicated three comorbidities weighted as 1 or one comorbidity weighted as 1 and one comorbidity weighted as 2; and a CCI score ≥ 4 indicated an estimated 10-year survival rate of less than 53%.
The primary endpoints were grouped as the incidence of SUs, the improvement rate and cure rate of gastrointestinal haemorrhage, the DDD, the DUI and the DDD/100 patient-days. The secondary endpoints included types of unreasonable medication orders for PPIs, the PPI utilization rate and PPI costs.
Statistical analysis
In this study, statistical analysis was conducted using SPSS 25.0 software (SPSS Inc., Chicago, IL, USA) for Windows. We used propensity score matching (PSM) to reduce the cofounding bias when comparing the clinical outcomes between the groups. To apply PSM, logistic regression was employed to calculate the propensity score values, which included age, sex, in-hospital departments, the CCI score and the PPI medication purpose. Nearest neighbour matching (1:1) was used as the matching method to calculate the standardized differences before and after PSM. When the variable fell between 0.0 ± 0.001, the matching then was stopped as a sign of reaching equilibrium. Continuous variables are presented as medians along with standard deviations (SDs) and were tested by grouped t tests. Other quantitative data are presented as the upper quartile (Q1) and lower quartile (Q3). Q2 is represented as the median. The number of patients (percent) was described categorically, and frequency comparison was analysed by the chi-square test or Wilcoxon rank sum test. P values equal to or less than 0.05 were considered statistically significant.
Results
A flow chart of the prospective prescription review is shown in Fig. 1. This figure shows how the intervention was performed on the rational use check of PPIs.
Table 1 presents the comparisons of PPI use and PPI costs. The number of PPIs used and PPI costs were significantly lower in the postintervention group than in the preintervention group (P < 0.001).
According to the data shown in Fig. 2, the number of unreasonable medical orders was 2736 and 4847 in the pre- and postintervention groups, respectively. The rationality evaluation results were categorized as follows: frequency of PPIs, PPIs course, drug interactions, PPIs for special populations, contraindications, administration route, dosage and incompatibility. The most common problem was the dosage, with 1060 (38.74%) and 1848 (38.13%) patients in the pre- and postintervention groups, respectively. The composition ratios of the frequency of PPIs and drug interactions were significantly higher in the preintervention group than in the postintervention group (P < 0.01). The PPI course in the preintervention group had a higher composition ratio than that in the postintervention group (P < 0.05). Of note, the composition ratio of PPIs for the special populations in the preintervention group was significantly lower than that in the postintervention group (P < 0.01).
As shown in Fig. 3, the number of medication orders in the pre- and postintervention groups was 30,888 and 30,379, respectively. The proportion of oral PPIs increased significantly after intervention (29.30% vs. 34.56%, p < 0.01), and there was a significant difference in unreasonable medical orders (8.86% vs. 15.96%, p < 0.01) between the two groups.
The review points of intravenous PPIs were presented as follows: upper gastrointestinal bleeding, vomiting blood (+), fasting, coma, faecal occult blood (+) and indwelling gastric tube. When doctors prescribed intravenous PPIs, the most common review point they chose was fasting (3633, 40.15%), followed by upper gastrointestinal bleeding (1550, 17.19%) and coma (1443, 15.95%) (Fig. 4).
The characteristics of the patients included in the analysis are shown in Table 2. Since the characteristics of age, sex, department, and CCI score were not comparable between the two groups, PSM was applied to make them comparable. After the adjustment for the demographic variables by PSM analysis, there were no significant differences in age, sex, department, CCI or purpose of PPI use between the two groups.
The purpose of PPI use was divided into prevention and treatment. For the utilization of PPIs for prevention, the total DDDs (231,765 vs. 202,541) and the DDDs/100 patient-days (110.71 ± 70.02 vs. 100.71 ± 69.68) were substantially decreased in the postintervention group (P < 0.001). Moreover, the DUIs between the two groups were 1.52 and 1.4, respectively. The number of days stayed in the hospital was significantly different between the two groups. For the utilization of PPIs for treatment, DUI and DDDs/100 patient-days were significantly different between the pre- and postintervention groups. The incidence of SUs in the postintervention group was 44.95%, and that in the preintervention group was 51.93% (P < 0.05). The improvement rate and cure rate of gastrointestinal haemorrhage in the two groups were not significantly different (Table 3).
Discussion
Previous studies have shown that clinical pharmacists have achieved satisfactory results in ICUs, surgical wards and medical wards regarding the interventions of reviewing indications for SUP, educating residents, and making ward rounds [12, 23−24]. The uniqueness of this study is that unlike some studies requiring that clinical pharmacists review prescriptions [25, 26], the tasks for clinical pharmacists were to set reasonable interception rules and wait for feedback from doctors when alerts occurred, which is a more efficient and cost-effective method. The findings in this study show that in the postintervention group, the total PPI utilization rate (PPIs used) and PPI costs decreased significantly compared to those in the preintervention group. The total PPI utilization rate in this study was lower than some of the previous studies domestically and worldwide [16, 27]. This means that reminding doctors of the utilization rules with this system has achieved the initial goal. In addition, the clinical pharmacists in our hospital have given PPI recommendations in clinical pharmacists’ consultations, which to some extent promoted the rational use of PPIs [28]. The findings demonstrated a significant reduction in PPI costs, which is consistent with what Chen QY et al. reported [29]. In October 2019, the government officially implemented the “4 + 7” centralized procurement policy and the price of drugs was greatly adjusted; Shanghai was among the 11 pilot cities. Chinese researchers found that the “4 + 7” policy had positive effects in promoting the substitution of generic drugs for original drugs, reducing drug prices and promoting rational drug use [30, 31]. For the change in PPI costs shown in Table 1, although PPI prices decreased several times during the study period, based on the consumption of drugs, we observed that there was a significant difference in the DDDs between the preintervention group and postintervention group (241,579 vs. 212,346, p < 0.001). The significant decrease in consumption suggested that even though the PPI prices remained stable during the study period, the PPI costs could be significantly reduced after the intervention. This indirectly indicated the significance of the system in reducing PPI costs. Furthermore, we do not need to take cost measurement into consideration in this study. Because clinical pharmacists do not have to spend much time reviewing prescriptions, salaries related to costs were partly saved, unlike the method presented in Bao ZW et al. [25].
We achieved the increased utilization of oral PPIs, instead of intravenous PPIs in this study. As indicated in a previous study [32] and expert consensus [33], for SUP, intravenous PPIs can be selected only when patients are unable to eat, which emphasizes the recommended use of oral PPIs. To improve the current status that includes a high utilization rate of intravenous PPIs and physicians’ lack of realization of indications for intravenous PPIs, we used this system to double check the appropriateness of intravenous PPIs (Fig. 1). Before an intravenous PPI medical order is prescribed, the reasons why intravenous PPIs rather than oral PPIs should be used must be selected (Fig. 4). All the interventions led to a significant reduction in utilization. For the intervention on the various types of irrational drugs, the setting of the rules was more detailed, which means that a prescription could be issued only after the rules were met. For example, one of the rules is that the routine treatment course of intravenously administered PPIs should be less than 7 days. If the treatment course exceeds this duration, the doctor should make sure that the patient is still fasting in the system. Due to the strict restrictions of the rules, the irrational prescriptions of medication frequency and treatment course and those with DRPs were significantly reduced. It is worth noting that the irrational utilization rate of special drug users, including pregnant women, children and people with liver and kidney dysfunction, significantly increased, demonstrating the advantage of this intervention method in intercepting unreasonable prescriptions for these groups over a previous study [13]. We set the rules for this group according to the drug instructions so that more clinical pharmacists’ efforts could influence them.
SUs have the characteristics of a low incidence rate and high mortality. According to the latest finding [34], the bleeding risk of ICU patients receiving SUP can be reduced by approximately 60%. Therefore, prevention is important to reduce the occurrence of SUs, and early application of acid suppressants has been shown to be an effective method. Among the recommended acid suppressants, oral PPIs ranked as the first choice by the guidelines [20, 35]. In this study, the incidence of SUs decreased after the intervention. In addition, the ratio of oral administration was significantly increased, while the ratio of intravenous administration was significantly reduced. The findings of this study showed a much better improvement than the reported research over 20 tertiary hospitals domestically, and this research demonstrated that the use rate of PPIs in hospitalized patients was 57.4% (of which intravenous administration accounted for 82.9%) [36]. Hohl CM et al. [37] reported that a reduced hospital stay could be achieved by pharmacist prescription review. In line with this finding, this study showed a significantly shorter hospital stay in the group that had PPIs for prevention. Furthermore, it is worth noting that the DUI and DDDs/100 patient-days*100 in the postintervention group were significantly lower than those in the preintervention group both for prevention and treatment, demonstrating that the frequency of clinical use and rational drug use was significantly improved. This improvement could be attributed to the implementation of a prospective review system on rational PPI use, with which physicians’ prescriptions could be prospectively reviewed by clinical pharmacists. However, for DUI, the results after the intervention were much higher than the previous findings reported by Zhang Y et al. [16] and Ying J et al. [38], which means multidimensional measures should be implemented to further reduce the DUI. An important issue identified in this study was that the DDDs/100 patient-days after the intervention were 100.71 ± 69.68 and 172.89 ± 100.81 for prevention and treatment, respectively, which were still much higher than the findings of previously reported studies [12, 16]. The reason was that our result covered all the indications of PPIs over the entire inpatient setting, including rational and irrational indications, instead of irrational indications or those limited to only one department.
To the best of our knowledge, this is the first retrospective study to evaluate the improvement of PPI use, patients’ clinical outcomes and medical expenses after implementing a prospective prescription review system in the entire inpatient setting. To reduce bias, a propensity score method was used to match the patients’ conditions. While this study has many methodological strengths, several limitations still exist. First, although this prospective prescription review system reflected the whole picture of how PPIs were used in the real-world inpatient setting, it was a single-centre study. To further study the advancement and advantages of this model, multicentre studies are needed. Second, based on the physicians’ relatively low recognition of the clinical pharmacists’ work, the current acceptance rate of prospective prescription review is only approximately 80%, which means that 20% of physicians choose to sign a guarantee to circumvent the obstruction of the system. Improving the physicians’ recognition is a goal that requires time to complete. A considerable number of physicians believe that clinical pharmacists should improve their professional level [39, 40]. Therefore, continuous improvement of clinical pharmacists’ abilities may be able to reduce these research limitations to some extent. Third, due to some inherent deficiencies in the design of the system, patients who need PPIs but are not prescribed PPIs cannot be included in the unreasonable medication use statistics. To address these issues, more reasonable review rules should be made. Finally, as pointed out in many Chinese studies [41, 42], National Centralized Drug Procurement has been implemented by the Chinese government since 2019. During procurement, the average bid-winning drug price was reduced by 52%. Therefore, the positive effect of the system on total drug costs cannot be accurately evaluated. To counteract this issue, evaluation could be performed after drug prices remain stable.
Conclusion
In this study, the implementation of the prospective prescription review system on rational PPI use correlated with reduced PPI costs, more rational PPI medications and better clinical outcomes, including a lower incidence rate of SUs and shorter in-hospital days for patients using PPIs for SUP. It is essential that clinical pharmacists and their methods to improve clinical medication use help physicians achieve better medical care quality. To obtain the best effect of this system, clinical pharmacists should develop more rational medication rules to cover more drugs. Furthermore, improving the expertise of pharmacists for higher recognition by physicians is meaningful not only for the system but also for pharmaceutical care.
Data Availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- AST:
-
Acid-suppressive therapy
- CCI:
-
Charlson Comorbidity Index
- DDD:
-
Defined daily dose
- DDDs:
-
Total consumption of PPI(g)/DDD
- DDDs/100 patient-days:
-
PPI use density
- DDIs:
-
Drug-drug interactions
- DRPs:
-
Drug-related problems
- DUI:
-
Drug utilization index
- EMR:
-
Electronic Medical Record System
- ICU:
-
Intensive Care Unit
- NSAIDs:
-
Nonsteroidal anti-inflammatory drugs
- PDCA:
-
Plan-do-check-act
- PIPU:
-
Prophylactic injectable proton pump inhibitor use
- PPI:
-
Proton pump inhibitor
- PSM:
-
Propensity score matching
- SUs:
-
Stress ulcers
- SUP:
-
Stress ulcer prophylaxis
References
Wei J, Chang J, Jiang R, Kang D, Li L, You C, Zhang J, Zhao G, Gao L, Huang Q, Luo D, Zhang H, Wu H, Wang S, Wang R. Risk factors for stress ulcer bleeding in neurocritical patients: a multi-center study. Chin J Neurosurg. 2018;34(2):129–33.
Larsen MD, Schou M, Kristiansen AS, Hallas J. The influence of hospital drug formulary policies on the prescribing patterns of proton pump inhibitors in primary care. Eur J Clin Pharmacol. 2014;70(7):859–65.
Patterson Burdsall D, Flores HC, Krueger J, Garretson S, Gorbien MJ, Iacch A, Dobbs V, Homa T. Use of proton pump inhibitors with lack of diagnostic indications in 22 midwestern US skilled nursing facilities. J Am Med Dir Assoc. 2013;14:429–32.
Forgacs I, Loganayagam A. Overprescribing proton pump inhibitors. BMJ. 2008;336(7634):2–3.
Maes ML, Fixen DR, Linnebur SA. Adverse effects of proton-pump inhibitor use in older adults: a review of the evidence. Ther Adv Drug Saf. 2017;8(9):273–97.
Kockerling D, Nathwani R, Forlano R, Manousou P, Mullish BH, Dhar A. Current and future pharmacological therapies for managing cirrhosis and its complications. World J Gastroenterol. 2019;25(8):888–908.
Lazarus B, Chen Y, Wilson FP, Sang Y, Chang AR, Coresh J, Grams ME. Proton Pump inhibitor use and the risk of chronic kidney disease. JAMA Intern Med. 2016;176(2):238–46.
Ma YJ, Cao ZX, Li Y, Feng SY. Proton pump inhibitor use increases hepatic encephalopathy risk: a systematic review and meta-analysis. World J Gastroenterol. 2019;25(21):2675–82.
Metz DC. Examining the potential relationship between proton pump inhibitor use and the risk of bone fracture. Gastroenterol Hepatol. 2011;7(12):831–3.
Cena C, Traina S, Parola B, Bo M, Fagiano R, Siviero C. Prescription of proton pump inhibitors in older adults with complex polytherapy. Eur J Hosp Pharm. 2020;27(6):341–5.
Khalili H, Dashti-Khavidaki S, Hossein Talasaz AH, Tabeefar H, Hendoiee N. Descriptive analysis of a clinical pharmacy intervention to improve the appropriate use of stress ulcer prophylaxis in a hospital infectious disease ward. J Manag Care Pharm. 2010;16(2):114–21.
Masood U, Sharma A, Bhatti Z, Carroll J, Bhardwaj A, Sivalingam D, Dhamoon AS. A Successful Pharmacist-Based Quality Initiative to Reduce Inappropriate Stress Ulcer Prophylaxis Use in an Academic Medical Intensive Care Unit. Inquiry. 2018 Jan-Dec;55:1–5.
Buckley MS, Park AS, Anderson CS, Barletta JF, Bikin DS, Gerkin RD, O’Malley CW, Wicks LM, Garcia-Orr R, Kane-Gill SL. Impact of a clinical pharmacist stress Ulcer Prophylaxis Management Program on Inappropriate Use in Hospitalized Patients. Am J Med. 2015;128(8):905–13.
Ye ZK, Liu Y, Cui XL, Liu LH. Critical appraisal of the quality of clinical practiceguidelines for stress ulcer prophylaxis. PLoS ONE. 2016;11(5):e0155020.
Xin CW, Dong Z, Lin MM, Li GH. The impact of pharmaceutical interventions on the rational use of proton pump inhibitors in a chinese hospital. Patient Prefer Adherence. 2017;12:21–6.
Zhang Y, Yang H, Kong J, Liu L, Ran L, Zhang X, Yun J, Gu Q. Impact of interventions targeting theinappropriate useof proton-pump inhibitors by clinical pharmacists in a hepatobiliary surgery department. J Clin Pharm Ther. 2021;46(1):149–57.
Hong Y, Ye ZQ, Gao Z, Rao Y. Continuous improvement onthe rationality of prophylacticinjectable PPIs usage by aclinical pharmacist-led guidance team at a Chinesetertiary teaching hospital. J Int Med Res. 2020;48(10):1–15.
Bian J, Wei L, Shao X, Wu K, Zhen J. Investigation and analysis of prescription review and evaluation in chinese hospitals. Chin hosp. 2020;24(2):8–11.
Xie H, Zhang H, Peng J, Li L, Geng Y, Ge W. Prospective prescription review system promotes safe use of Analgesics, improves clinical outcomes, and saves medical costs in Surgical Patients: insights from Nanjing Drum Tower Hospital. Adv Therapy. 2022;39(1):441–54.
Bo Y, Li YQ, Ren X, Li ZS. Expert Recommendations on Stress Ulcer Prevention and Treatment (2018).Natl Med J China.2018;98(42):3392-5.
Quenot JP, Thiery N, Barbar S. When should stress ulcer prophylaxis be used in the ICU? CurrOpin Crit Care. 2009;15(2):139–43.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Meng HY, Yip G, Edwards A, D’Intini V, Tong E. Appropriateness of proton pump inhibitor use in patients admitted under the general medical unit. J Pharm Pract Res. 2019;49(5):447–53.
ChelseaLT, Cindy B, Sherilyn JY, Bekeart L, Anglemyer A, Tsourounis C, Rennke S. An Interprofessional Approach to reducing the overutilization of stress Ulcer Prophylaxis in Adult Medical and Surgical Intensive Care Units. Annals of Pharmacotherapy.2014;48(4).
Bao Z, Ji C, Jing H, Luo C, Fang W. Clinical and economic impact of pharmacist interventions on sampled outpatient prescriptions in a chinese teaching hospital. BMC Health Serv Res. 2018;18(1):519.
Renaudin P, Coste A, Audurier Y, Berbis J, Canovas F, Jalabert A, Castet-Nicolas A, Mercier G, Villiet M, Dagneaux L, Breuker C. Clinical, economic, and Organizational Impact of the clinical pharmacist in an orthopedic and trauma surgery Department. J Patient Saf. 2021;17(8):e1507–13.
Ramirez E, Lei SH, Borobia AM, Piñana E, Fudio S, Muñoz R, Campos A, Carcas AJ, Frias J. Overuse of PPIs in patients at admission, during treatment, and at discharge in atertiary spanish hospital. Curr Clin Pharmacol. 2010;5(4):288–97.
Fan X, Chen D, Bao S, Bai R, Fang F, Dong X, Zhang Y, Zhang X, Ma Y, Zhai X. Integrating Multidisciplinary Individualized Medication Recommendations into the Traditional Pharmacists’ Consultation Method: A Retrospective Study Using Propensity Score Matching Analysis. Inquiry. 2022 Jan-Dec;59:469580221081437.
Chen Q, Wang Q, Zhang Y. Clinical intervention increases rational use of Proton Pump inhibitors in the general surgery Department. Front Pharmacol. 2022;13:864081.
Wang Y, Xu W, Lu N, Zhang S, Shang B, Liu C, et al. Analysis of the effect of “4 + 7”centralized procurement policy implementation: based on the drug sales data of 9 pilot regions. Chin J Health Policy. 2021;14(02):36–43.
He J, Tang M, Cong L, Xu Y, Song J, Chen M et al. The impact of National Centralized drug procurement on the clinical management and drug use. Chin Health Resour. 2021:1–3.
Nasser SC, Nassif JG, Dimassi HI. Clinical and cost impact of intravenous proton pump inhibitor use in non-ICU patients. World J Gastroenterol. 2010;16(8):982–6.
Writing Group of Expert Consensus on the Preventive Application of Proton Pump Inhibitors. Expert consensus on the preventive application of proton pump inhibitors. J Chin Phys. 2018;12(20):1775–81.
Scarpignato C, Gatta L, Zullo A, Blandizzi C, SIF-AIGO-FIMMG Group. Italian society of Pharmacology, the Italian Association of Hospital Gastroenterologists, and the Italian Federation of General Practitioners. Effective and safe proton pump inhibitor therapy in acid -related diseases -A position paper addressing benefits and potential harms of acid suppression. BMC Med. 2016;14(1):179.
Zhao YP. Prevention and treatment of stress related mucosal disease: consensus of experts in general surgery in China (2015). Chin J Pract Surg. 2015;35(7):728–30.
Mao XF, Yang ZW. Medical big data analysis of the clinical off-label use of proton pump inhibitors. The J Pharm Pract. 2020;38(2):184–8.
Hohl CM, Partovi N, Ghement I, Wickham ME, McGrail K, Reddekopp LN, Sobolev B. Impact of early in-hospital medication review by clinical pharmacists on health services utilization. PLoS ONE. 2017;12:e0170495.
Ying J, Li LC, Wu CY, Yu ZW, Kan LD. The status of proton pump inhibitor use: a prescription survey of 45 hospitals in China. Rev EspEnferm Dig. 2019;111(10):738–43.
Wu TX, Wang B, Wang YD. Evaluation of clinical pharmaceutical care by doctors in five “top three. Hosp Beijing Chin Pharm J. 2016;36:5066–8.
B´echet C, Pichon R, Giordan A, Bonnabry P. Hospital pharmacistsseen through the eyes of physicians: qualitative semi-structured interviews. Int J Clin Pharm. 2016;38(6):1–14.
Wang N, Yang Y, Xu LX, Mao ZF, Cui D. Influence of Chinese National Centralized drug procurement on the price of policy-related drugs: an interrupted time series analysis. BMC Public Health. 2021;21(1):1883.
Long H, Yang Y, Geng X, Mao Z, Mao Z. Changing characteristics of Pharmaceutical prices in China under centralized procurement policy: a Multi-Intervention interrupted Time Series. Front Pharmacol. 2022;13:944540.
Acknowledgements
The authors wish to thank the staff of the Pharmacy Department and all the physicians and patients for supporting the study.
Funding
Key Specialties Foundation of Clinical Pharmacy of Shanghai Municipal Health Commission in China, Grant/Award Number: SWLCYXZX-2018-001; Research on the Epidemiology of Severe Drug-induced Diseases of the Chinese Society of Toxicology, Grant/Award Number: CST2019CT304.
Author information
Authors and Affiliations
Contributions
XBZ and YBM conceived and designed this study. XCF wrote the manuscript. DXC participated in the modification of the manuscript. SWB, RB and FF managed the data collection. XHD analyzed the data. YYZ, XGZ and WJT contributed to revisions to the manuscript. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All methods were conducted following relevant guidelines and regulations. This study was approved by the Research Ethics Committee of Tongji University affiliated East Hospital Review Board (2020-092). The need for written informed consent was waived by the Research Ethics Committee of Tongji University affiliated East Hospital due to the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fan, X., Chen, D., Bao, S. et al. Prospective prescription review system correlated with more rational PPI medication use, better clinical outcomes and reduced PPI costs: experience from a retrospective cohort study. BMC Health Serv Res 23, 1014 (2023). https://doi.org/10.1186/s12913-023-09931-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-09931-5