Abstract
Background
Multidisciplinary team meeting (MDM) processes differ according to clinical setting and tumour site. This can impact on decision making. This study aimed to evaluate the translation of MDM recommendations into clinical practice across solid tumour MDMs at an academic centre.
Methods
A retrospective audit of oncology records was performed for nine oncology MDMs held at Liverpool Hospital, NSW, Australia from 1/2/17–31/7/17. Information was collected on patient factors (age, gender, country of birth, language, postcode, performance status, comorbidities), tumour factors (diagnosis, stage) and MDM factors (number of MDMs, MDM recommendation). Management was audited up to a year post MDM to record management and identify reasons if discordant with MDM recommendations. Univariate and multivariable regression analyses were performed to assess for factors associated with concordant management.
Results
Eight hundred thirty-five patients were discussed, median age was 65 years and 51.4% were males. 70.8% of patients were presented at first diagnosis, 77% discussed once and treatment recommended in 73.2%. Of 771 patients assessable for concordance, management was fully concordant in 79.4%, partially concordant in 12.8% and discordant in 7.8%. Concordance varied from 84.5% for lung MDM to 97.6% for breast MDMs. On multivariable analysis, breast and upper GI MDMs and discussion at multiple MDMs were significantly associated with concordant management. The most common reason for discordant management was patient/guardian decision (28.3%).
Conclusion
There was variability in translation of MDM recommendations into clinical practice by tumour site. Routine measurement of implementation of MDM recommendations should be considered as a quality indicator of MDM practice.
Similar content being viewed by others
Introduction
Multidisciplinary team meetings (MDMs) are a cornerstone of oncology management. MDMs can significantly alter management plans [1–7], are highly likely to recommend care in accordance with clinical practice guidelines [2, 5, 8–11] and increase utilisation rates of treatment [12–14]. MDMs have been documented to improve diagnostic and staging practice, reduce time to treatment and improve survival in some cancers [14–17].
The structure and process of MDMs varies in different clinical settings and for different tumour sites. This can impact on MDM decision making and whether MDM recommendations are implemented into clinical practice [3, 18]. In a systematic review by Lamb et al., MDM decisions could not be implemented in 1–16% of cases often due to patient preferences or comorbidities precluding MDM recommended treatment [3]. An UK study found that MDM recommendations were translated into practice in 91.3% of cases across 14 tumour sites [19]. A German study reported 66% full implementation and 14% partial implementation of MDM decisions across three tumour types [20]. Other studies have shown variable implementation rates of 88% in skin cancer [10], 70–84% in head and neck cancer [6, 20], 80–96% in upper gastrointestinal cancers [13, 21–23], 67–96% in lung cancer [7, 24–26], 97% in thoracic cancers [4], 64–91% in brain cancer [20, 27], 80–90% in colorectal cancer [5, 13, 17, 28], 78% in gynaecological cancer [29], 82–95% in breast cancer [30–33], and 59–73% in sarcomas [20].
There is a paucity of Australian data regarding the clinical translation of MDM recommendations. These are confined to head and neck cancer [6], lung cancer [7], genitourinary cancer [1, 13], gastrointestinal cancer [13] and breast cancer [32, 33]. These are largely small studies of individual tumour site MDMs. The aim of this study was to comprehensively evaluate the translation of MDM recommendations into clinical practice for all solid tumour site MDMs at an Australian academic oncology centre and investigate whether there was significant variation by MDM type. We hypothesised that there would be significant variation in clinical translation of MDM recommendations by MDM type due to the different underlying patient characteristics of different cancer populations and differences in complexity of management. The secondary aim was to identify factors associated with MDM concordant management and identify reasons for discordant management.
Methods
This was a retrospective audit of oncology and medical records for nine solid tumour site MDMs which occurred between the 1st February and 31st July 2017 at Liverpool Hospital, NSW, Australia. All MDMs were held solely within Liverpool Hospital except for the lung MDM which was videoconferenced with Campbelltown Hospital. These MDMs are attended by all medical specialists involved in diagnosing or treating the particular cancer as well as pathologists, radiologists, nuclear medicine physicians and /or palliative care physicians where relevant. In terms of additional staff, all MDMs are attended by nurse care coordinators, the head and neck MDM by a dietitian and speech pathologist, the upper gastrointestinal MDM by a dietitian and the breast MDM by a geneticist. Electronic meeting agendas recorded in MOSAIQ® were used to identify patients. All patients listed in the MDM agendas were audited and excluded only if there was no evidence of MDM discussion. Ethics approval was obtained for this study from the SWSLHD Human Research Ethics Committee.
All MDMs were electronically documented in either MOSAIQ® or Powerchart™. Five MDMs used a template for recording MDM data either in MOSAIQ® (skin, lung, gynae-oncology) or Powerchart™ (colorectal, upper gastrointestinal). The subheadings used in each template are shown in Table 1. Except for the lung MDM, all data was recorded during the meeting as free text under these subheadings. For the lung MDM, some data was collected in a systematic format before the meeting and the rest was filled in as free text during the meeting. The remaining MDMs used documented MDM discussion and recommendations as free text.
Four researchers extracted data for this study. To ensure consistency, a data collection template was used and a random audit performed by a second investigator of 10% of each MDM data. For patients discussed on multiple occasions, data were collected for all MDMs which occurred during the study period. The data collected included patient factors (age, gender, country of birth, preferred language, residential postcode, Eastern Cooperative Oncology Group (ECOG) performance score, Charlson comorbidity index (CCI) [34]), tumour factors (diagnosis, diagnosis date, stage according to AJCC 7th edition) and MDM factors (date, consensus, treatment intent).
Patient’s culturally and linguistically diverse (CALD) status was categorised into “Non-CALD”, “CALD, English”, “CALD, Non-English” or “Unknown” based on country and birth and language. Non-CALD patients included those born in Australia and in countries (Canada, USA, UK, New Zealand and South Africa) where Australia has received significant numbers of English speaking migrants. CALD patients were all those born elsewhere. Postcode of residence was used to assign the Index of Relative Socio-economic Disadvantage (IRSD) quintile [35]. ECOG performance score was recorded if documented in clinical notes a month either side of the MDM date. CCI was calculated by scoring patient comorbidities [34] and then categorised into groups (None, 1–2 and 3+).
MDM presentation was categorised into “MDM Specific Cancer” if this was related to the tumour site of the MDM, “Other Cancer” if this was a primary cancer different to the MDMs tumour site, “Non-Cancer” if the presentation was not related to cancer and “Unknown” groups. Stage was categorised into four groups for data analysis “0–3”, “4/Malignant central nervous system (CNS) tumour”, “Benign tumours” and “Unknown”.
MDM Consensus was categorised as “No further treatment/Clinical follow up”, “Treatment Recommended” and “Other”. “Treatment recommended” included surgery, radiotherapy, systemic therapy and palliative care. The “other” category included recommendations for further imaging or biopsy or genetic testing. For patients presented at multiple MDMs, an overall MDM consensus and management intent was derived after the last MDM. Management intent was categorised as either “Palliative”, “Curative” or “Unknown” as determined by MDM notes and treatment offered.
To assess concordance of management with MDM recommendation, management was audited up to 1 year after the MDM. Patients were categorised as concordance “not assessable” if there was loss to follow-up (including death) after MDM presentation. For the remaining patients, concordance was grouped into “Fully concordant”, “Partially concordant”, and “Not concordant”. Fully concordant was defined as completion of all MDM recommended management within 1 year of discussion, partially concordant was completion of some but not all recommended management within a year and not concordant was lack of implementation of any MDM recommendations. Where management was not concordant with MDM recommendations, medical records were reviewed to ascertain the reason and categorised as “Patient/Guardian Decision”, “Clinician Decision”, “Comorbidity”, “Change in Stage”, “Change in Performance status”, “Other” (for reasons other than previous labels) or “Unknown”.
Statistical analysis was performed using Excel and IBM® SPSS Statistics, V26 (IBM Corporation, New York, USA). Patients whose concordance was not assessable were excluded from concordance rates calculations. MDM consensus was grouped into concordant (fully or partially) and non-concordant for analyses and the proportions in each group for potential influencing factors were tested for statistical significance through chi-square test. These factors were further tested for their strength of relationship with concordance level using univariate and multivariable logistic regression analyses. The factors tested were age, gender, country of birth, preferred language, CALD status, IRSD quintile, ECOG Performance Status score, CCI score, MDM tumour site, stage, reason for presentation, number of MDMs, management and overall consensus. Those factors with a p-value less than 0.2 on univariate analysis were entered into a combined multivariable model to assess their individual effect on concordance in presence of other factors.
Results
There were 835 patients discussed at the MDMs during the 6 month period (Table 2). The lung, breast and upper gastrointestinal MDMs were busiest whilst the skin and genitourinary MDMs had the fewest patient discussions. Overall median age of patients was 65 years but this varied from 53 years in the neuro-oncology MDM to 70 years in the lung MDM. 25.1% came from a CALD Non-English background, highest for breast MDM patients (35.4%) and lowest for skin MDM patients (6.5%). 54.9% resided in the two lowest socioeconomic quintiles.
ECOG performance status was unknown in 42.5% of patients and was only well recorded for the lung MDM. 12.2% had a Charlson Comorbidity Index (CCI) of 3 or higher but this varied from 6.8% in the neuro-oncology MDM to 23.8% in the lung MDM. 44.7% of presented cases were Stage 0–3 and 28.4% were either Stage 4 or malignant CNS tumour. Stage 0 comprised 14 patients with in-situ cancers. The head and neck, lung and upper gastrointestinal MDMs had a higher proportion of patients with stage 4 disease. The only discussion of benign pathology was at the neuro-oncology MDM.
88.3% of presentations were for the MDM specific tumour and 70.8% were presented at first diagnosis. 77% of patients were discussed at one MDM and 19.9% at a second MDM. The most common recommendation was for treatment (73.2%). The neuro-oncology MDM was most likely to recommend no further treatment or clinical follow-up. Overall management intent was curative in 74.1%. Palliative management was more likely to be recommended by the lung and colorectal MDMs.
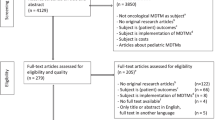
For analysis of concordant management with MDM recommendations, 64 patients were excluded due to loss to follow-up (n = 50), patient death shortly after MDM (n = 5), no documented management recommendations (n = 7) and other reasons (n = 2). Of the remaining 771 patients, MDM recommendations were fully translated in 612 (79.4%) patients and partially translated in 99 (12.8%) patients. Clinical management was not concordant with MDM recommendations in 60 (7.8%) patients. Concordance by tumour site MDM is shown in Fig. 1. Full concordance ranged from 67.9% in the genitourinary MDM to 90.4% in the neuro-oncology MDM. Any concordance was equally high for the breast (97.6%), neuro-oncology (97.3%) and gynae-oncology (97%) MDMs and lowest for the lung MDM (84.5%).
The commonest reason for non-concordant management was patient or guardian decision (28.3, 95% CI 18.2–40.4%) (Table 3). In 16.7% (95% CI 9.6–28.4%) there was lack of documentation of implementation of MDM recommendations. Clinician decision was responsible for 10% (95%CI 4.7–20.1%) of discordant reasons, and change in performance status or disease stage, 5% (95% CI 1.7–13.7%) each. Reasons were unable to be ascertained in 20% (95% CI 11.8–31.8%).
On univariate analysis, patients discussed at breast, neuro-oncology, upper GI and gynae-oncology cancer specific MDMs and had multiple MDMs during the study period showed significantly higher management concordance whereas patients with increasing age, CCI score 3+, unknown presenting diagnosis, unknown stage, unknown treatment intent, and with other consensus had significantly lower concordance (Table 4). After these significant variables were included in a multivariable model, age was no longer significantly associated with management concordance although the odds ratio reduced with increasing age (Table 4). Factors that remained significantly associated with concordance included tumour site, number of MDM discussions and overall consensus. Patients discussed at the breast (OR 5.61, 95% CI 1.51–20.82, p = 0.01) and upper gastrointestinal MDMs (OR 2.93, 95% CI 0.99–8.60, p = 0.05) had significantly higher concordance with MDM recommendations compared to those discussed at lung MDMs. Patients discussed at multiple MDMs were more likely (OR 2.92, 95% CI 1.17–7.23, p = 0.02) to have concordant management. Those whose overall consensus was other, were less likely to have concordant management (OR 0.19, 95% CI 0.07–0.51, p = 0.001).
Discussion
This study provides a comprehensive audit of solid tumour MDM practice at an academic institution. Four MDMs (head and neck, gynae-oncology, neuro-oncology and genitourinary) were held only at Liverpool Hospital. Liverpool Hospital is the sole tertiary referral hospital in South Western Sydney Local Health District providing the only surgical services for head and neck cancers, gynae-oncology and neuro-oncology. Additional MDMs existed at secondary hospitals in SWSLHD for breast cancer (2), upper gastrointestinal cancer (1) and lung cancer (1). The number of patients discussed varied amongst the MDMs. This is partially explained by the varied incidence of cancers and availability of other MDMs. For the major tumour sites, the number of patients discussed at the Liverpool Hospital MDMs represented approximately 14% of genitourinary cancers, 45% of breast cancers, 32% of bowel cancers and 59% of respiratory cancers diagnosed in SWSLHD for a 6 month period [36]. There is an underrepresentation of discussion of genitourinary cases at MDMs, a similar finding to Atwell et al. [37] In Australia, the decision to discuss cases at a MDM is made by the clinician and not mandated by legislation as in France [25] or for cancer society certification as in Germany [20].
Overall there was a high rate of translation of MDM recommendations into clinical practice although this did vary by MDM tumour site. The highest rates of any concordance were seen in the breast and neuro-oncology MDMs. Patient presentations at these MDMs are usually post-operative, as per clinician preference, hence the decision is often about adjuvant therapies only. The younger age of the neuro-oncology patients and lower comorbidity burden in both groups may make it easier to implement recommendations. On multivariable analysis, breast and upper gastrointestinal MDMs were significantly associated with concordant management compared to the lung MDM, although the latter result was of borderline significance. For all the remaining MDMs, odds ratios were greater than one suggesting higher concordance than the lung MDM although this did not reach statistical significance. Lung cancer patients are usually presented de novo where a choice between multiple treatment modalities must be made. In addition these patients had the highest median age and higher rates of comorbidities which impacts on the ability to implement MDM recommendations. Previous analysis in this patient group has shown that although the lung MDM recommends guideline-based treatment in 71% [11] only 54% of patients receive this, largely due to declining performance status, large tumour volumes and comorbidities [8].
Discussion at multiple MDMs was significantly associated with concordant management. This is likely to reflect the collection of further information whether this is patient related (eg assessment of comorbidities or preference) or cancer related (eg imaging or pathology) to better characterise the patient and tailor the MDM recommendation. All the necessary information may not always be present at the first MDM discussion. Goolam-Hossen et al. reported availability of new clinical information in upper GI MDMs as a reason for management change in one third of discordant cases [23]. A survey of clinicians found that a barrier to non-implementation of MDM recommendations was lack of consideration of patient choice or comorbidities [38].
MDM consensus of “other” was significantly associated with lack of concordant management. This category had a small number of patients with diverse MDM recommendations so no firm conclusions can be drawn. Management concordance declined with age although this was not significant on multivariable analysis. Studies of breast MDMs have found older age (> 70–75 years) [31, 33] and younger age (< 35 years) [33] were associated with discordant management. Similarly, concordance declined with increasing CCI score but did not reach statistical significance, suggesting MDMs were taking this into account when making recommendations. Of note, sociodemographic factors such as cultural and linguistic diversity and socioeconomic disadvantage were not associated with translation of MDM recommendations confirming equity of care in a diverse patient population. This may reflect Australia’s universal health care system. In contrast, an American study of lung cancer MDMs found that health insurance status and race were significantly associated with discordant care [24].
Comparisons of management concordance with MDM recommendations in the literature are complicated because of different study populations and use of methodologies (Table 5). Some studies measured only specific MDM recommendations such as adjuvant treatment for breast cancer [32] or radiotherapy for lung cancer [26] whilst others like ours recorded all decisions including biopsy, imaging, treatment, observation and supportive care [4, 7, 17, 24, 27, 28]. Some studies excluded recommendations for investigations, supportive care or management of recurrent disease [23] whilst others included recommendations for clinical trials and genetics referrals [33].
This study reports concordance rates per patient. Other studies have reported concordance rates either per patient, per decision or both (Table 5). Reporting concordance per MDM decision will identify if there are specific management recommendations that are not being implemented. Conversely, reporting concordance per patient enables us to gain an overview of overall patient management allowing for multifaceted recommendations which are common. However, the downside of this is management will be considered partially concordant if any recommendations such as further investigations are not implemented.
We chose to report both full and partial concordance with MDM recommendations as management decisions often involve multiple recommendations and may involve multiple MDM presentations. Only Caudron et al. [10] and Hollunder et al. [20] also report full and partial concordance for MDM recommendations. Others have explicitly defined concordance as having all aspects of MDM recommendation implemented [7, 30]. However it is unclear how the majority of studies approach this as they report concordant or discordant translation of MDM recommendations often after just the first MDM. Despite all these caveats, our rates of MDM recommendation concordance with clinical practice are in keeping with published literature across all tumour sites.
The commonest reason for non-concordant management was patient or guardian decision seen in 28.3% similar to the 31–36% reported in the other multiple MDM studies [19, 20]. Patient choice is a common reason for non-concordant management in breast MDMs ranging from 42 to 71%, usually in relation to the acceptance of adjuvant therapy after surgery [21, 30, 32]. In other cancer MDMs patient decision is responsible for discordant management in 11–54% in lung cancer [7, 24, 25], 18–34% in upper gastrointestinal cancers [21, 23], 44% in skin cancer [10], 45% in head and neck cancers [20], 33% in neurological tumours [20] and 14% in sarcomas [20]. Clinician decision not to implement MDM recommendations comprised 10% of reasons, less than the 23–24% reported by the other multiple MDM studies [19, 20]. In other studies this varies from 20% for breast [31], 30% for liver cancer [39] and 8–61% for lung MDMs [24, 25]. A possible reason for these differences is that it is sometimes hard to separate pure clinician decision from other causes such as patient’s poor performance status and comorbidity, which may have been included encompassed in clinician decision as a reason.
We found comorbidity as cause on discordant management in only 1.7% of cases, unlike other studies which reported this as being a major factor for certain tumour types. De Ieso et al. found comorbidity to be a reason for discordance in 33% of cases [19] whilst it was not listed as a reason at all by Hollunder et al. [20], perhaps being incorporated into either patient or clinician decision. It is a major reason for discordance in upper gastrointestinal MDM management (42–45%) [21, 23, 28]. It is sometimes included as clinician decision [24] or combined with patient deterioration [19]. The low impact of comorbidity is a surprising finding. It may be that MDMs take patient comorbidities into account when making management recommendations or that this factor may have been poorly recorded as a decision making factor in patients notes, and may be part of the 20% unknown reasons in our study. The unknown reasons could not be ascertained due to lack of documentation and are likely to represent patient or clinician preference, or comorbidities precluding MDM recommended management.
Rather than identifying specific reasons, a better approach may be to classify justifiable and unjustifiable reasons for discordant management [30]. Patients preference, performance status and comorbidities would all be considered justifiable whilst clinician decision with no other reason or unknown reason would be considered unjustifiable. Measuring the clinical translation of MDM recommendations should be considered a quality indicator for MDMs. Given the vast differences in healthcare settings and patient populations, benchmarks are not appropriate. However, identifying and investigating those who received discordant care is important to ensure the reason is valid and that there is equity of cancer care across different sociodemographic patient populations. A NHS report on effective MDMs states that processes should be in place to ensure MDM recommendations are implemented and that the MDM is notified of any significant changes to the management plan [40]. In Germany, certification of MDMs by the German Cancer Society requires any deviation from MDM recommendations to be documented and assessed [20].
This study is limited by its retrospective nature, with inevitable missing data and inability to ascertain reasons for discordant management in some cases. In addition, Australia’s universal health care system may limit applicability in overseas jurisdictions. The strengths of this study are its large patient cohort and inclusion of all patients discussed at solid tumour MDMs in an academic institution.
Moving forward we plan to perform regular audit and feedback of MDM recommended treatment with treatment received and investigate where there is discordance. However as it will be difficult to report on multifaceted recommendations, these audits will largely be confined to specific anti-cancer treatments ie systemic therapy, radiotherapy and surgery. Since completion of this study, the head and neck, gynae-oncology, CNS and breast MDMs have developed or improved their standardised templates in MOSAIQ® to better record MDM discussion and recommendations in a systematic fashion enabling audit. A template report measuring specific treatment recommendations against treatment received has already been created for the Lung MDM which documents everything including treatment received in MOSAIQ®. This will be more challenging to do for MDMs which document in other electronic medical records and which lack systematic recording of recommendations.
Conclusion
There was a high rate of translation of MDM recommendations into clinical practice for all solid tumour MDMs in South-Western Sydney although this was variable across tumour sites. Breast and upper gastrointestinal MDMs and multiple MDM discussions were significantly associated with concordant management. Sociodemographic factors did not impact on management concordance. The most common reason for discordant management was patient or guardian decision. Routine measurement of implementation of MDM recommendations should be considered as a quality indicator of MDM practice.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available as per the ethics committee approval of this study. They are available from the corresponding author on reasonable request after seeking further approval from the South Western Sydney Local Health District Human Research Ethics Committee.
References
Rao K, Manya K, Azad A, Lawrentschuk N, Bolton D, Davis ID, et al. Uro-oncology multidisciplinary meetings at an Australian tertiary referral Centre--impact on clinical decision-making and implications for patient inclusion. BJU Int. 2014;114(S1):50–4. https://doi.org/10.1111/bju.12764.
Brauer DG, Strand MS, Sanford DE, Kushnir VM, Lim KH, Mullady DK, et al. Utility of a multidisciplinary tumor board in the management of pancreatic and upper gastrointestinal diseases: an observational study. HPB. 2017;19(2):133–9. https://doi.org/10.1016/j.hpb.2016.11.002.
Lamb BW, Brown KF, Nagpal K, Vincent C, Green JS, Sevdalis N. Quality of care management decisions by multidisciplinary cancer teams: a systematic review. Ann Surg Oncol. 2011;18(8):2116–25. https://doi.org/10.1245/s10434-011-1675-6.
Schmidt HM, Roberts JM, Bodnar AM, Kunz S, Kirtland SH, Koehler RP, et al. Thoracic multidisciplinary tumor board routinely impacts therapeutic plans in patients with lung and esophageal cancer: a prospective cohort study. Ann Thorac Surg. 2015;99(5):1719–24. https://doi.org/10.1016/j.athoracsur.2014.11.019.
AlFarhan HA, Algwaiz GF, Alzahrani HA, et al. Impact of GI tumor board on patient management and adherence to guidelines. J Global Oncol. 2018:1–8.
Brunner M, Gore SM, Read RL, Alexander A, Mehta A, Elliot M, et al. Head and neck multidisciplinary team meetings: effect on patient management. Head Neck. 2015;37(7):1046–50. https://doi.org/10.1002/hed.23709.
Ung KA, Campbell BA, Duplan D, Ball D, David S. Impact of the lung oncology multidisciplinary team meetings on the management of patients with cancer. Asia-Pac JCO. 2016;12:e298–304.
Boxer MM, Duggan KJ, Descallar J, Vinod SK. Do patients discussed at a lung cancer multidisciplinary team meeting receive guideline-recommended treatment? Asia-Pac JCO. 2016;12:52–60.
Conron M, Phuah S, Steinfort D, Dabscheck E, Wright G, Hart D. Analysis of multidisciplinary lung cancer practice. Int Med J. 2007;37(1):18–25. https://doi.org/10.1111/j.1445-5994.2006.01237.x.
Caudron A, Chaby G, Dadban A, Andrejak C, Dhaille F, Bagot M, et al. Multidisciplinary team meetings in oncology: first analysis of benefits and evaluation of activity in a dermatology unit in France. Eur J Dermatol. 2010;20(6):778–84. https://doi.org/10.1684/ejd.2010.1097.
Vinod SK, Sidhom MA, Delaney GP. Do multidisciplinary meetings follow guideline-based care? J Oncol Pract. 2010;6(6):276–81. https://doi.org/10.1200/JOP.2010.000019.
Boxer MM, Vinod SK, Shafiq J, Duggan KJ. Do multidisciplinary team meetings make a difference in the management of lung cancer? Cancer. 2011;117(22):5112–20. https://doi.org/10.1002/cncr.26149.
Au-Yeung GH, Aly A, Bui A, Vermeltfoort CM, Davis ID. Uptake of oncology multidisciplinary meeting recommendations. Med J Aust. 2012;196:36–7 Letter.
Zhao S, Qi W, Chen J. Role of a multidisciplinary team in administering radiotherapy for esophageal cancer. BMC Cancer. 2020;20(1):974. https://doi.org/10.1186/s12885-020-07467-z.
Prades J, Remue E, van Hoof E, Borras JM. Is it worth reorganising cancer services on the basis of multidisciplinary teams (MDTs)? A systematic review of the objectives and organisation of MDTs and their impact on patient outcomes. Health Policy. 2015;119(4):464–74. https://doi.org/10.1016/j.healthpol.2014.09.006.
Heinke MY, Vinod SK. A review on the impact of lung cancer multidisciplinary care on patient outcomes. Transl Lung Cancer Res. 2020;9(4):1639–53. https://doi.org/10.21037/tlcr.2019.11.03.
Munro A, Brown M, Niblock P, Steele R, Carey F. Do multidisciplinary team (MDT) processes influence survival in patients with colorectal cancer? A population-based experience. BMC Cancer. 2015;15(1):686. https://doi.org/10.1186/s12885-015-1683-1.
Lamb BW, Sevdalis N, Taylor C, Vincent C, Green JS. Multidisciplinary team working across different tumour types: analysis of a national survey. Ann Oncol. 2012;23(5):1293–300. https://doi.org/10.1093/annonc/mdr453.
De Ieso PB, Coward JI, Letsa I, et al. A study of the decision outcomes and financial costs of multidisciplinary team meetings (MDMs) in oncology. Br J Cancer. 2013;109(9):2295–300. https://doi.org/10.1038/bjc.2013.586.
Hollunder S, Herrlinger U, Schmolders J, et al. Cross-sectional increase of adherence to multidisciplinary tumor board decisions. BMC Cancer. 2018;18:396.
Blazeby JM, Wilson L, Metcalfe C, Nicklin J, English R, Donovan JL. Analysis of clinical decision-making in multi-disciplinary cancer teams. Ann Oncol. 2006;17(3):457–60. https://doi.org/10.1093/annonc/mdj102.
Bumm R, Feith M, Lordick F, Herschbach P, Siewert JR. Impact of multidisciplinary tumor boards on diagnosis and treatment of esophageal cancer. Eur Surg. 2007;39(3):136–40. https://doi.org/10.1007/s10353-007-0333-5.
Goolam-Hossen T, Metcalfe C, Cameron A, Rocos B, Falk S, Blazeby JM. Waiting times for cancer treatment: the impact of multi-disciplinary team meetings. Behav Inform Technol. 2011;30(4):467–71. https://doi.org/10.1080/0144929X.2011.553747.
Osarogiagbon RU, Phelps G, McFarlane J, Bankole O. Causes and consequences of deviation from multidisciplinary care in thoracic oncology. J Thorac Oncol. 2011;6(3):510–6. https://doi.org/10.1097/JTO.0b013e31820b88a7.
Leo F, Venissac N, Poudenx M, Otto J, Mouroux J. Multidisciplinary management of lung cancer: how to test its efficacy? J Thorac Oncol. 2007;2(1):69–72. https://doi.org/10.1097/JTO.0b013e31802bff56.
Loh J, Stevens G, Stevens W, Kolbe J. Concordance between thoracic multidisciplinary meeting recommendations for radiation therapy and actual treatment for lung cancer. J Med Imag Radiat Oncol. 2012;56(6):696–702. https://doi.org/10.1111/j.1754-9485.2012.02460.x.
Lutterbach J, Pagenstecher A, Spreer J, Hetzel A, Velthoven Vv, Nikkhah G, et al. The brain tumor board: lessons to be learned from an interdisciplinary conference. Onkologie. 2005;28(1):22–6. https://doi.org/10.1159/000082124.
Wood JJ, Metcalfe C, Paes A, Sylvester P, Durdey P, Thomas MG, et al. An evaluation of treatment decisions at a colorectal cancer multi-disciplinary team. Color Dis. 2008;10(8):769–72. https://doi.org/10.1111/j.1463-1318.2007.01464.x.
Chekerov R, Denkert C, Boehmer D, et al. Online tumor conference in the clinical management of gynecological cancer: experience from a pilot study in Germany. Int J Gynecol Ca. 2008;18(1):1–7. https://doi.org/10.1111/j.1525-1438.2007.00971.x.
Rajan S, Foreman J, Wallis MG, Caldas C, Britton P. Multidisciplinary decisions in breast cancer: does the patient receive what the team has recommended? Br J Cancer. 2013;108(12):2442–7. https://doi.org/10.1038/bjc.2013.267.
English R, Metcalfe C, Day J, Rayter Z, Blazeby JM. A prospective analysis of implementation of multi-disciplinary team decisions in breast cancer. Breast J. 2012;18(5):459–63. https://doi.org/10.1111/j.1524-4741.2012.01270.x.
Pattanasri M, Elder K, Nickson C, Cooke S, Machalek D, Rose A, et al. Uptake of adjuvant breast cancer treatments recommended by multi-disciplinary meetings. ANZ J Surg. 2018;88(7-8):745–50. https://doi.org/10.1111/ans.14368.
Samarasinghe A, Chan A, Hastrich D, et al. Compliance with multidisciplinary team meeting management recommendations. Asia-Pacific JCO. 2019;15:337–42.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. https://doi.org/10.1016/0021-9681(87)90171-8.
Australian Bureau of Statistics. Socio-Economic Indexes for Areas. Commonwealth of Australia. http://www.abs.gov.au/websitedbs/censushome.nsf/home/seifa. Published 2011. Accessed 2 Dec 2020.
Cancer Institute NSW. Cancer Statistics NSW. NSW Government. https://www.cancer.nsw.gov.au/research-and-data/cancer-data-and-statistics/cancer-statistics-nsw#//. Accessed 2 Dec 2020.
Atwell D, Vignarajah DD, Chan BA, Buddle N, Manders PM, West K, et al. Referral rates to multidisciplinary team meetings: is there disparity between tumour streams? J Med Imag Radiat Oncol. 2019;63(3):378–82. https://doi.org/10.1111/1754-9485.12851.
Jalil R, Ahmed M, Green JS, Sevdalis N. Factors that can make an impact on decision-making and decision implementation in cancer multidisciplinary teams: an interview study of the provider perspective. Int J Surg. 2013;11(5):389–94. https://doi.org/10.1016/j.ijsu.2013.02.026.
Gashin L, Tapper E, Babalola A, Lai KC, Miksad R, Malik R, et al. Determinants and outcomes of adherence to recommendations from a multidisciplinary tumour conference for hepatocellular carcinoma. HPB. 2014;16(11):1009–15. https://doi.org/10.1111/hpb.12280.
National Cancer Action Team. The Characteristics of an Effective Multidisciplinary Team (MDT). London; 2010. Available at: http://secure-web.cisco.com/1LHufu6CLl4vFSNDBpJCUUYBFitHhVRLYFdY2KpRBZ20EUgg1zyffIKl55F9LaY_hIJMeyInndmlHFX_RrmdKNVepAHP7ROHZunEUipcDuT1W6Wm486KiwJPWDPO2B4D0tYtnK2xQ68mzM1MGwEr6TQX2I4oJ_jVp3N_pRcuppGF1Om8quXB5Na26lnFleC_pFQhT8HL7S9LKdIYyPAw3OfpPAYJxin1HsXQXKbp72VHz7enBQcekWDGj9U1HfcaF5jMl-_LxG9xg6nJsVLioITnt4T2CDSaeg_g4N3T-WH0wnx6VlMrkvNugoit_GtHyvgXki7E-vC-wol_XTGrxVDnK56kG90GbTHPgWhtOOnoZfBYa31YEXc5OimN4v8h5FHwG18QRp7OWTPyMCmkxT2FZaQ3l3PtH6HcfBwVW6Eea_HdxXbVVTLqgGbZlxFUdOp1mksHUekWGGbXJ4znMm1I6yjEgfdd1Dtk69oF2o_n4UzZ79D4WlddasOZbT9sC/http%3A%2F%2Fwww.ncin.org.uk%2Fview%3Frid%3D136 Accessed 2 Dec 20
Acknowledgements
We thank Sandy Avery for reviewing the study protocol and obtaining funding, and Nasreen Kaadan for her help in retrieving MDM agendas.
Funding
This work was supported by a Cancer Institute NSW grant.
Author information
Authors and Affiliations
Contributions
SV: Conceptualisation, wrote study protocol, supervised data collection, interpreted results, wrote original draft. NW: data collection for 6 MDMs, data analysis and interpretation, review and editing. SK: submitted ethics, data collection for 1 MDM, review and editing. KD: developed data collection template, data collection for 1 MDM, review and editing. MI: Data collection for 1 MDM, review and editing. JS: helped draft the study protocol, supervised data collection and analysis, interpreted results, review and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study and its methodology was approved by the South Western Sydney Local Health District Human Research Ethics Committee. The study was conducted in accordance with local guidelines and regulations. The requirement for patient informed consent was waived by the South Western Sydney Local Health District Human Research Ethics Committee as this was a retrospective study which did not involve any intervention.
Consent for publication
Not applicable.
Competing interests
There are no competing interests. No authors declare any conflict of interest in relation to this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Vinod, S.K., Wellege, N.T., Kim, S. et al. Translation of oncology multidisciplinary team meeting (MDM) recommendations into clinical practice. BMC Health Serv Res 21, 461 (2021). https://doi.org/10.1186/s12913-021-06511-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-021-06511-3