Abstract
Background
Staff shortages limit access to health services. The bidirectional benefits of allied health clinical placements are understood in the domains of student learning, health service delivery, and future workforce development. Still, the benefits to current workforce outcomes remain unknown. This review provides insights into the effects of allied health student placements in acute and primary care settings, particularly on healthcare staff's knowledge and procedural skills.
Methods
This search was based on the integrative review process established by Whittemore and Knafl in 2005. In October 2023, the first author (MH) searched five major electronic databases: Medline-EBSCO, PubMed, CINAHL, Embase, and Scopus. The CLUSTER model was used to track additional references. The first three authors (MH, SM, and SC) were involved in screening, quality appraisal, and synthesis of the studies. Data were thematically synthesised and analysed.
Results
MeSH headings and keywords were used in key search areas: health education, health professional training, clinical placements, and allied health professions. The systematic search yielded 12 papers on allied health student placements across various healthcare settings in rural and metropolitan areas, with no high-quality methodologies measuring student placements' impact on staff knowledge and skills. Four main themes were identified from the analysis: meaningful student integration in service delivery, targeted educational support to healthcare staff, development of staff procedural skills and confidence, and the mechanisms of why student placements work in this aspect.
Conclusions
This review suggests that offering allied health student placement could be a promising approach to supporting rural healthcare staff in performing patient assessments and treatments proficiently and collaboratively. However, this requires further investigation to confirm.
Similar content being viewed by others
Introduction
Healthcare staff shortages limit access to health services [1]. Four key areas for immediate attention in the Australian health context are food and nutrition, dementia care, the use of restrictive practices, and palliative care [2]. Allied health professionals have an important role to play in each of these areas. However, there is a critical shortage of allied health professionals and a higher turnover rate among allied health workers across Australia [2, 3]. This shortage becomes more pronounced as the number of healthcare staff decreases with increasing remoteness [3]. Health service disparities persist between rural and metropolitan areas in Australia, with a gap in life expectancies (78 years compared to 82.5 years), a prevalence of chronic disease (21% vs 18% per 100,000 population), and potentially avoidable death rates (775.9 deaths vs 587.9 deaths per 100,000 population) [1, 4]. Current funding and employment models have led to issues with recruitment and retention of allied health professionals and a shortage of staff [5, 6]. For example, in 2018–19, only 29% of Australians used allied health services [7]. An additional challenge to upskilling healthcare staff is a lack of professional development opportunities [8, 9]. Student placements have been identified as a potential approach for health workforce capacity building and support of health services delivery, especially in rural areas [9,10,11].
Various clinical training placement models exist to facilitate learning opportunities for medicine, nursing, and allied health students by integrating them into health service delivery for patients [12]. These placement models include practice-based learning [13], experiential learning [14], service-learning [15], work-integrated learning [16], and integrated clinical placements [17]. Clinical placements benefit students, educational institutions, and healthcare organisations in different ways, including personal growth and professional experience for students, academic rigour and service to the community for universities, and a workforce fit to practice in healthcare organisations. Evidence shows that clinical placements of students with exposure to acute and primary healthcare contexts are associated with better impacts in terms of students’ intellectual transformation [18,19,20], workforce capacity building [21,22,23], and patient health outcomes [24, 25]. There remains a notable gap in research on allied health student placements that builds staff capability.
Educational and training resources designed for clinical supervision of allied health students during their placements can also serve as professional learning opportunities for healthcare staff. Professional development is imperative for healthcare staff to stay up to date with knowledge and technical skills and create innovative treatment planning. Complex and infrequently used clinical skills often deteriorate among health professionals, as confirmed in a systematic review by Main and Anderson [25] in Australia [26]. The National Health Workforce Strategy advocates for continuing professional education and training for health professionals so that professionals “maintain, improve, and broaden their knowledge, expertise, and competence, and develop the personal and professional qualities throughout their professional lives” [27]. Healthcare professionals have reported that ongoing education and training opportunities have improved their knowledge and procedural skills in client (e.g., patients, residents in aged care homes) care [28]. Since the COVID-19 pandemic, access to online professional development modules and training has improved [29]. However, a lingering question persists: can the co-creation of training programs and educational modules effectively contribute to the knowledge and skills development of both allied health students and healthcare staff?
A compelling association exists between student placements, health workforce capacity and capability building [30]. As noted earlier, student placements contribute to workforce recruitment and retention in rural and metropolitan areas by immersing them in health and social care settings. Throughout placements, students benefit from access to tutorials and clinical supervision [12, 15, 16]. Additionally, students and healthcare staff from different disciplines work collaboratively in a team during placements [31]. Pedagogical frameworks, including social learning theory [32], social constructivism [33], interprofessional learning [34], and community of practice [35] suggest that individuals working together learn with and from one another. The Royal Commission into Aged Care Quality and Safety in 2021 recommends strengthening allied health services [2], particularly in rural areas; therefore, a review of existing literature is important to inform how and why the placements work to enhance the capability of healthcare staff in service delivery.
Aims of the study
This review aims to synthesise the effects of allied health student placements on healthcare staff's knowledge and procedural skills in acute and primary care settings.
Two main questions guided this review:
Q1: How do the studies describe the integration of allied health students in services design and delivery in acute and primary care settings?
Q2: How do these studies describe the effectiveness of allied health student placements for current healthcare staff’s knowledge and procedural skills in acute and primary care settings?
Methods
This review adhered to the five steps of an integrative review process as its foundation, established by Whittemore and Knafl in 2005 [36]. These steps included problem identification, literature search, data evaluation, data analysis, and presentation. We systematically searched the literature and employed the Mixed Method Appraisal Tool (MMAT) to assess the quality and rigour of the selected papers [37]. The extracted data were then analysed and presented thematically.
Search strategy
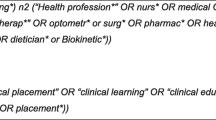
The systematic search for published documents was conducted following the PRISMA guidelines [38]. In October 2023, the first author (MH) searched five electronic databases: Medline-EBSCO, PubMed, Embase, CINAHL, and SCOPUS. A combination of MeSH headings and relevant concepts was used in crucial search areas: health education, health professional training, clinical placements, and allied health professions (the full search strategy is available in Table 1). The CLUSTER model was also employed to track sibling studies and citations for supplementary references.
Inclusion and exclusion criteria
The clinical placements are typically designed to immerse health students in real-life experience in acute and primary care settings with the aim of future workforce recruitment. Given the specific focus of this review on the impact of allied health student placements on the knowledge and procedural skills of existing healthcare staff, medical and nursing professions were not included in the search. The search was also limited to certain allied health disciplines based on the discussion with allied health clinicians and health service providers, such as physiotherapy, occupational therapy, dietetics, speech pathology, exercise physiology, social work, optometry, podiatry, psychology, and osteopathy. The inclusion criteria were articles and reports published in English, publication year 2001 to the present, descriptions of actual allied health student placements, and the placements aimed at enhancing the capacity and capabilities of current healthcare staff. Aligning with this review’s objectives and considering the scarcity of studies conducted in rural locations, the search was not restricted solely to rural placements. While the primary outcomes of allied health student placements predominantly centred on student learning, patient health and wellbeing, and workforce recruitment and retention, the studies that explored these aspects as their primary focus were not excluded when they identified the placements’ contribution to healthcare staff. Two reviewers, MH and HG independently screened the records retrieved by title, abstract, and full text. Discrepancies were discussed with a third reviewer, SM.
Quality appraisal
The MMAT criteria were used to assess the quality of studies, using a scale that spanned from 0, indicating no criteria met, to 5, indicating all criteria met, as detailed by Hong et al. in 2018. [37] To evaluate the studies, two reviewers, MH and HG, conducted separate assessments, allocating scores out of 5 (0—Unclear/No and 1: Yes). Through a consensus-driven process, it was determined that the papers included in this review exhibited a quality level that ranged from moderate (with a score of 3) to high (with a score of 5), as indicated in Table 2.
Data extraction and analysis
Three reviewers, MH, SM, and SC, read the papers meeting the inclusion criteria multiple times to extract data. The extracted data were recorded separately by these three reviewers into Excel spreadsheets, with any discrepancies carefully cross-checked (Table 2). The extracted data included the study characteristics (author, year, country of origin, study design, study participants); characteristics of allied health student placements (placement setting, focus, participants, type of placement, the level of student involvement in service delivery); outcome data for existing healthcare staff’s knowledge and skills, as well as the limitations of these placements. Given that the selected studies were heterogeneous in methodologies, a thematic data synthesis was deemed the most appropriate approach [45]. The categories and sub-themes were independently identified by the reviewers, MH, SM, and SC, and were subsequently deliberated upon during review team meetings to determine the final themes and validate interpretations.
Results
Figure 1 illustrates the selection process of the studies reviewed. Twelve papers that met the inclusion criteria represented the highest number over the past decade. Among these, eight studies used mixed methods for evaluating the placements, while two were qualitative and two were quantitative methodologies. The selected placements were mainly in Australia (10), with all papers originating from high-income countries, including the USA (1) and Canada (1). The healthcare settings were diverse across the placements; half were in residential aged care homes, while the rest were in hospitals, community health services, clinical skills centres, patient training centres, and non-government health organisations. The study participants included students, patients/residents, healthcare staff, health service managers, clinical educators, and relevant key stakeholders like family members and community organisations. Rural placement was reported in the majority of studies (7), but no studies compared the effects of different locations.
All twelve studies focused on either allied health student learning outcomes or service delivery across a range of settings by placing students. Most placement programs narrowly focused on the professional development of existing healthcare staff, while exclusive focus on this aspect was identified in four placement programs facilitated in hospitals, residential aged care homes, and community health services [39, 47, 49, 50]. Undergraduate and postgraduate students from different allied health disciplines participated in the placements, including physiotherapy, occupational therapy, nutrition and dietetics, social work, and speech pathology. Some studies featured the collaboration between medicine, nursing, and allied health students [40, 46, 47, 50]. Various types of placements were discussed, such as clinical placement [41, 48]; work-integrated learning [42]; interprofessional team placement [40, 43, 49]; service-learning placement [39, 44, 47, 50]; and simulated learning [51]. Interprofessional education was reported in most of the studies (8), and four studies provided information on the duration of placements, which ranged from four to ten weeks; in addition to detailing the types and focuses of the placements, the synthesis of outcome data revealed four key themes.
Meaningful student integration in service delivery
The integration of allied health students in health service delivery for patients was identified as a powerful and essential part of all placement programs. Student involvement in health service delivery was described by their engagement in a wide range of activities, from administration tasks and priority assessments to developing and implementing treatment plans and evaluating interventions. Eight studies reported direct engagement of students in developing treatment plans and designing and delivering services. Examples included person centred exercise programs, developing a sensory garden, implementing craft and cooking sessions for residents with dementia and training and upskilling care staff [39, 40, 44, 46,47,48,49,50]. In contrast, four placement programs were restricted to organisations’ priority assessments [41, 42, 51]; shadowing a care worker and spending time with residents [43]; and planning and evaluation of interventions [41, 42, 51]. Student involvement in delivering direct health services to patients was identified in both urban and rural healthcare settings.
The extent of students’ involvement in delivering health services to patients was somewhat related to the degree to which the placement supported the capacity and capability building of existing healthcare staff. Integrating students in administrative tasks, priority assessments, and evaluation of the treatments contributed to staffing management and timely task completion, as well as a cultural shift towards collaboration among the staff [41,42,43, 51]. Direct engagement of students in treatment plans and patient/resident care management was highly beneficial to a healthcare staff’s reflection and clinical reasoning [39, 40, 44, 46,47,48, 50]. Of note, none of the studies measured the causal relationships between the level of student integration in service delivery and the professional development of healthcare staff.
Targeted education support to healthcare staff
All studies reported that the placements led to an increase in knowledge, or had the potential to do so, for both students and healthcare staff. During these placements, various learning activities were offered to students, which, in turn, enhanced the knowledge of healthcare staff. For instance, learning activities like Grand Rounds and interprofessional education were implemented [44, 46, 47, 50, 51]. Key areas of learning for healthcare staff were identified in one evaluation study of interprofessional team placement in residential aged care homes [50], including mealtime positioning, post-stroke positioning, and medication management in palliative care. Additionally, one qualitative study described how the placements allowed healthcare staff to reorient themselves with the theories and methods behind the treatments [46]. Attending education and training sessions also helped the rural healthcare staff become familiar with the roles and responsibilities of other health disciplines [44].
Three studies reported that students generated new data and knowledge based on local evidence during their placements [41, 42, 50]. Two of the studies included rural placement of students [41, 50], but all the studies confirmed that the students provided healthcare staff with current and innovative knowledge. This new knowledge supported the staff in strategic planning and prioritising patient assessments and treatments.
Development of staff procedural skills and confidence
Eight studies highlighted that allied health student placements were useful in developing procedural skills among healthcare staff. In four of these placements, student training sessions enhanced the healthcare staff’s efficiency in service delivery by reorienting them with the standards and procedures of the treatments [39, 46, 49, 50]. Healthcare skills development various skills, including critical reflection, clinical reasoning, patient flow management, timely assessment and treatment of patients, continuity of care, clinical communication, patient safety, and evidence-based practice. The Delphi study conducted by MacBean et al. [43] in inpatient training centres in Australia provided insights into how the placements broaden the healthcare staff’s scope of practice in speech pathology, which was further complemented by the qualitative study of Kemp et al. [41] in Australian community health services. [42, 51] Healthcare staff also gained confidence in performing clinical tasks during the student placements, with their abilities being questioned and affirmed [46, 47, 50]. Interprofessional team placements were found to be effective in two studies for team skills development [49, 50]. Both rural and urban healthcare staff benefited equally from student placements in healthcare settings.
Why do student placements work? Insights into the mechanisms
This review identified the mechanisms underlying how the allied health student placements supported the professional development of healthcare staff in seven studies. While a cross-sectional study indicated non-statistically significant disadvantages of student placements in regional and rural residential aged care homes [48], six studies, spanning various healthcare settings, reported functional improvements in health service delivery attributed to student placements [39, 40, 42, 46, 49, 50], regardless of the locations. These functional improvements in service delivery were because of additional training and resources, as well as active engagement in teaching, facilitating, and managing students within healthcare settings, which were identified as supportive for healthcare staff’s professional development [40, 46, 50]. Collaborative practice was found to be instrumental in reducing hierarchical culture among healthcare staff [43, 49]. Additionally, the placements contributed to early patient readiness for discharge, providing staff with flexibility in using client care modalities, and questions from students increased staff awareness of evidence-based practice [39, 50].
In order to facilitate discussions, the findings of this review are positioned within a general system theory framework (Fig. 2), enabling the assessment of inputs, transformational processes, outputs, and the environment within acute and primary healthcare settings.
Discussion
The role of allied health student placements in fostering professional development of healthcare staff is promising, with most of the studies in this review showing positive evidence. Service-based placements, with a meaningful integration of students in health service delivery, show the most potential. Service-based placements might work by offering Grand Rounds and interprofessional education sessions to healthcare staff in critical areas of client care, generating new knowledge that can form powerful local evidence, and enhancing healthcare staff's understanding of other health professionals and service providers that can promote the collaborative practice. Regardless of the locations, active engagement in supervising and educating students and increasing awareness of training sessions have proved to be beneficial for healthcare staff in developing their professional knowledge and skills in client care.
There is a strong evidence base for the integration of allied health students into various aspects of client care, but engagement has varied. Student involvement in service delivery can be particularly powerful as it primarily emphasises the improvement of patient accessibility and utilisation of health services that are otherwise not accessible to them, especially in rural communities [52, 53]. In the studies included in this integrative review, students played vital roles in the development of treatment plans, treatment of patients, and evaluation of interventions, and this integration was found to be beneficial to current health workforce capacity and capability building. Previous placement programs involving medical and nursing students corroborate the positive outcomes, citing the development of confidence and proficiency in both students and healthcare staff [54, 55]. These programs recognised the bi-directional benefits of clinical placements. Since 2021, the Rural Health Multidisciplinary Training (RHMT) in Aged Care Program has supported University Departments of Rural Health (UDRHs) in Australia to expand their capacity to facilitate health student placements in aged care settings. This review is timely to inform clinical educators by providing insights to design education sessions that meet the learning needs of students and staff.
Within the limited number of studies available for review,education sessions during student placements appear to be important for developing professional knowledge and skills of healthcare staff. This review strengthens the previous study findings in medicine and nursing placements in acute care settings, stating that Grand Rounds and interprofessional education opportunities increased healthcare staff and students’ awareness of different aspects of client care and expertise of their own and other professions [56,57,58,59]. These ongoing sessions cover various aspects of client care and are likely to equip staff with theories behind the treatments. Rural healthcare staff often have limited access to professional development opportunities, as well as supervision of students that has the potential to add a new perspective to the staff workloads [11, 59, 60]. Rural healthcare staff in community settings may also have limited time to engage with professional learning opportunities in their normal work routine, so embedding opportunities for ongoing education in the workplace through student placements may be beneficial. Opportunities must be explored in collaboration with healthcare and community partners to ensure professional development and training is co-designed and co-delivered to meet their staff’s unique needs. Creating ongoing learning opportunities for staff and engaging them in student supervision is vital to the success of placements.
In terms of creative learning, the student placements’ contribution to generating new and local evidence emerges with some supporting findings. Many studies explored how students are engaged in reciprocal learning relationships with peers and healthcare staff in the domains of clinical knowledge and procedural skills [58, 61]. Students bring new or different perspectives, up-to-date knowledge of evidence-based practice, do not have the workload expectations, and are not restricted by funding requirements. This allows students to bring a different perspective. Students often have more time to complete projects and create resources, and when co-designed with staff and patients, such resources can enhance both staff learning and patient outcomes. However, these bi-directional learning benefits receive less attention from educators and rural health service providers. It may be unclear what students could add to the knowledge and skills of staff who are already registered and experienced in delivering services. Evidence is limited on how to design education sessions for different learner groups.
The review suggests that active engagement of healthcare staff is often absent in student placements. While clinical educators currently take the responsibility for student supervision and management, a potential improvement could involve active engagement of healthcare staff in these aspects during placements, which may help address the two remaining questions. First, whether it is important to create collaborative learning environments before offering student-led education of staff. This could enhance understanding and knowledge of both staff and student roles, increasing collegiality and co-design of learning and knowledge. A second question is whether adding a co-supervision role for healthcare staff in the allied health student placements (by adapting the models of medicine and nursing placements in rural communities) is a viable option to enhance staff engagement. This role could upskill the current health workforce in rural areas, increasing the capacity to take student placements. This role may combine rural knowledge with an understanding of student models and seek to implement changes in practices developed from student placements.
Limitations
Developing the search strategy was challenging because of the diversity in placements, disciplines, settings, and associated terminology. This resulted in a search that yielded only 12 eligible studies for review. Since allied health student placements in rural healthcare settings have expanded across high-income countries in recent years, there will likely be articles under review about unsuccessful placements that could have provided additional insights. Further rigorous investigations are required to strengthen the evidence surrounding student placements’ contribution to improving rural health staff knowledge and procedural skills in client care. These investigations could delve into the unique workforce outcomes associated with individual allied health disciplines and consider the different levels of study among students (undergraduate vs postgraduate).
Conclusions
This review is the first synthesis of the impact of allied health student placements on the professional development of our current health workforce. To enhance staff knowledge and skills and address shortages, particularly in rural and remote communities, this review indicates the importance of student integration in the delivery of health services. A collaborative learning approach to increase the knowledge of students and staff and improve staff engagement in placements that promote interprofessional learning is key to the professional development of current staff in any healthcare setting. While there is little evidence of the generation of new knowledge by students during their placements, there is no indication that these placements disadvantage healthcare staff in relation to their professional development. Clinical educators may consider establishing co-supervision roles for rural healthcare staff to foster interactions between staff and students and to enhance positive learning experiences for both parties. Individually tailored and co-designed professional development opportunities could be important, for instance, to assist rural healthcare staff in reducing adverse events and ensuring adequate health services and the quality of integrated care.
Availability of data and materials
All data generated or analysed during this study are included in this article.
References
Australian Institute of Health and Welfare. Rural and remote health. Cat. no. PHE 255. Canberra: AIWH. 2023. Available at https://www.aihw.gov.au/reports/rural-remote-australians/rural-and-remote-health
Royal Commission into Aged Care Quality and Safety. A Summary of Final Report. Final Report Volume 1. 2022. Available at https://agedcare.royalcommission.gov.au/sites/default/files/2021-03/final-report-executive-summary.pdf
Savy P, Warburton J, Hodgkin S. Challenges to the provision of community aged care services across rural Australia: perceptions of service managers. Rural Remote Health. 2017;17(2):1–1.
Australian Institute of Health and Welfare. Older Australians. Health – Selected conditions. Canberra: AIWH. 2023. Available at https://www.aihw.gov.au/reports/older-people/older-australia-at-a-glance/contents/health-functioning/health-disability-status
Calderone L, Bissett M, Molineux M. Understanding occupational therapy practice in residential aged care facilities under the aged care funding instrument: a qualitative study. Aust Occup Ther J. 2022;69(4):447–55.
National Rural Health Alliance. 2021–2022 Pre-budget submission. Canberra: NRHA. 2021. Available at https://treasury.gov.au/sites/default/files/2021-05/171663_national_rural_health_alliance.pdf
National Rural Health Alliance. Media Release. Number don’t lie: increased investment in rural health care urgently needed. Canberra: NRHA. 2023. Available at https://www.ruralhealth.org.au/sites/default/files/media-files/mr-2023-09-11-response-aihw-data-release.pdf
Adams M. Education to prepare health professionals for rural practice: a scoping review. Aust Int J Rural Educ. 2023;33(1):17–40.
Brown LJ, Wakely L, Little A, Heaney S, Cooper E, Wakely K, May J, Burrows JM. Immersive place-based attachments in rural australia: an overview of an allied health program and its outcomes. Educ Sci. 2022;13(1):2.
Greenhill JA, Walker J, Playford D. Outcomes of Australian rural clinical schools: a decade of success building the rural medical workforce through the education and training continuum. Rural Remote Health. 2015;15(3):100–13.
Held FP, Roberts C, Daly M, Brunero C. Learning relationships in community-based service-learning: a social network analysis. BMC Med Educ. 2019;19(1):1.
Thistlethwaite JE. Practice-based learning across and between the health professions: a conceptual exploration of definitions and diversity and their impact on interprofessional education. Int J Pract-based Lear Health Soc Care. 2013;1(1):15–28.
Yardley S, Teunissen PW, Dornan T. Experiential learning: AMEE guide No. 63. Med Teach. 2012;34(2):e102–15.
Jones D, McAllister L, Lyle D. Interprofessional academic service-learning in rural Australia: exploring the impact on allied health student knowledge, skills, and practice. A qualitative study. Int J Pract-Based Lear Health Soc Care. 2015;3(2):1–6.
Billett S. Learning through work: workplace affordances and individual engagement. J Work Learn. 2001;13(5):209–14.
Roberts C, Daly M, Held F, Lyle D. Social learning in a longitudinal integrated clinical placement. Adv Health Sci Educ. 2017;22:1011–29.
Ulenaers D, Grosemans J, Schrooten W, Bergs J. Clinical placement experience of nursing students during the COVID-19 pandemic: a cross-sectional study. Nurse Educ Today. 2021;99:104746.
Greenlees NT, Pit SW, Ross LJ, McCormack JJ, Mitchell LJ, Williams LT. A novel blended placement model improves dietitian students’ work-readiness and wellbeing and has a positive impact on rural communities: a qualitative study. BMC Med Educ. 2021;21(1):1–2.
Walsh SM, Versace VL, Thompson SC, Browne LJ, Knight S, Lyle DM, Argus G, Jones M. Supporting nursing and allied health student placements in rural and remote Australia: a narrative review of publications by university departments of rural health. Med J Aust. 2023;219:S14–9.
Thackrah RD, Thompson SC. Learning from follow-up of student placements in a remote community: a small qualitative study highlights personal and workforce benefits and opportunities. BMC Med Educ. 2019;19(1):1–9.
Woolley T, Gupta TS, Stewart RA, Hollins A. A return-on-investment analysis of impacts on James Cook University medical students and rural workforce resulting from participation in extended rural placements. Rural Remote Health. 2021;21(4):1–1.
Coe S, Marlow A, Mather C. Whole of community facilitators: an exemplar for supporting rural health workforce recruitment through students’ professional experience placements. Int J Environ Res Public Health. 2021;18(14):7675.
Moran A, Nancarrow S, Cosgrave C, Griffith A, Memery R. What works, why and how? A scoping review and logic model of rural clinical placements for allied health students. BMC Health Serv Res. 2020;20:1–8.
Pigott A, Patterson F, Birch S, Oakley P, Doig E. The health service impact of an occupational therapy practice placement model: Student-resourced service delivery of groups. Focus on Health Professional Education: A Multi-Disciplinary Journal. 2022;23(2):21–34.
Main PA, Anderson S. Evidence for continuing professional development standards for regulated health practitioners in Australia: a systematic review. Hum Resour Health. 2023;21(1):1–6.
APHRA & National Boards. Continuing professional development. 2023. Accessed on 15 November 2023: https://www.ahpra.gov.au/Registration/Registration-Standards/CPD.aspx
Aleo G, Pagnucci N, Walsh N, Watson R, Lang D, Kearns T, et al. The effectiveness of continuing professional development for the residential long-term care workforce: a systematic review. Nurse Educ Today. 2024;137:106161. https://doi.org/10.1016/j.nedt.2024.106161.
NSW Productivity Commission. New thinking on continuing professional development. Discussion Paper. 2022. Accessed on 15 November 2023: https://www.productivity.nsw.gov.au/sites/default/files/2023-01/20221215-new-thinking-on-continuing-professional-development.pdf
Attrill S, Foley K, Gesesew HA, Brebner C. Allied health workforce development for participant-led services: structures for student placements in the National Disability Insurance Scheme. BMC Med Educ. 2023;23(1):1–3.
Lauckner HM, Rak CN, Hickey EM, Isenor JE, Godden-Webster AL. Interprofessional and collaborative care planning activities for students and staff within an academic nursing home. J Interprofessional Educ Pract. 2018;13:1–4.
Horsburgh J, Ippolito K. A skill to be worked at: using social learning theory to explore the process of learning from role models in clinical settings. BMC Med Educ. 2018;18(1):1–8.
Hayes C. Explaining approaches in pedagogic practice for healthcare assistants. British J Healthc Assistants. 2014;8(8):398–405.
Steinert Y. Learning together to teach together: interprofessional education and faculty development. J Interprof Care. 2005;19(sup1):60–75.
Ranmuthugala G, Plumb JJ, Cunningham FC, Georgiou A, Westbrook JI, Braithwaite J. How and why are communities of practice established in the healthcare sector? A systematic review of the literature. BMC Health Serv Res. 2011;11(1):1–6.
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–53.
Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, Gagnon MP, Griffiths F, Nicolau B, O’Cathain A, Rousseau MC. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34(4):285–91.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:71.
Clarke V, Braun V, Hayfield N. Thematic analysis. Qual Psychol: Pract Guide Res Methods. 2015;3:222–48.
Buchanan J, Jenkins S, Scott L. Student clinical education in Australia: a University of Sydney scoping study. Sydney: The University of Sydney; 2014.
Johnston C, Newstead C, Walmsley S, MacDonald L. Allied health student clinical placements in residential aged care facilities: staff opinions, attitudes, and support needs. Internet J Allied Health Sci Pract. 2014;12(4):11.
Kemp C, van Herwerden L, Molloy E, Kleve S, Brimblecombe J, Reidlinger D, Palermo C. How do students offer value to organisations through work integrated learning? A qualitative study using Social Exchange Theory. Adv Health Sci Educ. 2021;26:1075–93.
Longman JM, Barraclough F, Swain LS. The benefits and challenges of a rural community-based work-ready placement program for allied health students. Rural Remote Health. 2020;20(3):1–7.
MacBean N, Theodoros D, Davidson B, Hill AE. Simulated learning environments in speech-language pathology: An Australian response. Int J Speech Lang Pathol. 2013;15(3):345–57.
Campbell N, Stothers K, Swain L, Cairns A, Dunsford E, Rissel C, Barker R. Health services in northern Australia depend on student placements post COVID-19. Aust N Z J Public Health. 2020;44(6):521.
Mu K, Chao CC, Jensen GM, Royeen CB. Effects of interprofessional rural training on students’ perceptions of interprofessional health care services. J Allied Health. 2004;33(2):125.
Nguyen KH, Seaman K, Saunders R, Williams E, Harrup-Gregory J, Comans T. Benefit–cost analysis of an interprofessional education program within a residential aged care facility in Western Australia. J Interprof Care. 2019;33(6):619–27.
Nisbet G, Thompson T, McAllister S, Brady B, Christie L, Jennings M, Kenny B, Penman M. From burden to benefit: a multi-site study of the impact of allied health work-based learning placements on patient care quality. Adv Health Sci Educ. 2023;28(3):759–91.
Reid C, Barbaro R. Student placements in rural health services: developing an interdisciplinary model. National Rural Health Alliance. 2019. Available at https://www.ruralhealth.org.au/15nrhc/sites/default/files/D8-3_Reid%2C%20Barbaro.pdf
Seaman KL, Williams E, Saunders R, Harrup-Gregory J, Pratt K, Loffler H, Hallsworth A. Evaluating the outcomes for interprofessional education programs in residential aged care. Cognitive Decline Partnership Centre, Brightwater Care Group. 2016. Available at https://cdpc.sydney.edu.au/wp-content/uploads/2019/06/IPE_consumer_report_final.pdf
Seaman KL, Bulsara CE, Saunders RD. Interprofessional learning in residential aged care: providing optimal care for residents. Aust J Prim Health. 2015;21(3):360–4.
Campbell N, Moore L, Farthing A, Anderson J, Witt S, Lenthall S, Petrovic E, Lyons C, Rissel C. Characteristics of nursing and allied health student placements in the Northern territory over time (2017–2019) and placement satisfaction. Aust J Rural Health. 2021;29(3):354–62.
Molloy E, Lew S, Woodward-Kron R, Delany C, Dodds A, Lavercombe M, Hughson J. Medical student clinical placements as sites of learning and contribution. Melbourne: University of Melbourne; 2018.
ANMJ Staff. Student nurses drawn to primary healthcare. Australian Nursing and Midwifery Journal. 2022. Available at https://anmj.org.au/student-nurses-drawn-to-primary-healthcare/
Furr S, Lane SH, Martin D, Brackney DE. Understanding roles in health care through interprofessional educational experiences. British J Nur. 2020;29(6):364–72.
Rizk N, Jones S, Shaw MH, Morgan A. Using forum theater as a teaching tool to combat patient bias directed toward health care professionals. MedEdPORTAL. 2020;16:11022.
Al-Jayyousi GF, Abdul Rahim H, Alsayed Hassan D, Awada SM. Following interprofessional education: health education students’ experience in a primary interprofessional care setting. J Multidiscip Healthc. 2021;14:3253–65. https://doi.org/10.2147/JMDH.S318110.
Spaulding EM, Marvel FA, Jacob E, Rahman A, Hansen BR, Hanyok LA, Martin SS, Han HR. Interprofessional education and collaboration among healthcare students and professionals: a systematic review and call for action. J Interprof Care. 2021;35(4):612–21.
Mangiameli J, Hamiduzzaman M, Lim D, Pickles D, Isaac V. Rural disability workforce perspective on effective inter-disciplinary training—a qualitative pilot study. Aust J Rural Health. 2021;29(2):137–45.
Spiers MC, Harris M. Challenges to student transition in allied health undergraduate education in the Australian rural and remote context: a synthesis of barriers and enablers. Rural Remote Health. 2015;15(2):176–92.
Cosgrave C, Maple M, Hussain R. An explanation of turnover intention among early-career nursing and allied health professionals working in rural and remote Australia-findings from a grounded theory study. Rural Remote Health. 2018;18(3):1–7.
Ferns J, Hawkins N, Little A, Hamiduzzaman M. The escape room experience: exploring new ways to deliver interprofessional education. Innovations in Education and Teaching International. 2022:1–12.
Acknowledgements
We are thankful to Harry Gaffney who contributed to the review process.
Funding
Not funded.
Author information
Authors and Affiliations
Contributions
MH, SM, SC synthesised and analysed the data regarding the impact of allied health student placements and prepared initial draft of the manuscript. LG, JH, FB, PH, EC, NB, KT, CW, and VF contributed to the conceptualisation and was a major contributor in writing the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hamiduzzaman, M., Miles, S., Crook, S. et al. An integrative review of the impact of allied health student placements on current staff’s knowledge and procedural skills in acute and primary care settings. BMC Med Educ 24, 657 (2024). https://doi.org/10.1186/s12909-024-05632-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-024-05632-7