Abstract
Background
Electrocardiogram (ECG) is one of the most commonly performed examinations in emergency medicine. The literature suggests that one-third of ECG interpretations contain errors and can lead to clinical adverse outcomes. The purpose of this study was to assess the quality of real-time ECG interpretation by senior emergency physicians compared to cardiologists and an ECG expert.
Methods
This was a prospective study in two university emergency departments and one emergency medical service. All ECGs were performed and interpreted over five weeks by a senior emergency physician (EP) and then by a cardiologist using the same questionnaire. In case of mismatch between EP and the cardiologist our expert had the final word. The ratio of agreement between both interpretations and the kappa (k) coefficient characterizing the identification of major abnormalities defined the reading ability of the emergency physicians.
Results
A total of 905 ECGs were analyzed, of which 705 (78%) resulted in a similar interpretation between emergency physicians and cardiologists/expert. However, the interpretations of emergency physicians and cardiologists for the identification of major abnormalities coincided in only 66% (k: 0.59 (95% confidence interval (CI): 0.54–0.65); P-value = 1.64e-92). ECGs were correctly classified by emergency physicians according to their emergency level in 82% of cases (k: 0.73 (95% CI: 0.70–0.77); P-value ≈ 0). Emergency physicians correctly recognized normal ECGs (sensitivity = 0.91).
Conclusion
Our study suggested gaps in the identification of major abnormalities among emergency physicians. The initial and ongoing training of emergency physicians in ECG reading deserves to be improved.
Similar content being viewed by others
Introduction
Electrocardiograms (ECGs) are routine exams in the emergency department (ED). ECG is a painless, noninvasive way to diagnose many acute heart diseases, but misinterpretation may lead to inappropriate care. Breen CJ et al. reported major errors in up to 33% of ECG interpretations, and up to 11% resulted in inappropriate care [1]. A meta-analysis by Cook et al. published in 2020 highlights deficiencies in ECG interpretation [2]. There is no such thing as an established standard method for “teaching” ECG interpretation [1, 3]. The development of new diagnostic tools, such as ECG interpretation algorithms, is undeniable, but various studies have shown their current limitations [4, 5]. Overreliance on artificial aid may also lead to inappropriate care [6]. ED doctors must be able to correctly analyze ECGs; most recently, many publications have assessed students’ or residents’ ECG reading capacity in the emergency department [2, 7,8,9] with or without training. In 2022, ECG interpretation competency among healthcare professionals and students was assessed [10]. However, few studies have assessed the ECG analysis capacity of senior emergency physicians [2], particularly in front of cardiologists who confirm or reject the initial interpretation in daily practice. This study aimed to assess the ability of ECG interpretation by emergency physicians compared to cardiologists and an ECG expert.
Methods
Study design and setting
This observational and prospective study was conducted in two emergency departments (Bichat University Hospital, Paris, and Beaujon University Hospital, Clichy) of two university hospitals and in one emergency medical service (Beaujon University Hospital, Clichy) over 6 weeks in 2019, between September 23 and October 27.
We included all 12- or 18-lead ECG performed in these three centers and interpreted during working hours day or night by senior emergency physicians who completed a questionnaire. We excluded all ECGs interpreted by juniors or medical students, all questionnaires without ECGs, or ECGs without questionnaires and ECGs considered uninterpretable by cardiologists.
There was a unique ECG per patient, and the questionnaire was anonymous, without epidemiological data and principally focusing on the reason for ED visit (appendix).
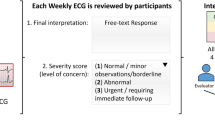
It was designed according to a protocol recently published [4]: it proposed 56 ECG abnormalities divided into 3 categories: urgent, significant and nonsignificant abnormalities.
The questionnaire followed the iterative thought process of an emergency physician who needs ECG to perform appropriate care for the patient. A question about its normality was first raised. If it was not normal, the emergency degree had to be mentioned as well as its significant characteristics.
We defined “Urgent” abnormalities requiring extreme urgent care; “Significant” abnormalities requiring serious consideration and relative emergency; “non-significant” minor or non-specific abnormalities; and “Normal” ECG without abnormality including normal variant. All ECGs were numbered and then separated from the questionnaire completed by emergency physicians.
An identical empty questionnaire was attached to each ECG and had been randomly distributed to 16 senior cardiologists of Bichat hospital. They performed a second analysis of the ECGs and completed the questionnaire unaware of the first analysis. Only the reason for ED consultation was known by cardiologists.
If there was a discordant interpretation between the emergency physician and cardiologist, we sought the opinion of an ECG expert (Dr Pierre Taboulet). The expert gave his interpretation independently, and the latter was considered the reference. If the expert’s interpretation was the same as that of the cardiologist, it was considered that there was a consensus between the cardiologist and the expert. If the expert’s interpretation differed from that of the cardiologist, he would reread the ECG, having taken note of the interpretations of both the emergency physician and the cardiologist, in order to reach a consensus after discussion. Finally, if no consensus was made for an ECG, it was decided to arbitrarily exclude it from this study.
Statistical analysis
The primary endpoint was to assess the quality of ECG interpretation by emergency physicians, defined as the level of concordance to those performed by cardiologists/experts for major anomaly recognition (urgent and significant). This was assessed by the ratio of agreement and Cohen’s kappa coefficient (k) with their 95% confidence interval (CI) [11, 12]. The ECG reading quality was respectively qualified as excellent, good, average, or poor if ≥ 90, ≥ 80, ≥70, ≤ 70% of the major abnormalities were correctly identified by the emergency physicians.
The kappa coefficient measures the interpretive agreement between the two raters.
We defined:
-
Perfect agreement 0.8 < kappa < 1.
-
Strong agreement 0.6 < kappa < 0.8.
-
Moderate agreement 0.4 < kappa < 0.6.
-
Weak agreement 0.2 < kappa < 0.4.
-
Very weak agreement 0 < kappa < 0.2.
As a secondary endpoint, we observed the performance of emergency physicians in classifying an electrocardiogram according to its level of emergency. Specificity (Sp), sensitivity (Se), positive predictive value and negative predictive value with their 95% CI were also calculated.
Data analyses were performed using R version 4.2.2. All statistical tests were two tailed, and a p-value of less than 0.05 was considered statistically significant.
Results
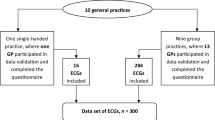
We collected 918 ECGs and analyzed 905 ECGs (Fig. 1).
Nine were excluded, five by emergency physicians because questionnaires were not correctly completed or not attached to the right ECG, and four by cardiologists and/or experts because they considered them uninterpretable (artefacts, errors due to electrode position and one to pathological issues due to resuscitation after cardiac arrest). There were 296 discordant ECGs between emergency physicians and cardiologists. The expert reread all 296 ECGs. Among which he agreed with the cardiologists for 150 ECGs, with the emergency physicians for 81 ECGs and with neither for the remaining 65.
We reported 63 different reasons for consultation, and the most common were chest pain (16%), discomfort (8%), abdominal pain (6%), dyspnea (3%), fall (3%) and palpitations (3%). The reason was not mentioned for 319 ECGs (35%). Cardiologists and experts (C/E) classified 49 urgent (5%), 246 significant (27%), 200 nonsignificant (22%) and 410 (45%) normal ECGs. Emergency physicians listed 61 urgent (7%), 232 significant (26%), 178 non-significant (20%) and 434 (48%) normal ECGs (Fig. 2).
The most common urgent anomalies (Table 1) detected by C/E were atrial fibrillation with a heart rate greater than 120 bpm (29%), NSTEMI (non-ST elevation myocardial infarction) (22%) and STEMI (ST elevation myocardial infarction) (19%).
The most common significant anomalies detected by C/E (Table 2) were tachycardia with a heart rate above 100 bpm (28%), complete right bundle branch block (14%), atrial fibrillation with a heart rate between 45 and 120 bpm (12%), rhythm driven by a pacemaker between 45 and 120 bpm (9%), chronic STEMI sequels (8%) and ventricular hypertrophy (8%). ECG interpretations by emergency physicians matched those by C/E in 78% of cases.
Primary endpoint:
In 66% of cases, emergency physicians and cardiologists/experts identified the same major (urgent and significant) abnormalities for 196 (38+158) ECGs out of 295 (49+246). The Kappa coefficient (k) was 0.59 (95% confidence interval (CI): 0.54–0.65); P-value = 1.64e-92 (Table 3).
Among the 49 ECGs classified as urgent by the cardiologists/experts, 38 (78%) were correctly interpreted by the emergency physicians (k = 0.69 (95% CI: 0.59–0.79); P-value = 3.5e-40).
Among the 246 ECGs showing the most serious abnormalities recognized by the cardiologists/experts and classified as significant, 158 (64%) were correctly interpreted by the emergency physicians (k = 0.62 (95% CI: 0.57–0.69); P-value = 1.65e-96)).
Secondary endpoint:
ECGs were consistently classified in 82% of the cases on the degree of urgency (without looking at the diagnosis accuracy) between cardiologists/experts and emergency physicians (Table 4). Namely, emergency physicians identified 41 out of 49 ECGs (84%) classified as “urgent” by cardiologists/experts, and similarly, 195 out of 246 ECGs (79%) classified as “significant”, 136 out of 200 ECGs (68%) classified as “non significant”, and 373 out of 410 ECGs (91%) classified as normal by cardiologists/experts.
The Kappa coefficient was 0.73 (0.70–0.77); P-value ≈ 0. The weighted Kappa was 0.78 (74–0.81) with linear weighting and 0.81 (0.81–0.81) with quadratic weighting (Table 4).
The ability of the emergency physicians to discerning normal ECGs (91%) was globally good but less accurate for “urgent” (85%), “significant” (79%) and “non-significant” (68%) ECGs.
However, the specificity of recognition of normal ECGs (88%) was not better than that of “urgent” (98%), “significant” (94%) and “non-significant” (94%) ECGs (Table 5).
The positive predictive value was better for normal ECGs (86%), then in decreasing order for significant (84%), non-significant (76%) and urgent (67%) ECGs. In contrast, the negative predictive value was better for urgent ECGs (99%) than for normal (92%), significant (92%) and non-significant (91%) ECGs.
Regarding the three most frequent emergency abnormalities present on ECGs, atrial fibrillation with a heart rate greater than 120 bpm seemed to be moderately recognized by emergency physicians (Se = 0.79). Meanwhile, they appeared to be very good at identifying ECGs compatible with ST- coronary syndrome (Se = 0.91) and ST + coronary syndrome (Se = 1) (Table 5).
Discussion
Emergency physicians showed good capacity to correctly identify major abnormalities. The recognition accuracy of major anomalies present on an ECG was critical because these anomalies might an impact patient management. Similarly, discordant classification between a normal ECG and a “non-significant” ECG could not harm the patient. Kappa coefficients were calculated to support these results, which was a measure of inter-rater agreement. The agreement between cardiologists/experts and emergency physicians was moderate for major abnormalities.
The overall agreement in the interpretation of ECGs between emergency physicians and cardiologists/experts is much better than the agreement in the interpretation of major abnormalities. This could be explained by the fact that a large proportion of the ECGs included in the study were normal and that the ability to identify them by emergency physicians was excellent. The results can be generalized to the French population consulting the emergency department, notably because of the large sample size but also because the reasons leading to the consultation during which the ECGs were performed in our study were similar to the reasons for consultation identified in the other studies [13]. Additionally, the high proportion of normal ECGs and the most frequently recognized abnormalities were similar to other studies [4, 13].
Beyond discerning the correct abnormality, it is more important to correctly classify an ECG according to its emergency level. This is mainly because “urgent” ECGs require rapid management, and “significant” ECGs have clinical significance for the diagnostician and may lead to additional investigations or advice from a cardiologist.
In general, ECG classification according to their degree of urgency by emergency physicians seemed good, but emergency physicians tended to recognize more urgent abnormalities than C/E. This could lead to overmedicalization, which could be harmful to the patient. They also had more difficulties to recognize nonsignificant abnormalities. The Kappa linear weighting and quadratic weighting were higher than the unweighted Kappa coefficient for the classification of the different ECGs. This means that the consistency of ECG classification between the two evaluators (emergency physicians vs. cardiologists/experts) appears to be higher when the clinical significance of the abnormality is taken into account.
The sensitivity of the emergency physicians concerning the recognition of normal ECGs was globally good but less efficient for other stages of emergency. On the other hand, the specificity of recognition of normal ECGs was worse than that of the others. In other words, emergency physicians recognized normal ECGs well but abnormalities too often. Moreover, when they considered an ECG as “non urgent”, the probability that this ECG was indeed not an emergency was very high.
Among the three most frequent emergency abnormalities present on ECGs performed in the emergency department, atrial fibrillation with a heart rate greater than 120 bpm was moderately recognized by emergency physicians. While, they were very good at matching ECGs compatible with STEMI and N-STEMI.
Our results were consistent with those in the literature [1]. ECG interpretation proved to be a difficult exercise [1, 2]. Some studies have shown that noncardiologists make more ECG interpretation errors than cardiologists [2, 10]. Interpretation algorithms can reduce the time needed to interpret ECGs and can reduce ECG interpretation errors [1]. However, they have been shown to be less accurate than physicians and should only be used as an additional interpretation tool for a trained provider [1, 3]. While continuing education of emergency physicians in ECG analysis is a major issue [14, 15], evidence of the need for universal predefined training to achieve and maintain ECG interpretation skills is not available [1]. Several methods could be used, such as simulation [16], self-study [17] or work-shops [18].
The implementation of an ECG reading checklist in emergency departments could possibly decrease the rate of ECG misinterpretation. A double reading of emergency ECGs by an ECG expert could be considered to catch potential misdiagnoses. The development of an interactive interpretation aid application with a training function could meet the need for continuing education of residents.
Limitations
The study was a multicentric study, but it concerns 3 centers in Ile de France that are geographically close. Moreover, the vast majority of the doctors practicing in the EMS also work in one of the emergency departments. A multicentric study integrating several emergency services spread all over France would truly represent the performances of French emergency physicians concerning the interpretation of ECG.
Clinical experience increased ECG interpretation competency [19, 20]. In the present study, the population of emergency physicians who answered the questionnaire was not analyzed: training and number of years as a senior.
The study shows that the ability of emergency physicians to identify major anomalies is poor. However, the interpretation of an ECG is always carried out in a precise clinical context (age, history, symptomatology and clinical examination) with blood tests and possible advice from the cardiologist.
It should be noted that the cardiologists did not have this information. The absence of a global context makes the interpretation of ECGs more difficult for them.
We chose cardiologists and experts as the reference for ECG interpretation in our study because it has been proven that cardiologists are the best for ECG interpretation. However, the literature indicates that the accuracy of ECG interpretation by cardiologists was 74.9% [2]. As this was not perfect, choosing cardiologists as the reference for interpretation represents a bias. Double analysis by the cardiologists and by the expert allowed us to limit this bias.
Our consecutive cases study assessed both specificity (consecutive cases have a large number of normal ECGs). But sensitivity is also important, and this requires a large number of true positives. The methods for such studies could be a combination of case control and consecutive in order to have lots of normal and lots of abnormal.
Conclusion
The overall interpretation accuracy of ECGs in our study seems to be good, and emergency physicians seem to be quite good at determining the degree of urgency of an ECG. However, their reading of major anomalies is poor compared to cardiologists.
The initial and ongoing training of emergency physicians in ECG reading should be improved.
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CI:
-
Confidence Interval
- ECG:
-
Electrocardiogram
- ED:
-
Emergency Department
- EP:
-
Emergency Physician
- Se:
-
Sensitivity
- Sp:
-
Specificity
References
Breen CJ, Kelly GP, Kernohan WG. ECG interpretation skill acquisition: a review of learning, teaching and assessment. J Electrocardiol. 2019;:S0022-0736(18)30641-1.
Cook DA, Oh S-Y, Pusic MV. Accuracy of Physicians’ Electrocardiogram Interpretations: a systematic review and Meta-analysis. JAMA Intern Med. 2020;180:1461–71.
Auseon AJ, Schaal SF, Kolibash AJ, Nagel R, Lucey CR, Lewis RP. Methods of teaching and evaluating electrocardiogram interpretation skills among cardiology fellowship programs in the United States. J Electrocardiol. 2009;42:339–44.
Smith SW, Walsh B, Grauer K, Wang K, Rapin J, Li J, et al. A deep neural network learning algorithm outperforms a conventional algorithm for emergency department electrocardiogram interpretation. J Electrocardiol. 2019;52:88–95.
Shah AP, Rubin SA. Errors in the computerized electrocardiogram interpretation of cardiac rhythm. J Electrocardiol. 2007;40:385–90.
Bogun F, Anh D, Kalahasty G, Wissner E, Bou Serhal C, Bazzi R, et al. Misdiagnosis of atrial fibrillation and its clinical consequences. Am J Med. 2004;117:636–42.
Ginde AA, Char DM. Emergency medicine residency training in electrocardiogram interpretation. Acad Emerg Med. 2003;10:738–42.
Hartman ND, Wheaton NB, Williamson K, Quattromani EN, Branzetti JB, Aldeen AZ. A Novel Tool for Assessment of Emergency Medicine Resident Skill in determining diagnosis and management for Emergent Electrocardiograms: a Multicenter Study. J Emerg Med. 2016;51:697–704.
Bilello LA, Pascheles C, Grossman SA, Chiu DT, Singleton JM, Rosen CL. Electrocardiogram interpretation: emergency medicine residents on the front lines. Am J Emerg Med. 2019;37:1000–1.
Amini K, Mirzaei A, Hosseini M, Zandian H, Azizpour I, Haghi Y. Assessment of electrocardiogram interpretation competency among healthcare professionals and students of Ardabil University of Medical Sciences: a multidisciplinary study. BMC Med Educ. 2022;22:448.
Cohen J. A coefficient of Agreement for Nominal Scales. Educ Psychol Meas. 1960;20:37–46.
Fleiss JL, Cohen J, Everitt BS. Large sample standard errors of kappa and weighted kappa. Psychol Bull. 1969;72:323–7.
Peschanski N, Chouihed T, Charpentier S, Ameur L, Andrianjafy H, Soulat L, et al. Épidémiologie électrocardiographique en urgence. Étude ECG-Day 1. Ann Fr Med Urgence. 2016;6:240–5.
Werner K, Kander K, Axelsson C. Electrocardiogram interpretation skills among ambulance nurses. Eur J Cardiovasc Nurs. 2016;15:262–8.
Ratanawongsa N, Thomas PA, Marinopoulos SS, Dorman T, Wilson LM, Ashar BH, et al. The reported validity and reliability of methods for evaluating continuing medical education: a systematic review. Acad Med. 2008;83:274–83.
Cook DA, Hamstra SJ, Brydges R, Zendejas B, Szostek JH, Wang AT, et al. Comparative effectiveness of instructional design features in simulation-based education: systematic review and meta-analysis. Med Teach. 2013;35:e867–898.
Riding NR, Drezner JA. Performance of the BMJ learning training modules for ECG interpretation in athletes. Heart. 2018;104:2051–7.
Baral PK, Jajčanin-Jozić N, Deller S, Macheroux P, Abramić M, Gruber K. The First structure of dipeptidyl-peptidase III provides insight into the Catalytic mechanism and Mode of substrate Binding*♦. J Biol Chem. 2008;283:22316–24.
Tahboub OY, Yilmaz UD. Nurses’ Knowledge and Practices of Electrocardiogram Interpretation. Int Cardio Res J. 2019;13.
Viljoen CA, Millar RS, Manning K, Hoevelmann J, Burch VC. Clinically contextualised ECG interpretation: the impact of prior clinical exposure and case vignettes on ECG diagnostic accuracy. BMC Med Educ. 2021;21:417.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Alice Perrichot: Data curation; Formal analysis; Investigation; Software; Visualization; Roles/Writing - original draft;Pradeebane Vaittinada Ayar: Formal analysis; Methodology; Validation; Writing - review & editingPierre Taboulet: Conceptualization; formal analysis; methodology; validationMatthieu Gay: Formal analysis; Writing - review & editingChristophe Choquet: Formal analysis; Writing - review & editingEnrique Casalino: Formal analysis; Writing - review & editingPhilippe Gabriel Steg: Conceptualization; Formal analysis; ResourcesSonja Curac: Conceptualization; Formal analysis; Methodology; Project administration; Supervision; Validation; Writing - review & editingPrabakar Vaittinada Ayar: corresponding author, Data curation; Formal analysis; Software; Supervision; Validation; Visualization; Roles/Writing - original draft; Writing - review & editingAll authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The work conformed to the Declaration of Helsinki. ED senior physicians involved in the study were clearly informed of the study objectives, and consent was obtained from all participants. Moreover, the data were treated in the strictest confidentiality without any patient’s demographic data. Local ethics committees approved the study (Comité éthique des Hôpitaux Universitaires Paris Nord Val de Seine).
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Perrichot, A., Vaittinada Ayar, P., Taboulet, P. et al. Assessment of real-time electrocardiogram effects on interpretation quality by emergency physicians. BMC Med Educ 23, 677 (2023). https://doi.org/10.1186/s12909-023-04670-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-023-04670-x