Abstract
Aim
As periodontitis and dyslipidemia are diseases that occur with high incidence, the relationship between them has attracted much attention. Previous studies on these diseases have tended to focus on lipid parameters and periodontitis, we aimed to investigate the relationship between dyslipidemia and periodontitis.
Materials and methods
A comprehensive search to identify the studies investigating the relationship between dyslipidemia and periodontitis was performed on PubMed, Web of Science and Cochrane Library before the date of August, 2023. Studies were considered eligible if they contained data on abnormal blood lipid parameters and periodontitis. Studies that reported mean differences and 95% confidence intervals or odds ratios were used.
Results
A total of 73 publications were included in the meta-analysis. Hyper total cholesterol (TC), triglycerides (TGs), low-density lipoprotein (LDL), very low-density lipoprotein (VLDL) and lower high-density lipoprotein (HDL) levels are risk factors for periodontitis. Periodontal disease is a risk factor for high TG and low HDL levels. Three months after periodontal treatment, the levels of TC, TG and HDL were significantly improved, and statin treatment only improved gingival index (GI) levels compared to that of the dietary control.
Conclusions
The findings reported here suggest that the mutual promotion of periodontitis and dyslipidemia can be confirmed. Non-surgical periodontal therapy may improve lipid abnormalities. It can’t be demonstrated whether systematic application of statins have a better effect on the improvement in periodontal status in patients with dyslipidemia compared to that of the control.
Similar content being viewed by others
Introduction
Periodontitis involves inflammation that extends deep into tissues and causes loss of supporting connective tissue and alveolar bone [1]. The term ‘periodontal diseases’ encompasses a wide variety of chronic inflammatory conditions involving the gingiva (or gums, which are the soft tissue surrounding the teeth), bone and ligament (the connective tissue collagen fibres that anchor a tooth to alveolar bone) that support teeth [2]. In 2017, the age-standardized prevalence of severe periodontitis was 9.8%, and the number of prevalent cases was 796 million [3]. Gum recession and alveolar bone resorption are typical manifestations of periodontal disease (Pd). Severe periodontitis causes bleeding gums, impaired chewing, and eventually tooth loss. Epidemiologically, periodontitis is associated with several chronic disorders, such as cardiovascular disease, type 2 diabetes mellitus (T2DM), rheumatoid arthritis, inflammatory bowel disease (IBD), Alzheimer’s disease, nonalcoholic fatty liver disease and certain cancers [4]. Multiple parameters, including probing depth (PD), clinical attachment level (CAL), and bleeding on probing (BOP) must be recorded at six locations per tooth to accurately diagnose periodontitis [2]. The plaque index (PI) and gingival index (GI) are also important indicators. The critical risk factor for periodontitis is subgingival plaque. The development of periodontitis is associated with a subgingival microbial community that is imbalanced and enriched with species such as Porphyromonas gingivalis, Tannerella forsythia and Treponema denticola. In addition to bacteria, smoking and some systemic diseases, such as diabetes and osteoporosis, are crucial risk factors for periodontitis [5,6,7].
Dyslipidemia is a disorder that involves lipoproteins in plasma. Laboratory examination showed elevated TC, elevated TG, elevated LDL, elevated VLDL or reduced HDL. There is now a broad consensus that dyslipidemia is a major risk factor for developing cardiovascular disease (CVD). Dyslipidemia can also contribute to the risk of an ischaemic cerebrovascular accident. Since 2002, Asia has been rapidly urbanized and the dietary habits and lifestyles of people have changed, and the prevalence of dyslipidemia has also increased; a large national survey conducted in 2013–2014 in 163,641 Chinese adults showed that the most common forms of dyslipidemia are low plasma HDL-cholesterol levels (20.4% of the population) and high plasma triglyceride levels (13.8%) [8].
Since the 1990s, the relationship between periodontitis and dyslipidemia has attracted considerable interest due to the damage these diseases cause to human health. However, the conclusions of these studies are not completely consistent. To gain expertise on the current standings of research and clinical implications, we searched multiple databases and identified the following relevant directions of research: 1. The influence of dyslipidemia on periodontitis, 2. The influence of periodontitis on dyslipidemia, 3. The influence of periodontal treatment on dyslipidemia, and 4. The effect of blood lipid treatment on periodontitis. In this review, we produced a comprehensive summary of the connection between periodontitis and dyslipidemia.
Materials and methods
This review was conducted and reported according to the PRISMA statement [9] and the Cochrane Handbook [10].
Principal question
Is there an association between dyslipidemia and periodontitis? Will the treatment of dyslipidemia or periodontitis influence the other disease?
Search strategy
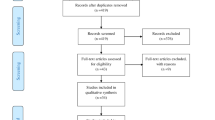
The following electronic databases were searched for dates before August 1st, 2023: PubMed, Web of Science and Cochrane Library. The detailed search strategy is shown in Fig. 1.
Two independent reviewers screened records for potentially eligible titles and abstracts and subsequently reviewed full texts to determine the inclusion in the meta-analysis. Disagreements were resolved with a third reviewer to reach a consensus.
Study selection
Abstracts and references were managed using EndNote. The criteria for selecting the eligible articles were as follows: (I) cross-sectional studies, cohort studies, case–control studies and clinical trials. (II) The main goal was to research the relationship between dyslipidemia and periodontitis. (III) When the study population was repeated, we used the most recent study that involved the largest study population. (IV) Studies on syndromes, such as metabolic syndrome (MetS) or Coronary heart disease (CHD), in which the blood lipids were described but the blood lipid levels were not described were excluded. (V) All in vitro and in vivo animal experiments were excluded.
Data extraction
We extracted the data on the author, year, country, study design, sample size, diagnosis criteria for periodontal disease, BMI match or correction, mean age, age ratio, sex ratio, matching or correction factor, effect index and quality evaluation. We will list them separately in Tables 1, 2, 3 and 4.
Clinical definitions of periodontal disease
To eliminate the diagnosis bias, we made the following definitions:
-
a.
Secure periodontitis:
At least one site with a probing depth (PD) ≥ 4 mm in every quadrant and radiographic evidence of bone loss, or.
At least two sites in non-adjacent teeth with interproximal attachment loss ≥3 mm, or.
At least two sites with PD ≥ 4 mm and CAL ≥ 3 mm, or.
A community periodontal index (CPI) score of 4 in at least one quadrant, or.
For cases in which no CAL or PD is reported, radiographic marginal alveolar bone loss is ≥30%
-
b.
Insecure periodontitis:
Periodontitis was defined only by PD or CAL but without a clear definition.
Quality assessment
The quality of the included case–control studies and cohort studies was assessed using the Newcastle–Ottawa Scale (NOS). The article quality was assessed as follows: low quality = 0–4; moderate quality = 5–6; high quality = 7–9. The methodological quality of the cross-sectional studies included was assessed using an 11-item checklist recommended by the Agency for Healthcare Research and Quality (AHRQ). An item was scored “0” if it was answered “NO” or “UNCLEAR”; if it was answered “YES”, then the item scored 1″. Article quality was assessed as follows: low quality = 0–3; moderate quality = 4–7; high quality = 8–11 [84]. The quality of the randomized controlled trial was assessed using the Cochrane Collaboration’s tool for assessing the risk of bias in randomized trials. Detailed quality evaluation is listed in Supplementary Tables S1, 2, 3, 4.
Data analysis
For continuous data, the pooled effect was estimated as the mean difference (MD) and the 95% confidence interval (CI). For the dichotomous data, the pooled effect was estimated as the odds ratio (OR) and 95% CI. All pooled estimates were obtained using the random effects model of DerSimonian and Laird, which considers both within-study and between-study variations and provides more conservative estimates than those of a fixed-effects model [85, 86]. The heterogeneity among studies was assessed using the I2 statistic, which determines the proportion of variability across studies that is due to heterogeneity rather than sampling error [87]. A P value less than 0.10 or an I2 -value over 50% indicates substantial heterogeneity.
If heterogeneity existed in the pooled studies, meta-regressions were performed to explain the sources of between-study heterogeneity, and these sources included the published year, region, study design, total sample size, quality of study, age, sex, BMI matched, periodontal diagnosis and multi-variable analysis.
To examine the influence of each study on the pooled estimates, sensitivity analyses were conducted using the leave-one-out method, which removes one study each time and repeats the analysis [88]. Egger’s and Begg’s tests were used to detect publication bias in all meta-analyses.
All statistical analyses were carried out using R 3.6.1 software. P values less than 0.05 were considered statistically significant, except when otherwise specified.
Results
Literature search
The literature search identified 687 relevant publications. A total of 205 duplicates were removed. Screening the titles and abstracts resulted in the elimination of 267 studies that failed to meet any of the inclusion criteria, and all proceedings and books were removed. We also excluded all animal experiments and in vitro experiments.Twenty-one reviews and meta-analyses were removed. A total of 115 papers were selected for full-text screening. In 18 articles, Mets or CHD was used as the research object but without a blood lipid index, and 20 articles did not include data on the relationship between periodontitis and blood lipids; we excluded these articles from our current investigation. 6 studies contained repetitive populations, and we used the most recent study with the largest study population. After the quadratic search for reviews, we finally identified 73 articles. (Fig. 1).
Association between dyslipidemia and periodontitis: periodontitis as the outcome
-
i.
TC and periodontitis
Twenty-four studies evaluated the difference in the serum TC level between periodontitis and healthy control groups with the mean (SD). TC levels were higher in patients with periodontitis than in controls, with a pooled mean difference of 11.29 mg/dL (95%-CI: 6.52, 16.06, p < 0.01). There was significant heterogeneity between the studies (I2 = 88%, p < 0.01) (Fig. 2a). Meta-regression showed that the sources of the heterogeneity may be diagnosis of periodontitis (P diagnosis) (p = 0.041) and BMI matching (p = 0.073) (Table S5). The result was robust regardless if any one study was omitted (Supplementary Fig. 1-a). No significant publication bias was found after Egger’s (p = 0.148) and Begg’s tests (p = 0.275).
Forest plot of mean difference for comparisons:periodontitis versus non-periodontitis. (a) periodontitis have high serum TC level; (b) periodontitis have high serum TG level; (c) periodontitis have high serum LDL level; (d) periodontitis have low serum HDL level; (e) periodontitis have high serum VLDL level. Abbreviations: TC:Total cholesterol, TG: triglycerides, LDL: low-density lipoprotein, HDL: high-density lipoprotein, VLDL: very low-density lipoprotein
Sixteen studies reported the OR values to evaluate the association between the serum TC level and periodontitis. The pooled OR was 1.83 (95%-CI: 1.40, 2.38, p < 0.01), and substantial heterogeneity between the studies was found (I2 = 77%, p < 0.01) (Fig. 3a), indicating that a high TC level is a risk factor for periodontitis. Meta-regression showed that the sources of the heterogeneity were the year of publication (p < 0.001), study design (p < 0.001), age ratio (p < 0.001), P diagnosis (p = 0.001) and adjusted OR (p = 0.001) (Table S5). The result was robust regardless if any one study was omitted (Supplementary Fig. 2-a). A significant publication bias was found after Egger’s (p < 0.001) and Begg’s tests (p = 0.021).
-
ii.
TG and periodontitis
Forest plot of OR values for different lipids levels with the risk of periodontitis. a high TC level is associated with the high risk of periodontitis; (b) high TG level is associated with the high risk of periodontitis; (c) high LDL level is associated with the high risk of periodontitis; (d) low HDL level is associated with the high risk of periodontitis. Abbreviations: TC:Total cholesterol, TG: triglycerides, LDL: low-density lipoprotein, HDL: high-density lipoprotein
Twenty-six studies evaluated the difference in the serum TG level between periodontitis and healthy control groups with the mean (SD). TG levels were higher in periodontitis patients than in controls, with a pooled mean difference of 23.92 mg/dL (95%-CI: 15.52, 32.31, p < 0.01). There was significant heterogeneity between the studies (I2 = 100%, p = 0) (Fig. 2b). The meta-regression did not find any significant source of heterogeneity (Table S5). The result was robust regardless if any one study was omitted (Supplementary Fig. 1-b). No significant publication bias was found after Egger’s(p = 0.336) and Begg’s tests (p = 0.061).
Seventeen studies reported the OR values to evaluate the association between the serum TG level and periodontitis. The pooled odds ratio was 1.58 (95%-CI: 1.32, 1.90). We used the random effect model due to the presence of heterogeneity between studies (I2 = 71%, p < 0.01) (Fig. 3b), indicating that TG levels were significantly associated with periodontitis and that high TG levels are a risk factor for periodontitis. Meta-regression showed that the sources of the heterogeneity were the year of publication (p = 0.004), study design (p < 0.001), total sample size (p < 0.001), age (p = 0.001), P diagnosis (p = 0.001) and adjusted OR (p = 0.001) (Table S5). The result was robust regardless of if any one study was omitted (Supplementary Fig. 2-b). A significant publication bias was found after Egger’s(p = 0.003) and Begg’s tests(p = 0.006) .
-
iii.
LDL and periodontitis
Twenty two studies evaluated the difference in the serum LDL level between periodontitis and healthy control groups with the mean (SD). LDL levels were higher in periodontitis patients than in controls, with a pooled mean difference of 6.26 mg/dL (95% CI: 1.91, 10.61, p < 0.01). There was significant heterogeneity between the studies (I2 = 92%, p < 0.01). (Fig. 2c) However, the meta-regression did not find any significant source of heterogeneity (Table S5). The result was robust regardless if any one study was omitted (Supplementary Fig. 1-c). No significant publication bias was found after Egger’s(p = 0.277) and Begg’s tests (p = 0.271).
Nine studies reported the OR values to evaluate the association between the serum LDL level and periodontitis. The pooled OR was 2.11 (95%-CI: 1.32, 3.40, p < 0.01), indicating that LDL levels were significantly associated with periodontitis and that high LDL levels are a risk factor for periodontitis. We used the random effect model due to the presence of heterogeneity between studies (I2 = 71%, p < 0.01) (Fig. 3c). Meta-regression showed that the sources of the heterogeneity were the study design (p < 0.001), total sample size (p = 0.014), and P diagnosis (p = 0.018) (Table S5). The result was robust regardless if any one study was omitted (Supplementary Fig. 2-c). A significant publication bias was found after Egger’s(p = 0.277) and Begg’s tests (p = 0.271).
-
iv.
HDL and periodontitis
Twenty-four studies evaluated the difference in the serum HDL level between periodontitis and healthy control groups with the mean (SD). The HDL levels were lower in periodontitis patients, and the pooled mean difference for the HDL levels in the periodontitis patients and healthy control groups was − 3.45 mg/dL (95%-CI: − 4.47, − 2.44 mg/dL, p < 0.01). There was significant heterogeneity between the studies (I2 = 64%, p < 0.01) (Fig. 2d). Meta-regression showed that age may be the source of the heterogeneity (p = 0.003) (Table S5). The result was robust regardless if any one study was omitted (Supplementary Fig. 1-d). No significant publication bias was found after Egger’s(p = 0.427) and Begg’s tests (p = 0.843).
Thirteen studies reported the OR values to evaluate the association between the serum HDL level and periodontitis. The pooled OR was 1.25 (95% CI: 1.15, 1.35, p < 0.01), indicating that a low HDL level is a risk factor for periodontitis. There was no significant evidence for heterogeneity between the studies (I2 = 0%, p = 0.64) (Fig. 3d). The result was robust regardless if any one study was omitted (Supplementary Fig. 2-d). A significant publication bias was found after Egger’s(p = 0.030) and Begg’s tests (p = 0.961).
-
xxii.
VLDL and periodontitis
Four studies evaluated the difference in the serum VLDL level between periodontitis and healthy control groups with the mean (SD). The VLDL levels were higher in periodontitis patients than in controls, with a pooled mean difference of 8.69 mg/dL (95% CI: 2.20, 15.18, p < 0.01). There was significant heterogeneity between the studies (I2 = 81%, p < 0.01) (Fig. 2e). No significant publication bias was found after Egger’s(p = 0.266). and Begg’s tests (p = 0.174).
Some studies were not included in our meta-analysis due to the lack of information utilized. Saxlin T reported an association between high serum triglycerides and low HDL-cholesterol levels with periodontal pockets by quintiles [39]. Akkaloori Anitha stated that the mean LDL and VLDL levels were significantly higher and the HDL levels were lower in periodontal patients than in healthy controls [12].
Association between dyslipidemia and periodontitis: dyslipidemia as the outcome
Periodontitis and dyslipidemia
Three studies reported OR values to evaluate the association between periodontitis and dyslipidemia. Periodontitis was a risk factor for abnormal increases in TG levels, with a pooled OR of 1.17 (95% CI: 1.04, 1.33). There was no significant heterogeneity between studies (I2 = 5%, p = 0.37) (Fig. 4a). The result was meaningless when the study by Fukui N, 2012 was omitted (Supplementary Fig. 3-a). No significant publication bias was found after Egger’s(p = 0.769) and Begg’s tests (p = 1.000).
Periodontitis was a risk factor for abnormal decreases in HDL levels, with a pooled OR of 1.40 (95% CI: 1.23, 1.60, p < 0.01), and there was no significant heterogeneity among the studies (I2 = 0%, p = 0.69) (Fig. 4b). The result was robust regardless if any one study was omitted (Supplementary Fig. 3-b). No significant publication bias was found after Egger’s(p = 0.746) and Begg’s tests (p = 1.000).
Since the pathological changes in other indicators, including TC, LDL and VLDL, are often not regarded as classic indicators of dyslipidemia, we only analysed the results of hyper TG and low LDL.
-
i.
PD and dyslipidemia
Eight studies evaluated the difference in the PD level between dyslipidemia patients and healthy control groups with the mean (SD). The PD levels were higher in dyslipidemia patients than in controls, with a pooled mean difference of 0.41 mm (95%-CI: 0.23, 0.58, p < 0.01). There was significant heterogeneity between the studies (I2 = 66%, p < 0.01) (Fig. 5a). Meta-regression showed that the sources of the heterogeneity may include the year of publication (p = 0.038) and region (p = 0.038) (Table S6). The result was robust regardless if any one study was omitted (Supplementary Fig. 4-a). No significant publication bias was found after Egger’s(p = 0.178) and Begg’s tests (p = 0.095).
-
ii.
CAL and dyslipidemia
Forest plot of mean difference for comparisons: dyslipidemia versus non- dyslipidemia (a) dyslipidemia have deeper PD; (b) dyslipidemia have more CAL (c) dyslipidemia have more BOP but not significant; (d) dyslipidemia have bigger PI; (e) dyslipidemia have bigger GI but not significant, Abbreviations: PD: probing depth, CAL: clinical attachment level, BOP: bleeding on probing, PI: plaque index, GI: gingival index
Eight studies evaluated the difference in the CAL level between dyslipidemia patients and healthy control groups with the mean (SD). The CAL levels were higher in dyslipidemia patients, with a pooled mean difference of 0.56 mm (95%-CI: 0.35, 0.78, p < 0.01). There was significant heterogeneity between studies (I2 = 62%; p < 0.01) (Fig. 5b). However, no significant source of heterogeneity was found through the meta-regression (Table S6). The result was robust regardless if any one study was omitted (Supplementary Fig. 4-b). No significant publication bias was found after Egger’s (p = 0.519) and Begg’s tests (p = 0.532).
-
iii.
BOP and dyslipidemia
Four studies evaluated the difference in the BOP level between dyslipidemia patients and healthy control groups with the mean (SD). No significant difference in BOP levels was found between dyslipidemia patients and healthy controls. There was significant heterogeneity between studies (I2 = 97%; p < 0.01) (Fig. 5c). Meta-regression showed that the sources of the heterogeneity may be the year of publication (p < 0.001), total sample size (p = 0.004), age (p < 0.001) and sex ratio (p = 0.002) (Table S6). The result was significant when the study by Lutfioglu M, 2017 [61] was omitted (Supplementary Fig. 4-c). No significant publication bias was found after Egger’s(p = 0.848) and Begg’s tests (p = 0.497).
-
iv.
PI and dyslipidemia
Six studies evaluated the difference in the PI level between dyslipidemia patients and healthy control groups with the mean (SD). PI levels were higher in dyslipidemia patients, with a pooled mean difference of 0.27 (95%-CI: 0.07, 0.47, p < 0.01). There was significant heterogeneity between studies (I2 = 82%; p < 0.01) (Fig. 5d). Meta-regression showed that the sources of the heterogeneity may be sex (p = 0.013) (Table S6). The result was meaningless when the study of Dogan B, 2015 or Shivakumar T, 2013 was omitted (Supplementary Fig. 4-d). No significant publication bias was found after Egger’s(p = 0.379) and Begg’s tests (p = 0.453).
-
xxii.
GI and dyslipidemia
Four studies evaluated the difference in the GI level between dyslipidemia patients and healthy control groups with a mean (SD). No significant difference in GI level was found between dyslipidemia patients and healthy control groups (Fig. 5e). Meta-regression showed that the sources of the heterogeneity may be Study design(p < 0.001), Quality(p < 0.001) and Gender ratio(p < 0.001) (Table S6). The result was robust regardless if any one study was omitted (Supplementary Fig. 4-e). No significant publication bias was found after Egger’s(p = 0.193) and Begg’s tests (p = 0.050).
Effect of periodontal treatment on blood lipids
Three studies evaluated the difference in the association between non-surgical periodontal treatment groups and the control groups with the mean (SD). No significant publication bias was found after Egger’s and Begg’s tests (p > 0.05).
-
i.
Nonsurgical periodontal treatment and TC
Compared with the control group, the level of TC in the serum of patients who received a non-surgical periodontal treatment was decreased significantly after 3 months, and the pooled mean difference for TC in the treatment and control groups was − 8.32 mg/dL (95% CI: − 16.59, − 0.05, p = 0.05). There was no significant heterogeneity between the studies (I2 = 0, p = 0.75) (Fig. 6a2). The result was meaningless regardless if any one study was omitted (Supplementary Fig. 5-a2).
Forest plot of mean difference for comparisons: periodontal treatment versus non-treatment among periodontitis patients. (a1–2) periodontitis treatment can decrease the TC level after 3 months; (b1–2) periodontitis treatment can decrease the TG level after 3 months; (c1–2) periodontitis treatment can increase the HDL level after 3 months; (d1–2) periodontitis treatment do not significantly decrease the LDL level after 3 months. Abbreviations: TC:Total cholesterol, TG: triglycerides, HDL: high-density lipoprotein, LDL: low-density lipoprotein
Several studies that reported positive results were excluded from the meta-analysis because they did not have the standardized clinical data we needed. DUAN Jinyu et al. reported that 3 months after a nonsurgical periodontal treatment, the cholesterol levels were significantly reduced. With 5.72 mmol/l as the diagnostic criterion, four of eight hypercholesterolemia patients returned to normal serum cholesterol levels [67]. The research by A. Surdumacove produced similar results; compared with the control group that received only oral hygiene guidance, the test group that received a non-surgical periodontal treatment exhibited a significant decrease in TC levels after 1 month [71]. Zuza EP et al. reported an interesting result: after non-surgical periodontal treatments, TC levels in obese patients were significantly reduced 3 months later, but the same results were not observed in nonobese patients [77].
-
ii.
Nonsurgical periodontal treatment and TG
Compared with the control group, the level of TG in the serum of patients who received the non-surgical periodontal treatment was decreased significantly after 3 months, with a pooled mean difference of − 36.13 mmol/L (95% CI: − 53.63, − 18.62, p < 0.01). There was no significant heterogeneity between the studies (I2 = 0, p = 0.77) (Fig. 6b2). The result was robust regardless if any one study was omitted (Supplementary Fig. 5-b2).
Considering the results of other studies, with 1.70 mmol/l as the diagnostic criterion, DUAN Jinyu reported that the serum cholesterol levels in five of 15 hypertriglyceridaemia patients returned to normal after the non-surgical periodontal treatment. The observation period was 3 months [71]. This article was not included in the meta-analysis because there were no specific parameters. Zuza EP also reported similar results [77].
-
iii.
Nonsurgical periodontal treatment and HDL
Compared with the control group, the level of HDL in the serum of patients who received the non-surgical periodontal treatment was increased significantly after 3 months, with a pooled mean difference of 3.98 mmol/L (95% CI: 1.71, 6.25, p < 0.01). There was no significant heterogeneity between the studies (I2 = 0, p = 0.81) (Fig. 6c2). The result was meaningless when the study by Fu YW, 2016 was omitted (Supplementary Fig. 5-c2).
-
iv.
Nonsurgical periodontal treatment and LDL
Finally, we performed a meta-analysis of the LDL levels in serum. Analysis of these studies showed that there was no statistically significant difference in the LDL levels between the treatment and control groups after 3 months of treatment (Fig. 6d2). The result was significant when the study by Fu YW, 2016 was omitted (Supplementary Fig. 5-a).
Effect of lipid treatment on periodontitis
Five studies evaluated the difference in the association between the lipid treatment and periodontitis with the mean (SD). No significant publication bias was found after Egger’s and Begg’s tests (p > 0.05).
Compared with that of the control group, the level of GI in the dyslipidemia patients who received the lipid treatment decreased significantly, with a pooled mean difference of − 0.15 (95%-CI: − 0.25, − 0.06, p < 0.01). There was no significant heterogeneity between the studies (I2= 0, p = 0.92) (Fig. 7e).
Forest plot of mean difference for comparisons: lipid-lowering treatment versus non-treatment among hyperlipidemia patients. a lipid-lowering treatment can decrease PD; (b) lipid-lowering treatment do not significantly decrease CAL (c) lipid-lowering treatment do not significantly decrease BOP; (d) lipid-lowering treatment do not significantly decrease PI; (e) lipid-lowering treatment can decrease GI. Abbreviations: PD: probing depth, CAL: clinical attachment level, BOP: bleeding on probing, PI: plaque index, GI: gingival index
We found no statistically significant difference in PD, CAL, BOP, or PI between the treatment and control groups (Fig. 7). Through meta-regression, it was determined that the sources of the heterogeneity may be the total sample size for PD (p = 0.017), study design for CAL (p = 0.007), and age for PI (p = 0.028) (Table S7).
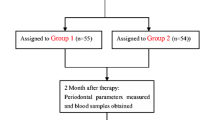
The following results are reported in related studies that are not included in the forest map. Özlem FENTOĞLU reported that 2 months after the periodontal treatment and lipid treatment, PI, GI, BOP, and PD in the statin treatment group were significantly reduced, while similar results were observed in the diet control group [57].
Discussion
Dyslipidemia is a representative metabolic disease, which is widely speculated to be the important agents that promotes periodontitis. In our study, we set out to determine whether dyslipidemia has similar effects on periodontitis as diabetes mellitus and if it reduces blood lipid levels to help treat periodontitis in patients with dyslipidemia.
Our research results are as follows: first, increasing plasma TC, TG, LDL and reduced HDL levels were risk factors for periodontitis. The periodontal parameters CAL, PD and PI of patients with dyslipidemia were significantly worse. Second, compared with that of the baseline, the plasma lipid levels of patients with dyslipidemia who completed the periodontal treatment were significantly improved after 3 months. Third, for patients with dyslipidemia, periodontal parameters except GI were not significantly improved with statins when compared with the diet control therapy. Our research has identified the association between dyslipidemia and periodontitis, we speculate that cytokines may be the key to linking the two diseases. Bacteria are the major pathogenic factors of periodontal disease. The stimulation of microbes promotes the secretion of cytokines in hosts to promote inflammation by autocrine or paracrine signalling [89]. Bacteria are very important in promoting the progression of periodontitis and the pathological manifestations of active periodontitis. For example, IL-1 and TNF-α affect the function of endothelial cells, leading to the accumulation of neutrophils and monocytes at the site of inflammation [90]. Probing depth (PD), clinical attachment loss (CAL), and bleeding on probing (BOP) are closely related to the increase in MMP levels, pathogens in dental plaque are able to stimulate host cells to increase their MMP release [91]. By means of the analysis of 10 researches, including 485 periodontitis patients and 379 healthy controls, Lin Zhang find that the salivary MMP-8 levels were significantly higher in periodontitis patients compared with healthy controls [92]. Indeed, a decrease in the levels of MMPs in the crevicular fluid has been observed after the treatment of periodontitis. This demonstrates that the levels of MMPs are in a dynamic balance with the state of hygiene and health of periodontal tissues [93, 94]. These inflammatory factors are also related to the development of dyslipidemia.
Several lines of evidence suggested that patients with dyslipidemia exhibited higher TNF-α plasma concentrations, which correlated significantly with the concentrations of VLDL, triglycerides and cholesterol and correlated negatively with HDL cholesterol [93,94,95]. The use of fenofibrate to treat hyperlipoproteinemia IIB leads to decreased levels of TC, TG, and LDL, which correlate with a decreased concentration of TNF-α [96].
Özlem Fentoğlu found significant correlations between serum and gingival crevicular fluid cytokines (IL-1β and TNF-α) and the TC/HDL ratio in patients with dyslipidemia [56]. A study showed that plasma free fatty acid and glycerol concentrations increased transiently after an injection of TNF [97].
Based on the studies above, we found that cytokines (especially TNF-α) play a critical role in the occurrence and development of periodontitis and dyslipidemia. Perhaps this is an important reason why the two diseases interact with each other. We speculate that the treatment of one disease may also affect the development of the other.
As a standard method for treating periodontitis, non-surgical periodontal treatment has been used in clinical work for a long time. Many studies have shown that after an effective periodontal treatment, the blood lipid levels in plasma are significantly improved. Research by Fu YW et al. showed that the levels of TNF-α, IL-1β, and IL-6 in the periodontal treatment group were significantly lower than those treated only with supragingival scaling [69].
As a conventional drug for the treatment of dyslipidemia, statins have been reported to inhibit the immune reactivity of inflammatory cells [98]. Lin SK found that simvastatin inhibited the effects of TNF-α in a dose-dependent manner [99]. Several studies have documented that when atorvastatin gel is placed subgingivally as an adjunct to scaling and root planning, it leads to significant periodontal regeneration [100, 101]. However, in our study, one unanticipated result was that for patients with dyslipidemia who received the systemic therapy, statins did not significantly improve periodontal parameters except GI when compared with that of the diet control therapy. The limited number of studies available may undermine the accuracy of the results.
This study indicates that there is a bi-directional correlation between dyslipidemia and chronic periodontitis. Controlling blood lipid levels may improve the effect of non-surgical periodontal treatments on periodontitis. Maintaining periodontal health is also beneficial for the conditions of lipids in dyslipidemia patients. We can also perform combined treatment when necessary.
We are aware that our study has limitations that should be considered. First, studies with invalid or negative results tend not to be published, so it is difficult to completely prevent publication bias. Second, due to the different diagnoses of periodontitis or dyslipidemia in different countries, our inclusion criteria cannot be completely unified. In this study, significant heterogeneity was found, perhaps due to the region (European/Americas or Asian), criterion of Pd diagnosis, publication year, study design, age ratio, etc., which may undermine the validity of the results. Third, regarding the effect of lipid treatments on periodontitis, the limited number of available studies limits the ability to obtain a comprehensive result.
Conclusion
Overall, we can conclude that there is a bi-direction relationship between dyslipidemia and periodontitis. Periodontal therapy can improve the condition of dyslipidemia, but we did not observe a periodontitis-improving effect when statins were systematically used.
Availability of data and materials
All data generated or analyzed during the present study are included in this published article.
Abbreviations
- TC:
-
Total Cholesterol
- TGs:
-
Triglycerides
- LDL:
-
Low-density lipoprotein
- HDL:
-
High-density lipoprotein
- GI:
-
Gingival index
- Pd:
-
Periodontal disease
- T2DM:
-
Type 2 diabetes mellitus
- IBD:
-
Inflammatory bowel disease
- PD:
-
Probing Depth
- CAL:
-
Clinical attachment level
- BOP:
-
Bleeding on probing
- PI:
-
Plaque index
- CVD:
-
Cardiovascular disease
- CPI:
-
Community periodontal index
- NOS:
-
Newcastle–Ottawa Scale
- AHRQ:
-
Agency for Healthcare Research and Quality
- MD:
-
Mean difference
- CI:
-
Confidence interval
References
Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. Lancet (London, England). 2005;366(9499):1809–20. https://doi.org/10.1016/S0140-6736(05)67728-8.
Kinane DF, Stathopoulou PG, Papapanou PN. Periodontal diseases. Nat Rev Dis Primers. 2017;3:17038. https://doi.org/10.1038/nrdp.2017.38.
GBD 2017 Oral Disorders Collaborators, Bernabe E, Marcenes W, Hernandez CR, Bailey J, Abreu LG, Alipour V, Amini S, Arabloo J, Arefi Z, Arora A, Ayanore MA, Bärnighausen TW, Bijani A, Cho DY, Chu DT, Crowe CS, Demoz GT, Demsie DG, Dibaji Forooshani ZS, et al. Global, regional, and National Levels and trends in burden of Oral conditions from 1990 to 2017: A systematic analysis for the global burden of disease 2017 study. J Dent Res. 2020;99(4):362–73. https://doi.org/10.1177/0022034520908533.
Hajishengallis G, Chavakis T. Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities. Nat Rev Immunol. 2021;21(7):426–40. https://doi.org/10.1038/s41577-020-00488-6.
Leite F, Nascimento GG, Scheutz F, López R. Effect of smoking on periodontitis: A systematic review and Meta-regression. Am J Prev Med. 2018;54(6):831–41. https://doi.org/10.1016/j.amepre.2018.02.014.
Preshaw PM, Alba AL, Herrera D, Jepsen S, Konstantinidis A, Makrilakis K, Taylor R. Periodontitis and diabetes: a two-way relationship. Diabetologia. 2012;55(1):21–31. https://doi.org/10.1007/s00125-011-2342-y.
Xu S, Zhang G, Guo JF, Tan YH. Associations between osteoporosis and risk of periodontitis: A pooled analysis of observational studies. Oral Dis. 2021;27(2):357–69. https://doi.org/10.1111/odi.13531.
Pirillo A, Casula M, Olmastroni E, Norata GD, Catapano AL. Global epidemiology of dyslipidaemias. Nat Rev Cardiol. 2021;18(10):689–700. https://doi.org/10.1038/s41569-021-00541-4.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clin Res ed). 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods Group, Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clin Res ed). 2011;343:d5928. https://doi.org/10.1136/bmj.d5928.
Al-Otaibi DH, Babay NA, Habib SS, Almas K. Assessment of lipid profile in Saudi type 2 diabetic and non-diabetic periodontal patients. Saudi Med J. 2008;29(5):723–7.
Akkaloori A, Parthasarathi P, Anjum MS, Gadde P, Mocherla M, Rao Y. Association between chronic periodontal disease and cardiovascular risk factor hyperlipidemia. J Dr Ntr Univ Health Sci. 2014; https://doi.org/10.4103/2277-8632.146628.
Banihashemrad SA, Moeintaghavi A, Rafighdoost A. Relationship between cholesterol and triglyceride blood values and periodontal parameters in patients of Mashhad health center. New York State Dent J. 2008;74(5):65–6.
Bullon P, Jaramillo R, Santos-Garcia R, Rios-Santos V, Ramirez M, Fernandez-Palacin A, Fernandez-Riejos P. Relation of periodontitis and metabolic syndrome with gestational glucose metabolism disorder. J Periodontol. 2014;85(2):e1–8. https://doi.org/10.1902/jop.2013.130319.
Cury EZ, Santos VR, Maciel S, Gonçalves T, Zimmermann GS, Mota R, Figueiredo LC, Duarte PM. Lipid parameters in obese and normal weight patients with or without chronic periodontitis. Clin Oral Investig. 2018;22(1):161–7. https://doi.org/10.1007/s00784-017-2095-1.
Iacopino AM, Cutler CW. Pathophysiological relationships between periodontitis and systemic disease: recent concepts involving serum lipids. J Periodontol. 2000;71(8):1375–84. https://doi.org/10.1902/jop.2000.71.8.1375.
Doraiswamy S, Yen VA. The plasma lipid level in periodontal health and disease- a case-control study. J Evol Med Dent Sci. 2017;6(48):3728–30. https://doi.org/10.14260/Jemds/2017/804.
Fentoğlu Ö, Tözüm Bulut M, Doğan B, Kırzıoğlu FY, Kemer Doğan ES. Is the relationship between periodontitis and hyperlipidemia mediated by lipoprotein-associated inflammatory mediators? J Periodontal Implant Sci. 2020;50(3):135–45. https://doi.org/10.5051/jpis.2020.50.3.135.
Golpasand H, Tian Y, Meng H, Hou J, Xu L, Zhang L, Shi D, Lu R, Feng X, Wang X, Chen Z. Associations of apolipoprotein E and low-density lipoprotein receptor-related protein 5 polymorphisms with dyslipidemia and generalized aggressive periodontitis in a Chinese population. J Periodontal Res. 2015;50(4):509–18. https://doi.org/10.1111/jre.12237.
Golpasand Hagh L, Zakavi F, Hajizadeh F, Saleki M. The association between hyperlipidemia and periodontal infection. Iran Red Crescent Med J. 2014;16(12):e6577. https://doi.org/10.5812/ircmj.6577.
Güler B, Doan E, Onba K. The relationship between monocyte count to high-density lipoprotein ratio and severity of inflammation in aggressive periodontitis: a retrospective analysis. Meandros Med Dent J. 2020;21(2):122–7. https://doi.org/10.4274/meandros.galenos.2020.41033.
Hamissi J, Shahsavarani MT, Hamissi H. A comparison of serum lipid profile between periodontitis patients and healthy individuals. Iran Red Crescent Med J. 2011;13(4):283–4. https://doi.org/10.5681/jpid.2010.005.
Han SJ, Yi YJ. The association between dyslipidemia, oral health behavior, and periodontal disease: The Korea National Health and Nutrition Examination Survey. Quintessence Int (Berlin, Germany : 1985). 2019;50(5):394–401. https://doi.org/10.3290/j.qi.a42294.
Kalburgi V, Leburu S, Warad S. Saliva as a surrogate to explore the association between lipid profiles and chronic periodontitis: A case-control study. Dent Res J. 2014;11(6):619–23.
Kim SR, Nam SH. Association between periodontal disease and levels of triglyceride and Total cholesterol among Korean adults. Healthcare (Basel, Switzerland). 2020;8(3):337. https://doi.org/10.3390/healthcare8030337.
Koshy BS, Mahendra J. The association between periodontal status, serum lipid levels, lipoprotein associated Phosholipase A2 (Lp-PLA2) in chronic periodontitis subjects and healthy controls. J Clin Diagnostic Res : JCDR. 2017;11(9):ZC17–21. https://doi.org/10.7860/JCDR/2017/27628.10565.
Kumar KR, Ranganath V, Naik R, Banu S, Nichani AS. Assessment of high-sensitivity C-reactive protein and lipid levels in healthy adults and patients with coronary artery disease, with and without periodontitis--a cross-sectional study. J Periodontal Res. 2014;49(6):836–44. https://doi.org/10.1111/jre.12172.
Kushiyama M, Shimazaki Y, Yamashita Y. Relationship between metabolic syndrome and periodontal disease in Japanese adults. J Periodontol. 2009;80(10):1610–5. https://doi.org/10.1902/jop.2009.090218.
Lee JB, Yi HY, Bae KH. The association between periodontitis and dyslipidemia based on the fourth Korea National Health and nutrition examination survey. J Clin Periodontol. 2013;40(5):437–42. https://doi.org/10.1111/jcpe.12095.
Lee S, Im A, Burm E, Ha M. Association between periodontitis and blood lipid levels in a Korean population. J Periodontol. 2018;89(1):28–35. https://doi.org/10.1902/jop.2017.170111.
Lösche W, Karapetow F, Pohl A, Pohl C, Kocher T. Plasma lipid and blood glucose levels in patients with destructive periodontal disease. J Clin Periodontol. 2000;27(8):537–41. https://doi.org/10.1034/j.1600-051x.2000.027008537.x.
Machado AC, Quirino MR, Nascimento LF. Relation between chronic periodontal disease and plasmatic levels of triglycerides, total cholesterol and fractions. Braz Oral Res. 2005;19(4):284–9. https://doi.org/10.1590/s1806-83242005000400009.
Moeintaghavi A, Haerian-Ardakani A, Talebi-Ardakani M, Tabatabaie I. Hyperlipidemia in patients with periodontitis. J Contemp Dent Pract. 2005;6(3):78–85.
Moghaddam SA, Abbasi S, Moghaddam ES, Moghaddam AA. Triglyceride and cholesterol levels in patients with chronic periodontitis. 2015. https://doi.org/10.17795/jhealthscope-19928.
Monteiro AM, Jardini MA, Alves S, Giampaoli V, Aubin EC, Figueiredo Neto AM, Gidlund M. Cardiovascular disease parameters in periodontitis. J Periodontol. 2009;80(3):378–88. https://doi.org/10.1902/jop.2009.080431.
Nibali L, D’Aiuto F, Griffiths G, Patel K, Suvan J, Tonetti MS. Severe periodontitis is associated with systemic inflammation and a dysmetabolic status: a case-control study. J Clin Periodontol. 2007;34(11):931–7. https://doi.org/10.1111/j.1600-051X.2007.01133.x.
Penumarthy S, Penmetsa GS, Mannem S. Assessment of serum levels of triglycerides, total cholesterol, high-density lipoprotein cholesterol, and low-density lipoprotein cholesterol in periodontitis patients. J Indian Soc Periodontol. 2013;17(1):30–5. https://doi.org/10.4103/0972-124X.107471.
Sandi RM, Pol KG, Basavaraj P, Khuller N, Singh S. Association of Serum Cholesterol, triglyceride, high and low density lipoprotein (HDL and LDL) levels in chronic periodontitis subjects with risk for cardiovascular disease (CVD): A cross sectional study. J Clin Diagnostic Res: JCDR. 2014;8(1):214–6. https://doi.org/10.7860/JCDR/2014/6686.3927.
Saxlin T, Suominen-Taipale L, Kattainen A, Marniemi J, Knuuttila M, Ylöstalo P. Association between serum lipid levels and periodontal infection. J Clin Periodontol. 2008;35(12):1040–7. https://doi.org/10.1111/j.1600-051X.2008.01331.x.
Shi D, Meng HX, Xu L, Zhang L, Chen ZB, Feng XH. Zhonghua kou qiang yi xue za zhi = Zhonghua kouqiang yixue zazhi. Chin J Stomatol. 2006;41(7):401–2.
Shimazaki Y, Saito T, Yonemoto K, Kiyohara Y, Iida M, Yamashita Y. Relationship of metabolic syndrome to periodontal disease in Japanese women: the Hisayama study. J Dent Res. 2007;86(3):271–5. https://doi.org/10.1177/154405910708600314.
Sridhar R, Byakod G, Pudakalkatti P, Patil R. A study to evaluate the relationship between periodontitis, cardiovascular disease and serum lipid levels. Int J Dent Hyg. 2009;7(2):144–50. https://doi.org/10.1111/j.1601-5037.2008.00318.x.
Taleghani F, Shamaei M, Shamaei M. Association between chronic periodontitis and serum lipid levels. Acta Med Iran. 2010;48(1):47–50. https://doi.org/10.2298/VSP1209771P.
Thapa S, Wei F. Association between high serum Total cholesterol and periodontitis: National Health and nutrition examination survey 2011 to 2012 study of American adults. J Periodontol. 2016;87(11):1286–94. https://doi.org/10.1902/jop.2016.150648.
Thomas B, Prasad RB, Shetty S, Vishakh R. Comparative evaluation of the lipid profile in the serum of patients with type II diabetes mellitus and healthy individuals with periodontitis. Contemp Clin Dent. 2017;8(1):96–101. https://doi.org/10.4103/ccd.ccd_1160_16.
Wang Y, Zhong-Rong WU, Shang SH, Dong WL, Zhong-Qin LI, Hua LI, et al. The investigation of the correlation between serum lipid and periodontitis in officeholders of Wuhan. Chin J Conserv Dent. 2007; https://doi.org/10.1016/j.jaci.2004.04.006.
Zhou SY, Xiao WM, Ouyang XY. Lipoprotein-associated phospholipase A2 and serum lipid levels in subjects with chronic periodontitis and hyperlipidemia. Chin J Dent Res : Off J Sci Sec Chin Stomatol Assoc (CSA). 2012;15(1):25–9.
Guan X, Wang X, Li Y, Xu J, He L, Xu L, Xu X, Meng H. Glucose and lipid metabolism indexes and blood inflammatory biomarkers of patients with severe periodontitis: A cross-sectional study. J Periodontol. 2023;94(4):554–63. https://doi.org/10.1002/JPER.22-0282.
Zhang F, Zhao D, Xu X, Wen P, Li H, Yu R, Cheng T, Zheng Z, Yang H, Yang C, Yao J, Jin L. Periodontitis links to concurrent metabolic disorders and abnormal liver function in pregnant women. Oral Dis. 2022; https://doi.org/10.1111/odi.14364. Advance online publication.
Chen C, Zhu J, Deng X, Yang Z, Lin W, Ma Y, Huang S, Chen L, Liu Y, Zhu F. Severe periodontitis is associated with the serum levels of hypersensitive C reactive protein and lipoprotein-associated phospholipase A2 in the patients of acute ischemic stroke. J Clin Neurosci : Off J Neurosurg Soc Australasia. 2021;88:232–6. https://doi.org/10.1016/j.jocn.2021.04.007.
Almeida Abdo J, Cirano FR, Casati MZ, Ribeiro FV, Giampaoli V, Casarin R, Pimentel SP. Influence of dyslipidemia and diabetes mellitus on chronic periodontal disease. J Periodontol. 2013;84(10):1401–8. https://doi.org/10.1902/jop.2012.120366.
Awartani F, Atassi F. Evaluation of periodontal status in subjects with hyperlipidemia. J Contemp Dent Pract. 2010;11(2):033–40. https://doi.org/10.5005/jcdp-11-2-33.
D’Aiuto F, Sabbah W, Netuveli G, Donos N, Hingorani AD, Deanfield J, Tsakos G. Association of the metabolic syndrome with severe periodontitis in a large U.S. population-based survey. J Clin Endocrinol Metab. 2008;93(10):3989–94. https://doi.org/10.1210/jc.2007-2522.
Doğan B, Fentoğlu Ö, Kırzıoğlu FY, Kemer ES, Köroğlu BK, Aksu O, Çarsancaklı SA, Orhan H. Lipoxin A4 and neutrophil/lymphocyte ratio: A possible Indicator in achieved systemic risk factors for periodontitis. Med Sci Monit : Int Med J Exp Clin Res. 2015;21:2485–93. https://doi.org/10.12659/MSM.895115.
Fentoğlu O, Oz G, Taşdelen P, Uskun E, Aykaç Y, Bozkurt FY. Periodontal status in subjects with hyperlipidemia. J Periodontol. 2009;80(2):267–73. https://doi.org/10.1902/jop.2009.080104.
Fentoğlu Ö, Köroğlu BK, Hiçyılmaz H, Sert T, Özdem M, Sütçü R, Tamer MN, Orhan H, Ay ZY, Öztürk Tonguç M, Kırzıoğlu FY. Pro-inflammatory cytokine levels in association between periodontal disease and hyperlipidaemia. J Clin Periodontol. 2011;38(1):8–16. https://doi.org/10.1111/j.1600-051X.2010.01644.x.
Fentoğlu Ö, Kırzıoğlu FY, Bulut MT, Kumbul Doğuç D, Kulaç E, Önder C, Günhan M. Evaluation of lipid peroxidation and oxidative DNA damage in patients with periodontitis and hyperlipidemia. J Periodontol. 2015;86(5):682–8. https://doi.org/10.1902/jop.2015.140561.
Fukui N, Shimazaki Y, Shinagawa T, Yamashita Y. Periodontal status and metabolic syndrome in middle-aged Japanese. J Periodontol. 2012;83(11):1363–71. https://doi.org/10.1902/jop.2012.110605.
Katz J, Flugelman MY, Goldberg A, Heft M. Association between periodontal pockets and elevated cholesterol and low density lipoprotein cholesterol levels. J Periodontol. 2002;73(5):494–500. https://doi.org/10.1902/jop.2002.73.5.494.
Kemer Doğan ES, Kırzıoğlu FY, Doğan B, Fentoğlu Ö, Kale B. The effect of menopause on the relationship between hyperlipidemia and periodontal disease via salivary 8-hydroxy-2′-deoxyguanosine and myeloperoxidase levels. Acta Odontol Scand. 2018;76(2):92–7. https://doi.org/10.1080/00016357.2017.1386798.
Lutfioğlu M, Aydoğdu A, Atabay VE, Sakallioğlu EE, Avci B. Gingival crevicular fluid oxidative stress level in patients with periodontal disease and hyperlipidemia. Braz Oral Res. 2017;31:e110. https://doi.org/10.1590/1807-3107bor-2017.vol31.0110.
Scardina GA, Pisano T, Cacioppo A, Messina P. Periodontal alteration of the microcirculation and hypercholesterolemia: a possible correlation? South Med J. 2011;104(2):116–20. https://doi.org/10.1097/SMJ.0b013e318205ddf1.
Shivakumar T, Patil VA, Desai MH. Periodontal status in subjects with hyperlipidemia and determination of association between hyperlipidemia and periodontal health: a clinicobiochemical study. J Contemp Dent Pract. 2013;14(5):785–9. https://doi.org/10.5005/jp-journals-10024-1403.
Yu ZR, Liu LS, Luan QX, Wang XY, Li P, Sha YQ, Liu X. Beijing da xue xue bao. Yi xue ban = J Peking Univ Health Sci. 2012;44(4):633–8.
Zhu H, Ye G, Xie Y, Zhu K, Zhu F, Chen Q. Association of high-density lipoprotein cholesterol and periodontitis severity in Chinese elderly: a cross-sectional study. Clin Oral Investig. 2022;26(7):4753–9. https://doi.org/10.1007/s00784-022-04439-4.
Jung Y, Kim JH, Shin AR, Song KB, Amano A, Choi YH. Association of Adiposity with periodontitis and metabolic syndrome: from the third National Health and nutrition examination survey of United States. Int J Environ Res Public Health. 2023;20(3):2533. https://doi.org/10.3390/ijerph20032533.
Duan JY, Ou-Yang XY, Zhou YX. Beijing da xue xue bao. Yi xue ban = J Peking Univ Health Sci. 2009;41(1):36–9.
Fentoğlu O, Sözen T, Oz SG, Kale B, Sönmez Y, Tonguç MO, Gürgan CA, Aykaç Y, Kirzioğlu FY. Short-term effects of periodontal therapy as an adjunct to anti-lipemic treatment. Oral Dis. 2010;16(7):648–54. https://doi.org/10.1111/j.1601-0825.2010.01668.x.
Fu YW, Li XX, Xu HZ, Gong YQ, Yang Y. Effects of periodontal therapy on serum lipid profile and proinflammatory cytokines in patients with hyperlipidemia: a randomized controlled trial. Clin Oral Investig. 2016;20(6):1263–9. https://doi.org/10.1007/s00784-015-1621-2.
Lösche W, Marshal GJ, Apatzidou DA, Krause S, Kocher T, Kinane DF. Lipoprotein-associated phospholipase A2 and plasma lipids in patients with destructive periodontal disease. J Clin Periodontol. 2005;32(6):640–4. https://doi.org/10.1111/j.1600-051X.2005.00725.x.
Surdumacovei, A., Rudnic, I., Martu, I., Solomon, S., Pasarin, L., & Martu, S. (2013). Studies regarding the bidirectional relationship between the periodontal disease and hyperlipidaemia.
Nassar PO, Walker CS, Salvador CS, Felipetti FA, Orrico SR, Nassar CA. Lipid profile of people with diabetes mellitus type 2 and periodontal disease. Diabetes Res Clin Pract. 2012;96(1):35–9. https://doi.org/10.1016/j.diabres.2011.11.017.
Nibali L, Rizzo M, Li Volti G, D’Aiuto F, Giglio RV, Barbagallo I, Pelekos G, Donos N. Lipid subclasses profiles and oxidative stress in aggressive periodontitis before and after treatment. J Periodontal Res. 2015;50(6):890–6. https://doi.org/10.1111/jre.12283.
Nicolaiciuc, O. , IG Ursărescu, I Mârţu, L Păsărin, Zaharescu, A. M. , & Luchian, I. , et al. Study on the Effects of Classical Periodontal Therapy on the Lipid Profile in Hyperlipidemic and Chronic Periodontitis Patients.
Oz SG, Fentoglu O, Kilicarslan A, Guven GS, Tanrtover MD, Aykac Y, Sozen T. Beneficial effects of periodontal treatment on metabolic control of hypercholesterolemia. South Med J. 2007;100(7):686–91. https://doi.org/10.1097/SMJ.0b013e31802fa327.
Tawfig A. Effects of non-surgical periodontal therapy on serum lipids and C-reactive protein among hyperlipidemic patients with chronic periodontitis. J Int Soc Prev Community Dent. 2015;5(Suppl 1):S49–56. https://doi.org/10.4103/2231-0762.156524.
Zuza EP, Barroso EM, Fabricio M, Carrareto AL, Toledo BE, Pires R, J. Lipid profile and high-sensitivity C-reactive protein levels in obese and non-obese subjects undergoing non-surgical periodontal therapy. J Oral Sci. 2016;58(3):423–30. https://doi.org/10.2334/josnusd.16-0173.
Kolte AP, Kolte RA, Bawankar PV, Bajaj VA. Assessment and correlation of the influence of non-surgical periodontal therapy on serum lipid profile and cytokines in patients with stage III periodontitis. Int J Dent Hyg. 2023;21(2):298–304. https://doi.org/10.1111/idh.12639.
Fentoğlu Ö, Kirzioğlu FY, Tözüm Bulut M, Kurgan Ş, Koçak H, Sütcü R, Kale Köroğlu B, Günhan M. Serum Lp-PLA2: as a novel viewpoint in periodontal treatment of hyperlipidaemics. Turk J Med Sci. 2015;45(3):619–26. https://doi.org/10.3906/sag-1406-75.
Sangwan A, Tewari S, Singh H, Sharma RK, Narula SC. Periodontal status and hyperlipidemia: statin users versus non-users. J Periodontol. 2013;84(1):3–12. https://doi.org/10.1902/jop.2012.110756.
Sangwan A, Tewari S, Singh H, Sharma RK, Narula SC. Effect of hyperlipidemia on response to nonsurgical periodontal therapy: statin users versus nonusers. Eur J Dentist. 2016;10(1):69–76. https://doi.org/10.4103/1305-7456.175685.
Sayar F, Fallah S, Akhondi N, Jamshidi S. Association of serum lipid indices and statin consumption with periodontal status. Oral Dis. 2016;22(8):775–80. https://doi.org/10.1111/odi.12545.
Sayar F, Akhondi N, Fallah S, Moalemnia AA, Cheraghi A. Association of Serum Triglyceride Level and Gemfibrozil Consumption with Periodontal Status. J Periodontol. 2017;88(5):457–63. https://doi.org/10.1902/jop.2016.160366.
Hu J, Dong Y, Chen X, Liu Y, Ma D, Liu X, Zheng R, Mao X, Chen T, He W. Prevalence of suicide attempts among Chinese adolescents: A meta-analysis of cross-sectional studies. Compr Psychiatry. 2015;61:78–89. https://doi.org/10.1016/j.comppsych.2015.05.001.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88. https://doi.org/10.1016/0197-2456(86)90046-2.
Li B, Lu Y, Wang L, Zhang CX. Folate intake and breast cancer prognosis: a meta-analysis of prospective observational studies. Eur J Cancer Prevention : Off J Eur Cancer Prevention Org (ECP). 2015;24(2):113–21. https://doi.org/10.1097/CEJ.0000000000000028.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ (Clin Res ed). 2003;327(7414):557–60. https://doi.org/10.1136/bmj.327.7414.557.
Patsopoulos NA, Evangelou E, Ioannidis JP. Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int J Epidemiol. 2008;37(5):1148–57. https://doi.org/10.1093/ije/dyn065.
Birkedal-Hansen H. Role of cytokines and inflammatory mediators in tissue destruction. J Periodontal Res. 1993;28(6 Pt 2):500–10. https://doi.org/10.1111/j.1600-0765.1993.tb02113.x.
Page RC. The role of inflammatory mediators in the pathogenesis of periodontal disease. J Periodontal Res. 1991;26(3 Pt 2):230–42. https://doi.org/10.1111/j.1600-0765.1991.tb01649.x.
Franco C, Patricia HR, Timo S, Claudia B, Marcela H. Matrix metalloproteinases as regulators of periodontal inflammation. Int J Mol Sci. 2017;18(2):440. https://doi.org/10.3390/ijms18020440.
Zhang L, Li X, Yan H, Huang L. Salivary matrix metalloproteinase (MMP)-8 as a biomarker for periodontitis: A PRISMA-compliant systematic review and meta-analysis. Medicine. 2018;97(3):e9642. https://doi.org/10.1097/MD.0000000000009642.
Luchian I, Goriuc A, Sandu D, Covasa M. The Role of Matrix Metalloproteinases (MMP-8, MMP-9, MMP-13) in Periodontal and Peri-Implant Pathological Processes. Int J Mol Sci. 2022;23(3):1806. https://doi.org/10.3390/ijms23031806.
Chen X, Xun K, Chen L, Wang Y. TNF-alpha, a potent lipid metabolism regulator. Cell Biochem Funct. 2009;27(7):407–16. https://doi.org/10.1002/cbf.1596.
Jovinge S, Hamsten A, Tornvall P, Proudler A, Båvenholm P, Ericsson CG, Godsland I, de Faire U, Nilsson J. Evidence for a role of tumor necrosis factor alpha in disturbances of triglyceride and glucose metabolism predisposing to coronary heart disease. Metab Clin Exp. 1998;47(1):113–8. https://doi.org/10.1016/s0026-0495(98)90203-7.
Madej A, Okopień B, Kowalski J, Zieliński M, Wysocki J, Szyguła B, Kalina Z, Herman Z. Stezenia czynnika martwicy nowotworów alfa w surowicy pacjentów z hiperlipoproteinemia IIb przed i po podjeciu teràpii fenofibratem mikronizowanym [levels of tumor necrosis factor alpha in serum of patients with hyperlipoproteinemia IIB before and after micronized fenofibrate therapy]. Polskie Arch Med Wewnetrznej. 1998;99(4):308–13.
Van der Poll T, Romijn JA, Endert E, Borm JJ, Büller HR, Sauerwein HP. Tumor necrosis factor mimics the metabolic response to acute infection in healthy humans. Am J Phys. 1991;261(4 Pt 1):E457–65. https://doi.org/10.1152/ajpendo.1991.261.4.E457.
Kajimoto K, Miyauchi K, Kasai T, Shimada K, Kojima Y, Shimada A, Niinami H, Amano A, Daida H. Short-term 20-mg atorvastatin therapy reduces key inflammatory factors including c-Jun N-terminal kinase and dendritic cells and matrix metalloproteinase expression in human abdominal aortic aneurysmal wall. Atherosclerosis. 2009;206(2):505–11. https://doi.org/10.1016/j.atherosclerosis.2009.03.028.
Lin SK, Kok SH, Lee YL, Hou KL, Lin YT, Chen MH, Wang CC, Hong CY. Simvastatin as a novel strategy to alleviate periapical lesions. J Endod. 2009;35(5):657–62. https://doi.org/10.1016/j.joen.2009.02.004.
Shirke PY, Kolte AP, Kolte RA, Bawanakar PV. Evaluation of the clinical efficacy of 1.2% atorvastatin in the treatment of periodontal intraosseous defects by CBCT: A randomized controlled clinical trial. J Dent Res, Dent Clin, Dent Prospects. 2019;13(3):183–91. https://doi.org/10.15171/joddd.2019.029.
Pradeep AR, Kumari M, Rao NS, Martande SS, Naik SB. Clinical efficacy of subgingivally delivered 1.2% atorvastatin in chronic periodontitis: a randomized controlled clinical trial. J Periodontol. 2013;84(7):871–9. https://doi.org/10.1902/jop.2012.120393.
Acknowledgements
Not applicable.
Funding
This article was supported by National Natural Science Foundations of China (No. 82101017, 81972532); Guangdong Basic and Applied Basic Research Foundation (2020A1515110741).
Author information
Authors and Affiliations
Contributions
MWT, ZZL, LB and WZ designed the study. MWT, ZZL, LB and FJ extracted, analyzed, and interpreted the data. MWT drafted the manuscript. ZZL, YLS, LDJ and SZY review the manuscript. GJY and HQN revised the manuscript. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ma, W., Zou, Z., Yang, L. et al. Exploring the bi-directional relationship between periodontitis and dyslipidemia: a comprehensive systematic review and meta-analysis. BMC Oral Health 24, 508 (2024). https://doi.org/10.1186/s12903-023-03668-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-023-03668-7