Abstract
Background
The aim of this study was to investigate the characteristics and clinical outcomes of patients with nonsmoking small cell lung cancer (SCLC) using a nationwide registry in Korea.
Methods
The Korean Association for Lung Cancer developed a registry in cooperation with the Korean Central Cancer Registry (KCCR) and surveyed approximately 10% of recorded lung cancer cases.
Results
From 2014 to 2016, the KCCR registered 1,043 patients newly diagnosed with SCLC among a total of 8,110 lung cancer patients. In subgroup analysis, Kaplan meier survival analysis showed that the overall survival (OS) was significantly shorter in the nonsmoking subgroup than the ever-smoking subgroup of SCLC patients with extensive disease (6.99 vs. 9.68 months; P = 0.016). Among SCLC patients with limited disease, OS was also shorter in the nonsmoking subgroup, without statistical significance (19.4 vs. 23.5 months; P = 0.247). In a multivariate analysis using a Cox regression model, never smoking was not associated with shorter OS, but older age, extensive stage, poor performance status (Eastern Cooperative Oncology Group grade ≥ 2), male sex, no prophylactic cranial irradiation, and no active treatment (chemotherapy and/or radiotherapy) were associated with poor prognosis.
Conclusion
This evaluation of an unbiased nationwide survey dataset revealed that a significant proportion of Korean SCLC patients were never-smokers. No history of smoking appeared to be a significant prognostic factor according to the univariate analysis but was confirmed to be statistically insignificant through a multivariate analysis of the total population. Reasons for a poor prognosis may include the possibility that a high rate of the elderly population is composed of nonsmokers who did not receive active treatment.
Similar content being viewed by others
Background
Small cell lung cancer (SCLC) accounts for 10% to 15% of all lung cancers, although the incidence of SCLC has been declining with the decreasing prevalence of smoking [1]. SCLC is an aggressive malignancy with a short doubling time, high fraction ratio, and early development of distant metastasis [2]. SCLC is commonly viewed as a smoker’s disease and is very rare in those who have never been smokers [3]. In fact, nonsmoking-related SCLC may be a disease entity that is distinct from smoking-related SCLC. Recent research has found that significant differences exist regarding age distribution, sex, race, and mutational profiles between smokers and never-smokers with SCLC [4, 5]. Previous studies of prognosis have reported conflicting results, with some showing better survival among patients with SCLC who were never-smokers [3, 4, 6, 7], whereas others have reported no differences in survival [5].
To date, existing published data on SCLC in never-smokers largely originate from single-institution, retrospective studies [8,9,10]. Given the rarity of cases, a large, population-based study to investigate nonsmoking-related SCLC is warranted. We used the Korean Association for Lung Cancer (KALC) Registry (KALC-R), a nationwide unbiased registry developed by the KALC in cooperation with the Korean Central Cancer Registry (KCCR), and included about 10% of all lung cases in Korea [11].
In the present study, we retrospectively analyzed the clinical features and treatment strategies of nonsmoking SCLC patients and compared their clinical outcomes with those of smoking-related SCLC. Further, we identified independent predictors of survival among patients with SCLC. Stratifying SCLC subgroups based on smoking history may lead to treatment advances in managing this historically “recalcitrant” cancer.
Materials and methods
Study population and methods
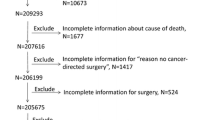
Our study used data from the KALC-R, a database created using a retrospective sampling survey by the KCCR and the Lung Cancer Registration Committee [11]. Data from 13 regional cancer centers and 39 hospitals in Korea are included in this database, with the sample size of each hospital determined by the probability of selection according to the number of registrations. Patients were stratified by the date of diagnosis; sex; age; and their Surveillance, Epidemiology, and End Results program summary stage. Excluding multiple primary cancer patients, 2,621 patients in 2014, 2,660 patients in 2015, and 2,829 patients in 2016 were selected from the 52 centers through systematic sampling methods [12]. Of the total 8,110 patients registered between 2014 and 2016, those with no survival data and no smoking history were excluded, and 1,043 SCLC patients were selected. Finally, 154 never-smoker SCLC patients and 889 ever-smoker SCLC patients were compared and their data were analyzed to investigate differences between their clinical characteristics, treatment modalities, and clinical outcomes.
Based on a standardized protocol, the data of age, sex, body mass index (BMI), smoking history, symptoms, results of radiologic findings, Eastern Corporative Oncology Group (ECOG) performance status (PS) at the time of diagnosis, clinical stage, treatment modalities, and survival status were collected. The registered patients were followed until December 31, 2018 [12].
Statistical analysis
Continuous variables are expressed as mean ± standard deviation or median (range) values and categorical variables are expressed as percentages. Continuous variables were compared using the Mann–Whitney U test, and categorical variables were compared using the chi-squared test. Risk factors for mortality were analyzed using Cox proportional hazards models. Survival was analyzed by the Kaplan–Meier method and compared by log-rank tests. All p-values were two-tailed, with statistical significance set at p < 0.05. All statistical analyses were performed using the Statistical Package for the Social Sciences version 20.0 (IBM Corp., Armonk, NY, USA).
Results
Prevalence of nonsmoking SCLC and patient characteristics by smoking history
The proportion of nonsmoking SCLC was steadily reduced from 2014 to 2016 (16.6% in 2014, 15.0% in 2015, and 12.7% in 2016) without statistically significance (P = 0.722) (Fig. 1). The median age of all study participants was 71 years. Never-smoking SCLC was more prevalent in women than in men (50.6% vs. 7.0%; P < 0.001). The proportion of extensive disease according to PS displayed a higher trend in the nonsmoking subgroup even though there was no statistically significant significance between those with and without a smoking history. Meanwhile, the proportions of receiving chemotherapy and treatment completeness were lower in the nonsmoking subgroup. The proportion of receiving best supportive care was not different between the two subgroups, but the receipt of local therapy only without chemotherapy was higher in the nonsmoking group (Table 1).
The total number of cycles of initial chemotherapy was not different between the two groups, and there was no differences in regimen of initial chemotherapy between two groups (Table 2).
At the diagnosis of SCLC, the proportion of patients with one or more symptoms was not different between the two groups, but those with hemoptysis (P = 0.063) or weight loss (P = 0.023) were less common in the never-smoker group. Radiologic findings such as mass diameter and structural invasion were similar, with the exception of recurrent laryngeal nerve invasion (Table 3).
Prognostic factors and survival analysis
Overall survival (OS) was significantly shorter in the nonsmoking SCLC subgroup (11.03 vs. 15.15 vs. 14.30 months; P < 0.01) than in the current and ex-smoker subgroups. During subgroup analysis, OS was found to be shorter in the nonsmoking subgroup than in the ever-smoking subgroup of extensive-disease (ED)-SCLC patients (6.99 vs. 9.68 months; P = 0.016), but the OS was not different between the nonsmoking and ever-smoking subgroups among limited-disease (LD)-SCLC patients (19.4 vs. 23.5 months; P = 0.247) (Fig. 2).
In a multivariate analysis using a Cox regression model, never smoking was not associated with OS, but older age, extensive stage, poor PS (ECOG grade ≥ 2), male sex, no prophylactic cranial irradiation (PCI), and no active treatment (chemotherapy and/or radiotherapy) were associated with poor prognosis (Table 4).
We further performed subgroup analysis according to disease status. In the subgroup analysis of LD-SCLC, never smoking was significantly associated with poor OS after adjusting confounding factors. Also, symptoms observed at diagnosis were independently associated with poor prognosis, while treatment of PCI or chemotherapy was independently associated with favorable prognosis. In ED-SCLC patients, older age, poor PS, and brain or liver metastasis were independently associated with poor prognosis, but smoking status was not associated with clinical outcomes (Table 5).
Discussion
Our study indicated that never-smokers are prevalent in SCLC in Korea. During the study period, the prevalence of never-smoking SCLC was steadily reduced, without statistical significance. The proportions of female sex and elderly age were significantly higher in the never-smoking SCLC group. We also found that ever-smokers were more likely to receive chemotherapy and/or radiotherapy, while never-smokers were more likely to receive radiotherapy only. The proportions of ED-SCLC and poor PS exhibited a higher trend among never-smokers even though there was no statistical significance. Clinical symptoms such as hemoptysis or weight loss were more frequently demonstrated in the ever-smoker group than the never-smoker group. In Kaplan Meier survival analysis, never-smoking SCLC patients had significantly shorter OS periods relative to ever-smokers in both the total study population and ED-SCLC subgroup. However, never smoking was significantly associated with poor OS in LD-SCLC but not in ED-SCLC patients after adjusting confounding factors. Meanwhile, older age, ED, poor PS, male sex, and not receiving PCI or active treatment such as chemotherapy and/or radiotherapy were significantly associated with a shorter OS in the total population.
In our study, the prevalence of nonsmoking SCLC was 14.8%, which is higher than that reported in non-Asian countries and contradicts the traditional belief that SCLC is a smoker’s disease. The prevalence of never-smoker SCLC was reported to be only 2.5% to 3.4% in non-Asian countries [3, 13]. In contrast, some studies carried out in Asia revealed a greater incidence of cases. In Chinese populations, the proportion of never-smoking SCLC was 22.8%, which is higher than our results [6]. Our findings are in line with those of a previous independent study reporting a high prevalence (about 13.0%) of never-smokers among SCLC patients in Korea [7, 14]. The high proportion of never-smokers among Asian lung cancer patients could not be explained exactly but is suggested to be attributed to ethnic differences. Also, secondhand smoking status, occupational carcinogen exposure, and other important risk factors involved in carcinogenesis could not be analyzed in our study [15]. Finally, the proportion of elderly patients was higher in the never-smoker subgroup in our study. The average annual growth in the aging rate in Korea is 3.3%, which is the fastest rate among 37 OECD countries. Korea has had an aging society since 2000 and is expected to demonstrate an ultra-aged society in 2026 [16]. Lung cancer is an aging-related disease, and nonsmoking SCLC is thought to occur in the elderly by accumulating exposure to other environmental factors, regardless of smoking, in an aging society [17].
Previous studies of prognosis have reported conflicting results. Some studies demonstrated that never-smokers with SCLC had a better prognosis than that of smokers with SCLC [3, 4, 6, 7]. Researchers hypothesized that this phenomenon may be partly attributed to the fact that never-smokers have fewer comorbidities and can better tolerate the treatment [18]. Other studies have reported no survival differences between nonsmoking and smoking SCLC patients [5]. In our study, never smoking appeared to be a significantly poor prognostic factor according to the univariate analysis but was confirmed to be statistically insignificant through a multivariate analysis of the total population. However, nonsmoking SCLC had a significantly poor prognosis relative to smoking SCLC in LD patients in the multivariate analysis. Contrary to as predicted by nonsmoking, the reasons for a poor prognosis may include the possibility of a high number of elderly patients among nonsmokers who did not receive active treatment and because the proportion of treatment completeness was lower.
Elderly SCLC patients are difficult to treat by standard methods for many reasons; for example, they often have multiple comorbidities and poor PS. Among patients diagnosed with SCLC, about 43% are 70 years of age or older and 10% are 80 years of age or older [19]. In elderly SCLC patients with good PS, platinum-based chemotherapy plus thoracic radiotherapy and carboplatin-based chemotherapy are recommended for LD- and ED-SCLC, respectively. Even when patients are old and have poor PS, treatment with chemotherapy is suggested if the poor PS is due to SCLC [20]. In our study, the proportions of treatment completeness and receiving chemotherapy were lower and that of receiving local therapy only was higher in the nonsmoking group, which had a higher proportion of elderly patients. Our findings are in line with those of a previous study where patients aged 70 years or younger were treated with best supportive care in only 17% to 23% of cases, but the percentage increased with higher age up to 75% of those aged 85 years or older [21]. Elderly SCLC patients experienced more severe adverse events, completed treatment less often, and died during treatment more frequently than younger patients [22]. However, active treatment, including chemotherapy and/or radiotherapy, has improved the survival of SCLC patients younger than 80 years of age [21]. It is necessary to consider active treatment in elderly SCLC patients who are not very old, taking into account their general condition.
The prognosis of never-smoking SCLC is known to be better than that of ever-smoking SCLC, even though a recent study reported the prognosis is not different between the two groups [5,6,7]. Further, radon-related SCLC, one type of nonsmoking SCLC, demonstrates aggressive features [23]. The exact molecular mechanisms of nonsmoking SCLC are not known; for example, different molecular signatures might exist at MEK and mTOR pathways [24]. Another theory is that SCLC is phenotypically transformed from pulmonary adenocarcinoma with epidermal growth factor receptor mutation (EGFR) mutations as an acquired-resistance mechanism during EGFR-tyrosine kinase inhibitor treatments [25, 26]. Among 28 genetically evaluable nonsmoking SCLC patients in Korea, EGFR mutations were detected in four cases [7]. Further investigation of relevant genetic and environmental factors in the context of never-smoking SCLC is needed.
Previous studies have reported conflicting results regarding the association between smoking status and age [27, 28]. In our study, ever smokers were significantly younger and had a slightly more favorable LD-SCLC than never-smokers did. These findings could be explained by that more frequent screenings for lung cancer in former smokers resulted in the detection of early-stage lung cancer [18]. Ever-smokers with less advanced disease and younger age showed more favorable OS outcomes in our study.
The substantial prevalence of SCLC among never-smokers is not explained conclusively, but there is evidence to suggest that documentation of smoking status is varied and can differ between various studies. Smoking history is subject to recall biases and self-reported reliability, and there may be a small misclassification of smokers as nonsmokers [27]. Other patients with risk factors for SCLC, such as exposure to environmental tobacco smoking, some work-related fumes, and indoor radon, might be included in the never-smoking SCLC group even though we could not analyze these risk factors in our study because the data collection did not consider these variables [23]. Of the types of nonsmoking SCLC, indoor radon-related SCLC is an aggressive type, and age at diagnosis is higher for histologic types other than this type in never-smokers [29].
One of the problems with SCLC is a late diagnosis, and presenting symptoms at the time of diagnosis can indicate a poor prognosis [23]. Contrary to other histologic tumor types, the central location of SCLC could cause symptoms earlier on and lead to early detection in the localized stages of the disease. In our study, the proportions of patients having one or more symptoms at the time of diagnosis were not similar but hemoptysis and weight loss were more frequently found in the ever-smoker group. It is estimated that nonsmokers with less symptoms who do not receive regular screening could receive a lung cancer diagnosis at a late age and carry a poorer prognosis.
This study had several limitations. First, this was a retrospective study lacking information such as secondhand smoking status and comorbidities. Also, due to the structure of the data, progression-free survival could not be confirmed, so there is a limitation in not confirming the relationship between smoking status and disease control after treatment. However, our study also had strengths given its use of an unbiased sampling method to sample a representative population of patients with lung cancer using a nationwide survey. Also, the number of patients in this study was relatively high. Our study will help broaden the understanding of the current epidemiologic status of SCLC and clinical characteristics in Korea.
Conclusions
In conclusion, this evaluation of an unbiased nationwide survey dataset revealed that a significant proportion of Korean SCLC patients were never-smokers. Never smoking appeared to be a significant prognostic factor according to the univariate analysis but was confirmed to be statistically insignificant through a multivariate analysis of the total population. These patients were older and showed a tendency not to receive active treatments. Active treatment of SCLC in aged patients not older than 80 years can improve survival, so a better understanding of the impact of treatment and toxic effects would enable physicians to discuss the risks and benefits of treatment with never-smoking patients.
Availability of data and materials
The datasets used and/or analyzed during the current study have been kept confidential and are not available publicly because the KALC and the Ministry of Health and Welfare, KCCR do not allow researchers to provide data personally or share publicly, but are available from the corresponding author upon reasonable request.
Abbreviations
- SCLC:
-
Small cell lung cancer
- KCCR:
-
The Korean Central Cancer Registry
- OS:
-
Overall survival
- KALC:
-
The Korean Association for Lung Cancer
- KALC-R:
-
The Korean Association for Lung Cancer Registry
- KCCR:
-
The Korean Central Cancer Registry
- BMI:
-
Body mass index
- ECOG:
-
Eastern Corporative Oncology Group
- PS:
-
Performance status
- ED:
-
Extensive-disease
- LD:
-
Limited-disease
- PCI:
-
Prophylactic cranial irradiation
- HR:
-
Hazard ratio
- TRT:
-
Thoracic radiotherapy
- CI:
-
Confidence interval
- EGFR:
-
Epidermal growth factor receptor mutation
References
American Society of Clinical Oncology: Lung Cancer—Small Cell: Statistics. https://www.cancer.net/cancer-types/lung-cancer-small-cell/statistics (2021). Accessed 12 May 2021.
Sabari JK, Lok BH, Laird JH, Poirier JT, Rudin CM. Unravelling the biology of SCLC: implications for therapy. Nat Rev Clin Oncol. 2017;14:549–61.
Ou SH, Ziogas A, Zell JA. Prognostic factors for survival in extensive stage small cell lung cancer (ED-SCLC): the importance of smoking history, socioeconomic and marital statuses, and ethnicity. J Thorac Oncol. 2009;4:37–43.
Cardona AF, Rojas L, Zatarain-Barrón ZL, Ruiz-Patiño A, Ricaurte L, Corrales L, et al. Multigene mutation profiling and clinical characteristics of small-cell lung cancer in never-smokers vs. heavy smokers (Geno1.3-CLICaP). Front Oncol. 2019;9:254.
Thomas A, Mian I, Tlemsani C, Pongor L, Takahashi N, Maignan K, et al. Clinical and genomic characteristics of small cell lung cancer in never smokers: results from a retrospective multicenter cohort study. Chest. 2020;158:1723–33.
Liu X, Jiang T, Li W, Li X, Zhao C, Shi J, et al. Characterization of never-smoking and its association with clinical outcomes in Chinese patients with small-cell lung cancer. Lung Cancer. 2018;115:109–15.
Sun JM, Choi YL, Ji JH, Ahn JS, Kim KM, Han J, et al. Small-cell lung cancer detection in never-smokers: clinical characteristics and multigene mutation profiling using targeted next-generation sequencing. Ann Oncol. 2015;26:161–6.
Varghese AM, Zakowski MF, Yu HA, Won HH, Riely GJ, Krug LM, et al. Small-cell lung cancers in patients who never smoked cigarettes. J Thorac Oncol. 2014;9:892–6.
Torres-Durán M, Ruano-Ravina A, Kelsey KT, Parente-Lamelas I, Provencio M, Leiro-Fernández V, et al. Small cell lung cancer in never-smokers. Eur Respir J. 2016;47:947–53.
Kurahara Y, Kawaguchi T, Tachibana K, Atagi S, Hayashi S, Kitaichi M, et al. Small-cell lung cancer in never-smokers: a case series with information on family history of cancer and environmental tobacco smoke. Clin Lung Cancer. 2012;13:75–9.
Choi CM, Kim HC, Jung CY, Cho DG, Jeon JH, Lee JE, et al. Report of the Korean Association of Lung Cancer Registry (KALC-R), 2014. Cancer Res Treat. 2019;51:1400–10.
Lee SY, Hong YK, Ji W, Lee JC, Choi CM. Active treatment improves overall survival in extremely older non-small cell lung cancer patients: a multicenter retrospective cohort study. Cancer Res Treat. 2021;53:104–11.
Schild SE, Zhao L, Wampfler JA, Daniels TB, Sio T, Ross HJ, et al. Small-cell lung cancer in very elderly (≥ 80 years) patients. Clin Lung Cancer. 2019;20:313–21.
Lee C, Kang KH, Koh Y, Chang J, Chung HS, Park SK, et al. Characteristics of lung cancer in Korea, 1997. Lung Cancer. 2000;30:15–22.
Tavares e Castro A, Clemente J, Carvalho L, Freitas S, Cemlyn-Jones J. Small-cell lung cancer in never-smokers: a case series. Lung Cancer. 2016;93:82–7.
Statistic Korea: 2020 Statistics on the Aged. http://kostat.go.kr/portal/eng/pressReleases/1/index.board?bmode=read&aSeq=388599 (2020). Accessed 12 May 2021.
Venuta F, Diso D, Onorati I, Anile M, Mantovani S, Rendina EA. Lung cancer in elderly patients. J Thorac Dis. 2016;8:S908–14.
Clément-Duchêne C, Stock S, Xu X, Chang ET, Gomez SL, West DW, et al. Survival among never-smokers with lung cancer in the cancer care outcomes research and surveillance study. Ann Am Thorac Soc. 2016;13:58–66.
Owonikoko TK, Ragin CC, Belani CP, Oton AB, Gooding WE, Taioli E, et al. Lung cancer in elderly patients: an analysis of the surveillance, epidemiology, and end results database. J Clin Oncol. 2007;25:5570–7.
Jett JR, Schild SE, Kesler KA, Kalemkerian GP. Treatment of small cell lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143:e400S – e419.
Janssen-Heijnen ML, Maas HA, Siesling S, Koning CC, Coebergh JW, Groen HJ. Treatment and survival of patients with small-cell lung cancer: small steps forward, but not for patients >80. Ann Oncol. 2012;23:954–60.
Stinchcombe TE, Fan W, Schild SE, Vokes EE, Bogart J, Le QT, et al. A pooled analysis of individual patient data from National Clinical Trials Network clinical trials of concurrent chemoradiotherapy for limited-stage small cell lung cancer in elderly patients versus younger patients. Cancer. 2019;125:382–90.
Torres-Durán M, Curiel-García MT, Ruano-Ravina A, Provencio M, Parente-Lamelas I, Hernández-Hernández J, et al. Small-cell lung cancer in never-smokers. ESMO Open. 2021;6: 100059.
Ogino A, Choi J, Lin M, Wilkens MK, Calles A, Xu M, et al. Genomic and pathological heterogeneity in clinically diagnosed small cell lung cancer in never/light smokers identifies therapeutically targetable alterations. Mol Oncol. 2021;15:27–42.
Zakowski MF, Ladanyi M, Kris MG. EGFR mutations in small-cell lung cancers in patients who have never smoked. N Engl J Med. 2006;355:213–5.
Tatematsu A, Shimizu J, Murakami Y, Horio Y, Nakamura S, Hida T, et al. Epidermal growth factor receptor mutations in small cell lung cancer. Clin Cancer Res. 2008;14:6092–6.
Toh CK. The changing epidemiology of lung cancer. Methods Mol Biol. 2009;472:397–411.
Wakelee HA, Chang ET, Gomez SL, Keegan TH, Feskanich D, Clarke CA, et al. Lung cancer incidence in never smokers. J Clin Oncol. 2007;25:472–8.
Torres-Durán M, Ruano-Ravina A, Parente-Lamelas I, Leiro-Fernández V, Abal-Arca J, Montero-Martínez C, et al. Lung cancer in never-smokers: a case-control study in a radon-prone area (Galicia, Spain). Eur Respir J. 2014;44:994–1001.
Acknowledgements
The data used for this study were provided by the Korean Association for Lung Cancer and the Ministry of Health and Welfare, Korea Central Cancer Registry.
Funding
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute(KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (Grant Number: HI21C0651).
Author information
Authors and Affiliations
Consortia
Contributions
HSK, CDY, and SJK contributed to the conception and design of the study, data analysis and interpretation, and the drafting and substantial revision of this manuscript. JUL, CKP, and SHL contributed to the acquisition of data. HSK, CDY, SHL, and SJK revised the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was reviewed and approved by the appropriate institutional review board at the National Cancer Center (NCC2018-0193), which waived the need to gather informed consent due to the retrospective nature of the study. This study was conducted in compliance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
Conflicts of interest relevant to this article do not exist.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kang, H.S., Lim, J.U., Yeo, C.D. et al. Characteristics and clinical outcomes of patients with nonsmoking small cell lung cancer in Korea. BMC Pulm Med 22, 200 (2022). https://doi.org/10.1186/s12890-022-01989-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-022-01989-x