Abstract
Clinical trials on cancer treatments frequently exclude patients with prior cancer, but more evidence is needed to understand their possible effects on outcomes. This study analyzed the prognostic impact of prior cancer in newly diagnosed non-small cell lung cancer (NSCLC) patients while accounting for various patient and cancer characteristics. Using population-based cancer registry data linked with administrative claims data, this retrospective cohort study examined patients aged 15–84 years diagnosed with NSCLC between 2010 and 2015 in Japan. Cox proportional hazards models were used to estimate the hazard ratios (HRs) and 95% confidence intervals (CIs) of all-cause mortality in patients with versus without prior cancer. The analysis was stratified according to NSCLC stage and diagnostic time intervals between prior cancers and the index NSCLC. We analyzed 9103 patients (prior cancer: 1416 [15.6%]; no prior cancer: 7687 [84.4%]). Overall, prior cancer had a non-significant mortality HR of 1.07 (95% CI: 0.97–1.17). Furthermore, prior cancer had a significantly higher mortality hazard for diagnostic time intervals of 3 years (HR: 1.23, 95% CI: 1.06–1.43) and 5 years (1.18, 1.04–1.33), but not for longer intervals. However, prior cancer in patients with more advanced NSCLC did not show a higher mortality risk for any diagnostic time interval. Smoking-related prior cancers and prior cancers with poorer prognosis were associated with poorer survival. NSCLC patients with prior cancer do not have an invariably higher risk of mortality, and should be considered for inclusion in clinical trials depending on their cancer stage.
Similar content being viewed by others
Introduction
The improved survival of cancer patients has inadvertently led to an increase in the number of persons with multiple primary cancers1,2,3,4. Despite the growing prevalence of newly diagnosed cancer patients with a history of cancer (e.g., 18.7% in the US and 11.1% in Japan)4,5, such patients are often excluded from clinical trials due to concerns that their presence may unduly affect outcomes and distort conclusions6,7,8,9,10,11. Overall, 80% of trials excluded lung cancer patients with prior cancer. The estimated proportion of patients with lung cancer excluded because of prior cancer ranged from 0 to 18%7. The omission of these patients may limits the generalizability of findings from clinical trials and observational research, resulting in a dearth of evidence on new treatment modalities for cancer survivors6,7,8,9,10,11.
Previous studies have produced conflicting findings on the prognostic impact of prior cancer in newly diagnosed lung cancer patients. While some studies have reported that prior cancer did not reduce survival in early-stage, locally advanced, or advanced lung cancer patients12,13,14; others have noted that the prognostic impact of prior cancer can vary according to lung cancer stage15,16,17,18. In contrast, several studies have indicated that prior cancer negatively impacts survival in lung cancer patients after adjusting for clinical prognostic factors19,20,21. Accordingly, there is a need for multicenter studies that explore the impact of prior cancer on survival in large cancer populations while adjusting for known clinical prognostic factors. Furthermore, studies should also consider lung cancer stage, the diagnostic time intervals between prior cancers and new cancers, and the diverse characteristics of prior cancers, including stage, smoking-relatedness22,23.
More research is required to facilitate the evidence-driven development of eligibility criteria for clinical cancer research. To contribute to this evidence base, this study was conducted to provide clinically comparable estimates of the prognostic impact of prior cancer in newly diagnosed non-small cell lung cancer (NSCLC) patients in a Japanese prefecture with consideration to patient characteristics, cancer characteristics, and diagnostic time interval.
Materials and methods
Study design and data sources
This multicenter retrospective cohort study was conducted on newly diagnosed NSCLC patients to compare their mortality risk with and without prior cancer using a database that linked population-based cancer registry data with administrative claims data.
Cancer registry data were acquired from the Osaka Cancer Registry (OCR), which was founded in 1962 with the aim of registering and monitoring all malignant tumors and benign intracranial tumors in residents of Osaka Prefecture—Japan’s third largest metropolis24. The registry data include each patient’s age at diagnosis, sex, method of cancer detection, cancer site, histology, stage, treatment, and vital status information (verified through death certificates and official resident registries). The OCR contains high-quality data that have been used in the International Agency for Research on Cancer’s “Cancer Incidence in Five Continents” Volumes III to XI25.
The claims data were generated by acute care hospitals under Japan’s Diagnosis Procedure Combination Per-Diem Payment System for the purpose of reimbursement from insurers. These data incorporate clinical summaries and detailed claims records of treatments that are not included in cancer registry data26.
Linked data were collected from 35 cancer care hospitals with cooperation from the Council for Coordination of Designated Cancer Care Hospitals (Osaka, Japan). These 35 hospitals treat approximately half of all cancer patients within Osaka Prefecture. The cancer registry data and claims data were linked at the patient level, and the record linkage rate was estimated to be 98%18,27,28.
Study population
The study population comprised patients who received a new diagnosis of NSCLC between 2010 and 2015, which was designated the index cancer for this study. Patients who fulfilled the following criteria were included in the analysis: (1) aged 15–84 years at the NSCLC diagnosis, (2) pathological diagnosis of NSCLC, (3) survived for 3 months or more after the NSCLC diagnosis, (4) claims data could be linked with OCR data, and (5) registration in the OCR through sources other than death certificate only. Lung cancer was identified using the ICD-10 code of C34.x, and NSCLC histology was determined using the relevant International Classification of Diseases for Oncology, Third Edition morphological codes. The study patients were identified as those with a diagnosis of adenocarcinoma (morphological codes: 8140, 8211, 8230–8231, 8250–8260, 8323, 8480–8490, 8550–8552, 8570–8574, 8576), squamous cell carcinoma (8041–8045), adenosquamous carcinoma (8560), large cell carcinoma (8010–8012, 8014–8031, 8035, 8310), or NSCLC-not otherwise specified (8046). We excluded patients aged 85 years or older with reference to the previous clinical trials29,30. Patients who were diagnosed with the index NSCLC were followed for a minimum of 3 years after lung cancer diagnosis.
We divided the patients into 2 groups: a Prior Cancer Group (patients with a history of prior cancer) and a No Prior Cancer Group (those without any history of prior cancer). Prior cancer was defined as the most recent cancer diagnosed before the index NSCLC, and was identified based on multiple cancer records in the OCR in accordance with the guidelines of the International Agency for Research on Cancer and the International Association of Cancer Registries31. We obtained information on all prior cancers that were diagnosed between 1975 and 2015 from the OCR database.
Multiple cancers of the same site in a patient were integrated into a single cancer based on stage (most advanced) and order of occurrence (most recent). We identified 44 prior cancer sites using their corresponding ICD-10 codes (Supplementary Table 1)32.
Study outcome
The study outcome measure was overall survival, which was calculated from the date of the index NSCLC diagnosis to the date of all-cause death or the date of censoring (i.e., last confirmed survival date).
NSCLC characteristics
For each patient, we analyzed age, sex, method of cancer detection, histology, stage, treatment, use of tyrosine kinase inhibitors targeting epidermal growth factor receptor or anaplastic lymphoma kinase in any line of treatment, current or past smoking status, and diagnosis year for the index NSCLC. The methods of cancer detection included screening and medical check-up, incidental detection during follow-up examination for another disease, and other/unknown (mostly involving detection based on subjective symptoms)33. NSCLC stage at diagnosis was specified according to the Surveillance, Epidemiology, and End Results (SEER) system, and included localized, regional, distant, and other/unknown34. Treatment included radiotherapy only, chemotherapy only, chemoradiotherapy, surgery only, surgery plus chemotherapy and/or radiotherapy, and other/unknown (including no treatment).
We used the Barthel Index to measure performance in activities of daily living at the index NSCLC diagnosis as a substitute for the Eastern Cooperative Oncology Group-Performance Status (ECOG-PS)28. Patients were defined as having severe dependence for Barthel Index scores of 35 or lower (corresponding to ECOG-PS 3 or 4), moderate dependence for scores of 40–55 (ECOG-PS 2), and mild or no dependence for scores of 60 or higher (ECOG-PS 0 or 1)35.
Body mass index at the index NSCLC diagnosis was categorized into underweight (< 18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), and obese (≥ 30 kg/m2)28.
The Quan version of the Charlson Comorbidity Index (CCI) scores18,36 were categorized into 0, 1, and 2 or more12. Primary and metastatic solid tumors were excluded from the CCI scores due to their potential overlap with the prior and index cancers. Furthermore, interstitial lung disease (ICD-10 code: J84.x) was analyzed as an independent covariate due to its strong prognostic implications in lung cancer37.
Finally, we analyzed the Area Deprivation Index of each patient’s area of residence as a socioeconomic indicator38. Area Deprivation Index scores were divided into quartiles, and categorized from Q1 (least deprived) to Q4 (most deprived). Missing values were categorized as “unknown”.
Prior cancer characteristics
For patients in the Prior Cancer Group, we calculated the number, the stage, and the sites of prior cancers, as well as the diagnostic time interval between the most recent prior cancer and the index NSCLC. Prior cancers were categorized according to the following 3 characteristics: smoking-relatedness, prognosis, and SEER summary stage at diagnosis. Smoking-related prior cancers included cancers of the mouth, pharynx, larynx, lung, esophagus, stomach, liver, pancreas, kidney, urinary bladder (renal pelvis, ureter, or bladder), colorectum, uterine cervix, and acute myeloid leukemia19,39,40,41,42. All other cancers were regarded as non–smoking-related cancers. Next, prognoses of the prior cancers were categorized based on their survival rates; cancers with better prognosis and cancers with poorer prognosis were defined as those with ≥ 50% and < 50%, respectively, of the median 10-year relative survival rate (Supplementary Table 2)43. All other cancers with unknown survival rates were categorized as “unknown”.
Statistical analysis
Categorical variables were analyzed as proportions, and continuous variables were analyzed as median (interquartile range).
For the survival analysis, we excluded synchronous prior cancers from the Prior Cancer Group due to their possible influence on the timing and method of treatment. Using the criteria proposed by Moertel et al.44 synchronous prior cancers were defined as those that occurred within 6 months before the index NSCLC diagnosis. First, a Cox proportional hazards model was constructed to calculate the hazard ratio (HR) and 95% confidence interval (CI) of all-cause mortality in the Prior Cancer Group relative to the No Prior Cancer Group; this model examined all prior cancers within the OCR records linking with claims data, regardless of their diagnostic time intervals before the index NSCLC diagnosis. The model adjusted for the following covariates at the index NSCLC diagnosis: age, sex, method of cancer detection, treatment, body mass index, Barthel Index, CCI, interstitial lung disease, tyrosine kinase inhibitor use, smoking status, diagnosis year, and Area Deprivation Index. Next, we constructed additional Cox proportional hazards models to examine the impact of prior cancer on survival when the diagnostic time intervals were limited to within 1, 3, 5, 10, and 15 years before the index NSCLC diagnosis. These analyses were also stratified according to the index NSCLC stage. In each NSCLC stage, patients whose prior cancer occurred within the stipulated diagnostic time interval were categorized into the Prior Cancer Group, and patients without any prior cancer or whose prior cancer did not occur within the stipulated diagnostic time interval were categorized into the No Prior Cancer Group.
To examine the impact of prior cancers according to their characteristics, we constructed 3 Cox proportional hazards models. In Model 1, prior cancers were divided into smoking-related and non–smoking-related cancers. In Model 2, prior cancers were divided into those with better prognosis and poorer prognosis. In Model 3, prior cancers were categorized according to their stage at diagnosis.
Statistical significance was set at 5% (two-sided). All analyses were performed using STATA version 16 (Stata Corporation, College Station, TX, USA).
Sensitivity analysis
Previous studies have reported that lung cancer patients with prior cancer do not have significantly poorer survival than those without prior cancer12,13,14. A possible explanation for those observations is that cancer patients with prior cancer may have longer lead times before a new cancer diagnosis (i.e., earlier detection) due to more frequent screening or prompt healthcare-seeking behavior for potential tumor symptoms. A previous study reported that the estimated mean lead times (MLTs) are 3.4, 1.1, and 1.1 months for lung cancer patients in stages I/II, III, and IV, respectively, under the assumption that only patients with prior cancer are susceptible to lead time bias45. To investigate the robustness of our results, we considered lead time bias in the Prior Cancer Group using 1 × MLT, 2 × MLT, and 3 × MLT. The survival analysis was then performed by subtracting the various MLT durations from survival time in the Prior Cancer Group according to index NSCLC stage45,46. In this sensitivity analysis, we regarded localized cancers as stage I/II, regional cancers as stage III, and distant cancers as stage IV.
Ethics approval and consent to participate
This study was approved by the Kyoto University Graduate School of Medicine Ethics Committee (Approval No. R1808) and the Research Ethics Committee of Osaka International Cancer Institute (Approval No. 19143). The dataset was provided by the OCR with no personally identifiable information, and was processed independently in compliance with the Act on Promotion of Cancer Registries of Japan. Both ethics committees waived the need for informed consent in accordance with the Japanese government’s Ethical Guidelines for Medical and Health Research Involving Human Subjects, which allow for the opt-out approach for the secondary use of existing data. The study was performed in accordance with the ethical standards established in the Declaration of Helsinki.
Results
Baseline characteristics of the patients
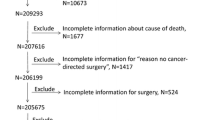
The patient selection process is presented in Fig. 1. We first identified 9,103 index NSCLC patients who met the inclusion criteria. Among these, 1416 (15.6%) patients had 1 prior cancer or more. For the survival analysis, we excluded 253 patients with synchronous prior cancers. Table 1 summarizes the baseline characteristics of the NSCLC patients. In the No Prior Cancer Group, the median age (interquartile range) was 70 (64–75) years and women comprised 34.7% of the patients. In the Prior Cancer Group, the median age (interquartile range) was 73 (67–77) years and women comprised 29.5% of the patients. The median survival time (interquartile range) was 24.0 (12.9–46.2) months in the No Prior Cancer Group and 29.0 (15.9–47.0) months in the Prior Cancer Group.
Characteristics of prior cancer
The characteristics of prior cancer in the Prior Cancer Group are shown in Supplementary Table 3. The majority of patients in the Prior Cancer Group had only 1 prior cancer before the index NSCLC in both sexes. The cumulative proportion of patients whose most recent prior cancer was diagnosed within 5 years before the index NSCLC diagnosis was 62.1% (64.1% in male patients and 56.6% in female patients). The most common and least common prior cancer stages were localized and distant, respectively. The most common prior cancer sites were stomach (26.7%), prostate (14.9%), and colon (13.7%) among male patients; and breast (31.3%), stomach (15.8%), and colon (9.6%) among female patients. Smoking-related cancers accounted for 75.1% of all prior cancers in male patients and 48.8% of all prior cancers in female patients.
Impact of prior cancer on survival according to diagnostic time interval and index NSCLC stage
The results of the Cox proportional hazards analyses according to diagnostic time interval are presented in Table 2. The adjusted HR of the Prior Cancer Group (ref: No Prior Cancer Group) for all-cause mortality was 1.07 (95% CI: 0.97–1.17), regardless of diagnostic time interval between the most recent prior cancer and the index NSCLC. When the diagnostic time intervals were limited to 3 and 5 years, the mortality HRs of the Prior Cancer Group were 1.23 (95% CI: 1.06–1.43) and 1.18 (1.04–1.33), respectively. When the diagnostic time intervals were limited to 1, 10, and 15 years, the Prior Cancer Group did not show any significantly higher hazards for mortality than the No Prior Cancer Group (Table 2). Area Deprivation Index scores were not associated with prognosis. When including all prior cancers regardless of diagnostic time interval in the analysis, the Prior Cancer Group was not significantly associated with mortality in regional and distant NSCLC patients, but had a significantly higher mortality hazard in localized NSCLC patients (Fig. 2). Among the limited diagnostic time intervals, the Prior Cancer Group had consistently higher mortality hazards in localized and regional NSCLC patients (except for diagnostic time intervals of 1 year), but not in distant NSCLC patients.
Impact of prior cancer on survival in NSCLC patients according to diagnostic time interval and index NSCLC stage. HRs were calculated using Cox proportional hazards models on all-cause mortality in NSCLC patients stratified by diagnostic time interval (between the most recent prior cancer and the index cancer) and index NSCLC stage. The No Prior Cancer Group was used as the reference category. For all diagnostic time intervals in these models, there were 3328 localized NSCLC patients, 2191 regional NSCLC patients, and 3244 distant NSCLC patients. Abbreviations: CI, confidence interval; HR, hazard ratio; NSCLC, non-small cell lung cancer.
Impact of prior cancer on survival according to prior cancer characteristics
Additional analyses were performed to examine the heterogeneous effects of prior cancers according to their characteristics (Fig. 3). Here, we categorized prior cancers according to smoking-relatedness (Model 1), prognosis (Model 2), and stage at diagnosis (Model 3). Smoking-related prior cancers (HR: 1.11; 95% CI: 1.001–1.22) in Model 1 and prior cancers with poorer prognosis (HR: 1.35; 95% CI: 1.09–1.67) in Model 2 showed higher mortality hazards than the No Prior Cancer Group. In Model 3, the mortality hazard appeared to increase together with prior cancer stage, but this relationship was not significant.
Impact of prior cancer on survival in NSCLC patients according to prior cancer characteristics. HRs were calculated using 3 Cox proportional hazards models on all-cause mortality in NSCLC patients. In Model 1, NSCLC patients were divided into no prior cancer, smoking-related prior cancer, and non–smoking-related prior cancer. In Model 2, NSCLC patients were divided into no prior cancer, prior cancer with better prognosis, and prior cancer with poorer prognosis. In Model 3, NSCLC patients were divided into no prior cancer, localized prior cancer, regional prior cancer, and distant prior cancer. The No Prior Cancer Group was used as the reference category. Abbreviations: CI, confidence interval; HR, hazard ratio; NSCLC, non-small cell lung cancer.
Sensitivity analysis
To assess the robustness of our results, we considered lead time bias in the Prior Cancer Group. The Prior Cancer Group was not significantly associated with mortality in distant NSCLC patients, but had a significantly higher mortality hazard in localized NSCLC patients (Table 3). These findings were consistent with the results of the main analysis.
Discussion
Using a large dataset consisting of cancer registry data linked with claims data, this study analyzed the impact of prior cancer on survival in newly diagnosed NSCLC patients. Our analysis provides new insight into this relationship with consideration to patient characteristics, cancer characteristics, and diagnostic time intervals. Our results were consistent when incorporating the potential for the lead-time bias among the cancer survivors.
We found that longer diagnostic time intervals between the prior cancers and index NSCLC were generally characterized by smaller effect sizes (mortality HRs). For diagnostic time intervals of 3 and 5 years, prior cancer was significantly associated with a higher mortality hazard. However, this relationship was not observed for other diagnostic time intervals. Although many clinical trials employ a 5-year exclusion window for prior cancers without a clear rationale7,47, our findings indicate that this criterion may be justified. Nevertheless, the 5-year exclusion window may not be necessary for clinical trials involving patients with more advanced NSCLC as our analysis showed that prior cancer was not associated with prognosis in these patients. A possible explanation could be that regional/distant NSCLC is already associated with poorer prognosis, which may have a greater impact on survival than a history of prior cancer. Prior cancer may have little or no prognostic impact in patients with more advanced NSCLC. There is the growing prevalence of lung cancer patients with prior cancer and the cumulative proportions of the most recent prior cancers diagnosed within 5 years before the lung cancer diagnosis were 69.4% (male) and 65.0% (female)4. These may indicate that relatively large numbers of lung cancer patients will not be eligible for clinical trials by the 5-year exclusion window.
Our findings from the main analysis were supported by the sensitivity analysis that accounted for potential lead time bias45, which was often neglected in previous studies on the association between prior cancer and prognosis in NSCLC patients12,13,14. Our study therefore provides robust evidence that the prognostic impact of prior cancers is influenced by the index NSCLC stage.
In addition to assessing the prognostic implications of prior cancer according to diagnostic time interval, we also examined the heterogeneous effects of prior cancer according to their characteristics. Here, we found that smoking-related prior cancers had a significantly negative impact on survival in newly diagnosed NSCLC patients. This may be because smoking-related cancer survivors have a higher risk of being cigarette smokers, which is an important prognostic factor for NSCLC17,48. In addition, prior cancers with poorer prognosis were associated with higher mortality for the index NSCLC. This suggests that the sites of prior cancer and their associated survival rates should be taken into account when evaluating their prognostic impact.
Strengths and limitations
A strength of this study was the inclusion of diagnostic time intervals between the prior cancers and index lung cancer, and we propose that these intervals should be considered in the eligibility criteria for clinical trials on NSCLC patients. Another strength was the categorization of prior cancer according to its characteristics, which enabled a more in-depth analysis of which aspects of prior cancer could affect survival. Furthermore, by linking cancer registry data with claims data, we were able to account for many known prognostic factors (e.g., performance in activities of daily living, comorbidities, and smoking status) that are frequently absent from registry-based studies.
Our study has several limitations. First, we did not have access to information on TNM classification, gene mutations, and ECOG-PS, which are often used in clinical practice. As alternatives to these indicators, we used SEER summary staging, tyrosine kinase inhibitor use, and the Barthel Index due to their availability in the claims data. Second, although the OCR has been in operation since 1962 and has accumulated cancer incidence data from over a million patients in Osaka Prefecture, our findings should be validated using data from other regions or countries. Third, our study was conducted using cancer registry data linked with administrative claims data from approximately half of all cancer patients within Osaka Prefecture. Therefore, the study population may not be representative of the entire population in the study region, and could be susceptible to selection bias.
Cancer treatment should be provided to patients with prior cancer based on an empirical understanding of their possible prognostic relevance. As the number of cancer survivors increases steadily, there is a need to increase their representation in clinical cancer research in order to generate evidence for their treatment and improve the generalizability of results.
In conclusion, NSCLC patients with prior cancer do not have an invariably higher risk of mortality than those without prior cancer. NSCLC patients with prior cancer should be considered for inclusion in clinical trials, especially for studies on regional and distant NSCLC. More inclusive clinical trials are required to better inform treatment strategies, and our findings underscore the need to revisit the eligibility criteria for cancer survivors in clinical research.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- CCI:
-
Charlson comorbidity index
- ECOG-PS:
-
Eastern Cooperative Oncology Group-Performance Status
- ICD-10:
-
International classification of diseases, tenth revision
- NSCLC:
-
Non-small cell lung cancer
- OCR:
-
Osaka Cancer Registry
- SEER:
-
Surveillance, epidemiology, and end results
- MLT:
-
Mean lead times
References
Tabuchi, T., Ito, Y., Ioka, A., Miyashiro, I. & Tsukuma, H. Incidence of metachronous second primary cancers in Osaka, Japan: Update of analyses using population-based cancer registry data. Cancer Sci 103, 1111–1120 (2012).
Xia, W. et al. Improvement of survival for non-small cell lung cancer over time. Onco Targets Ther. 10, 4295–4303 (2017).
Mao, R. et al. The burdens of lung cancer involved multiple primary cancers and its occurring patterns-SEER Analysis between 1973 and 2006. Sci. Rep. 7, 6451 (2017).
Sato, A. et al. Increasing trends in the prevalence of prior cancer in newly diagnosed lung, stomach, colorectal, breast, cervical, and corpus uterine cancer patients: A population-based study. BMC Cancer 21, 264 (2021).
Murphy, C. C., Gerber, D. E. & Pruitt, S. L. Prevalence of prior cancer among persons newly diagnosed with cancer: An initial report from the surveillance, epidemiology, and end results program. JAMA Oncol. 4, 832–836 (2018).
Bradley, C. J. et al. Antineoplastic treatment of advanced-stage non-small-cell lung cancer: Treatment, survival, and spending (2000 to 2011). J. Clin. Oncol. 35, 529–535 (2017).
Gerber, D. E., Laccetti, A. L., Xuan, L., Halm, E. A. & Pruitt, S. L. Impact of prior cancer on eligibility for lung cancer clinical trials. J. Natl. Cancer Inst. 106, dju302 (2014).
Brooks, G. A. et al. Hospitalization and survival of medicare patients treated with carboplatin plus paclitaxel or pemetrexed for metastatic, nonsquamous, non-small cell lung cancer. JAMA Netw. Open 1, e183023–e183023 (2018).
Duma, N. et al. Characterization of comorbidities limiting the recruitment of patients in early phase clinical trials. Oncologist 24, 96–102 (2019).
Kim, E. S. et al. Modernizing eligibility criteria for molecularly driven trials. J. Clin. Oncol. 33, 2815–2820 (2015).
Kim, E. S. et al. Broadening eligibility criteria to make clinical trials more representative: American Society of Clinical Oncology and Friends of Cancer Research Joint Research Statement. J. Clin. Oncol. 35, 3737–3744 (2017).
Laccetti, A. L., Pruitt, S. L., Xuan, L., Halm, E. A. & Gerber, D. E. Effect of prior cancer on outcomes in advanced lung cancer: Implications for clinical trial eligibility and accrual. J. Natl. Cancer Inst. 107, djv002 (2015).
Pruitt, S. L., Laccetti, A. L., Xuan, L., Halm, E. A. & Gerber, D. E. Revisiting a longstanding clinical trial exclusion criterion: Impact of prior cancer in early-stage lung cancer. Br. J. Cancer 116, 717–725 (2017).
Laccetti, A. L., Pruitt, S. L., Xuan, L., Halm, E. A. & Gerber, D. E. Prior cancer does not adversely affect survival in locally advanced lung cancer: A national SEER-medicare analysis. Lung Cancer 98, 106–113 (2016).
Liu, J. et al. Impact of prior cancer history on the overall survival of younger patients with lung cancer. ESMO Open 5, e000608 (2020).
Monsalve, A. F. et al. Variable impact of prior cancer history on the survival of lung cancer patients. Lung Cancer 127, 130–137 (2019).
Kawaguchi, T. et al. Performance status and smoking status are independent favorable prognostic factors for survival in non-small cell lung cancer: A comprehensive analysis of 26,957 patients with NSCLC. J. Thorac. Oncol. 5, 620–630 (2010).
Morishima, T. et al. Impact of comorbidities on survival in gastric, colorectal, and lung cancer patients. J. Epidemiol. 29, 110–115 (2019).
Aguilo, R. et al. Multiple independent primary cancers do not adversely affect survival of the lung cancer patient. Eur. J. Cardiothorac. Surg. 34, 1075–1080 (2008).
Li, F. et al. Multiple primary malignancies involving lung cancer. BMC Cancer 15, 696 (2015).
Komatsu, H. et al. Prognosis associated with synchronous or metachronous multiple primary malignancies in patients with completely resected non-small cell lung cancer. Surg. Today 49, 343–349 (2019).
Tabuchi, T., Ozaki, K., Ioka, A. & Miyashiro, I. Joint and independent effect of alcohol and tobacco use on the risk of subsequent cancer incidence among cancer survivors: A cohort study using cancer registries. Int. J. Cancer 137, 2114–2123 (2015).
Zhou, H. et al. Impact of prior cancer history on the overall survival of patients newly diagnosed with cancer: A pan-cancer analysis of the SEER database. Int. J. Cancer 143(7), 1569–1577 (2018).
Tsukuma, H. et al. Incidence of second primary cancers in Osaka residents, Japan, with special reference to cumulative and relative risks. Jpn. J. Cancer Res. 85, 339–345 (1994).
Bray, F. et al. Cancer Incidence in Five Continents Vol. XI (International Agency for Research on Cancer, 2017).
Hayashida, K., Murakami, G., Matsuda, S. & Fushimi, K. History and profile of diagnosis procedure combination (DPC): Development of a real data collection system for acute inpatient care in Japan. J. Epidemiol. 31, 1–11 (2021).
Morishima, T. et al. Between-hospital variations in 3-year survival among patients with newly diagnosed gastric, colorectal, and lung cancer. Sci. Rep. 12, 7134 (2022).
Morishima, T., Sato, A., Nakata, K. & Miyashiro, I. Geriatric assessment domains to predict overall survival in older cancer patients: An analysis of functional status, comorbidities, and nutritional status as prognostic factors. Cancer Med. 9, 5839–5850 (2020).
Hotta, K., Ueoka, H., Kiura, K., Tabata, M. & Tanimoto, M. An overview of 48 elderly-specific clinical trials of systemic chemotherapy for advanced non-small cell lung cancer. Lung Cancer 46, 61–76 (2004).
Jatoi, A. et al. Should elderly non-small-cell lung cancer patients be offered elderly-specific trials? Results of a pooled analysis from the North Central Cancer Treatment Group. J. Clin. Oncol. 23, 9113–9119 (2005).
Group R.W. International rules for multiple primary cancers (ICD-O-third edition). Eur. J. Cancer Prev. 14, 307–308 (2005).
World Health Organization. International Statistical Classification of Diseases and Health Related Problems 2nd edn. (World Health Organization, 2004).
Department of Public Health and Medical Affairs Osaka Prefectural Government & Cancer Control Center Osaka International Cancer Institute. Annual Report of Osaka Cancer Registry vol. 84: Cancer Incidence and Treatment in 2016 and Cancer Survival in 2011 in Osaka. Osaka Prefectural Government (2020).
Young, J. L. Jr, Ries, L. A. G., Fritz, A. G., Hurlbut, A. A. SEER summary staging manual-2000: Codes and coding instructions. National Cancer Institute (NIH Pub, Bethesda, MD, 2001)
Hernandez-Quiles, C. et al. Concordance of Barthel Index, ECOG-PS, and Palliative Performance Scale in the assessment of functional status in patients with advanced medical diseases. BMJ Support. Palliat. Care 7, 300–307 (2017).
Quan, H. et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am. J. Epidemiol. 173, 676–682 (2011).
Naccache, J. M. et al. Lung cancer and interstitial lung disease: A literature review. J. Thorac. Dis. 10, 3829–3844 (2018).
Nakaya, T. et al. Associations of all-cause mortality with census-based neighbourhood deprivation and population density in Japan: A multilevel survival analysis. PLoS ONE 9, e97802 (2014).
Warren, G. W., Alberg, A. J., Kraft, A. S. & Cummings, K. M. The 2014 Surgeon General’s report: “The health consequences of smoking–50 years of progress”: A paradigm shift in cancer care. Cancer 120, 1914–1916 (2014).
Shiels, M. S. et al. Cigarette smoking prior to first cancer and risk of second smoking-associated cancers among survivors of bladder, kidney, head and neck, and stage I lung cancers. J. Clin. Oncol. 32, 3989–3995 (2014).
Fircanis, S., Merriam, P., Khan, N. & Castillo, J. J. The relation between cigarette smoking and risk of acute myeloid leukemia: An updated meta-analysis of epidemiological studies. Am. J. Hematol. 89, E125-132 (2014).
Ugai, T. et al. Smoking and subsequent risk of acute myeloid leukaemia: A pooled analysis of 9 cohort studies in Japan. Hematol. Oncol. 36, 262–268 (2018).
Ito, Y. et al. Long-term survival and conditional survival of cancer patients in Japan using population-based cancer registry data. Cancer Sci. 105, 1480–1486 (2014).
Moertel, C. G., Dockerty, M. B. & Baggenstoss, A. H. Multiple primary malignant neoplasms. I. Introduction and presentation of data. Cancer 14, 221–230 (1961).
Ge, Z., Heitjan, D. F., Gerber, D. E., Xuan, L. & Pruitt, S. L. Estimating lead-time bias in lung cancer diagnosis of patients with previous cancers. Stat. Med. 37, 2516–2529 (2018).
Duffy, S. W. et al. Correcting for lead time and length bias in estimating the effect of screen detection on cancer survival. Am. J. Epidemiol. 168, 98–104 (2008).
Gerber, D. E., Pruitt, S. L. & Halm, E. A. Should criteria for inclusion in cancer clinical trials be expanded?. J. Comp. Eff. Res. 4, 289–291 (2015).
Gritz, E. R., Talluri, R., Fokom Domgue, J., Tami-Maury, I. & Shete, S. Smoking behaviors in survivors of smoking-related and non–smoking-related cancers. JAMA Netw. Open 3, e209072 (2020).
Acknowledgements
We are grateful to Dr. Takahiro Higashi (National Cancer Center Japan) for his technical assistance in the record linkage process, and to the staff of the 35 hospitals for providing the administrative claims data.
Funding
This study was supported by a grant from the Ministry of Health, Labour and Welfare of Japan [Grant Number H30-Gantaisaku-Ippan-009], a Grant-in-Aid for Early-Career Scientists from the Japan Society for the Promotion of Science [Grant Number JP20K18869], and a Special Research Grant from the Taiju Life Social Welfare Foundation. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization, Data Curation, and Methodology: A.S. Investigation, Writing – Original Draft, and Writing – Review & Editing: A.S., T.M., M.T., K.N., K.K., I.M. Supervision: K.K., I.M. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
K. Kawakami has received research funds from Eisai Co., Ltd.; Kyowa Kirin Co., Ltd.; Sumitomo Dainippon Pharma Co., Ltd.; Pfizer Inc.; Stella Pharma Corporation; CMIC Co., Ltd.; Suntory Beverage & Food Ltd.; Mitsubishi Corporation, and Real World Data Co., Ltd.; consulting fees from LEBER Inc.; JMDC Inc.; Shin Nippon Biomedical Laboratories Ltd.; Kaken Pharmaceutical Co., Ltd.; and Advanced Medical Care Inc.; executive compensation from Cancer Intelligence Care Systems, Inc.; honoraria from Mitsubishi Chemical Holdings Corporation, Mitsubishi Corporation, Pharma Business Academy, and Toppan Inc.; and holds stock in Real World Data Co., Ltd. The sponsors had no control over the interpretation, writing, or publication of this work. No potential conflicts of interest were disclosed by the other authors.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sato, A., Morishima, T., Takeuchi, M. et al. Survival in non-small cell lung cancer patients with versus without prior cancer. Sci Rep 13, 4269 (2023). https://doi.org/10.1038/s41598-023-30850-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-30850-2
- Springer Nature Limited
This article is cited by
-
Prognostic factors and nomogram for pulmonary resected high-grade neuroendocrine carcinomas: a 20-year single institutional real-world experience
Orphanet Journal of Rare Diseases (2024)