Abstract
Background
Contraceptive usage in Ethiopia is significantly influenced by the decision-maker at the household level. Joint decision-making involving both women and their husbands/partners is considered ideal for improving contraceptive uptake among women and for managing health outcomes related to contraceptive side effects. However, there is a lack of substantial evidence regarding the prevalence and impact of joint decision-making on contraceptive use in Ethiopia. Therefore, the current study aimed to assess the magnitude of joint decision-making on contraceptive use and its determinant factors among married, contraceptive-using, reproductive-age women in Ethiopia.
Methods
This study was conducted based on the Ethiopian Demographic and Health Survey (EDHS) 2016 data. A total weighted sample of 3,669 married, contraceptive-using, reproductive-age women were included in the study. Multilevel logistic regression was employed due to the hierarchical nature of the data. Variables with a p-value of ≤ 0.2 in the bivariate multilevel analysis were included in the multivariable multilevel analysis. The adjusted odds ratio (AOR) with a 95% confidence interval (CI) was used to determine the direction and strength of associations. Variables with a p-value of < 0.05 in the multivariable multilevel analysis were considered statistically significant for joint decision-making on contraceptive use.
Results
The prevalence of joint decision-making on contraceptive use in Ethiopia was 78.81% [95% CI: 71.35-74.23%]. Several factors were found to be statistically significant in relation to joint decision-making on contraceptive use: Women educational level primary, secondary, and higher (Adjusted odds’ ratio (AOR = 1.5; CI 1.2–1.9), (AOR = 1.9; CI 1.3–2.9), and (AOR = 2.1; CI 1.2–3.5) respectively, protestant in religion (AOR = 1.7; CI 1.7–2.5), wealth status rich (AOR = 1.4; CI 1.1–1.9), media exposure (AOR = 1.4; CI 1.1–1.9), and community poverty high (AOR = 0.6; CI 0.6–0.9).
Conclusions
In Ethiopia, the majority of contraceptive users are married, reproductive-age women, and their decision to use contraceptives is typically made jointly with their husbands or partners. Factors positively associated with joint decision-making on contraceptive use include women’s educational level (primary, secondary, and higher), being Protestant, having a higher wealth status, and media exposure. Conversely, women living in communities with high poverty levels are less likely to make joint decisions about contraceptive use. Health care providers, health care programmers and policy makers should be focused on these determinant factors to enhance joint decision-making in women’s contraceptive use in Ethiopia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
High fertility rates can create an imbalance in the economy of a given nation and are one of the causes of the loss of both maternal and neonatal lives [1]. Especially in developing nations, rapid population growth resulting from high fertility rates jeopardizes social and economic development [2]. Currently, the expected population growth of Ethiopia is very high. Evidence suggests that if the current rate of population growth continues, the total population of Ethiopia will reach 130.5 million by the mid-2030s [3]. Family planning is a crucial tool to balance population growth with the economy on a global scale. It is also important for improving the health status of women and children and for maintaining the stability of the ecosystem in general [6,7,8,9].
There has been an improvement in healthcare service coverage, including family planning services, over time [10, 11]. There is evidence showing that the current modern contraceptive prevalence rate in Ethiopia has reached 36.7% [12]. This improvement has had a significant impact on maternal, neonatal, and child health outcomes. The maternal mortality ratio has decreased to 412 per 100,000 live births [13]. Family planning is not only crucial for the health of women and neonates but also serves as a cornerstone for women’s empowerment. It facilitates the advancement of educational attainment among female adolescents by allowing them to plan their futures more effectively [14, 15]. Currently, the adolescent fertility rate has declined globally.
[16]. Despite the above improvements in the coverage of contraceptive use,, there is a high prevalence of unmet needs in Ethiopia.
Africa region is known for the high prevalence of unmet needs [17]. The prevalence of unmet need among reproductive-age women in Ethiopia is 22% [18]. The high prevalence of unmet needs among the population has negative consequences for health outcomes and productivity [19, 20]. Many women have died due to the consequences of unintended pregnancies and short birth intervals [21, 22].
Decision-making power is a crucial factor in accessing healthcare services, including contraceptive use. Evidence suggests that women’s decision-making power has a significant positive impact on attending the continuum of maternal care [23].
Despite the advantages of decision-making on the utilization of family planning in developing countries, including Ethiopia, there has been insufficient attention to whether decisions are made collaboratively or jointly [24]. In many households, including those in developing countries, the decision-maker for family planning use is often the partner or husband [25]. From clinical experience, women who seek contraceptive services often report opposition from their partners or husbands. This significant influence from husbands can lead to unplanned pregnancies, which frequently result in unsafe abortions—one of the direct causes of maternal mortality [26]. On the other hand, women who cannot make contraceptive decisions either by themselves or jointly with their husbands may resort to using contraceptives secretly. This secrecy can create difficulties in accessing timely consultations from healthcare providers if contraceptive-induced side effects occur [27, 28]. Another issue that arises when there is no joint decision-making process about contraceptive use among couples is that many women in Ethiopia may face challenges in accessing their preferred method. For most women in Ethiopia, the first choice of contraceptive is injectables, as supported by the EDHS 2016 report [29]. From clinical experience, lack of decision-making power is a significant reason why some women opt for injectable contraceptives. Injectables are chosen because they are not visible to their husbands once administered, unlike other methods such as implants or Jadelle, which are preferred less due to their visibility on the arm. This lack of decision-making power indirectly affects women’s health, as injectable contraceptives have higher side effects and may lead to more challenging fertility return compared to implants or Jadelle [30].
This hidden sexual and reproductive health issue can be addressed by fostering a culture of joint decision-making on contraceptive use among couples. Intra-familial decision-making is a crucial determinant for women’s access to maternal health care services, including family planning [31, 32]. From evidences the decision maker at the house hold level for contraceptive use can be women independently, or husband/partner independently, or both women and husband or other relatives [33,34,35]. Most literature indicates that when there is joint decision-making for contraceptive use at the household level, the probability of using contraceptives is higher [36]. There is evidence suggesting that contraceptive use coverage can be significantly improved by cultivating a culture of joint decision-making at the household level [35]. The basic challenge is the involvement of husbands/partners in contraceptive use decision-making. Evidence from sub-Saharan Africa indicates that husbands/partners are often reluctant to participate in these decisions [37]. From clinical experience, when husbands/partners are the primary decision-makers regarding contraceptive use, women may either experience unintended pregnancies or have to use contraceptives secretly. Using contraceptives without the permission of their husbands/partners can lead to several negative consequences. Joint decision-making on family planning involves both the woman and her partner/husband agreeing on aspects such as the choice of contraceptive method, its uptake, and the continuation of use while evaluating any ongoing side effects [35]. This approach is preferred when considering the decision-making process during contraceptive provision, and supportive data are needed to promote it across the population. However, there is limited evidence on joint decision-making for contraceptive use among married reproductive-age women, with most studies focusing on women’s or husbands’ decision-making power independently. Identifying the factors that hinder joint decision-making is crucial for addressing the hidden challenges women face.
Therefore, this study aims to assess the prevalence of joint decision-making on contraceptive use among married reproductive-age women in Ethiopia, using secondary data from the EDHS 2016. The findings of this study can provide valuable insights for program managers involved in contraceptive provision.
Methods
Study design, area and period
This study utilized data from the Ethiopian Demographic and Health Survey (EDHS) 2016, a cross-sectional survey conducted from January 18, 2016, to June 27, 2016. The analysis involved secondary data from the EDHS 2016. Ethiopia, an eastern African country, is known as the second most populous nation in Africa, following Nigeria.
Source population
All married and non-pregnant reproductive-age women in Ethiopia.
Study population
All married and non-pregnant women and contraceptive users during the time of the survey in Ethiopia were the study population in this study.
Sample size determination and sampling procedure
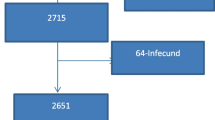
The process for determining the sample size for this study involved several steps: first accessing Data: The first step was to access the EDHS 2016 dataset from the DHS website (http://www.measuredhs.com). Second data Selection: The second step was to select the women’s file (IR) to determine the minimum sample size. Reproductive-age women who were in union, not pregnant, and currently using contraceptives at the time of the survey were included, while other reproductive-age women were excluded using STATA version 14 commands. Third the final sample size was determined by applying the weighting variable (V005) to the IR file dataset. The minimum sample size used for this study was 3,669 married, non-pregnant, and currently contraceptive-using women at the time of the survey.The primary variable for analysis was who makes the decision regarding contraceptive use (V632), which has four possible responses: respondent, husband/partner, joint decision, and other [38]. From the V632 variable, the computed sample size was 3,669. The data collection for the EDHS 2016 used a two-stage stratified sampling technique: First Stage: Enumeration Areas (EAs) were selected. A total of 645 EAs were accessed using a sampling frame from the 2007 population and housing census. EAs were stratified into urban (202 EAs) and rural (443 EAs) before selection. Second Stage: Households were selected using a systematic random sampling technique. A total of 16,650 households were selected, with 12,688 men and the remaining households comprising women.
For additional details about the sampling technique, procedure, and the survey questionnaire, one can refer to the EDHS 2016 report [29].
Study variables
Dependent variable
In this study, joint decision-making on contraceptive use was the outcome variable. It was a categorical variable measured by a yes/no response. Contraceptive-using women were asked whether the decision regarding contraceptive use was made jointly or independently. A “joint decision” was defined as a decision made collaboratively by both the woman and her husband/partner.
Independent variables
Totally 22 individual-level variables( age of women, age of husband, women education, sex of household head, religion, relation to house holed head, exposure to mass media, parity, number of under 5 children in the household, history of pregnancy termination, fertility preference, husband desire for children, information on family planning, visited by a health worker, field worker talk about family planning, visited a health facility, at health facility talk about family planning and distance to reach health facility ) and 4 community-level variables were included in this study.
Data processing and statistical analysis
The data for this study were extracted from the women’s file (IR) dataset of the EDHS 2016 and were recoded to fit the analysis requirements. Descriptive statistics, such as median and proportion, were used for summarizing the data. Binary multilevel logistic regression was used to calculate the COR for all individual-level variables. Variables with a p-value of ≤ 0.2 in the bivariate analysis were considered for the adjusted model. Due to the hierarchical nature of the EDHS data, multilevel logistic regression analysis was performed with four models: Model I (Null Model): This model assessed the cluster-level variance or clustering effect of the outcome variable. Model II: This model identified individual-level variables associated with the outcome variable (joint decision-making on contraceptive use). Model III: This model identified community-level variables associated with the outcome variable. Model IV (Final Model): This model combined both individual and community-level variables to identify those significantly associated with the outcome. An adjusted odds ratio (AOR) with a 95% confidence interval was used to measure the strength and direction of associations, with a p-value of < 0.05 indicating statistical significance.
Intra-Class Correlation Coefficient (ICC): This estimated the percentage of variation due to clustering. The ICC for the null model was 21.3%, indicating that 21.3% of the variability in joint decision-making on contraceptive use was due to cluster-level effects. Median Odds Ratio (MOR): This measure indicates the median value of the odds ratio between the highest and lowest odds ratios for variation in the outcome variable. The MOR for the null model was 2.4 (95% CI: 2.1–2.8). Proportion Change in Variance (PCV): This measures the amount of variation explained by the final model. The PCV for the fourth model was 8%, meaning that only 8% of the variability was explained by the model, while 92% remained unexplained.
[39].
Deviance (-2 log likelihood)
This statistic was used for model comparison. The model with the lowest deviance value was selected for interpreting the findings. Deviance measures how well the model fits the data, with lower values indicating a better fit. [detailed description of variables recording at Table 1].
Results
Socio-demographic characteristics of the study participants
Among the 3,669 married, non-pregnant, and contraceptive-using reproductive-age women: Age Group 20–34 years: 2,412 (66%), Age of Household Head 31–59 years: 2,394 (65%), No Formal Education: 1,948 (53%), Husbands with Primary Education: 1,445 (39%), Female Household Head: 3,274 (89%), Orthodox Religion: 1,877 (51%), Unemployed: 2,308 (63%), Rich: 1,876 (51%), Reside in Rural Areas: 2,806 (76%), Wife of the Household Head: 3,111 (85%), and No Exposure to Newspaper: 3,256 (89%)(Table 2).
Obstetric related characteristics of participants in Ethiopia
Among all participants: Multiparous (having had more than one child): 2,646 (72%), Number of Under-5 Age Children (1 child): 1,803 (49%), No History of Pregnancy Termination: 3,365 (92%) and Fertility Preference for Another Child: 2,059 (56%) (Table 3).
Health care services related characteristics of participants
Among all respondents: Women no Information about Family Planning: 2,396 (65%), Not Visited by Health Workers in the Past 12 Months: 2,397 (65.3%), Visited Health Facility in the Past 12 Months: 2,061 (56%) and Distance to Health Facility a Big Problem: 1,995 (54%) (Table 4).
Prevalence of joint decision on contraceptive use among married reproductive age women in Ethiopia
The prevalence of joint decision on contraceptive use among married reproductive age women in Ethiopia was found to be 78.81%; 95% [71.35-74.23%] (Fig. 1).
Multilevel logistic regression analysis of determinant factors for joint decision making on contraceptive use in Ethiopia, EDHS 2016
In the bivariate multilevel logistic regression analysis, six variables were statistically significant with the outcome variable. In the multivariable multilevel logistic regression analysis, five variables remained statistically significant with joint decision-making on contraceptive use in Ethiopia: Women’s Educational Level, Religion, Wealth Status, Media Exposure and Community Poverty.
In the multivariable multilevel logistic regression analysis, the following factors were significantly associated with joint decision-making on contraceptive use:
Primary Education: 1.5 times more likely to decide jointly (AOR = 1.5; 95% CI: 1.2–1.9) compared to women with no formal education. Secondary Education: 1.9 times more likely to decide jointly (AOR = 1.9; 95% CI: 1.3–2.9) compared to women with no formal education. Higher Education: 2.1 times more likely to decide jointly (AOR = 2.1; 95% CI: 1.2–3.5) compared to women with no formal education. Protestant: 1.7 times more likely to decide jointly (AOR = 1.7; 95% CI: 1.7–2.5) compared to women who are Orthodox. Rich: 1.4 times more likely to decide jointly (AOR = 1.4; 95% CI: 1.1–1.9) compared to women with poor wealth status. With Media Exposure: 1.4 times more likely to decide jointly (AOR = 1.4; 95% CI: 1.1–1.7) compared to women with no media exposure. High Community Poverty: 40% less likely to decide jointly (AOR = 0.6; 95% CI: 0.6–0.9) compared to women in communities with low poverty (Table 5).
Discussion
Joint decision-making on contraceptive use among married reproductive-age women is crucial for reducing maternal mortality in Ethiopia by addressing complications arising from unintended pregnancies [35].
Availability of data on the magnitude of joint decision-making on contraceptive use among married reproductive-age women is essential for guiding the design of new approaches by program managers. The prevalence of joint decision-making in this study is 78.81%, which is higher compared to the 71.6% reported in a study conducted in Mozambique [40], Zambia 65.8% [41] and wolayita sodu 71.4% [42]. The slight difference in the magnitude of joint decision-making on contraceptive use between this study (78.81%) and the study conducted in Mozambique (71.6%) may be attributed to differences in study populations and data sources. In this study, the population was extracted from the EDHS 2016 data, focusing specifically on married, non-pregnant, contraceptive users. In contrast, other studies often used primary data and included all married reproductive-age women, regardless of contraceptive use. This broader denominator could result in a lower prevalence rate compared to the more specific population studied in the current analysis.
The magnitude of joint decision-making on contraceptive use in this study (78.81%) is lower than findings reported in different regions of Ethiopia, 92.4% [24], 83.4% [43], 81% [44], 78% [45].The variation in the magnitude of joint decision-making on contraceptive use might be due to differences in geographical scope and socio-demographic factors. In this study, the prevalence was derived from an aggregate of all regions in Ethiopia, potentially leading to a lower rate compared to studies conducted in specific regions. Additionally, previous studies often focused on urban areas with higher educational attainment and greater exposure to mass media, which can enhance joint decision-making. In contrast, the current study includes both urban and rural participants, where rural areas may have lower educational levels and less media exposure, contributing to the observed lower prevalence.
Women with educational levels of primary, secondary, and higher are 1.2, 1.9, and 2.1 times more likely to jointly decide on contraceptive use with their husbands/partners compared to women with no educational attainment. This association can be explained by the following factors: Increased Persuasion Skills: Higher educational attainment often enhances women’s ability to effectively communicate and persuade their husbands/partners about the benefits of contraceptive use. Informed Partners: Educated women are more likely to have husbands/partners who are also informed about the advantages of contraceptive use, making them more supportive and cooperative. Freedom and Autonomy: Educated couples are generally more open to joint decision-making due to greater awareness and understanding of family planning. Educated husbands/partners are often more supportive of their wives’ health decisions, including contraceptive use. These insights are supported by various studies indicating that higher education levels among women and their partners are associated with increased joint decision-making on maternal health care services, including contraception [24, 31, 32, 46, 47].
Participants who identify as Protestant are 1.7 times more likely to make joint decisions about contraceptive use with their husbands/partners compared to those who identify as Orthodox. This difference may be attributed to religious beliefs, where Orthodox Christianity might view family planning as sinful, leading to resistance from Orthodox husbands/partners. This explanation aligns with evidence showing that religious beliefs can significantly influence contraceptive practices and decision-making in Ethiopia [44, 48, 49].
Women with higher wealth status were 1.4 times more likely to make joint decisions about contraceptive use with their husbands/partners compared to those with lower wealth status. This association might be explained by the greater access that wealthier individuals have to information and resources, including mass media, which can increase awareness and understanding of contraceptive options. Additionally, higher wealth status often correlates with better education and healthcare access, which can further enhance the likelihood of collaborative decision-making regarding contraceptive use [50,51,52]. Another possible explanation could be that women with poorer wealth status often engage in laborious activities, and their husbands may perceive contraceptive use as less favorable due to concerns about its impact on their workload or economic productivity. This perception might lead to less cooperation and reluctance in making joint decisions about contraceptive use. Economic constraints and the physical demands of labor-intensive work can influence attitudes towards family planning and decision-making in ways that differ from those of wealthier individuals.
Participants with media exposure were 1.4 times more likely to make joint decisions about contraceptive use with their husbands/partners compared to those without media exposure. This finding aligns with various studies showing that media exposure positively influences contraceptive use. Media campaigns and information dissemination through television, radio, and other platforms can increase awareness and knowledge about contraceptive options, thereby fostering more informed and collaborative decision-making among couples [50, 51, 53, 54]. [55]; Women living in high community poverty were 40% less likely to make joint decisions with their husbands/partners about contraceptive use compared to those in lower community poverty settings. Poverty can affect contraceptive uptake in several ways: Limited Access to Resources: High poverty can restrict access to healthcare services, including family planning, which might hinder joint decision-making if both partners cannot access or afford the services. Educational Barriers: Communities with high poverty often have lower levels of education, which can affect both partners’ awareness and understanding of contraceptive options and their benefits. This lack of education can lead to less informed decision-making. Cultural and Social Norms: In poorer communities, traditional and cultural norms may be more pronounced, potentially leading to resistance to contraceptive use or joint decision-making. Economic Pressures: Economic constraints can create stress and impact relationships, potentially reducing the likelihood of collaborative decision-making about family planning. These points are supported by existing literature, which highlights how socio-economic factors like poverty can influence both the availability of contraceptive options and the dynamics of decision-making within households [56,57,58].
Conclusions
In Ethiopia, joint decision-making on contraceptive use among married reproductive-age women is prevalent. Factors positively associated with joint decision-making include:
-
Women’s Educational Level: Higher educational attainment (primary, secondary, and higher) is associated with increased likelihood of joint decision-making.
-
Religion: Women identifying as Protestant are more likely to make joint decisions compared to those who are Orthodox.
-
Wealth Status: Women from richer households are more likely to decide jointly with their partners.
-
Media Exposure: Women who have media exposure are more likely to engage in joint decision-making regarding contraceptive use. Conversely, women living in communities with high poverty levels are less likely to make joint decisions about contraceptive use.
The ministry of education should give attention on improving women educational status at national level to increase joint decision for contraceptive use.
Health care providers should give attention for those remote to media exposure at the time of contraceptive provision. Special attention should be given for those women in high community poverty.
Data availability
All out put based data are available within the manuscript and additionally the data set can be accessed from www.measuredhs.com.
Abbreviations
- AOR:
-
Adjusted Odds Ratio
- CI:
-
Confidence Interval
- DHS:
-
Demographic and Health Survey
- EDHS:
-
Ethiopian Demographic and Health Survey
- EAs:
-
Enumeration Areas
- ICC:
-
Intra- Class Correlation Coefficient
- MOR:
-
Median Odds Ratio
- PCV:
-
Proportion Change In variance
- PHC:
-
Population and Housing Census
References
Zimicki S. The relationship between fertility and maternal mortality. Contraceptive Use and Controlled Fertility, Health Issues for Women and Children. 1989.
Birdsall NM, Griffin CC. Fertility and poverty in developing countries. J Policy Model. 1988;10(1):29–55.
DATA S. Population Reference Bureau.
Haub C, Kaneda T. World Population Data Sheet. Population Reference Bureau. Washington, DC, USA. 2013.
Bongaarts J, Cleland JC, Townsend J, Bertrand JT, Gupta MD. Family planning programs for the 21st century: rationale and design. 2012.
Canning D, Schultz TP. The economic consequences of reproductive health and family planning. Lancet. 2012;380(9837):165–71.
Kavanaugh ML, Anderson RM. Contraception and beyond: the health benefits of services provided at family planning centers. New York: Guttmacher Institute; 2013.
Starbird E, Norton M, Marcus R. Investing in family planning: key to achieving the sustainable development goals. Global Health: Sci Pract. 2016;4(2):191–210.
Bongaarts J. Can family planning programs reduce high desired family size in sub-saharan Africa? Int Perspect Sex Reproductive Health. 2011;37(4):209–16.
Worku AG, Tessema GA, Zeleke AA. Trends of modern contraceptive use among young married women based on the 2000, 2005, and 2011 Ethiopian demographic and health surveys: a multivariate decomposition analysis. PLoS ONE. 2015;10(1):e0116525.
Shiferaw S, Abdullah M, Mekonnen Y, Maïga A, Akinyemi A, Amouzou A, et al. Trends in contraceptive use and distribution of births with demographic risk factors in Ethiopia: a sub-national analysis. Global Health Action. 2015;8(1):29720.
Yesuf KA, Muluneh A, Asrese ET. Geographical variation and factor associated with modern contraceptive utilization among Young married women aged between 15–24 years: spatial and multilevel analysis of EDHS 2016. 2020.
Gitobu CM, Gichangi PB, Mwanda WO. The effect of Kenya’s free maternal health care policy on the utilization of health facility delivery services and maternal and neonatal mortality in public health facilities. BMC Pregnancy Childbirth. 2018;18(1):1–11.
Olika AK, Kitila SB, Terfa YB, Olika AK. Contraceptive use among sexually active female adolescents in Ethiopia: trends and determinants from national demographic and health surveys. Reproductive Health. 2021;18(1):1–11.
Zewde B. Women Empowerment in Ethiopia 2020.
Santelli JS, Song X, Garbers S, Sharma V, Viner RM. Global trends in adolescent fertility, 1990–2012, in relation to national wealth, income inequalities, and educational expenditures. J Adolesc Health. 2017;60(2):161–8.
Widmer ED, Ganjour O. Family salience across nations: configurations of morphological conditions. Family Continuity and Change: Springer; 2017. pp. 33–59.
Yesuf KA, Birhanu AY, Nigatu AM. Spatial Distribution and Factors Associated with Unmet Need for Family Planning Among Married Women Aged Between 15–49 Years: Spatial and Multilevel Analysis of EDHS 2016. Available at SSRN 3669133.
Roos N, von Xylander SR. Why do maternal and newborn deaths continue to occur? Best Pract Res Clin Obstet Gynecol. 2016;36:30–44.
Mason KO, editor. editor The impact of women’s social position on fertility in developing countries. Sociological forum. Springer; 1987.
Klima CS. Unintended pregnancy: consequences and solutions for a worldwide problem. J Nurse-Midwifery. 1998;43(6):483–91.
Shifti DM, Chojenta C, Holliday E, Loxton D. Effects of short birth interval on neonatal, infant and under-five child mortality in Ethiopia: a nationally representative observational study using inverse probability of treatment weighting. BMJ open. 2021;11(8):e047892.
Hou X, Ma N. Empowering women: the effect of women’s decision-making power on reproductive health services uptake–Evidence from Pakistan. World Bank Policy Research Working Paper. 2011(5543).
Bogale B, Wondafrash M, Tilahun T, Girma E. Married women’s decision making power on modern contraceptive use in urban and rural southern Ethiopia. BMC Public Health. 2011;11(1):1–7.
Bernasek A, Bajtelsmit VL. Predictors of women’s involvement in household financial decision-making. Financial Couns Plann. 2002;13(2):39–47.
Belton S, Whittaker AM, Barclay L. Maternal mortality, unplanned pregnancy, and unsafe abortion in Timor-Leste: a situational analysis. Alola and UNFPA; 2009.
Forsberg KE, Lassemo R, Lukasse M. Contraceptive consultations: A cross-sectional study of Norwegian women’s experiences and opinions. Eur J Midwifery. 2019;3.
Garrett CC, Vaisey A. ‘Most women really actually do just appreciate being asked’: clinicians’ views on integrating sexual wellbeing into contraceptive care. Cult Health Sex. 2020:1–15.
Csa I. Central statistical agency (CSA)[Ethiopia] and ICF. Ethiopia demographic and health survey, Addis Ababa, Ethiopia and Calverton, Maryland, USA. 2016.
Bahamondes L, Lavín P, Ojeda G, Petta C, Diaz J, Maradiegue E, et al. Return of fertility after discontinuation of the once-a-month injectable contraceptive Cyclofem®. Contraception. 1997;55(5):307–10.
Ghose B, Feng D, Tang S, Yaya S, He Z, Udenigwe O, et al. Women’s decision-making autonomy and utilisation of maternal healthcare services: results from the Bangladesh Demographic and Health Survey. BMJ open. 2017;7(9):e017142.
Ganle JK, Obeng B, Segbefia AY, Mwinyuri V, Yeboah JY, Baatiema L. How intra-familial decision-making affects women’s access to, and use of maternal healthcare services in Ghana: a qualitative study. BMC Pregnancy Childbirth. 2015;15(1):1–17.
Tadesse M, Teklie H, Yazew G, Gebreselassie T. Women’s empowerment as a determinant of contraceptive use in Ethiopia further analysis of the 2011 Ethiopia demographic and health survey. DHS Furth Anal Rep. 2013;82.
Tiruneh FN, Chuang K-Y, Ntenda PA, Chuang Y-C. Factors associated with contraceptive use and intention to use contraceptives among married women in Ethiopia. Women Health. 2016;56(1):1–22.
Eshete A, Adissu Y. Women’s joint decision on contraceptive use in gedeo zone, southern ethiopia: a community based comparative cross-sectional study. International journal of family medicine. 2017;2017.
Lai S-L, Tey N-P. Contraceptive use in Cambodia: does household decision-making power matter? Culture. Health Sexuality. 2020;22(7):778–93.
Vouking MZ, Evina CD, Tadenfok CN. Male involvement in family planning decision making in sub-saharan Africa-what the evidence suggests. Pan Afr Med J. 2014;19.
Croft TN, Marshall AM, Allen CK, Arnold F, Assaf S, Balian S. Guide to DHS statistics. Rockville: ICF. 2018;645.
Asratie MH, Kassie BA, Belay DG. Prevalence of contraceptive non-use due to Husbands/Partners influence among Married women in Ethiopia: a Multilevel Analysis using demographic and health survey 2016 data. Front Reproductive Health. 2022;4.
Mboane R, Bhatta MP. Influence of a husband’s healthcare decision making role on a woman’s intention to use contraceptives among Mozambican women. Reproductive Health. 2015;12(1):1–8.
Mutombo N, Bakibinga P. The effect of joint contraceptive decisions on the use of Injectables, Long-Acting and Permanent methods (ILAPMs) among married female (15–49) contraceptive users in Zambia: a cross-sectional study. Reproductive Health. 2014;11(1):1–8.
Abraham W, Adamu A, Deresse D. The involvement of men in family planning an application of transtheoretical model in Wolaita Soddo Town South Ethiopia. Asian J Med Sci. 2010;2(2):44–50.
Bekele T, Gebremariam A, Tura P. Contraceptive choice and switching pattern among married women in rural community of South East Ethiopia. Family Med Med Sci Res. 2014;3:133.
Tuloro T, Deressa W, Ali A, Davey G. The role of men in contraceptive use and fertility preference in Hossana Town, southern Ethiopia. Ethiop J Health Dev. 2006;20(3).
Bayray A. Assessment of male involvement in family planning use among men in south eastern zone of Tigray, Ethiopia. Sch J Med. 2012;2(2):1–10.
Sultana A. Factors effect on women autonomy and decision-making power within the household in rural communities. J Appl Sci Res. 2011;7(1):18–22.
Hameed W, Azmat SK, Ali M, Sheikh MI, Abbas G, Temmerman M, et al. Women’s empowerment and contraceptive use: the role of independent versus couples’ decision-making, from a lower middle income country perspective. PLoS ONE. 2014;9(8):e104633.
Hill NJ, Siwatu M, Robinson AK. My religion picked my birth control: the influence of religion on contraceptive use. J Relig Health. 2014;53(3):825–33.
Hogan DP, Biratu B. Social identity and community effects on contraceptive use and intentions in southern Ethiopia. Stud Fam Plann. 2004;35(2):79–90.
Haq I, Sakib S, Talukder A. Sociodemographic factors on contraceptive use among ever-married women of reproductive age: evidence from three demographic and health surveys in Bangladesh. Med Sci. 2017;5(4):31.
Kabir A. Determinants of the current use of contraceptive methods in Bangladesh. J Med Sci. 2001;1:296–301.
Osmani AK, Reyer JA, Osmani AR, Hamajima N. Factors influencing contraceptive use among women in Afghanistan: secondary analysis of Afghanistan Health Survey 2012. Nagoya J Med Sci. 2015;77(4):551.
Do M, Hutchinson P, Omoluabi E, Akinyemi A, Akano B. Partner discussion as a mediator of the effects of Mass Media exposure to FP on contraceptive use among young nigerians: evidence from 3 Urban cities. J Health Communication. 2020;25(2):115–25.
Jacobs J, Marino M, Edelman A, Jensen J, Darney B. Mass media exposure and modern contraceptive use among married west African adolescents. Eur J Contracept Reproductive Health Care. 2017;22(6):439–49.
Chaudhry IS, Nosheen F. The determinants of women empowerment in Southern Punjab (Pakistan): an empirical analysis. Eur J Social Sci. 2009;10(2):216–29.
Lakew Y, Reda AA, Tamene H, Benedict S, Deribe K. Geographical variation and factors influencing modern contraceptive use among married women in Ethiopia: evidence from a national population based survey. Reproductive Health. 2013;10(1):1–10.
Alsaleem MA, Khalil SN, Siddiqui AF, Alzahrani MM, Alsaleem SA. Contraceptive use as limiters and spacers among women of reproductive age in southwestern, Saudi Arabia. Saudi Med J. 2018;39(11):1109.
Viswan SP, Ravindran TS, Kandala N-B, Petzold MG, Fonn S. Sexual autonomy and contraceptive use among women in Nigeria: findings from the demographic and health survey data. Int J Women’s Health. 2017;9:581.
Acknowledgements
Our deepest gratitude is goes to the measure DHS program for the permission of access and uses the 2016 EDHS data.
Funding
No, any fund had taken for this research.
Author information
Authors and Affiliations
Contributions
Melaku Hunie Asratie wrote the main manuscriptDaniel Gashaneh Belay and Getayeneh Antehunegn Tesema performed the statistical analysis.All authors reviewed the manuscript and approved the submission.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Since the study was a secondary data analysis of publically available survey data from the measure DHS program, ethical approval and participant consent were not necessary for this particular study. We requested DHS Program and permission was granted to download and use the data for this study from http://www.dhsprogram.com. The Institution Review Board approved procedures for DHS public-use datasets do not in any way allow respondents, households, or sample communities to be identified. There were no names of individuals or household addresses in the data file. The geographic identifiers only go down to the regional level (where regions are typically very large geographical areas encompassing several states/provinces). Each enumeration area (Primary Sampling Unit) has a PSU number in the data file, but the PSU numbers do not have any labels to indicate their names or locations. In surveys that collect GIS coordinates in the field, the coordinates are only for the enumeration area (EA) as a whole, and not for individual households, and the measured coordinates are randomly displaced within a large geographic area so that specific enumeration areas cannot be identified.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding author.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Asratie, M.H., Tesema, G.A. & Belay, D.G. Joint decision on contraceptive use and determinant factors among married women of reproductive ages (15–49) in Ethiopia: a multilevel analysis using Ethiopian Demographic and Health Survey; 2016 data. BMC Public Health 24, 2252 (2024). https://doi.org/10.1186/s12889-024-19715-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19715-z