Abstract
Background
Different evidence suggested that couples often disagree about the desirability of pregnancy and the use of contraceptives. Increased women's decision-making on contraceptives is identified as a key solution that can change the prevailing fertility and contraceptive utilization pattern in SSA. Therefore, this study aimed to determine determinants of contraceptive decision-making among married women in Sub-Saharan Africa.
Methods
The data source of this study was the standard demographic and health survey datasets of 33 Sub-Saharan Africa countries. Reproductive age group women aged (15–49 years) currently married who are not pregnant and are current users of contraceptive preceding three years the survey was included from the individual record (IR file) file between 2010 and 2018. Since the outcome variable is composed of polychotomous categorical having multiple-choice, the Multinomial logistic regression (MNLR) model was applied.
Results
A total of 76,516 married women were included in this study. Maternal age 20–35 and 36–49 years were more likely to had decision making on contraceptive use in both women-only and joint (women and husband/partner category (referance = husband/partner) (RRR = 1.2; 95% CI = 1.05–1.41, RRR = 1.18; 1.04–1.33 and RRR = 1.38; 95% CI = 1.17–1.61, RRR = 1.27; 1.11–1.47)] respectively. Married women with higher education were more likely to decide by women-only category on contraceptive use (referance = husband/partner) (RRR = 1.26; 95% CI = 1.06–1.49). Women only decision-making to use contraceptives relative to the husband/partner only decreases by a factor of 0.86 (95% CI = 0.80–0.93) among rural than urban residences. Women only or joint decision making to use contraceptives was 1.25 and 1.35 times more likely relative to husband/partner decision making respectively among women who had work than that of had no work. The relative risk of women's decision to use family planning relative to husband increased among couples who had a marital duration of ≥ 10 years (RRR = 1.14; 95% CI = 1.06–1.22). But it has no significant effect on joint decision making. Respondents found in the richest wealth index category increase the relative risk of joint decision-making relative to husband/partner (RRR = 1.33; 95% CI = 1.20–1.47) compared to the poorest category.
Conclusions
Decision-making to use contraceptives among married women varies greatly by socio-demographic characteristics. The finding of this study showed that women's age, women educational status, residence, duration of the marriage, family economy, and country income were significantly associated with contraceptive decision-making. Therefore to promote ideal family planning decision making, there is a need to formulate policies and design programs that target women's socio-demographic characteristics and modern contraceptive interventions should be promoted by considering empowering women on decision making.
Similar content being viewed by others
Background
Family planning is a foremost concern for many developing countries where poor perinatal, intra-natal, postnatal, and child health care services are practiced [1]. The number of children the couples want to have vicissitudes over time [2]. All most all the countries where the fertility rate exceeds five children per woman are in Sub-Saharan Africa (SSA) [3,4,5,6]. In the late 1990s, the total fertility rate reached below the replacement level (1.7 per woman) in Europe, northern America, and Australia, consequently, Japan reached below the replacement level in the late 1950s and it has declined further [7, 8]. Increasing women’s decision-making is documented as an important solution that can change prevailing fertility and contraceptive use pattern in SSA [9,10,11,12]. Different evidence strongly affirmed that women who are actively involved in household decision-making can control their fertility through the adoption of modern contraception [13].
The Decision-making power of women in family planning is defined as a woman's capability to freely decide independently or discuss with their partner about family planning needs and choices [14]. Contraceptive utilization is commonly compromised by power dynamics between women and her partner as well as those perpetrated by society [9, 15,16,17]. Decisions about contraceptive use and childbearing may be confounded by unequal power relations [16]. Where couples disagree on fertility preferences or desires, men’s power in a relationship may contribute to greater unmet need and contraception allows women to reduce unwanted, unplanned pregnancies and unsafe abortions [15]. Women have been playing a great role, not only in the enhancement of family well-being but also in the progress of the financial, political social, and ecological atmosphere [18]. Despite the influence that partners may have on decisions, women commonly use family planning covertly, indicating that men and women do not always make decisions as a unit; instead, some women make decisions individually [16, 19].
Women's general participation in decision-making is an important factor in increasing the use of contraceptives [14]. In SSA secret use of contraceptives among women accounts for between 6 and 20% of all contraceptive use [20, 21]. A short interpregnancy interval put endangers the new baby, mother, and previous child [17, 22] (15—2,3). According to the 2015 Global Report, the proportion of reproductive age group women who were married or living in union and used modern contraceptive methods were 57.4% globally, 86% in East Asia, 72% in Latin America, and the Caribbean, 28.5% in Africa and not greater than 22% in SSA [23, 24].
Worldwide, in 2019, 50% of all women of the reproductive age were using some form of contraceptive however, in the same year, Sub-Sahara Africa uses some forms of contraceptive were only 29% [25]. Due to the minimal utilization of contraceptives in Africa, particularly in SSA, women are exposed to unintended pregnancy and as WHO recently reported, around 40% of pregnancy was unplanned [23, 26]. High fertility poses health risks for mothers, children, substantially slow economic growth, and exacerbates environmental degradation [27,28,29,30]. As the fertility rate remains high, the youth dependency ratio also increases exponentially [23].
In low and middle-income countries particularly in SSA, continued rapid population growth presents a challenge for achieving sustainable development [25]. Research shows that couples often disagree about the desirability of pregnancy and the use of contraceptives [31]. Therefore, the objective of this study was to assess determinants of contraceptive decision-maker among couples in Sub-Saharan Africa.
Methods
Data sources
The study made use of pooled data from current Demographic and Health Surveys (DHS) conducted from 2010 to 2018 among 33 Sub-Saharan Africa countries.. These 33 countries were included in the study because they had current DHS data and also all the variables of interest for this study. Our study included these 33 countries under the DHS program to provide holistic and in-depth evidence of women contraceptive decision making in SSA.
The DHS Program has been working with developing countries around the world to collect data about significant health issues including fertility. This standard Demographic and Health Survey is a population-based survey, nationally representative, contains high-quality data that follow standardized data collection procedures, have consistent content over time, and is collected through uniform questionnaires.
The survey target groups were women aged 15–49 and men aged 15–59 in randomly selected households in each country with a multi-stage stratified cluster sampling design for each country. The study involved a cluster sampling process (i.e. enumeration areas [EAs]), followed by systematic household sampling within the selected EAs. The sample frame usually excludes nomadic and institutional groups such as prisoners and hotel occupants. Detailed information was collected on the background characteristics of the respondents including maternal health and child health [32]. The data for this study were extracted from the individual record (IR file) file from the standard DHS dataset of Sub-Saharan Africa countries with at least one survey from 2010 -2018. A total of 76,516 currently married women who are not pregnant and are current users of family planning were included from 18 low income, 11 lower middle income and 4 upper-middle-income Sub-Saharan countries (11 East African, 6 Central African, 13 West African, and 3 South African countries).
Eligibility identification
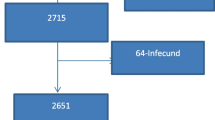
Reproductive age group women aged (15–49 years) currently married women who are not pregnant and are current users of family planning preceding three years the survey in the selected enumeration areas in 33 Sub-Saharan African countries included for this study. Whereas, countries (Central Africa Republic, Eswatini, Sao Tome Principe, Madagascar, and Sudan) did not have a DHS survey report after the 2010/2011 survey year were excluded. As well, three Sub-Saharan Countries (Botswana, Mauritania, and Eritrea) were excluded due to the dataset was not freely available. The outcome variable of this study was the decision-maker to use contraceptives.
Dependent variables
The dependent variable had three (3) categories namely: the women-only decision making (coded as 1), joint (mother and husband/partner) decision making (coded as 2), and husband/partner-only decision making on contraceptive utilization (coded as 3).
Statistical analysis
The analysis began with the computation of contraceptive decision-making among married women from 33 Sub Sharan Africa countries. Secondly, we appended the dataset and this generated a total sample of 76,516. After appending, we compute v005/1,000,000 (Women’s individual sample weight/1,000,000) to develop weighted country-based and socio-demographic characteristics (Tables 1, 2).
Multinomial logistic regression (MNLR) model is generally applicable when the outcome variable is composed of polychotomous categorical having multiple choice. It is a simple extension of logistic regression that allows each category of unordered responsive variables to be compared to an arbitrary references category providing several logit regression models.
Multinomial logistic regression models are equivalent to simultaneous estimation of multiple logits where each of the categories is compared to one selected based category.
Let Yi1be 1 if the ith decision-maker is manly women-only and 0 otherwise. Similarly, Yi2 be 1 if the ith decision-maker is jointly(women/husband/partner and 0 otherwise. Yi3 be 1 if the ith decision-maker is manly husband/partner and 0 otherwise.
All variables included in bivariate analysis were analyzed in the multinomial logit model. A multinomial logistic regression model was used to estimate variations in the probability of decision-makers to use contraceptives. When using multinomial logistic regression, the relative risk ratios were determined for all independent variables for each category of the dependent variable except the reference category, which is omitted from the analysis. The regression model was fitted to the data to explore the association between a set of independent variables explaining the likelihood of decision making on contraceptive a woman decision making on contraceptive as opposed to being in all other categories. The form of the equation fitted to the data was as follows:
A dependent variable (contraceptive decision-making) that had 3 categories, is represented by m in the equation above, and this requires the calculations for (m-1) equations, one for each category relative to the reference category to describe the likelihood of contraceptive decision making and the independent variables. For the women-only category of the dependent variable, for example, the following equation derived from the latter is then estimated:
In the multinomial logistic regression, the husband-only is the comparison category. The model parameter estimates and the attendant Relative Risk Ratios (RRR) for the multinomial logit model is that for a unit change in the predictor variable, the logit of outcome m relative to the reference group is expected to change by its respective parameter estimate given that the variables in the model are held constant. The RRRs can be obtained by exponentiation of the multinomial logit coefficients (\({e}^{\mathbf{c}\mathbf{o}\mathbf{e}\mathbf{f}\mathbf{f}\mathbf{i}\mathbf{c}\mathbf{e}\mathbf{n}\mathbf{t}}\)), or by specifying the rrr option. The alpha threshold for significant results was set at p = 0.05 (95%).
Results
Weighted and unweighted samples in SSA using the recent Demographic and Health Survey data
Thirty-three(33) SSA countries were included in this study. More than half 42,304 (55.23%) of the respondents were found in the East Africa region with greater than one in ten 9,286 (12.14%) respondents being concentrated in Malawi. Whereas greater than one forth 196, 56 (25.7%) of the participants were found in the West African region with around one in 24 (5.83%) concentrated in Nigeria (Table 1).
Descriptive characteristics
Around two-third 49,383 (64.5%) of the married women were found in the age category of 20–35 years. Greater than half 46,052 (58.2%) of the married women live in rural areas. There is a somewhat uniform distribution of wealth index. Around three fourth of the respondents were engaged to work and, about half of them belong to the household member of less than six. Three in five 47,361 (61.7%) of the married women were living in a low-income country. About 58.2% of the respondents were from the East Africa Sub-region of SSA. Finally, around two-third (66%) of decision-makers to use contraceptives were jointly (both mother and husband/partner) (Table 2).
Bivariate analysis
Table 3 shows the bivariate relationship between some selected explanatory variables. Current maternal age, residence, maternal occupation, duration of the marriage, economic status of the family, and country were significantly associated (p < 0.05) with the outcome variable (Table 3).
Multivariate results
Table 4 represents the results of multinomial regression procedures. Maternal age significantly influenced contraceptive decision-making by women-only and jointly (mother and husband). Maternal age 20–35 and 36–49 years increase the relative risk of contraceptive decision making in both mothers only and joint category (relative to the risk husband category) (RRR = 1.22; 95% CI = 1.06–1.41, RRR = 1.18; 1.04–1.33 and RRR = 1.38; 95% CI = 1.18–1.62, RRR = 1.27; 1.11–1.47)] respectively.
Holding other variables constant, having higher maternal education increases the relative risk of contraceptive decision-making among mother only category (RRR = 1.26; 95% CI = 1.06–1.50). However in the joint category the relative risk of deciding to use family planning increases starting from primary education up to higher education. The relative risk of women deciding to use contraceptives relative to husbands decreased by a factor of 0.86 (95% CI = 0.80–0.93) among rural residences than urban. However, the relative risk of joint decision to use family planning relative to husband increase by a factor of 1.08; 95% CI = 1.01–1.16) among rural inhabitants as compared to urban. The relative risk of women or joint decision to use family planning relative to husband decision making power category was 1.25 and 1.35 times that of had no work respectively.
The relative risk of women deciding to use contraceptives relative to the husband only increase among couples who had a marital duration of ≥ 10 years (RRR = 1.14; 95% CI = 1.06–1.22). But it has no significant effect in jointly decision-making to use family planning. The richer and the richest family were at a greater risk of falling into the women decide to use family planning category and at less risk of falling into the husband category than the poorest (RRR = 1.10; 95% CI = 1.01–1.21 and RRR = 1.28; 95% CI = 1.14–1.43) respectively.
However keep other variables constant, married women found in the richest wealth index category increase the relative risk of joint decision to use family planning relative to husband (RRR = 1.33; 95% CI = 1.20–1.47) compared to poorest. The relative risk of women and joint decision to use family planning relative to the husband only increase by a factor of 1.83 (95% CI = 1.57–2.12) and 0.68 (95% CI = 0.59–0.79) respectively among respondents found in upper-middle-income countries.
Discussion
Gender-based power inequalities can contribute to poor health outcomes, for example, hindering communication between partners about reproductive health decision making, constraining women to access to reproductive health survises and by women's and men's attainment to sexual health and pleasure [33]. Throughout resource constraint countries, a considerable proportion of women who do not want to become pregnant were not using contraception. The reason for this “unmet need” for contraception could be women facing multiple barriers to using contraception.
Similarly, in some regions of Africa, there are also noticeable differences.
Although women's empowerment is a key to using contraceptives [19], most partners give the inferior position to women in all aspects of decision-making in developing countries [34]. Besides, little is known about determinants to decision-making to use contraceptives among married women in Sub-Sahara African countries. This study found out that the maternal age group from 20–35 and 36–49 years were significantly more likely to decide for using contraceptives by mothers only and joint (mother and husband/partner) compared to age less than 20 years. This finding affirmed the study was done in [35,36,37,38] that showed women with increasing age tend to be gate higher decision-making power for using contraception.
Women with higher education were significantly more likely to have contraceptive decision-making by mothers only compared to those who had no education. However joint (mother and husband/partner decision-making power for using contraceptives were significantly more likely among women who attended primary, secondary and higher education compared that of non-educated. This is consistent with the previous studies [36, 39].
The possible justification is, education empowers women to be independent and equips them with the essential information that may important for deciding their reproductive health issues. In addition, educated women were undergone collective decision-making with their husbands regarding their health care, child health care, and visiting family members or relatives which is important to share experiences and exercise their human and reproductive rights. Studies suggested that greater gender equality may encourage women's autonomy and may facilitate the uptake of contraceptives because of increased female participation in decision-making power [40].
Women only decision making to use contraceptives relative to husband/parent only decision-making power decrease among rural residences than urban counterparts. However, jointly decision making to use contraceptives relative to husband/partner only decision-making increase among rural inhabitants as compared to urban. Studies suggested that geographic variation in the utilization of family planning methods is influenced by several factors like cultural beliefs such as values attached to male dominancy [41] and the presence and quality of reproductive health survises [42]. Similar evidence has been reported from Hundurance [43] and the study conducted in [44] showed that urban women were more likely to make the decision on contraceptive use than rural inhabitants. The possible justification could be urban societies are egalitarian and in contrast, rural societies are patriarchal.
So in a patriarchal society, the majority of the decision including contraceptive utilization has been taken by a husband due to women's economic dependency and existing non-beneficiary traditional culture, however, a joint decision is also practiced in this community instead of mather alone. This study demonstrated that women who had been in marital union for ten or more years were more likely to have women-only decision-making to use contraceptives (relative to the husband-only decision-making power) as compared to those who had been in marital union for less than ten years. This was consistent with a study conducted in [45, 46]. This might be due to the time that partners have spent together has been shown to correlate with marital satisfaction, increase effective communication in marriage often remains impressive, and develop conflict resolution strategies.
Constraint economic resources can inhibit the ability of women to decide on their human and reproductive rights including contraceptive decision-making. likewise in this study, the richer and richest households increase the likelihood of women-only decision-making to use contraceptives (relative to husbands/ partner decision making as compared to those who found in the poorest wealth classification. Similarly, women found in the richest households were had an increased relative risk of joint decision-making to use family planning (relative to husband /partner only decision making to use family planning) compared to the poorest household wealth status.
Inadation women live in the upper-middle-income country increase the likelihood of women decision making to use family planning in relative husband only decision making power as compared to the low-income country. However, the couple's found in upper-middle-income countries decrease the likelihood of joint decision-making to use family planning relative to the husband only compared to in low middle-income countries. Because development and poverty are the most determinants of human and reproductive rights including reproductive decision-making power. Apart from this numerous cultural practices regarding reproductive health decision-making power are associated with countries' development [47] and a challenge for the economy and even political growth. Evidence also supports this finding that women's ability to make household decision-making is enhanced while they are working. Their economic condition stops them from making or even daily household purchases.
The relation between women's empowerment and autonomy in decision-making appears straightforward. Women who had worked were significantly more likely to report to participate in the decision-making process compared to those women who had not been exposed to work [48]. Partner involvement in obstetric decision-making improves the uptake of maternal health services. In addition, in this study, the overall estimate of decision-making to use contraceptives for women only, husband/partner only, and joint (women and spouse) were 24.36%, 9.6%, and 66.04% respectively. A study conducted in Senegal showed that only 6.26% of women have the opportunity to decide on their health. In contrast, 80.33% and 9.66% of their health decider were husband/ partner and jointly respectively [49]. Elsewhere, in several developing countries, studies have shown how certain cultural norms affect women's autonomy in deciding their health [50].
Conclusions
decision making to use contraceptives among women varies greatly by demographic and socio-economic characteristics. The finding of this study showed that maternal age, maternal educational status, residence, duration of the marriage, family economic status, and country income were significantly associated with contraceptive decision making. Therefore, to promote ideal contraceptive decision making, there is a need to formulate policies and design programs that target women with low education, and Earlier marital age. Attention should be paid to women found in low-income families and low-income countries. Modern contraceptive interventions should be promoted by considering empowering women in decision-making.
Limitation
There may be threats of internal and external validity because some of the observations were dropped during data cleaning since the study considered currently married women who are not pregnant and are current users of family planning. Therefore the study may be suffered from selection bias. Caution is needed while generalizing this study since it focused on only currently married women who are not pregnant and are current users of family planning. Nevertheless, since we were used the national representative dataset in SSA, the finding could be a true representative for this group of women.
Availability of data and materials
All the data sets are available on the hand of the corresponding author.
Abbreviations
- DHS:
-
Demographic and Health Survey
- MNLR:
-
Multinomial logistic regression
- RRR:
-
Relative risk ratio
- SSA:
-
Sub Saharan Africa
- WHO:
-
World Health Organization
References
United Nations Department of Economic and Social Affairs, Population Division (2019). World Population Prospects 2019.
Zabin LS, Huggins GR, Emerson MR, Cullins VE. Partner effects on woman’s intention to conceive: “not with this parbrer.” Fam Plann Perspect. 2000;32:39–44.
Wesley Y, Smeltzer SH, Redeker N, Walkeq S, Palumbo P. Reproductive decision making among mothers with HIV-I. Health Care forWomenlnternational. 2000;31(4):291–30.
Moyo W, Mbizvo MT. Desire for a future pregnancy among women from Zimbabwe about their self-perceived risk of HIV infection child mortality spontaneous abortion. 4JD S and Behnaior. 2004;8(1):9-1.
Abbasi-Shavaz MJ. Low fertility in Asia: pathways, consequences and policy implication. UN Expert Group Meeting on Fertility, Changing Population Trends and Development: Challenges and Opportunities New York, 21–22 October 2013.
Rammohan A. Fertility transition in South and Southeast Asia. ASEAN Econ Bull. 2004;21(2):183–97.
Bongaarts and Casterline: Fertility transition: is sub-Saharan Africa different? NIH Public Access, Popul Dev Rev. 2013;38(Suppl 1):153–68.
Bongaarts J, Feeney G. On the quantum and tempo of fertility. Popul Dev Rev. 1998;24(2):271–91.
Mbacké C. The persistence of high fertility in sub-Saharan Africa: a comment. Popul Dev Rev. 2017;43:330–7.
Mokomane Z. Work-family interface in sub-Saharan Africa: challenges and responses. Berlin: Springer; 2013.
Upadhyay UD, Karasek D. Women’s empowerment, and ideal family size: an examination of DHS empowerment measures in sub-Saharan Africa. Int Perspect Sex R H. 2012;38(2):78–89.
Miedema SS, Haardörfer R, Girard AW, Yount KM. Women’s empowerment in East Africa: development of a cross-country comparable measure. World Dev. 2018;110:453–64.
Hogan DP, Beranhu B, Hailemariam A. Household organization, women’s autonomy, and contraceptive behavior in southern Ethiopia. Stud Fam Plann. 1999;30(4):302–14.
Eshete A, Adissu Y. Women’s joint decision on contraceptive use in Gedeo zone, Southern Ethiopia: a community-based comparative cross-sectional study. Int J Family Med. 2017;2017:9.
World Health Organization. WHO| family planning/contraception: fact sheet No 351; 2015. Accessed 26 Dec 2016.
Malhotra A, Schuler SR, Boender C. Measuring women’s empowerment as a variable in international development, Washington, DC: World Bank, June 28, 2002. network/hdr_net/GDI_GEM_Measuring_Womens_Empowerment.pdf. Accessed 15 May 2012.
Sedgh G, Hussain R. Reasons for contraceptive nonuse among women having an unmet need for contraception in developing countries. Stud Fam Plann. 2014;45(2):151–69.
Rezapour Z, Ansari H. Studying the factors associated with women’s participation in family decision-making (Case study: northern Khorasan, Iran). Eur J Exp Biol. 2014;4(1):553–6.
Do M, Kurimoto N. Women's empowerment and choice of contraceptive methods in selected African countries. Int Perspect Sex Reprod Health. 2012:23–33.
Biddlecom E, Bolaji F. Covert contraceptive use: prevalence, motivations, and consequences. Stud Fam Plan. 1998;29:360–72.
Department of Health, Medical Research Council, OrcMacro: South Africa Demographic and Health Survey 2003. Pretoria; 2007.
CSA-Ethiopia ICF. Ethiopia Demographic and Health Survey 2011. Central Statistical Agency of Ethiopia and ICF International Addis Ababa, Maryland, USA Ethiopia and Calverton, 2012.
Canning D, Raja S, Yazbeck AS. Africa's demographic transition: dividend or disaster? https://openknowledge.worldbank.org/handle/10986/22036. Accessed 05 Dec 2018.
Bearak J, Popinchalk A, Alkema L, Sedgh G. Global, regional, and subregional trends in unintended pregnancy and its outcomes from 1990 to 2014: estimates from a Bayesian hierarchical model. Lancet Glob Health. 2018;6(4):e380–9.
United Nation, Department of Economics, World Fertility and Family Planning. 2020, Highlights.
Chola L, et al. Cost and impact of scaling up interventions to save the lives of mothers and children: taking South Africa closer to MDGs 4 and 5. Glob Health Action. 2015;8:27265.
Bulatao RA, Lee RD, editors. Determinants of fertility in developing countries. New York: Academic Press; 1983. p. 1–2.
Caldwell JC. Theory of fertility decline. New York: Academic Press; 1982.
Easterlin R. An economic framework for fertility analysis. Stud Fam Plann. 1975;6(3):54–63.
Notestein FW. Economic problems of population change. In Proceedings of the eighth international conference of agricultural economics. London: Oxford University Press; 1953. p. 13–31.
Blackstone SR, Iwelunmor J. Determinants of contraceptive use among Nigerian couples: evidence from 2013 Demographic and Health Survey. Contracep Reprod Med. 2017;2(9):1–8.
The DHS Program. [Cited]. http://dhsprogram.com/.data/data-collection.cfm.
Speizer AIS, Carter LWM. Gender relations and reproductive decision making in honduras. Int Fam Plan Perspect. 2005;31(3):131–9.
Bourey C, Stephenson R, Bartel D, Rubardt M. Pile sorting innovations: exploring gender norms, power, and equity in sub-Saharan Africa. Glob Public Health. 2012;7(9):995–1008.
Hameed W, Azmat SK, Ali M, Shelkh MI, Abbas G, Temmerman M, et al. Women’s empowerment and contraceptive use: the role of independent versus couples’ decision-making, from a lower middle income country perspective. PLoS ONE. 2014;9(8):e104633.
Darteh EK, Doku DT, Esia-Donkoh K. Reproductive health decision making among Ghanaian women. Reprod Health. 2014;11:1–8.
Tadesse SY, AragawEmiru A, Tafere aE, Asresie MB. Women’s autonomy decision making power on postpartum modern contraceptive use and associated factors in North West Ethiopia. Hindawi Adv Public Health. 2019;Article ID 1861570.
Darteh EK, Doku DT, Esia-Donkoh K. Reproductive health decision-making among Ghanaian women. Reprod Health. 2014;11:1–8.
Sujatha DS, Reddy GB. Women’s education, autonomy, and fertility behaviour. Asia Pac J Soc Sci. 2009;1(1):35–50.
Hakim A, Salway S, Mumtaz Z. Women’s autonomy and uptake of contraception in Pakistan. Asia Pac Popul J. 2003;18(1):63–82.
Ntozi J. High fertility in rural Uganda. Kampala: Fountain Publishers; 1995.
Tsui AO, Ochoa LH. The role of family planning programs as a fertility determinant. In: Ross JPJ, editor. Service proximity as a determinant of contraceptive behavior: evidence from cross-National Studies of survey data. London: Oxford University Press; 1992.
Ilene S, Lisa C. Gender relations and reproductive decision making in honduras. Int Fam Plan Perspect. 2005;31:131–9.
Bogale B, Wondafrash M, Tilahun T, Girma E. Married women’s decision-making power on modern contraceptive use in urban and rural southern Ethiopia. BMC Public Health. 2011;11:1–7.
Tadele A, Tesfay A, Kebede A. Factors influencing decision-making power regarding reproductive health and rights among married women in Mettu rural district, south-west, Ethiopia. Reprod Health. 2019;16:1–9.
Upadhyay UD, Karasek D. Women’s empowerment and ideal family size: an examination of dhs empowerment measures in Sub-Saharan Africa. Int Perspect Sex Reprod Health. 2012;38(2):78–89.
Ghana Statistical Service (GSS), Ghana Health Service (GHS), and ICF Macro: Ghana Demographic and Health Survey 2008. Accra, Ghana: GSS, GHS, and ICF Macro; 2009.
Bogale B, Wondafrash M, Tilahun T, Girma E. Married women’s decision-making power on modern contraceptive use in urban and rural southern Ethiopia. BMC Public Health. 2011;11:342.
Sougou NM, Bassoum O, Faye A, Leye MMM. Women’s autonomy in health decisionmaking and its effect on access to family planning services in Senegal in 2017: a propensity score analysis. BMC Public Health. 2020;20:1–9.
Singh SK, Sharma B, Vishwakarma D, Yadav G, Srivastava S, Maharana B. Women’s empowerment and use of contraception in India: macro and micro perspectives emerging from NFHS-4 (2015–16). Sex Reprod Healthc Off J Swed Assoc Midwives. 2019;19:15–23.
Acknowledgements
Our deepest gratitude goes to the Demographic and Health Survey (DHS) data archivist that allows accessing the dataset.
Funding
No fund was accepted from any organization for this research.
Author information
Authors and Affiliations
Contributions
All stated authors DT, SAT, MMA, AD, MT, MT, TSD, and BK were involved in this study from the inception to design, acquisition, analysis, and interpretation of data and drafting of the manuscript. All authors agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The World Medical Association Declaration of Helsinki guidance was followed in designing and conducting this study. We obtained ethical clearance from Debre Tabor University research and ethical review committee (approval number: DTU/678/ June 29/2020). Waiver of written informed consent on January 13, 2020, was secured from the International Review Board of Demographic and Health Surveys (DHS) program data archivists to download the dataset for this study. The dataset was not shared or passed on to other bodies. The requested data were treated strictly confidential and were used only for the study purpose. No attempt was done to interact with any individual respondent or household included in the survey. Complete information regarding the ethical issue was available in the DHS report.
Consent for publication
Not applicable for this section.
Competing interests
We declare that there is no competing interest with anyone else.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tesfa, D., Tiruneh, S.A., Azanaw, M.M. et al. Determinants of contraceptive decision making among married women in Sub-Saharan Africa from the recent Demographic and Health Survey data. BMC Women's Health 22, 52 (2022). https://doi.org/10.1186/s12905-022-01636-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-022-01636-x