Abstract
Background
Many married women of reproductive age with husbands or partners are less cooperative in using contraceptives, often resulting in unintended pregnancies or secret contraceptive use. This private use of contraceptives causes women to suffer from side effects without proper support, and many women in Ethiopia die due to unintended pregnancies. However, the involvement of husbands or partners in the contraceptive decision-making process in Ethiopia is often neglected. There is also a lack of evidence regarding the determinants of husbands’ or partners’ decision-making power on contraceptive use in Ethiopia.
Objective
This study aimed to assess the determinants of low involvement of husbands/partners in women’s contraceptive use decision-making processes in Ethiopia.
Methods
This study was based on Ethiopian Demographic and Health Survey data, collected from January 18 to June 27, 2016. Weighted samples of 3,669 reproductive-age women were included. Husbands’/partners’ independent decision-making was measured by whether the husband/partner decided independently or alone about contraceptive use, categorized as “Yes” or “No”. A multilevel logistic regression model was fitted, and ICC (Intra-class Correlation Coefficient), MOR (Median Odds Ratio), PCV (Proportion Change in Variance), and deviance were used to assess model fitness and comparison. Variables with a p-value of ≤ 0.2 in the bivariate analysis were considered candidates for multivariable multilevel analysis. An adjusted odds ratio with a 95% confidence interval was used to determine both the direction and strength of the association, and a p-value of < 0.05 was used to declare statistical significance.
Results
Husbands’/partners’ independent decision-making in women’s contraceptive use was found to be 5.41% [4.72-6.19%]. Significant factors associated with this included: Husbands/partners aged 31–59 years (Adjusted Odds Ratio (AOR) = 1.3; Confidence Interval (CI) 2.3–5.4) and over 59 years (AOR = 2.3; CI 1.2–4.3), Educational level of husbands/partners: primary education (AOR = 3.2; CI 2.9–4.3), secondary education (AOR = 3.9; CI 2.7–4.4), and higher education (AOR = 4.3; CI 2.8-5.0), Media exposure (AOR = 4.5; CI 2.2–5.4), History of pregnancy termination (AOR = 3.3; CI 2.6–4.1), Perception that distance to health facilities is not a significant problem (AOR = 3.0; CI 1.7–4.7) and Urban residency (AOR = 3.5; CI 1.6–4.2).
Conclusions
In Ethiopia, the involvement of husbands/partners in the contraceptive use decision-making process is low. To increase their decision-making power, attention should be given to factors such as age, educational level, media exposure, history of pregnancy termination, distance to health facilities, and urban residency.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Family planning provision plays a crucial role in improving economic status, increasing the proportion of educated women, and reducing under-five mortality and maternal deaths related to pregnancy and childbirth. [1,2,3,4,5]. The Sustainable Development Goals (SDGs) critically emphasize eradicating extreme poverty and hunger, achieving universal primary education, promoting gender equality and women’s empowerment, reducing under-five mortality by two-thirds, and reducing maternal deaths related to childbirth by three-quarters by 2030 [6]. Unless we improve the strategies and approaches for the provision of family planning, it will be difficult to achieve all the Sustainable Development Goals by the current timeline [7]. Recently published evidence shows that Sustainable Development Goals, particularly those related to fertility, maternal, and child health, are pressing concerns for developing countries. These goals require attention at three levels: community, household, and health facility [7, 8].
Despite some improvements in the modern contraceptive prevalence rate—rising from 6% in 2000 to 35% by 2016—there remains a significant burden of unmet needs in Ethiopia [9, 10]. In particular, the unmet need for postpartum family planning is pervasive [11], It is an underlying cause of maternal, neonatal, child, and adolescent deaths [12,13,14] and the challenge to achieve the sustainable development goal [15].
Therefore, maintaining a focus on contraceptive use is crucial for achieving the Sustainable Development Goal related to reducing maternal mortality from unsafe abortion and preventing neonatal and child deaths resulting from maternal mortality [16, 17]. One key area that needs attention to increase contraceptive use and reduce unmet needs is cultivating a culture of husbands’/partners’ involvement in women’s contraceptive decision-making at the community, household, and health facility levels [18, 19]. Importantly, the World Health Organization (WHO, 2016) universally recommends the involvement of supportive husbands/partners in maternal healthcare services, including postpartum contraceptive use [20]. Additionally, in developing countries, women’s decision-making power regarding contraceptive use is often constrained by the disapproval or lack of support from their husbands/partners [21]. Unfortunately, one out of ten married women in Ethiopia who do not use contraceptives reported that their reason for not using them was the influence of their husbands/partners [22]. In the patriarchal societies of Ethiopia, married women of reproductive age are often pressured to have more children against their will due to the influence of their husbands/partners. This exploitation contributes to high rates of maternal and neonatal deaths today, often due to complications from short birth intervals and adverse pregnancy outcomes [23, 24]. The magnitude of short interbirth intervals in Ethiopia is high [25, 26], Additionally, Ethiopia faces a high maternal mortality ratio of 412 per 100,000 live births and a high neonatal mortality rate of 49 per 1,000 live births [9]. According to a World Health Organization report, a woman in a developing country dies every 8 min due to complications from unsafe abortion [27].
When husbands/partners are less cooperative in the contraceptive decision-making process, their wives may resort to using contraceptives secretly [22]. Studies have shown that secret use of contraceptives ranges from 6–20% [28]. Among married women of reproductive age, secret contraceptive use is a serious but often neglected issue. It affects the choice of contraceptive methods, follow-up for side effects, and can lead to complications related to workload. Various studies highlight the negative impacts of secret contraceptive use due to a lack of cooperation from husbands/partners. [29].
In general, both the direct and indirect consequences of limited husbands’/partners’ involvement in women’s contraceptive decision-making can be mitigated by identifying and addressing the prohibiting factors within the scientific community.
For achieving the desired family size and delaying the age of reproduction, cultural factors play a significant role. The philosophy of modern family planning advocates that children should be born by choice rather than by chance. However, many people still adhere to the opposite belief—that children are to be born by chance [30]. Primarily, sociocultural factors are the most significantly associated with husbands’/partners’ involvement in women’s contraceptive decision-making processes in low- and middle-income countries [31, 32].
To address this issue effectively, data is needed to illustrate the low involvement of husbands/partners in women’s contraceptive decision-making and to identify the major determinant factors at the community, household, individual, and health facility levels. While various studies have explored women’s decision-making power regarding contraceptive use, comprehensive data on these factors is still required [21, 33, 34]. In Ethiopia, there is a lack of evidence regarding husbands’/partners’ decision-making power in women’s contraceptive use and the associated factors. Therefore, this study aims to assess the determinants—both individual-level and community-level factors—that contribute to the low involvement of husbands/partners in women’s contraceptive decision-making process. In this study, an independent decision-maker is defined as the husband/partner alone in the context of women’s contraceptive use. Ensuring husbands’/partners’ cooperation in contraceptive decision-making is crucial for reducing maternal and neonatal mortality associated with high fertility rates, unintended pregnancies, and unsafe abortions [35,36,37]. This finding could serve as a landmark for program implementers to take action at the community level. Furthermore, the results of this study could provide a foundation for guiding policymakers in designing innovative approaches to foster the involvement of husbands/partners in women’s contraceptive decision-making process.
Methods
Study design, area and period
The study was conducted using secondary data collected through a cross-sectional survey from January 18, 2016, to June 27, 2016. The data were sourced from the Ethiopian Demographic and Health Survey (EDHS 2016), which covered nine regions (Amhara, Tigray, Oromia, Benishangul-Gumuz, Somali, Harari, Gambella, Southern Nations, Nationalities, and Peoples’ Region (SNNPR), and Afar) as well as two administrative cities (Dire Dawa and Addis Ababa). At the time of the survey, Ethiopia had a total population of 102 million, with 44,339,400 individuals under the age of 14. In 2016, the total fertility rate was 4.46, the prevalence of modern contraceptive use was 36.7%, and the prevalence of unmet needs among married women of reproductive age was 22% [9]. In Ethiopia, family planning services are provided to clients free of charge [38].
Source population
The source population for the study comprised all married women of reproductive age in Ethiopia.
Study population
The study population consisted of all married, non-pregnant women of reproductive age who were using contraceptives at the time of the Ethiopian Demographic and Health Survey 2016.
Data source
The official database of the DHS Program (www.measuredhs.com) was used to access the data. First, the objective of the study was explained, and permission was subsequently requested to utilize the data for the current study.Sample size determination and sampling procedure.
During the Ethiopian Demographic and Health Survey data collection, a two-stage stratified sampling technique was employed, with stratification based on urban and rural areas. In the first stage, 645 enumeration areas (EAs) were selected with probability proportional to the size of the EA, and with independent selection within each sampling stratum. In the second stage, a systematic random sampling technique was used to select households. The sampling procedure is described in detail in the Ethiopian Demographic and Health Survey 2016 report [9].
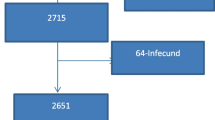
The sample size for this study was determined using the EDHS 2016 data, specifically from the women’s dataset (IR). The final sample size was adjusted using the weighting variable V005. A total weighted sample of 3,669 married, non-pregnant women of reproductive age who were using contraceptives was included in the analysis (Fig. 1).
Study variables
Dependent variable
The outcome variable in this study was measured based on the woman’s self-report regarding who makes the decision about contraceptive use at the time of the survey. The variable of interest was “V632,” which identifies the decision-maker and includes four possible responses: respondent, husband/partner, joint decision, and other [39]. The responses were then dichotomized into “Yes” or “No,” indicating whether husbands/partners are considered independent decision-makers in women’s contraceptive use decision-making process.
Flow of participant selection.
Operational definition
Husbands/partners were categorized as independent decision-makers in women’s contraceptive use decision-making based on the variable V632. The categorization was dichotomized as follows: “mainly respondent, joint decision, and other” were coded as 0 (No), and “mainly husband/partner alone” was coded as 1 (Yes).
Independent variables
All those independent variables were grouped into two major classifications (Socio-demographic factors, and obstetrical and health care service-related factors). During analysis, the age of husbands/partners’, husbands/partners level of education, religion, sex of household head, wealth status, exposure to mass media, history of pregnancy termination, fertility desire, and information on family planning use. All information about independent variables is clearly elaborated in Table 1 (Table 1).
Data processing and statistical analysis [40]
The statistical software STATA version 14 was used to extract and perform both descriptive and analytical analyses. Descriptive statistics, such as median and proportion, were presented as a summary of the data.
Since the EDHS data was collected considering clusters as the study unit, this violated the independence assumption of a standard logistic regression model. Consequently, multilevel logistic regression analysis was employed. First, the intra-class correlation coefficient (ICC) of the null model was calculated to assess the variation in the outcome variable (husbands’/partners’ involvement in contraceptive use decision-making) across different clusters. The ICC was found to be 25.1%, indicating a significant clustering effect that required consideration in the analysis using an advanced statistical model. The median odds ratio (MOR), another indicator of clustering effect, was 2.6 (CI: 2.3–2.9) in the null model [40,41,42].
Fixed effects were used to assess the relationship between the outcome variable and the independent variables. The crude odds ratio (COR) with a 95% confidence interval was employed to measure both the direction and strength of the association. In the bivariate multilevel analysis, variables with a p-value of ≤ 0.2 were selected for inclusion in the adjusted model. Finally, in the multivariable multilevel analysis, the association between the outcome variable and explanatory variables was evaluated using an adjusted odds ratio (AOR) with a 95% confidence interval, and statistical significance was determined at a p-value of < 0.05 [40,41,42].
Random effects (measures of variability) were assessed using the intra-class correlation coefficient (ICC), median odds ratio (MOR), proportion change in variance (PCV), and deviance (-2 log-likelihood ratio) [40,41,42].
Intra-class correlation coefficient (ICC)
The ICC measures the variation in the outcome variable (husbands’/partners’ involvement in contraceptive use decision-making) between clusters. In the null model, the ICC was 25.1%, indicating that, regardless of other factors such as socio-demographic, obstetrical, and healthcare service-related factors, 25.1% of the variation in the outcome variable was attributable to differences between clusters [40,41,42].
Median odds ratio (MOR)
The MOR quantifies the median odds ratio between the highest and lowest odds ratios due to clustering effects, providing an alternative way to express cluster-level variance in terms of odds ratios. In this study, the MOR in the null model was 2.6 (95% CI: 2.3–2.9), indicating a significant clustering effect. It was calculated as follows: MOR = exp. [√ (2xVA) X0.6745], MOR = e0.95√VA where VA = cluster level variance [40,41,42].
Proportion change in variance (PCV)
PCV measures the percentage of variation in husbands’/partners’ decision-making power regarding contraceptive use that is explained by the model with the available variables. In this study, the PCV of the final model was 18%, indicating that 18% of the variability was explained by the model, while the remaining 82% was not explained by the model [40,41,42].
Deviance (-2 log-likelihood)
Deviance measures the total variation explained by both individual and community-level factors. It is used for model comparison, with the model exhibiting the lowest deviance being preferred for interpreting the findings. In this study, Model IV had the lowest deviance and was selected for interpretation [40, 41].
Results
Out of 3669 married women of reproductive age, 2412 (66%) were aged 20–34. Among all participants, 1445 (39%) had husbands who attended primary education. Additionally, 1877 (51%) identified as orthodox. In this study, 1989 (54%) had media exposure. Regarding community factors, 2451 (67%) had low community women’s education, while 2241 (61%) were in high community poverty (Table 2).
Obstetric and health care services related characteristics of participants in Ethiopia
Out of all participants, 3365 (92%) had no history of pregnancy termination. Additionally, 2396 (65%) had no information about family planning. (Table 3).
Prevalence of husbands/partners’ decision-maker on contraceptive use in Ethiopia
The magnitude of husbands/partners decision makers on contraceptive use in Ethiopia was found to be 5.41%; 95% [4.72-6.19%] (Fig. 2).
Multilevel logistic regression analysis of determinant factors for husbands/partners’ involvement in women’s contraceptive use decision making process in Ethiopia
In the bivariate multilevel logistic regression analysis, twelve variables were significantly associated with husbands’/partners’ decision-making power regarding contraceptive use in Ethiopia. In the multivariable multilevel logistic regression analysis, six variables remained significantly associated: the age of husbands/partners, their educational level, media exposure, history of pregnancy termination, distance to a health facility, and residency.
Husbands/partners aged 31–59 and over 59 were 1.3 and 2.3 times more likely to make decisions about contraceptive use, respectively, compared to those under 31 (AOR = 1.3; 95% CI: 0.7–2.3 and AOR = 2.3; 95% CI: 1.2–4.3). Husbands/partners with primary, secondary, and higher education levels were 3.2, 3.8, and 4.3 times more likely, respectively, to make decisions about contraceptive use compared to those with no formal education (AOR = 3.2; 95% CI: 2.9–4.3, AOR = 3.8; 95% CI: 2.7–4.4, and AOR = 4.3; 95% CI: 2.8-5.0).
Women with media exposure were 4.5 times more likely to have husbands/partners make decisions about contraceptive use (AOR = 4.5; 95% CI: 2.2–5.4) compared to women without mass media exposure. Women with a history of pregnancy termination were 3.3 times more likely to have their husbands/partners make decisions about contraceptive use (AOR = 3.3; 95% CI: 2.6–4.1) compared to women with no history of pregnancy termination. Participants who reported that distance to a health facility was not a significant problem were 3.0 times more likely to have husbands/partners decide on contraceptive use (AOR = 3.0; 95% CI: 1.7–4.7) compared to those who found distance to be a significant problem. Women residing in urban areas were 3.5 times more likely to have their husbands/partners make decisions about contraceptive use (AOR = 3.5; 95% CI: 1.6–4.2) compared to women living in rural areas.
The Median Odds Ratios (MOR) for models I, II, III, and IV were 2.6, 2.44, 2.4, and 2.34, respectively. The Proportion Change in Variance (PCV) for models II, III, and IV were 10%, 13%, and 18%, respectively (Table 4).
Discussion
Empowering husbands/partners to be independent decision-makers in women’s contraceptive choices can indeed have a positive impact on maternal, neonatal, and child mortality rates. When husbands/partners are involved in the decision-making process, it can lead to increased access to and consistent use of contraceptives, which in turn can help in better family planning, reducing unintended pregnancies, and ultimately decreasing maternal, neonatal, and child mortality. This involvement can also foster better communication and collaboration within the family, leading to improved health outcomes for women and children. [36, 43, 44]. The low percentage of husbands’/partners’ independent decision-making in the contraceptive choices of women in Ethiopia, at 5.41%, indicates a significant gap in involvement compared to studies in other regions like Nigeria, where the rate was 89%. The disparity highlights the need for more research to identify specific factors contributing to this low engagement level in Ethiopia. Understanding these determinants can help develop targeted interventions to enhance husbands’/partners’ involvement in women’s contraceptive decision-making processes, ultimately leading to improved reproductive health outcomes for women and children in the country. [45],. The disparities in educational levels and residency between studies can indeed significantly influence husbands’/partners’ involvement in women’s contraceptive decision-making processes. In the context of Ethiopia, where a higher percentage of participants had no formal education, compared to other studies with more educated participants, this could contribute to the lower levels of involvement observed. Additionally, the difference in data sources (secondary analysis versus primary data collection) and the demographic composition of participants (urban versus rural) can also impact reported levels of husbands’/partners’ involvement. These socio-demographic factors are key considerations for understanding and addressing male involvement in family planning decisions, ultimately promoting better reproductive health outcomes for women in Ethiopia.
It’s interesting to note the contrast in husbands’/partners’ involvement in contraceptive decision-making between Ethiopia and Malawi. While the current study in Ethiopia reported better levels of involvement, Malawi faced challenges with reported zero involvement. Factors like the age, educational status, history of terminated pregnancies, media exposure, distance to health facilities, and residency all play significant roles in determining husbands’/partners’ involvement in contraceptive decision-making processes. Understanding and addressing these factors are essential for promoting greater male involvement in family planning decisions, which can have positive impacts on reproductive health outcomes.The association between husbands’/partners’ age and their involvement in contraceptive decision-making processes is a significant finding. In the current study in Ethiopia, it was observed that husbands/partners in the age groups of 31–59 and over 59 were 1.3 and 2.3 times more likely to be involved in these decisions compared to those under 31. This mirrors similar findings in studies conducted in Nigeria, showcasing a trend where older age groups tend to exhibit higher levels of involvement in family planning discussions. Understanding age-related dynamics can help tailor interventions to enhance male involvement in contraceptive decision-making across different settings. [46, 47]. The premise that older husbands/partners are more likely to be involved in contraceptive decision-making due to a decreased demand for more children and an increased demand for contraception aligns with existing evidence. As individuals age, their family planning preferences often shift towards smaller family sizes or maintaining the current number of children. This shift in desires can lead to a greater interest in contraceptive use and active participation in decision-making processes related to family planning. Understanding these nuanced motivations can inform targeted strategies to promote male involvement in contraceptive decisions across different age groups. [48]. The correlation between husbands’/partners’ educational levels and their involvement in contraceptive decision-making is a notable finding corroborated by research in Ethiopia. The study indicates that individuals with primary, secondary, and higher education levels are 3.2, 3.9, and 4.3 times more likely to participate in these decisions compared to those with no formal education. This underscores the positive relationship between education and engagement in family planning discussions, highlighting the importance of educational interventions in fostering male involvement in contraceptive decision-making processes. [49, 50]. Educational initiatives that inform individuals about the benefits of family planning can indeed play a crucial role in increasing male involvement in decision-making processes. By understanding the positive impact of family planning on reducing maternal morbidity associated with high fertility rates, individuals may be more inclined to actively participate in discussions related to contraceptive use. Moreover, education can help individuals grasp the significance of family planning in achieving desired family sizes and promoting the overall well-being of both partners and children. Through targeted educational efforts, promoting awareness and understanding of family planning concepts can lead to greater engagement and support for reproductive health decisions [51]. Research from the Philippines, India, Ghana, Indonesia and Malawi suggest a strong association between media exposure and increased involvement of husbands/partners in contraceptive decision-making processes. Individuals with media exposure are reportedly 4.5 times more likely to participate in these discussions compared to those without media exposure. This underscores the influential role of media in disseminating information about family planning and reproductive health, ultimately fostering greater male engagement in decision-making. By leveraging media platforms to promote awareness and education on contraceptive use, key messages can reach broader audiences, encouraging more inclusive and informed discussions within relationships [52,53,54,55,56]. Absolutely! Exposure to mass media plays a critical role in shaping individuals’ knowledge and understanding of family planning. Through media channels, individuals can access information about the demographic, human rights, and health implications of family planning, including the potential risks associated with high fertility rates. By highlighting the positive impact of family planning on women’s and children’s health, media exposure can empower individuals to make informed decisions regarding contraceptive use and engage in discussions about family planning within their relationships. This increased knowledge can lead to more supportive and collaborative decision-making processes, ultimately benefiting the health and well-being of families [57, 58]. Absolutely! When husbands/partners are exposed to information highlighting the benefits of family planning and the importance of their involvement in contraceptive decision-making, it can positively influence their attitudes and behaviors. By fostering a greater understanding of the health and social implications of family planning, media campaigns can encourage husbands/partners to actively participate in these discussions, leading to more collaborative decision-making processes within relationships. This increased participation can ultimately contribute to improved communication, mutual understanding, and support for family planning choices, creating a more inclusive and informed approach to reproductive health. Women with a history of pregnancy termination are 3.3 times more likely to have their husbands/partners involved in the contraceptive use decision-making process compared to women without such a history. This increased likelihood may be due to the fact that women who have previously terminated a pregnancy are often less inclined to engage in subsequent pregnancies. As a result, they may have a stronger desire to use contraceptives, making it more likely that their husbands/partners will be involved in the decision-making process [59, 60], Additionally, husbands/partners whose wives have experienced pregnancy terminations are more likely to be counseled by healthcare providers about family planning options. This counseling often occurs when they accompany their wives to health facilities for the termination procedure, thus increasing their engagement in family planning decisions [28, 35, 61].
Women for whom distance to the nearest health facility is not a significant issue are 3.0 times more likely to have their husbands/partners involved in the contraceptive use decision-making process compared to women for whom distance is a significant problem. Various studies have demonstrated that easy access to health facilities is a key determinant for effective utilization of maternal health care services, including contraceptive use, in Ethiopia [62,63,64,65].
Living closer to a health facility not only facilitates easier access to health services but also increases the likelihood of being reached by fieldwork and outreach programs. These programs help inform both women and their husbands/partners about the benefits of contraceptive use, potentially leading to greater involvement of husbands/partners in the contraceptive decision-making process.
Furthermore, women residing in urban areas are 3.5 times more likely to have their husbands/partners involved in the contraceptive use decision-making process compared to those living in rural areas. This finding is consistent with studies conducted in Nigeria [66], Mozambican [67], and Ghana [68]. Women in urban areas have high media exposure compared to women in rural [53, 69]. This increased accessibility to health facilities and outreach programs in urban areas means that husbands/partners are more likely to be informed about family planning options. Consequently, they are more likely to be involved in the contraceptive use decision-making process.
Conclusions
The involvement of husbands/partners in women’s contraceptive use decision-making was generally low in Ethiopia. However, several factors were positively associated with their involvement, including: Age of husbands/partners 31–59, and > 59, educational level of husbands/partners primary, secondary, and higher, positive media exposure, distance not a big problem, and urban residency were positively associated with husbands/partners’ involvement in women’s contraceptive use decision making process in Ethiopia.
Data availability
All output based data are available within the manuscript and additionally, the data set can be accessed from www.measuredhs.com.
Abbreviations
- AOR:
-
Adjusted Odds Ratio
- CI:
-
Confidence Interval
- DHS:
-
Demographic and Health Survey
- EDHS:
-
Ethiopian Demographic and Health Survey
- EAs:
-
Enumeration Areas
- ICC:
-
Intra- Class Correlation Coefficient
- MOR:
-
Median Odds Ratio
- PCV:
-
Proportion Change In variance
- PSU:
-
Primary Sampling Unit
- SDG:
-
Sustainable Development Goal
References
Campbell AA. The role of family planning in the reduction of poverty. J Marriage Fam. 1968:236–45.
Bailey MJ, Malkova O, Norling J. Do family planning programs decrease poverty? Evidence from public census data. CESifo Economic Stud. 2014;60(2):312–37.
Erfani A. The impact of family planning on women’s educational advancement in Tehran, Iran. 2012.
Islam S, Hasan M. Women knowledge, attitude, approval of family planning and contraceptive use in Bangladesh. Asia Pac J Multidisciplinary Res. 2016;4(2):76–82.
Utomo B, Sucahya PK, Romadlona NA, Robertson AS, Aryanty RI, Magnani RJ. The impact of family planning on maternal mortality in Indonesia: what future contribution can be expected? Popul Health Metrics. 2021;19(1):1–13.
Doyle MW, Stiglitz JE. Eliminating extreme inequality: a sustainable development goal, 2015–2030. Ethics Int Affairs. 2014;28(1):5–13.
Bali Swain R, Yang-Wallentin F. Achieving sustainable development goals: predicaments and strategies. Int J Sustainable Dev World Ecol. 2020;27(2):96–106.
Pedercini M, Zuellich G, Dianati K, Arquitt S. Toward achieving sustainable development goals in Ivory Coast: simulating pathways to sustainable development. Sustain Dev. 2018;26(6):588–95.
Csa I. Central statistical agency (CSA)[Ethiopia] and ICF. Ethiopia demographic and health survey, Addis Ababa, Ethiopia and Calverton, Maryland, USA. 2016.
Demographic CE. Health Survey-2011. Central Statistical Agency Addis Ababa. Ethiopia ICF International Calverton, Maryland, USA. 2012. 2016.
Getaneh T, Negesse A, Dessie G, Desta M, Moltot T. Predictors of unmet need for family planning in Ethiopia 2019: a systematic review and meta analysis. Archives Public Health. 2020;78(1):1–11.
Teshome L, Belayihun B, Zerihun H, Moges F, Equar A, Asnake M. Modern contraceptives use and associated factors among adolescents and youth in Ethiopia. Ethiop J Health Dev. 2021;35(5).
Alem AZ, Agegnehu CD. Magnitude and associated factors of unmet need for family planning among rural women in Ethiopia: a multilevel cross-sectional analysis. BMJ open. 2021;11(4):e044060.
Girma Garo M, Garoma Abe S, Dugasa Girsha W, Daka DW. Unmet need for family planning and associated factors among currently married women of reproductive age in Bishoftu town, Eastern Ethiopia. PLoS ONE. 2021;16(12):e0260972.
Lee BX, Kjaerulf F, Turner S, Cohen L, Donnelly PD, Muggah R, et al. Transforming our world: implementing the 2030 agenda through sustainable development goal indicators. J Public Health Policy. 2016;37(1):13–31.
Goodkind D, Lollock L, Choi Y, McDevitt T, West L. The demographic impact and development benefits of meeting demand for family planning with modern contraceptive methods. Global Health Action. 2018;11(1):1423861.
Chola L, McGee S, Tugendhaft A, Buchmann E, Hofman K. Scaling up family planning to reduce maternal and child mortality: the potential costs and benefits of modern contraceptive use in South Africa. PLoS ONE. 2015;10(6):e0130077.
Al Riyami A, Afifi M, Mabry RM. Women’s autonomy, education and employment in Oman and their influence on contraceptive use. Reprod Health Matters. 2004;12(23):144–54.
DeRose LF, Ezeh AC. Decision-making patterns and contraceptive use: evidence from Uganda. Popul Res Policy Rev. 2010;29(3):423–39.
Organization WH. World health statistics 2016: monitoring health for the SDGs sustainable development goals. World Health Organization; 2016.
Bogale B, Wondafrash M, Tilahun T, Girma E. Married women’s decision making power on modern contraceptive use in urban and rural southern Ethiopia. BMC Public Health. 2011;11(1):1–7.
Asratie MH, Belay DG. Prevalence of contraceptive non-use due to Husbands/Partners influence among Married women in Ethiopia: a Multilevel Analysis using demographic and Health Survey 2016 data. Frontiers in Reproductive Health.27.
Shachar BZ, Lyell DJ. Interpregnancy interval and obstetrical complications. Obstet Gynecol Surv. 2012;67(9):584–96.
Norton M. New evidence on birth spacing: promising findings for improving newborn, infant, child, and maternal health. Wiley Online Library; 2005.
Aychiluhm SB, Tadesse AW, Mare KU, Abdu M, Ketema A. A multilevel analysis of short birth interval and its determinants among reproductive age women in developing regions of Ethiopia. PLoS ONE. 2020;15(8):e0237602.
Tesema GA, Worku MG, Teshale AB. Duration of birth interval and its predictors among reproductive-age women in Ethiopia: Gompertz gamma shared frailty modeling. PLoS ONE. 2021;16(2):e0247091.
Haddad LB, Nour NM. Unsafe abortion: unnecessary maternal mortality. Reviews Obstet Gynecol. 2009;2(2):122.
Biddlecom AE, Fapohunda BM. Covert contraceptive use: prevalence, motivations, and consequences. Studies in family planning. 1998:360 – 72.
Hall KS, Manu A, Morhe E, Dalton VK, Challa S, Loll D, et al. Bad girl and unmet family planning need among sub-saharan African adolescents: the role of sexual and reproductive health stigma. Qualitative Res Med Healthc. 2018;2(1):55.
Imam A, Maidala BH. The socio-cultural factors affecting family planning services in Nigeria. Br J Social Economic Res. 2018;3(3):33–9.
Onyango MA, Owoko S, Oguttu M. Factors that influence male involvement in sexual and reproductive health in western Kenya: a qualitative study. Afr J Reprod Health. 2010;14(4).
Kabagenyi A, Jennings L, Reid A, Nalwadda G, Ntozi J, Atuyambe L. Barriers to male involvement in contraceptive uptake and reproductive health services: a qualitative study of men and women’s perceptions in two rural districts in Uganda. Reproductive Health. 2014;11(1):1–9.
Yonas Tadesse S, Emiru AA, Tafere TE, Asresie MB. Women’s Autonomy Decision Making Power on Postpartum Modern Contraceptive Use and Associated Factors in North West Ethiopia. Advances in Public Health. 2019;2019.
Hameed W, Azmat SK, Ali M, Sheikh MI, Abbas G, Temmerman M, et al. Women’s empowerment and contraceptive use: the role of independent versus couples’ decision-making, from a lower middle income country perspective. PLoS ONE. 2014;9(8):e104633.
Rasch V, Lyaruu MA. Unsafe abortion in Tanzania and the need for involving men in postabortion contraceptive counseling. Stud Fam Plann. 2005;36(4):301–10.
Blackstone SR, Nwaozuru U, Iwelunmor J. Factors influencing contraceptive use in sub-saharan Africa: a systematic review. Int Q Community Health Educ. 2017;37(2):79–91.
Klima CS. Unintended pregnancy: consequences and solutions for a worldwide problem. J Nurse-Midwifery. 1998;43(6):483–91.
Gonie A, Wudneh A, Nigatu D, Dendir Z. Determinants of family planning use among married women in bale eco-region, Southeast Ethiopia: a community based study. BMC Womens Health. 2018;18(1):1–10.
Croft TN, Marshall AM, Allen CK, Arnold F, Assaf S, Balian S. Guide to DHS statistics. Rockville: ICF. 2018;645.
Asratie MH, Kassie BA, Belay DG. Prevalence of contraceptive non-use due to Husbands/Partners influence among Married women in Ethiopia: a Multilevel Analysis using demographic and health survey 2016 data. Front Reproductive Health. 2022;4.
Hunie Asratie M, Belay DG. Pooled prevalence and determinants of completion of Maternity Continuum of Care in Sub-saharan Africa: a multi-country analysis of recent demographic and health surveys. Front Global Women’s Health. 2022;3:56.
Tesema GA, Mekonnen TH, Teshale AB. Spatial distribution and determinants of abortion among reproductive age women in Ethiopia, evidence from Ethiopian Demographic and Health Survey 2016 data: spatial and mixed-effect analysis. PLoS ONE. 2020;15(6):e0235382.
Rahman M. Women’s autonomy and unintended pregnancy among currently pregnant women in Bangladesh. Matern Child Health J. 2012;16(6):1206–14.
Singh A, Singh A, Mahapatra B. The consequences of unintended pregnancy for maternal and child health in rural India: evidence from prospective data. Matern Child Health J. 2013;17(3):493–500.
Ijadunola MY, Abiona TC, Ijadunola KT, Afolabi OT, Esimai OA, OlaOlorun FM. Male involvement in family planning decision making in Ile-Ife, Osun State, Nigeria. Afr J Reprod Health. 2010;14(4).
Blackstone SR, Iwelunmor J. Determinants of contraceptive use among Nigerian couples: evidence from the 2013 demographic and Health Survey. Contracept Reproductive Med. 2017;2(1):1–8.
Eshete A, Adissu Y. Women’s joint decision on contraceptive use in gedeo zone, southern ethiopia: a community based comparative cross-sectional study. International journal of family medicine. 2017;2017.
Belay AD, Mengesha ZB, Woldegebriel MK, Gelaw YA. Married women’s decision making power on family planning use and associated factors in Mizan-Aman, South Ethiopia: a cross sectional study. BMC Womens Health. 2016;16(1):1–6.
Wondim G, Degu G, Teka Y, Diress G. Male involvement in Family Planning utilization and Associated Factors in Womberma District, Northern Ethiopia: community-based cross-sectional study. Open Access J Contracept. 2020;11:197.
Chekole MK, Kahsay ZH, Medhanyie AA, Gebreslassie MA, Bezabh AM. Husbands’ involvement in family planning use and its associated factors in pastoralist communities of Afar. Ethiopia Reproductive Health. 2019;16(1):1–7.
Gahungu J, Vahdaninia M, Regmi PR. The unmet needs for modern family planning methods among postpartum women in Sub-saharan Africa: a systematic review of the literature. Reproductive Health. 2021;18(1):1–15.
Das P, Samad N, Al Banna H, Sodunke TE, Hagan JE, Ahinkorah BO, et al. Association between media exposure and family planning in Myanmar and Philippines: evidence from nationally representative survey data. Contracept Reproductive Med. 2021;6(1):1–12.
Ghosh R, Mozumdar A, Chattopadhyay A, Acharya R. Mass media exposure and use of reversible modern contraceptives among married women in India: an analysis of the NFHS 2015–16 data. PLoS ONE. 2021;16(7):e0254400.
Olaleye DO, Bankole A. The impact of mass media family planning promotion on contraceptive behavior of women in Ghana. Popul Res Policy Rev. 1994;13(2):161–77.
Ardiansyah B. Effect of Mass Media on Family Planning Choices in Indonesia. 2016.
Zamawe C, Banda M, Dube A. The effect of mass media campaign on men’s participation in maternal health: a cross-sectional study in Malawi. Reproductive Health. 2015;12(1):1–7.
Cleland J, Bernstein S, Ezeh A, Faundes A, Glasier A, Innis J. Family planning: the unfinished agenda. Lancet. 2006;368(9549):1810–27.
Page BI, Shapiro RY. The rational public: University of Chicago Press; 2010.
Kimport K, Foster K, Weitz TA. Social sources of women’s emotional difficulty after abortion: lessons from women’s abortion narratives. Perspect Sex Reprod Health. 2011;43(2):103–9.
Coleman PK, Reardon DC, Cougle JR. Substance use among pregnant women in the context of previous reproductive loss and desire for current pregnancy. Br J Health Psychol. 2005;10(2):255–68.
Prata N, Bell S, Fraser A, Carvalho A, Neves I. Partner support for family planning and modern contraceptive use in Luanda. Angola Afr J Reproductive Health. 2017;21(1):35–48.
Okwaraji YB, Webb EL, Edmond KM. Barriers in physical access to maternal health services in rural Ethiopia. BMC Health Serv Res. 2015;15(1):1–8.
Defar A, Okwaraji YB, Tigabu Z, Persson LÅ, Alemu K. Distance, difference in altitude and socioeconomic determinants of utilisation of maternal and child health services in Ethiopia: a geographic and multilevel modelling analysis. BMJ open. 2021;11(2):e042095.
Asratie MH, Muche AA, Geremew AB. Completion of maternity continuum of care among women in the post-partum period: magnitude and associated factors in the northwest, Ethiopia. PLoS ONE. 2020;15(8):e0237980.
Gebreyesus A. Determinants of client satisfaction with family planning services in public health facilities of Jigjiga town, Eastern Ethiopia. BMC Health Serv Res. 2019;19(1):1–10.
Feyisetan BJ. Spousal communication and contraceptive use among the Yoruba of Nigeria. Popul Res Policy Rev. 2000;19(1):29–45.
Mboane R, Bhatta MP. Influence of a husband’s healthcare decision making role on a woman’s intention to use contraceptives among Mozambican women. Reproductive Health. 2015;12(1):1–8.
Tawiah E. Factors affecting contraceptive use in Ghana. J Biosoc Sci. 1997;29(2):141–9.
Gashu KD, Yismaw AE, Gessesse DN, Yismaw YE. Factors associated with women’s exposure to mass media for Health Care Information in Ethiopia. A case-control study. Clin Epidemiol Global Health. 2021;12:100833.
Acknowledgements
Our deepest gratitude goes to the measure DHS program for the permission of access and uses the 2016 EDHS data.
Funding
No, any fund had taken for this research.
Author information
Authors and Affiliations
Contributions
Melaku Hunie Asratie wrote the main manuscript text Melaku Hunie Asratie, Daniel Gashaneh Belay, Adugnaw Zeleke Alem, Dagmawi Chilot, Nuhamin Tesfa Tsega, Anteneh Ayelign Kibret, Mehari Woldemariam Merid & Fantu Mamo Aragaw performed the analysis and reviewed the manuscript and approved the submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Since the study was a secondary data analysis of publically available survey data from the measure DHS program, ethical approval and participant consent were not necessary for this particular study. We requested DHS Program and permission was granted to download and use the data for this study from http://www.dhsprogram.com. The Institution Review Board approved procedures for DHS public-use datasets do not in any way allow respondents, households, or sample communities to be identified. There were no names of individuals or household addresses in the data file. The geographic identifiers only go down to the regional level (where regions are typically very large geographical areas encompassing several states/provinces). Each enumeration area (Primary Sampling Unit) has a PSU number in the data file, but the PSU numbers do not have any labels to indicate their names or locations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Asratie, M.H., Belay, D.G., Alem, A.Z. et al. What are the associated factors of low husbands/partners independent decision-maker in women’s contraceptive use decision-making process in Ethiopia? Multilevel analysis. BMC Public Health 24, 2185 (2024). https://doi.org/10.1186/s12889-024-19572-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19572-w