Abstract
Background
Overweight and obesity are one of the most significant risk factors of the twenty-first century related to an increased risk in the occurrence of non-communicable diseases and associated increased healthcare costs. To estimate the future impact of overweight, the current study aimed to project the prevalence of overweight and obesity to the year 2030 in Belgium using a Bayesian age-period-cohort (APC) model, supporting policy planning.
Methods
Height and weight of 58,369 adults aged 18+ years, collected in six consecutive cross-sectional health interview surveys between 1997 and 2018, were evaluated. Criteria used for overweight and obesity were defined as body mass index (BMI) ≥ 25, and BMI ≥ 30. Past trends and projections were estimated with a Bayesian hierarchical APC model.
Results
The prevalence of overweight and obesity has increased between 1997 and 2018 in both men and women, whereby the highest prevalence was observed in the middle-aged group. It is likely that a further increase in the prevalence of obesity will be seen by 2030 with a probability of 84.1% for an increase in cases among men and 56.0% for an increase in cases among women. For overweight, it is likely to see an increase in cases in women (57.4%), while a steady state in cases among men is likely. A prevalence of 52.3% [21.2%; 83.2%] for overweight, and 27.6% [9.9%; 57.4%] for obesity will likely be achieved in 2030 among men. Among women, a prevalence of 49,1% [7,3%; 90,9%] for overweight, and 17,2% [2,5%; 61,8%] for obesity is most likely.
Conclusions
Our projections show that the WHO target to halt obesity by 2025 will most likely not be achieved. There is an urgent necessity for policy makers to implement effective prevent policies and other strategies in people who are at risk for developing overweight and/or obesity.
Similar content being viewed by others
Background
In the European region, the prevalence of overweight increased from 48.0% in 1980 to 59.6% in 2015, and that of obesity from 14.5% in 1980 to 22.9% in 2015 [1]. Not only obesity is known as an important risk factor contributing to many negative health outcomes, such as cardiovascular disease, type 2 diabetes, colorectal, prostate and renal cancer, and many other non-communicable diseases [2,3,4,5,6,7,8], but also overweight is associated with these same negative health outcomes, albeit to a less severe extend [9].
Because of the large increase in cases in the past decade, overweight and obesity are now both considered as a global epidemic [10]. Belgium is no exception to this situation: obesity prevalence rose from 9.0% in 1978 to 15.0% in 1993 in a subsample of working, middle-aged men [11], and kept rising since. Consequently, a global obesity target to halt obesity at 2010 levels by 2025 was adopted during the World Health Assembly in 2013 [12], whereby consensus was reached to prevent a further growth in the number of men and women with obesity above the observed prevalence in 2010.
As obesity has been recognized as a major public health problem in Europe, research on its likely evolution in European countries is necessary. To this end, a variety of statistical models has been applied to the European context, such as linear extrapolations and wave functions. The diversity in methodologies employed differed substantially, and not all were able to yield realistic obesity estimates for the near future [13,14,15,16,17,18,19,20,21,22]. To better comprehend the complexity underlying the overweight and obesity epidemic, and obtain reliable and valid projections, it is important to consider the contributing risk factors. These factors may include socio-demographic factors such as age, sex, and education, but also lifestyle habits such as sedentary lifestyles and the consumption of high-calorie foods [1, 23,24,25]. For example, there is a known sex gradient in the impact of overweight and obesity, whereby the risk for developing asthma [26] and diabetes [27] is different between men and women. In addition, it is important to consider the so-called generation effect, i.e. the degree to which individuals are receptive to societal and social changes. These effects specifically feature the common exposures of people from the same birth cohort, such as common nutritional habits, smoking habits, and others [28,29,30,31]. Hence, the birth of age-period-cohort (APC) analysis, whereby the age effect reflects the association between age and weight status, the period effects reflects the evolution of weight over time, and the birth cohort effect reflects the degree to which an individual’s weight is receptive to societal and social changes.
An important issue in trend analysis is the limited availability of longitudinal data at regular time intervals [32]. Instead, epidemiologists often have to rely on repeated cross-sectional data to obtain long-term trends in overweight and obesity, whereby only basic information on age and sex is available for future populations based on population projections. Here is where the APC analysis excels as its estimated projections consider disentangled trends in age, period and cohort (i.e. generation) for overweight and obesity.
To date, only a limited number of studies have undertaken APC analyses to the prevalence rates of overweight and obesity, among which the number of European studies is scarce [10, 24, 33,34,35]. In addition, many of these studies did not consider the complex sampling process of the population microdata at hand, or have built further on the recent critiques regarding APC analysis [36, 37]. Lastly, the current pool of available studies mainly focused on estimating the APC effects, but the APC-analysis could be expanded by including other specific effects such as sex, and education. Therefore, the current study aims to (1) evaluate the age-period-cohort and other important effects based on the past and current data, and (2) estimate case projections using a APC modelling approach for a period of 10 years. To this end, a flexible Bayesian hierarchical APC model will be applied to population microdata available through the Belgian Health Interview Survey.
Methods
Data
Statistical analyses were performed using the datasets of the Belgian Health Interview Survey (BHIS), which was organized for the first time in 1997 by Sciensano, the Belgian Institute for Health, and contains a series of repeated cross-sectional sample surveys [38,39,40]. So far, six national health surveys have been carried out – in 1997, 2001, 2004, 2008, 2013 and 2018. The goal was to collect information on lifestyle and chronic diseases for approximately 10,000 individuals in each survey round. The survey applies a stratified multistage, clustered sampling method for each survey year. The combination of the large net sample size and the elaborate sampling methodology ensures that each sample is representative for the Belgian population, and that any trend found using the subsequent health surveys can be generalized to the larger Belgian population. More details on the sampling procedure have been published elsewhere (Demarest et al., 2013). The sole inclusion criteria to be eligible for the health interview study is a registration in the national register. For the current study, participants were only included if they had an age larger than or equal to 18. The survey was carried out in line with the Belgian privacy legislation and approved by the ethical committee of Ghent University.
In the current study, information on age, sex, education level, migration background, urbanization level, income level, and self-reported height and weight of participants was included from the different waves of BHIS [39].
The education level was used as a proxy indicator of the socio-economic status of the household and all its members. This indicator is based on the highest education level of the reference person or his/her partner and allocated to each member of the household. Possible values are “primary or no degree”, “secondary inferior”, “secondary superior”, and “superior education” following the ISCED-11 classification, whereby superior education includes all obtained degrees higher than secondary superior [41].
The income level is calculated based on the ‘total available income of the household’, for which an equivalent scale is applied [42]. This allows comparing incomes of different households taking their size and composition into account. The different members of the household receive a specific weight: 1.0 for the first adult member of the household, 0.5 for each additional adult (18+ years) and 0.3 for each child (< 18 years). The total available income of the household is divided by the sum of the weights of all the members of the household to calculate the equivalent income. The income levels (quintiles) include “< 750 euro”, “750–1000 euro”, “1000–1500 euro”, “1500–2500 euro”, and “> 2500 euro”, which are hereafter referred to as quantiles 1 to 5.
The level of urbanization was determined based on morphological and functional characteristics of the municipalities. Two morphological criteria are used to classify the municipalities: the population density and the area of habitation. Three criteria are used to describe the functional characteristics of the municipalities: the commercial function, the educative function and the employment rate. Based on these attributes, municipalities are labelled as “Big cities and dense agglomerations”, “Suburban”, “Urbanized municipalities”, or “Rural”.
The estimate for body mass index (BMI) was based on self-reported height and weight, and categorized as normal weight (0–25 kg/m2), overweight (≥ 25 kg/m2), and obese (≥ 30 kg/m2) [43].
Population projection data were retrieved from the Belgian Federal Planning Bureau (https://www.plan.be/publications), Belgium [44].
Data analysis
To model the number of cases with overweight and obesity using age, period, and cohort effects, an age-period-cohort (APC) analysis was performed. We have built two separate models, one with overweight and one with obesity as dependent variable.
Independent variable
As explanatory variables, the models considered sex, education level, migration background, urbanization level, and income level as fixed independent categorical effects, and the categorical age, period and cohort effects as random effects. In the forecasting model, fixed effects that were not available as strata in the demography projections from the Belgian Federal Planning Bureau were excluded.
Dependent variable
The dependent variable was obesity and overweight, which were dichotomized based on the BMI of each individual.
Statistical model
One of the major issues in classical APC models is the linear dependency between the age effect, the period effect, and cohort effect. To tackle this linear dependency, the hierarchical age-period-cohort (HAPC) model has been introduced, which can include a mix of fixed and random effects [45,46,47]. Applying these HAPC models in a Bayesian framework allows for a direct interpretation of future trends in terms of credibility (e.g., how likely will overweight and obesity increase by at least 10%), whereas in the frequentist setting the projected uncertainty intervals cannot be interpreted as credibility. Hence, Bayesian HAPC models have been applied more frequent to forecast future trends in prevalence and incidence of cancer [48, 49], but to our knowledge, no study has applied the Bayesian APC model to forecast future trends in the prevalence of overweight and obesity.
Using the Bayesian framework, APC models [48] were fitted using the INLA package (Version 20.3.17) [50]. INLA stands for Integrated Nested Laplace Approximation, a novel approach that makes Bayesian inference faster compared to the computer-intensive Bayesian Markov chain Monte Carlo methods. More information on the INLA package can be found elsewhere (https://www.r-inla.org/). The number of overweight or obese individuals, yij, in age group i and period j was modelled as a Binomial process with the mean equal to the product of the population at risk, Nij, and the estimated prevalence. The logit of the prevalence, ηij, was estimated as a linear combination of the age, period and cohort effects, respectively αi, βj and γk, where k = M(I − i) + j is the birth cohort, M is the number of periods per age group and I is the number of age groups.
Second-order random walk priors (RW2) were applied to the age, period and cohort effects. These RW2 effects are particularly well-suited to model unequal time intervals in the APC effects [51]. Log-gamma priors were applied to the precision parameters with scale and shape parameters of 1 and 0.00005 for each of the age, period and cohort effects. Modelling priors were based on the methodology from Cameron & Baade (2019) and Riebler & Held (2010). Model selections for factors and priors was based on information criteria: DIC, Deviance information criterion, and WAIC, Watanabe–Akaike information criterion. Projected temporal trends were described as the median and 95% credibility intervals (CrI) around the median were constructed based on the 2.5 and 97.5% quantile of the posterior distribution.
In addition, based on the marginal posterior distribution of the modelled count, we calculated the probability, P(yt + x > yt + m × yt), that a projected rate in year t + x is greater than the modelled value in the final year of observed data (t = 2018), by some margin m (expressed as percentage increase, %). All statistical analyses were performed in R 4.1.0 [52].
Model validation
Model fit and predictive accuracy were assessed by fitting the model to the repeated cross-sectional sample surveys [38]. The explained variance (R2) and root mean squared error (RMSE) between the observed and projected prevalence counts were calculated for different priors and models. More details on the model validation are provided in Supplementary material A.
Results
Population
In total, the sample included 73,681 participants across all surveys. More information on the final sample that was selected for the analysis sample is depicted in the flowchart (Fig. 1). The raw socio-demographic, and health-related characteristics of each cohort are listed in Table 1. The average age across the different cross-sectional cohorts ranged from 44 to 51 years. The majority of participants were females with proportions ranging from 52 to 54%. Over time, the proportion of participants with a higher education has increased from 29% in 1997 to 41% in 2018. The level of urbanization has remained stable over time with the majority of participants living in big cities (47%), and a minority living in a suburban (13%) or rural area (15%) in 2018. The income distribution shows an increase of incomes in the higher quintiles (Quintile 4 and 5) and a decrease in the lower quintiles (Quintile 1 and 2). The number of non-EU immigrants has doubled from 5.2% in 1997 to 11.0% in 2018.
Past and present trends in overweight and obesity
The rate of overweight in the population adjusted for the survey design increased by 8.9% from 45,348 [45,192; 45,504] per 100,000 in 1997 to 49,412 [49,257; 49,567] per 100,000 in 2018, while the rate of obesity in the population increased by 25.9% from 12,978 [12,892; 13,066] in 1997 to 16,339 [16,238; 16,440] in 2018. Summary measures of model fit in terms of DIC and WAIC for the overweight and obesity model are presented in Table 2. DIC and WAIC were the lowest for the model including age, period, and cohort effects together with all fixed effects (sex, urbanisation level, education level, income and nationality). Sex (Woman vs Man) was identified as a risk factor for overweight (OR = 0.55; 95% CrI = [0.55; 0.55]), but was a negligible risk factor for obesity (OR = 0.97; 95% CrI = [0.96; 0.97]). Superior education (OR = 0.67; 95% CrI = [0.66; 0.67]) was associated with decreased odds for overweight compared to no education or primary degree, whereas both superior education (OR = 0.49; 95% CrI = [0.49; 0.49]) and higher secondary education (0.74; 95% CrI = [0.74; 0.75]) were associated with decreased odds for overweight compared to the group with no education or primary degree. Middle incomes (Quantile 3) showed a higher risk of obesity and overweight compared to the lowest incomes (Quantile 1), but the highest incomes (Quantile 5) showed a reduced risk with an estimated OR of 0.92 [0.92; 0.92] for overweight and 0.83 [0.83; 0.84] for obesity. More information on the estimated fixed effects for obesity and overweight can be found in Table 3.
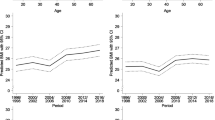
Figures 2 and 3 depicts the disentangled age, cohort, and period effects by sex for the occurrence of overweight and obesity in the Belgian population. The prevalence of overweight and obesity is the highest for the middle-aged groups in both men and women. In addition, the prevalence of overweight and obesity has increased over time in men and women. In men, the observed increase was stronger compared to the increase in women. Lastly, there was a clear increase in the prevalence of obesity and overweight among the oldest generations. However, since the generations born from 1915 and onwards the cohort effect has remained relatively stable.
Future trends in overweight and obesity
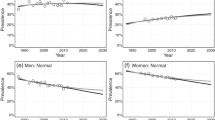
Modelled and projected rates with their 95% credibility interval (CrI) for overweight and obesity are given by sex in Fig. 4. The explained variance in prevalence expressed as the coefficient of determination (R2) by the overweight model equalled 80.6 and 76.0%, and the explained variance in prevalence by the obesity model equalled 76.7 and 58.3% for men and women, respectively.
Predicted prevalence rates for overweight and obesity. Plotted by year. The modelled observed data is depicted in black. Projections are depicted from the vertical line onwards for the period 2019–2030 in white, with quantiles from the estimated marginal posterior distribution of the projected prevalence. The colours reflect the credibility intervals expressed as quantile, coloured consecutively from dark blue to yellow
Temporal trends in rates for overweight in men showed a steady state to a slight decrease from 54,764 [54,764; 55,125] per 100,000 in 2018 towards a projected 53,616 [36,291; 70,866] cases per 100,000 in 2025, and 52,273 [21,216; 83,249] cases per 100,000 in 2030. In women, the projection showed a potential strong increase in cases from 44,070 [43,884; 44,255] per 100,000 in 2018 towards a projected 46,147 [19,666; 74,114] per 100,000 in 2025, and 49,147 [7275; 90,899] per 100,000 in 2030. In contrast, a high increase was observed for obesity in men from 17,453 [17,322; 17,585] cases per 100,000 in 2018 towards 22,497 [13,622; 35,616] cases per 100,000 in 2025, and 27,566 [9938; 57,358] cases per 100,000 in 2030. In women, the rate of increase was almost as high compared to men with cases increasing from 15,246 [15,125; 15,369] cases per 100,000 in 2018 towards 15,954 [6354; 35,020] cases per 100,000 in 2025, and 17,186 [2552; 61,803] cases per 100,000 in 2030.
Probabilities for exceeding a certain threshold m (> 0%, > 5%, > 10%, > 25%, > 50%, and > 100%) based on the marginal posterior distribution of the modelled counts are listed in Table 4. In men, there is a 43.3% probability for an increase in the rate of overweight by the year 2025 and 2030. The probability for an increase in the number of men with obesity by the year 2025 and 2030 are much higher in comparison, with estimated probabilities of 86.7% and 84.1%, respectively. In women, there is a 56.0% and 57.4% probability for an increase in the rate of overweight by the year 2025 and 2030, respectively. The probability for an increase in the number of women with obesity by the year 2025 and 2030 are much higher in comparison, with estimated probabilities of 54.6% and 56.0%, respectively.
As depicted in Fig. 5, the age structure of men and women with overweight and obesity has changed over time. In 2018, 57.7% and 61.8% of men, respectively with overweight and obesity, had an age between 36 and 65 years. Similarly, 51.5% and 53.9% of men, respectively with overweight and obesity, had an age between 36 and 65 years. The current projections estimate that these proportions will drop in 2030 to 53.6% and 50.4% in men, and 43.8% and 47.8% in women, whereby the proportion of men and women with obesity will mainly increase in the youngest (< 36 years) age category.
Discussion
Our analyses based on nationally representative data collected over six large scale health interview surveys, covering a period spanning over 20 years from 1997 to 2018, showed a disturbing picture of the future overweight and obesity epidemic in Belgium, assuming similar future increase rates as observed in the past. In men, an increase in overweight is less likely, whereby the probability of an increase by 2030 equals 43.3%. In contrast, an increase in obesity by 2030 is very likely with a probability of 84.1%. In women, an increase in overweight and obesity will likely be reached by 2030 with a respective probability of 57.4% and 56.0%.
Past and current trends in overweight and obesity
The age, period and cohort effects are similar to those reported in previous reports [1, 35], whereby the number of men and women with overweight and obesity has increased over time among all generations. The current trends indicate that overweight and obesity do not occur among specific generations, but rather affect all generations with an increasing trend over time among all generations. In addition, higher prevalence rates of overweight and obesity were demonstrated among middle-aged women and men. More specifically, among Belgians, a middle-age man, born before 1970 with no higher education and a middle income has the highest risk for being overweight and obesity at present. Among these risk factors, the highest were sex and education. It is well-known that sex plays an important role in the metabolic and genetic predisposition of overweight and obesity, whereby overweight and obesity do not only occur more frequent among men, but also yield an increased risk for developing overweight-related disorders among men [53, 54]. Socio-economic factors also play an important role in the occurrence of overweight, whereby healthier behaviour could be driven by a higher health-literacy, which in its turn relates to higher education levels [55].
Projections in overweight and obesity
Our projections indicate that Belgium is unlikely to meet the global obesity target to halt obesity “at 2010 levels” by 2025, which was adopted during the World Health Assembly in 2013 [12]. The current projected prevalence rates for overweight and obesity will likely be higher in both sexes compared to their respective 2010 prevalence estimates. In another study, it was estimated that the global rate of overweight in established economic markets would rise to 36.3% by 2030 following population projections and a steady prevalence rate of 2005. The same study estimated an increase to 30.0% when modelling the prevalence based on past data. Likewise, the obesity prevalence was estimated at 22.1% and 36.2% [21]. These estimates are lower compared to ours, however, the observed prevalence in 2018 already exceeded the projection for overweight by 10.6%, which indicates that these previous estimates were rather too conservative. Similar to our results, most study reports agree that the growth in cases with obesity is faster compared to the growth in cases with overweight [13,14,15,16,17,18,19,20,21,22]. The increase in overweight and obesity likely results from a complex interaction between changes in the food environment, physical activity, socioeconomic, environmental, and genetic factors [1]. For example, the number of low quality away from home food consumptions, a known environmental risk factor for overweight and obesity [56], has grown over the years. Assuming trends in behaviour are likely to evolve similarly to the past, the number of cases with overweight and/or obesity are very likely to increase further. Efforts have been made to halt the rise of overweight, but prevention is a complex issue and requires collective efforts from the governments, the scientific and the medical communities, the industry, and various social organizations towards the changing of dietary and lifestyle habits.
Policy implications
We argue, in accordance with the current evidence, that a multi-faceted approach will be necessary to halt a further increase in cases. This approach should include policy guidelines and legislation that focuses on prevention, but also include treatments that are considered effective for people with overweight and obesity. The main pillar to reach a halt in cases is the prevention of overweight and obesity. Prevention should already start in childhood and early adolescence by implementing health promotion in schools including offering healthy snacks and meals, and promoting sufficient levels of physical activity [57]. Further prevention can be achieved by implementing the prioritized food environment policies [58]. If prevention fails, healthcare workers can rely on effective treatment strategies, which mainly focus on lifestyle and behavioural changes in nutrition and physical activity, or – in the worst case – pharmacotherapy or bariatric Surgery [59,60,61]. Next, it is important to consider the socio-demographic gradient in overweight and obesity. It is known that some groups are more prone to develop overweight or obesity. Therefore, it is important implement policies that target this socio-demographic gradient in cases [62].
Without taking action, the rise in cases will likely follow the projected trajectory, whereby the rates of disease burden and associated healthcare cost of non-communicable diseases will also rise [63, 64]. The fact that environmental and behavioural forces fuelling the obesity epidemic are unlikely to be modified overnight, and even effective prevention programs may take years to show a significant impact [13], further emphasized the importance of prioritizing overweight and obesity on the healthcare agenda.
Lastly, the current forecasted rate of increase might have been exacerbated by the COVID-19 pandemic, as government introduced a myriad of measures such as cancellation of small gatherings, quarantine, lockdowns, and individual movement restrictions to combat the spread of the coronavirus [65]. Consequently, decreases in physical activity and increases in sedentary behaviours during lockdowns have been reported by different studies [66, 67], resulting in a potential increase of overweight and obesity in the current generations [68].
Strengths and limitations
APC models account for trends in risk factors, without requiring measurements of exposures. Projected counts are hence susceptible to unforeseeable changes, which might result in an over- or underestimate the actual future prevalence. The key assumption in the APC models is, as with any projection model, a continuation of the observed historical trends. However, evaluating the validity of that assumption is impossible.
Despite the wide uncertainty in projections beyond 5 or 10 years, governments require longer term projections for effective planning and policy development. The increased uncertainty provides a more realistic picture of the accuracy of projections, particularly when unforeseen interventions and changing circumstances (e.g. COVID-19) that could take place are considered. Since the cohort is a linear combination of age and period, the effects are not identifiable and cannot provide statistical evidence of change in prevalence [69]. Nevertheless, the models provide information on the prevalence and distribution across the population. The current study includes a large population of individual data over a time-span of 10 years. These data were modelled using a well-described modelling strategy including the incorporation of weights according to the sampling procedure, which results in realistic projections of future scenarios.
BMI has been defined according to the WHO definition, and based on self-reported estimates for weight and height. Consequently, the actual number of participants with obesity and overweight might have been higher as BMI is on average underestimated by 0.97 kg/m2 [70].
In a next step, future research could focus on integrating policy-decisions based on a scenario-based modelling approach. For example, including information on the level of physical activity or nutritional habits, and associated policy interventions could be expressed in terms of the changes in projected rate.
Conclusions
In conclusion, an alarming increase in the prevalence of overweight and obesity is predicted with a very likely increase in the prevalence of overweight and obesity among Belgian adults within the next 10 years. There is an urgent need to implement food environment policies, support preventive strategies, and support effective treatments to halt the increase in cases with overweight and obesity.
Availability of data and materials
The data that support the findings of this study are available from the Health Interview at Sciensano but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Health Interview team at Sciensano.
References
Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metabolism. 2019;92:6–10.
Sowers JR. Obesity as a cardiovascular risk factor. Am J Med. 2003;115:37–41.
Hannon TS, Rao G, Arslanian SA. Childhood obesity and type 2 diabetes mellitus. Pediatrics. 2005;116:473–80.
De Pergola G, Silvestris F. Obesity as a major risk factor for Cancer. J Obes. 2013;2013:e291546.
Shiri R, Lallukka T, Karppinen J, Viikari-Juntura E. Obesity as a risk factor for sciatica: a Meta-analysis. Am J Epidemiol. 2014;179:929–37.
Zhang T-T, Liu Z, Liu Y-L, Zhao J-J, Liu D-W, Tian Q-B. Obesity as a risk factor for low Back pain. Clin Spine Surg. 2018;31:22–7.
Grazio S, Balen D. Obesity: risk factor and predictor of osteoarthritis. Lijec Vjesn. 2009;131:22–6.
Reilly JJ, Methven E, McDowell ZC, Hacking B, Alexander D, Stewart L, et al. Health consequences of obesity. ArchDisChild. 2003;88:748–52.
Collaborators G 2015 O. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27.
Vidra N, Bijlsma MJ, Trias-Llimos S, Janssen F. Past trends in obesity-attributable mortality in eight European countries: an application of age-period-cohort analysis. Int J Public Health. 2018;63:683–92.
Charafeddine R, Van Oyen H, Demarest S. Trends in social inequalities in obesity: Belgium, 1997 to 2004. PrevMed. 2008;48:54–8.
Organization WH, others. European health report 2015: targets and beyond-reaching new frontiers in evidence. Copenhagen: World Health Organization. Regional Office for Europe; 2015.
Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity. 2008;16:2323–30.
Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378:815–25.
Sassi F, Devaux M, Cecchini M, Rusticelli E. The obesity epidemic: analysis of past and projected future trends in selected OECD countries. Paris: OECD; 2009.
Schneider H, Dietrich ES, Venetz WP. Trends and stabilization up to 2022 in overweight and obesity in Switzerland, comparison to France, UK, US and Australia. Int J Environ Res Public Health. 2010;7:460–72.
Thomas DM, Weedermann M, Fuemmeler BF, Martin CK, Dhurandhar NV, Bredlau C, et al. Dynamic model predicting overweight, obesity, and extreme obesity prevalence trends. Obesity. 2014;22:590–7.
Pineda E, Sanchez-Romero LM, Brown M, Jaccard A, Jewell J, Galea G, et al. Forecasting future trends in obesity across Europe: the value of improving surveillance. Obes Facts. 2018;11:360–71.
Keaver L, Webber L, Dee A, Shiely F, Marsh T, Balanda K, et al. Application of the UK foresight obesity model in Ireland: the health and economic consequences of projected obesity trends in Ireland. PLoS One. 2013;8:e79827.
McPherson K, Marsh T, Brown M, Britain G. Tackling obesities: future choices: Modelling future trends in obesity and the impact on health. UK: Government Office for Science; 2007.
Kelly T, Yang W, Chen C-S, Reynolds K, He J. Global burden of obesity in 2005 and projections to 2030. Int J Obes. 2008;32:1431–7.
Janssen F, Bardoutsos A, Vidra N. Obesity prevalence in the long-term future in 18 European countries and in the USA. Obes Facts. 2020;13:514–27.
Kanter R, Caballero B. Global gender disparities in obesity: a review. Adv Nutr. 2012;3:491–8.
Masters RK, Reither EN, Powers DA, Yang YC, Burger AE, Link BG. The impact of obesity on US mortality levels: the importance of age and cohort factors in population estimates. Am J Public Health. 2013;103:1895–901.
Reither EN, Olshansky SJ, Yang Y. New forecasting methodology indicates more disease and earlier mortality ahead for today’s younger Americans. Health Aff (Millwood). 2011;30:1562–8.
Chen Y, Dong G, Lin K, Lee Y. Gender difference of childhood overweight and obesity in predicting the risk of incident asthma: a systematic review and meta-analysis. Obes Rev. 2013;14:222–31.
Kautzky-Willer A, Harreiter J, Pacini G. Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes mellitus. Endocr Rev. 2016;37:278–316.
Reither EN, Hauser RM, Yang Y. Do birth cohorts matter? Age-period-cohort analyses of the obesity epidemic in the United States. Soc Sci Med. 2009;69:1439–48.
Slade T, Chapman C, Swift W, Keyes K, Tonks Z, Teesson M. Birth cohort trends in the global epidemiology of alcohol use and alcohol-related harms in men and women: systematic review and metaregression. BMJ Open. 2016;6:e011827.
Trzesniewski KH, Donnellan MB. Rethinking “generation me”: a study of cohort effects from 1976-2006. Perspect Psychol Sci. 2010;5:58–75.
Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357:370–9.
Lien N, Henriksen HB, Nymoen LL, Wind M, Klepp K-I. Availability of data assessing the prevalence and trends of overweight and obesity among European adolescents. Public Health Nutr. 2010;13:1680–7.
Diouf I, Charles MA, Ducimetière P, Basdevant A, Eschwege E, Heude B. Evolution of obesity prevalence in France: an age-period-cohort analysis. Epidemiol Camb Mass. 2010;21:360.
Jiang T, Gilthorpe MS, Shiely F, Harrington JM, Perry IJ, Kelleher CC, et al. Age-period-cohort analysis for trends in body mass index in Ireland. BMC Public Health. 2013;13:1–7.
Dobson A, Hockey R, Chan H-W, Mishra G. Flexible age-period-cohort modelling illustrated using obesity prevalence data. BMC Med Res Methodol. 2020;20:1–9.
Bell A, Jones K. The hierarchical age-period-cohort model: why does it find the results that it finds? Qual Quant. 2018;52:783–99.
Bell A. Age period cohort analysis: a review of what we should and shouldn’t do. Ann Hum Biol. 2020;47:208–17.
Demarest S, Van der Heyden J, Charafeddine R, Drieskens S, Gisle L, Tafforeau J. Methodological basics and evolution of the Belgian health interview survey 1997–2008. Arch Public Health. 2013;71:24.
Nguyen D, Hautekiet P, Berete F, Braekman E, Charafeddine R, Demarest S, et al. The Belgian health examination survey: objectives, design and methods. Arch Public Health. 2020;78:1–10.
Demarest S. Méthodologie. In: Van der Heyden J, Gisle L, Demarest S, Drieskens S, Hesse E, editors. Tafforeau J, editors. Bruxelles: ISP - Direction Opérationelle Santé Publique et Surveillance; 2010. p. 31–44.
Statistics UI for. International standard classification of education: ISCED 2011. Int Stand Classif EducISCED 2011. 2012.
Indicators DWP on S. The OECD list of social indicators. Organisation for Economic Co-operation and Development; [Washington, DC: Sold; 1982.
WHO. Body mass index - BMI. https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi. Accessed 15 Dec 2021.
Donnay P. Demografische vooruitzichten 2017-2070 Bevolking en huishoudens; 2018.
Yang Y, Land KC. A mixed models approach to the age-period-cohort analysis of repeated cross-section surveys, with an application to data on trends in verbal test scores. Sociol Methodol. 2006;36:75–97.
Yang Y, Land KC. Age-period-cohort analysis of repeated cross-section surveys - fixed or random effects? Sociol Methods Res. 2008;36:297–326.
Bell A, Jones K. Another ‘futile quest’? A simulation study of Yang and Land’s hierarchical age-period-cohort model. Demogr Res. 2014;30:333–60.
Riebler A, Held L. The analysis of heterogeneous time trends in multivariate age–period–cohort models. Biostatistics. 2010;11:57–69.
Riebler A, Held L. Projecting the future burden of cancer: Bayesian age–period–cohort analysis with integrated nested Laplace approximations. Biom J. 2017;59:531–49.
Rue H, Martino S, Chopin N. Approximate Bayesian inference for latent Gaussian models by using integrated nested Laplace approximations. J R Stat Soc Ser B Stat Methodol. 2009;71:319–92.
Smith TR, Wakefield J. A review and comparison of age-period-cohort models for Cancer incidence. Stat Sci. 2016;31:591–610.
R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2021.
Zore T, Palafox M, Reue K. Sex differences in obesity, lipid metabolism, and inflammation—a role for the sex chromosomes? Mol Metab. 2018;15:35–44.
Tramunt B, Smati S, Grandgeorge N, Lenfant F, Arnal J-F, Montagner A, et al. Sex differences in metabolic regulation and diabetes susceptibility. Diabetologia. 2020;63:453–61.
Svendsen MT, Bak CK, Sørensen K, Pelikan J, Riddersholm SJ, Skals RK, et al. Associations of health literacy with socioeconomic position, health risk behavior, and health status: a large national population-based survey among Danish adults. BMC Public Health. 2020;20:1–12.
Jeffery RW, Baxter J, McGuire M, Linde J. Are fast food restaurants an environmental risk factor for obesity? Int J Behav Nutr Phys Act. 2006;3:1–6.
Weihrauch-Blüher S, Kromeyer-Hauschild K, Graf C, Widhalm K, Korsten-Reck U, Jödicke B, et al. Current guidelines for obesity prevention in childhood and adolescence. Obes Facts. 2018;11:263–76.
Djojosoeparto SK, Kamphuis C, Vandevijvere S, Murrin C, Stanley I, Romaniuk P, et al. Strength of EU-level food environment policies and priority recommendations to create healthy food environments. Eur J Pub Health. 2022;32(3):504–11.
Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. N Engl J Med. 2017;376:254–66.
Styne DM, Arslanian SA, Connor EL, Farooqi IS, Murad MH, Silverstein JH, et al. Pediatric obesity—assessment, treatment, and prevention: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2017;102:709–57.
Ryan DH, Kahan S. Guideline recommendations for obesity management. Med Clin. 2018;102:49–63.
Løvhaug AL, Granheim SI, Djojosoeparto SK, Harrington JM, Kamphuis C, Poelman MP, et al. The potential of food environment policies to reduce socioeconomic inequalities in diets and to improve healthy diets among lower socioeconomic groups: an umbrella review. BMC Public Health. 2022;22:1–14.
Ampofo AG, Boateng EB. Beyond 2020: Modelling obesity and diabetes prevalence. Diabetes Res Clin Pract. 2020;167:108362.
Collaboration NRF, others. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet. 2016;387:1377–96.
Haug N, Geyrhofer L, Londei A, Dervic E, Desvars-Larrive A, Loreto V, et al. Ranking the effectiveness of worldwide COVID-19 government interventions. Nat Hum Behav. 2020;4:1303–12.
Stockwell S, Trott M, Tully M, Shin J, Barnett Y, Butler L, et al. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open Sport Exerc Med. 2021;7:e000960.
Drieskens S, Berger N, Vandevijvere S, Gisle L, Braekman E, Charafeddine R, et al. Short-term impact of the COVID-19 confinement measures on health behaviours and weight gain among adults in Belgium. Arch Public Health. 2021;79:1–10.
Clemmensen C, Petersen MB, Sørensen TI. Will the COVID-19 pandemic worsen the obesity epidemic? Nat Rev Endocrinol. 2020;16:469–70.
Fosse E, Winship C. Analyzing age-period-cohort data: a review and critique. Annu Rev Sociol. 2019;45:467–92.
Drieskens S, Demarest S, Bel S, De Ridder K, Tafforeau J. Correction of self-reported BMI based on objective measurements: a Belgian experience. Arch Public Health. 2018;76:1–8.
Acknowledgements
The authors would like to acknowledge the survey participants, the interviewers that were involved in the survey, and each member of the health interview team.
Funding
The Health Interview Survey is financed by the federal government (FSP Public Health), the Flemish Community, the French Community, the Brussels’ Region, the Walloon Region and the German Community.
Author information
Authors and Affiliations
Contributions
R.D.P. and B.D. wrote the main manuscript text. V.G. and M.C. performed the data management and descriptive statistics. R.D.P. and C.F. performed the APC-analysis and future projections based on the Bayesian APC model. S.D. coordinated and performed the survey in which data was gathered used in this manuscript. All authors contributed to the manuscript text and reviewed the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The survey was carried out in line with the Belgian privacy legislation and approved by the ethical committee of Ghent University. Participants gave informed consent prior to study participation.
Consent for publication
There are no details on individual participants within the manuscript.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
De Pauw, R., Claessens, M., Gorasso, V. et al. Past, present, and future trends of overweight and obesity in Belgium using Bayesian age-period-cohort models. BMC Public Health 22, 1309 (2022). https://doi.org/10.1186/s12889-022-13685-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-13685-w