Abstract
Background
In India, the prevalence of depression among older adults dealing with multiple health conditions varies between rural and urban areas due to disparities in healthcare access and cultural factors. The distinct patterns observed underscore the necessity for tailored research and interventions to address mental health inequalities among multimorbid older patients in diverse geographic contexts.
Methods
This study used data from the Longitudinal Ageing Study in India (LASI) wave 1 (2017–18). A total of 7,608 adults aged ≥ 60 years who were diagnosed with two or more chronic conditions (such as hypertension, diabetes, cancer, chronic lung disease, chronic heart diseases, stroke, bone/joint disease, any neurological or psychiatric diseases, and high cholesterol) were included in this study. Descriptive statistics, bivariate analysis, logistic regression estimates, and Fairlie decomposition method were used to accomplish the study’s objectives.
Results
The prevalence of depression among older adults with multimorbidity was 9.48% higher in rural areas (38.33%) than in urban areas (28.85%).. Older adults with multimorbidity belonging to the scheduled caste group were 40% more likely to experience depression. Moreover, those with multimorbidity and any form of disability in activities of daily living (ADL) were 93% more likely to experience depression than those without disability, whereas those with multimorbidity and perceived good general health were 65% less likely to suffer from depression than those with poor self-perceived health. Additionally, decomposition analysis revealed that education (35.99%), caste status (10.30%), IADL disability (19.30%), and perceived discrimination (24.25%) were the primary factors contributing to the differences in depression prevalence among older adults with multimorbidity between rural and urban areas.
Conclusions
We found significant rural–urban differences in depression among older Indians with multimorbidity. The findings underscore the need for targeted interventions that address the unique challenges faced by older patients in rural areas, including lack of social capital, discrimination, and limited resources that enable access to healthcare services. Policymakers and healthcare professionals must collaboratively design and implement effective strategies to improve the mental health and overall well-being of rural older adults, particularly those with multiple comorbidities.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
The growing issue of age-related multimorbidity and depression [1] in low- and middle-income countries (LMICs) poses a serious challenge to global health care systems [2]. Multimorbidity, which affects the majority of older adults, is the occurrence of two or more chronic diseases in an individual at the same time [3]. Depression [4], which is underdiagnosed and untreated along with other chronic diseases, has a negative impact on the overall health of individuals [5].
Findings from the burgeoning literature suggest a relationship between multimorbidity and depression, despite the lack of specific mechanisms between them [6]. Since they have a lower quality of life, more frequent use of medical services, and higher degrees of disability, pain, and cognitive impairment, people with multimorbidity are more susceptible to depressive disorders [6]. Barnett et al. (2012) suggested that depression with comorbidities covaries in a dose-dependent manner, such that an increase in the number of comorbid conditions is associated with a greater likelihood of depressive disorders and other mental health issues [3]. In addition, there is probably a statistically negative association between the prevalence of physical ailments and depression, and it was also evident from the study of Thombs et al. (2006) that subsequent depression is commonly associated with medical history [7].
According to recent estimates, 3.3 percent of Indians reported having depressive disorders, while nearly one in four had multimorbidity [8, 9]. Considering the situation in India, depression is a growing problem for individuals, especially older ones and is a substantial contributor to the future burden of the disease. The Global Burden of Disease Survey showed that those with multiple diseases were more likely to experience depressive symptoms than those without any diseases [10]. A recent study in India also reported that older adults with more chronic conditions are more vulnerable to depressive symptoms [11]. A study by Shubham et al. (2023) [12] investigated urban–rural differences in depressive symptoms among older adults with an urban disadvantage in India. Previous studies have also shown that individuals residing in urban areas may be more likely to experience depression than those living in rural areas because of the diminution in social connections and social isolation [13, 14]. The most recent studies on multimorbidity and associated depression among older adults in India were conducted in community settings [15,16,17,18].
However, researchers have been intrigued by the potential factors contributing to the differences in mental disorders between rural and urban areas [19,20,21,22,23,24]. A cross-sectional study that pooled data from a multicentre randomized controlled clinical trial in Canada found that adults with multiple chronic conditions and access to healthcare services in rural areas exhibited better mental health than their urban counterparts [24]. The difference in services between rural and urban areas is often of concern, making studies examining the differences between rural and urban depression important [25]. Moreover, a previous study found that urban–rural differences in depression [12] vary by country; therefore, it is suggested to conduct country-specific studies on urban–rural differences in depression to predict the essential approaches to managing the conditions.
Although there is a substantial amount of research on the risk factors and urban–rural gradients in depression among older population, none of these studies have examined the differences between urban and rural depression in older people with multiple chronic conditions. Thus, it is imperative to examine the differences between urban and rural areas regarding the mental health needs of aging individuals with multiple chronic conditions to effectively plan and implement mental health services and programs for rural communities where such needs may be insufficiently met. This study investigated the rural–urban gradient of depression among older Indian adults. The factors that contribute to rural–urban differences in the prevalence of depression among older adults with multiple chronic conditions were also decomposed in this study.
Materials and methods
Data source
This study utilized data from the Longitudinal Ageing Study in India (LASI) wave 1, a large-scale survey specifically for older adults aged 45 years and above, which is a longitudinal study of health and ageing [26]. Eventually, a unit of observation of LASI will be LASI’s age-eligible households (LEH) [26]. The LASI from the chosen families consisted of all males and females who were 45 years of age or older, as well as their spouses, irrespective of their age [26]. LASI offers reliable, organized, and ongoing scientific data on the population of older persons (aged 45 and over), including their physical, social, psychological, and economic well-being [26]. The targeted sample was chosen using a multistage stratified area probability cluster sampling design and consisted of non-institutionalized inhabitants of India's 31 states and six Union Territories [26].
The total household response rate was 96%, while the overall individual response rate was 87% (rural,89.6%; urban,83.6%) [26]. Each household and age-eligible individual provided a written informed consent. Four consent forms—household informed consent, individual informed consent, consent for the collection of blood samples for storage and subsequent use (DBS), and proxy consent—were used in compliance with the protection of human subjects [26]. The Indian Council of Medical Research (ICMR) provided the required instructions and ethical clearance to conduct the LASI.
Selection of the study sample
In this study, we included adults aged 60 years and above with comprehensive information on reported depression. Figure 1 shows detailed information on the inclusion and exclusion criteria for the study sample of older adults with multimorbidities. The presence of two or more chronic diseases is referred to as multimorbidity [27]. Nine distinct chronic diseases were covered by the LASI survey: (1) hypertension or high blood pressure, (2) diabetes, (3) cancer, (4) any chronic lung disease such as asthma, (5) chronic heart diseases, (6) stroke, (7) bone/joint disease, (8) any neurological or psychiatric diseases, and (9) high cholesterol [26]. These self-reports of chronic diseases were diagnosed [28] as was assessed through the question, "Has any health professional ever diagnosed you with the following chronic conditions or diseases?" [29]. An individual was coded as "No multimorbidity" if they had only one chronic disease or none at all and "Multimorbidity" if they had two or more chronic diseases [29]. Finally, the sample in this study included 7,608 older adults aged 60 years and above living with multiple chronic conditions. Among the study sample, 56.23% older adults resided in rural areas (in villages with a size that varies from 0–10,000 population) and 43.77% older adults resided in urban areas (in towns, wards and Census Enumeration Blocks).
Variable description
Outcome variable
The outcome of interest i.e., depressive symptoms was measured based on the Centre for Epidemiologic Studies Depression Scale (CES-D-10) among older adults, and it has four scale options, ranging from (1) rarely or never (< 1 day) to (4) most of the time (5–7 days). Respondents were asked ten different questions regarding their experiences over the past week, including difficulty concentrating, feeling depressed, low energy, afraid of something, alone, irritated by things, everything is an effort, and feeling cheerful, hopeful, and satisfied [26]. Among the 10 items on the scale, the first seven were based on negative symptoms, and the final three on positive symptoms. Those who responded to negative symptoms by stating "rarely or never (1 day)" and "occasionally (1 or 2 days)" were given a zero score, while the other two categories were coded as one. In addition, when positive symptoms were present, scoring was reversed. The composite score spanned a scale of 0 to 10, where a value of four or higher was considered indicative of depression [30].
The detailed measurements of the explanatory variables in this study are provided in Table 1.
Statistical analysis
Descriptive statistics and bivariate analysis have been used to compute the prevalence of depression with multimorbidity by socio-demographic, health-behavioural, psychosocial and household factors. The prevalence of depression among older adults with multimorbidity has been presented separately for rural and urban areas and conducted two sample proportion tests to compare the proportion of two independent groups of older patients in rural and urban areas [41]. Further, we performed binary logistic regression analysis [42] in the subsample of urban and rural to examine the difference in the magnitude of the associations between various background characteristics and depression among older adults with multimorbidity. All the results from the logistic regression analyses have been presented in the form of an odds ratio (OR) with 95% confidence interval (CI).
Following that, we used Fairlie decomposition to figure out the explanatory variables that contributed to the rural–urban difference in depression. The Blinder-Oaxaca decomposition is a frequently used method to identify and measure the variables associated with differences in the mean level of outcome between groups. While the Blinder-Oaxaca technique is used in linear models, the Fairlie, (2005) technique is suitable for non-linear models. The Fairlie decomposition method is a straightforward approach employed to estimate outcomes from a logit or probit model, originally introduced by Fairlie in 1999 [43]. The results of the decomposition have been explained in terms of coefficient and percent contribution by socio-demographic, health and behavioural, psychosocial and household factors. According to the Fairlie decomposition for a non-linear equation, Y = (kβ) can be written as,
where N R and N U indicate the sample size for rural and urban respectively, \({y}^{-R}\) and \({y}^{-U}\) are the average probability of the binary outcome of the interest (i.e., depression) for the group rural and urban, F is the cumulative distribution function from the logistic estimates, \({k}_{i}^{R}\) and \({k}_{i}^{U}\) are the set of the average value of the independent variable and \({\beta }^{-R}\) and \({\beta }^{-U}\) are the estimates of the beta coefficient for the rural and urban, respectively. All the analyses were conducted using STATA version 17.0 (Stata Corp, LP, college station, Texas) and sample weights were applied to adjust the effect of complex survey design.
Results
Background characteristics of the study population
Table 2 presents the demographic and socioeconomic characteristics of the respondents stratified by rural–urban sector in India. Among rural residents, little more than 56% aged 60–69 years and around 13% aged 80 + years whereas, in urban areas, 58% aged 60–69 years and 8.11% aged 80 + years. Notably, a significant percentage of both rural (70.58%) and urban (37.19%) residents lacked primary education, indicating high levels of illiteracy. When it came to obesity, urban dwellers (16.19%) had a higher prevalence compared to their rural counterparts (7.69%). In rural areas 35.69% and 62.71% were living with ADL and IADL difficulties, however, it was 25.95% and 48.79% in urban areas, respectively. Furthermore, 34.50% and 28.06% of the rural and urban respondents reported poor SRH, respectively. 50.11% and 40.78% of older adults residing in rural and urban areas were experiencing pain, respectively. 76.34% and 80.33% of the rural and urban older adults were not physically active, respectively. 13.05% rural and 10.58% urban older adults found be consuming alcohol. Additionally, 38.16%, and 27.12% of rural older adults were widowed, and never worked, respectively. Further, in urban areas 39.38% were widowed, and 37.10% were currently not working.
Rural–urban differences in the prevalence of depression among multimorbid older adults
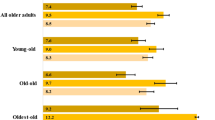
Table 3 presents an analysis of depression prevalence among older adults with multimorbidity based on various background characteristics. Specifically, older adults aged 80 and above residing in rural areas (49.12%) reported a higher prevalence of depression compared to their urban counterparts (32.73%), indicating a substantial difference of 16.39% (p ≤ 0.005). Furthermore, older adults with multimorbidity having secondary education exhibited a considerably greater disparity in depression prevalence between rural and urban areas, with rates of 37.05% and 16.64%, respectively. Older adults with multimorbidity experiencing ADL and IADL disabilities also reported a higher disparity in the prevalence of depression, with differences of 12.28% (p ≤ 0.001) and 13.41% (p ≤ 0.001), respectively. A total of 44.5% rural and 36.11% urban dwellers with multimorbidity reported pain. Moreover, among behavioural factors, significant higher urban–rural differences were found among older adults with multimorbidity who rarely engage in any physical activity, indicating a difference of 25.05% (p ≤ 0.001). Significant rural–urban differences in depression prevalence were also observed among older adults with multimorbidity who were not in marital union (45.62% vs. 28.07%), those who were never worked (42.93% vs. 27.04%), individuals belonging to the poorest strata (48.79% vs. 33.90%), and those residing in the northeast region of India (24.62% vs. 10.31%).
The greater prevalence of depression was observed among older adults with multimorbidity living in rural areas (38.33%) than urban areas (28.85%) (Fig. 2).
Estimates of multivariable logistic regression
Figures 3 and 4 presents the risk factors of depression among older adults with multimorbidity, separately for rural and urban areas. The findings presented in Fig. 3 indicate that in rural areas, older adults with primary education are significantly less likely to experience depression compared to those who are illiterate (AOR: 0.71; CI: 0.51- 0.99). Older adults facing difficulties in ADL are 1.93 times more likely to suffer from depression (AOR: 1.93; CI: 1.50–2.49), while those with IADL difficulties are 1.32 times more likely to experience depression (AOR: 1.32; CI: 1.03–1.70). Additionally, older adults who rate their overall health as very good are 0.65 times less likely to be depressed compared to those who report very poor self-rated health (AOR: 0.35; CI: 0.15–0.80). In terms of weight, compared to underweight respondents, obese individuals (AOR: 0.35; CI: 0.20–0.60) and overweight individuals (AOR: 0.52; CI: 0.37–0.72) are less likely to experience depression. Furthermore, older adults who are in a current marital union are 0.30 times less likely to suffer from depression compared to their counterparts (AOR: 0.70; CI: 0.54–0.90).
In urban areas (Fig. 4), older adults with difficulties in ADL have a 1.73 times higher likelihood of experiencing depression (AOR: 1.73; CI: 1.24–2.41). Older adults who report very poor self-rated health are more likely to suffer from depression compared to those who report very good self-rated health (AOR: 0.19; CI: 0.07–0.54). Additionally, older adults who rarely engage in any form of physical activity are less likely to develop depression compared to those who never participate in physical activity (AOR: 0.32; CI: 0.12–0.84).
Fairlie decomposition analysis of the contributing factors
Table 4 shows the findings of detailed decomposition of rural–urban differences of depression with multimorbidity among older adults. Percent contribution has been computed by division of each coefficient value of each factor included in the study by the total coefficient value and then multiplied by 100. Results from the decomposition analysis found that education and caste explained 46 percent of the rural–urban inequality in the prevalence of depression with multimorbidity among older adults. ADL disability, IADL disability and self-rated health are the other significant predictors that explained nearly 5 percent, 19 percent and 19 percent of the rural–urban inequality in the prevalence of depression with multimorbidity among older adults respectively. Perceived discrimination and ill-treatment behaviour also significantly explained 24 percent and 5 percent of the rural–urban inequality in the prevalence of depression with multimorbidity among older adults respectively.
Discussion
Based on nationally representative data from the LASI wave 1, the current study examined how the place of residence of an individual has influenced the prevalence of depression among older adults with co-morbid conditions in India. The prevalence of depression with multimorbidity among older persons significantly differed by 9.48% between rural and urban areas (38.33% vs 28.85% respectively). Socioeconomic variables such as education, work and caste status, psychosocial variables such as perceived discrimination, health insurance coverage and ill-treatment, and health-related variables such as ADL/IADL disability, self-rated health, experiences of pain and BMI contributed significantly to the rural–urban differences in depression prevalence among older adults with multimorbidity.
By evaluating the prevalence of depression among multimorbid older patients across various socio-demographic and socioeconomic groups, our study made an additional contribution to current knowledge and our findings have potential implications for framing policies. We observed an increased prevalence of depression with multimorbidity especially among participants in higher age groups, females and those with lower levels of education and wealth. The age and gender differentials in the levels of physical discomfort and psychological strain brought on by multimorbidity may explain this predicament, and the possibility of higher financial costs associated with the disease may also lead to greater depression levels among economically poor older people [3, 44]. Clinicians should consider the mental health of older patients especially women and oldest people when managing multimorbidity and provide immediate psychological assistance. Also, it is important to ensure that older adults with multimorbidity have access to an affordable treatment, especially in rural areas, which can significantly enhance their physical and mental well-being [45].
Our findings indicate significant variations in the association between self-rated health, ADL disability and experiences of pain with depression among older multimorbid patients in rural and urban areas. Limited healthcare facilities in rural regions can lead to potential delays in addressing physical and mental health conditions, including depression [46]. In contrast, urban areas benefit from better healthcare resources, allowing for prompt interventions influencing the connection between self-rated health and depression in older patients [32]. Increased community engagement and available social resources further contribute to better perceptions of own health. Limited opportunities in rural settings may affect the ability of older individuals to maintain independence in ADL, contributing to feelings of helplessness and depression. Conversely, greater community resources and engagement options in urban settings may positively impact older patients’ ability to manage ADL, potentially serving as a protective factor against depression in multimorbid patients [47]. Additionally, environmental factors, economic disparities, cultural attitudes, and lifestyle variations further contribute to the complex interplay between experiences of pain and depression in older patients [48, 49]. Understanding these multifaceted factors is essential for tailoring interventions and healthcare strategies to address the unique challenges faced by older patients in rural and urban settings dealing with the complex relationship between pain and depression [50, 51].
Furthermore, we found that older adults with multimorbidity living in both urban and rural areas reported higher levels of depression when they had no insurance coverage, experienced discrimination or ill-treatment, and the rates were higher in rural areas, which is in line with previous studies [52, 53]. This led us to the assumption that older adults who lived in rural areas tend to receive treatment for their chronic illnesses and, therefore, more likely to experience depressive symptoms, which was in line with the study of Keats, M [54]. The gender-based findings of our study imply that the prevalence of depression among multimorbid older women in rural areas may be linked to the role overload, which arises from a combination of work and domestic responsibilities [19]. Similar findings were reported in other cross-sectional studies in the US using data from the National Health Interview Survey (NHIS) [20]. The authors of the study posited that rural residents are more likely to exhibit characteristics associated with depression, such as poverty, chronic diseases, limitations in daily activities, and poor health status [20]. In contrast, a study in Canada revealed that the risk factors associated with depressive symptoms among adults aged 45–85 were somehow similar in rural and urban areas [23]. The findings suggest the need to research further "area-sensitive" healthcare interventions to have deeper understanding of social and environmental factors to the double burden of chronic conditions and mental illnesses in rural areas [55].
Decomposition analysis revealed that gender and caste are the two important factors contributing to the rural–urban difference in the prevalence of depression among multimorbid older patients. Similar to our findings, another study revealed that sex strongly influenced the association between multimorbidity and psychological well-being, and women with multimorbidity were more likely to experience depression [56]. Previous studies also revealed that women had a higher probability of experiencing psychological distress [57, 58]. A number of factors cause the significant adverse effects of multimorbidity on depression in older Indian women. One explanation for gender disparities is that women may be more predisposed to chronic diseases than men when they live in poverty, which increases the risk of further illnesses and the disease overburdening which ultimately lead to elevated depressive symptoms. Traditional Indian culture may also be an important factor that could explain the gender differences in depression among older patients in rural and urban areas. According to India's traditional culture, men should be the ones to participate in community-related meetings, while women should handle most household matters for the family [59]. When older women adequately care for themselves and their families, they have little time left over for socializing, which increases the demand for their time off. As a result, they find it challenging to manage their stress associated with chronic diseases, which leaves them vulnerable to mental health issues. Because of this, women with multimorbidity are more vulnerable than males to experiencing mental health issues.
BMI is also another important contributor to rural–urban differences in the prevalence of depression with multimorbidity among older adults, which is in accordance with the growing body of research [60,61,62,63,64]. This may be due to a range of factors, including limited access to healthcare services [65], social isolation [66], and greater exposure to environmental stressors [67, 68]. Research has shown that obesity is associated with an increased risk of depression, as well as a range of other health conditions such as diabetes, cardiovascular disease, and cancer [69]. However, we found an increased prevalence of depression among underweight older multimorbid patients in rural areas but not in urban areas. Overall, the urban–rural difference in the relationship between obesity and depression among multimorbid older patients is complex and multifactorial. More research is needed to better understand the underlying mechanisms driving these differences and to develop targeted interventions to reduce the burden of depression and multimorbidity in both rural and urban communities.
The strength of the study includes the reasonably large study samples, repeated measures, and validated questionnaires used to assess depression with multimorbidity among older adults. Another advantage is that we also compared the prevalence of depression among people with multiple morbidities in rural and urban settings. This finding may have significant medical implications for preventing and treating depression in older Indian adults. However, some limitations are also there. First, a number of people were excluded from the LASI survey either institutionalized or bedridden and may have multimorbidity and are more vulnerable to depression. Second, the CESD-10 was used to identify depression, which is not considered a clinical diagnosis and could contribute to misclassification bias given different cut points used in different studies for the probable depression. However, epidemiology research among older adults in India has shown that the CESD-10 is reliable and valid, as many studies have used this scale to measure depression [18, 70]. Third, the cross-sectional nature of the study does not allow any causal associations in this study; and there can be bidirectional or reciprocal associations, for example, between self-rated health and depression among multimorbid older patients. Fourth, self-reported data may make depression more likely to be misreported. In India, older people who need financial and physical help in their later years rely on their relatives. As a result, older adults could be afraid to disclose their mental health status in front of their relatives during the investigation. Moreover, due to the lack of data, we were unable to adjust factors like antidepressant medication use. Future research is required to confirm the findings considering these limitations.
Conclusions
The findings of the study shed light on the prevalence of depression among multimorbid older patients is a significant health concern that affects both rural and urban populations. However, there are notable differences between these two groups that have important implications for healthcare policy and delivery. Overall, older patients living in rural areas tend to experience higher rates of depression than those living in urban areas. This can be attributed to a variety of factors, including higher rates of disability, poor perceived health and limited access to healthcare services due to non-coverage of health insurance and discrimination, and lower social status. Additionally, rural communities often lack the resources and infrastructure necessary to adequately address the mental health needs of older patients.
In contrast, older adults with multimorbidity living in urban areas tend to have greater access to healthcare services and a wider range of support systems, which can help mitigate the risk factors of depressive symptoms. However, urban areas also have their own unique challenges, such as higher rates of economic inequalities and crime, which can exacerbate mental health issues. Given these differences, it is clear that a one-size-fits-all approach to addressing depression among older patients is not effective. Instead, healthcare policies and delivery systems must be tailored to the specific needs of each population. This may involve increasing access to mental health services in rural areas, developing community-based support systems, and addressing social determinants of health such as poverty and social exclusion. In addition, further research is needed to better understand the complex interplay among factors associated with depression in multimorbid persons, and rural–urban differences among those patients. Ultimately, addressing depression with multimorbidity among older adults in rural and urban areas will require a coordinated effort from policymakers, healthcare providers, and community organizations. By working together, we can develop effective solutions that reduce the risk factors of chronic conditions and depression, and improve the quality of life for older adults in all communities.
Availability of data and materials
The data are publicly available on the website,
References
Wainberg ML, Scorza P, Shultz JM, Helpman L, Mootz JJ, Johnson KA, et al. Challenges and opportunities in global mental health: a research-to-practice perspective. Curr Psychiatry Rep. 2017;19:1–10.
WHO. World report on ageing and health. World Health Organization; 2015.
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. The Lancet. 2012;380(9836):37–43.
Unützer J, Katon W, Sullivan M, Miranda J. Treating depressed older adults in primary care: narrowing the gap between efficacy and effectiveness. Milbank Q. 1999;77(2):225–56.
Newman AB, Brach JS. Gender gap in longevity and disability in older persons. Epidemiol Rev. 2001;23(2):343–55.
Read JR, Sharpe L, Modini M, Dear BF. Multimorbidity and depression: a systematic review and meta-analysis. J Affect Disord. 2017;221:36–46.
Thombs BD, Bass EB, Ford DE, Stewart KJ, Tsilidis KK, Patel U, et al. Prevalence of depression in survivors of acute myocardial infarction: review of the evidence. J Gen Intern Med. 2006;21:30–8.
Pati S, Swain S, Hussain MA, Van Den Akker M, Metsemakers J, Knottnerus JA, et al. Prevalence and outcomes of multimorbidity in South Asia: a systematic review. BMJ Open. 2015;5(10): e007235.
Lépine JP, Briley M. The increasing burden of depression. Neuropsychiatr Dis Treat. 2011;7(sup1):3–7.
Abegunde DO, Mathers CD, Adam T, Ortegon M, Strong K. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet. 2007;370(9603):1929–38.
Meher T, Muhammad T, Gharge S. The association between single and multiple chronic conditions and depression among older population in India: A comparative study between men and women. Int J Geriatr Psychiatry. 2022;37(1).
Kumar S, Chauhan S, Patel R, Kumar M, Simon DJ. Urban-rural and gender differential in depressive symptoms among elderly in India. Dial Health. 2023;2: 100114.
Mueller DP. The current status of urban-rural differences in psychiatric disorder. An emerging trend for depression. J Nerv Ment Dis. 1981;169(1):18–27.
Wirth L. Urbanism as a Way of Life. Am J Sociol. 1938;44(1):1–24.
Ansari S, Anand A, Hossain B. Multimorbidity and depression among older adults in India: Mediating role of functional and behavioural health. PLoS ONE. 2022;17(6): e0269646.
Olanrewaju O, Trott M, Smith L, López Sánchez GF, Carmichael C, Oh H, et al. Chronic physical conditions, physical multimorbidity, and quality of life among adults aged≥ 50 years from six low-and middle-income countries. Qual Life Res. 2022;1–11.
Singh S, Shri N, Dwivedi LK. An association between multimorbidity and depressive symptoms among Indian adults based on propensity score matching. Sci Rep. 2022;12(1):15518.
Muhammad T, Pai M, Ansari S. Gender differences in the association between cardiovascular diseases and major depressive disorder among older adults in India. Dial Health. 2023;2: 100107.
Weaver A, Himle JA, Taylor RJ, Matusko NN, Abelson JM. Urban vs rural residence and the prevalence of depression and mood disorder among African American women and non-Hispanic white women. JAMA Psychiat. 2015;72(6):576–83.
Probst JC, Laditka SB, Moore CG, Harun N, Powell MP, Baxley EG. Rural-urban differences in depression prevalence: implications for family medicine. Fam Med Kansas City. 2006;38(9):653.
Rost K, Zhang M, Fortney J, Smith J, Smith Jr GR. Rural-urban differences in depression treatment and suicidality. Med Care. 1998;1098–107.
Nzeadibe CT, Igboeli EE, Ajaero CK. Rural-urban differences in the prevalence and predictors of depression among adolescents in South Africa. South Afr J Child Health. 2018;2018(1):s71–4.
St John PD, Menec V, Tate R, Newall NE, Cloutier D, O’Connell M. Depressive symptoms in adults in rural and urban regions of Canada: a cross-sectional analysis of the Canadian Longitudinal Study on Aging. BMJ Open. 2021;11(12): e048090.
Bonnell LN, Clifton J, Rose GL, Waddell EN, Littenberg B. Urban-rural differences in mental and physical health among primary care patients with multiple chronic conditions: A secondary analysis from a randomized clinical trial. Int J Environ Res Public Health. 2022;19(23):15580.
Gruebner O, Rapp MA, Adli M, Kluge U, Galea S, Heinz A. Cities and Mental Health. Dtsch Arztebl Int. 2017;114(8):121–7.
International Institute for Population Sciences (IIPS). National Programme for Health Care of Elderly (NPHCE), MoHFW, Harvard T. H. Chan School of Public Health (HSPH) and the University of Southern California (USC). 2020;1–632.
Van den Akker M, Buntinx F, Knottnerus JA. Comorbidity or multimorbidity: what’s in a name? A review of literature. Eur J Gen Pract. 1996;2(2):65–70.
McKenna SP. Measuring patient-reported outcomes: moving beyond misplaced common sense to hard science. BMC Med. 2011;9(1):1–12.
Srivastava S, Joseph KJV, Dristhi D, Muhammad T. Interaction of physical activity on the association of obesity-related measures with multimorbidity among older adults: a population-based cross-sectional study in India. BMJ Open. 2021;11(5): e050245.
Kumar S, Nakulan A, Thoppil SP, Parassery RP, Kunnukattil SS. Screening for depression among community-dwelling elders: usefulness of the center for epidemiologic studies depression scale. Indian J Psychol Med. 2016;38(5):483–5.
Chauhan S, Srivastava S, Kumar P, Patel R. Decomposing urban-rural differences in multimorbidity among older adults in India: a study based on LASI data. BMC Public Health. 2022;22(1):502.
Saha A, Rahaman M, Mandal B, Biswas S, Govil D. Rural urban differences in self-rated health among older adults: examining the role of marital status and living arrangements. BMC Public Health. 2022;22(1):2175.
Barman P, Sarif N, Saha A. Association between natural hazards and postnatal care among the neonates in India: a step towards full coverage using geospatial approach. BMC Emerg Med. 2023;23(1):76.
Barman P, Saha A, Dakua M, Roy A. Does the intensity of religiosity and spirituality in later life improve mental well-being? Evidence from India. J Relig Spiritual Aging. 2022;1–21.
Saha A, Mandal B, Muhammad T, Barman P, Ahmed W. Gender-specific determinants of overweight and obesity among older adults in India: evidence from a cross-sectional survey, 2017–18. BMC Public Health. 2023;23:2313.
Mandal B, Pradhan KC, Mohanty P, Muhammad T. Migration status, physical limitations and associated self-rated health: a study of older Indian adults. BMC Geriatr. 2023;23(1):316.
Wuorela M, Lavonius S, Salminen M, Vahlberg T, Viitanen M, Viikari L. Self-rated health and objective health status as predictors of all-cause mortality among older people: A prospective study with a 5-, 10-, and 27-year follow-up. BMC Geriatr. 2020;20:1–7.
Wen CP, Cheng TYD, Tsai SP, Chan HT, Hsu HL, Hsu CC, et al. Are Asians at greater mortality risks for being overweight than Caucasians? Redefining obesity for Asians. Public Health Nutr. 2009;12(4):497–506.
Banerjee S, Kumar P, Srivastava S, Banerjee A. Association of anthropometric measures of obesity and physical activity with cardio-vascular diseases among older adults: Evidence from a cross-sectional survey, 2017–18. PLoS ONE. 2021;16(12): e0260148.
Saha A, Muhammad T, Mandal B, Adhikary M, Barman P. Socio-demographic and behavioral correlates of excess weight and its health consequences among older adults in India: Evidence from a cross-sectional study, 2017–18. PLoS ONE. 2023;18(10): e0291920.
Johnson RA, Verrill S, Moore DH. Two-sample rank tests for detecting changes that occur in a small proportion of the treated population. Biometrics. 1987;1:641–55.
Osborne JW. Best practices in quantitative methods. Sage; 2008.
Bauer TK, Sinning M. An extension of the Blinder-Oaxaca decomposition to nonlinear models. AStA Adv Stat Anal. 2008;92:197–206.
Chen F, Wei G, Wang Y, Liu T, Huang T, Wei Q, et al. Risk factors for depression in elderly diabetic patients and the effect of metformin on the condition. BMC Public Health. 2019;19:1–9.
Moran O, Doyle J, Smith S, Giggins O, Dinsmore J. Investigating the needs and concerns of older adults with multimorbidity and their healthcare professionals for conceivable digital psychotherapeutic interventions. Digital Health. 2022;8:20552076221089096.
Fortney JC, Pyne JM, Turner EE, Farris KM, Normoyle TM, Avery MD, Hilty DM, Unützer J. Telepsychiatry integration of mental health services into rural primary care settings. Int Rev Psychiatry. 2015;27(6):525–39.
Rubio E, Lázaro A, Sánchez-Sánchez A. Social participation and independence in activities of daily living: a cross sectional study. BMC Geriatr. 2009;9:1–1.
Remes O, Mendes JF, Templeton P. Biological, psychological, and social determinants of depression: a review of recent literature. Brain Sci. 2021;11(12):1633.
Mills SE, Nicolson KP, Smith BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth. 2019;123(2):e273–83.
Reynolds CF 3rd, Jeste DV, Sachdev PS, Blazer DG. Mental health care for older adults: recent advances and new directions in clinical practice and research. World Psychiatry. 2022;21(3):336–63.
Baker R, Camosso‐Stefinovic J, Gillies C, Shaw EJ, Cheater F, Flottorp S, Robertson N, Wensing M, Fiander M, Eccles MP, Godycki‐Cwirko M. Tailored interventions to address determinants of practice. Cochrane Database Syst Rev. 2015(4).
Yan C, Liao H, Ma Y, Xiang Q, Wang J. Association among multimorbidity, physical disability and depression trajectories: a study of urban–rural differences in China. Qual Life Res. 2021;30:2149–60.
You L, Yu Z, Zhang X, Wu M, Lin S, Zhu Y, et al. Association between multimorbidity and depressive symptom among community-dwelling elders in Eastern China. Clin Interv Aging. 2019;2273–80.
Keats MR, Cui Y, DeClercq V, Dummer TJB, Forbes C, Grandy SA, et al. Multimorbidity in Atlantic Canada and association with low levels of physical activity. Prev Med (Baltim). 2017;105:326–31.
Regitz-Zagrosek V. Sex and gender differences in health: Science & Society Series on Sex and Science. EMBO Rep. 2012;13(7):596–603.
Jiao C, Leng A, Nicholas S, Maitland E, Wang J, Zhao Q, et al. Multimorbidity and mental health: the role of gender among disease-causing poverty, rural, aged households in China. Int J Environ Res Public Health. 2020;17(23):8855.
Lin H, Jin M, Liu Q, Du Y, Fu J, Sun C, et al. Gender-specific prevalence and influencing factors of depression in elderly in rural China: A cross-sectional study. J Affect Disord. 2021;288:99–106.
Donner NC, Lowry CA. Sex differences in anxiety and emotional behavior. Pflügers Archiv Eur J Physiol. 2013;46(5):601–26.
Cerrato J, Cifre E. Gender inequality in household chores and work-family conflict. Front Psychol. 2018;9:1330.
Xiang X, An R. Obesity and onset of depression among US middle-aged and older adults. J Psychosom Res. 2015;78(3):242–8.
Forman-Hoffman VL, Yankey JW, Hillis SL, Wallace RB, Wolinsky FD. Weight and depressive symptoms in older adults: direction of influence? J Gerontol B Psychol Sci Soc Sci. 2007;62(1):S43-51.
Romano E, Ma R, Vancampfort D, Firth J, Felez-Nobrega M, Haro JM, et al. Multimorbidity and obesity in older adults from six low-and middle-income countries. Prev Med (Baltim). 2021;153: 106816.
Cui J, Sun X, Li X, Ke M, Sun J, Yasmeen N, et al. Association between different indicators of obesity and depression in adults in Qingdao, China: a cross-sectional study. Front Endocrinol (Lausanne). 2018;9:549.
Ahmadi SM, Keshavarzi S, Mostafavi SA, Bagheri LK. Depression and obesity/overweight association in elderly women: a community-based case-control study. Acta Med Iran. 2015;53(11):686–9.
Asante D, Rio J, Stanaway F, Worley P, Isaac V. Psychological distress, multimorbidity and health services among older adults in rural South Australia. J Affect Disord. 2022;309:453–60.
Alcañiz M, Riera-Prunera MC, Solé-Auró A. "When I Retire, I'll Move Out of the City": Mental Well-being of the Elderly in Rural vs. Urban Settings. Int J Environ Res Public Health. 2020;17(7).
Li LW, Liu J, Xu H, Zhang Z. Understanding rural-urban differences in depressive symptoms among older adults in China. J Aging Health [Internet]. 2015;28(2):341–62.
Lin L, Bai S, Qin K, Wong CKH, Wu T, Chen D, et al. Comorbid depression and obesity, and its transition on the risk of functional disability among middle-aged and older Chinese: a cohort study. BMC Geriatr. 2022;22(1):275.
Blasco BV, García-Jiménez J, Bodoano I, Gutiérrez-Rojas L. Obesity and depression: its prevalence and influence as a prognostic factor: A systematic review. Psychiatry Investig. 2020;17(8):715–24.
Han KM, Ko YH, Yoon HK, Han C, Ham BJ, Kim YK. Relationship of depression, chronic disease, self-rated health, and gender with health care utilization among community-living elderly. J Affect Disord. 2018;241:402–10.
Acknowledgements
The National Institute on Aging (R01 AG042778, R01 AG030153), the United Nations Population Fund, and the Government of India's Ministry of Health and Family Welfare all provided funding for the Longitudinal Aging Study in India Project. This particular study did not receive any funding.
Funding
The present research did not receive any grant from any funding agency, commercial entity, or not-for-profit organization.
Author information
Authors and Affiliations
Contributions
(i) AS contributed to the design of the work, acquisition, analysis of data. (ii) AS, TM and BM have participated in writing. (ii) AS, BM, WA and TM drafted the article and contributed to critical intellectual content and interpretation of the data. (iii) AS, BM, TM and WA have edited the final manuscript. (iv) AS, BM, TM and WA read, reviewed and approved the version to be published, (iv) AS, BM, TM and WA each author have participated adequately in work to take public responsibility for relevant portions of the content. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The survey agencies that conducted the field survey for the data collection have collected prior informed consent (written and verbal) from the respondent. Informed consent was obtained from all subjects and/or their legal guardian(s). The Indian Council of Medical Research (ICMR) extended the necessary guidance and ethical approval for conducting the LASI survey. The study is approved by the ethics committee of ICMR. All experimental protocols were approved by Indian Council of Medical Research. All the methods were conducted using relevant guidelines.
Informed consent was taken from a closed one/guardian or LAR (Legally authorized representative) prior to participation by an illiterate person.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Saha, A., Mandal, B., Muhammad, T. et al. Decomposing the rural–urban differences in depression among multimorbid older patients in India: evidence from a cross-sectional study. BMC Psychiatry 24, 60 (2024). https://doi.org/10.1186/s12888-023-05480-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-023-05480-7