Abstract
Background
The effectiveness of nitric oxide (NO) in reducing the risk of bronchopulmonary dysplasia (BPD) remains debatable. In this study, we performed a meta-analysis to guide clinical decision-making regarding the significance of inhaled NO (iNO) on the potential occurrence and outcomes of BPD in premature infants.
Methods
Data from clinical randomized controlled trials (RCTs) published in PubMed, Embase, Cochrane Library, Wanfang, China National Knowledge Infrastructure (CNKI) and Chinese Scientific Journal Database VIP databases for premature infants were searched from inception to March 2022. Review Manager 5.3 statistical software was used for heterogeneity analysis.
Results
Of the 905 studies retrieved, 11 RCTs met the screening criteria of this study. Our analysis showed that the iNO group was associated with a significantly lower incidence of BPD than the control group (relative risk [RR] = 0.91, 95% confidence interval (CI) 0.85-0.97, P = 0.006). We also observed no significant difference in the incidence of BPD between the two groups at the initial dose of 5 ppm (ppm) (P = 0.09) but those treated with 10 ppm iNO had a significantly lower incidence of BPD (RR = 0.90, 95%CI 0.81-0.99, P = 0.03). However, it should be noted that although the iNO group had an increased risk for necrotizing enterocolitis (NEC) (RR = 1.33, 95%CI 1.04-1.71, P = 0.03), cases treated with an initial dose of 10 ppm revealed no significant difference in the incidence of NEC compared with the control group (P = 0.41), while those treated with an initial dosage of 5 ppm of iNO had a significantly greater NEC rates than the control group (RR = 1.41, 95%CI 1.03-1.91, P = 0.03). Further, we observed no statistically significant differences in the incidence of in-hospital mortality, intraventricular hemorrhage (IVH) (Grade 3/4) or periventricular leukomalacia (PVL) and pulmonary hemorrhage (PH) between the two treatment groups.
Conclusions
This meta-analysis of RCTs showed that iNO at an initial dosage of 10 ppm seemed more effective in reducing the risk of BPD than conventional treatment and iNO at an initial dosage of 5 ppm in preterm infants at a gestational age of ≤34 weeks who required respiratory support. However, the incidence of in-hospital mortality and adverse events between the overall iNO group and Control were similar.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Bronchopulmonary dysplasia (BPD) is a severe respiratory condition that negatively impacts the survival of premature infants. The early survival rate of preterm infants has significantly improved with new developments in intensive care unit (ICU) technology. The prevalence of BPD in premature newborns at gestational age less than 28 weeks is reported to range from 48 to 68% [1]. The pathophysiology of BPD has shifted dramatically as a result of changes in epidemiology, clinical symptoms and prenatal and postnatal management of preterm infants. The “new” BPD is more frequent in premature newborns with a gestational age of less than 26 weeks and a birth weight of less than 1000 g [2]. Early non-invasive management of BPD includes the use of antenatal corticosteroids (ANS) to accelerate lung maturation in preterm birth from 24 weeks to 34 weeks of gestation [3], surfactant administration via a small catheter in spontaneously breathing infants to avoid mechanical respiratory support [4], inhaled bronchodilators to decrease airway resistance and wheezing and increase dynamic compliance [5], and many more [6]. However, the outcomes of current preventions for BPD remain unsatisfactory and should be further improved.
Nitric oxide (NO), a vasoactive chemical generated and released by vascular endothelial cells, selectively relaxes pulmonary vascular smooth muscle [7]. NO has selective diastolic effects on the pulmonary artery, which might minimize lung tissue oxidative damage and improve lung development, alveolarization and vascular remodeling [7]. The US Food and Drug Administration has approved inhaled NO (iNO) for the treatment of neonates aged ≥34 weeks with hypoxemic respiratory failure (HRF) and persistent pulmonary hypertension (PPHN) [8].
However, because iNO treatment might produce major adverse events such as oxidative stress damage and bleeding, the National Institutes of Health does not recommend it in premature infants [9]. Peluso et al. conducted a population-based cross-sectional research on premature infants at gestational age less than 35 weeks and found that iNO use increased from 2011 to 2016 compared to 2004 to 2010 [10]. Currently, there are disagreements regarding patient selection, age of inclusion, initial and maximum dose, course of treatment and efficacy on the usage of iNO. In this study, we performed a systematic review and meta-analysis to comprehensively and objectively evaluate the efficacy and safety of iNO in the prevention of BPD to aid clinical decision-making.
Methods
Literature search and selection criteria
We conducted a literature search on PubMed, EMBASE and the Cochrane Library from the databases’ inception to March 2022 using keywords “bronchopulmonary dysplasia” or “dysplasia, bronchopulmonary” combined with the terms “infant, premature”, “infants, premature”, “premature infant”, “preterm infants”, “infant, preterm”, “infants, preterm”, “preterm infant”, “premature infants”, “neonatal prematurity”, “prematurity, neonatal”, and “nitric oxide”, “oxide, nitric”, “nitrogen monoxide”, “monoxide, nitrogen”, “nitric oxide, endothelium-derived”, “endothelium-derived nitric oxide”, “nitric oxide, endothelium-derived”, “endogenous nitrate vasodilator”, “nitrate vasodilator, endogenous”, “vasodilator, endogenous nitrate”, “mononitrogen monoxide”, “monoxide, mononitrogen”. The languages used in the search were in Chinese and English. We also searched literature from the Wanfang, China National Knowledge Infrastructure (CNKI) and Chinese Scientific Journal Database VIP databases using Chinese terminologies of the same keywords and time period.
Using the above-mentioned search approach, two investigators independently screened the titles, abstracts and full texts of potentially eligible studies. Literature meeting the following criteria were included: (1) randomized controlled trials (RCTs); (2) involved premature infants at a gestational age ≤ 34 weeks who had HRF and received respiratory assistance; and (3) compared iNO to an inhalation placebo. Overall, the iNO group comprised premature infants who underwent conventional measure plus iNO, whereas the control group underwent conventional measure plus inhalation placebo. Studies were excluded if they: (1) were case reports, literature reviews, conference abstracts or systematic evaluations, (2) contained retrospective, non-random or incorrect random methods literature, (3) included animal experiments, (4) were repeated publication of research literature, and (5) did not have complete data of interest for this study or full text.
Data abstraction
Two investigators worked independently on the literature screening, data extraction and literature quality rating. Disagreements were handled by a third researcher. The last name of the first author, year of publication, sample size, age of enrollment, iNO start and maximum dose, duration of iNO, primary endpoints and diagnostic criteria were all collected from eligible papers using a predesigned excel form. Induced in-hospital mortality and BPD incidence were the key outcome metrics. Treatment safety data, based on the incidence of intraventricular hemorrhage (IVH) (Grade 3/4) or periventricular leukomalacia (PVL), pulmonary hemorrhage (PH) and necrotizing enterocolitis (NEC), were collected as secondary outcomes of measures, and subgroup analysis was performed on the initial iNO treatment dose of 5 ppm (ppm) and ≥ 10 ppm. In addition, the diagnosis of BPD was based on “classical” BPD criteria [11,12,13] in 5 studies [14,15,16,17,18], “new” BPD criteria [19, 20] in 5 studies [21,22,23,24,25].
Quality assessment
Two independent reviewers assessed the study designs. We used the Cochrane Systematic Review Manual to evaluate the quality of the observational studies based on the following six sections [26]: random allocation method; hidden allocation scheme; blind method to research objects, researchers and statisticians of research results; integrity of result data; publication bias; and other sources of bias. In the statistical process, the quality assessment was classified as follows. All indexes with low risk were evaluated as having low bias risk and the literature was of high quality; studies with more than 1 item of uncertainty risk were assessed as the risk of uncertainty bias, and studies with more than 1 item of high risk were assessed as the risk of high bias.
Statistical analysis
The Review Manager 5.3 software was used to conduct the meta-analyses. Heterogeneity was assessed using the Chi-square test. The fixed-effect model was adopted for analysis since I2 ≤ 50% and P ≥ 0.1 suggested statistical homogeneity between studies. The random-effect model was employed to analyze studies with I2 > 50% or P < 0.1. Dichotomous variables were analyzed using relative risk [RR] with 95% confidence interval (CI). Funnel plot was used to assess the risk of publication bias. P < 0.05 was used to determine statistical significance.
Results
Literature retrieval and basic features
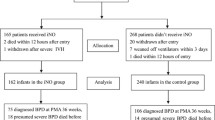
A total of 905 studies were initially retrieved. Following an initial screening, 172 studies were excluded due to duplication and after screening the title and abstract of the remaining records, 708 studies were further excluded. Following full-text assessments of the remaining studies, 11 RCTs were found eligible for this study, comprising 10 English and 1 Chinese literature [14,15,16,17,18, 21,22,23,24,25, 27]. There were 3651 preterm infants in all. Figure 1 illustrates the flow chart of literature retrieval, and Table 1 shows the characteristics of included research.
Quality assessment
Among the 11 RCT studies included in this study, 7 had a low risk of bias [14, 17, 18, 21,22,23,24], 2 had an uncertain risk of bias [16, 25], while the remaining 2 had a high risk of bias [15, 27]. Funnel plot results showed that most of the studies were located at the upper part of the funnel without obvious asymmetry, suggesting that there was no significant publication bias (Fig. 2).
Main outcome measures
Rate of in-hospital mortality
Eleven studies evaluated the effects of iNO versus Control on the in-hospital mortality of premature infants [14,15,16,17,18, 21,22,23,24,25, 27]. The fixed-effect model was employed because the heterogeneity test revealed that I2 = 29% and P = 0.17. The meta-analysis results showed no statistically significant difference in the in-hospital mortality rates between the iNO and control groups (RR = 1.02, 95% CI 0.89-1.16, P = 0.79, Fig. 3).
Rate of BPD
Eleven studies [14,15,16,17,18, 21,22,23,24,25, 27] examined the prevalence of BPD in the iNO and control groups. The fixed-effect model was employed as the heterogeneity test revealed that I2 = 0% and P = 0.91. The meta-analysis results revealed a significant difference in the rate of BPD between the two groups (RR = 0.91, 95% CI 0.85-0.97, P = 0.006), with iNO being significantly superior to Control in reducing the incidence of BPD. Subgroup analysis with varied initial treatment doses revealed no significant difference in the incidence of BPD between the iNO group and the control group at the initial dose of 5 ppm (RR = 0.92, 95% CI 0.84-1.01, P = 0.09). However, for a dose of ≥10 ppm, iNO was associated with a lower incidence of BPD compared with the control group (RR = 0.90, 95% CI 0.81-0.99, P = 0.03, Fig. 4).
Secondary outcome measures
Rate of IVH (grade 3/4) or PVL
Eight studies [15,16,17,18, 22,23,24, 27] documented the incidence of IVH (Grade 3/4) or PVL. The fixed-effect model was employed as the heterogeneity test revealed that I2 = 40% and P = 0.11. The results revealed no significant difference in the incidence of IVH (Grade 3/4) or PVL between the iNO group and the control group (RR = 0.92, 95% CI 0.77-1.09, P = 0.34, Fig. 5).
Rate of PH
Four investigations [16, 17, 23, 25] examined the prevalence of PH in the iNO and control groups. The fixed-effect model was employed because the heterogeneity test revealed that I2 = 0% and P = 0.83. The results of the meta-analysis revealed no significant difference in PH rate between the iNO and control groups (RR = 0.83, 95% CI 0.55-1.25, P = 0.37, Fig. 6).
Rate of NEC
Nine studies [14,15,16,17, 22,23,24,25, 27] assessed the prevalence of NEC in the iNO and control groups. The fixed-effect model was employed as the heterogeneity test revealed that I2 = 20% and P = 0.27. The meta-analysis results revealed a significant difference in NEC rate between the two groups (RR = 1.33, 95% CI 1.04-1.71, P = 0.03), indicating that iNO was associated with an increase in NEC incidence compared with the control group. However, iNO at an initial dose of ≥10 ppm had similar incidence of NEC to the control group (RR = 1.20, 95% CI 0.78-1.84, P = 0.41), while iNO at the initial dose of 5 ppm was associated with a significantly higher incidence of NEC than the control group (RR = 1.41, 95% CI 1.03-1.91, P = 0.03, Fig. 7).
Discussion
In conclusion, the meta-analysis results revealed a reduced incidence rate of BPD following the iNO measure but no statistically significant difference in in-hospital mortality versus the control group. Even though the designs of the available RCTs for the early use of iNO in preterm newborns varied, we did not observe a significant reduction in mortality and the differences were not statistically significant. Moreover, BPD incidence decreased by 10% (P = 0.03) when the initial dose of iNO was ≥10 ppm compared to the control group. Due to the varied methodologies and oxygenation indicators investigated in each included study, a direct meta-analysis could not be conducted. However, based on the study’s findings, we hypothesize that iNO decreased the incidence of BPD because it could increase oxygenation. Although multiple factors may influence BPD, inflammation is one of its most critical primary causes [28]. Earlier studies suggested that low NO levels could reduce lung inflammation [29], whereas subsequent research revealed that high NO levels could also exacerbate lung inflammation [30]. iNO may alleviate lung inflammation by reducing the incidence of BPD; however, the incidence of BPD could not be reduced significantly due to the dual effect of NO and contradictory results obtained from different tests. Additional research is required to determine whether pulmonary inflammation causes BPD and whether there are changes in inflammatory conditions, such as inflammatory factor levels. In this study, we also investigated the potential adverse effects of iNO based on the incidence of IVH (Grade 3/4) or PVL, PH, and NEC. INO had no statistically significant association with the incidence of IVH (Grade 3/4) or PVL and PH, but it may have increased the risk of NEC (subgroup analysis, iNO at an initial dose of 5 ppm versus control, P = 0.03; Fig. 7).
The results of nine studies comparing the incidence of NEC in the iNO group and the control group indicated that the incidence of NEC was 30% higher in the iNO group than in the control group, indicating that iNO may increase the risk of NEC, which was consistent with the findings of Van Meurs et al. [24]. Mercier et al. [23] reported a correlation between the induction of NEC by iNO and the gestational age of premature infants, which requires further investigation in future studies. The initial dose of ≥10 ppm was not statistically significant (P = 0.41) based on subgroup analysis employing varying initial treatment dosages. Askie et al. [31] also reported that a higher starting dose might be associated with improved HRF treatment outcomes in premature infants. In addition, the incidence of NEC in the iNO group was nearly 40% higher than in the control group (P = 0.03), suggesting that iNO may increase the risk of NEC in preterm newborns at an initial dose of 5 ppm. According to a 2016 review [32], excessive nitric oxide synthase (NOS) expression in the intestinal tract with high NO or superoxide nitrite levels led to epithelial cell loss and microbial infection, which resulted in NEC. Further research is necessary to determine whether iNO could increase the expression of NOS in the intestinal tract or result in excessive NO or superoxide nitrite production. In a clinical trial conducted in 2012 [33], iNO therapy was found to increase nitrite and nitrate levels in whole blood by approximately twofold, possibly due to a reduction in the oxygen-carrying capacity of blood cells in preterm newborns, thereby inducing NEC due to hypoxia in the digestive tract.
Although we demonstrated the potential effects of different doses of iNO on preventing the occurrence of BPD, the survival outcome was not significantly higher than with conventional treatment. Other potential alternatives to reduce the risk of BPD occurrence include early vitamin D, postnatal corticosteroids, and antibiotics [34,35,36]. Ge et al. found that early vitamin D supplementation (800 IU/day within 48 hours of birth for 28 days) could significantly reduce the incidence of BPD in premature infants [34]. According to Ramaswamy et al., an early, cumulative dose of systemic dexamethasone may be the best regimen for preventing mortality or BPD at 36 weeks postmenstrual age among 14 regimens from 62 studies [36]. Ozdemir et al. [35] concluded that clarithromycin effectively prevented BPD in preterm infants weighing between 750 and 1200 g and colonized with Ureaplasma urealyticum. Comparatively, we found in this study that the initial dose of iNO may be associated with BPD and NEC, which has important clinical implications for iNO prevention of BPD.
Several limitations were present in this study. (1) The “classical” and “new” forms of BPD have distinct diagnostic criteria. The “classical” BPD is based on RDS and emphasizes oxygen dependence and lung damage demonstrated by clinical and imaging evidence without grading the severity of BPD. Therefore, clinical criteria must be updated to evaluate the severity and long-term prognosis of BPD. (2) The limited overall sample size and the small number of included research samples affect the reliability of this study to some degree. (3) There was no subgroup analysis on birth weight, the start time of inhalation, and iNO inhalation dose range of preterm infants, which affected the reliability of this study. For optimal iNO clinical guidance, further research is required to clarify the clinical significance of iNO based on neonatal birth weight, persistent period, and inhalation range.
Conclusions
This review of RCTs on preterm infants at a gestational age of ≤34 weeks who require respiratory support indicates that iNO at an initial dosage of 10 ppm appeared more effective in reducing the risk of BPD than conventional treatment. In comparison, iNO at an initial dosage of 5 ppm had a comparable incidence of in-hospital mortality and adverse events compared with conventional treatment plus placebo. More research is required to improve the in-hospital mortality and safety of iNO in this setting.
Availability of data and materials
All data used during the study are available from the corresponding author by request.
Abbreviations
- NO:
-
Nitric oxide
- BPD:
-
Bronchopulmonary dysplasia
- iNO:
-
Inhaled NO
- RCTs:
-
Randomized controlled trials
- CNKI:
-
China National Knowledge Infrastructure
- RR:
-
Relative risk
- CI:
-
Confidence interval
- ppm:
-
Parts per million
- NEC:
-
Necrotizing enterocolitis
- IVH:
-
Intraventricular hemorrhage
- PVL:
-
Periventricular leukomalacia
- PH:
-
Pulmonary hemorrhage
- ICU:
-
Intensive care unit
- ANS:
-
Antenatal corticosteroids
- HRF:
-
Hypoxemic respiratory failure
- PPHN:
-
Persistent pulmonary hypertension
- NOS:
-
Nitric oxide synthase
References
Kinsella JP, Parker TA, Galan H, Sheridan BC, Halbower AC, Abman SH. Effects of inhaled nitric oxide on pulmonary edema and lung neutrophil accumulation in severe experimental hyaline membrane disease. Pediatr Res. 1997;41:457–63.
Merritt TA, Deming DD, Boynton BR. The ‘new’ bronchopulmonary dysplasia: challenges and commentary. Semin Fetal Neonatal Med. 2009;14:345–57.
Effect of corticosteroids for fetal maturation on perinatal outcomes. NIH Consens Statement. 1994;12(2):1-24.
Muehlbacher T, Bassler D, Bryant MB. Evidence for the Management of Bronchopulmonary Dysplasia in Very Preterm Infants. Children (Basel). 2021;8:298.
Khalaf MN, Hurley JF, Bhandari V. A prospective controlled trial of albuterol aerosol delivered via metered dose inhaler-spacer device (MDI) versus jet nebulizer in ventilated preterm neonates. Am J Perinatol. 2001;18:169–74.
Hwang JS, Rehan VK. Recent advances in bronchopulmonary dysplasia: pathophysiology, prevention, and treatment. Lung. 2018;196:129–38.
Klinger JR, Kadowitz PJ. The nitric oxide pathway in pulmonary vascular disease. Am J Cardiol. 2017;120:S71–s9.
Barrington KJ, Finer N, Pennaforte T, Altit G. Nitric oxide for respiratory failure in infants born at or near term. Cochrane Database Syst Rev. 2017;1:Cd000399.
Cole FS, Alleyne C, Barks JD, Boyle RJ, Carroll JL, Dokken D, et al. NIH consensus development conference statement: inhaled nitric-oxide therapy for premature infants. Pediatrics. 2011;127:363–9.
Peluso AM, Othman HF, Karnati S, Sammour I, Aly HZ. Epidemiologic evaluation of inhaled nitric oxide use among neonates with gestational age less than 35 weeks. Pediatr Pulmonol. 2022;57:427–34.
Walsh MC, Yao Q, Gettner P, Hale E, Collins M, Hensman A, et al. Impact of a physiologic definition on bronchopulmonary dysplasia rates. Pediatrics. 2004;114:1305–11.
Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM. Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics. 1988;82:527–32.
Toce SS, Farrell PM, Leavitt LA, Samuels DP, Edwards DK. Clinical and roentgenographic scoring systems for assessing bronchopulmonary dysplasia. Am J Dis Child. 1984;138:581–5.
Ballard RA, Truog WE, Cnaan A, Martin RJ, Ballard PL, Merrill JD, et al. Inhaled nitric oxide in preterm infants undergoing mechanical ventilation. N Engl J Med. 2006;355:343–53.
Dani C, Bertini G, Pezzati M, Filippi L, Cecchi A, Rubaltelli FF. Inhaled nitric oxide in very preterm infants with severe respiratory distress syndrome. Acta Paediatr. 2006;95:1116–23.
Kinsella JP, Cutter GR, Walsh WF, Gerstmann DR, Bose CL, Hart C, et al. Early inhaled nitric oxide therapy in premature newborns with respiratory failure. N Engl J Med. 2006;355:354–64.
Schreiber MD, Gin-Mestan K, Marks JD, Huo D, Lee G, Srisuparp P. Inhaled nitric oxide in premature infants with the respiratory distress syndrome. N Engl J Med. 2003;349:2099–107.
Van Meurs KP, Hintz SR, Ehrenkranz RA, Lemons JA, Ball MB, Poole WK, et al. Inhaled nitric oxide in infants >1500 g and <34 weeks gestation with severe respiratory failure. J Perinatol. 2007;27:347–52.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005;116:1353–60.
Hasan SU, Potenziano J, Konduri GG, Perez JA, Van Meurs KP, Walker MW, et al. Effect of inhaled nitric oxide on survival without bronchopulmonary dysplasia in preterm infants: a randomized clinical trial. JAMA Pediatr. 2017;171:1081–9.
Kinsella JP, Cutter GR, Steinhorn RH, Nelin LD, Walsh WF, Finer NN, et al. Noninvasive inhaled nitric oxide does not prevent bronchopulmonary dysplasia in premature newborns. J Pediatr. 2014;165:1104–8.e1.
Mercier JC, Hummler H, Durrmeyer X, Sanchez-Luna M, Carnielli V, Field D, et al. Inhaled nitric oxide for prevention of bronchopulmonary dysplasia in premature babies (EUNO): a randomised controlled trial. Lancet. 2010;376:346–54.
Van Meurs KP, Wright LL, Ehrenkranz RA, Lemons JA, Bethany Ball M, Kenneth Poole W, et al. Inhaled nitric oxide for premature infants with severe respiratory failure. N Engl J Med. 2005;353:13–22.
Wei Q, Pan X, Li Y, Feng L, Yao L, Liu G, et al. Efficacy of inhaled nitric oxide in premature infants with hypoxic respiratory failure. Chin J Contemp Pediatr. 2014;16:805–9.
Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:Ed000142.
Hascoet JM, Fresson J, Claris O, Hamon I, Lombet J, Liska A, et al. The safety and efficacy of nitric oxide therapy in premature infants. J Pediatr. 2005;146:318–23.
Sahni M, Bhandari V. Patho-mechanisms of the origins of bronchopulmonary dysplasia. Mol Cell Pediatr. 2021;8:21.
Grisham MB, Jourd'Heuil D, Wink DA. Nitric oxide. I. Physiological chemistry of nitric oxide and its metabolites:implications in inflammation. Am J Phys. 1999;276:G315–21.
Sharma JN, Al-Omran A, Parvathy SS. Role of nitric oxide in inflammatory diseases. Inflammopharmacology. 2007;15:252–9.
Askie LM, Ballard RA, Cutter GR, Dani C, Elbourne D, Field D, et al. Inhaled nitric oxide in preterm infants: an individual-patient data meta-analysis of randomized trials. Pediatrics. 2011;128:729–39.
Grishin A, Bowling J, Bell B, Wang J, Ford HR. Roles of nitric oxide and intestinal microbiota in the pathogenesis of necrotizing enterocolitis. J Pediatr Surg. 2016;51:13–7.
Ibrahim YI, Ninnis JR, Hopper AO, Deming DD, Zhang AX, Herring JL, et al. Inhaled nitric oxide therapy increases blood nitrite, nitrate, and s-nitrosohemoglobin concentrations in infants with pulmonary hypertension. J Pediatr. 2012;160:245–51.
Ge H, Qiao Y, Ge J, Li J, Hu K, Chen X, et al. Effects of early vitamin D supplementation on the prevention of bronchopulmonary dysplasia in preterm infants. Pediatr Pulmonol. 2022;57:1015–21.
Ozdemir R, Erdeve O, Dizdar EA, Oguz SS, Uras N, Saygan S, et al. Clarithromycin in preventing bronchopulmonary dysplasia in Ureaplasma urealyticum-positive preterm infants. Pediatrics. 2011;128:e1496–501.
Ramaswamy VV, Bandyopadhyay T, Nanda D, Bandiya P, Ahmed J, Garg A, et al. Assessment of postnatal corticosteroids for the prevention of bronchopulmonary dysplasia in preterm neonates: a systematic review and network Meta-analysis. JAMA Pediatr. 2021;175:e206826.
Acknowledgements
We express our appreciation to reviewers for their helpful comments on this manuscript.
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
Yi Zheng and Qi Wu were responsible for research design, data analysis, manuscript writing and revision. Shuping Han assisted in completing the analysis interpretation. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zheng, Y., Wu, Q. & Han, S. Inhaled nitric oxide in premature infants for preventing bronchopulmonary dysplasia: a meta-analysis. BMC Pediatr 23, 139 (2023). https://doi.org/10.1186/s12887-023-03923-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-023-03923-4