Abstract
Background
This study aims to compare the levels of intraocular cytokines between Fuchs uveitis syndrome (FUS) eyes and the senile cataract eyes. The association between inflammatory cytokine levels and cataract severity in FUS is evaluated to find the possible mechanism of cataract in FUS eyes.
Methods
A retrospective study of 28 eyes with FUS was performed. Auxiliary examinations were performed, including ophthalmic examinations, laser flare-cell photometry, and levels of inflammatory cytokines in the aqueous humor were measured. The control group included 25 eyes with senile cataract. Data on the aqueous humor inflammatory cytokines were compared between the two groups. The association between the aqueous humor cytokine levels and severity of posterior subcapsular cataract was assessed.
Results
There were 28 eyes with FUS in 27 patients. Unilateral involvement was noted in 26 patients (96.30%). Stellate keratic precipitates (KPs) were noted in 16 eyes (57.14%). Heterochromia was observed in 21.43% of affected eyes. Posterior subcapsular cataract (PSC) was observed in 16 of the 28 eyes. Eyes with FUS had significantly higher aqueous humor (AH) cytokine levels (VEGF, bFGF, IL-6, IL-8 and IL-10) compared with the control eyes (P < 0.05). There was a statistically significant positive correlation between the severity of cataract and IL-6 and IL-8 levels in the AH (τ = 0.664 and 0.634, respectively; P = 0.001, P = 0.002, respectively).
Conclusions
Expression of VEGF, bFGF, IL-6, IL-8 and IL-10 in the AH of FUS patients was significantly higher than in senile cataract eyes, and the aqueous humor levels of IL-6 and IL-8 were significantly positively associated with the severity of posterior subcapsular cataract. Our results imply that an inflammation mechanism may be involved in the early development of cataract in FUS.
Similar content being viewed by others
Background
Fuchs uveitis syndrome (FUS) is an intraocular inflammatory condition which was first described in 1906 by Fuchs [1]. FUS is an unilateral chronic recurrent non-granulomatous uveitis syndrome in about 90% of cases and accounts for 2 ~ 11% of uveitis, characterized by diffuse distribution of stellate keratic precipitates (KP), heterochromia, iris depigmentation, iris atrophy and early cataract formation [1]. Although the trigger mechanism of FUS is unknown, many studies have shown that immunological factors may play a role in the development of FUS [2,3,4]. However, few studies have compared inflammatory cytokine levels in the aqueous humor of FUS patients and normal eyes until now.
The most common complications in FUS patients are complicated cataract and glaucoma. Due to the long-term effects of inflammation, the average incidence of cataract in FUS is around 50% [5,6,7,8]. Cataract is a common complication of chronic or recurrent uveitis, which may be caused by intraocular inflammation, long-term use of corticosteroids, or a synergistic effect of both [9]. Vascular endothelial growth factor (VEGF) and pro-inflammatory cytokines play a role in the development of cataract in patients with non-infectious uveitis. However, no study has assessed the association between inflammatory cytokine levels and the severity of cataract.
The aims of this study were to evaluate the clinical, demographic characteristics, aqueous humor (AH) inflammatory cytokines during follow-up in Chinese patients diagnosed with FUS, to compare the AH inflammatory cytokines in FUS and the senile cataract eyes and to assess the association between the AH cytokine levels and the severity of posterior subcapsular cataract (PSC).
Methods
Study design and participants
We reviewed the medical records of 27 patients diagnosed with FUS who were admitted to our department, the Department of Ophthalmology, Beijing Chaoyang Hospital, Capital Medical University during May 2018 to May 2019. To serve as controls, 25 senile cataract patients who underwent surgery for cataract removal and intraocular lens implantation were enrolled. This study was performed in accordance with the standards of the Declaration of Helsinki. Considering the existence of invasive examination (paracentesis of anterior chamber) in this study, we have ethically recruited patients by explaining potential risk and they have voluntarily agreed for research analysis. Written informed consent was obtained from the subjects after potential risks involved with the study were explained to them. This study was approved by the Institutional Review Board of Beijing Chaoyang Hospital (No. 2018-4-3-3).
Diagnostic criteria: Diagnosis of FUS was principally based on the criteria of Kimura et al. [10]. The major criteria included the presence of (i) diffuse KPs (stellate or non-stellate), (ii) mild anterior chamber reaction defined as up to 2+ cells and flare, (iii) absence of posterior synechiae, and (iv) absence of ciliary congestion or red eye. The minor criteria for diagnosis included (i) heterochromia of the iris with/without iris depigmentary changes, (ii) presence of multiple nodules on iris, (iii) presence of vitreous opacities, and (iv) unilateral or bilateral involvement (one eye only was enrolled). Two of the four major criteria with or without the presence of minor criteria were required for diagnosis.
The demographic and clinical characteristics were obtained from each participant. Data included age, gender, ocular and medical history. 16 AH samples were obtained from patients with classical clinical signs of FUS while the disease was active. The other 11 patients did not undergo AH testing due to personal reasons. The intraocular antibody synthesis of rubella virus (RV) was confirmed by using the antibody index (AI) described in the literature [11].
Regular ophthalmologic examinations
Regular ophthalmic examinations, including slit-lamp biomicroscopy, best-corrected visual acuity (BCVA) on the Snellen chart, intraocular pressure (IOP), and fundoscopy with dilated pupils. Some detailed ophthalmic characteristics, such as keratic precipitates, iris atrophy, iris nodules, anterior chamber reaction and vitreous reaction were also evaluated. Evaluation of aqueous cells was done by laser flare photometry (Model KOWA FM-600, Hamamatsu Factory, Japan). The main manifestation of complicated cataract in FUS patients is PSC. PSC is classified from grade 1 to 5, according to the Lens Opacities Classification System III (LOCS III) [12].
Aqueous humor cytokine levels assessment
AH samples were collected. Patients were given topical anesthesia, and a 1-ml syringe was inserted at the peripheral cornea parallel to the iris. AH samples of 100 μL were extracted. The concentration of 6 immune mediators were measured with BD™ Cytometric Bead Array Kit (CBA), a BD FACScalibur flow cytometer and BD CBA software (Becton, Dickinson & Co, Franklin Lakes, NJ, USA): VEGF, basic fibroblast growth factor (bFGF), interleukin-6 (IL-6), interleukin-8 (IL-8), interleukin-10 (IL-10) and vascular cell adhesion molecule (VCAM). The detection thresholds of the assays were: VEGF 4.5 pg/ml, bFGF 3.4 pg/ml, IL-6 1.6 pg/ml, IL-10 0.13 pg/ml, VCAM 12.2 pg/ml, IL-8 1.2 pg/ml.
The levels of cytokines in the AH of the senile cataract group were also examined. The senile cataract group was used as the control group to analyze the elevated degree of inflammatory cytokine levels in the aqueous humor of FUS patients. Rubella virus (RV) IgG antibodies in the AH were measured quantitatively with a commercial ELISA kit (Virion/serion GmbH, Würzburg, Germany) in AH. The antibody activities were expressed in international units per mL (IU/mL). The assay was conducted according to the manufacturer’s instructions. Data analysis was performed using SERION easy base 4PL software.
Statistical analysis
The Mann-Whitney U test were used to compare parameters between the two groups. Descriptive statistics were calculated as the median, interquartile range (IQR) for non-normally distributed variables. To assess the difference in AH cytokine levels between FUS patients and the normal controls, box plots was created to allow visualization of the data. Kendall’s tau-b rank correlation was used to evaluate associations between age, the AH cytokine levels and severity of cataract. All analyses were performed with SPSS Statistics, version 22.0 (SPSS Inc., Chicago, IL, USA), and P < 0.05 was considered statistically significant 2-sided.
Results
Demographics and symptoms
The present study included 27 patients diagnosed with FUS. 15 (55.56%) of the patients were male, 12 (44.44%) of the patients were female. The median age at diagnosis was 32.00 years old (IQR 10.00). The median follow-up time was 19.00 months (IQR 15.00). The right eye was involved in 17 patients (62.96%) and the left eye was involved in 9 patients (33.33%), while 1 patients (3.70%) had bilateral involvement. Decreased visual acuity or blurred vision were the most common complaints at presentation (16 eyes, 57.14%). 11 patients (40.74%) had no symptoms. (Table 1).
Ocular findings
Stellate KPs were found in 16 (57.14%) FUS eyes. Anterior chamber (AC) reaction was observed in all of the affected eyes. Aqueous cells were observed in only 10 eyes, and aqueous flare was observed in 19 eyes. Although there were varying degrees of iris depigmentation in some patients, 6 of the eyes (21%) presented with heterochromia. 2 eyes (7.14%) had iris atrophy. Iris nodules were observed in 35.71% of the affected eyes. At diagnosis, 16 eyes (57.14%) presented with lens opacity: posterior subcapsular cataract (PSC), the median nuclear opalescence obtained from LOCS III was 2.00 (IQR 2.00). The duration of eyes with PSC was 18 (2.5) months, and the duration of eyes without PSC was 12 (0.5) months. Vitreous cells were noted in 7 eyes (25.00%). (Table 2).
Complications
The most common complication was PSC (16 eyes, 57.14%), followed by epiretinal membrane (4 eyes, 14.28%) and chorioretinal lesion (3 eyes, 10.71%). Observed complications were presented in Table 3.
Growth factors, AH cytokines and RV antibody levels
Growth factors and AH cytokines levels of 16 FUS eyes and 25 senile cataract eyes were showed in Table 4. Statistically significant differences were found between the two groups (Fig. 1). The mean concentrations of VEGF and bFGF in FUS eyes were higher than in the cataract eyes (P = 0.014; P = 0.026). The median (IQR) of IL-6, IL-8 and IL-10 were 36.35 (88.625) pg/mL, 17.90 (47.70) pg/mL and 3.25 (10.35) pg/mL, respectively. The FUS eyes had significantly higher AH cytokine levels (IL-6, IL-8 and IL-10) compared with the cataract eyes (P < 0.001). Levels of VCAM in FUS eyes were higher than in cataract eyes (P < 0.001). Viral antibody levels of RV were also shown in Table 4. 11 (68.75%) patients had a positive outcome for intraocular antibody production against RV, with IgG more than 20 IU/mL.
Correlation between AH cytokine levels and severity of PSC
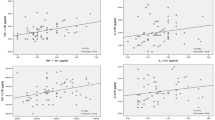
The main manifestation of complicated cataract in FUS patients is PSC. A correlation analysis between severity of PSC and age, levels of VEGF, bFGF, IL-6, IL-8 and IL-10 were shown in Table 5. There was a statistically significant positive correlation between the severity of PSC and IL-6, IL-8 levels (τ = 0.664 and 0.634, respectively; P = 0.001, P = 0.002, respectively). But there were no correlation between the severity of PSC and age, VEGF, bFGF and IL-10 levels (τ = 0.058, 0.117, 0.208 and 0.127, respectively; P > 0.05). (Table 5).
The severity of PSC can be classified as grade 1 to 5 according to the LOCS III grading system, as mentioned above. The number of patients with grade 5 PSC was 0. The scatter plot graph showing the relationship between IL-6 and IL-8 levels and PSC grade was shown in Fig. 2.
Discussion
Fuchs uveitis syndrome is an unilateral chronic recurrent non-granulomatous uveitis syndrome first described in 1906 by Fuchs, and its diagnosis is determined based on clinical manifestations [1]. In this paper, the clinical manifestations and ocular signs of 27 patients were studied in detail. We found FUS patients were characterized by a mild uveitis with characteristic stellate KPs, iris heterochromia, iris nodule, complicated cataract and vitreous inflammatory reaction in this study. Immune mediators play a crucial role in specific viral intraocular inflammation. The incidence of complicated cataract in FUS patients is positively correlated with the AH inflammatory cytokine levels.
The clinical features of FUS have been described in many studies, including blurred vision [13, 14], stellate KP [13, 15, 16], iris heterochromia [14], iris nodules [17], anterior chamber and vitreous opacities [18]. FUS is the most easily misdiagnosed uveitis because a comprehensive understanding of it is lacking, there are hidden incidence and its pathological mechanisms are complex. In the present study, the most common symptoms were blurred vision and floaters. Stellate KPs were noted in 16 eyes (57%). Heterochromia was observed in 21% of affected eyes. Iris nodules were present in 36% of the affected eyes. These results are similar to the above-mentioned studies.
FUS is an unilateral chronic recurrent non-granulomatous uveitis syndrome accounts for 2 ~ 11% of all uveitis. In our study, we tried to detect the levels of cytokines in the AH of FUS patients and showed several cytokines were significantly increased compared to the controls. Vascular endothelial growth factor (VEGF) is produced by endothelial cells, activated T lymphocytes [19]. It increases vascular permeability significantly and is associated with inflammatory and immune-mediated pathology [20,21,22]. VEGF concentrations increased significantly in the plasma of Behçet disease (BD) patients and in the AH of patients with uveitis with associated cystoid macular edema (CME) [23, 24]. Paroli et al. [25] found VEGF levels were significantly higher in both the AH and serum of uveitis patients as compared with control subjects. Simsek et al. [26] also suggested that VEGF levels were higher in the AH of patients with FUS than healthy controls. In the present study, we found that VEGF levels were significantly higher in FUS patients compared to controls, emphasizing the possible role of VEGF in intraocular inflammatory diseases.
Ocular inflammation occurs in a variety of human disease states, inflammation is thought to be initiated by eye-reactive T cells [27, 28]. The T helper 1 (TH1) cells secrete IFN-γ, TNF-α, IL-2, IL-8 and mediate cellular immunity, activate macrophages to kill intracellular pathogens, and play an important role in immune regulation in the induction of organ-specific autoimmune diseases and anti-infective immunity. The Th2 cells secrete cytokines including IL-4, IL-5, IL-6, IL-10, IL-13 [29] and mainly support humoral immunity, resisting extracellular pathogens. Some inflammatory factors may play an important role in the pathogenesis of FUS. In our study, we detected significantly increased levels of inflammatory factors (IL-6, IL-8 and IL-10) in FUS eyes compared with senile cataract eyes.
Some researchers believed that there is a correlation between the level of intraocular inflammatory factors and IOP, and conducted studies on patients with different diseases, but came to opposite conclusions. Takai et al. found the levels of TGF-1β, IL-8, and SAA were positively correlated with IOP in patients with open-angle glaucoma, indicating that cytokine networks in aqueous humor may have critical roles in IOP elevations [30]. Pohlmann et al. [31] examined clinical characteristics of Posner-Schlossman-Syndrome (PSS) and Fuchs’ Uveitis (FU) patients and found that immune mediators correlate negatively with IOP in the PSS patients. They also substantiated a similar composition of cytokines in PSS patients suffering from ocular hypertension and thus offers a potential explanation model for a negative correlation between mediators and IOP. We also analyzed the IOP level and did not detect significant difference between the two groups. Perhaps there is a correlation between the IOP level and the level of inflammatory factors in FUS patients. But we did not did not get similar results may be limited by small sample size, future study with large sample size should be carried out to confirm the correlation between IOP and the intraocular cytokines.
IL-6 can stimulate the proliferation, differentiation and function of cells involved in immune responses and play an important role in anti-infective immune response. Pohlmann D et al. [31] found that IL-6 was significantly higher in FUS and PSS patients compared to controls. In another study, T. gondii patients had twofold higher levels of IL-6 as compared to healthy subjects, which seems to confirm the presence of an inflammatory state [32]. Our study also found an increase in the level of IL-6 in FUS patients.
High IL-10 levels are mainly associated with active infectious uveitis and are considered to be important in early stages of infection [33]. In the previous study, a significant positive correlation between VKH disease and high levels of IL-10 was found by El-Asrar et al. [34]. Sijssens et al. [33] found that high IL-10 levels are associated with active infectious uveitis are considered to be important in early stage of infection. Joanna et al. also found the level of IL-10 to be fivefold higher in the course of toxoplasmosis than in healthy controls [32]. In FUS patients, increased levels of IL-10 are assumed to imply a distinctively acute inflammation triggered by RV. In our study, we detected significantly increased levels of IL-10 in FUS patients compared with normal eyes.
IL-8 has a role in chemokine functions. Mo JS et al. [35] found that IL-8 played a key role in the pathogenesis of intraocular inflammation in a rabbit model of uveitis. In the studies of humans, high levels of IL-8 have been detected in the aqueous humor of patients with acute anterior uveitis [36], Behçet disease (BD) or Vogt-Koyanagi-Harada (VKH) disease [37, 38]. Simsek et al. [26] also emphasized IL-8 levels were significantly higher in the aqueous humor of patients with FUS than in the AH of control subjects. We also found high IL-8 levels in FUS patients. IL-8 is a cytokine secreted by TH1 cells, which mainly mediate the production of immune antibodies related to the organism’s local inflammatory reaction and participate in cellular immunity and delayed hypersensitivity inflammation. IL-8 may act as a marker for inflammation in the AH in FUS. In our study, we detected immune mediators (IL-6, IL-8 and IL-10) increased significantly in FUS patients compared with cataract eyes, suggesting that IL-6, IL-10 and IL-8 may play an important role in anti-infective immune response and contribute to the viral response in FUS.
Cataract is a common complication of chronic or recurrent uveitis and is a sequelae to chronic intraocular inflammation and topical corticosteroid therapy. Cataracts occur in many types of uveitis, such as juvenile idiopathic arthritis-associated uveitis, BD, VKH and ocular toxoplasmosis. Cataract occurs in 17–36% of ocular BD patients and the most frequent complication is cataract [39, 40]. In VKH, cataract is the most common complication, with a prevalence of about 40%. The expression of pro-inflammatory cytokines in the cataract formation of non-infectious uveitis is gradually understood. Recurrent uveitis attacks may lead to lens permeability, then result in cataract [41]. Previous studies have emphasized that cataract is the most common complications in FUS patients [13, 16, 42]. Tugal-Tutkun et al. [16] found a 56% risk of cataract formation in FUS patients over their 8-year follow-up period. Yang et al. [13] found cataract was appeared in 70.7% of their FUS patients. Similarly, cataract was observed in 57.14% of patients in our study. The use of hormonal drugs to treat of inflammation also promotes the development of cataract.
Our research speculated that the occurrence of complicated cataract in FUS patients may be closely related to intraocular inflammation. Previous studies have confirmed that there is a correlation between inflammatory factors in the AH of uveitis patients and the occurrence of cataract. Tumor necrosis factor-α (TNF-α) can increase the mRNA level of laminin and type IV collagen, cause lens capsule fibrosis and the proliferation and migration of lens epithelial cells (LEC), thereby promoting the development of cataract. Transforming growth factor-β (TGF-β), which can induce lens cell pathology and lead to fibrotic cataract formation [43]. Recently, few studies have explored the association between cataract in FUS patients and the high expression of inflammatory cytokines in the AH. Thus, the relationship between the levels of intraocular cytokines and cataract in FUS is evaluated in this study.
Previous studies have confirmed that IL-1 can promote the proliferation of LEC and collagen synthesis, then resulting in the formation of cataract [44]. There are also some researches revealed that IL-1β can promote the expression of IL-6 and IL-8 through different pathways. Hu et al. [45] first reported the expression and secretion of IL-6 by human uveal melanocytes (UMs) and found IL-1β increases expression and secretion of IL-6 via the p38 MAPK/NF-kappaB pathway. Liu et al. [46] revealed that IL-1β induces IL-6 production in Müller cells by activation of IL-6 promoter activity predominantly through the p38 MAPK/NF-κB pathway. IL-1β potently stimulates IL-8 expression in Müller cells mainly through the p38 MAPK and ERK1/2 pathways [47]. Chang et al. [48] also found the important role of IL-1β in pulpal inflammatory responses via stimulation of IL-8 and ICAM-1 expression and secretion. The triggering effects of the inflammatory mediators, such as IL-1 and IL-6, may have an early stimulating effect on posterior capsular opacification (PCO) formation, and the actions of IL-1 may be mediated through the production of IL-6 [44].
The correlations between the severity of cataract and age, and AH cytokines (VEGF, bFGF, IL-6, IL-8 and IL-10) were explored in the present study. There was a statistically significant positive correlation between the severity of cataract in FUS patients and IL-6 and IL-8 level. These results confirmed that the occurrence of complicated cataract in FUS patients is positively correlated with the high expression of inflammatory factors. Further studies are needed to confirm their exact effect on the course of uveitis and complicated cataract.
The study has also several limitations. Firstly, this study only analyzed some inflammatory factors (IL-6, IL-10 and IL-8) in the AH of FUS patients, but did not explore the progression of other inflammatory factors in the AH, such as IL-1, TNF-α and TGF-β during the course of FUS, and their associations with cataract formation. Secondly, the sample size of this study was relatively small, which may have limited the statistical strength of the analysis.
Conclusions
In conclusion, the present results showed that in the current study the expression of inflammatory factors in the AH of FUS patients is significantly increased, and further revealed a positive correlation between the levels of IL-6 and IL-8 levels in the AH and the PSC grade in FUS, which may help to explain the early formation of cataract in FUS.
Availability of data and materials
A supplemental material which included the primary data has been uploaded accordingly (see Additional file 1).
Abbreviations
- AH:
-
Aqueous humor
- AI:
-
Antibody index
- BCVA:
-
Best-corrected visual acuity
- BD:
-
Behçet disease
- EGF:
-
Epidermal growth factor
- FUS:
-
Fuchs uveitis syndrome
- IL:
-
Interleukin
- IOP:
-
Intraocular pressure
- KP:
-
Keratic precipitates
- LEC:
-
Lens epithelial cells
- MMP:
-
Matrix metalloproteinase
- PSC:
-
Posterior subcapsular cataract
- PSS:
-
Posner–Schlossman Syndrome
- RV:
-
Rubella virus
- TGF:
-
Transforming growth factor
- TNF:
-
Tumor necrosis factor
- TH:
-
T helper
- Ums:
-
Human uveal melanocytes
- VCAM:
-
Vascular cell adhesion molecule
- VEGF:
-
Vascular endothelial growth factor
- VKH:
-
Vogt–Koyanagi–Harada syndrome
References
Fuchs EI. Ueber Komplikationen der Heterochromie. Ophthalmologica. 1906;15:191–212.
Stunf S, Petrovec M, Žigon N, Hawlina M, Kraut A, de Groot-Mijnes JDF, et al. High concordance of intraocular antibody synthesis against the rubella virus and Fuchs heterochromic uveitis syndrome in Slovenia. Mol Vis. 2012;18:2909–14.
de Groot-Mijnes JDF, ten Dam-van Loon NH, Weersink AJL, van Loon AM, Rothova A. Relationship between rubella virus and Fuchs heterochromic uveitis; 2 patients. Ned Tijdschr Geneeskd. 2007;151:2631–4.
de Groot-Mijnes JDF, de Visser L, Rothova A, Schuller M, van Loon AM, Weersink AJL. Rubella virus is associated with fuchs heterochromic iridocyclitis. Am J Ophthalmol. 2006;141:212–4.
Elgohary MA, McCluskey PJ, Towler HMA, Okhravi N, Singh RP, Obikpo R, et al. Outcome of phacoemulsification in patients with uveitis. Br J Ophthalmol. 2007;91:916–21.
Foster CS, Rashid S. Management of coincident cataract and uveitis. Curr Opin Ophthalmol. 2003;14:1–6.
Javadi M-A, Jafarinasab M-R, Araghi A-AS, Mohammadpour M, Yazdani S. Outcomes of phacoemulsification and in-the-bag intraocular lens implantation in Fuchs’ heterochromic iridocyclitis. J Cataract Refract Surg. 2005;31:997–1001.
Tejwani S, Murthy S, Sangwan VS. Cataract extraction outcomes in patients with Fuchs’ heterochromic cyclitis. J Cataract Refract Surg. 2006;32:1678–82.
Thorne JE, Woreta FA, Dunn JP, Jabs DA. Risk of cataract development among children with juvenile idiopathic arthritis-related uveitis treated with topical corticosteroids. Ophthalmology. 2010;117:1436–41.
Kimura SJ, Hogan MJ, Thygeson P. Fuchs’ syndrome of heterochromic cyclitis. AMA Arch Ophthalmol. 1955;54:179–86.
Ruokonen PC, Metzner S, Ucer A, Torun N, Hofmann J, Pleyer U. Intraocular antibody synthesis against rubella virus and other microorganisms in Fuchs’ heterochromic cyclitis. Graefes Arch Clin Exp Ophthalmol Albrecht Von Graefes Arch Klin Exp Ophthalmol. 2010;248:565–71.
Chylack LT, Wolfe JK, Singer DM, Leske MC, Bullimore MA, Bailey IL, et al. The Lens Opacities Classification System III. The Longitudinal Study of Cataract Study Group. Arch Ophthalmol Chic Ill 1960. 1993;111:831–6.
Yang P, Fang W, Jin H, Li B, Chen X, Kijlstra A. Clinical features of Chinese patients with Fuchs’ syndrome. Ophthalmology. 2006;113:473–80.
Nalçacıoğlu P, Çakar Özdal P, Şimşek M. Clinical characteristics of Fuchs’ uveitis syndrome. Turk J Ophthalmol. 2016;46:52–7.
Labbé A, Dupas B, Offret H, Baudouin C, Labetoulle M. Evaluation of keratic precipitates and corneal endothelium in Fuchs’ heterochromic cyclitis by in vivo confocal microscopy. Br J Ophthalmol. 2009;93:673–7.
Tugal-Tutkun I, Güney-Tefekli E, Kamaci-Duman F, Corum I. A cross-sectional and longitudinal study of Fuchs uveitis syndrome in Turkish patients. Am J Ophthalmol. 2009;148:510–515.e1.
Arellanes-García L, del Carmen P-DM, Recillas-Gispert C. Fuchs’ heterochromic iridocyclitis: clinical manifestations in dark-eyed Mexican patients. Ocul Immunol Inflamm. 2002;10:125–31.
Bouchenaki N, Herbort CP. Fuchs’ uveitis: failure to associate Vitritis and disc Hyperfluorescence with the disease is the major factor for misdiagnosis and diagnostic delay. Middle East Afr J Ophthalmol. 2009;16:239–44.
Ferrara N, Gerber H-P, LeCouter J. The biology of VEGF and its receptors. Nat Med. 2003;9:669–76.
Bates DO, Hillman NJ, Williams B, Neal CR, Pocock TM. Regulation of microvascular permeability by vascular endothelial growth factors. J Anat. 2002;200:581–97.
Clavel G, Bessis N, Lemeiter D, Fardellone P, Mejjad O, Ménard J-F, et al. Angiogenesis markers (VEGF, soluble receptor of VEGF and angiopoietin-1) in very early arthritis and their association with inflammation and joint destruction. Clin Immunol Orlando Fla. 2007;124:158–64.
Dvorak HF, Brown LF, Detmar M, Dvorak AM. Vascular permeability factor/vascular endothelial growth factor, microvascular hyperpermeability, and angiogenesis. Am J Pathol. 1995;146:1029–39.
Cekmen M, Evereklioglu C, Er H, Inalöz HS, Doganay S, Türköz Y, et al. Vascular endothelial growth factor levels are increased and associated with disease activity in patients with Behçet’s syndrome. Int J Dermatol. 2003;42:870–5.
Erdem F, Gündoğdu M, Kiki I, Ali Sari R, Kiziltunç A. Vascular endothelial and basic fibroblast growth factor serum levels in patients with Behçet’s disease. Rheumatol Int. 2005;25:599–603.
Paroli MP, Teodori C, D’Alessandro M, Mariani P, Iannucci G, Paroli M. Increased vascular endothelial growth factor levels in aqueous humor and serum of patients with quiescent uveitis. Eur J Ophthalmol. 2007;17:938–42.
Simsek M, Cakar Ozdal P, Akbiyik F, Citirik M, Berker N, Ozdamar Erol Y, et al. Aqueous humor IL-8, IL-10, and VEGF levels in Fuchs’ uveitis syndrome and Behçet’s uveitis. Int Ophthalmol. 2019;39:2629–36.
Caspi RR. Immune mechanisms in uveitis. Springer Semin Immunopathol. 1999;21:113–24.
Forrester JV, McMenamin PG. Immunopathogenic mechanisms in intraocular inflammation. Chem Immunol. 1999;73:159–85.
Mosmann TR, Cherwinski H, Bond MW, Giedlin MA, Coffman RL. Two types of murine helper T cell clone. I. Definition according to profiles of lymphokine activities and secreted proteins. J Immunol Baltim Md 1950. 1986;136:2348–57.
Takai Y, Tanito M, Ohira A. Multiplex cytokine analysis of aqueous humor in eyes with primary open-angle Glaucoma, exfoliation Glaucoma, and cataract. Investig Opthalmology Vis Sci. 2012;53:241.
Pohlmann D, Schlickeiser S, Metzner S, Lenglinger M, Winterhalter S, Pleyer U. Different composition of intraocular immune mediators in Posner-Schlossman-syndrome and Fuchs’ uveitis. PLoS One. 2018;13:e0199301.
Matowicka-Karna J, Dymicka-Piekarska V, Kemona H. Does toxoplasma gondii infection affect the levels of IgE and cytokines (IL-5, IL-6, IL-10, IL-12, and TNF-alpha)? Clin Dev Immunol. 2009;2009:374696.
Sijssens KM, Rijkers GT, Rothova A, Stilma JS, Schellekens PAWJF, de Boer JH. Cytokines, chemokines and soluble adhesion molecules in aqueous humor of children with uveitis. Exp Eye Res. 2007;85:443–9.
El-Asrar AMA, Struyf S, Kangave D, Al-Obeidan SS, Opdenakker G, Geboes K, et al. Cytokine profiles in aqueous humor of patients with different clinical entities of endogenous uveitis. Clin Immunol Orlando Fla. 2011;139:177–84.
Mo JS, Matsukawa A, Ohkawara S, Yoshinaga M. Role and regulation of IL-8 and MCP-1 in LPS-induced uveitis in rabbits. Exp Eye Res. 1999;68:333–40.
Verma MJ, Lloyd A, Rager H, Strieter R, Kunkel S, Taub D, et al. Chemokines in acute anterior uveitis. Curr Eye Res. 1997;16:1202–8.
Kaburaki T, Fujino Y, Kawashima H, Merino G, Numaga J, Chen J, et al. Plasma and whole-blood chemokine levels in patients with Behcet’s disease. Graefes Arch Clin Exp Ophthalmol Albrecht Von Graefes Arch Klin Exp Ophthalmol. 2003;241:353–8.
Abu El-Asrar AM, Struyf S, Descamps FJ, Al-Obeidan SA, Proost P, Van Damme J, et al. Chemokines and gelatinases in the aqueous humor of patients with active uveitis. Am J Ophthalmol. 2004;138:401–11.
Hooper PL, Rao NA, Smith RE. Cataract extraction in uveitis patients. Surv Ophthalmol. 1990;35:120–44.
Pivetti Pezzi P, Gasparri V, De Liso P, Catarinelli G. Prognosis in Behcet’s disease. Ann Ophthalmol. 1985;17:20–5.
Gupta R, Murray PI. Chronic non-infectious uveitis in the elderly: epidemiology, pathophysiology and management. Drugs Aging. 2006;23:535–58.
Liesegang TJ. Clinical features and prognosis in Fuchs’ uveitis syndrome. Arch Ophthalmol Chic Ill 1960. 1982;100:1622–6.
Shu DY, Lovicu FJ. Enhanced EGF receptor-signaling potentiates TGFβ-induced lens epithelial-mesenchymal transition. Exp Eye Res. 2019;185:107693.
Meacock WR, Spalton DJ, Stanford MR. Role of cytokines in the pathogenesis of posterior capsule opacification. Br J Ophthalmol. 2000;84:332–6.
Hu D-N, Chen M, Zhang DY, Ye F, McCormick SA, Chan C-C. Interleukin-1beta increases baseline expression and secretion of interleukin-6 by human uveal melanocytes in vitro via the p38 MAPK/NF-kappaB pathway. Invest Ophthalmol Vis Sci. 2011;52:3767–74.
Liu X, Ye F, Xiong H, Hu D-N, Limb GA, Xie T, et al. IL-1β induces IL-6 production in retinal Müller cells predominantly through the activation of p38 MAPK/NF-κB signaling pathway. Exp Cell Res. 2015;331:223–31.
Liu X, Ye F, Xiong H, Hu D, Limb GA, Xie T, et al. IL-1β Upregulates IL-8 production in human Müller cells through activation of the p38 MAPK and ERK1/2 signaling pathways. Inflammation. 2014;37:1486–95.
Chang M-C, Lin S-I, Pan Y-H, Lin L-D, Wang Y-L, Yeung S-Y, et al. IL-1β-induced ICAM-1 and IL-8 expression/secretion of dental pulp cells is differentially regulated by IRAK and p38. J Formos Med Assoc Taiwan Yi Zhi. 2019;118:1247–54.
Acknowledgments
Not Applicable.
Funding
This work is supported by Scientific Research Program of Beijing Municipal Commission of Education (Grant Number: KM202010025020) and Beijing Chaoyang 1351 talent training program (Grant Number: CYXX-2017-21). These fundings had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. This funding will not lead to any conflict of interests regarding the publication.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by HW and YT. The first draft of the manuscript was written by HW and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the local ethics committee of Beijing Chaoyang Hospital and with the 2013 Helsinki declaration. Written informed consent was obtained from each patient before the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Demographic and clinical data in this study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, H., Tao, Y. Relationship between the higher inflammatory cytokines level in the aqueous humor of Fuchs uveitis syndrome and the presence of cataract. BMC Ophthalmol 21, 108 (2021). https://doi.org/10.1186/s12886-021-01860-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-021-01860-3