Abstract
Background
[18 F]-Fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) has the ability to detect local and/or regional recurrence as well as distant metastasis. We aimed to evaluate the prognosis value of PET/CT in locoregional recurrent nasopharyngeal (lrNPC).
Methods
A total of 451 eligible patients diagnosed with recurrent I-IVA (rI-IVA) NPC between April 2009 and December 2015 were retrospectively included in this study. The differences in overall survival (OS) of lrNPC patients with and without PET/CT were compared in the I-II, III-IVA, r0-II, and rIII-IVA cohorts, which were grouped by initial staging and recurrent staging (according to MRI).
Results
In the III-IVA and rIII-IVA NPC patients, with PET/CT exhibited significantly higher OS rates in the univariate analysis (P = 0.045; P = 0.009; respectively). Multivariate analysis revealed that with PET/CT was an independent predictor of OS in the rIII-IVA cohort (hazard ratio [HR] = 0.476; 95% confidence interval [CI]: 0.267 to 0.847; P = 0.012). In the rIII-IVA NPC, patients receiving PET/CT sacns before salvage surgery had a better prognosis compared with MRI alone (P = 0.036). The recurrent stage (based on PET/CT) was an independent predictor of OS. (r0-II versus [vs]. rIII-IVA; HR = 0.376; 95% CI: 0.150 to 0.938; P = 0.036).
Conclusion
The present study showed that with PET/CT could improve overall survival for rIII-IVA NPC patients. PET/CT appears to be an effective method for assessing rTNM staging.
Similar content being viewed by others
Background
Nasopharyngeal carcinoma (NPC), arising from the squamous cells of epithelial lining in the nasopharynx, has an extremely marked geographical variations which was prevalent in Southern China [1, 2]. The crude incidence rate of NPC has reached 1.5 per 100,000 individuals, as reported by Globocan 2018 [3]. Over the years, advancements in treatment modalities, such as magnetic resonance imaging (MRI), intensity-modulated radiotherapy (IMRT), and induction chemotherapy (IC), have contributed to improved outcomes for NPC patients, with 5-year survival rates ranging from 85 to 90% [1, 4]. However, a subset of patients, approximately 10–20%, still experience locoregional tumor residues or recurrence [1, 4]. Therefore, it’s crucial to implement effective routine examinations for local and/or regional surveillance that can detect recurrence at an earlier stage and provide valuable guidance for treatment decisions [5].
MRI is the primary method used for routine monitoring of locoregional recurrence nasopharyngeal carcinoma (lrNPC) due to its high anatomical resolution and ability to provide detailed soft tissue contrast images [6, 7]. It can also provide accurate diagnosis, staging, and guidance for treatment of recurrence [7, 8]. Notably, [18 F]-Fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) is highly recommended as a systemic diagnostic tool in NPC due to its superior ability to detect both primary and/or regional recurrence as well as distant metastasis [9,10,11]. It is undeniable that [18 F]-FDG PET/CT is unable to detect skull base involvement and intracranial extension, as well as brown fat throughout the head and neck region, which may be one of the reasons why radiotherapists prefer MRI for staging and target area delineation in the initial diagnosis of nasopharyngeal carcinoma in clinical practice [12,13,14]. However, several studies have demonstrated that PET/CT has higher sensitivity and specificity compared to MRI in the diagnosis of local and lymph node recurrence in NPC at recurrence [15,16,17]. A meta-analysis by Li et al. showed that patients MRI versus (vs.). PET-CT had lower sensitivity (0.83 vs. 0.92) and specificity (0.78 vs. 0.89) in diagnosis of local recurrence and residue of NPC after IMRT [16]. Similarly, OuYang et al. reported that PET/CT vs. MRI had a higher sensitivity in detecting local (93.9% vs.79.3%; P < 0.001) and lymph nodes (90.9% vs. 67.6%; P < 0.001) recurrence and achieved more accurately recurrence staging (rStage) in NPC [17]. Altogether, it indicated that PET/CT can provide more accurate imaging for lrNPC. However, as an expensive examination, it is unclear whether PET/CT is necessary to perform after MRI or other imaging modalities have already detected the tumor with locoregional recurrence. In other words, it is unknown whether the advantages of PET/CT can translate into improved prognosis for lrNPC patients. Therefore, the aim of this study was to evaluate the prognostic value of PET/CT in lrNPC.
Materials and methods
Patients
A total of 451 eligible patients diagnosed with recurrent I-IVA nasopharyngeal carcinoma (NPC) between April 2009 and December 2015 were retrospectively identified from the NPC-specific database at the Sun Yat-sen University Cancer Center, which included a total of 10,126 patients. Inclusion criteria: (1) pathologically confirmed as NPC; (2) with MRI; (3) without distant metastasis at initial diagnosis and first recurrence; (4) confirmed with recurrent NPC with regular follow-up > 6 months after the end of first course radiotherapy. Exclusion criteria: (1) other malignant tumors; (2) insufficient monitoring data; (3) pregnancy or lactation. We then screened out Cohort B (III-IVA), Cohort C (rIII-IVA), and Cohort D (with PET/CT) based on eligible patients’ initial staging, recurrent staging (according to MRI), and whether PET/CT was performed at the time of recurrence detection, respectively (Fig. 1). The study protocol was approved by the committees of the Institutional Review Boards at Sun Yat-sen University Cancer Center.
Flow diagram of the study. Cohort B (III-IVA), Cohort C (rIII-IVA), and Cohort D (with PET/CT) were grouped according to initial staging, recurrent staging, and whether PET/CT was performed at the time of recurrence detection, respectively. Abbreviations: r: Recurrent; N: number; NPC: nasopharyngeal carcinoma; MRI: magnetic resonance imaging; PET/CT: positron emission tomography/computed tomography. *Based on the eighth edition of the Union for International Cancer Control/American Joint Committee on Cancer (UICC/AJCC) staging system according to MRI
Clinical characteristics
All clinical characteristics were obtained prior to retreatment for recurrent NPC. Each patient underwent following evaluations: physical examination, head and neck magnetic resonance imaging, and biopsy of the nasopharynx or cervical lymph nodes. Additionally, we collected the features of PET-CT, biopsy pathology, and cervical sonography within two months at the time of performing MRI. Blood examination variables before recurrent treatment included lactate dehydrogenase (LDH), C-reactive protein (rCRP), albumin (rALB), lymphocyte counts, neutrophil counts, and plasma Epstein-Barr virus (rEBV) DNA loads. Other demographic information of the patients was collected, including age, gender, history of re-radiotherapy, surgery, chemotherapy, initial T stage, recurrent T stage (rT stage), initial N stage, and recurrent N stage (rN stage).
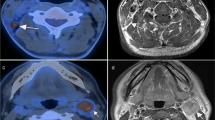
MRI and PET/CT protocol
MR images of the nasopharynx and neck regions were assessed using a 1.5-T or 3.0-T system prior to retreatment initiation. The evaluation included non-enhanced fast spin-echo (FSE) and enhanced fat-suppressed T1-weighted images (T1WIs) with a repetition time (TR) of 500–550 ms and an echo time (TE) of 10–15 ms on the axial, sagittal, and coronal planes. Additionally, all patients underwent T2-weighted FSE sequences with a TR of 4000–5500 ms and a TE of 90–110 ms in the axial plane. The scanning section thicknesses were 5 mm for the axial plane and 2–3 mm for the sagittal and coronal planes.
[18 F] FDG PET/CT images were acquired using the PET/CT scanner (Discovery ST, GE Healthcare, Waukesha, WI; or Biograph mCT, Siemens Healthcare, Erlangen, Germany) following PET/CT guidelines for tumor imaging [18]. Prior to the PET scan, a low-dose CT scan was performed. For the Discovery ST scanner, the CT scan parameters were as follows: automatic tube current modulation, tube voltage of 140 kV, collimation of 16 × 1.25 mm, rotation time of 0.8 s, and a slice thickness of 3.75 mm. For the Biograph mCT scanner, the CT scan parameters were as follows: tube current of 80–200 mAs, voltage of 120 kV, collimation of 32 × 1.25 mm, rotation time of 0.5s, and a slice thickness of 3 mm. Subsequent emission images were acquired for 3 min per bed position in two dimensions (2D) for the Discovery ST scanner or 1.5–2 min per bed in three dimensions (3D) with 6 to 8 beds for the Biograph mCT scanner. Before the injection of [18 F] FDG, patients fasted for over 6 h to control blood glucose levels. The patients were then injected with a specific dose of [18 F] FDG based on their body weight. Imaging was performed 55–80 min after the injection. PET/CT images were reconstructed using an ordered subset expectation maximization iterative image reconstruction method, and the slice thickness was 2 mm (3D) in a 200 × 200 matrix or 3.25 mm (2D) in a 128 × 128 matrix. And Chest radiography/computed tomography (CT), skeletal scintigraphy, and abdominal sonography/CT were performed to rule out distant metastasis.
Follow-up and outcomes
The primary endpoint was overall survival (OS) defined as freedom from the date of recurrent NPC diagnosis to the death due to any cause. Patients were followed every 3 months during the first 2 years after retreatment, then once every 6 months or until death. During follow-up period, various diagnostic procedures were conducted, including plasma EBV-DNA screening, physical examination, abdominal ultrasound, chest X-ray, and MRI of the nasopharynx and neck. For advanced or suspected distant metastasis, PET/CT or skeletal scintigraphy was recommended, and biopsies were performed if necessary.
Statistical analysis
The optimal cutoff value of LDH was achieved according to previous study, and of other continuous variables were determined by maximally selected rank statistics method with the “maxstat” package (Fig.S1) [19, 20]. The unadjusted actuarial rates were estimated using the Kaplan-Meier method, and differences between groups were assessed using the log-rank test. Multivariate analyses were conducted using the Cox proportional hazards model to calculate hazard ratios with a 95% confidence level (CI). Statistical significance was defined as two-tailed P-values < 0.05. All statistical analyses were performed using SPSS version 27.0 (IBM Corporation, Armonk, NY) and R (version 4.2.1) (http://www.r-project.org).
Results
Patients
A total of 451 NPC patients were enrolled in the study, with a median follow-up period of 32.6 months (interquartile range [IQR]: 15.8–47.2 months) and 164/451 (36.3%) patients died. The OS rates at 1, 3, and 5 years were 89.7%, 66.8%, and 52.4%, respectively. Baseline characteristics were shown in Table 1. Among these patients, 377 (83.6%), 174 (38.6%), and 132 (29.3%) were III-IVA stage, rIII-IVA stage, and with PET/CT, respectively (Fig. 1). After diagnostic recurrence, 29/451 (6.4%) patients experienced distant metastases (including 6 cases of lung, 9 cases of liver, 5 cases of bone, 1 case of mediastinal, and 8 cases of two or more sites).
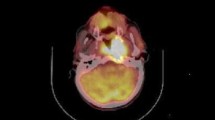
With PET/CT vs. MRI alone in prognosis
When patients were assigned to MRI alone and with PET/CT groups, there was no significant difference between them in terms of OS (P = 0.120; Fig. 2A). However, subgroup analysis revealed that in the III-IVA (B cohort) NPC, patients who with PET/CT exhibited significantly higher 5-year OS rates (MRI vs. with PET/CT: 45.2% vs. 56.4%, P = 0.045) (Table S1; Fig. 2C). Conversely, in the I-II group, there was no significant difference in OS revealed by log-rank test (P = 0.434; Fig. 2B); Similarly, significant difference in 5-year OS was also observed in the rIII-IVA (C cohort) patients (MRI: 21.0% vs. with PET/CT: 48.4%; P = 0.009), but not in rI-II cohort (P = 0.832; Table S1; Fig. 2D, E). Then, we excluded cases with censored data in B and C cohorts and conducted a multivariate analysis including rEBV DNA, rCRP, rALB, rNLR, retreatment strategies, and PET/CT in the III-IVA and rIII-IVA groups. The results demonstrated that with PET/CT was an independent predictor of OS in the rIII-IVA category (HR = 0.476; 95% CI: 0.267 to 0.847; P = 0.012), but not in the the III-IVA group (HR = 0.731; 95% CI: 0.459 to 1.165; P = 0.188) (Table 2; Table S2). Subsequently, to further investigate the value of PET/CT, a subset of 121 cases with complete data and maximum standardized uptake value (SUVmax) in Cohort D was selected for analysis. In the univariate analysis, it was found that patients classified as r0-rII (based on PET/CT) and SUVmax < 11.9 indicated better OS rates (P = 0.023; P = 0.015, respectively; Table 3).
Kaplan–Meier curves of overall survival for NPC patients stratified by the MRI and with PET/CT groups: (A) Total; (B) I-II; (C) III-IVA; (D) r0-II; (E) rIII-IVA. Abbreviations: NPC: nasopharyngeal carcinoma; r: Recurrent; MRI: magnetic resonance imaging; PET/CT: positron emission tomography/computed tomography. *Based on the eighth edition of the Union for International Cancer Control/American Joint Committee on Cancer (UICC/AJCC) staging system according to MRI
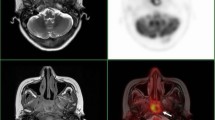
With PET/CT vs. MRI alone in staging
In cohort D, all patients underwent PET/CT and MRI scans. The rStage evaluated by MRI was r0 ([30/132] 22.7%), rI ([13/132] 9.8%), rII ([35/132] 26.5%), rIII ([24/132] 18.2%), and rIVA ([30/132] 22.7%) (Table S4; Fig. 3). In contrast, PET/CT resulted in a different distribution of rStage, with r0 ([4/132] 3%), rI ([9/132] 6.8%), rII ([36/132] 27.3%), rIII ([44/132] 33.3%), and rIVA ([39/132] 29.5%) (Table S4; Fig. 3). These results suggest that undergoing PET/CT is more likely to lead to an upstaging of rStage compared to MRI. Moreover, Using PET/CT sacns, rStage was identified as an independent predictor of OS (r0-rII vs. rIII-IVA; HR = 0.376; 95% CI: 0.150 to 0.938; P = 0.036) (Table 3); there were no significant differences in OS between those who underwent MRI (Table 3).
Comparison of the different stages of rT category(A), rN category(B), and rStage(C) for locoregional recurrent nasopharyngeal carcinoma staged by MRI and PET/CT. Abbreviations: r: Recurrent; NPC: nasopharyngeal carcinoma; MRI: magnetic resonance imaging; PET/CT: positron emission tomography/computed tomography. *Based on the eighth edition of the Union for International Cancer Control/American Joint Committee on Cancer (UICC/AJCC) staging system. P values were calculated using the Chi-squared test, ***P < 0.001
Treatment modified based on PET/CT
There were no significant statistical differences in terms of treatment strategies between the MRI alone and with PET/CT groups in the rIII-IVA and III-IVA NPC, as indicated in Supplementary Table S3 and Figure S2. However, there was a higher tendency for patients in the rIII-IVA and III-IVA groups who underwent PET/CT to receive surgery, while a smaller proportion received palliative treatment compared to patients in the r0-II and I-II stages (Fig. S3). In other words, the application of PET/CT increased the likelihood of patients receiving surgery. Furthermore, in the rIII-IVA NPC, patients receiving PET/CT sacns before salvage surgery had a better prognosis compared with MRI alone (P = 0.036) (Fig. 4 and Table S5).
Discussion
The present study enrolled the recurrent NPC patients without distant metastasis to investigate the prognostic role of PET/CT. The findings demonstrated that with PET/CT was an independent predictor of OS in lrNPC patients with stage rIII-IVA disease (HR = 0.476; P = 0.012; Table 2). Using PET/CT sacns, rStage was identified as an independent predictor of OS (r0-rII vs. rIII-IVA; HR = 0.376; 95% CI: 0.150 to 0.938; P = 0.036) (Table 3). Additionally, in the rIII-IVA NPC, patients receiving PET/CT sacns before salvage surgery had a better prognosis (Fig. 4; Table S5).
Of note, numerous studies have demonstrated the superiority of PET/CT over MRI in diagnosing primary and/or regional recurrence and accurately staging the recurrence of NPC after IMRT [15,16,17]. The present study is the first attempt to investigate whether these advantages of PET/CT can translate into improved prognosis in lrNPC. A previous study found that the rT3-4N0M0 NPC staged by PET/CT plus MRI had a higher 3-year OS than patients staged using MRI alone (adjusted HR = 0.34; P = 0.005) [17]. In contrast, for NPC patients with III-IVA and rIII-IVA staged by MRI, we found that with PET/CT also resulted in a better prognosis compared to MRI alone (P = 0.045 and P = 0.009, respectively) (Table S1; Fig. 2C, E). Furthermore, with PET/CT was identified as an independent predictor of OS in the rIII-IVA groups (HR = 0.476; P = 0.012; Table 2). However, there was no statistically significant difference between MRI alone and with PET/CT for all lrNPC in terms of OS (P = 0.120; Fig. 2A). These results suggest that the inclusion of PET/CT is necessary, particularly for patients with recurrent stage III-IVA disease who have already been evaluated using MRI.
We attempted to investigate the reasons behind the improved prognosis associated with the use of PET/CT. There was no statistically significant difference in terms of treatment strategies between MRI alone and with PET/CT in the rIII-IVA NPC. However, there was a tendency for a greater proportion of patients to undergo re-radiotherapy with PET/CT, which might provide a survival benefit, as shown in Supplementary Table S3 and Figure S2. We also observed that the application of PET/CT increased the likelihood of patients undergoing surgery (Fig. S3). One of the possible reasons is that surgeons may be more willing to use PET/CT for preoperative evaluation to rule out distant metastases. Additionally, our further study found that preoperative PET/CT could improve prognosis in rIII-IVA patients undergoing salvage surgery compared with MRI alone, suggesting that PET/CT may also provide a more precise surgical scope. In general, more precise identification of tumors often leads to more precise radiotherapy. Huang et al. demonstrated that PET/CT parameters could accurately delineate the target tumor for NPC radiotherapy [21]. Altogether, we hypothesized that based on the results of PET/CT, patients may receive more accurate surgical coverage and precise radiotherapy, which could render the improved prognosis.
Currently, the recurrent TNM (rTNM) of the Union for International Cancer Control/American Joint Committee on Cancer (UICC/AJCC) staging system is still widely used to predict recurrent NPC prognosis [14, 22]. However, there are variations in outcomes among patients with lrNPC in the same stage, as determined by rTNM [22,23,24]. Notably, the majority of rTNM staging was based on MRI evaluation. Interestingly, Sun et al. developed a nomogram that incorporated rT-stage (mostly evaluated by MRI) as well as other factors and demonstrated satisfactory performance in predicting OS for lrNPC [25]. Similarly, Wen et al. combined rT-stage (based on PET/CT) and other baseline parameters to construct a prediction model for lrNPC, which also achieved ideal discrimination for OS [26]. In our study, we identified rStage-PET/CT (based on PET/CT) was an independent predictor of OS. (r0-rII vs. rIII-IVA; HR = 0.376; P = 0.036) (Table 3). While there was no statistically significant difference in terms of OS among rStage based on MRI scans (Table 3). What’s more, consistent with previous studies, we also found that with PET/CT was more likely to result in upstaging of rStage compared to MRI (Table S3; Fig. 3) [17]. Therefore, based on the available evidence, PET/CT appears to be a more effective method than MRI for assessing recurrent TNM staging.
PET/CT parameters have been shown to provide valuable information about tumor metabolism, particularly the SUVmax of [18 F] FDG. Several studies have demonstrated that SUVmax is associated with prognosis in cancers [26,27,28,29]. Lin et al. revealed that a higher SUVmax of distant metastatic lesions was an unfavorable risk factors for OS (P = 0.005) in the metastatic NPC [28]. In de novo recurrent NPC patients, Yan et al. discovered the high SUVmax of metastatic lesions (≥ 10) at diagnosis independently predicted poor survival [27]. Our study found that SUVmax < 11.9 was associated with better 5-year OS rates (P = 0.011; Table 3) in the univariate analysis. However, it did not emerge as an independent predictor for OS in lrNPC. It is worth noting that these findings should be further explored in larger sample sizes or prospective studies to validate their significance.
Several shortcomings should be acknowledged. Firstly, the study design was retrospective, which may introduce selection bias. Therefore, further prospective studies are needed to validate the findings. Secondly, due to the limited sample size, the evaluation of PET/CT parameters across different treatment modalities might exist bias. Future studies can further investigate our findings in both endemic and non-endemic cohorts. Thirdly, other potential indicators derived from PET/CT, such as metabolic tumor volume (MTV) and total lesion glycolysis (TLG) can be adopted for prognosis prediction [26, 30]. Lastly, in present study, we adopted OS as the endpoint. Subsequent studies could consider using progression-free survival (PFS) as an endpoint indicator, which may provide more information on relapse associated with mortality.
Conclusions
To our knowledge, this study represents the first confirmation that the utilization of PET/CT can enhance the survival outcomes of patients with the rIII-IVA NPC. Additionally, PET/CT appears to be a more effective method than MRI for assessing rTNM staging.
Data availability
The datasets generated and/or analyzed during the current study at the Sun Yat-sen University Cancer Center are not publicly available due to Chinese law and regulations but are available from the corresponding author on reasonable request.
Change history
25 April 2024
A Correction to this paper has been published: https://doi.org/10.1186/s12885-024-12276-9
References
Chen YP, Chan ATC, Le QT, Blanchard P, Sun Y, Ma J. Nasopharyngeal carcinoma. Lancet. 2019;394(10192):64–80.
Qiao H, Tan XR, Li H, Li JY, Chen XZ, Li YQ, Li WF, Tang LL, Zhou GQ, Zhang Y, et al. Association of Intratumoral Microbiota with prognosis in patients with nasopharyngeal carcinoma from 2 hospitals in China. JAMA Oncol. 2022;8(9):1301–9.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Zhang MX, Li J, Shen GP, Zou X, Xu JJ, Jiang R, You R, Hua YJ, Sun Y, Ma J, et al. Intensity-modulated radiotherapy prolongs the survival of patients with nasopharyngeal carcinoma compared with conventional two-dimensional radiotherapy: a 10-year experience with a large cohort and long follow-up. Eur J Cancer. 2015;51(17):2587–95.
Lu T, Xu H, Huang W, Zong J, Pan C, Huang C, Xiao Y, Chen B, Li J, Pan J, et al. Constructing an individualized surveillance framework for nasopharyngeal carcinoma based on a dynamic risk-adapted approach. Radiother Oncol. 2023;185:109716.
Lee AWM, Ng WT, Chan JYW, Corry J, Mäkitie A, Mendenhall WM, Rinaldo A, Rodrigo JP, Saba NF, Strojan P, et al. Management of locally recurrent nasopharyngeal carcinoma. Cancer Treat Rev. 2019;79:101890.
Meng K, Tey J, Ho FCH, Asim H, Cheo T. Utility of magnetic resonance imaging in determining treatment response and local recurrence in nasopharyngeal carcinoma treated curatively. BMC Cancer. 2020;20(1):193.
Lu ZJ, Liu T, Lin JY, Pei ST, Guo L, Liu SL, Mai HQ. Identifying the prognostic value of MRI-based tumor response and predicting the risk of radio-resistance in re-radiotherapy for locally recurrent nasopharyngeal carcinoma. Radiother Oncol. 2023;183:109635.
Tang LQ, Chen QY, Fan W, Liu H, Zhang L, Guo L, Luo DH, Huang PY, Zhang X, Lin XP, et al. Prospective study of tailoring whole-body dual-modality [18F]fluorodeoxyglucose positron emission tomography/computed tomography with plasma Epstein-Barr virus DNA for detecting distant metastasis in endemic nasopharyngeal carcinoma at initial staging. J Clin Oncol. 2013;31(23):2861–9.
Qiu HZ, Zhang X, Liu SL, Sun XS, Mo YW, Lin HX, Lu ZJ, Guo J, Tang LQ, Mai HQ, et al. M1 stage subdivisions based on (18)F-FDG PET-CT parameters to identify locoregional radiotherapy for metastatic nasopharyngeal carcinoma. Ther Adv Med Oncol. 2022;14:17588359221118785.
Chen C, Xu T, Qiu X, Xie S, You Z, Hu Y, Zheng Y, Liang Z, Huang C, Chen T, et al. Selectively recommend (18)F-FDG PET/CT for patients with de novo nasopharyngeal carcinoma in endemic areas. Radiat Oncol. 2021;16(1):229.
Li H, Kong Z, Xiang Y, Zheng R, Liu S. The role of PET/CT in radiotherapy for nasopharyngeal carcinoma. Front Oncol. 2022;12:1017758.
Tang LL, Guo R, Zhang N, Deng B, Chen L, Cheng ZB, Huang J, Hu WH, Huang SH, Luo WJ, et al. Effect of Radiotherapy alone vs Radiotherapy with Concurrent Chemoradiotherapy on Survival without Disease Relapse in patients with low-risk nasopharyngeal carcinoma. A Randomized Clinical Trial. JAMA. 2022;328(8):728–36.
Pan JJ, Ng WT, Zong JF, Chan LL, O’Sullivan B, Lin SJ, Sze HC, Chen YB, Choi HC, Guo QJ, et al. Proposal for the 8th edition of the AJCC/UICC staging system for nasopharyngeal cancer in the era of intensity-modulated radiotherapy. Cancer. 2016;122(4):546–58.
Wei J, Pei S, Zhu X. Comparison of 18F-FDG PET/CT, MRI and SPECT in the diagnosis of local residual/recurrent nasopharyngeal carcinoma: a meta-analysis. Oral Oncol. 2016;52:11–7.
Li Z, Li Y, Li N, Shen L. Positron emission tomography/computed tomography outperforms MRI in the diagnosis of local recurrence and residue of nasopharyngeal carcinoma: an update evidence from 44 studies. Cancer Med. 2019;8(1):67–79.
OuYang PY, Liu ZQ, Lin QG, He Y, Guo ZX, Yao WY, Xu SK, Peng QH, Xiao SM, Li J, et al. Benefit of [(18)F] FDG PET/CT in the diagnosis and salvage treatment of recurrent nasopharyngeal carcinoma. Eur J Nucl Med Mol Imaging. 2023;50(3):881–91.
Delbeke D, Coleman RE, Guiberteau MJ, Brown ML, Royal HD, Siegel BA, Townsend DW, Berland LL, Parker JA, Hubner K, et al. Procedure guideline for tumor imaging with 18F-FDG PET/CT 1.0. J Nucl Med. 2006;47(5):885–95.
Zhao Q, Dong A, Cui C, Ou Q, Ruan G, Zhou J, Tian L, Liu L, Ma H, Li H. MRI-Based metastatic nodal number and Associated Nomogram Improve Stratification of Nasopharyngeal Carcinoma patients: potential indications for individual induction chemotherapy. J Magn Reson Imaging. 2022.
Huang L, Sim AYL, Wu Y, Liang Z, Li K, Du Y, Ong EHW, Tan HQ, Wee JTS, Xie Y, et al. Lactate dehydrogenase kinetics predict chemotherapy response in recurrent metastatic nasopharyngeal carcinoma. Ther Adv Med Oncol. 2020;12:1758835920970050.
Huang Z, Tang S, Chen Z, Wang G, Shen H, Zhou Y, Wang H, Fan W, Liang D, Hu Y, et al. TG-Net: combining transformer and GAN for nasopharyngeal carcinoma tumor segmentation based on total-body uEXPLORER PET/CT scanner. Comput Biol Med. 2022;148:105869.
You R, Zou X, Wang SL, Jiang R, Tang LQ, Zhang WD, Li L, Zhang MX, Shen GP, Guo L, et al. New surgical staging system for patients with recurrent nasopharyngeal carcinoma based on the AJCC/UICC rTNM classification system. Eur J Cancer. 2015;51(13):1771–9.
Liu Q, Sun X, Li H, Zhou J, Gu Y, Zhao W, Li H, Yu H, Wang D. Types of Transnasal Endoscopic Nasopharyngectomy for recurrent nasopharyngeal carcinoma: Shanghai EENT Hospital Experience. Front Oncol. 2020;10:555862.
Li W, Liu Q, Xu H, Wang H, Zhang H, Liu Q, Wang J, Hu L, Li H, Sun X, et al. Innovative Fudan rT staging in endoscopic surgery for recurrent nasopharyngeal carcinoma. Head Neck. 2023;45(2):355–64.
Sun XS, Liang YJ, Jia GD, Liu SL, Liu LT, Guo SS, Sun R, Luo DH, Chen QY, Tang LQ, et al. Establishment of a prognostic nomogram to identify optimal candidates for local treatment among patients with local recurrent nasopharyngeal carcinoma. Oral Oncol. 2020;106:104711.
Dongxiang W, Liting L, Yujing L, Meijuan L, Shanshan G, Longbin X, Yanzhou C, Meiling C, Kang N, Haiqiang M et al. Prediction of outcomes in patients with local recurrent nasopharyngeal carcinoma: development and validation of a four-factor prognostic model integrating baseline characteristics and [(18)F]FDG PET/CT parameters. Eur Radiol. 2022.
Yan W, Sun C, Ou X, Hu C. Prognostic value of pre-treatment FDG PET/CT SUVmax for metastatic lesions in de novo metastatic nasopharyngeal carcinoma following chemotherapy and locoregional radiotherapy. Cancer Imaging. 2023;23(1):21.
Lin HC, Chan SC, Cheng NM, Liao CT, Hsu CL, Wang HM, Lin CY, Chang JT, Ng SH, Yang LY, et al. Pretreatment (18)F-FDG PET/CT texture parameters provide complementary information to Epstein-Barr virus DNA titers in patients with metastatic nasopharyngeal carcinoma. Oral Oncol. 2020;104:104628.
Alessi A, Lorenzoni A, Cavallo A, Padovano B, Iacovelli NA, Bossi P, Alfieri S, Serafini G, Colombo CB, Cicchetti A, et al. Role of pretreatment 18F-FDG PET/CT parameters in predicting outcome of non-endemic EBV DNA-related nasopharyngeal cancer (NPC) patients treated with IMRT and chemotherapy. Radiol Med. 2019;124(5):414–21.
Kulanthaivelu R, Kohan A, Hinzpeter R, Liu ZA, Hope A, Huang SH, Waldron J, O’Sullivan B, Ortega C, Metser U, et al. Prognostic value of PET/CT and MR-based baseline radiomics among patients with non-metastatic nasopharyngeal carcinoma. Front Oncol. 2022;12:952763.
Acknowledgements
Not applicable.
Funding
Cancer Innovative Research Program of Sun Yat-sen University Cancer Center (CIRP-SYSUCC-0005).
Author information
Authors and Affiliations
Contributions
All authors have reviewed and approved the final manuscript. ZD, GYW, and LLT carried out the conception and design of the study. JM, LLT and CX were responsible for providing study materials or patients. ZD, DYD, and GJT conducted data collection, analysis, and interpretation. The manuscript was written by JM, ZD, GYW and CX. All authors are accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study protocol approval by the institutional ethics committee. Informed consent was waived as the study only involved the retrospective inclusion of deidentified data.
Consent for publication
Not applicable.
Abbreviations
FDG Fluorodeoxyglucose.
PET/CT Positron emission tomography/computed tomography.
lrNPC Locoregional recurrent nasopharyngeal.
r Recurrent/recurrence.
OS Overall survival.
HR Hazard ratio.
MRI Magnetic resonance imaging.
IMRT Intensity-modulated radiotherapy.
IC Induction chemotherapy.
VS Versus.
CT Computed tomography.
LDH Lactate dehydrogenase.
CRP C-reactive protein.
ALB Albumin.
EBV Epstein-Barr virus.
FSE Fast spin-echo.
TR Repetition time.
TE Echo time.
2D Two dimensions.
3D Three dimensions.
AUC Area under the curve.
ROC Receiver operating characteristic.
IQR Interquartile range.
SUVmax Maximum standardized uptake value.
UICC/AJCC Union for International Cancer Control/American Joint Committee. on Cancer.
MTV Metabolic tumor volume.
TLG Total lesion glycolysis.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: Tables 1 to 3 were erroneously omitted. These have now been included in the published article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary table S1 Univariate analysis for overall survival in the III-IVA* and rIII-IVA* NPC.
Supplementary Material 2
Supplementary table S2Univariate and multivariate Cox regression analysis for overall survival in the III-IVA* NPC.
Supplementary Material 3
Supplementary table S3Characteristics of the III-IVA* and rIII-rIVA* stage NPC in the MRI alone and with PET/CT groups.
Supplementary Material 4
Supplementary table S4Recurrent NPC staged by PET/CT and MRI.
Supplementary Material 5
Supplementary table S5Univariate analysis for overall survival in the recurrent NPC without distant metastasis.
Supplementary Material 1
Supplementary fig. S1 Maximally selected rank statistics for identifying the optimal cut-off value of the rALB = 39.4(A), rCRP = 10.5(B), SUVmax = 11.9(C), and rNLR = 3.7(D). Abbreviations: r: Recurrent; ALB: Albumin; CRP: C-reactive protein; SUVmax: maximum standardized uptake value; NLR: neutrophil-to-lymphocyte ratio.
Supplementary Material 2
Supplementary fig. S2 The proportions of salvage surgery, palliative treatment, and re-radiotherapy in the rIII-IVA NPC patients for the MRI and with PET/CT groups. Abbreviations: NS: no significance; MRI: magnetic resonance imaging; PET/CT: positron emission tomography/computed tomography.
Supplementary Material 3
Supplementary fig. S3 The percentages on the vertical axis refer to the proportions of salvage surgery, palliative treatment, and re-radiotherapy in the with PET/CT group subtracted from the values in the MRI alone group. For III-IVA and rIII-IVA, there were higher percentages of salvage surgery and lesser palliative treatment. Abbreviations: r: Recurrent; MRI: magnetic resonance imaging; PET/CT: positron emission tomography/computed tomography.
Note: All the recurrent stages were based on the eighth edition of the Union for International Cancer Control/American Joint Committee on Cancer (UICC/AJCC) staging system according to MRI.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dong, Z., Wang, GY., Dai, DY. et al. Prognostic value of pre-treatment [18F] FDG PET/CT in recurrent nasopharyngeal carcinoma without distant metastasis. BMC Cancer 24, 466 (2024). https://doi.org/10.1186/s12885-024-12189-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12189-7