Abstract
Background
The efficacy of olanzapine as an antiemetic agent in cancer chemotherapy has been demonstrated. However, few high-quality reports are available on the evaluation of olanzapine’s efficacy and safety at a low dose of 5 mg among patients treated with carboplatin regimens. Therefore, in this study, we investigated the efficacy and safety of 5 mg olanzapine for managing nausea and vomiting in cancer patients receiving carboplatin regimens and identified patient-related risk factors for carboplatin regimen-induced nausea and vomiting treated with 5 mg olanzapine.
Methods
Data were pooled for 140 patients from three multicenter, prospective, single-arm, open-label phase II studies evaluating the efficacy and safety of olanzapine for managing nausea and vomiting induced by carboplatin-based chemotherapy. Multivariable logistic regression analyses were performed to determine the patient-related risk factors.
Results
Regarding the endpoints of carboplatin regimen-induced nausea and vomiting control, the complete response, complete control, and total control rates during the overall study period were 87.9, 86.4, and 72.9%, respectively. No treatment-related adverse events of grade 3 or higher were observed. The multivariable logistic regression models revealed that only younger age was significantly associated with an increased risk of non-total control. Surprisingly, there was no significant difference in CINV control between the patients treated with or without neurokinin-1 receptor antagonist.
Conclusions
The findings suggest that antiemetic regimens containing low-dose (5 mg) olanzapine could be effective and safe for patients receiving carboplatin-based chemotherapy.
Similar content being viewed by others
Background
Chemotherapy-induced nausea and vomiting (CINV) is the most distressing side effect of cancer chemotherapy [1, 2]. Furthermore, it can have a strong negative impact on patients’ quality of life (QOL) [3]. Carboplatin (CBDCA), a second-generation platinum compound, is a key drug for the treatment of a variety of cancers and used commonly. CBDCA with a target area under the curve [AUC] ≥ 4 mg/mL/min is classified as a moderate-emetic-risk chemotherapy (MEC) or high-emetic-risk chemotherapy (HEC) [4,5,6,7]. The latest international antiemetic guidelines recommend a three-drug combination comprising 5-hydroxytryptamine-3 receptor antagonist (5-HT3RA), dexamethasone (DEX), and neurokinin-1 receptor antagonist (NK1RA) as standard antiemetic prophylaxis for CINV in patients receiving CBDCA-based chemotherapy [4,5,6,7]. However, control of CBDCA-induced nausea and vomiting remains poor even with a standard triplet therapy and is associated with some patient-related risk factors such as female sex, younger age, and alcohol use (frequency or unit of alcohol per week) [8,9,10,11]. In patients with lung cancer, the complete response (CR) rate, defined as the absence of emetic episodes and no administration of rescue medication for CINV, has been reported to be 80–90% [12,13,14,15]. In contrast, in female patients or patients with gynecologic cancer receiving CBDCA, the CR rate was approximately 62% [16, 17]. Given this context, further efforts are warranted to control CBDCA-induced nausea and vomiting in female and younger patients to improve their QOL.
Olanzapine is an antipsychotic drug classified as a multi-acting, receptor-targeted agent that has various affinities for multiple receptors, including dopaminergic D1, D2, D3, and D4 receptors, serotonergic 5-TH2A, 5-HT2B, 5-HT3, and 5-HT6 receptors, histamine H1 receptors, and muscarinic acetylcholine M1, M2, M3, and M4 receptors [18]. It has been reported to be a highly effective antiemetic drug in patients receiving MEC and/or HEC [19,20,21,22,23,24]. However, thus far, most of the reports have been about the efficacy of olanzapine 10 mg in HEC. Navari et al. demonstrated that a four-drug combination including 10 mg olanzapine was superior to standard antiemetic triplet therapy for patients, but patients who received olanzapine had significantly more severe sedation than those receiving placebo [23]. To solve this problem, a comparative study of 5 and 10 mg of olanzapine was conducted, and 5 mg olanzapine was found to have a comparable effect with a lesser sedative effect [25]. The research group continued to conduct the J-FORCE study, which examined a four-drug combination including 5 mg olanzapine for patients receiving high-dose cisplatin [24]. This study demonstrated that 5 mg olanzapine was superior to the placebo and did not have a significant effect on daytime somnolence.
However, no large-scale trials have evaluated the efficacy of olanzapine in MEC, especially at a dose of 5 mg. The efficacy and safety of 5 mg olanzapine for antiemetic prophylaxis in patients receiving CBDCA-based chemotherapy has been reported in only three phase II studies [26,27,28]. Tanaka et al. and Iihara et al., respectively, reported the efficacy of a four-drug combination consisting of olanzapine, NK1RA, 5-HT3RA, and DEX in 33 patients with lung cancer and 57 patients with gynecological cancer [26, 27]. Sakai et al. reported the efficacy of a three-drug combination consisting of olanzapine, 5-HT3RA, and DEX in 50 patients with thoracic malignancies [28]. The overall CR rates in these trials were 78.9% [27], 93.9% [26], and 94.0% [28]. It is questionable whether the CR rate is comparable in patients having thoracic malignancies treated with or without NK1RA treatment and if it differs greatly between patients with lung cancer and those with gynecological cancer. Thus, this study was aimed at evaluating the efficacy and safety of 5 mg olanzapine for the management of nausea and vomiting in cancer patients receiving CBDCA-based chemotherapy based on data from three prospective multicenter phase II trials. Another objective of the study was to identify patient-related risk factors for CBDCA-induced nausea and vomiting treated with 5 mg olanzapine.
Methods
Study design
Pooled data of 140 patients from three multicenter, prospective, single-arm, open-label, phase II studies were analyzed. The results of these studies have been previously published [26,27,28]. A flow diagram of the present study is shown in Fig. 1. The studies in question were conducted in patients who were scheduled to receive CBDCA-based chemotherapy (AUC: ≥ 4 mg/mL/min). The antiemetic regimens used in the three studies are shown in Table 1. The studies were registered with the University Hospital Medical Information Network, number UMIN000026739 (Study 1), UMIN000031646 (Study 2), and UMIN000031267 (Study 3).
The study flow diagram. In all, 140 patients who received carboplatin-based chemotherapy were analyzed from three multicenter, prospective, single-arm, open-label, phase II studies. 5-HT3RA, 5-hydroxytryptamine-3 receptor antagonist; DEX, dexamethasone; NK1RA, neurokinin-1 receptor antagonist; OLZ, olanzapine
Data collection
The patients enrolled in these three studies were aged ≥20 years; had lung cancer (Study 1), gynecologic cancer (Study 2), and thoracic malignancies (Study 3); and were chemotherapy-naïve (Study 1); and had no history of treatment with MEC and/or HEC (Studies 2 and 3). Data were collected from patients’ self-reported diaries. Patients completed a daily diary on days 1–5 (Studies 1 and 3) and days 1–7 (Study 2) from the initiation of CBDCA treatment. Patients reported experiencing nausea, somnolence, and decreased concentration by using a four-point scale (none, mild, moderate, and severe). Adverse events were graded according to the Common Terminology Criteria for Adverse Events (CTCAE) version 4.0. The data sources included patient-related risk factors such as sex, age, habitual alcohol consumption (defined as exceeding occasional drinking including occasionally consuming alcohol with meals or during social occasions, travel, parties etc.), motion sickness, morning sickness, and Eastern Cooperative Oncology Group performance status (ECOG PS). The endpoints were CR rate, which was defined as no emetic episodes and no administration of rescue medication for CINV; and complete control (CC) rate, which was defined as no emetic episodes, no use of rescue medication, and no significant nausea (defined as no more than mild nausea); and total control (TC) rate, which was defined as no emetic episodes, no use of rescue medication, and no nausea. The assessment periods for CINV were 0–120 h after CBDCA initiation (overall), 0–24 h after CBDCA initiation (acute), and 24–120 h after CBDCA initiation (delayed).
Statistical analysis
Patient characteristics, rate of CINV control, and treatment-related adverse events were summarized using descriptive statistics or reported in terms of frequencies and proportions of total patients. Univariable and multivariable logistic regression analyses were performed to determine the patient-related risk factors associated with non-CR, non-CC, and non-TC during the overall study period. The cut-off age was determined using the Youden index in receiver operating characteristic (ROC) curve analysis [29]. Youden’s index was calculated as the maximum value using the following formula: sensitivity – (1 – specificity). Sensitivity analysis using three propensity score (PS) methods was also performed to reduce the effects of confounding factors. The PS of the co-administration of NK1RA (i.e., NK1RA inclusive regimen) was estimated for each patient using a logistic regression model which included age and sex [30]. In the PS-matching analysis, 1:1 matching without replacement (greedy nearest neighbor matching algorithm) with a caliper width equal to 0.2 of the standard deviation of the logit of the PS was applied to create a matched sample [31]. We also used PS-adjusted (including the PS as an additional covariate), and inverse probability of treatment weighting (IPTW) methods [32]. The results are shown as odds ratios (ORs) and 95% confidence intervals (CIs). All statistical analyses were performed using JMP 15.0.0 and SAS version 9.4 (SAS Institute, Inc., Cary, NC, USA). All p-values were two-sided, and statistical significance was set at a P value < 0.05.
Results
Study patients
Demographic data and patient characteristics are shown in Table 2. The median patient age was 68 years (range, 34–85 years). The numbers of female and male patients were 76 (54.3%) and 64 (45.7%), respectively. The number of patients who received NK1RA was 90 (64.3%).
Control of CINV
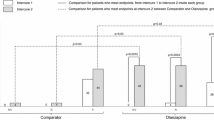
As shown in Fig. 2, the CR, CC, and TC rates during the overall period were 87.9, 86.4, and 72.9%, respectively. The corresponding rates during the acute period were 98.6, 98.6, and 96.4%. The CR, CC, and TC rates in the delayed period were 88.6, 87.1, and 73.6%, respectively. The rates of nausea, significant nausea, and vomiting during the overall period were 26.4, 4.3, and 8.6%, respectively. The corresponding rates during the acute period were 2.9, 0.7, and 0.7%. The rates of nausea, significant nausea, and vomiting during the delayed period were 25.7, 4.3, and 8.6%, respectively.
Risk factors affecting CINV control
Using the ROC curve method, the cut-off values of age were predicted to be 55, 61, and 59 years for non-CR, non-CC, and non-TC, respectively, during the overall study period. The AUC values based on the ROC curve for non-CR, non-CC, and non-TC were 0.654, 0.629, and 0.677, respectively. For the present study, the cut-off value for age was set to 60 years. The risk analysis results for non-CR, non-CC, and non-TC during the overall study period are shown in Table 3. Multivariable logistic regression models showed that younger age was significantly associated with an increased risk of non-TC in the overall study period (adjusted OR, 3.08; 95% CI, 1.17–8.12; P = 0.023). In contrast, the co-administration of NK1RA, i.e., number of antiemetics, was not significantly associated with non-CR (adjusted OR, 1.43; 95% CI, 0.33–6.14; P = 0.628), non-CC (adjusted OR, 1.89; 95% CI, 0.46–7.78; P = 0.378), and non-TC (adjusted OR, 1.47; 95% CI, 0.49–4.46; P = 0.492) during the overall study period.
Sensitivity analysis of the co-administration of NK1RA
The risk analysis results for non-CR, non-CC, and non-TC during the overall study period are shown in Table 4. Except for IPTW analysis of non-TC, the other sensitivity analyses using the three PS methods showed similar results. The co-administration of NK1RA was not significantly associated with non-CR, non-CC, and non-TC during the overall study period.
Safety
The treatment-related adverse events associated with olanzapine administration are shown in Table 5. Evaluation based on CTCAE version 4.0 revealed that the rates of grade 2 somnolence were as low as 2.9%, and there were no instances of somnolence of grade 3 or higher. The assessment of patients’ self-reported diaries, wherein they rated their symptoms using a four-point scale (none, mild, moderate, and severe), revealed the incidence of somnolence and decreased concentration were 85.7 and 60.0%, respectively (Fig. 3). The incidence of moderate and severe somnolence was 22.1%, while that of decreased concentration was only 7.1%.
Discussion
In this integrated analysis, antiemetic therapy with 5 mg olanzapine showed a high CR rate against CBDCA-induced nausea and vomiting. Moreover, the treatment had an acceptable safety profile. Navari et al. reported a head-to-head comparison of the effect of 10 mg olanzapine versus aprepitant (fosaprepitant) when combined with palonosetron and DEX for cyclophosphamide/doxorubicin or cisplatin-based regimens in two phase III trials [19, 33]. In these two studies, there were no significant differences in CR between the olanzapine and aprepitant (fosaprepitant) regimens in any evaluation period. In contrast, treatment with 10 mg olanzapine resulted in significantly higher control of nausea in the delayed and overall periods than that of aprepitant (fosaprepitant). In this integrated analysis, nausea was observed in only 26.4% of the patients, with a particularly significant nausea (moderate-to-severe nausea) rate of only 4.3%, indicating excellent nausea control. The findings of this study are in line with those of previous studies on 10 mg olanzapine.
In the present study, we analyzed the risk factors affecting CINV control using non-CR, non-CC, and non-TC during the overall study period. In the multivariable analyses, the only patient-related risk factors detected even with the addition of olanzapine were younger age for patients with non-TC. Younger age is a well-known risk factor for CINV [8,9,10,11]. This suggests that the combination of olanzapine may be able to counteract patient-related risk factors in cases of severe CINV. In the present study, the cut-off value for age was set to 60 years for non-TC in the overall period based on the ROC curve method. This is consistent with our previous analysis of the age cut-off for nausea in 608 patients who received the first cycle of chemotherapy [34]. Therefore, further development of antiemetic therapy is needed to completely control nausea, especially in younger patients.
To the best of our knowledge, there are no studies that have evaluated the efficacy of adding NK1RA to antiemetic therapy consisting of olanzapine, 5HT3RA, and DEX in MEC and HEC. Multivariable analysis showed that there was no statistically significant difference in CINV control between the patients treated with or without NK1RA. Sensitivity analysis using PS-matched, PS-adjusted, and IPTW methods yielded consistent results, except for the IPTW result in non-TC. Therefore, except in young patients, olanzapine may be used in combination with NK1RA de-escalation, which appears to be a reasonable treatment approach as a prophylactic antiemetic for CBDCA-based chemotherapy. Thus, this should be confirmed with a randomized comparison including older and younger patients in future research.
The question remains as to why NK1RA might be omitted by combining olanzapine here. Recently, the efficacy of mirtazapine, an antidepressant that has affinity for serotonin (5-TH2A, 5-HT2C, 5-HT3, 5-HT6), histamine (H1), adrenaline (ɑ1), and muscarinic receptors, as well as olanzapine, has been reported as an antiemetic treatment for cancer chemotherapy [35, 36]. Stimulation of 5HT2 or 5HT1A by mirtazapine and the interactions between mirtazapine and neurokinin-1 have also been shown. Furthermore, the drug may exert its anti-nausea and antiemetic effects indirectly by inhibiting the NK-1 receptor [37]. However, the effect of olanzapine on the NK1 receptor is not clear and warrants further investigation.
Excessive sedation is an adverse event that should be noted when administering 10 mg olanzapine. No grade 3 or higher somnolence was observed in this integrated analysis. Patient diary reports of somnolence ranged from 51.4 to 72.9% over 5 days. The percentage of patients with moderate-to-severe somnolence ranged from 5.7 to 14.3%. In the J-FORCE study, which examined a four-drug combination including 5 mg olanzapine for patients receiving high-dose cisplatin, the overall incidence of somnolence in the olanzapine group ranged from 70.5 to 76.6%, with the incidence in the moderate-to-severe group being 11.0 to 14.2% [24]. The incidence of somnolence in the placebo group in the J-FORCE study ranged from 67.8 to 76.7% overall and from 7.4 to 19.5% in the moderate-to-severe group. Our results are comparable to those of the J-FORCE study and suggest that olanzapine therapy administered 4 days after dinner does not have a significant effect on daytime somnolence. With regard to decreased concentration due to somnolence, the overall rate was 26.4 to 44.3%, while that for moderate-to-severe somnolence was 0.7 to 3.6%. In the J-FORCE study, the incidence of decreased concentration was comparable between the olanzapine group (overall: 40.4 to 51.0%, moderate to severe: 4.8 to 7.9%) and placebo group (overall: 35.6 to 55.7%, moderate to severe: 4.0 to 14.1%). This suggests that olanzapine administration had no effect on the difficulty experienced in daily life.
The present study has some limitations. First, all the studies included in this integrated analysis had an open-label and single-arm design. Second, three phase II studies used quite broad definition of the habitual alcohol consumption [26,27,28]. In CINV studies, alcohol use has traditionally been as weekly frequency of consumption [drinks/week]; no, rarely, occasionally, regularly, sometimes, every day or units/weeks [8,9,10,11]. The present study used the same definition as J-FORCE study, a large phase III trial of 5 mg olanzapine [24]. Furthermore, the results were obtained only in the Japanese population, and thus, they may not be extrapolatable to patients globally.
However, the present study showed that 5 mg olanzapine combined with 5-HT3RA and DEX with/without NK1RA could be an effective and safe standard treatment for patients treated with CBDCA-based chemotherapy with an AUC ≥ 4 mg/mL/min. In the future, a phase III trial comprising a head-to-head comparison of the efficacy and safety of 5 mg olanzapine versus NK1RA when combined with 5-HT3RA and DEX for patients receiving CBDCA-based chemotherapy is warranted.
Conclusion
In conclusion, a low dose of 5 mg olanzapine combined with 5-HT3RA and DEX with/without NK1RA could be an effective and safe standard treatment for patients treated with an AUC of ≥4 mg/mL/min of CBDCA-based combination chemotherapy.
Availability of data and materials
The data that support the findings of this study are available from the study groups of study 1, study 2, and study 3 but restrictions apply to the availability of these data, which were used under license for the current study, and therefore, the data are not publicly available. However, data are available from the authors upon reasonable request and with permission of the study groups.
Abbreviations
- 5-HT3RA:
-
5-Hydroxytryptamine-3 receptor antagonist
- AUC:
-
Area under the curve
- CBDCA:
-
Carboplatin
- CC:
-
Complete control
- CI:
-
Confidence interval
- CINV:
-
Chemotherapy-induced nausea and vomiting
- CR:
-
Complete response
- CTCAE:
-
Common terminology criteria for adverse events
- DEX:
-
Dexamethasone
- ECOG PS:
-
Eastern cooperative oncology group performance status
- HEC:
-
High-emetic-risk chemotherapy
- IPTW:
-
Inverse probability of treatment weighting
- MEC:
-
Moderate-emetic-risk chemotherapy
- NK1RA:
-
Neurokinin-1 receptor antagonist
- OR:
-
Odds ratio
- PS:
-
Propensity score
- ROC:
-
Receiver operating characteristic
- S-1:
-
Tegafur plus gimeracil plus oteracil potassium
- TC:
-
Total control
References
Kuchuk I, Bouganim N, Beusterien K, Grinspan J, Vandermeer L, Gertler S, et al. Preference weights for chemotherapy side effects from the perspective of women with breast cancer. Breast Cancer Res Treat. 2013;142(1):101–7. https://doi.org/10.1007/s10549-013-2727-3.
Sun CC, Bodurka DC, Weaver CB, Rasu R, Wolf JK, Bevers MW, et al. Rankings and symptom assessments of side effects from chemotherapy: insights from experienced patients with ovarian cancer. Support Care Cancer. 2005;13(4):219–27. https://doi.org/10.1007/s00520-004-0710-6.
Fernández-Ortega P, Caloto MT, Chirveches E, Marquilles R, Francisco JS, Quesada A, et al. Chemotherapy-induced nausea and vomiting in clinical practice: impact on patients' quality of life. Support Care Cancer. 2012;20(12):3141–8. https://doi.org/10.1007/s00520-012-1448-1.
Roila F, Molassiotis A, Herrstedt J, Aapro M, Gralla RJ, Bruera E, et al. 2016 MASCC and ESMO guideline update for the prevention of chemotherapy- and radiotherapy-induced nausea and vomiting and nausea and vomiting in advanced cancer patients. Ann Oncol. 2016;27(suppl 5):v119–33. https://doi.org/10.1093/annonc/mdw270.
Hesketh PJ, Kris MG, Basch E, Bohlke K, Barbour SY, Clark-Snow RA, et al. Antiemetics: ASCO Guideline Update. J Clin Oncol. 2020;38(24):2782–97. https://doi.org/10.1200/JCO.20.01296.
NCCN Clinical Practice Guidelines in Oncology: Antiemesis. Version 1. 2021. https://www.nccn.org/professionals/physician_gls/pdf/antiemesis.pdf. Accessed 11 Apr 2021.
Aogi K, Takeuchi H, Saeki T, Aiba K, Tamura K, Iino K, et al. Optimizing antiemetic treatment for chemotherapy-induced nausea and vomiting in japan: update summary of the 2015 Japan society of clinical oncology clinical practice guidelines for antiemesis. Int J Clin Oncol. 2021;26(1):1–17.
Hesketh PJ, Aapro M, Street JC, Carides AD. Evaluation of risk factors predictive of nausea and vomiting with current standard-of-care antiemetic treatment: analysis of two phase III trials of aprepitant in patients receiving cisplatin-based chemotherapy. Support Care Cancer. 2010;18(9):1171–7. https://doi.org/10.1007/s00520-009-0737-9.
Warr DG, Street JC, Carides AD. Evaluation of risk factors predictive of nausea and vomiting with current standard-of-care antiemetic treatment: analysis of phase 3 trial of aprepitant in patients receiving adriamycin-cyclophosphamide-based chemotherapy. Support Care Cancer. 2011;19(6):807–13. https://doi.org/10.1007/s00520-010-0899-5.
Hilarius DL, Kloeg PH, van der Wall E, van den Heuvel JJ, Gundy CM, Aaronson NK. Chemotherapy-induced nausea and vomiting in daily clinical practice: a community hospital-based study. Support Care Cancer. 2012;20(1):107–17. https://doi.org/10.1007/s00520-010-1073-9.
Sekine I, Segawa Y, Kubota K, Saeki T. Risk factors of chemotherapy-induced nausea and vomiting: index for personalized antiemetic prophylaxis. Cancer Sci. 2013;104(6):711–7. https://doi.org/10.1111/cas.12146.
Ito Y, Karayama M, Inui N, Kuroishi S, Nakano H, Nakamura Y, et al. Aprepitant in patients with advanced non-small-cell lung cancer receiving carboplatin-based chemotherapy. Lung Cancer. 2014;84(3):259–64. https://doi.org/10.1016/j.lungcan.2014.03.017.
Kusagaya H, Inui N, Karayama M, Fujisawa T, Enomoto N, Kuroishi S, et al. Evaluation of palonosetron and dexamethasone with or without aprepitant to prevent carboplatin-induced nausea and vomiting in patients with advanced non-small-cell lung cancer. Lung Cancer. 2015;90(3):410–6. https://doi.org/10.1016/j.lungcan.2015.11.009.
Kitazaki T, Fukuda Y, Fukahori S, Oyanagi K, Soda H, Nakamura Y, et al. Usefulness of antiemetic therapy with aprepitant, palonosetron, and dexamethasone for lung cancer patients on cisplatin-based or carboplatin-based chemotherapy. Support Care Cancer. 2015;23(1):185–90. https://doi.org/10.1007/s00520-014-2339-4.
Miya T, Kobayashi K, Hino M, Ando M, Takeuchi S, Seike M, et al. Efficacy of triple antiemetic therapy (palonosetron, dexamethasone, aprepitant) for chemotherapy-induced nausea and vomiting in patients receiving carboplatin-based, moderately emetogenic chemotherapy. SpringerPlus. 2016;5(1):2080. https://doi.org/10.1186/s40064-016-3769-x.
Tanioka M, Kitao A, Matsumoto K, Shibata N, Yamaguchi S, Fujiwara K, et al. A randomised, placebo-controlled, double-blind study of aprepitant in nondrinking women younger than 70 years receiving moderately emetogenic chemotherapy. Br J Cancer. 2013;109(4):859–65. https://doi.org/10.1038/bjc.2013.400.
Yahata H, Kobayashi H, Sonoda K, Shimokawa M, Ohgami T, Saito T, et al. Efficacy of aprepitant for the prevention of chemotherapy-induced nausea and vomiting with a moderately emetogenic chemotherapy regimen: a multicenter, placebo-controlled, double-blind, randomized study in patients with gynecologic cancer receiving paclitaxel and carboplatin. Int J Clin Oncol. 2016;21(3):491–7. https://doi.org/10.1007/s10147-015-0928-y.
Brafford MV, Glode A. Olanzapine: an antiemetic option for chemotherapy-induced nausea and vomiting. J Adv Pract Oncol. 2014;5(1):24–9. https://doi.org/10.6004/jadpro.2014.5.1.8.
Navari RM, Gray SE, Kerr AC. Olanzapine versus aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a randomized phase III trial. J Support Oncol. 2011;9(5):188–95. https://doi.org/10.1016/j.suponc.2011.05.002.
Tan L, Liu J, Liu X, Chen J, Yan Z, Yang H, et al. Clinical research of olanzapine for prevention of chemotherapy-induced nausea and vomiting. J Exp Clin Cancer Res. 2009;28(1):131. https://doi.org/10.1186/1756-9966-28-131.
Babu G, Saldanha SC, Kuntegowdanahalli Chinnagiriyappa L, Jacob LA, Mallekavu SB, Dasappa L, et al. The efficacy, safety, and cost benefit of olanzapine versus aprepitant in highly emetogenic chemotherapy: a pilot study from South India. Chemother Res Pract. 2016;2016:3439707.
Wang X, Wang L, Wang H, Zhang H. Effectiveness of olanzapine combined with ondansetron in prevention of chemotherapy-induced nausea and vomiting of non-small cell lung cancer. Cell Biochem Biophys. 2015;72(2):471–3. https://doi.org/10.1007/s12013-014-0489-0.
Navari RM, Qin R, Ruddy KJ, Liu H, Powell SF, Bajaj M, et al. Olanzapine for the prevention of chemotherapy-induced nausea and vomiting. N Engl J Med. 2016;375(2):134–42. https://doi.org/10.1056/NEJMoa1515725.
Hashimoto H, Abe M, Tokuyama O, Mizutani H, Uchitomi Y, Yamaguchi T, et al. Olanzapine 5 mg plus standard antiemetic therapy for the prevention of chemotherapy-induced nausea and vomiting (J-FORCE): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2020;21(2):242–9. https://doi.org/10.1016/S1470-2045(19)30678-3.
Yanai T, Iwasa S, Hashimoto H, Ohyanagi F, Takiguchi T, Takeda K, et al. A double-blind randomized phase II dose-finding study of olanzapine 10 mg or 5 mg for the prophylaxis of emesis induced by highly emetogenic cisplatin-based chemotherapy. Int J Clin Oncol. 2018;23(2):382–8. https://doi.org/10.1007/s10147-017-1200-4.
Tanaka K, Inui N, Karayama M, Yasui H, Hozumi H, Suzuki Y, et al. Olanzapine-containing antiemetic therapy for the prevention of carboplatin-induced nausea and vomiting. Cancer Chemother Pharmacol. 2019;84(1):147–53. https://doi.org/10.1007/s00280-019-03868-5.
Iihara H, Shimokawa M, Hayasaki Y, Fujita Y, Abe M, Takenaka M, et al. Efficacy and safety of 5 mg olanzapine combined with aprepitant, granisetron and dexamethasone to prevent carboplatin-induced nausea and vomiting in patients with gynecologic cancer: a multi-institution phase II study. Gynecol Oncol. 2020;156(3):629–35. https://doi.org/10.1016/j.ygyno.2020.01.004.
Sakai C, Shimokawa M, Iihara H, Fujita Y, Ikemura S, Hirose C, et al. Low-dose olanzapine plus granisetron and dexamethasone for carboplatin-induced nausea and vomiting in patients with thoracic malignancies: A prospective multicenter phase II trial. Oncologist. 2021;26(6):e1066-e1072. https://doi.org/10.1002/onco.13772.
Pepe MS. The statistical evaluation of medical tests for classification and prediction. New York, USA: Oxford University Press; 2003.
Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55. https://doi.org/10.1093/biomet/70.1.41.
Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10(2):150–61. https://doi.org/10.1002/pst.433.
D’Agostino RB. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17(19):2265–81. https://doi.org/10.1002/(SICI)1097-0258(19981015)17:19<2265::AID-SIM918>3.0.CO;2-B.
Navari RM, Nagy CK, Le-Rademacher J, Loprinzi CL. Olanzapine versus fosaprepitant for the prevention of concurrent chemotherapy radiotherapy-induced nausea and vomiting. J Community Support Oncol. 2016;14(4):141–7. https://doi.org/10.12788/jcso.0245.
Iihara H, Fujii H, Yoshimi C, Yamada M, Suzuki A, Matsuhashi N, et al. Control of chemotherapy-induced nausea in patients receiving outpatient cancer chemotherapy. Int J Clin Oncol. 2016;21(2):409–18. https://doi.org/10.1007/s10147-015-0908-2.
Cao J, Ouyang Q, Wang S, Ragaz J, Wang X, Teng Y, et al. Mirtazapine, a dopamine receptor inhibitor, as a secondary prophylactic for delayed nausea and vomiting following highly emetogenic chemotherapy: an open label, randomized, multicenter phase III trial. Investig New Drugs. 2020;38(2):507–14. https://doi.org/10.1007/s10637-020-00903-8.
Maleki A, Ghadiyani M, Salamzadeh J, Salari S, Banihashem S, Tavakoli-Ardakani M. Comparison of mirtazapine and olanzapine on nausea and vomiting following anthracycline-cyclophosphamide chemotherapy regimen in patients with breast cancer. Iran J Pharm Res. 2020;19(3):451–64. https://doi.org/10.22037/ijpr.2020.113955.14584.
Chang FL, Ho ST, Sheen MJ. Efficacy of mirtazapine in preventing intrathecal morphine induced nausea and vomiting after orthopedic surgery. Anaesthesia. 2010;65(12):1206–11. https://doi.org/10.1111/j.1365-2044.2010.06561.x.
Acknowledgments
We are grateful to all the patients and their families for participating in this study. We would like to thank Editage (www.editage.com) for English language editing.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
S.Y., H.I., R.U., H.K. and N.I. conceived the study. S.Y., H.I., R.U., H.K. and N.I. conducted the claim data analysis. H.K. and R.U. performed the statistical analyses. Y.O. and K.M. provided technical support. S.Y., H.I., R.U., H.K., K.T., Y.F., M.A., H.I., M.K., Y.H., C.H., T.S., K.N., A.S. and N.I. contributed to the interpretation of data and assisted in the preparation of the manuscript. S.Y., H.I., R.U., and H.K. drafted the initial manuscript. S.Y., H.I., R.U., H.K. A. S., Y.O., K.M., and N.I. conducted the critical revision of the manuscript. All authors reviewed the manuscript. The authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Study 1 was approved by the Medical review board of Hamamatsu University Graduate School of Medicine (16–296). Studies 2 and 3 were approved by the Medical review board of Gifu University Graduate School of Medicine (30–002, 2018–19). These studies were conducted according to the Declaration of Helsinki and the ethical guidelines for clinical studies. Written informed consent was obtained from all patients. For this integrated study, study 1 was as an opt-out method for the secondary use of data with the approval of the Medical review board of Hamamatsu University Graduate School of Medicine (20–335), and for study 2 and 3, patient written informed consent was obtained for the secondary use of data.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yamamoto, S., Iihara, H., Uozumi, R. et al. Efficacy and safety of 5 mg olanzapine for nausea and vomiting management in cancer patients receiving carboplatin: integrated study of three prospective multicenter phase II trials. BMC Cancer 21, 832 (2021). https://doi.org/10.1186/s12885-021-08572-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-021-08572-3