Abstract
Background
Impaired immune response in multiple myeloma renders the patients vulnerable to infections, such as COVID-19, and may cause worse response to vaccines. Researchers should analyze this issue to enable the planning for special preventive measures, such as increased booster doses. Therefore, this meta-analysis aimed to evaluate the response and efficacy of COVID-19 vaccines in patients with multiple myeloma.
Methods
This meta-analysis followed PRISMA 2020 guidelines, conducting a comprehensive database search using specified keywords. Study selection involved a two-phase title/abstract and full-text screening process. Data extraction was performed by two researchers, and statistical analysis involved meta-analysis, subgroup analysis based on vaccine dosage and study time, random effects meta-regression, and heterogeneity testing using the Q test.
Results
The meta-analysis revealed that patients with multiple myeloma (MM) had a lower likelihood of developing detectable antibodies after COVID-19 vaccination compared to healthy controls (Log odds ratio with 95% CI: -3.34 [-4.08, -2.60]). The analysis of antibody response after different doses showed consistent lower seropositivity in MM patients (after first dose: -2.09, [-3.49, -0.69], second: -3.80, 95%CI [-4.71, -3.01], a booster dose: -3.03, [-5.91, -0.15]). However, there was no significant difference in the mean level of anti-S antibodies between MM patients and controls (Cohen’s d -0.72, [-1.86, 0.43]). Evaluation of T-cell responses indicated diminished T-cell-mediated immunity in MM patients compared to controls. Seven studies reported clinical response, with breakthrough infections observed in vaccinated MM patients.
Conclusions
These findings highlight the impaired humoral and cellular immune responses in MM patients after COVID-19 vaccination, suggesting the need for further investigation and potential interventions.
Similar content being viewed by others
Introduction
Multiple myeloma (MM) patients are notably vulnerable to viral and bacterial infections [1]. Data from a comprehensive population-based study indicate that these patients have a 7-fold higher risk for bacterial and a 10-fold increased risk for viral infections [1]. Additionally, the study reveals that approximately 22% of deaths among all MM patients documented in the nationwide Swedish Cancer Registry at one year of follow-up were attributed to infections [1]. Various immune effector mechanisms are compromised due to their disease in MM patients even before the initiation of antimyeloma therapy [2]. A survey reported that about half of these patients experience one or more periods of infection in the year preceding antimyeloma therapy, with 43% experiencing infections in the first six months following therapy initiation [3]. Conversely, the risk of inpatient mortality due to COVID-19 was approximately 34% among adult patients with hematological malignancies [4]. These findings accented to the necessity of urgent action to identify preventive treatment options for these patients. Vaccination has emerged as one of the most successful preventive interventions against infections, saving millions of lives. However, both Myeloma itself and antimyeloma therapy can reduce immune competence and impair the development of long-term immunological memory. This issue poses a significant obstacle to effective vaccination in patients with MM [2]. A study involving 52 MM patients and their response to vaccination against influenza, S. pneumoniae and Haemophilus influenzae type b (Hib) revealed that only 19% of MM patients could develop effective antibody titers to all three strains of vaccine and 10% against two viral strains of the vaccine [5]. Another study in 2015 had better results showing that 9–19% of patients already had sufficient antibody titers against at least one strain of influenza virus. This number increased by 20–40% after a single dose vaccination and doubled after the second boost [6]. Novel vaccines even show better performances in hematologic malignancies. 80.2% of these patients could express sufficient humoral response in a trial with two doses of the new adjuvanted recombinant varicella zoster virus glycoprotein E vaccine [7]. Vaccination against Hepatitis B is also recommended in MM patients who live in or travel to areas endemic for hepatitis B or patients with sexual partners with chronic hepatitis B infection [8]. Vaccination against several bacterial agents like Pneumococci, Hemophilus influenzae, and Meningococci has also been studied and recommended in MM patients [9,10,11,12].
Vaccination against SARS-CoV-2 constitutes a major preventive option, especially for vulnerable patients [13]. However, patients with MM were left out from most SARSCoV-2 mRNA vaccine trials, resulting in limited information regarding the safety and efficacy of vaccines in this population [2]. Available data demonstrate that the antibody response provoked by COVID-19 in patients with hematological malignancies against SARS-CoV-2 is ineffective [14]. As COVID-19 persists in increasing the morbidity and mortality rate in these patients, synthesizing evidence to inform decision-making and provide recommendations becomes imperative. Consequently, we aimed to run a meta-analysis to evaluate the antibody response, and efficacy following vaccination against SARS-CoV-2 in patients with MM.
Methods
Overview and database search
This meta-analysis followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2020 guidelines. First, we searched the databases of PubMed, Embase, Web of Science, and Cochrane on August 19th, 2022. Keywords for “Multiple Myeloma”, “COVID-19”, and “Vaccination” were chosen from the related previous studies and medical subject headings (MeSH) website to build the search strategy. All the keywords were searched as title/abstract/keywords in the databases. Supplementary Table 1 contains the search terms for each database.
Study selection
All the records were downloaded into EndNote software and the duplicates were removed both by the application and manually. Then the records were uploaded to the Covidence database and duplicates were once again removed by the website. The records then underwent a two-phase screening process. First, they were screened based on their title and abstract. The approved records were then screened by their full texts and the eligible studies were included in this meta-analysis. Whenever any disagreements arose between the two researchers involved in the screening process (A.K. & H.H.), they discussed the matter to solve the problem. If disagreements remained, they sought another independent opinion for final decision.
A researcher (A.K.) went through the citations of the included articles to find any possible suitable records manually. These manual records then entered the full text screening and they were combined with eligible studies through database searching to determine the overall included studies.
Inclusion/exclusion criteria
We included all the original English studies that compared response to COVID-19 vaccines in patients with MM compared to healthy controls. If the study did not specifically report the patients with MM, but rather reported the data for patients with plasma cell disorders as a whole without individual data for MM subgroup, we included them to avoid data loss only if the percentage of patients with MM were 85% or more of the overall patients. To eliminate the bias related to the inclusion of research involving patients with other plasma cell disorders (PCD) besides MM, we conducted a meta-regression analysis to assess the impact of incorporating these studies. Therefore, the exclusion criteria were the following:
-
1.
No MM groups.
-
2.
Not original, i.e., reviews or commentaries.
-
3.
Case reports and case series.
-
4.
No healthy control groups.
-
5.
No vaccines, or vaccines other than COVID-19.
-
6.
Non-human studies.
-
7.
Same settings published elsewhere; this is particularly true when similar authors report the updates of similar patients in a future study, in such case, we included the later study.
-
8.
Abstracts or studies without full texts.
-
9.
Non-English studies.
Data extraction
We designed an excel sheet before data extraction. Two researchers extracted the data of the included studies into the excel sheet (P.F.T. & M.H.), and two other independent researchers (H.H. & A.K.) rechecked the extracted data for validity. After checking the validity of the extracted data, it was used for the synthesis of the systematic review and meta-analysis.
The data extraction excel sheet contained the following information:
Study title, first author, country, year, study design, controls and matching status, types of assessed vaccines, doses received, characteristics of cases and controls, including their numbers, mean age (SD), disease status, and treatments received, anti-spike antibody responses in cases and controls, including the criteria used for response, mean (SD) antibody titers, number of positive humoral responses to vaccine, and any other subgroups that antibody responses are reported for, cellular immunity response in cases and controls, including response criteria, mean (SD) T-cell response based on the criteria, number of patients with positive response, other cellular immunity components than T-cells measured, and any other subgroups that cellular immunity responses are reported for, and finally, clinical response to the vaccines in cases and controls, including, number of COVID-19 infections, severe COVID-19 cases, deaths, hospitalization, ICU admission, and any other clinical criteria for any other subgroups mentioned in the studies.
Statistical analysis
The statistical analysis in this study involved conducting a meta-analysis using Stata version 17. The analysis was performed on two different groups of studies. The first group included studies that measured the AB concentration separately in cases and controls, while the second group included studies that reported the number of AB-positive and AB-negative patients.
Subgroup analysis was then conducted based on the dosage of the vaccine and the study time after vaccine injection. This allowed for the examination of potential differences in outcomes based on these factors.
To further explore the factors influencing the outcomes, random effects meta-regression was performed. The meta-regression analysis included three factors: vaccine type, time after injection, and whether the study focused on MM or PCD. These factors were considered as potential sources of heterogeneity in the meta-analysis.
To assess the heterogeneity and test for group differences among the included studies, the Q test was used. The Q test helps to evaluate whether the observed variations among the effect sizes across the studies are due to chance or represent genuine differences.
Quality assessment
We used the Newcastle-Ottawa scale (NOS) to assess the quality of the included studies [15]. The total score is out of nine, and we considered a study of poor quality if they could not receive at least four.
Results
Study selection
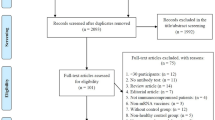
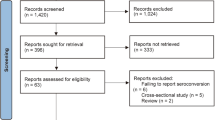
Our systematic search strategy yielded 288 relevant studies, of which 137 were duplicates. Then, a total of 70 studies were excluded after screening through title and abstract. We reviewed the full text of 81 studies, and 47 were excluded for the reasons demonstrated in Fig. 1. Finally, 35 studies were eligible for inclusion, and 12 studies were included in the meta-analysis. The flow diagram is shown in Fig. 1.
Quality assessment
The results of the quality assessment of the included studies are shown in Supplementary Table 2. The quality assessment was based on selection, comparability of cases and controls based on the design or analysis, and exposure. All included studies had sufficient quality with quality score ranging from 4 to 9.
Study characteristics
The included studies were conducted in either 2021 or 2022. Most of the studies were conducted in Europe (24), followed by the United States (13), while the least number of studies (4) were conducted in Asia. Thirty-four of the included studies were cohort studies; the remainders were three case-control studies and one cross-sectional study. Seventeen studies included healthy participants as controls. A total of 13,274 patients with a confirmed diagnosis of MM and 509,844 healthy controls were included in the selected studies. The median age of MM patients ranged from 62.9 to 83.0 years. All of the participants received either one or two doses of the following vaccines Pfizer (BNT162b2), AstraZeneca (ChAdOx1 nCoV-19), Moderna (mRNA-1273), or Janssen/Johnson & Johnson (Ad.26.COV2). Additionally, three and one studies evaluated vaccine response after the third and the fourth dose of the Pfizer or Moderna vaccine, respectively. Most selected studies evaluated B-cell response after vaccination, while only six considered T-cell response after vaccination. Also, six studies measured antibodies against COVID-19 prior to vaccination. More detailed characteristics of the included studies in this systematic review are outlined in Table 1.
B-cell response
Percentage of AB positive and negative patients
Our selected studies evaluated humoral response after COVID-19 vaccination by measuring SARS-CoV-2 spike IgG antibody (anti-S) or neutralizing antibody (nAb). Thirty-three studies reported antibody response, of which the detected antibody level was reported in sixteen studies. Our meta-analysis on eleven studies revealed that, compared with healthy controls, patients suffering from MM were less likely to form detectable antibodies after COVID-19 vaccination (Log odds ratio with 95% CI: -3.34 [-4.08, -2.60]), and substantial heterogeneity was identified (I²=64.47%). It should be noted that antibody response was evaluated at different time spans in six of the analyzed studies. Detailed results with the number of antibody responses in MM patients and controls are presented in the forest plot (Fig. 2). A distinct publication bias was detected, revealing an asymmetry in the funnel plot (Supplementary Fig. 1). As shown in Fig. 3 MM patients were less seropositive compared to healthy controls after first (log odds ratio − 2.09, 95%CI [-3.49, -0.69], I2 = 50.65%), second (log odds ratio − 3.80, 95%CI [-4.71, -3.01], I2 = 59.89%), and a booster dose (log odds ratio − 3.03, 95%CI [-5.91, -0.15]). No significant difference was detected between the groups (p = 0.10). We then stratified the antibody response in these studies based on the timing of assessment after vaccination (< 30 days and ≥ 30 days). Likewise, seropositivity was lower in MM patients compared with healthy controls regardless of the time passed from the vaccination (Fig. 4). The analysis results of all subgroups are represented in Fig. 5.
Antibody titration
Next, we focused our analysis on seven studies reporting the anti-S titration (Fig. 6). Interestingly, analysis showed no significant difference in mean level of anti-S between MM patients and healthy controls (Cohen’s d -0.72, 95% CI [-1.86, 0.43]), and a high level of heterogeneity (I2 = 98.99%). The high degree of heterogeneity in response to COVID-19 vaccination could be due to differences in the population, laboratory kits, measurement methods, and timing of titration after vaccination. In addition, an evidence of publication bias was noted in this analysis (Supplementary Fig. 2).
T-cell responses
Only six studies evaluated T-cell-mediated immunity after COVID-19 vaccination (Table 2). Henriquez et al. measured IFN-γ production by T-cells after ex vivo stimulation with S1 or S2, three months after the first dose of BNT162b2 in MM patients and healthy controls. The IFN-γ was significantly lower in patients with MM compared with the controls [40]. In the study of Storti et al., vaccine-induced T cell response (spike-specific CD4 + or CD8 + T cell producing at least one of the three cytokines of IL-2 or IFN-γ or TNF-α) in MM patients and pre-malignant-monoclonal-gammopathies was evaluated by flow cytometry. Their results indicated that MM patients had a reduced T-cell response to complete vaccination and showed less cytotoxic IFN-γ + and TNF-α + CD8 + T cells than monoclonal gammopathy of undetermined significance (MGUS). Additionally, booster immunization improved cellular response to COVID-19 vaccination in both newly diagnosed MM (MMD) patients and relapsed/refractory MM (MMR) patients [41]. Wagner et al. analyzed the cellular response in 102 subjects, including healthy controls, IBD patients, MM patients, and patients with solid tumors. After the second dose, controls had a clear T-cell response upon stimulation with the S1 subunit. T cells of solid tumor patients secreted IL-2, IFN-γ, IL-17a and GM-CSF, and IL-10, while only IFN-γ, IL-17a, and IL-10 were induced in MM patients’ T-cells. IFN-γ and IL-2 were positively correlated to humoral response in controls and IBD patients, whereas only IL-2 was associated with antibody level in MM patients and patients with solid tumors [42]. In the study of Enssle et al. MM patients showed a diminished T-cell response after stimulation with the receptor-binding domain (RBD), the S2-protein, and CEF/CEFT control peptides following two doses of SARS-CoV-2 vaccination compared with controls. Lower frequencies of IFN-γ or interleukin-2 secreting CD4 + T cells were observed, whereas CD8 + T-cells did not differ between MM patients and the controls after stimulation [43]. Although CD4 + T cells were significantly lower in serological non-responders after the second vaccination, no positive correlation was observed between T-cell and serologic responses in patients with MM. Interestingly, T-cell response among serological responders and non-responders did not differ significantly [43]. Later, Enssle et al., evaluated variant specific T-cell response after the third dose of COVID-19 vaccination. Their results showed that patients with MM had a strong CD4+ T cell response against the (wild type) WT strain, while immune responses against Omicron was lower than the controls [44]. Zaleska et al. demonstrated specific SARS-CoV‐2 cytotoxic T-cells to evaluate immune response after mRNA vaccines in patients with hematologic malignancies. They found CD8 + T‐cell immune responses against SARS‐CoV‐2 spike epitope (YLQPRTFLL) in all HLA‐A*02 positive MM (n = 17). Notably, they reported a negative correlation between YLQPRTFLL‐specific CD8 + T-cells and antibody response [45]. Additionally, in MM patients, an increase in EM‐specific CD8 + T cells shortly after vaccination was observed, which decreased after 12 weeks [45].
Clinical response
Seven of evaluated studies reported clinical response among vaccinated MM patients. In the study of Fillmore et al. on 1606 vaccinated MM patients and matched 1606 unvaccinated MM patients, among the vaccinated group, 14 (0.87%) were infected with COVID-19 following vaccination. In this matched cohort, vaccine effectiveness in MM patients was 22.2%, 14 days after the second dose [46]. In the study of Ghandili et al. of 82 vaccinated MM patients, one patient developed COVID-19 25 days after her first vaccination. At this time, the patient had no detectable antibody, while after infection, she was positive for nucleocapsid and spike antibodies [47]. Among a cohort of 60 MM patients with no history of SARS-CoV-2 infection, four were infected after one dose (n = 2) or two doses (n = 2) of BNT162b2, and all of them were receiving anti-CD38 immunotherapy [40]. During the prospective study of Ntanasis-Stathopoulos et al., between the third and fourth doses of BNT162b2, 34 (16.9%) were COVID-19 positive. The demographics and antibody levels of COVID-19-positive and negative patients were compared, and they had similar characteristics [48]. In a study by Schiller Salton, six months after the second vaccination, four of them186 patients developed COVID-19 at least one week following the latest vaccine dose (1 died, 1 had a severe disease but recovered, and 2 had a mild disease). Two patients didn’t have a serological response one month after the second vaccination, which was converted after their COVID‐19 resolution. One patient had a positive antibody response one month after vaccination, and his disease was mild [49]. Storti et al. monitored 40 patients with MM, SMM, or MGUS after the booster dose for about four months. The clinical follow-up didn’t show any disease progression. Three patients developed COVID-19 infections [41]. In a study conducted by Wang et al., MM patients’ risk for breakthrough infections after complete vaccination was 17.4% higher than the 4.5% in vaccinated patients without cancer. The risks for breakthrough infection did not differ based on race or ethnicity [50].
Discussion and conclusions
To comprehensively evaluate the clinical response of COVID vaccines, it is insufficient to solely assess the B-cell and antibody response, as the crucial involvement of T-cell response in the body’s defense against the disease must also be considered [51, 52]. In contrast to the valuable findings of Gagelmann et al. that reported a pooled antibody response of 76% (95% CI: 67–83; I²=92%) in MM patients, our study endeavors to provide a more comprehensive analysis by systematically assessing two additional components of vaccine response in this patient population [13]. Besides, in order to ensure inclusivity and minimize data gaps, we aimed to incorporate all available studies in which the proportion of MM patients exceeded 85%. As depicted in the Supplementary Tables 3&4 showcasing our meta-regression analysis, there was no discernible difference in the outcome variable between studies solely comprising MM patients and those including 15% or less of other PCDs. Also, the results indicate that vaccine type and antibody measurement time did not significantly influence the observed outcomes, as evidenced by the lack of meaningful differences in the meta-regression analysis.
Different methodologies were employed by various studies to evaluate the impact of MM on the B-cell response, with seven studies using the mean and standard deviation of the antibody concentration in both case and control groups, while eleven studies measured the number of antibody positive and negative patients in each group. Our analysis incorporated both sets of studies, with results indicating a significant decrease in antibody concentration in the MM group as compared to the healthy control group (p = 0.00) in studies that utilized the mean and standard deviation method, as well as in studies that counted the number of antibody positive patients (p = 0.00). The subgroup analysis of the AB positive and negative studies based on the dosage of the vaccine demonstrates that the magnitude of the impact, as measured by the log odds ratio, was strongest for the second dose (-3.804), followed by the first dose (-2.091) and then the booster dose (-3.030). However, it is important to note that the sample size for the booster dose subgroup was only one study, which may limit the reliability of this finding (Supplementary Table 5).
The findings of a recent meta-analysis parallel our study [53], highlighting a diminished immune response among patients with MM following COVID-19 vaccination. However, our study differs in several significant respects. Notably, we integrated healthy controls into our analysis, serving as a comparative reference point. Furthermore, we included more studies in our analysis. Additionally, in addition to assessing B-cell and T-cell responses, we expanded our investigation to include evaluations of clinical responses.
Because of the compromised immune system in the disease which is exacerbated by immunosuppressive therapies, individuals with hematological malignancies are more likely to develop reduced vaccine response. Over the years, increasing evidence has revealed significant dysfunction of the immune system in individuals with MM [54, 55]. Consequently, both B-cell precursors and normal plasma cells are compromised, leading to consistent immune deficiency in patients with MM [56]. Additionally, despite an increase in effector cells like natural killer (NK) cells and cytotoxic CD8 + T cells in both bone marrow and peripheral blood, they fail to control disease progression, indicating a profound immunosuppressive environment [57]. Furthermore, dendritic cells exhibit alterations in MM, including diminished expression of co-stimulatory molecules and impaired initiation of allogeneic T-cell responses [58].
To our knowledge, no comprehensive review has evaluated the T-cell and clinical response of MM patients after COVID-19 vaccination at once, despite the critical role that these structures play in vaccine response. Therefore, this systematic review aims to fill this gap in the literature and provide a comprehensive evaluation of the vaccine response in MM patients. Most of the studies showed weaker T-cell response alongside antibody response among MM patients. The results of the evaluated studies in clinical response section indicates varying rates of COVID-19 infections among vaccinated MM patients, ranging from 0.87 to 17.4%. Some patients who experienced breakthrough infections had no detectable antibodies, while others exhibited a delayed serological response. These findings underscore the importance of continuous monitoring and potential risk factors for breakthrough infections in MM patients despite vaccination, emphasizing the need for further research in this area.
Data availability
Data are available upon a request to the corresponding author.
References
Blimark C, et al. Multiple myeloma and infections: a population-based study on 9253 multiple myeloma patients. Haematologica. 2015;100(1):107–13.
Gavriatopoulou M, et al. SARS-CoV-2 vaccines in patients with multiple myeloma. Hemasphere. 2021;5(3):e547.
Ludwig H, Meckl A, Engelhardt M. Compliance with vaccination recommendations among patients with multiple myeloma: a Real World Experience. Hemasphere. 2021;5(7):e597.
Vijenthira A, et al. Outcomes of patients with hematologic malignancies and COVID-19: a systematic review and meta-analysis of 3377 patients. Blood. 2020;136(25):2881–92.
Robertson JD, et al. Immunogenicity of vaccination against influenza, Streptococcus pneumoniae and Haemophilus influenzae type B in patients with multiple myeloma. Br J Cancer. 2000;82(7):1261–5.
Hahn M, et al. Efficacy of single versus boost vaccination against influenza virus in patients with multiple myeloma. Haematologica. 2015;100(7):e285–8.
Dagnew AF, et al. Immunogenicity and safety of the adjuvanted recombinant zoster vaccine in adults with haematological malignancies: a phase 3, randomised, clinical trial and post-hoc efficacy analysis. Lancet Infect Dis. 2019;19(9):988–1000.
Terrault NA, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 2018;67(4):1560–99.
Ludwig H, et al. Recommendations for vaccination in multiple myeloma: a consensus of the European Myeloma Network. Leukemia. 2021;35(1):31–44.
Geno KA, et al. Pneumococcal capsules and their types: past, Present, and Future. Clin Microbiol Rev. 2015;28(3):871–99.
Palazzo M, et al. Revaccination after autologous hematopoietic stem cell transplantation is safe and effective in patients with multiple myeloma receiving Lenalidomide maintenance. Biol Blood Marrow Transpl. 2018;24(4):871–6.
Rieger CT, et al. Anti-infective vaccination strategies in patients with hematologic malignancies or solid tumors-Guideline of the Infectious Diseases Working Party (AGIHO) of the German Society for Hematology and Medical Oncology (DGHO). Ann Oncol. 2018;29(6):1354–65.
Gagelmann N, et al. Antibody response after vaccination against SARS-CoV-2 in adults with hematological malignancies: a systematic review and meta-analysis. Haematologica. 2022;107(8):1840–9.
Ljungman P, et al. COVID-19 and stem cell transplantation; results from an EBMT and GETH multicenter prospective survey. Leukemia. 2021;35(10):2885–94.
Newcastle-. Ottawa scale (NOS), available online at: https://www.ohri.ca/programs/clinical_epidemiology/nosgen.pdf, accessed: April 4th, 2023.
Abdallah AO, Mahmoudjafari Z, Atieh T, Ahmed N, Cui W, Shune L, et al. Neutralizing antibody responses against SARS-CoV-2 in patients with plasma cell disorders who are on active treatment after two doses of mRNA vaccination. Eur J Haematol. 2022;109(5):458–64. https://doi.org/10.1111/ejh.13826.
Abella E, Trigueros M, Pradenas E, Muñoz-Lopez F, Garcia-Pallarols F, Ben Azaiz Ben Lahsen R, et al. Efficacy of SARS-CoV-2 vaccination in patients with monoclonal gammopathies: a cross sectional study. Life Sci Alliance. 2022;5(12):e202201479. https://doi.org/10.26508/lsa.202201479.
Bird S, Panopoulou A, Shea RL, Tsui M, Saso R, Sud A, et al. Response to first vaccination against SARS-CoV-2 in patients with multiple myeloma. Lancet Haematol. 2021;8(6):e389–e392. https://doi.org/10.1016/S2352-3026(21)00110-1.
Bitoun S, Henry J, Vauloup-Fellous C, Dib N, Belkhir R, Mouna L, et al. Response to COVID-19 mRNA vaccination in multiple myeloma is conserved but impaired compared to controls. J Hematol Oncol. 2021;14(1):166. https://doi.org/10.1186/s13045-021-01183-2.
Chan WY, Howells L, Wilson W, Sanchez E, Ainley L, Chavda SJ, et al. Serological response to the BNT162b2 mRNA or ChAdOx1 nCoV-19 COVID-19 vaccine after first and second doses in patients with plasma cell disorders: influence of host and disease factors. Br J Haematol. 2022;196(3):e21–e26. https://doi.org/10.1111/bjh.17864.
Chung DJ, Shah GL, Devlin SM, Ramanathan LV, Doddi S, Pessin MS, et al. Disease- and therapy-specific impact on humoral immune responses to COVID-19 vaccination in hematologic malignancies. Blood Cancer Discov. 2021;2(6):568–76. https://doi.org/10.1158/2643-3230.BCD-21-0139.
Fattizzo B, Bortolotti M, Rampi N, Cavallaro F, Giannotta JA, Bucelli C, et al. Seroconversion to mRNA SARS-CoV-2 vaccines in hematologic patients. Front Immunol. 2022;13:852158. https://doi.org/10.3389/fimmu.2022.852158.
Ghandili S, Schönlein M, Wiessner C, Becher H, Lütgehetmann M, Brehm TT, et al. Lymphocytopenia and anti-CD38 directed treatment impact the serological SARS-CoV-2 response after prime boost vaccination in patients with multiple myeloma. J Clin Med. 2021;10(23):5499. https://doi.org/10.3390/jcm10235499.
Giuseppe M, Claudia R, Antonella M, Angelo S, Domenico P. Long follow-up of symptomatic multiple myeloma patients after Covid-19 vaccination (BNT162b2): a single-institution retrospective experience. Leuk Res Rep. 2022;18:100342. https://doi.org/10.1016/j.lrr.2022.100342.
Greenberg RS, Ruddy JA, Boyarsky BJ, Werbel WA, Garonzik-Wang JM, Segev DL, et al. Safety and antibody response to two-dose SARS-CoV-2 messenger RNA vaccination in patients with multiple myeloma. BMC Cancer. 2021 Dec 27;21(1):1354. https://doi.org/10.1186/s12885-021-09097-5.
Gung C, McGuire R, George M, Abdulkareem A, Belden KA, Porcu P, et al. Antibody response to SARS-CoV-2 vaccination in patients with lymphoproliferative disorders and plasma cell dyscrasias: anti-lymphoma therapy as a predictive biomarker of response to vaccination. Front Oncol. 2022;12:840451. https://doi.org/10.3389/fonc.2022.840451.
Haggenburg S, Hofsink Q, Lissenberg-Witte BI, Broers AEC, van Doesum JA, van Binnendijk RS, et al. Antibody response in immunocompromised patients with hematologic cancers who received a 3-dose mRNA-1273 vaccination schedule for COVID-19. JAMA Oncol. 2022;8(10):1477–483. https://doi.org/10.1001/jamaoncol.2022.3227.
Haggenburg S, Lissenberg-Witte BI, van Binnendijk RS, den Hartog G, Bhoekhan MS, Haverkate NJE, et al. Quantitative analysis of mRNA-1273 COVID-19 vaccination response in immunocompromised adult hematology patients. Blood Adv. 2022;6(5):1537–546. https://doi.org/10.1182/bloodadvances.2021006917.
Hallmeyer S, Thompson MA, Fitzpatrick V, Liao Y, Mullane MP, Medlin SC, et al. Characteristics of patients with hematologic malignancies without seroconversion post-COVID-19 third vaccine dosing. Biol Methods Protoc. 2023;8(1):bpad002. https://doi.org/10.1093/biomethods/bpad002.
Marasco V, Carniti C, Guidetti A, Farina L, Magni M, Miceli R, et al. T-cell immune response after mRNA SARS-CoV-2 vaccines is frequently detected also in the absence of seroconversion in patients with lymphoid malignancies. Br J Haematol. 2022;196(3):548–58. https://doi.org/10.1111/bjh.17877.
Nooka AK, Shanmugasundaram U, Cheedarla N, Verkerke H, Edara VV, Valanparambil R, et al. Determinants of neutralizing antibody response after SARS CoV-2 vaccination in patients with myeloma. J Clin Oncol. 2022;40(26):3057–3064. https://doi.org/10.1200/JCO.21.02257.
Pimpinelli F, Marchesi F, Piaggio G, Giannarelli D, Papa E, Falcucci P, et al. Fifth-week immunogenicity and safety of anti-SARS-CoV-2 BNT162b2 vaccine in patients with multiple myeloma and myeloproliferative malignancies on active treatment: preliminary data from a single institution. J Hematol Oncol. 2021;14(1):81. https://doi.org/10.1186/s13045-021-01090-6.
Ramasamy K, Sadler R, Jeans S, Varghese S, Turner A, Larham J, et al. COVID symptoms, testing, shielding impact on patient-reported outcomes and early vaccine responses in individuals with multiple myeloma. Br J Haematol. 2022;196(1):95–98. https://doi.org/10.1111/bjh.17764.
Re D, Seitz-Polski B, Brglez V, Carles M, Graça D, Benzaken S, et al. Humoral and cellular responses after a third dose of SARS-CoV-2 BNT162b2 vaccine in patients with lymphoid malignancies. Nat Commun. 2022;13(1):864. https://doi.org/10.1038/s41467-022-28578-0.
Stampfer SD, Goldwater MS, Jew S, Bujarski S, Regidor B, Daniely D, et al. Response to mRNA vaccination for COVID-19 among patients with multiple myeloma. Leukemia. 2021;35(12):3534–541. https://doi.org/10.1038/s41375-021-01354-7.
Terao T, Yamashita T, Fukumoto A, Kamura Y, Ikeda D, Kuzume A, et al. Low clinical protective response to SARS-CoV-2 mRNA COVID-19 vaccine in patients with multiple myeloma. Int J Hematol. 2022;115(5):737–47. https://doi.org/10.1007/s12185-022-03300-4.
Terao T, Naduka T, Ikeda D, Fukumoto A, Kamura Y, Kuzume A, et al. Depletion of CD38-positive regulatory T cells by anti-CD38 monoclonal antibodies induces a durable response to SARS-CoV-2 vaccination in patients with plasma cell dyscrasia. Br J Haematol. 2022;197(4):417–21. https://doi.org/10.1111/bjh.18079.
Terpos E, Trougakos IP, Gavriatopoulou M, Papassotiriou I, Sklirou AD, Ntanasis-Stathopoulos I, et al. Low neutralizing antibody responses against SARS-CoV-2 in older patients with myeloma after the first BNT162b2 vaccine dose. Blood. 2021;137(26):3674–676. https://doi.org/10.1182/blood.2021011904.
Thompson MA, Hallmeyer S, Fitzpatrick VE, Liao Y, Mullane MP, Medlin SC, et al. Real-world third COVID-19 vaccine dosing and antibody response in patients with hematologic malignancies. J Patient Cent Res Rev. 2022;9(3):149–57. https://doi.org/10.17294/2330-0698.1952.
Henriquez S, et al. Anti-CD38 therapy impairs SARS-CoV-2 vaccine response against alpha and delta variants in patients with multiple myeloma. Blood. 2022;139(6):942–6.
Storti P et al. Impact of omicron variant on the response to sars-cov-2 mrna vaccination in multiple myeloma. 2022.
Wagner A, et al. SARS-CoV-2-mRNA booster vaccination reverses non-responsiveness and early antibody waning in Immunocompromised patients - A Phase Four Study comparing Immune responses in patients with solid cancers, multiple myeloma and inflammatory bowel disease. Front Immunol. 2022;13:889138.
Enssle JC, et al. Enhanced but variant-dependent serological and cellular immune responses to third-dose BNT162b2 vaccination in patients with multiple myeloma. Cancer Cell. 2022;40(6):587–9.
Enssle JC, et al. Severe impairment of T-cell responses to BNT162b2 immunization in patients with multiple myeloma. Blood. 2022;139(1):137–42.
Zaleska J et al. Response to anti-SARS-CoV-2 mRNA vaccines in multiple myeloma and chronic lymphocytic leukemia patients. Int J Cancer, 2022.
Fillmore NR, et al. Inadequate sars-cov-2 vaccine effectiveness in patients with multiple myeloma: a large nationwide veterans affairs study. Blood. 2021;138(SUPPL 1):400.
Ghandili S et al. Post-vaccination Anti-SARS-CoV-2-Antibody response in patients with multiple myeloma correlates with low CD19 + B-Lymphocyte Count and Anti-CD38 Treatment. Cancers (Basel), 2021; 13(15).
Ntanasis-Stathopoulos I, et al. Second booster BNT162b2 restores SARS-CoV-2 humoral response in patients with multiple myeloma, excluding those under Anti-BCMA therapy. Hemasphere. 2022;6(8):e764.
Schiller Salton N, et al. Attenuated humoral immune response following anti-SARS-CoV-2 vaccine in heavily pretreated patients with multiple myeloma and AL amyloidosis. Am J Hematol. 2021;96(12):E475–8.
Wang L, et al. COVID-19 breakthrough infections, hospitalizations and mortality in fully vaccinated patients with hematologic malignancies: a clarion call for maintaining mitigation and ramping-up research. Blood Rev. 2022;54:100931.
Chen Y, et al. Dynamic SARS-CoV-2-specific B-cell and T-cell responses following immunization with an inactivated COVID-19 vaccine. Clin Microbiol Infect. 2022;28(3):410–8.
Keppler-Hafkemeyer A, et al. Potent high-avidity neutralizing antibodies and T cell responses after COVID-19 vaccination in individuals with B cell lymphoma and multiple myeloma. Nat Cancer. 2023;4(1):81–95.
Chuleerarux N, et al. Immunogenicity of SARS-CoV-2 vaccines in patients with multiple myeloma: a systematic review and meta-analysis. Blood Adv. 2022;6(24):6198–207.
Pratt G, Goodyear O, Moss P. Immunodeficiency and immunotherapy in multiple myeloma. Br J Haematol. 2007;138(5):563–79.
Noonan K, Borrello I. The immune microenvironment of myeloma. Cancer Microenviron. 2011;4(3):313–23.
Rawstron AC, et al. B-lymphocyte suppression in multiple myeloma is a reversible phenomenon specific to normal B-cell progenitors and plasma cell precursors. Br J Haematol. 1998;100(1):176–83.
Pérez-Andres M, et al. Characterization of bone marrow T cells in monoclonal gammopathy of undetermined significance, multiple myeloma, and plasma cell leukemia demonstrates increased infiltration by cytotoxic/Th1 T cells demonstrating a squed TCR-Vbeta repertoire. Cancer. 2006;106(6):1296–305.
Ratta M, et al. Dendritic cells are functionally defective in multiple myeloma: the role of interleukin-6. Blood. 2002;100(1):230–7.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
H.H: Writing, original draft, Statistical analysis, Figure preparation, Study screening; P.F: Writing, original draft, Table preparation; A.K: Writing: revision, Conceptualization, Supervision, Study screening; S.M.H: Writing: original draft; M.M: Writing: original draft; M.A: Table preparation, Study screening, M.A.S: Data extraction; A.H: Writing: revision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests regarding any contents published in this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Harandi, H., Fallahtafti, P., Karimi, A. et al. Examining the immunological responses to COVID-19 vaccination in multiple myeloma patients: a systematic review and meta-analysis. BMC Geriatr 24, 411 (2024). https://doi.org/10.1186/s12877-024-05006-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05006-0