Abstract
This commentary discusses the findings of a study by Tsuchida et al. on the effect of annual hospital admissions of out-of-hospital cardiac arrest patients on survival and neurological outcomes in OHCA patients in the context of existing literature on the topic, and the implications on future studies investigating the volume-outcome relationship in cardiac arrest.
Similar content being viewed by others
This commentary discusses the findings of a study by Tsuchida et al. on the effect of annual hospital admissions of out-of-hospital cardiac arrest (OHCA) patients on survival and neurological outcomes in OHCA patients in the context of existing literature on the topic, and the implications on future studies investigating the volume-outcome relationship in cardiac arrest.
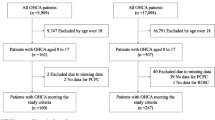
Tsuchida et al. reported the results of a retrospective study which analysed the data of 3632 patients hospitalised for OHCA of cardiac aetiology at 86 hospitals from the Japanese Association for Acute Medicine OHCA registry, a nationwide multihospital prospective database. The main finding of the study was that transport of OHCA patients with prehospital return of spontaneous circulation (ROSC) to a high-volume centre may improve neurological outcomes at 30 days (OR 1.955, 95% confidence interval [CI] 1.033–3.851) [1]. They did not find any significant association between centre volume and survival or neurological outcomes in patients without prehospital ROSC.
The objective of this editorial commentary is to reconcile the conflicting results of current studies regarding the association of centre volume and outcomes in patients with OHCA. The key question we aim to discuss is: Does centre volume alone truly impact outcomes in OHCA patients? Currently, the evidence for high-volume centres remains largely inconclusive. A systematic review by Yeung et al. concluded from pooled data from two studies (n = 3673) that care at a cardiac arrest centre (CAC), the definition of which includes ‘high case volume centres’, was associated with increased likelihood of surviving to hospital discharge with favourable neurological outcome compared to other hospitals (OR 2.22 95% CI 1.74–2.84) [2]. As a result, the International Liaison Committee on Resuscitation (ILCOR) guidelines were updated to recommend that adult non-traumatic OHCA cardiac arrest patients be cared for in CACs rather than in non-CACs [3]. While Tsuchida et al.'s findings add to the pool of evidence for high-volume centres, there is still a significant number of studies that have not found a significant association between centre volume and survival or neurological outcomes. For example, a recent systematic review undertaken by the authors of this letter found no association between centre volume and neurological outcomes, although there may be a slight survival benefit [4]. These findings are diametrically opposed to that of Tsuchida et al.'s. A possible reason for this discrepancy, and a major limitation of many studies on centre volume, is hospital characteristics. The additional neurological benefit in patients with prehospital ROSC who were sent to high volume centres could be attributed to the hospitals’ availability of 24/7 access to percutaneous coronary intervention (PCI) or therapeutic temperature management (TTM), or extracorporeal membrane oxygenation (ECMO). These features comprise the bundle of interventions available in CACs, which was shown in a recent systematic review and meta-analysis by Yeo et al. to improve survival and neurological outcomes [5]. Another recent study by Yoon et al. also found that amongst patients who achieved prehospital ROSC, transfer to a CAC was associated with a higher probability of favourable neurological recovery and survival to discharge compared to conveyance to a non-CAC [6]. Unfortunately, as mentioned by Tsuchida et al., limited information was available on the differences in hospital characteristics, thereby precluding the utilization of factors related to hospitals as covariates in their generalized estimating equations [1]. This is a significant limitation as 24/7 PCI and TTM are important confounders of survival and neurological benefit in OHCA patients. While Tsuchida et al. performed a subgroup analysis for patients who were transported to ECMO-capable hospitals, it is important to note that most of the low- and middle-volume hospitals included in their study were also ECMO-capable and there was no significant difference in ECMO-capability amongst the volume tertiles (p = 0.061). This may have accounted for the lack of significant association found between hospital volume and survival or neurological outcomes in the subgroup of patients sent to ECMO-capable hospitals. Considering that even the smaller hospitals in this study were well-equipped with invasive and advanced technologies such as ECMO, which is currently not the case worldwide, the organisation of the Japanese territory in question may not be generalizable to the global setting not just in terms of availability of resources but also, different Emergency Medical Services (EMS), resuscitation practises on transport, and hospital organizations. This may have contributed to the difference in results with the recent systematic review [4]. While on the subject of ECMO, studies have also demonstrated the feasibility and benefits of extracorporeal cardiopulmonary resuscitation (ECPR) in increasing survival with good neurological outcomes [7], which indirectly increases the evidence in support of transporting and treating OHCA patients in CACs.
In conclusion, current evidence is insufficient to ascertain if centre volume should be a key factor in deciding where OHCA patients, regardless of patient characteristics, should be transported. Future studies are encouraged to adjust for other components of post-cardiac arrest care, such as 24/7 PCI, TTM and ECMO capability, to determine if centre volume alone is associated with survival or neurological outcomes in OHCA patients.
Availability of data and materials
Not applicable.
Abbreviations
- CAC:
-
Cardiac arrest centre
- CI:
-
Confidence interval
- ECPR:
-
Extracorporeal cardiopulmonary resuscitation
- ECMO:
-
Extracorporeal membrane oxygenation
- EMS:
-
Emergency medical services
- ILCOR:
-
International Liaison Committee on Resuscitation
- OHCA:
-
Out-of-hospital cardiac arrest
- PCI:
-
Percutaneous coronary intervention
- ROSC:
-
Return of spontaneous circulation
- TTM:
-
Therapeutic temperature management
References
Tsuchida T, Ono K, Maekawa K, et al. Effect of annual hospital admissions of out-of-hospital cardiac arrest patients on prognosis following cardiac arrest. BMC Emerg Med. 2022;22:121. https://doi.org/10.1186/s12873-022-00685-7.
Yeung J, Matsuyama T, Bray J, Reynolds J, Skrifvars MB. Does care at a cardiac arrest centre improve outcome after out-of- hospital cardiac arrest?—a systematic review. Resuscitation. 2019;137:102–15. https://doi.org/10.1016/j.resuscitation.2019.02.006.
Soar J, Maconochie I, Wyckoff MH, et al. 2019 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: summary from the basic life support; advanced life support; pediatric life support; neonatal life support; education, implementation, and teams; and first aid task forces. Circulation. 2019;140(24):e826–80. https://doi.org/10.1161/CIR.0000000000000734.
Goh AXC, Seow JC, Lai MYH, et al. Association of high-volume centers with survival outcomes among patients with nontraumatic out-of-hospital cardiac arrest: a systematic review and meta-analysis. JAMA Netw Open. 2022;5:e2214639. https://doi.org/10.1001/jamanetworkopen.2022.14639.
Yeo JW, Ng ZHC, Goh AXC, et al. Impact of cardiac arrest centers on the survival of patients with nontraumatic out‐of‐hospital cardiac arrest: a systematic review and meta‐analysis. J Am Heart Assoc. 0:e023806. https://doi.org/10.1161/JAHA.121.023806
Yoon H, Ahn KO, Park JH, Lee SY. Effects of pre-hospital re-arrest on outcomes based on transfer to a heart attack centre in patients with out-of-hospital cardiac arrest. Resuscitation. 2022;170:107–14. https://doi.org/10.1016/j.resuscitation.2021.11.012.
Scquizzato T, Bonaccorso A, Consonni M, et al. Extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest: a systematic review and meta-analysis of randomized and propensity score-matched studies. Artif Organs. 2022;46(5):755–62. https://doi.org/10.1111/aor.14205.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
AXCG drafted the manuscript under the supervision of AFWH. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Goh, A.X.C., Ho, A.F.W. Correspondence: is there an association between centre volume and survival or neurological outcomes among out-of-hospital cardiac arrest patients?. BMC Emerg Med 22, 197 (2022). https://doi.org/10.1186/s12873-022-00743-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12873-022-00743-0