Abstract
Previously, the SOS-KANTO 2012 studies, conducted in the Kanto area of Japan, reported a summary of outcomes in patients with out-of-hospital cardiac arrest (OHCA). This sub-analysis of the SOS-KANTO study 2017 aimed to evaluate the neurological outcomes of paediatric OHCA patients, by comparing the SOS-KANTO 2012 and 2017 studies. All OHCA patients, aged < 18 years, who were transported to the participating hospitals by EMS personnel were included in both SOS-KANTO studies (2012 and 2017). The number of survival patients with favourable neurological outcomes (paediatric cerebral performance category 1 or 2) at 1 month did not improve between 2012 and 2017. There was no significant difference in achievement of pre-hospital return of spontaneous circulation (ROSC) [odds ratio (OR): 2.00, 95% confidence interval (95% CI): 0.50–7.99, p = 0.50] and favourable outcome at 1 month [OR: 0.67, 95% CI: 0.11–3.99, p = 1] between the two studies, matched by age, witnessed arrest, bystander CPR, aetiology of OHCA, and time from call to EMS arrival. Multivariable logistic regression showed no significant difference in the achievement of pre-hospital ROSC and favourable outcomes at 1 month between the two studies.
Similar content being viewed by others
Introduction
Although 120,000 out-of-hospital cardiac arrests (OHCAs) occur annually in Japan, paediatric OHCAs are very rare, accounting for less than 1% of all cases1,2,3,4. OHCA in paediatric patients is a major global health concern, and there are approximately 1000–2000 cases in Japan annually. The survival rate is still poor, and only approximately 10–20% of paediatric patients survive 1 month after OHCA, despite a gradual improvement in the survival rate1,3,5. Previously, the SOS-KANTO 2002 and 2012 studies, conducted in the Kanto area of Japan, reported a summary of outcomes in OHCA patients. Compared to the SOS-KANTO 2002 study, favourable neurological outcomes at 1 month after OHCA in adult patients significantly improved in the SOS-KANTO 2012 study, which may be partly explained by the changes in Japanese law that expanded the therapeutic interventions that emergency medical service (EMS) personnel can perform in the pre-hospital setting. Under the amended laws, trained EMS personnel have been permitted to perform defibrillation since 2003, endotracheal intubation since 2004, and intravenous adrenaline administration with remote instruction from a doctor since 2006 in adult OHCA patients but not in paediatric OHCA patients aged < 8 years. Therapeutic procedures by EMS for paediatric OHCA patients aged < 8 years did not change between the study periods. In fact, EMS personnel can only perform bag-valve-mask ventilation and chest compression on paediatric OHCA patients during transport to the hospital. In some areas, ambulances with doctors or helicopters with doctors are in operation; doctors can perform endotracheal intubation or adrenalin administration via the intravenous or intraosseous route in the pre-hospital setting5,6,7,8.
This sub-analysis of the SOS-KANTO study 2017 aimed to evaluate the changes in pre-hospital procedures performed by EMS personnel or physicians and in-hospital treatment, and the outcomes of paediatric OHCA patients, by comparing the SOS-KANTO studies from 2012 and 2017.
Results
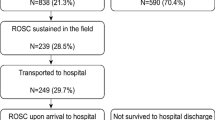
A total of 267 of the 17,098 OHCA patients from the SOS-KANTO 2012 study and 160 of the 9909 OHCA patients from the SOS-KANTO 2017 study met the inclusion criteria (Fig. 1).
Table 1 summarizes the baseline patient demographics and characteristics of the SOS-KANTO 2012 and 2017 groups. The median age was significant higher in the SOS-KANTO 2017 study than that in the SOS-KANTO 2012 study (3.5 vs. 1, p < 0.05). There were significant differences in arrest location and aetiology of OHCA between the two groups. (p < 0.05). Most paediatric patients [115 (71.9%) from the SOS-KANTO 2017 study and 165 (58.1%) from the SOS-KANTO 2012 study] suffered OHCA at home, and some experienced OHCA in a public place.
Table 2 shows the results of pre-hospital interventions. Bag-valve mask ventilation was the most frequently used method for advanced airway management by EMS personnel [131 (81.9%) in SOS-KANTO 2017 and 227 (85.0%) in SOS-KANTO 2012] followed by supraglottic airway device. Only 1 (0.6%) and 6 (2.2%) patients underwent endotracheal intubation in SOS-KANTO 2017 and 2012, respectively, but the difference was not significant. There were significant differences between the groups in the number of adrenalin doses, release of asphyxia, time from call to EMS arrival, and presence of physician at the pre-hospital scene.
Table 3 summarizes the in-hospital interventions. Fifteen (9.4%) and 11 (4.1%) patients achieved ROSC before reaching the hospital, and 25 (15.6%) and 51 (19.1%) patients achieved ROSC after reaching the hospital in SOS-KANTO 2017 and 2012, respectively. There was no significant difference in ROSC rate between the groups. There were also no significant differences in in-hospital interventions, such as endotracheal intubation, defibrillation, adrenalin administration, or target temperature management.
Table 4 shows the outcomes in the SOS-KANTO 2017 and 2012 studies. The number of surviving patients with favourable neurological outcome (PCPC 1 or 2) at 1 month did not improve between 2012 and 2017. In addition, the survival rate at 1 month showed a slight but not significant increase. The most frequent outcome in both studies was PCPC 6 (brain death or death).
The results of the multivariable logistic analysis for the achievement of pre-hospital ROSC and favourable neurological outcome are shown in Table 5. There was no significant difference in achievement of pre-hospital ROSC (OR: 2.00, 95% CI: 0.50–7.99, p = 0.50) and favourable outcome at 1 month (OR: 0.67, 95% CI: 0.11–3.99, p = 1) between the two study periods, matched by age, witnessed arrest, bystander CPR, aetiology of OHCA, and time from call to EMS arrival.
Discussion
This study compared epidemiological data on cardiopulmonary resuscitation in the Kanto area between 2012 and 2017. To our knowledge, this is the first large study to compare the outcome of paediatric OHCA in different periods in the Kanto area. Although there are several reports on paediatric OHCA based on analyses of the National Utstein Registry, a nationwide population-based OHCA registry, they all report neurological outcomes by cerebral performance category (CPC), and not PCPC4,5,7. The number of OHCA patients between SOS-KANTO 2012 and 2017 studies differ significantly. It is assumed that the number of OHCA patients were decreased and registration was delayed due to pandemic of COVID-19. In fact, although the study period was longer than previous study, the number of patients enrolled in the registry was half of previous study. According to the demographic data in Japan, the number of infant deaths has been decreased from 2292 in 2012 to 1512 in 2020, and this may be one of the factors. An analysis of SOS-KANTO registry data between 2012 and 2017 revealed no significant differences in one-month survival, with favourable neurological outcome set as the primary outcome, during the last 5 years of the period. Despite analysing the data by multivariable logistic regression and matching the groups by age, witnessed arrest, bystander CPR, time from call to EMS arrival, and aetiology of OHCA, there were no significant differences in favourable neurological outcome or achievement of pre-hospital ROSC between the two periods.
Although there were no significant differences in bystander CPR or witnessed arrest, which have been suggested as a predictors for favourable neurological outcome after OHCA, between the two periods, the rate of bystander CPR showed a slight increase from 43.1% in 2012 to 49.4% in 20179,10,11. There was no significant difference in one-month survival, with favourable neurological outcome set as the primary outcome, between two periods. In fact, there were no significant differences in the procedures performed at the pre-hospital scene by EMS personnel between the two periods. Pre-hospital care may be related to the lack of improvement in survival outcome. A comparison of SOS-KANTO 20202 and 2012 study of adults, the survival rate with favorable neurological outcome has been improved due to the approval of tracheal intubation in 2004, the administration of adrenaline in 2006 for EMS personnel, and widespread use of AED9,10. Since there was no change in pre-hospital care provided by EMS personnel for children between two study periods, it could be assumed that there was no change in outcomes. The rate of physician presence at the pre-hospital scene was higher in 2017 than that in 2012 (13.1% vs 4.5%, p < 0.05). The success rate of ROSC at the pre-hospital scene was higher in 2017 than in 2012. Although physician presence at the pre-hospital scene may have affected the success rate of ROSC, no significant differences were observed in the rate of advanced airway management or time to adrenaline administration, which limits the generalization of these findings. The success rate of ROSC at the pre-hospital scene was higher in 2017, but it was not linked to favourable neurological outcome.
Although limited to adults with OHCA, a comparison of the SOS-KANTO 2002 and 2012 studies showed improved favourable neurological outcome in 2012 compared to that in 200210. Increasing the frequency of bystander CPR and automated external defibrillator (AED) use and improving the therapeutic management after ROSC would be particularly beneficial to patients9,10. In this study period, there was no significant increase in the rate of bystander CPR or in the use of AED, even though CPR and AED are thought to have been become more popular among the general population9.
A predictor for the success of resuscitation at the pre-hospital scene in paediatric OHCA has not been yet established. Age, bystander CPR, and earlier initiation of CPR by EMS personnel are potential predictors for the success of resuscitation at the pre-hospital scene12,13,14,15,16,17,18,19,20,21. Although there are several reports of shockable rhythm as initial rhythm, related to 1-month survival or favourable neurological outcome, the reported rate of shockable rhythm in paediatric OHCA patients in Japan is very low (3.9–4.9%)14,16,19. In this study, the rate of paediatric OHCA patients with shockable rhythm was also very low (1.9% in 2017 and 2.6% in 2012). This may explain the low rate of favourable neurological outcome in the SOS-KANTO study in both periods.
Some previous studies on paediatric OHCA based on the National Utstein Registry reported no significant difference in favourable neurological outcome in paediatric OHCA patients between advanced airway management (AAM), such as endotracheal intubation (ETI) or supraglottic airway device (SGA), and bag-valve-mask ventilation (BVM) management at the pre-hospital scene5,7,8,22,23. In this study, there was also no significant difference between the two periods in AAM at the pre-hospital scene. A previous systematic review revealed no significant difference in survival discharge or favourable neurological outcome between AAM and BVM24, which suggests the importance of implementing reliable BVM ventilation rather than unreasonable AAM.
Pre-hospital AAM has an important role in paediatric OHCA since the respiratory aetiology is a major cause of this condition15,25,26,27. A previous report indicated that the neurological outcome of paediatric OHCA may be improved by ensuring reliable airway management by AAM in cases of non-cardiac aetiology8. For ensuring the airway management, EMS personnel can use ETI or SGA. Although ETI is more frequently used than SGA for airway management in the US, SGA is used more frequently than ETI in Japan23,28. It is because that the EMS system in Japan is different from that in other countries6. There are age restrictions on the procedures that can be performed by EMS personnel at the pre-hospital scene. For instance, EMS personnel is not allowed to perform ETI in patients younger than 8 years old by Japanese law.
No RCTs have been conducted on the effect of adrenaline administration in paediatric OHCA patients, and there are only a few observational studies on this subject29,30. In this paediatric OHCA study, the adrenaline effect was limited due to the small sample size and the fact that only descriptive evidence was provided. Instead, the current recommendation of adrenaline administration for paediatric cardiac arrest is based on adult OHCA studies. Therefore, we considered the evidence of adult OHCA for paediatric OHCA. Although, there is substantial evidence about the effect of adrenaline on adult cardiac arrest, the prognosis and neurological status after a long-term period remains controversial31. Although more doses of adrenaline were administered in 2017 than in 2012, there were no significant differences between the two periods in the time elapsed from call to adrenaline administration, time from call to EMS arrival, intervention at hospital, 1-month survival rate, or favourable neurological outcome. In addition, our results revealed a much lower proportion of adrenaline administration in the pre-hospital setting than the proportion reported in other countries. A previous study reported a proportion of 8.3% of adrenaline administration from 2007 to 20106. In our study, the proportion rate of adrenaline administration was also low (8.1%), and it has not changed in nearly decade. On the other hand, the proportion rate of adrenaline administration in the US is higher than that of our study (73.3% vs 8.1%)32. The difference might be due to differences in the EMS system, including the fact that there are age restrictions for intravenous access placement and adrenaline administration performed by EMS personnel in Japan. EMS personnel are not allowed to perform intravenous or interosseous access placement in paediatric patients aged < 8 years. Currently, EMS personnel can only provide BVM ventilation and chest compression to paediatric OHCA patients. The procedures that EMS personnel can perform have not changed since the last study period, which might explain the lack of significant differences between the two periods in terms of favourable neurological outcome or achievement of pre-hospital ROSC in paediatric OHCA patients. One of the special notes in this study is that one month survival rate was lower than other OHCA studies. One month survival rate was 11.9% in our study, but one month survival rate in therapeutic Hypothermia after Pediatric Cardiac Arrest Out-of-Hospital (THAPCA-OH) trial is significant differ at 33.4%33. The THAPCA clinical trial is a high-quality RCT that provides well-informed, evidence based information and is well worth reporting. Although a direct comparison between SOS-KANTO 2017 study and THAPCA-OH trial is not possible, there are some factors that could account for difference in survival rate. It has been reported that a shorter time to adrenaline administration improves the ROSC rate in pediatric OHCA, but in Japan, pre-hospital care of EMS personnel is legally restricted, EMS personnel cannot administer adrenaline, and must transport the patients with only BVM ventilation and chest compression32,34. The median time of first adrenaline administration in our study was 33 min, which differs significantly from previous study, median time was 7.6 min34. The rate of ROSC and rate of survival to hospital discharge are very low, because EMS personnel transport all OHCA patients to the hospital, unless a cadaveric reaction such as rigor mortis or cadaveric spots is manifested, regardless of the patient age in Japan12,13,14,35. It is assumed that these factors influence the difference in survival rate.
Our study has some strengths. First, our study used PCPC for assessing neurological outcome, which is different from the methods used in previous studies analysing the National Utstein Registry that reported neurological outcomes in paediatric OHCA patients using CPC. As the National Utstein Registry does not collect PCPC data, the SOS-KANTO study data are more suitable for assessing neurological outcomes in paediatric OHCA patients, and hence in this study, we used PCPC for neurological assessment. Another strength of our study was the comparison between paediatric patients from two large databases from 2012 and 2017 that were prospectively collected by EMS personnel and hospital staff in the same area.
There are also some limitations to our study. First, the SOS-KANTO study did not include all hospitals in the Kanto area; therefore, there may be a selection bias towards more academically focused or resource-rich hospitals that were able to join the SOS-KANTO study. Second, the procedures that EMS personnel are allowed to perform are slightly different from other countries; particularly, the EMS personnel are not permitted to perform interosseous access for OHCA patients, regardless of adults or children8,36. There is confounding bias, because the EMS personnel are not permitted to perform intravenous placement or adrenaline administration in paediatric OHCA patients aged < 8 years. Third, the SOS-KANTO study used retrospective data, and the accuracy, precision, or failure of the procedures performed by EMS personnel in the pre-hospital setting are not completely clear. Fourth, the frequency of autopsy in Japan is very low, and the aetiology of paediatric OHCA is sometimes diagnosed tentatively. Finally, as with all epidemiological studies, the integrity, validity, and ascertainment bias of the data are potential limitations.
In conclusion, this is the first large study to compare the outcome of paediatric OHCA in different periods in the Kanto area by PCPC. There was no significant difference in the achievement of pre-hospital ROSC and favourable outcomes at 1 month between the two study periods analysed by multivariable logistic regression. It is revealed that there was no change in outcomes between two study periods, and that outcomes differed significantly from the rest of the other countries. Besides, there was no change in pre-hospital care over this time period. Hopefully, our study and further research provide the paradigm shift in pre-hospital care by EMS personnel.
Methods
Study design
The SOS-KANTO 2012 study was undertaken in the Kanto area of Japan and included 68 hospitals. It was supported by the Kanto Regional Group of the Japanese Association for Acute Care Medicine between January 2012 and March 20139. More recently, the SOS-KANTO 2017 study was a prospective survey that aimed to collect the data on patients with OHCA in the Kanto area, between April 2019 and July 2021, with the participation of 46 hospitals. The study period of SOS-KANTO 2017 was longer than that of SOS-KANTO 2012 as it was not possible to collect enough data during the coronavirus disease pandemic. This study was approved by the relevant institutional review boards of all 46 hospitals.
Definitions and data collection
Cardiac arrest was defined as the absence of cardiac activity with pulse and normal breathing37. All OHCA patients who were transported to the participating hospitals by EMS personnel were included in both SOS-KANTO studies (2012 and 2017). This sub-analysis of the SOS-KANTO 2017 study included only paediatric patients (aged < 18). Pre- and in-hospital treatment were provided by EMS personnel, physicians and other healthcare providers38,39. EMS personnel collected the pre-hospital information and Utstein style outcome reports37. They collected information on the patients’ characteristics, initial cardiac rhythm, and the time course of resuscitation. Additional information included whether the arrest was witnessed by a bystander, whether a bystander initiated cardiopulmonary resuscitation (CPR), whether the patient was intubated, whether epinephrine was administered, and whether the patients achieved return of spontaneous circulation (ROSC) before arriving at the hospital.
The causes of cardiac arrest were defined by the physician at the hospital and were diagnosed as cardiac aetiology unless an obvious non-cardiac aetiology (i.e., cerebrovascular disease, respiratory disease, severe trauma, drowning, asphyxiation, or drug overdose) was observed.
A physician or institutional researcher collected the following in-hospital information; medications for resuscitation, interventions, laboratory data, length of hospital stay, and neurological outcome at 1 month from the cardiac arrest. Neurological outcome was evaluated using the Paediatric Cerebral Performance Category (PCPC) scale (1: good cerebral performance, 2: mild cerebral disability, 3: moderate cerebral disability, 4: severe cerebral disability, 5: come/vegetate state, 6: brain death/death)37.
Ethical approval and consent to participate
The Ethics Committee of Juntendo University Urayasu Hospital approved the SOS-KANTO 2017 study data analysis (approval number: 1-022) The requirement for patient or parent consent was waived by the Ethics Committee of Juntendo University Urayasu Hospital as this was an epidemiologic study that used anonymized data. We used the STROBE statement as a guide for reporting this study.
This study was approved by the Institutional Review of Juntendo University Urayasu Hospital, Chiba, Japan (1-022) and was conducted in accordance with the principles outlined in the 1964 Declaration of Helsinki and its later amendments.
Selection of participants
We evaluated paediatric patients aged < 18 years with cardiac arrest, who received CPR by the EMS personnel and were transported to the participating hospitals. We excluded cases with missing data on the following variables: (1) main outcomes at 1 month survival with favourable neurological outcome or ROSC; (2) time course of CPR by EMS personnel or physicians; (3) arrest witness or bystander CPR initiation; and (4) in-hospital treatment.
Outcome measures
The primary outcome measure was paediatric patient survival with favourable neurological outcome at 1 month from cardiac arrest, which was defined as PCPC Scale 1 or 2. The secondary outcome was the success rate of ROSC.
Statistical analysis
To display patient data, median with interquartile range (IQR) was used for numerical variables. Baseline patient characteristics from the SOS-KANTO 2012 and 2017 studies were compared using the chi-square test or Fisher’s exact test for frequencies, and a t-test or Mann–Whitney U-test was used for continuous variables, as appropriate. Differences were considered significant when the P-value was less than 0.05. To assess the independent effect of the study, multivariable logistic regression analysis was performed on the success rate of ROSC and favourable neurological outcome at 1 month. Age, witness arrest, bystander CPR, aetiology of OHCA, and time from call to EMS arrival were included as variables in the analysis. Data management and statistical analysis were performed using the EZR software (Y Kaneda, Saitama Medical Centre, Jichi Medical University, Saitama Japan).
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to including of privacy but are available from the corresponding author on reasonable request.
Abbreviations
- OHCA:
-
Out-of-hospital cardiac arrest
- EMS:
-
Emergency medical service
- CPR:
-
Cardiopulmonary resuscitation
- ROSC:
-
Return of spontaneous circulation
- PCPC:
-
Paediatric cerebral performance category
- IQR:
-
Interquartile range
- CPC:
-
Cerebral performance category
- AED:
-
Automated external defibrillator
- AAM:
-
Advanced airway management
- ETI:
-
Endotracheal intubation
- SGA:
-
Supraglottic airway device
- BVM:
-
Bag-valve-mask
References
Kitamura, T. et al. Nationwide improvements in survival from out-of-hospital cardiac arrest in Japan. Circulation 126, 2834–2843. https://doi.org/10.1161/circulationaha.112.109496 (2012).
Nakahara, S. et al. Association of bystander interventions with neurologically intact survival among patients with bystander-witnessed out-of-hospital cardiac arrest in Japan. JAMA 314, 247–254. https://doi.org/10.1001/jama.2015.8068 (2015).
Fukuda, T. et al. Conventional versus compression-only versus no-bystander cardiopulmonary resuscitation for pediatric out-of-hospital cardiac arrest. Circulation 134, 2060–2070. https://doi.org/10.1161/circulationaha.116.023831 (2016).
Fukuda, T. et al. Effect of prehospital epinephrine on out-of-hospital cardiac arrest: A report from the national out-of-hospital cardiac arrest data registry in Japan, 2011–2012. Eur. J. Clin. Pharmacol. 72, 1255–1264. https://doi.org/10.1007/s00228-016-2093-2 (2016).
Okubo, M. et al. Prehospital advanced airway management for paediatric patients with out-of-hospital cardiac arrest: A nationwide cohort study. Resuscitation 145, 175–184. https://doi.org/10.1016/j.resuscitation.2019.09.007 (2019).
Matsuyama, T. et al. Pre-hospital administration of epinephrine in pediatric patients with out-of-hospital cardiac arrest. J. Am. Coll. Cardiol. 75, 194–204. https://doi.org/10.1016/j.jacc.2019.10.052 (2020).
Fukuda, T. et al. Type of advanced airway and survival after pediatric out-of-hospital cardiac arrest. Resuscitation 150, 145–153. https://doi.org/10.1016/j.resuscitation.2020.02.005 (2020).
Ohashi-Fukuda, N., Fukuda, T., Doi, K. & Morimura, N. Effect of prehospital advanced airway management for pediatric out-of-hospital cardiac arrest. Resuscitation 114, 66–72. https://doi.org/10.1016/j.resuscitation.2017.03.002 (2017).
Group S.-K. S. Changes in pre- and in-hospital management and outcomes for out-of-hospital cardiac arrest between 2002 and 2012 in Kanto, Japan: The SOS-KANTO 2012 Study. Acute Med. Surg. 2, 225–233. https://doi.org/10.1002/ams2.102 (2015).
Group S.-K. S. Changes in treatments and outcomes among elderly patients with out-of-hospital cardiac arrest between 2002 and 2012: A post hoc analysis of the SOS-KANTO 2002 and 2012. Resuscitation 97, 76–82. https://doi.org/10.1016/j.resuscitation.2015.09.379 (2015).
Goto, Y., Funada, A. & Nakatsu-Goto, Y. Neurological outcomes in children dead on hospital arrival. Crit. Care 19, 410. https://doi.org/10.1186/s13054-015-1132-1 (2015).
Morrison, L. J. et al. Part 3: Ethics: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 122, S665-675. https://doi.org/10.1161/circulationaha.110.970905 (2010).
Lippert, F. K., Raffay, V., Georgiou, M., Steen, P. A. & Bossaert, L. European Resuscitation Council Guidelines for Resuscitation 2010 Section 10. The ethics of resuscitation and end-of-life decisions. Resuscitation 81, 1445–1451. https://doi.org/10.1016/j.resuscitation.2010.08.013 (2010).
Goto, Y., Maeda, T. & Nakatsu-Goto, Y. Decision tree model for predicting long-term outcomes in children with out-of-hospital cardiac arrest: A nationwide, population-based observational study. Crit. Care 18, R133. https://doi.org/10.1186/cc13951 (2014).
Atkins, D. L. et al. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: The Resuscitation Outcomes Consortium epistry-cardiac arrest. Circulation 119, 1484–1491. https://doi.org/10.1161/circulationaha.108.802678 (2009).
Kitamura, T. et al. Conventional and chest-compression-only cardiopulmonary resuscitation by bystanders for children who have out-of-hospital cardiac arrests: A prospective, nationwide, population-based cohort study. Lancet 375, 1347–1354. https://doi.org/10.1016/s0140-6736(10)60064-5 (2010).
Donoghue, A. J. et al. Out-of-hospital pediatric cardiac arrest: An epidemiologic review and assessment of current knowledge. Ann. Emerg. Med. 46, 512–522. https://doi.org/10.1016/j.annemergmed.2005.05.028 (2005).
Fallat, M. E. Withholding or termination of resuscitation in pediatric out-of-hospital traumatic cardiopulmonary arrest. Pediatrics 133, e1104-1116. https://doi.org/10.1542/peds.2014-0176 (2014).
Park, C. B. et al. Pediatric out-of-hospital cardiac arrest in Korea: A nationwide population-based study. Resuscitation 81, 512–517. https://doi.org/10.1016/j.resuscitation.2009.11.022 (2010).
Nitta, M. et al. Age-specific differences in outcomes after out-of-hospital cardiac arrests. Pediatrics 128, e812-820. https://doi.org/10.1542/peds.2010-3886 (2011).
Li, C. J. et al. Factors associated with sustained return of spontaneous circulation in children after out-of-hospital cardiac arrest of noncardiac origin. Am. J. Emerg. Med. 28, 310–317. https://doi.org/10.1016/j.ajem.2008.12.018 (2010).
Gausche, M. et al. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: A controlled clinical trial. JAMA 283, 783–790. https://doi.org/10.1001/jama.283.6.783 (2000).
Hansen, M. L. et al. A comparison of pediatric airway management techniques during out-of-hospital cardiac arrest using the CARES database. Resuscitation 120, 51–56. https://doi.org/10.1016/j.resuscitation.2017.08.015 (2017).
Lavonas, E. J. et al. Advanced airway interventions for paediatric cardiac arrest: A systematic review and meta-analysis. Resuscitation 138, 114–128. https://doi.org/10.1016/j.resuscitation.2019.02.040 (2019).
Young, K. D., Gausche-Hill, M., McClung, C. D. & Lewis, R. J. A prospective, population-based study of the epidemiology and outcome of out-of-hospital pediatric cardiopulmonary arrest. Pediatrics 114, 157–164. https://doi.org/10.1542/peds.114.1.157 (2004).
Sirbaugh, P. E. et al. A prospective, population-based study of the demographics, epidemiology, management, and outcome of out-of-hospital pediatric cardiopulmonary arrest. Ann. Emerg. Med. 33, 174–184. https://doi.org/10.1016/s0196-0644(99)70391-4 (1999).
Kuisma, M., Suominen, P. & Korpela, R. Paediatric out-of-hospital cardiac arrests—Epidemiology and outcome. Resuscitation 30, 141–150. https://doi.org/10.1016/0300-9572(95)00888-z (1995).
Fink, E. L. et al. Unchanged pediatric out-of-hospital cardiac arrest incidence and survival rates with regional variation in North America. Resuscitation 107, 121–128. https://doi.org/10.1016/j.resuscitation.2016.07.244 (2016).
Enright, K., Turner, C., Roberts, P., Cheng, N. & Browne, G. Primary cardiac arrest following sport or exertion in children presenting to an emergency department: Chest compressions and early defibrillation can save lives, but is intravenous epinephrine always appropriate?. Pediatr. Emerg. Care 28, 336–339. https://doi.org/10.1097/PEC.0b013e31824d8c78 (2012).
Tibballs, J. & Kinney, S. A prospective study of outcome of in-patient paediatric cardiopulmonary arrest. Resuscitation 71, 310–318. https://doi.org/10.1016/j.resuscitation.2006.05.009 (2006).
Gough, C. J. R. & Nolan, J. P. The role of adrenaline in cardiopulmonary resuscitation. Crit. Care 22, 139. https://doi.org/10.1186/s13054-018-2058-1 (2018).
Hansen, M. et al. Time to epinephrine administration and survival from nonshockable out-of-hospital cardiac arrest among children and adults. Circulation 137, 2032–2040. https://doi.org/10.1161/circulationaha.117.033067 (2018).
Moler, F. W. et al. Therapeutic hypothermia after out-of-hospital cardiac arrest in children. N. Engl. J. Med. 372, 1898–1908. https://doi.org/10.1056/NEJMoa1411480 (2015).
Banerjee, P. R. et al. Early on-scene management of pediatric out-of-hospital cardiac arrest can result in improved likelihood for neurologically-intact survival. Resuscitation 135, 162–167. https://doi.org/10.1016/j.resuscitation.2018.11.002 (2019).
Goto, Y., Maeda, T. & Goto, Y. N. Termination-of-resuscitation rule for emergency department physicians treating out-of-hospital cardiac arrest patients: An observational cohort study. Crit. Care 17, R235. https://doi.org/10.1186/cc13058 (2013).
Hasegawa, K., Tsugawa, Y., Camargo, C. A. Jr., Hiraide, A. & Brown, D. F. Regional variability in survival outcomes of out-of-hospital cardiac arrest: The All-Japan Utstein Registry. Resuscitation 84, 1099–1107. https://doi.org/10.1016/j.resuscitation.2013.03.007 (2013).
Jacobs, I. et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update and simplification of the Utstein templates for resuscitation registries. A statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa). Resuscitation 63, 233–249. https://doi.org/10.1016/j.resuscitation.2004.09.008 (2004).
Association, T. F. o. t. A. H. Guidelines 2000 for cardiopulmonary resuscitation and emergency cardiovascular care. Part 3: Adult basic life support. The American Heart Association in collaboration with the International Liaison Committee on Resuscitation. Circulation 102, I22– I59 (2000).
Field, J. M. et al. Part 1: EXECUTIVE summary: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 122, S640-656. https://doi.org/10.1161/circulationaha.110.970889 (2010).
Acknowledgements
As data for this were provided by SOS-KANTO 2017 study group, we wish to thank the member of the SOS-KANTO 2017 study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. T.I. collected and analysed the data and wrote the first draft of the manuscript. R.S., Y.E., S.A., M.Y. and S.O. provided critical review. All authors read and approved the final manuscript. The need for informed consent was waived by the Institutional Review Board due to the retrospective nature of the study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ishihara, T., Sasaki, R., Enomoto, Y. et al. Changes in pre- and in-hospital management and outcomes among children with out-of-hospital cardiac arrest between 2012 and 2017 in Kanto, Japan. Sci Rep 13, 10092 (2023). https://doi.org/10.1038/s41598-023-37201-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-37201-1
- Springer Nature Limited