Abstract
Background
Although the prognosis of patients treated at specialized facilities has improved, the relationship between the number of patients treated at hospitals and prognosis is controversial and lacks constancy in those with out-of-hospital cardiac arrest (OHCA). This study aimed to clarify the effect of annual hospital admissions on the prognosis of adult patients with OHCA by analyzing a large cohort.
Methods
The effect of annual hospital admissions on patient prognosis was analyzed retrospectively using data from the Japanese Association for Acute Medicine OHCA registry, a nationwide multihospital prospective database. This study analyzed 3632 of 35,754 patients hospitalized for OHCA of cardiac origin at 86 hospitals. The hospitals were divided into tertiles based on the volume of annual admissions. The effect of hospital volume on prognosis was analyzed using logistic regression analysis with multiple imputation. Furthermore, three subgroup analyses were performed for patients with return of spontaneous circulation (ROSC) before arrival at the emergency department, patients admitted to critical care medical centers, and patients admitted to extracorporeal membrane oxygenation-capable hospitals.
Results
Favorable neurological outcomes 30 days after OHCA for patients overall showed no advantage for medium- and high-volume centers over low-volume centers; Odds ratio (OR) 0.989, (95% Confidence interval [CI] 0.562-1.741), OR 1.504 (95% CI 0.919-2.463), respectively. However, the frequency of favorable neurological outcomes in OHCA patients with ROSC before arrival at the emergency department at high-volume centers was higher than those at low-volume centers (OR 1.955, 95% CI 1.033-3.851).
Conclusion
Hospital volume did not significantly affect the prognosis of adult patients with OHCA. However, transport to a high-volume hospital may improve the neurological prognosis in OHCA patients with ROSC before arrival at the emergency department.
Similar content being viewed by others
Background
Out-of-hospital cardiac arrest (OHCA) occurs in 250,000 to 300,000 patients worldwide each year [1]. Advances have been made in the management of cardiac arrest, including modern cardiopulmonary resuscitation (CPR), extracorporeal CPR, emergency cardiovascular therapy, and targeted temperature management [2]. However, the in-hospital survival and neurologically intact survival rates remain disappointingly low in patients with a successful return of spontaneous circulation (ROSC) [3].
The outcomes for patients with OHCA have been shown to improve with the quality of round-the-clock post-resuscitation care [4, 5], while the frequency of post-resuscitation care in the emergency department also exerts a positive impact on patient outcomes [6, 7]. Current European resuscitation guidelines also indicate that transport of OHCA patients to high-volume centres may improve prognosis [8, 9]. However, there is a coexistence of studies showing improved outcomes in hospitals with larger volume [10,11,12,13,14], and studies showing no improvement [15,16,17]. One conclusion drawn today from low-quality data is that cardiac arrest centers may be associated with improved outcomes at discharge, but the certainty of that evidence is very low [18].
The relationship between the number of surgeries performed in hospitals and patient outcomes has been studied since the 1980s [19, 20]. In recent years, several studies have reported on the relationship between patient outcomes and medical services rendered by hospitals and physicians in various fields, not limited to surgery [21]. Specialized clinical departments such as stroke and coronary artery care units were established prior to the establishment of specialized treatment facilities for patients with cardiac arrest, and the effect of these facilities on prognosis improvement has been proven [22, 23].
The prognosis of the OHCA of non-cardiac origin is extremely poor and our interest is in the improvemnt of prognosis of OHCA of cardiac origin. Therefore, this study was limited to cardiogenic OHCA. In this study, we evaluated the impact of the volume of annual hospital admissions on the prognosis of patients with OHCA using a large cohort from a nationwide study.
Methods
Participants/data source
This study conducted a post-hoc analysis of patients included in the Japanese Association for Acute Medicine OHCA (JAAM-OHCA) registry. This database is a nationwide multihospital prospective registry of hospital data collected according to the Utstein template, and in-hospital data, including treatments, arterial blood gas levels, and outcomes [24].
Setting
All Japanese emergency medical services (EMS) personnel can perform CPR in accordance with the Japanese resuscitation guidelines, which are based on the statement of the International Liaison Committee on Resuscitation. EMS personnel are legally prohibited from terminating resuscitation at the scene, and all patients with OHCA are transported to the hospital unless death is certain. The destination is usually not altered due to the cause of cardiac arrest. EMS usually transport patients with OHCA to the nearest emergency hospital, which is under the purview of the local medical control transports some cases, patients with ROSC may be transferred to a hospital that can provide more advanced care. In this registry, patient information is recorded when the hospital that first admitted the patient is a participating research hospital, and information on the prognosis is provided to the research facility by the transferring hospital. This registry includes all patients with OHCA, irrespective of internal or external causes. We used the JAAM-OHCA registry data for patients admitted between June 2014 and September 2017. Eighty-six hospitals and 35,754 patients were registered during this period.
Patients
The following cases were excluded from the analysis in this study were patients: (a) aged < 17 years, (b) with unknown initial rhythm, (c) who experienced ROSC upon contact with the EMS, (d) with an unknown prognosis 30 days after cardiac arrest, (e) with extrinsic cardiac arrest, (f) with cardiac arrest due to other medical causes, and (g) who died in the emergency department.
Outcomes and definitions
The primary outcome in this study was the neurological outcome 30 days after cardiac arrest, and the secondary outcome was survival 30 days after cardiac arrest. Neurological outcomes were evaluated using the cerebral performance category (CPC) scale [25]. Patients with a score of CPC 1 or CPC 2 were designated as having a favorable neurological outcome. Patients’ prognosis 30 days after cardiac arrest was obtained from their current condition if they were still hospitalized, or from telephone or written survey responses from registered facilities if they had been transferred or discharged from the hospital.
Study design
This retrospective analysis was conducted using a prospective registry (JAAM-OHCA registry).
Statistical analysis
Hospitals were divided into three equal groups according to the number of patients with OHCA of cardiac origin (i.e., patient volume) received per year. This classification of groups was based on the number of patients admitted after OHCA of cardiac origin. In the present study, patient volume was equally divided by the number of hospitals, resulting in an unequal number of patients in each group. We selected the following potential patient-related factors that may affect the prognosis: sex, age, contact between doctor and patient before arrival at hospital, motor score on the Glasgow coma scale upon arrival at the emergency department (ED), defibrillation performed by EMS, use of airway devices by EMS, types of airway devices used by the EMS, primary electrocardiography rhythm at the scene, witness by bystander, CPR initiated by a bystander, defibrillation performed by a bystander, intravenous fluid administration by EMS, dosage of adrenaline administered until arrival at the ED, presence of ROSC prior to arrival at the hospital, presence of ROSC on arrival at the hospital, time from calling the EMS to arrival at the scene, time from arrival at the scene to arrival at the ED, and laboratory data on arrival at the ED (serum urea nitrogen, serum creatinine, serum total protein, serum albumin, pH, partial pressure of carbon dioxide, partial pressure of oxygen, HCO3, base excess, lactate, and glucose). These variables were used for multiple imputation and generalized estimating equations described later in this section.
We also investigated the following four subgroups: patient with ROSC prior to arrival at hospital, patient with ROSC prior to arrival at hospital, patients who were transported to critical-care medical centers, and patients who were transported to ECMO-capable hospitals. The same outcomes, potential patient factors, and hospital-volume categories were used as those for the main population (patients with OHCA).
We presented the patient and hospital characteristics of the three tertiles of hospital volume (low, middle and high). Continuous variables were presented as medians with interquartile ranges and categorical variables were presented as numbers and percentages. The Jonckheere-Terpstra test and Cochran-Armitage trend test were used for continuous and categorical variables, respectively. Chi-square test was used for categorical variables with multi-category. We employed multiple imputation by chained equations to address missing data assuming the missing mechanism as missing at random, and 100 imputed datasets were created. Missing potential patient-related factors were imputed and the numbers of missing data were shown in a table of characteristics of patients. We performed generalized estimating equations to account for the clustering of patients within each hospital and to examine the association between hospital volume and survival 30 days after cardiac arrest or rehabilitation 30 days after cardiac arrest, adjusting for the above-mentioned patient factors except for pH, partial pressure of carbon dioxide and HCO3 since these variables were highly correlated with base excess. We also assessed linear trend by performing a trend test using contrasts of coefficients obtained from generalized estimating equations. Odds ratios and 95% confidence intervals (CIs) were calculated. All analyses were performed using R version 3.6.3. All reported p-values were two-tailed, and differences with p-values (p) < 0.05 were considered statistically significant.
Results
Flow of patients enrollments
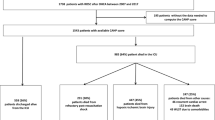
Adult patients with OHCA (n = 28,784) were retrieved from those enrolled in the JAAM-OHCA registry (n = 34,754). Patients under 17 years of age (n = 737), patients with missing data (n = 3816), and patients who had already attained ROSC at the time of EMS contact (n = 1417) were excluded. The current study also excluded patients with non-cardiac causes of OHCA (n = 13,601) and patients who died in the emergency room (n = 11,551), to ensure accurate assessment of the impact of the volume of annual hospital admissions on OHCA patients. Finally, the remaining 3632 patients with OHCA of cardiac origin were included in the analysis (Fig. 1).
Characteristics of hospitals and patients
Twenty-nine hospitals (250 patients) were categorized as low-volume, 28 hospitals (817 patients) were categorized as medium volume, and 29 hospitals (2565 patients) were categorized as high volume based on the number of patients admitted after OHCA of cardiac origin. The characteristics of the hospitals are presented in Table 1. The percentage of critical-care medical centers and number of doctors on the night/holiday shift were positively correlated with hospital volume (p < 0.001 and 0.018, respectively). Table 2 shows the characteristics of the patients included in the analysis based on hospital volume. Most characteristics related to the hospitals and patient transport did not differ significantly among the hospital-volume categories. However, the number of patients for whom physician care had been initiated prior to hospital arrival and the number of patients who required extracorporeal cardiopulmonary resuscitation (E-CPR) had higher percentages in high-volume hospital.
Primary outcome (neurological outcome 30 days after cardiac arrest)
Adjusted Odds ratio for favorable neurological outcomes 30 days after OHCA were presented in Fig. 2. In an analysis of the overall patients, there was no advantage of middle- and high-volume hospitals over low-volume hospitals (OR 0.989, 1.504, 95% CI 0.562-1.741, 0.919-2.463, respectively). A subgroup analysis focusing on patients transported to critical care medical centers also showed no advantage of middle- and high-volume hospitals over low-volume hospitals (OR 1.226, 1.562, 95% CI 0.649-2.316, 0.899-2.711, respectively). A subgroup analysis focused on patients transported to ECMO-capable hospitals showed the same results (OR 1.040, 1.574, 95% CI 0.565-1.913, 0.926-2.676, respectively). However, the frequency of favorable neurological outcomes in OHCA patients with ROSC before arrival at the emergency department at high-volume centers was higher than those at low-volume centers (OR 1.346, 95% CI 0.660-2.748). Conversely, the analysis for patients with OHCA who did not achieve ROSC before arrival at the ED showed no significant difference between neurological outcome and institutional volume (OR 0.800, 1.346, 95% CI 0.375-1.705, 0.660-2.748, respectively).
Adjusted odds ratio for favorable neurological outcomes 30 days after OHCA. Odds ratio of middle-volume hospitals and high-volume hospitals to low-volume hospital (reference) for favorable neurological outcomes 30 days after hospitalization. “n” in the figure indicates the number of patients. The number in “[]” represents the number of people who actually had a favorable neurological outcome. CI: confidence interval, ROSC: return of spontaneous circulation, ECMO: extracorporeal membrane oxygenation, OHCA: out-of-hospital cardiac arrest
Secondary outcome (survival 30 days after cardiac arrest)
The same analysis was performed with Outcome as 30 days survival after OHCA, but no significant results were found in all subgroups (Fig. 3). The characteristics of OHCA patients in each subgroup are shown in Additional files 1, 2, 3 and 4.
Adjusted odds ratio for 30-day survival after OHCA. Odds ratio of middle-volume hospitals and high-volume hospitals to low volume hospitals (reference) when the outcome is survival rate after 30 days of hospitalization. “n” in the figure indicates the number of patients. The number in “[]” represents the number of people who actually survived. CI: confidence interval, ROSC: return of spontaneous circulation, ECMO: extracorporeal membrane oxygenation, OHCA: out-of-hospital cardiac arrest
Discussion
This study retrospectively analyzed the effect of institutional volume on patient prognosis using data from 3632 adults hospitalized for OHCA of cardiac origin from more than 30,000 individuals registered with the nationwide OHCA registry. In particular, neurological outcomes tended to improve with increasing annual number of OHCA patients at the destination hospital, especially in OHCA patients who experienced ROSC prior to arrival at the ED.
For a long time, previous studies examining institutional volume and patient prognosis have failed to show consensus on various aspects of this association [10,11,12,13,14,15,16,17,18]. A recently published systematic review has shown that cardiac arrest centers may improve the prognosis of OHCA patients [18, 26], but it is inconclusive as to whether OHCA patients should be transported directly to a cardiac arrest center [27, 28].
The divergent conclusions in previous studies may be attributed to differences in the target patient populations: some studies that reported no association between hospital volume and patient prognosis included patients with OHCA of non-cardiac origin [15, 16]. In contrast, the cohort of studies that reported improvement in patient outcomes at high-volume hospitals was restricted to patients with OHCA of cardiac origin [12,13,14]. Patients whose transport time was 10 min or less [12] and those with a shockable rhythm [13] were reported to have a better prognosis. Therefore, previous studies suggested that patients who are likely to survive and have a favorable neurological outcome are more likely to benefit from hospital volume. In the present study, we found a significant improvement in the neurological outcome of hospital volume when limited to patients with ROSC before arrival at the ED (Fig. 2). This result is consistent with that of several previous studies.
Meanwhile, another large-scale study of patients with OHCA (whose sample size was comparable to the current study) reported that no correlation existed between hospital volume and prognosis [17]. There are several possible reasons for the lack of a significant correlation between the size of the hospital and patient prognosis. Hospital factors such as location (urban/rural), teaching status, and 24-h cardiac interventional services have been reported to be correlated with prognosis [11, 14]. Similar studies have reported that physical volume, and nurses and rehabilitation therapists affect patient prognosis [29,30,31,32,33], although these studies did not investigate patients with cardiac arrest.
In addition, E-CPR for out-of-hospital cardiac arrest has been reported to be effective and not, and is an area of discussion [34,35,36]. In this study, most facilities were able to provide E-CPR regardless of hospital volume, and the percentage of patients who actually received E-CPR ranged from 14.8 to 26.0%. The results of the subgroup analysis of this study did not demonstrate any benefits of transport to a hospital to be able to provide E-CPR.
Additionally, previous analysis suggested that the treatment effect of cardiac arrest centers may be significantly better for patients with shockable rhythm and without prehospital ROSC [26]. The results of this study indicate that patients with prehospital ROSC are more likely to benefit from high-volume hospitals, although there was no significant difference between institutional volume and patient outcomes in patients without prehospital ROSC. This result may be a rationale for transferring patients with prehospital ROSC to high-volume hospitals, and that patients without ROSC do not benefit from being transported to high volume hospitals. This contradicts the results of previous study [26], and the characteristics of patients who should be transferred to high-volume hospitals and cardiac arrest centers is a topic for future study.
Limitations
Although the sample size of this study was large, there was a bias in the number of patients in the groups, which was unavoidable owning to categorization, and may have affected the results. In this study, the number of patients included in the analysis was reduced from 34,754 to 3632, which has the effect of selection bias and survivor bias. This study was also limited to registry-participating hospitals, which resulted in a facility selection bias. This is because hospitals that participate in registries are more likely to be highly active. Moreover, there may be differences in the registration methods and omissions in registration depending on the hospital, which may affect the results. Limited information was available on the differences between hospitals and their respective characteristics. Hospitals characteristics besides the number of OHCA patients accepted may have affected the results, because we did not utilize factors related to hospitals as covariates in the generalized estimating equations.
The current study showed that the annual number of OHCA of cardiac origin patients admitted to a hospital may have a positive impact on favorable neurological prognosis, although other hospital characteristics were not considered. Further research is needed to identify the hospital characteristics with the optimal effect on OHCA patients.
Conclusions
The annual number of OHCA patients received by the hospital did not significantly affect the prognosis of adult OHCA patients in most cases, although it was beneficial in cardiac arrest patients who achieved ROSC before arrival at the hospital’s ED. Thus, transport to a high-volume hospital may improve prognosis.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to the large amount of data but are available from the corresponding author on reasonable request.
Abbreviations
- CI:
-
Confidence interval
- CPC:
-
Cerebral performance category
- CPR:
-
Cardiopulmonary resuscitation
- ECG:
-
Electrocardiogram
- E-CPR:
-
Extracorporeal cardiopulmonary resuscitation
- ECMO:
-
Extra corporeal membrane oxygenation
- ED:
-
Emergency department
- EMS:
-
Emergency medical services
- GCS:
-
Glasgow coma scale
- ICU:
-
Intensive care unit
- JAAM-OHCA:
-
Japanese Association for Acute Medicine out-of-hospital cardiac arrest
- OHCA:
-
Out-of-hospital cardiac arrest
- OR:
-
Odds ratio
- ROSC:
-
Return of spontaneous circulation
- VA-ECMO:
-
Veno-arterial extra corporeal membrane oxygenation
References
Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81(11):1479–87.
Mosier JM, Kelsey M, Raz Y, Gunnerson KJ, Meyer R, Hypes CD, et al. Extracorporeal membrane oxygenation (ECMO) for critically ill adults in the emergency department: history, current applications, and future directions. Crit Care. 2015;19:431.
Lemiale V, Dumas F, Mongardon N, Giovanetti O, Charpentier J, Chiche JD, et al. Intensive care unit mortality after cardiac arrest: the relative contribution of shock and brain injury in a large cohort. Intensive Care Med. 2013;39(11):1972–80.
Uray T, Sterz F, Weiser C, Schreiber W, Spiel A, Schober A, et al. Quality of post arrest care does not differ by time of day at a specialized resuscitation center. Medicine. 2015;94(14):e664.
Sunde K, Pytte M, Jacobsen D, Mangschau A, Jensen LP, Smedsrud C, et al. Implementation of a standardised treatment protocol for post resuscitation care after out-of-hospital cardiac arrest. Resuscitation. 2007;73(1):29–39.
Schober A, Holzer M, Hochrieser H, Posch M, Schmutz R, Metnitz P. Effect of intensive care after cardiac arrest on patient outcome: a database analysis. Crit Care. 2014;18(2):R84.
Shin SD, Suh GJ, Ahn KO, Song KJ. Cardiopulmonary resuscitation outcome of out-of-hospital cardiac arrest in low-volume versus high-volume emergency departments: an observational study and propensity score matching analysis. Resuscitation. 2011;82(1):32–9.
Semeraro F, Greif R, Böttiger BW, Burkart R, Cimpoesu D, Georgiou M, et al. European resuscitation council guidelines 2021: systems saving lives. Resuscitation. 2021;161:80–97.
Sinning C, Ahrens I, Cariou A, Beygui F, Lamhaut L, Halvorsen S, et al. The cardiac arrest centre for the treatment of sudden cardiac arrest due to presumed cardiac cause - aims, function and structure: Position paper of the Association for Acute CardioVascular Care of the European Society of Cardiology (AVCV), European Association of Percutaneous Coronary Interventions (EAPCI), European Heart Rhythm Association (EHRA), European Resuscitation Council (ERC), European Society for Emergency Medicine (EUSEM) and European Society of Intensive Care Medicine (ESICM). Eur Heart J Acute Cardiovasc Care. 2020;9(4_suppl):S193–s202.
Nguyen YL, Wallace DJ, Yordanov Y, Trinquart L, Blomkvist J, Angus DC, et al. The volume-outcome relationship in critical care: a systematic review and Meta-analysis. Chest. 2015;148(1):79–92.
Carr BG, Goyal M, Band RA, Gaieski DF, Abella BS, Merchant RM, et al. A national analysis of the relationship between hospital factors and post-cardiac arrest mortality. Intensive Care Med. 2009;35(3):505–11.
Cha WC, Lee SC, Shin SD, Song KJ, Sung AJ, Hwang SS. Regionalisation of out-of-hospital cardiac arrest care for patients without prehospital return of spontaneous circulation. Resuscitation. 2012;83(11):1338–42.
Spaite DW, Bobrow BJ, Stolz U, Berg RA, Sanders AB, Kern KB, et al. Statewide regionalization of postarrest care for out-of-hospital cardiac arrest: association with survival and neurologic outcome. Ann Emerg Med. 2014;64(5):496–506.e1.
Stub D, Smith K, Bray JE, Bernard S, Duffy SJ, Kaye DM. Hospital characteristics are associated with patient outcomes following out-of-hospital cardiac arrest. Heart. 2011;97(18):1489–94.
Kashiura M, Amagasa S, Moriya T, Sakurai A, Kitamura N, Tagami T, et al. Relationship between institutional volume of out-of-hospital cardiac arrest cases and 1-month neurologic outcomes: a post hoc analysis of a prospective observational study. J Emerg Med. 2020;59(2):227–37.
Callaway CW, Schmicker R, Kampmeyer M, Powell J, Rea TD, Daya MR, et al. Receiving hospital characteristics associated with survival after out-of-hospital cardiac arrest. Resuscitation. 2010;81(5):524–9.
Cudnik MT, Sasson C, Rea TD, Sayre MR, Zhang J, Bobrow BJ, et al. Increasing hospital volume is not associated with improved survival in out of hospital cardiac arrest of cardiac etiology. Resuscitation. 2012;83(7):862–8.
Yeung J, Matsuyama T, Bray J, Reynolds J, Skrifvars MB. Does care at a cardiac arrest Centre improve outcome after out-of-hospital cardiac arrest? - a systematic review. Resuscitation. 2019;137:102–15.
Luft HS. The relation between surgical volume and mortality: an exploration of causal factors and alternative models. Med Care. 1980;18(9):940–59.
Luft HS, Bunker JP, Enthoven AC. Should operations be regionalized? The empirical relation between surgical volume and mortality. 1979. Clin Orthop Relat Res. 2007;457:3–9.
Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med. 2002;137(6):511–20.
Langhorne P, Ramachandra S. Organised inpatient (stroke unit) care for stroke: network meta-analysis. Cochrane Database Syst Rev. 2020;4(4):Cd000197.
Killip T 3rd, Kimball JT. Treatment of myocardial infarction in a coronary care unit. A two year experience with 250 patients. Am J Cardiol. 1967;20(4):457–64.
Kitamura T, Iwami T, Atsumi T, Endo T, Kanna T, Kuroda Y, et al. The profile of Japanese Association for Acute Medicine - out-of-hospital cardiac arrest registry in 2014-2015. Acute Med Surg. 2018;5(3):249–58.
Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2(7872):81–4.
Yeo JW, Ng ZHC, Goh AXC, Gao JF, Liu N, Lam SWS, et al. Impact of cardiac arrest centers on the survival of patients with nontraumatic out-of-hospital cardiac arrest: a systematic review and Meta-analysis. J Am Heart Assoc. 2022;11(1):e023806.
Tagami T, Hirata K, Takeshige T, Matsui J, Takinami M, Satake M, et al. Implementation of the fifth link of the chain of survival concept for out-of-hospital cardiac arrest. Circulation. 2012;126(5):589–97.
Kang MJ, Lee TR, Shin TG, Sim MS, Jo IJ, Song KJ, et al. Survival and neurologic outcomes of out-of-hospital cardiac arrest patients who were transferred after return of spontaneous circulation for integrated post-cardiac arrest syndrome care: the another feasibility of the cardiac arrest center. J Korean Med Sci. 2014;29(9):1301–7.
Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349(22):2117–27.
Srinivas VS, Hailpern SM, Koss E, Monrad ES, Alderman MH. Effect of physician volume on the relationship between hospital volume and mortality during primary angioplasty. J Am Coll Cardiol. 2009;53(7):574–9.
Drummond AE, Pearson B, Lincoln NB, Berman P. Ten year follow-up of a randomised controlled trial of care in a stroke rehabilitation unit. BMJ. 2005;331(7515):491–2.
Kalra L, Eade J. Role of stroke rehabilitation units in managing severe disability after stroke. Stroke. 1995;26(11):2031–4.
Indredavik B, Bakke F, Slordahl SA, Rokseth R, Hâheim LL. Stroke unit treatment. 10-year follow-up. Stroke. 1999;30(8):1524–7.
Scquizzato T, Bonaccorso A, Consonni M, Scandroglio AM, Swol J, Landoni G, et al. Extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest: a systematic review and meta-analysis of randomized and propensity score-matched studies. Artif Organs. 2022;46(5):755–62.
Yannopoulos D, Bartos J, Raveendran G, Walser E, Connett J, Murray TA, et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single Centre, open-label, randomised controlled trial. Lancet. 2020;396(10265):1807–16.
Belohlavek J, Smalcova J, Rob D, Franek O, Smid O, Pokorna M, et al. Effect of intra-arrest transport, extracorporeal cardiopulmonary resuscitation, and immediate invasive assessment and treatment on functional neurologic outcome in refractory out-of-hospital cardiac arrest: a randomized clinical trial. JAMA. 2022;327(8):737–47.
Acknowledgements
We would like to thank Editage (https://online.editage.jp/) for English language editing.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
TT and MH contributed to study conception and manuscript preparation. KO and KM contributed to analysis of the data. MH contributed to manuscript preparation and revision for intellectual content. All authors read and approved the final manuscript version prior to submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The registry for this study was an epidemiological study with no treatment intervention, and informed consent was waived by The Ethics Committees of Hokkaido University. The experimental protocols were approved by The respective Ethics Committees of Kyoto University and Hokkaido University (approval number: 0130060). All experiments were performed in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplemental Table 1.
Characteristics of patients with OHCA who achieved ROSC before arrival at the ED.
Additional file 2: Supplemental Table 2.
Characteristics of patients with OHCA who were transported to a critical-care medical center.
Additional file 3: Supplemental Table 3.
Characteristics of patients with OHCA transported to ECMO-capable hospitals.
Additional file 4: Supplemental Table 4.
Characteristics of patients with OHCA who did not achieve ROSC before arrival at the ED.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tsuchida, T., Ono, K., Maekawa, K. et al. Effect of annual hospital admissions of out-of-hospital cardiac arrest patients on prognosis following cardiac arrest. BMC Emerg Med 22, 121 (2022). https://doi.org/10.1186/s12873-022-00685-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12873-022-00685-7