Abstract
Background
The prognostic performance of soluble CD40L (sCD40L) for illness severity in infectious diseases is rarely reported. We investigated the ability of sCD40L combined with Acute Physiology and Chronic Health Evaluation II (APACHE II) score to evaluate mortality in septic patients in the emergency department(ED).
Methods
We enrolled 222 septic patients in the ED of Beijing Chao-Yang Hospital from October 2020 to April 2021. Their serum sCD40L, PCT, lactate (Lac), Sequential Organ Failure Assessment (SOFA) score, Acute Physiology and Chronic Health Evaluation II (APACHE II) score were used to predict the prognosis of septic patients in terms of 28-day mortality. Serum sCD40L was detected by Human XL Cytokine Luminex. Logistic regression analysis and receiver operating characteristic (ROC) curves were used to assess the prognostic value of the variables.
Results
One hundred ninety-five patients met the inclusion criteria, divided into survival group (55 cases) and non-survival group (140 cases). sCD40L, PCT, Lac, SOFA and APACHE II score were found to independently predict 28-day mortality (P < 0.05). The AUC values of sCD40L, PCT, Lac, SOFA and APACHE II score were 0.662,0.727,0.704, 0.719 and 0.716, respectively. There was no difference in the diagnostic value of sCD40L compared with the PCT, Lac, SOFA score or APACHE II score (Z1 = 1.19, P = 0.234; Z2 = 0.77, P = 0.441; Z3 = 1.05, P = 0.294; Z4 = 0.97, P = 0.332). However, the combined evaluation of sCD40L + APACHE II (AUC:0.772, Z = 2.10, P = 0.036) was much better than sCD40L alone in predicting 28-day mortality.
Conclusion
The predictive value of sCD40L + APACHE II is better than sCD40L alone for 28-day mortality. sCD40L combined with APACHE II score is valuable for predicting 28-day mortality in elderly patients with sepsis.
Similar content being viewed by others
Background
Sepsis is an organ dysfunction syndrome caused by the body’s dysfunctional response to infection, mainly manifested as chills, fever (or hypothermia), palpitation, shortness of breath, mental state changes and other symptoms [1]. Septic patients are often critically ill and their condition seems to progress quickly, leaving little time for doctors to react, and that’s why early and prompt recognition and reasonable treatment can significantly reduce mortality [2]. With the rapid development of severe infection medical practices, many existing biomarkers can no longer meet the current clinical needs, such as the peak CRP levels, according to the latest research, did not independently predict mortality in patients with bacteremia in the ED [3] and new and more predictors need to be explored.
CD40L(CD154), a 39-kD transmembrane glycoprotein associated with tumor necrosis factor-α (TNF-α), was originally identified on stimulated CD4-positive T cells, mast cells, and basophils [4, 5]. CD40L has a variety of pro-inflammatory and pro-coagulant effects, including inflammation caused by interleukin-1, TNF-α, and tissue factors, as well as upregulation of endothelial cell adhesion molecules [6]. CD40L stimulates resting platelet activity by binding constitutionally expressed CD40 during cell contact [7]. When platelets are activated, they quickly carry CD40L to the cell surface [6]. Activated platelets release a large number of inflammatory mediators [8,9,10]. After activation and expression on the cell membrane surface, platelets release CD40L in a solute form (sCD40L) [11]. sCD40L as a platelet agonist is related to α II b β 3 ligand properties [12]. Platelet-derived sCD40L is involved in stimulating neutrophil activation and Mac-1(macrophage-1) expression, as well as promoting neutrophil lung infiltration and sepsis associated lung injury [13]. A few studies have found that the relationship between sCD40L and sepsis, and proved that the elevated serum sCD40L was associated with poor prognosis [14,15,16,17].
Hence, our study focuses on confirming whether sCD40L combined with APACHE II score can positively impact the mechanisms of prediction and have a satisfactory effect on the prognosis of patients with sepsis.
Methods
Patients and grouping
The study was a single-center observational study conducted in the emergency department of Beijing Chao-Yang Hospital. From October 2020 to April 2021, 222 consecutive septic patients according to Sepsis-3 (SOFA score ≥ 2) [18] were enrolled in our cohort. The exclusion criteria were as follows: age younger than 18 years, end-stage disease (malignant tumor with metastases, AIDS, end-stage kidney or liver disease), as well as patients who refused to participate in the study or who had some missing or incomplete data.
Data collection
Blood samples were taken on emergency admission. White blood cell count, blood biochemistry, blood gas and serum sCD40L levels were detected within 24 hours after admission. PCT, CRP, Lac, ALB(albumin), AST (aspartate aminotransferase), ALT (alanine transaminase) and Scr (serum creatinine) were tested in the lab. PCT was determined by Bio merieux Mini VIDAS immunoassay. Serum sCD40L concentration was detected by using Human XL Cytokine Luminex® Performance Assay 46-plex Fixed Panel (LKTM014B, R&D). The reference range of the level of sCD40L for predicting 28-day mortality is about 1.37 ng/ml to 6.07 ng/ml [13]. Each sample was measured in duplicate. The SOFA and APACHE II scores were calculated when patients arrived at the emergency department. All patients with sepsis were followed up for 28 days. The 28-day mortality was the end point of the study.
Statistical analysis
All data were analyzed using SPSS version 24.0 (SPSS Inc., Chicago, IL, USA). Data were expressed as mean ± standard deviation or median, and for normally distributed continuous variables, an independent sample T-test was used for comparison. The Mann-Whitney U test was used to compare the two groups of distributed data. The frequency was compared by Chi-square test. Multiple logistic regression analysis was used to determine the independent outcome predictors. Receiver operating characteristic (ROC) curves and the area under the curves (AUC) were conducted to compare the predictive value. The Kaplan-Meier curve was used to describe the cumulative survival rate. All statistical tests were 2-tailed, and P < 0.05 was considered statistically significant [19]. The combination of variables was realized through the ROC curve of SPSS software, which was a commonly used statistical method for sepsis research. The following logistic regression equation was developed based on the β-coefficient of the sCD40L and other variables: L = sCD40L + β1/β2*variable, which L is the combination value of sCD40L and other variables [20].
Results
Basic information and characteristics of the cohort
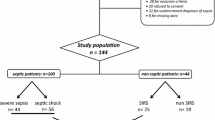
From October 2020 to April 2021, 222 patients with sepsis were screened consecutively. We excluded 27 patients declined to participate or with data missing or incomplete, and thus included 195 participants divided into survival group (55 cases) and non-survival group (140 cases), completed the 28-day follow-up (Fig. 1).
The median age of survival group was higher than non-survival group (71 vs 70, P < 0.05). The Median level of Lac, CRP, SOFA score, APACHE II score and sCD40L were much higher in non-survival group than in survival group(P < 0.05). The gender, COPD (chronic obstructive pulmonary disease), hypertension, DM (diabetes mellitus), CVD (cerebrovascular disease), CHF (congestive heart failure), WBC, AST and ALT were not different between survival group and non-survival group (Table 1).
The median of the sCD40L, Lac, PCT, CRP, SOFA and APACHE II scores are shown in Fig. 2. There were significant differences in the average levels of sCD40L, Lac, CRP and PCT, as well as SOFA or APACHE II score between survival and non-survival patients(P < 0.05).
Spearman’s correlations of sCD40L with other indicators
To investigate the correlations between sCD40L and WBC, PLT, AST, ALT, Lac, CRP, PCT, SOFA score and APACHE II score, Spearman’s correlation analysis was conducted (Table 2). Figure 3A, B showed the positive liner correlations of sCD40L with PCT (r = 0.183, P < 0.05) and sCD40L with APACHE II score (r = 0.148, P < 0.05).
Logistic regression analysis of the predictive value of septic patients
We used the multivariate logistic regression to analyze independent predictors for this study. The results presented that sCD40L, Lac, PCT, SOFA and APACHE II score were the independent predictors of 28-day mortality, but neither WBC nor CRP (Table 3).
The following logistic regression equation was developed based on the β-coefficient of the sCD40L,SOFA,APACHE II, Lac and PCT:
Which L is the combination value of sCD40L and other variables [20].
Predictive value of clinical prognosis in patients with sepsis
The ROC curves of sCD40L and the combination of all variables to predict the 28-day mortality of patients (Fig. 4A, B and Table 4). The AUCs of the sCD40L, Lac, PCT, SOFA and APACHE II scores for 28-day mortality were 0.662, 0.727, 0.704, 0.719 and 0.716, respectively. The combination values of variables for predicting 28-day mortality were as follows: sCD40L + SOFA: 0.775; sCD40L + APACHE II: 0.772; sCD40L + Lac: 0.762; sCD40L + PCT: 0.778. Statistically, there was no difference in the diagnostic value of sCD40L compared with the PCT, Lac, SOFA score or APACHE II score (Z1 = 1.19, P = 0.234; Z2 = 0.77, P = 0.441; Z3 = 1.05, P = 0.294; Z4 = 0.97, P = 0.332). However, sCD40L + APACHE II score (AUC:0.772, Z = 2.10, P = 0.036) was much better than sCD40L alone in predicting 28-day mortality.
The cumulative 28-day mortality of sepsis
The cumulative 28-day survival was lower in septic patients with sCD40L > 3060.31 pg/ml, Lac> 1.9 mmol/L, PCT > 0.12 ng/ml, SOFA score > 7.5 and APACHE II score > 18.5, respectively (Fig. 5). When comparing the combined diagnostic value of sCD40L with other factors, sCD40L + SOFA> 5242.81, sCD40L + APACHE II > 1469.31, sCD40L + Lac> 4416.91, sCD40L + PCT > 3091.99 showed a higher mortality rate (Fig. 6).
Discussion
The main finding of this study was that the predictive value of sCD40L + APACHE II score was better than sCD40L alone for 28-day mortality. sCD40L combined with APACHE II score had a higher predictive value for 28-day mortality in elderly patients with sepsis.
Our study found that serum sCD40L levels in the non-survival group were higher than those in the survival group, in agreement with previous studies [14,15,16,17]. Furthermore, serum sCD40L levels>3060.31 pg/ml were found associated with higher 28-day mortality by multiple logistic regression.
We considered age, temperature, respiratory rate, Lac, ALB, PCT, CRP, sCD40L, APACHE II score, and SOFA score as risk factors associated with mortality. Our outcomes showed that other factors, such as chronic diseases, WBC, Scr, AST, and ALT were not statistically different between survival and non-survival groups. We also found that some septic diagnosis variables were associated with 28-day mortality, such as sCD40L, Lac, PCT, APACHE II score and SOFA score.
It is likely that the pro-inflammatory and pro-thrombotic effects of serum sCD40L could increase the risk of death in patients with sepsis [21]. Platelet-derived mediators may be involved in the process of granulomatous chronic inflammation [22]. Activated platelets release a large number of inflammatory mediators [8,9,10]. Platelets are activated in damaged tissues, and certain foreign substances enter the body to activate platelets [23]. In the tumor necrosis factor superfamily, CD40L is involved in the occurrence of chronic inflammation associated with granuloma. CD40L-CD40, is involved in a variety of immunomodulatory and inflammation-related responses [24, 25]. CD40 induces macrophages to express cytokines, tissue factors, and matrix metalloproteinases (MMPs) [26,27,28]. CD40-CD40L interactions stimulates vascular endothelial cells and macrophages to induce adhesion and molecules [29, 30], generation of tissue factor(TF) [31, 32] and release of pro-inflammatory cytokines [33, 34], which participate in inflammatory response and thrombosis formation. CD40L could up-regulate TF and thrombomodulin [35, 36], as well as E-selection and vascular cell adhesion molecule-1(VCAM-1)independently of TNF-α or IL-1β. CD40L, which is shed from platelets or expressed on their surfaces, can activate endothelial cells(ECs), causing their activity to change to promote inflammation or thrombosis. After the expression of platelet cell membrane, CD40L is cleaved by specific enzymes into the sCD40L and released into the blood to function. sCD40L is mediated by GPIIb/IIIa, a surface glycoprotein that binds fibrinogen, and by MMPs [37]. All above effects can promote inflammation, endothelial thrombosis, organ dysfunction and even death.
Our study did not confirm any associations between serum sCD40L levels and platelet counts, although approximately 95% of sCD40L was derived from platelets [37], which was different from previous results presented by other scholars [14]. Traditionally, in most of the infections, platelet counts are often reduced, a phenomenon easily identifiable in patients with sepsis. Differently, sCD40L levels were considerably elevated in patients with sepsis, which can be considered a contradictory outcome. Although our study did not confirm the existence of a positive correlation between sCD40L levels and platelet count, our results are still of great significance and the shortcomings might be related to our insufficient sample size or lack of focus on plasma sCD40L. Our study was limited to serum sCD40L due to the previous reports that confirmed the levels of sCD40L in serum was significantly higher than that in plasma [38]. In a future follow-up study, we would like to expand the clinical sample size and continue to deepen the research on this topic.
We also found that sCD40L levels were positively associated with criteria of sepsis severity, such as APACHE II scores and PCT. In clinical diagnosis and treatment, the APACHE II score and PCT are commonly used to evaluate the severity of the disease. The higher the APACHE II score, the more critical the condition is, and the worse the prognosis, which is likely to imply higher risks of death. Similarly, the higher the PCT, the more severe the bacterial infection, which worsens the risk of developing severe disease and the overall clinical prognosis. Our results showed that sCD40L levels were significantly higher in the non-survival group than in the survival group and independently predicted 28-day mortality in septic patients. These outcomes are in good agreement with the results presented by Leonardo et al. [14]. In critical disease evaluation, sCD40L, PCT, and APACHE II score all have high predictive value. As a new biomarker, sCD40L, combined with PCT or APACHE II score has a greater predictive value and is of solid significance in critical disease evaluation.
Several limitations of our study were as follows: First, our study was a single-center study with a small sample size, requiring more centers and a larger number of samples to join the cohort; Second, this research only measured sCD40L levels in serum and not in plasma samples, and further study should be paid more attention to sCD40L levels both in serum and plasmas samples; Third, we determined sCD40L levels only 24 hours after admission, not one week or more, this might influence the results of the study, and further stratified studies on sample collection time would be carried out. Fourth, much more severe scores such as Mortality in Emergency Department Sepsis (MEDS) score and Predisposition, Infection, Response, and Organ dysfunction (PIRO) score should be added to our study to evaluate the severity of sepsis. There were also some positive aspects of our study, which was significant because it was the first time that sCD40L and APACHE II score had been successfully combined to assess the severity and clinical prognosis of septic patients. Meanwhile, the predictive value of sCD40L in sepsis was further proved.
Conclusion
This study suggests that the predictive value of sCD40L + APACHE II score is better than sCD40L alone for 28-day mortality. sCD40L combined with APACHE II score has a higher predictive value for 28-day mortality in elderly patients with sepsis.
Availability of data and materials
All data generated or analyzed in this study are included in this paper.
Abbreviations
- sCD40L:
-
soluble CD40L
- WBC:
-
white blood cell
- PCT:
-
procalcitonin
- Lac:
-
lactate
- CRP:
-
C-reactive protein
- ALB:
-
albumin
- Scr:
-
serum creatinine
- AST:
-
aspartate aminotransferase
- ALT:
-
alanine transaminase
- PLT:
-
platelet
- MAP:
-
mean arterial pressure
- RR:
-
respiratory rate
- HR:
-
heart rate
- TNF-α :
-
tumor necrosis factor-α
- Mac-1:
-
macrophages-1
- MMP:
-
matrix metalloproteinase
- ECs:
-
endothelial cells
- TF:
-
tissue factor
- VCAM-1:
-
adhesion molecule-1
- SOFA:
-
Sequential Organ Failure Assessment
- APACHE II:
-
Acute Physiology and Chronic Health Evaluation II
- MEDS:
-
Mortality in emergency department sepsis
- PIRO:
-
Predisposition, Infection, Response, and Organ dysfunction
- COPD:
-
chronic obstructive pulmonary disease
- CVD:
-
cerebrovascular disease
- CHF:
-
congestive heart failure
- DM:
-
diabetes mellitus
References
Girard TD, Ely EW. Bacteremia and sepsis in older adults. Clin Geriatr Med. 2007;23:633.
Kethireddy S, Bilgili B, Sees A, et al. Culture-negative septic shock compared with culture-positive septic shock: a retrospective cohort study. Crit Care Med. 2018;46:506.
Kurisu K, Yoshiuchi K, Ogino K, Okada Y, Oda T. Peak C-reactive protein levels do not predict 30-day mortality for bacteremia: a retrospective cohort study. J Infect Chemother. 2020;26:23.
Graf D, Korthäuer U, Mages HW, Senger G, Kroczek RA. Cloning of TRAP, a ligand for CD40 on human T cells. Eur J Immunol. 1992;22:3191.
Armitage RJ, Fanslow WC, Strockbine L, et al. Molecular and biological characterization of a murine ligand for CD40. Nature. 1992;357:80.
Henn V, Slupsky JR, Gräfe M, et al. CD40 ligand on activated platelets triggers an inflammatory reaction of endothelial cells. Nature. 1998;391:591.
Inwald DP, McDowall A, Peters MJ, Callard RE, Klein NJ. CD40 is constitutively expressed on platelets and provides a novel mechanism for platelet activation. Circ Res. 2003;92:1041.
Dewitte A, Tanga A, Villeneuve J, et al. New frontiers for platelet CD154. Exp Hematol Oncol. 2015;4:6.
Nurden AT, Nurden P, Sanchez M, Andia I, Anitua E. Platelets and wound healing. Front Biosci. 2008;13:3532.
Vieira-de-Abreu A, Campbell RA, Weyrich AS, Zimmerman GA. Platelets: versatile effector cells in hemostasis, inflammation, and the immune continuum. Semin Immunopathol. 2012;34:5.
Henn V, Steinbach S, Büchner K, Presek P, Kroczek RA. The inflammatory action of CD40 ligand (CD154) expressed on activated human platelets is temporally limited by coexpressed CD40. Blood. 2001;98:1047.
André P, Prasad KSS, Denis CV, et al. CD40L stabilizes arterial thrombi by a beta3 integrin--dependent mechanism. Nat Med. 2002;8:247.
Rahman M, Zhang S, Chew M, Ersson A, Jeppsson B, Thorlacius H. Platelet-derived CD40L (CD154) mediates neutrophil upregulation of mac-1 and recruitment in septic lung injury. Ann Surg. 2009;250:783.
Lorente L, Martín MM, Varo N, et al. Association between serum soluble CD40 ligand levels and mortality in patients with severe sepsis. Critic Care. 2011;15:R97.
Lorente L, Martín MM, Pérez-Cejas A, et al. Non-survivor septic patients have persistently higher serum sCD40L levels than survivors. J Crit Care. 2017;41:177.
Liang Y, Zhu C, Sun Y, et al. Persistently higher serum sCD40L levels are associated with outcome in septic patients. BMC Anesthesiol. 2021;21:26.
Chew M, Rahman M, Ihrman L, Erson A, Zhang S, Thorlacius H. Soluble CD40L (CD154) is increased in patients with shock. Inflam Res. 2010;59:979.
Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for Sepsis and septic shock (Sepsis-3). JAMA. 2016;315:801.
Yang L, Lin Y, Zhang X, Wei B, Wang J, Liu B. Predictive value of combination of Procalcitonin and predisposition, infection, response, and organ dysfunction (PIRO) system in septic patients with positive blood cultures in the emergency department. Infect Drug Resist. 2022;15:6189.
Sun W, Luo Z, Cao Z, Wang J, Zhang L, Ma Y. A combination of the APACHE II score, neutrophil/lymphocyte ratio, and expired tidal volume could predict non-invasive ventilation failure in pneumonia-induced mild to moderate acute respiratory distress syndrome patients. Ann Transl Med. 2022;10:407.
Semple JW, Freedman J. Platelets and innate immunity. Cell Mol Life Sci. 2010;67:499.
Tang L, Eaton JW. Natural responses to unnatural materials: A molecular mechanism for foreign body reactions. Mol Med. 1999;5:351.
van Kooten C, Banchereau J. CD40-CD40 ligand. J Leukoc Biol. 2000;67:2.
Schönbeck U, Libby P. The CD40/CD154 receptor/ligand dyad. Cell Mol Life Sci. 2001;58:4.
Malik N, Greenfield BW, Wahl AF, Kiener PA. Activation of human monocytes through CD40 induces matrix metalloproteinases. J Immunol. 1950;1996(156):3952.
Suttles J, Stout RD. Macrophage CD40 signaling: a pivotal regulator of disease protection and pathogenesis. Semin Immunol. 2009;21:257.
Stout RD, Suttles J. The many roles of CD40 in cell-mediated inflammatory responses. Immunol Today. 1996;17:487.
Yellin MJ, Brett J, Baum D, et al. Functional interactions of T cells with endothelial cells: the role of CD40L-CD40-mediated signals. J Exp Med. 1995;182:1857.
Kiener PA, Moran-Davis P, Rankin BM, Wahl AF, Aruffo A, Hollenbaugh D. Stimulation of CD40 with purified soluble gp39 induces proinflammatory responses in human monocytes. J Immunol. 1995;155:4917.
Slupsky JR, Kalbas M, Willuweit A, Henn V, Kroczek RA, Müller-Berghaus G. Activated platelets induce tissue factor expression on human umbilical vein endothelial cells by ligation of CD40. Thromb Haemost. 1998;80:1008.
Mach F, Schönbeck U, Bonnefoy JY, Pober JS, Libby P. Activation of monocyte/macrophage functions related to acute atheroma complication by ligation of CD40: induction of collagenase, stromelysin, and tissue factor. Circulation. 1997;96:396.
Karmann K, Hughes CC, Schechner J, Fanslow WC, Pober JS. CD40 on human endothelial cells: inducibility by cytokines and functional regulation of adhesion molecule expression. Proc Natl Acad Sci U S A. 1995;92:4342.
Thienel U, Loike J, Yellin MJ. CD154 (CD40L) induces human endothelial cell chemokine production and migration of leukocyte subsets. Cell Immunol. 1999;198:87.
Miller DL, Yaron R, Yellin MJ. CD40L-CD40 interactions regulate endothelial cell surface tissue factor and thrombomodulin expression. J Leukoc Biol. 1998;63:373.
Zhou L, Stordeur P, de Lavareille A, et al. CD40 engagement on endothelial cells promotes tissue factor-dependent procoagulant activity. Thromb Haemost. 1998;79:1025.
Furman MI, Krueger LA, Linden MD, Barnard MR, Frelinger AL, Michelson AD. Release of soluble CD40L from platelets is regulated by glycoprotein IIb/IIIa and actin polymerization. J Am Coll Cardiol. 2004;43:2319.
André P, Nannizzi-Alaimo L, Prasad SK, Phillips DR. Platelet-derived CD40L: the switch-hitting player of cardiovascular disease. Circulation. 2002;106:896.
Weber M, Rabenau B, Stanisch M, et al. Influence of sample type and storage conditions on soluble CD40 ligand assessment. Clin Chem. 2006;52:888.
Acknowledgments
We thank all participants for their cooperation and help.
Funding
This research did not receive any funding from any institution.
Author information
Authors and Affiliations
Contributions
JYW and BW wrote the research protocol. JY, XQZ and XHY helped conduct the study and performed data collection. LY performed the statistical analysis and drafted the manuscript. YGL and BW revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participant
The study was approved by Beijing Chao-Yang Hospital Ethics Committee (No.2021-KE-636). All participants signed written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, L., Yang, J., Zhang, X. et al. Predictive value of soluble CD40L combined with APACHE II score in elderly patients with sepsis in the emergency department. BMC Anesthesiol 24, 32 (2024). https://doi.org/10.1186/s12871-023-02381-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-023-02381-w