Abstract
Background
Trends in non-invasive measurements of blood hemoglobin (Hb) may be useful for identifying the need for transfusion in the perioperative period.
Methods
Crystalloid fluid (5–20 mL/kg) was administered intravenously or by mouth to 30 volunteers and 33 surgical patients in five non-randomized clinical studies where Hb was measured on 915 occasions by non-invasive (Radical-7™) and invasive methodology. The hemodilution curves were compared by volume kinetic analysis and linear regression, with the slope and scattering of the data as key outcome measures.
Results
The slope was 1.0, indicating unity between the two modes of measuring Hb when crystalloid fluid was infused in volunteers; however, only 40–45% of the variability in the non-invasive Hb could be explained by the invasive Hb. Patients undergoing major surgery, who showed the most pronounced hemodilution (median 24 g/L); non-invasive Hb explained 72% of the variability but indicated only half the magnitude of the invasive Hb changes (slope 0.48, P < 0.001 versus the volunteers). Simulations based on volume kinetic parameters from the volunteers showed 25% less plasma volume expansion after infusion when based on non-invasive as compared to invasive Hb, while no difference was found during infusion.
Conclusions
In volunteers the non-invasive Hb had good accuracy (low bias) but poor precision. In surgical patients the non-invasive Hb had good precision but systematically underestimated the hemodilution. Despite severe limitations, the non-invasive technology can be used to follow Hb trends during surgery if supported by occasional invasive measurements to assure acceptable quality of the hemodilution curve.
Trial registrations
ControlledTrials.gov NCT01195025, NCT01062776, NCT01458678, NCT03848507, and NCT01360333 on September 3, 2010, February 4, 2010, October 25, 2011, February 20, 2019, and May 25, 2011, respectively.
Similar content being viewed by others
Background
The measurement of the blood hemoglobin (Hb) concentration is a guide that determines when transfusion of erythrocytes should be initiated. Sporadic measurement of Hb is often performed during major surgery to evaluate when the Hb value corresponding to the “transfusion trigger” is reached. Continuous measurement of Hb would therefore be of substantial value to refine these decisions. For this purpose, non-invasive Hb analysis has been commercially available for about a decade in the form of the multi-wavelength pulse oximeter Radical-7™ from Masimo Inc.
Many studies have performed point-wise comparisons between non-invasive and invasive Hb [1,2,3,4,5,6,7,8,9,10,11,12,13], and the main problem with the non-invasive technology is its poor precision. Several studies show good accuracy but 95% limits of agreement with a range of 40 g/L or more [3,4,5,6,7,8,9], which makes non-invasive Hb measurements difficult to rely on.
A more essential clinical question is whether the changes in Hb agree over time in an individual patient. If this is the case, the pulse oximeter could be calibrated with the known invasive Hb when surgery starts and then be used to indicate relative changes. To study this possibility, we reviewed the linearity between changes in Hb level as given by non-invasive and invasive Hb monitoring, using data from five cohorts where the Hb level had shifted due to fluid therapy and/or hemorrhage.
The aim of the present report was to determine the reliability of the non-invasive Hb for tracking changes in invasive Hb. Our hypothesis was that the non-invasive alternative is a useful index of Hb changes. This issue was studied by direct comparisons of Hb trends and also by assessing kinetic analyses of plasma volume shifts based on either mode of Hb measurement.
Methods
Data from five case non-randomized clinical trials where the Hb concentration was altered by intravenous or oral administration of crystalloid fluid with and without hemorrhage was reviewed. All studies were approved by the appropriate local Ethics committee and were registered at ClinicalTrials.gov before any patient was recruited. This report adheres to the CONSORT guidelines.
Procedures
The five series comprised only euhydrated subjects.
-
Study 1 included the infusions of 25 mL kg− 1 of Ringer’s solution given 10 healthy male volunteers [11].
-
Study 2 evaluated the ability of volume kinetics to detect deliberately induced dehydration; here, only the 10 control infusions of 10 mL kg− 1 of Ringer’s were used [12].
-
Study 3 used repeated Hb sampling during a short infusion of 5 mL kg− 1 of Ringer’s in the morning before surgery; the cohort originally included 30 patients, but only 10 of them were randomly selected for inclusion in the present study to maintain balance between volunteers and surgical patients [13].
-
Study 4 included 23 patients who underwent open radical cystectomy and urinary diversion under general anesthesia combined with thoracic epidural analgesia. Baseline fluid maintenance of 1 mL kg− 1 h− 1 of Ringer’s until the end of the removal of the bladder and thereafter increased to 3 mL kg− 1 h− 1 of Ringer’s until the end of surgery. A fixed dose of 20% albumin solution (3 mL kg− 1; Albumin CSL 20%, CSL Behring, Bern, Switzerland) was given over 30 min until removal of the bladder (expected blood loss of > 500 mL) was started. Blood loss was replaced with the Ringer solution in a 1:1 ratio. A supportive administration of norepinephrine, starting at a rate of starting at 30 ng kg− 1 min− 1 (to maintain the mean arterial blood pressure at > 65 mmHg) and mini fluid challenges of 100 mL of Ringer’s (to maintain the hemodynamics pulse pressure variation > 10), until normovolemia was restored [14]. One unit of erythrocytes was transfused, but this was administered after data collection had been completed.
-
Study 5 comprised healthy volunteers who ingested 500 mL of isotonic saline by mouth [15].
Table 1 shows the details and characteristics of the five cohorts, which have been published with other study questions. Precise inclusion and exclusion criteria were given for the respective studies [11,12,13,14,15], but subjects with clinically apparent hemodynamic, hepatic, renal, or pulmonary impairment were not included in any of them.
Repeated non-invasive measurements of Hb and the perfusion index in the hand were obtained from a pulse oximeter (Radical 7, Masimo Corp., Irvine, CA). At the same points in time, a blood sample was obtained for later measurement of the Hb concentration at the hospital’s official chemical laboratory with a coefficient of variation of approximately 1.0%. Blood gas machines were not used.
Linear relationships
Linear relationships were evaluated by comparing non-invasive and invasive Hb on a regression plot. The scatter was used as the measure of precision and expressed as the coefficient of determination (r2) of the regression line. The coefficient of determination is the fraction of the variability of y (non-invasive Hb) that can be explained by x (invasive Hb). A high r2 is desirable, as it implies that data scattering around the regression line is small.
Whether the non-invasive decreases as much as the invasive Hb during hemodilution is a different issue. We use the slope, i.e. the steepness, of the regression line between these two variables to express the accuracy of a series of non-invasive measurements in the same subject. A slope lower than 1.0 means that the numerical change in non-invasive Hb is less than that for the invasive Hb. Values higher than 1.0 denote the opposite relationship.
Volume kinetics
The kinetics of the infusion fluid was studied by a mixed model approach on the non-invasive and invasive data separately. The first three were included while the fourth was excluded due to the large hemorrhage (median 950 mL) and the use of two infusion fluids. The fifth was also excluded because the oral ingestion of fluid would necessitate the use of a structurally different kinetic model than was used for the other studies.
The model had two dependent variables, the total urinary excretion and frequently measured plasma dilution. The latter was derived as the hemodilution divided by (1–baseline hematocrit). In turn, the hemodilution had been obtained as (Hbo–Hb)/Hb, in which Hbo is the baseline value and Hb denotes measurements taken at a later time.
The model has been created to reflect body physiology. Vc is thought to correspond to the plasma from which distribution and redistribution occurs to an extravascular space, Vt. Hence, a two-volume kinetic model with rate constants for distribution and re-distribution (k12 and k21), one route of elimination (k10), and one scaling factor between dilution and volume (Vc, central volume) was fitted to two dependent variables in all experiments on a single occasion, using the Phoenix software for nonlinear mixed effects, version 1.3 (NLME, Pharsight, St. Louis, MO). All flows are proportional to the value of the rate constant to the volume expansion of a fluid space, being Vc for k12 and k10, and Vt for k21. The estimate of k10 was stabilized by the measured urinary excretion, as described elsewhere [11,12,13]. The search routine used was the First-Order Conditional Estimation Extended Least Squares (FOCE ELS).
Statistics
Data are reported as the median (25th to 75th percentile) and kinetic parameters as the best estimate and 95% confidence interval. The agreement between the two modes of measuring Hb was illustrated by Bland-Altman plots that showed the mean difference (the agreement) and the associated 95% limits of agreement (i.e., ± 2 standard deviations of the differences). Point-wise comparisons been non-invasive and invasive Hb measurements has previously been reported from three of the five case series [11,12,13].
Relationships were studied by simple linear regression, where r2 = the coefficient of determination (the “scatter” of the data).
The number of experiments was set at 60, which was felt to be an appropriate number for outlining the relationship between non-invasive and invasive Hb. Power analysis was applied in the respective studies. P < 0.05 was statistically significant.
Results
At baseline, a statistically significant correlation was observed between the invasive and non-invasive measurement of Hb (Fig. 1a). The mean difference was only + 0.5 g L− 1, but the 95% limits of agreement ranged from − 20 to + 21 g/L (Fig. 1b).
Maximum and minimum Hb
The highest invasive Hb measured in the 63 patients was 136 (121–144) g L− 1 and the lowest 117 (107–130) g L− 1. For the non-invasive Hb, these values were 131 (123–141) g L− 1 and 117 (105–126) g L− 1, respectively (Table 2). The difference between highest and lowest was quite similar for the two modes of measuring Hb, at 14 (10–21) vs. 15 (11–20) g L− 1. Hb was ≤100 g L− 1 in 90 of the 915 invasive measurements (10%).
In the subsequent presentation, we refrain from making point-wise comparison between the two technologies but focus on the linearity between their relative changes in a series of measurements in the same subject when Hb is deliberately changed. The results are expressed as the scatter (precision) and slope (accuracy) of non-invasive Hb to indicate the invasive Hb.
Scattering
Overall, 46 (22–72)% of the changes of non-invasive Hb could be explained by changes in invasive Hb, i.e. the median “scatter” (r2) was 0.46. However, variability between the studies was considerable; the data were most closely assembled around the regression line during major surgery, r2 being 0.72 (Table 2).
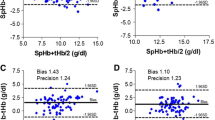
As a rule, the scatter decreased with the Hb range in each series; a greater difference between the highest and lowest invasive Hb led to a higher r2 for the relationship between the two variables (Fig. 1c).
Slope
The regression slope shows how much of a change in invasive Hb is indicated by non-invasive Hb on the average during an entire experiment. The non-invasive Hb could either underestimate (weak slope, < 1.0), predict well (good slope = 1.0), or overestimate (steep slope, > 1.0), respectively, the hemodilution given by the invasive Hb. Figure 2 shows three individual experiments where the slope factor for the regression was weak, good, and steep.
Three experiments with different slopes. Distances between the marks are set equal in each subplot to facilitate comparison. a Flat slope. The non-invasive Hb changes much less than the invasive Hb. b Normal slope. The rise in non-invasive Hb is similar to the rise of the invasive Hb. c Steep slope. Greater increase in non-invasive Hb than for the invasive technology
Overall, the slope factor was 0.57 (0.33–1.01) but it differed greatly depending on the presence of surgical stress, being 1.00 (0.80–1.14) in the volunteer studies and 0.48 (0.37–0.73) in in association with surgical stress (studies 3 and 4; P < 0.006).
In Study 4, the surgical hemorrhage volume was 950 (780–1225) mL and did not correlate with the data scattering or with the slope factor.
Hemodilution
Figure 3 compares all invasive and non-invasive hemodilution measurements in each sub-study. The patient mean hemodilution was 6.0 (3.5–10.3)% for the invasive and 4.9 (1.3–8.0)% for the non-invasive technologies (P < 0.01).
The non-invasive Hb underestimated the hemodilution given by the invasive Hb in the surgical stress studies, but not the volunteer studies; the difference between the patient mean hemodilution, as given by invasive and non-invasive Hb, was − 0.1 (− 2.4 to + 2.5)% in the volunteer studies but + 4.2 (1.0–8.3)% in the studies associated with surgical stress (P < 0.001).
Figure 4a compares, in each subject, the relationship between the mean hemodilution as given by invasive and non-invasive Hb.
Figure 4b shows the distribution of subjects between ranges of slope factors.
Low perfusion index
Only 15 of the 915 points of measurement (1.6%) were performed in the presence of a perfusion index of 1.0 or lower, and these low values occasionally distorted the data in Study 1 and 4 (Fig. 3f, Fig. 5).
Volume kinetics
Fitting the two-volume kinetic model to the data on plasma dilution and urinary excretion was successful for both the invasive and the non-invasive methods (Fig. 6a-c). The precision of the kinetic parameters was higher for the invasive Hb than for the non-invasive Hb (Table 3), and more outliers became apparent when the kinetic parameters were used to re-create the dependent variables (Fig. 6d and e).
Volume kinetics. Curve-fitting of the Hb data from Studies 1–3 as obtained by the (a) invasive and (b) non-invasive measurements. c Schematic drawing of the kinetic model. d The model-predicted versus the measured plasma dilution as obtained with the (d) invasive and (e) non-invasive Hb. f Simulation of the volume expansion of the central body fluid space (the plasma) when 1 L of Ringer’s acetate is infused over 30 min
The best estimates of all parameters, as shown in Table 3, were used to simulate the outcome of fictious infusions. Those plots showed that the simulated expansion of the plasma volume was smaller when the non-invasive Hb was used — a difference that can be explained by the combination of higher k12 and lower k21 (Fig. 6f).
Discussion
The five evaluated cohorts indicate the possibilities and limits of measuring Hb non-invasively. Overall, the difference between the highest and lowest Hb values was quite similar between the two technologies but, as shown many times before, there were wide limits of agreement at the baseline. Nevertheless, changes in Hb measured by the pulse oximeter often followed quite well the trends yielded by invasive measurement. However, this was not a universal finding. The non-invasive technique showed good precision but underestimated the magnitude of the invasive Hb changes in the presence of pre-surgical or surgical stress. By contrast, the precision was poor but the accuracy good in the volunteer studies.
Surgical setting versus non-stressed volunteers
The clinical question of whether erythrocytes should be transfused was most real in Study 4 where measurements were performed during major surgery. The blood loss during the data collection amounted to almost 1 l, and the patients received both Ringer’s and 20% albumin. Norepinephrine infusion was used to maintain the arterial pressure. The hemodilution was twice as large as that seen in any of the other studies.
The non-invasive Hb followed the trends observed in the invasive Hb quite well, with an overall r2 as high as 0.72 despite occasional outliers that were sometimes due to a low perfusion index. One should note that 0.72 is the mean linearity from individual analysis of each patient, whereas the r2 yielded by point-wise comparisons based on the pooled data from all patients in Study 4 was considerably lower, only 0.27. Importantly, the magnitude of the hemodilution changes was underestimated, and it usually amounted to only half of the invasive value (Fig. 3d).
The underestimation of the hemodilution by the non-invasive approach is shared by Study 3, which was performed in patients awaiting major open abdominal surgery. The fact that the two clinical studies show the same pattern — namely, a too small hemodilution indicated by the non-invasive Hb and, hence, a low slope factor — suggests that adrenergic stress limits the magnitude of the Hb changes detected by the non-invasive technology, albeit without distorting the trend over time.
Studies 1 and 2 were both performed in a similar way in volunteers, but using different amounts of crystalloid fluid. Both studies had slopes with a median value close to 1.0, and the non-invasive hemodilution was approximately 20% greater than that obtained with the invasive Hb. Hence, the relationship between the two modes of measurement was opposite to that obtained in the perioperative setting, which supports the notion that data obtained in volunteers cannot be uncritically assumed to be valid in stressful situations.
By contrast, the performance of the non-invasive technology with oral administration of fluid was disappointing. Here, non-invasive measurement usually showed no change at all, or a trend opposite to that obtained by the invasive Hb. However, the average hemodilution obtained by invasive sampling averaged only 3%, which then seems too small to overcome the between-subject variability of the non-invasive Hb technique to any reasonable degree.
Volume kinetics
Another issue is whether non-invasive monitoring can be used for the study of fluid population kinetics. For this purpose, the Hb data had to be converted to plasma dilution, which attains values that are approximately twice as large as the hemodilution. Previous studies have used non-invasive Hb for kinetic analysis in a two-stage approach, but with limited success [2, 12]. Here, all appropriate curves were analyzed in one single run, which offers a more stable output.
The analysis shown in Fig. 6 reveals that fitting the commonly used two-volume kinetic model to the present data produced more outliers and less precise estimates of the model parameters when based on the non-invasive as compared to the invasive technology. In our fictitious fluid experiment, the difference between the modes of measuring Hb became apparent during the distribution phase but not during infusion.
Present report versus the literature
Many previous studies have examined the methodological bias by making point-wise comparisons between invasive and non-invasive measurements of Hb, usually without separating intra- and inter-individual differences. Some studies show a bias of 1–2% [1,2,3,4], while studies in cardiac and emergency care report underestimations of the invasive Hb of as much as 12–18 g L− 1 by the non-invasive technique [5,6,7]. These results support our observation that changes in non-invasive Hb become too small in stressed settings. The precision has consistently been poor, with 95% limits of agreement being in the range of 40–50 g L− 1 [3, 8], or even wider [4,5,6,7]. The conclusion in a meta-analysis of 32 studies from 2016 confirmed that the mean difference between the two modes of measuring Hb is small, while the range between the 95% limits of agreement is too wide to allow clinical decisions to be based on them [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17].
Our review does not focus on point-wise comparisons; rather, it emphasizes a series of Hb changes, which we feel is more informative about the value of this monitoring in the perioperative setting. Here, hemodilution curves derived by the two modes of measuring Hb most often showed quite similar trends, but the many successful cases (high r2) were occasionally interrupted by curves showing poor agreement, so as to be misleading. Some of these were “switches” remain unexplained. The most stable indications were obtained in the surgical setting, where r2 was below 0.25 in only 2/23 patients, although the non-invasive Hb systematically underestimated the hemodilution. The scattering was aggravated in the presence of a very low perfusion index. By contrast, Chang et al. [10], found the accuracy of the Radical-7 to be good even when the perfusion index is below 1.0.
Limitations
Limitations of this analysis include that the invasive Hb was measured in venous blood while the non-invasive method is believed to represent arterial or capillary Hb. However, the two sites of measurement should not differ much in terms of Hb concentration [18]. The five series of Hb experiments were collected under different conditions, which are described in detail elsewhere, but these differences do form the basis of the present conclusions [11,12,13,14,15,16]. Data were collected over a period of almost 10 years, during which the algorithm for calculating non-invasive Hb is claimed to have been improved. However, more recent work on Hb during spinal surgery and liver transplantation [10, 19] show almost identical accuracy and precision for the non-invasive Hb as we reported in 2010 [2]. These authors also studied the concordance between changes in invasive and non-invasive Hb during surgery [10, 19]. However, we chose to present our results differently, as we obtained data at very short intervals, usually only 5–10 min, and up to 25 times per experiment.
Conclusions
Five series of Hb measurements showed that the linearity between invasive and non-invasive Hb data was strongest for the most pronounced hemodilution in surgical patients, albeit the hemodilution was underestimated. Data from volunteers yielded better accuracy but showed more scatter (poorer precision). Results were unreliable for hemodilution in the range of 3–4%. The non-invasive methodology has severe limitations, but Hb trends can be monitored relatively well during surgery to identify the need for erythrocyte transfusion if. However, we recommend that quality of the non-invasive Hb curve supported by timely invasive measurements.
Availability of data and materials
The data used for the kinetic analysis is available as Additional file.xls (studies 1, 2 and 3). Data for Studies 4 and 5 are available from the corresponding author on request.
Change history
29 October 2021
The funding note “Open access funding provided by Karolinska Institute” was added. The article has been updated.
Abbreviations
- CI:
-
Confidence interval
- CV:
-
Coefficient of variation
- Hb:
-
Hemoglobin
- k 12 :
-
Rate constant for fluid passing from the plasma to the extravascular fluid space
- k 21 :
-
Rate constant for fluid passing from the extravascular fluid space to the plasma
- k 10 :
-
Rate constant for fluid leaving the kinetic system as urine
- L:
-
Liter
- mL:
-
Milliliter
- r2 :
-
Coefficient of determination (“scatter”)
- SpHb:
-
Pulse co-oximetry hemoglobin
- V c :
-
Size of central body fluid space
- V t :
-
Size of peripheral (extravascular) body fluid space
References
Macknet MR, Allard M, Applegate RL, Rook J. The accuracy of noninvasive and continuous total hemoglobin measurement by pulse CO-oximetry in human subjects undergoing hemodilution. Anesth Analg. 2010;111(6):1424–6 https://doi.org/10.1097/ANE.0b013e3181fc74b9.
Hahn RG, Li Y, Zdolsek J. Non-invasive monitoring of blood haemoglobin for analysis of fluid volume kinetics. Acta Anaesthesiol Scand. 2010;54(10):1233–40 https://doi.org/10.1111/j.1399-6576.2010.02321.x.
Lamhaut L, Apriotesei R, Combes X, Lejay M, Carli P, Vivien B. Comparison of the accuracy of noninvasive hemoglobin monitoring by spectrophotometry (SpHb) and HemoCue® with automated laboratory hemoglobin measurement. Anesthesiology. 2011;115(3):548–54 https://doi.org/10.1097/ALN.0b013e3182270c22.
Miller RD, Ward TA, Shiboski SC, Cohen NH. A comparison of three methods of hemoglobin monitoring in patients undergoing spine surgery. Anesth Analg. 2011;112(4):858–63 https://doi.org/10.1213/ANE.0b013e31820eecd1.
Colquhoun DA, Forkin KT, Durieux ME, Thiele RH. Ability of the Masimo pulse CO-oximeter to detect changes in hemoglobin. J Clin Monit Comput. 2012;26(2):69–73 https://doi.org/10.1007/s10877-012-9335-3.
Nguyen B-V, Vincent J-L, Nowak E, Coat M, Paleiron N, Gouny P, et al. The accuracy of noninvasive hemoglobin measurement by multiwavelength pulse oximetry after cardiac surgery. Anesth Analg. 2011;113(5):1052–7 https://doi.org/10.1213/ANE.0b013e31822c9679.
Gayat E, Bodin A, Sportiello C, Boisson M, Dreyfus JF, Mathieu E, et al. Performance evaluation of a noninvasive hemoglobin monitoring device. Ann Emerg Med. 2011;57(4):330–3 https://doi.org/10.1016/j.annemergmed.2010.11.032.
Causey MW, Miller S, Foster A, Beekley A, Zenger D, Martin M. Validation of noninvasive hemoglobin measurements using the Masimo Radical-7 SpHb Station. Am J Surg. 2011;201(5):592–8 https://doi.org/10.1016/j.amjsurg.2011.01.020.
Berkow L, Rotolo S, Mirski E. Continuous noninvasive hemoglobin monitoring during complex spine surgery. Anesth Analg. 2011;113(6):1396–402 https://doi.org/10.1213/ANE.0b013e318230b425.
Chang FC, Lin JR, Liu FC. Validity of accuracy and trending ability of non-invasive continuous total hemoglobin measurement in complex spine surgery: a prospective cohort study. BMC Anesthesiol. 2019;19(1):117. https://doi.org/10.1186/s12871-019-0790-y.
Hahn RG, Bergek C, Gebäck T, Zdolsek J. Interactions between the volume effects of hydroxyethyl starch 130/0.4 and Ringer’s acetate. Crit Care. 2013;17(3):R104 https://doi.org/10.1186/cc12749.
Zdolsek J, Li Y, Hahn RG. Detection of dehydration by using volume kinetics. Anesth Analg. 2012;115(4):814–22. https://doi.org/ANE.0b013e318261f6ba. https://doi.org/10.1213/ANE.0b013e318261f6ba.
Hahn RG, Bahlmann H, Nilsson L. Dehydration and fluid volume kinetics before major open abdominal surgery. Acta Anaesthesiol Scand. 2014;58(10):1258–66. https://doi.org/aas.12416. https://doi.org/10.1111/aas.12416.
Löffel LM, Hahn RG, Engel D, Wuethrich PY. Intraoperative intravascular effect of ringer lactated and hyperoncotic albumin during hemorrhage in cystectomy patients. Anesth Analg. 2020; https://doi.org/10.1213/ane.0000000000005173, Publish Ahead of Print.
Zdolsek J, Metander AS, Hahn R. Volume kinetic evaluation of fluid turnover after oral intake of tap water, lemonade and saline in volunteers. BMC Sports Sci Med Rehabil. 2016;8(1):22. https://doi.org/10.1186/s13102-016-0045-x.
Bergek C, Zdolsek JH, Hahn RG. Accuracy of non-invasive hemoglobin (SpHb) depends on the type of infusion fluid. Eur J Anaesthesiol. 2012;29(12):586–92 https://doi.org/10.1097/EJA.0b013e3283592733.
Kim SH, Lilot M, Murphy LS, Sidhu KS, Yu Z, Rinehart J, et al. Accuracy of continuous noninvasive hemoglobin monitoring. Anesth Analg. 2016;119(2):332–46 https://doi.org/10.1213/ANE.0000000000000272.
Hahn RG, Lindahl C, Drobin D. Volume kinetics of acetated Ringer’s solution during experimental spinal anaesthesia. Acta Anaesthesiol Scand. 2011;55(8):987–94 https://doi.org/10.1011/j.1399-6576.2011.02493.x.
Huang PH, Shih BF, Tsai YF, Chung PCH, Liu FC, Yu HP, et al. Accuracy and trending of continuous noninvasive hemoglobin monitoring in patients undergoing liver transplantation. Transpl Proc. 2016;48(4):1067–70 https://doi.org/10.1016/j.transproceed.2015.12.121.
Acknowledgements
The authors are grateful to the co-authors and others who contributed to the original papers on which the present work is based.
Funding
Department funds from Research Unit, Södertälje Hospital. Open Access funding was provided by Karolinska Institutet. The funding organizations played no role in the design, analysis, and interpretation of the data and in writing the manuscript. Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Contributions
RGH and JHZ planned the studies but PYW planned Study 4. The data was collected by JHZ and co-workers and, in Study 4, by PYW. RGH made the calculations and wrote the manuscript. All authors read and approved the final manuscript.
Authors’ information
Robert G. Hahn: Researcher at Södertälje Hospital, Södertälje, Sweden: Professor of Anesthesia and Intensive care at Karolinska Institutet at Danderyds Hospital (KIDS), Stockholm, Sweden.
Patrick Y. Wuethrich: Clinical anesthetist at Inselspital, Bern University Hospital, and associate professor of anesthesia at the University of Bern, Switzerland.
Joachim H. Zdolsek: anesthesiologist at Linköping University Hospital, associate professor at Linköping University, Linköping Sweden.
Corresponding author
Ethics declarations
Consent to publication
Not applicable.
Ethics approval and consent to participate
Ethical approvals were obtained by the Regional Ethics Committee of Stockholm, Sweden, as 2009/1091–31/2 (on September 18, 2009); the Regional Ethics Committee of Linköping, Sweden, as M114–09 (June 17, 2009), 2011/101–31 May 20, 2011), and 2010/241–31 September 29, 2010); and by the Cantonal Ethics Committee KEK Bern, Switzerland, KEKBE ID 2018–02351 (on February 20, 2019). The corresponding registrations at ClinicalTrials.gov were NCT01195025, NCT 01062776, NCT01458678, NCT01360333, and NCT 03848507. All patients gave us their written informed consent to participate.
Competing interests
RGH holds a grant from Grifols for the study of 20% albumin as infusion fluid.
The other authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hahn, R.G., Wuethrich, P.Y. & Zdolsek, J.H. Can perioperative hemodilution be monitored with non-invasive measurement of blood hemoglobin?. BMC Anesthesiol 21, 138 (2021). https://doi.org/10.1186/s12871-021-01351-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-021-01351-4