Abstract
Background
Non-invasively continuous total hemoglobin (SpHb) measurement has not been assessed adequately in acute bleeding and rapid blood transfusion during surgery. Thus, we have assessed the efficacy of SpHb during both acute normovolemic hemodilution (ANH) and autologous blood transfusion (ABT).
Methods
Twenty-four patients undergoing urological and gynecological surgery were enrolled. ANH was induced by withdrawing blood of 800 g with simultaneous fluid administration. When surgical hemostasis was completed, collected blood was reinfused. Measurement of SpHb, perfusion index (PI) and real total Hb (tHb) were done before and after each 400 ml blood removal (−0, −400, −800 ml) and reinfusion (+0, +400, +800 ml).
Results
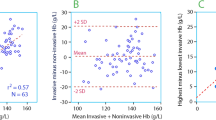
A Bland–Altman analysis for repeated measurements showed a bias (precision) g/dl of 1.12 (1.25), 1.43 (1.24) and 1.10 (1.23) for all data, during ANH and during ABT, respectively. Additionally, a bias (precision) increased with a reduction in tHb (g/dl): ≥10.0; 0.74 (1.30), 8.0–10.0; 1.15 (1.12) and <8.0; 1.60 (1.28). Although the difference between SpHb and tHb was almost zero before anesthesia induction, it became significant just before ANH and did not change further by ANH and ABT. Significant correlations between SpHb and tHb for all data (r = 0.75, n = 228, p < 0.001) were observed. PI slightly correlated with the difference between SpHb and tHb (r = 0.38, n = 216, p < 0.001). Furthermore, before and after induction of anesthesia, PI also correlated with the difference between SpHb and tHb (r = 0.42, n = 23, p = 0.048 and r = 0.51, n = 22, p = 0.016, respectively).
Conclusions
The present data suggest that SpHb may overestimate tHb during ANH and ABT. In addition, PI and tHb levels had an impact on the accuracy of SpHb measurements.



Similar content being viewed by others
References
Macknet MR, Allard M, Applegate RL 2nd, Rook J. The accuracy of noninvasive and continuous total hemoglobin measurement by pulse CO-Oximetry in human subjects undergoing hemodilution. Anesth Analg. 2010;111:1424–6.
Frasca D, Dahyot-Fizelier C, Catherine K, Levrat Q, Debaene B, Mimoz O. Accuracy of a continuous noninvasive hemoglobin monitor in intensive care unit patients. Crit Care Med. 2011;39:2277–82.
Berkow L, Rotolo S, Mirski E. Continuous noninvasive hemoglobin monitoring during complex spine surgery. Anesth Analg. 2011;113:1396–402.
Oriani G, Pavesi M, Oriani A, Bollina I. Acute normovolemic hemodilution. Transfus Apher Sci. 2011;45:269–74.
Matot I, Scheinin O, Jurim O, Eid A. Effectiveness of acute normovolemic hemodilution to minimize allogeneic blood transfusion in major liver resections. Anesthesiology. 2002;97:794–800.
Casati V, Benussi S, Sandrelli L, Grasso MA, Spagnolo S, D’Angelo A. Intraoperative moderate acute normovolemic hemodilution associated with a comprehensive blood-sparing protocol in off-pump coronary surgery. Anesth Analg. 2004;98:1217–23.
Terai A, Terada N, Yoshimura K, Ichioka K, Ueda N, Utsunomiya N, Kohei N, Arai Y, Yonei A. Use of acute normovolemic hemodilution in patients undergoing radical prostatectomy. Urology. 2005;65:1152–6.
Ginosar Y, Weiniger CF, Meroz Y, Kurz V, Bdolah-Abram T, Babchenko A, Nitzan M, Davidson EM. Pulse oximeter perfusion index as an early indicator of sympathectomy after epidural anesthesia. Acta Anaesthesiol Scand. 2009;53:1018–26.
Sebastiani A, Philippi L, Boehme S, Closhen D, Schmidtmann I, Scherhag A, Markstaller K, Engelhard K, Pestel G. Perfusion index and plethysmographic variability index in patients with interscalene nerve catheters. Can J Anaesth. 2012;59:1095–101.
Miller RD, Ward TA, Shiboski SC, Cohen NH. A comparison of three methods of hemoglobin monitoring in patients undergoing spine surgery. Anesth Analg. 2011;112:858–63.
Causey MW, Miller S, Foster A, Beekley A, Zenger D, Martin M. Validation of noninvasive hemoglobin measurements using the Masimo Radical-7 SpHb Station. Am J Surg. 2011;201:592–8.
Butwick A, Hilton G, Carvalho B. Non-invasive haemoglobin measurement in patients undergoing elective caesarean section. Br J Anaesth. 2012;108:271–7.
Lamhaut L, Apriotesei R, Combes X, Lejay M, Carli P, Vivien B. Comparison of the accuracy of noninvasive hemoglobin monitoring by spectrophotometry (SpHb) and HemoCue® with automated laboratory hemoglobin measurement. Anesthesiology. 2011;115:548–54.
Nguyen BV, Vincent JL, Nowak E, Coat M, Paleiron N, Gouny P, Ould-Ahmed M, Guillouet M, Arvieux CC, Gueret G. The accuracy of noninvasive hemoglobin measurement by multiwavelength pulse oximetry after cardiac surgery. Anesth Analg. 2011;113:1052–7.
Vos JJ, Kalmar AF, Struys MM, Porte RJ, Wietasch JK, Scheeren TW, Hendriks HG. Accuracy of non-invasive measurement of haemoglobin concentration by pulse co-oximetry during steady-state and dynamic conditions in liver surgery. Br J Anaesth. 2012;109:522–8.
Pries AR, Secomb TW. Rheology of the microcirculation. Clin Hemorheol Microcirc. 2003;29:143–8.
Maeda N. Erythrocyte rheology in microcirculation. Jpn J Physiol. 1996;46:1–14.
Naftalovich R, Naftalovich D. Error in noninvasive spectrophotometric measurement of blood hemoglobin concentration under conditions of blood loss. Med Hypotheses. 2011;77:665–7.
Acknowledgments
The authors are grateful to Professor Paul Hollister (Medical English Center, Hirosaki University Graduate School of Medicine, Hirosaki, Japan) for his useful suggestions. This work was supported by the Department of Anaesthesiology, Hirosaki University Graduate School of Medicine.
Conflict of interest
The author(s) declare that they have no competing interests.
Ethical standards
This study protocol was approved by Hirosaki University ethic committee. Zaifu-cho 5, Hirosaki 036-8562, Japan.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Saito, J., Kitayama, M., Oishi, M. et al. The accuracy of non-invasively continuous total hemoglobin measurement by pulse CO-Oximetry undergoing acute normovolemic hemodilution and reinfusion of autologous blood. J Anesth 29, 29–34 (2015). https://doi.org/10.1007/s00540-014-1863-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-014-1863-1