Abstract
Background
Acetabular cup positioning in total hip arthroplasty (THA) is closely related to outcomes. The literature has suggested cup parameters defined by the Lewinnek safe zone; however, the validity of such measures is in question. Several studies have raised concerns about the benefits of using the Lewinnek safe zone as a predictor of success. In this study we elected to use prospective surgeon targets as the basis for comparison to see how successful surgeons are positioning their cup using standard instruments and techniques.
Methods
A prospective, global, multicenter study was conducted. Cup positioning success was defined as a composite endpoint. Both cup inclination and version needed to be within 10° of the surgeon target to be considered a success. Radiographic analysis was conducted by a third-party reviewer.
Results
In 170 subjects, inclination, target versus actual, was 44.8° [standard deviation (SD 0.9°)] and 43.1° (SD 7.6°), respectively (p = 0.0029). Inclination was considered successful in 84.1% of cases. Mean version, target versus actual, was 19.4° (SD 3.9°) and 27.2° (SD 5.6°), respectively (p < 0.0001). Version was considered successful in 63.4% of cases, and combined position (inclination and version) was considered successful in 53.1%.
Conclusion
This study shows that with traditional methods of placing the cup intraoperatively, surgeons are only accurate 53.1% of the time compared with a predicted preoperative plan. This study suggests that the inconsistency in cup positioning based on the surgeon’s planned target is potentially another important variable to consider while using a mechanical guide or in freehand techniques for cup placement in THA.
Trial Registration: This study is registered on ClinicalTrials.gov, NCT03189303.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Acetabular cup positioning in total hip arthroplasty (THA) has been shown to be closely related to both short- and long-term outcomes. Malposition has been linked to higher rates of dislocation [1,2,3], impingement of the prosthetic neck against the acetabular rim [4], bearing surface wear [5,6,7,8,9,10,11,12,13,14,15], squeaking and ceramic breakage [16, 17], poor biomechanics [18, 19], leg length discrepancy [20], groin pain and reduced range of motion [21,22,23], pelvic osteolysis [3], and revision. Some studies have also demonstrated an increased risk of malposition with low-volume surgeons [23], higher patient body mass index (BMI) [23, 24], and minimally invasive surgical technique [25], although these findings have not been corroborated by other studies [23, 26,27,28]. Cup positioning success is often assessed in relation to the “safe zones” described by Lewinnek [29], who defined a range of 30–50° of inclination (abduction) and 5–25° of anteversion for minimizing dislocation risk. There are a number of investigations that cast doubt on this zone being adequate to predict cup positioning success for all patients and all approaches, since dislocation risk is comparable with placement outside of this “safe zone” [30,31,32,33]. There is also a growing body of evidence to support the need for unique strategies to combat spinopelvic issues [34, 35]. A surgeon should be able to place the cup in the orientation that best fits the needs of the patient [36] according to intraoperative landmarks [37]. As we develop a “true safe zone” it is critical that we understand how accurately we can achieve cup placement given a specific target and in this study we define success as the ability of the surgeon to orient the cup within 10° of their established target for radiographic inclination and version [38]. Secondarily, we collected short-term clinical outcomes and complications to allow for future study of any relevant correlations to cup position.
Materials and methods
A global, prospective, multicenter study was conducted at eight sites between August 2017 and December 2021. One experienced medium-volume (50–100 primary THA cases per year) surgeon performed all procedures at each center. Informed consent was collected for all subjects prior to participation. Preoperative assessments included Harris Hip Score [39], EQ-5D-5L [40, 41], radiographs [anteroposterior (AP) hip, AP pelvis, lateral], baseline patient reported early functional recovery outcomes, and surgeon preoperative planning details (target cup inclination and version angles and cup size based on surgeon’s preference). A Pinnacle acetabular cup (DePuy Synthes, Warsaw, IN, USA) was used in all cases. Surgeries were performed via posterior or anterolateral approach with the subject in lateral decubitus position. No imaging or navigation was used to aid in placement of the acetabular components. Surgeons could place the cup freehand or with a mechanical guide. Intraoperative complications were recorded, along with operative datapoints of primary diagnosis, ASA risk, surgery duration, surgical approach, incision measurement, screw use, bone class, and osteophyte removal. Date of discharge and discharge disposition was recorded. Postoperative assessments included Harris Hip Score, EQ-5D-5L, Forgotten Joint Score (FJS-12) [42], radiographs (AP hip, AP pelvis, lateral), and patient reported early functional recovery outcomes. Complications (all serious and device- or procedure-related) were recorded from the time of subject consent to end of study participation.
Statistical analysis
This study was not powered to detect a specific difference in the primary endpoint, instead the sample size was estimated to allow a certain margin of error in the proportion of acetabular cups successfully positioned as measured from postoperative radiographs. Cup positioning success was defined as a composite endpoint. Both cup inclination and cup version needed to be within 10° of the surgeon target to be considered a success. The number of subjects and the proportion with acetabular cup position success and its two-sided 95% confidence intervals were evaluated using the binomial exact method. Data from the films collected during the 6-week visit were used whenever available for primary endpoint analysis. If the films necessary for primary endpoint analysis were missing, incomplete or of poor quality, the films collected at the 12-week visit were used. Patient-reported outcomes scores were summarized with descriptive statistics.
Radiographic analysis
Acetabular cup inclination and version was measured as described by Wan et al. [43]. Inclination was defined as the angle between the face of the acetabular shell and the transverse axis of the subject via obturator foramen or pelvic tear drops, and version as the angle between the acetabular axis and the coronal plane; both were measured from standing AP pelvis radiographs. Additionally, if present, migration/subsidence, radiolucency, osteolysis, fracture, sclerotic lines, and heterotopic ossification were documented and summarized (femoral and acetabular). The AP standing radiographs had to comply with the following criteria: distance between the symphysis and the sacrococcygeal joint of ~ 30mm (10–40 mm) in men and 50 mm (40–60 mm) in women to exclude abnormal pelvic tilt in the sagittal plane [44, 45] and the coccyx centered on the pubic symphysis to exclude rotation of the pelvis in the transverse plane [45]. In the absence of a full lower extremity long standing AP X-ray view, proximal femur/pelvis vertical alignment was estimated from the weight-bearing AP pelvis X-ray view. Proximal femur/pelvis vertical alignment was determined by measuring the difference of the vertical distances between the left and right pelvic teardrops and the center of the respective femoral heads to provide an estimate of leg-length discrepancy [46]. All radiographic analysis was conducted by a single, independent, third-party, practicing board-certified musculoskeletal radiologist reviewer (Medical Metrics, Inc., Houston, TX, USA).
Patient demographics
A total of 184 subjects were enrolled in the study, 171 were treated. One subject was treated via anterior approach and was excluded from analysis, leaving a total of 170 in the per-protocol analysis set. Mean age was 65.8 (SD 8.9) years, mean BMI was 29.7 (SD 6.1), and 108 (63.5%) hips were women. Primary diagnosis was osteoarthritis in 150 (88.2%) hips. Acetabular bone class was reported as normal or good in 152 (89.4%) hips. Osteophytes were removed in 83 (48.8%) cases. Acetabular screws were used in 27 (15.9%) cases. Additional demographic and surgical details are presented in Table 1.
Results
One subject died due to an accident unrelated to their hip surgery. Eight intraoperative fractures were reported: three greater trochanter, three acetabular, one pubic rami, and one femoral. The other serious or hip-related complications reported were dislocation (two; one recurrent), wound secretion and infection treated with revision one day after the initial surgery (one), wound infection (one), acetabular loosening (one), lower extremity numbness (one), foot drop (one), renal insufficiency (one), and urosepsis (one).
Clinical outcomes are outlined in Table 2. The Harris hip score improved from a mean of 51.3 preoperatively to 92.7, 12 weeks postoperatively. The EQ-5D-5L score improved from a mean of 0.59 preoperatively to 0.85, 12 weeks postoperatively. The EQ-5D-VAS score improved from a mean of 67.9 preoperatively to 83.6, 12 weeks postoperatively. Patients stated they were “extremely” or “very” satisfied postsurgery, a combined 93.2% of the time. We reviewed any potential correlations between clinical outcomes and cup position but there were no significant differences between groups.
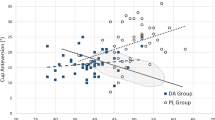
Cup positioning outcomes are outlined in Table 3; radiographic outcomes in Table 4. The mean inclination at the first available postoperative visit, target versus actual, was 44.8° (standard deviation 0.9°) and 43.1° (standard deviation 7.6°), respectively (p = 0.0029). The mean difference was −1.7°. A total of 138 of the 164 (84.1%) patients measured had a “successful” cup position with regards to abduction, or inclination, being within 10° of the stated target. The mean version at the first available postoperative visit, target versus actual, was 19.5° (standard deviation 3.9°) and 27.2° (standard deviation 5.6°), respectively (p < 0.0001). The mean difference was 7.8°. A total of 102 of the 161 (63.4%) patients measured had a “successful” cup position with regards to version, being within 10° of the stated target (Fig. 1).
For total cup positioning, 86 of 162 (53.1%) patients had a “successful” cup position with regards to inclination and version being within 10° plus or minus of the stated targets. Figure 2 is a scatter plot of the results of this study superimposed on Lewinnek’s “safe zone” for reference. Figure 3 shows the difference between the surgeon targets and the measured radiographic inclination and anteversion angles. We stratified cup positioning results by surgical approach and found that inclination and overall cup positioning varied between groups. Inclination was successful in 92.7% of anterolateral cases compared with 71.9% of posterior cases. There were not significant differences for version success or overall success.
Discussion
In this prospective, global, multicenter study, we compared the radiographic inclination and version angles of the cup with the pre-/intraoperatively defined target by the surgeon. We found that the mean radiographic inclination of the cup was slightly lower than targeted for with 84% within the desired range of ± 10°. The mean radiographic anteversion was significantly higher than targeted with 63% within the desired range of ± 10°. For the combined radiographic inclination and version, only 53% were within the desired zone. These data demonstrate that with traditional methods, surgeons are only able to implant a cup in a targeted orientation in slightly more than half of their patients.
Many studies have shown that a successful cup position by radiographic criteria and a perceived “safe zone” does not mean a successful outcome [47], and others have shown that a cup position out of the same “safe zone” does not mean failed outcomes [48]. Clearly the outcomes and possible complications, such as dislocation, are multifactorial and involve surgical approach, combined version (the cup and the femoral stem versions combined), pelvic tilt and obliquity, and spinal conditions. Table 5 shows the success rates of similar studies [23, 25, 27, 49,50,51,52,53]. As far as the authors are aware, this is the first prospective study conducted to review cup positioning success in THA as previous studies have utilized retrospective radiographic review to the Lewinnek safe zone instead of the prospective preoperative target.
The current study was not designed to determine a “safe zone” for acetabular cup position to predict stability and outcomes as many others have. The factors that constitute successful outcomes and prevent complications are multifactorial and should be individualized by each surgeon for each patient. Several methods have been described for improving the accuracy of implant positioning in everyday clinical practice, including intraoperative landmarks that can be safely used to control the orientation of the cup, such as the transverse acetabular ligament [37]. Increasing knowledge of spino-pelvic issues advocates tailored implant positioning for each patient with specific consideration to cup orientation. This study was designed to evaluate how accurate the cup position was compared to the surgeon target and the preoperative plan, using plain film radiographs.
Since mean BMI in our population was nearly 30, we reviewed cup positioning success by BMI category [less than 18.5 (underweight), 18.5–24.9 (normal), 25.0–29.9 (overweight), and 30.0 and over (obese)]. We found that cup positioning success increased with BMI. Overall cup positioning success was 42% for normal BMI, 46% for overweight, and 63% for obese. However, due to the relatively low numbers in these groups (36, 54, and 71, respectively), these results should be evaluated with caution.
Limitations of this study first include the fact that it is not a randomized study, but a prospective cohort study. Moreover, the study is multicenter, so different surgical landmarks, surgical approaches, and techniques have been used by these surgeons. However, all the procedures were performed in lateral decubitus position, without any imaging or navigation support and the comparison were not among different surgical techniques, but with regards to surgeons’ targets, thus depicting a common scenario of clinical practice by experienced surgeons with similar annual primary THA volumes. Also acknowledged is the fact that interpreting radiographs is an inherently subjective process. We attempted to mitigate this difference by using one third party reader for all radiographs. Making a measurement of a 3D position from a 2D radiograph is also inherently flawed but is what we have used as a historical standard. According to Wan et al. [43], we defined radiographic inclination and anteversion based on the coronal plane of the patient, as seen on the anteroposterior pelvic radiograph, but pelvic tilt and rotation have been shown to alter appearances greatly on radiographs, accounting for varied readings of angles and measurements. As this is a multicenter study across continents with many different radiology technicians taking films, patient position was likely not uniform, despite training all for standardization.
As a result of trying to interpret and place the cup as accurately as possible, newer techniques have started to become more popular such as using live fluoroscopy in the operating room, as well as using computer navigation. Both techniques are not without their own issues though, including a learning curve for use, increasing time in the operating room, issues for surgeons confident in operating on lateral decubitus, and adding a substantial cost to the procedure.
Conclusion
Acetabular cup position is a critical factor in THA. This study shows that with traditional methods of placing the cup intraoperatively, and by using traditional radiographic interpretation postoperatively, surgeons are only accurate 53.1% of the time with regard to both inclination and version, compared with a predicted preoperative plan. As more factors continue to become apparently increasingly important for patient outcomes, such as spinopelvic characteristics, the accuracy of cup placement will become more crucial. This study suggests that incorporating techniques to improve accuracy in the placement of the cup is also important to consider.
Availability of data and materials
Data will be made available on reasonable request.
References
Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stockl B (2005) Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Joint Surg Br 87(6):762
Dudda M, Gueleryuez A, Gautier E, Busato A, Roeder C (2010) Risk factors for early dislocation after total hip arthroplasty: a matched case–control study. J Orthop Surg (Hong Kong) 18(2):179
Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ (1998) Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty 13(5):530
Yamaguchi M, Akisue T, Bauer TW, Hashimoto Y (2000) The spatial location of impingement in total hip arthroplasty. J Arthroplasty 15(3):305
Korduba LA, Essner A, Pivec R, Lancin P, Mont MA, Wang A, Delanois RE (2014) Effect of acetabular cup abduction angle on wear of ultrahigh-molecular-weight polyethylene in hip simulator testing. Am J Orthop (Belle Mead NJ) 43(10):466
Patil S, Bergula A, Chen PC, Colwell CW Jr, D’Lima DD (2003) Polyethylene wear and acetabular component orientation. J Bone Joint Surg Am 85-A(Suppl 4):56
Tian JL, Sun L, Hu RY, Han W, Tian XB (2017) Correlation of cup inclination angle with liner wear for metal-on-polyethylene in hip primary arthroplasty. Orthop Surg 9(2):186
Korhonen RK, Koistinen A, Konttinen YT, Santavirta SS, Lappalainen R (2005) The effect of geometry and abduction angle on the stresses in cemented UHMWPE acetabular cups–finite element simulations and experimental tests. Biomed Eng Online 4:32
Hart AJ, Ilo K, Underwood R, Cann P, Henckel J, Lewis A, Cobb J, Skinner J (2011) The relationship between the angle of version and rate of wear of retrieved metal-on-metal resurfacings: a prospective, CT-based study. J Bone Joint Surg Br 93(3):315
Hart AJ, Muirhead-Allwood S, Porter M, Matthies A, Ilo K, Maggiore P, Underwood R, Cann P, Cobb J, Skinner JA (2013) Which factors determine the wear rate of large-diameter metal-on-metal hip replacements? Multivariate analysis of two hundred and seventy-six components. J Bone Joint Surg Am 95(8):678
Angadji A, Royle M, Collins SN, Shelton JC (2009) Influence of cup orientation on the wear performance of metal-on-metal hip replacements. Proc Inst Mech Eng Part H 223(4):449
De Haan R, Pattyn C, Gill HS, Murray DW, Campbell PA, De Smet K (2008) Correlation between inclination of the acetabular component and metal ion levels in metal-on-metal hip resurfacing replacement. J Bone Joint Surg Br 90(10):1291
Langton DJ, Jameson SS, Joyce TJ, Webb J, Nargol AV (2008) The effect of component size and orientation on the concentrations of metal ions after resurfacing arthroplasty of the hip. J Bone Joint Surg Br 90(9):1143
Kosak R, Kralj-Iglic V, Iglic A, Daniel M (2011) Polyethylene wear is related to patient-specific contact stress in THA. Clin Orthop Relat Res 469(12):3415
Little NJ, Busch CA, Gallagher JA, Rorabeck CH, Bourne RB (2009) Acetabular polyethylene wear and acetabular inclination and femoral offset. Clin Orthop Relat Res 467(11):2895
Affatato S, Traina F, Mazzega-Fabbro C, Sergo V, Viceconti M (2009) Is ceramic-on-ceramic squeaking phenomenon reproducible in vitro? A long-term simulator study under severe conditions. J Biomed Mater Res B Appl Biomater 91(1):264
Dalla Pria PZL, Esopi P, Masoni D (2010) Breakage and noises in ceramic on ceramic couplings. Eur Orthop Traumatol 1(2):53
Bonnin MP, Archbold PH, Basiglini L, Selmi TA, Beverland DE (2011) Should the acetabular cup be medialised in total hip arthroplasty. Hip Int 21(4):428
Kiyama T, Naito M, Shitama H, Maeyama A (2009) Effect of superior placement of the hip center on abductor muscle strength in total hip arthroplasty. J Arthroplasty 24(2):240
Parvizi J, Sharkey PF, Bissett GA, Rothman RH, Hozack WJ (2003) Surgical treatment of limb-length discrepancy following total hip arthroplasty. J Bone Joint Surg Am 85(12):2310
Bader RJ, Steinhauser E, Willmann G, Gradinger R (2001) The effects of implant position, design and wear on the range of motion after total hip arthroplasty. Hip Int 11(2):80
Widmer KH (2007) Containment versus impingement: finding a compromise for cup placement in total hip arthroplasty. Int Orthop 31(Suppl 1):S29
Barrack RL, Krempec JA, Clohisy JC, McDonald DJ, Ricci WM, Ruh EL, Nunley RM (2013) Accuracy of acetabular component position in hip arthroplasty. J Bone Joint Surg Am 95(19):1760
Elson LC, Barr CJ, Chandran SE, Hansen VJ, Malchau H, Kwon YM (2013) Are morbidly obese patients undergoing total hip arthroplasty at an increased risk for component malpositioning? J Arthroplasty 28(8 Suppl):41
Callanan MC, Jarrett B, Bragdon CR, Zurakowski D, Rubash HE, Freiberg AA, Malchau H (2011) The John Charnley Award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res 469(2):319
Todkar M (2008) Obesity does not necessarily affect the accuracy of acetabular cup implantation in total hip replacement. Acta Orthop Belg 74(2):206
Reize P, Geiger EV, Suckel A, Rudert M, Wulker N (2008) Influence of surgical experience on accuracy of acetabular cup positioning in total hip arthroplasty. Am J Orthop (Belle Mead NJ) 37(7):360
Pirard E, De Lint JA (2007) Anteversion of the acetabular component in obese patients. Hip Int 17(2):99
Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR (1978) Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 60(2):217
Abdel MP, von Roth P, Jennings MT, Hanssen AD, Pagnano MW (2016) What safe zone? The vast majority of dislocated THAs are within the lewinnek safe zone for acetabular component position. Clin Orthop Relat Res 474(2):386
Danoff JR, Bobman JT, Cunn G, Murtaugh T, Gorroochurn P, Geller JA, Macaulay W (2016) Redefining the acetabular component safe zone for posterior approach total hip arthroplasty. J Arthroplasty 31(2):506
Murphy WS, Yun HH, Hayden B, Kowal JH, Murphy SB (2018) The safe zone range for cup anteversion is narrower than for inclination in THA. Clin Orthop Relat Res 476(2):325
Reina N, Putman S, Desmarchelier R, Sari Ali E, Chiron P, Ollivier M, Jenny JY, Waast D, Mabit C, de Thomasson E, Schwartz C, Oger P, Gayet LE, Migaud H, Ramdane N, Fessy MH (2017) Can a target zone safer than Lewinnek’s safe zone be defined to prevent instability of total hip arthroplasties? Case–control study of 56 dislocated THA and 93 matched controls. Orthop Traumatol Surg Res 103(5):657
DelSole EM, Vigdorchik JM, Schwarzkopf R, Errico TJ, Buckland AJ (1910) Total hip arthroplasty in the spinal deformity population: does degree of sagittal deformity affect rates of safe zone placement, instability, or revision? J Arthroplasty 32(6):2017
Vigdorchik JM, Sharma AK, Madurawe CS, Pierrepont JW, Dennis DA, Shimmin AJ (2021) Prevalence of risk factors for adverse spinopelvic mobility among patients undergoing total hip arthroplasty. J Arthroplasty 36(7):2371
Zagra L, Benazzo F, Dallari D, Falez F, Solarino G, D’Apolito R, Castelli CC (2022) Current concepts in hip-spine relationships: making them practical for total hip arthroplasty. EFORT Open Rev 7(1):59
Meermans G, Grammatopoulos G, Innmann M, Beverland D (2022) Cup placement in primary total hip arthroplasty: how to get it right without navigation or robotics. EFORT Open Rev 7(6):365
Murray DW (1993) The definition and measurement of acetabular orientation. J Bone Joint Surg Br 75(2):228
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51(4):737
Rabin R, de Charro F (2001) EQ-5D: a measure of health status from the EuroQol Group. Ann Med 33(5):337
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, Bonsel G, Badia X (2011) Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 20(10):1727
Behrend H, Giesinger K, Giesinger JM, Kuster MS (2012) The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty 27(3):430
Wan Z, Malik A, Jaramaz B, Chao L, Dorr LD (2009) Imaging and navigation measurement of acetabular component position in THA. Clin Orthop Relat Res 467(1):32
Siebenrock KA, Kalbermatten DF, Ganz R (2003) Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res 407:241
Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, Siebenrock KA (2005) Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res 438:182
Meermans G, Malik A, Witt J, Haddad F (2011) Preoperative radiographic assessment of limb-length discrepancy in total hip arthroplasty. Clin Orthop Relat Res 469(6):1677
Elkins JM, Callaghan JJ, Brown TD (2015) The 2014 Frank Stinchfield Award: the “landing zone” for wear and stability in total hip arthroplasty is smaller than we thought: a computational analysis. Clin Orthop Relat Res 473(2):441
Seagrave KG, Troelsen A, Malchau H, Husted H, Gromov K (2017) Acetabular cup position and risk of dislocation in primary total hip arthroplasty. Acta Orthop 88(1):10
Bosker BH, Verheyen CC, Horstmann WG, Tulp NJ (2007) Poor accuracy of freehand cup positioning during total hip arthroplasty. Arch Orthop Trauma Surg 127(5):375
Digioia AM 3rd, Jaramaz B, Plakseychuk AY, Moody JE Jr, Nikou C, Labarca RS, Levison TJ, Picard F (2002) Comparison of a mechanical acetabular alignment guide with computer placement of the socket. J Arthroplasty 17(3):359
Hassan DM, Johnston GH, Dust WN, Watson G, Dolovich AT (1998) Accuracy of intraoperative assessment of acetabular prosthesis placement. J Arthroplasty 13(1):80
Leichtle U, Gosselke N, Wirth CJ, Rudert M (2007) Radiologic evaluation of cup placement variation in conventional total hip arthroplasty. Rofo 179(1):46
Saxler G, Marx A, Vandevelde D, Langlotz U, Tannast M, Wiese M, Michaelis U, Kemper G, Grutzner PA, Steffen R, von Knoch M, Holland-Letz T, Bernsmann K (2004) The accuracy of free-hand cup positioning—a CT based measurement of cup placement in 105 total hip arthroplasties. Int Orthop 28(4):198
Funding
This study was funded by: Medical Device Business Services, Inc. 700 Orthopaedic Drive, Warsaw, Indiana 46581. This study was funded by DePuy Synthes (Johnson & Johnson).
Author information
Authors and Affiliations
Contributions
G.M. conducted study surgeries, data acquisition, contributed to data analysis, and helped draft the manuscript. D.F. contributed to study design, data analysis, and helped draft the manuscript. L.Z. conducted study surgeries, data acquisition, contributed to data analysis, and reviewed the manuscript. R.H.M.t.B. conducted study surgeries, data acquisition, contributed to data analysis, and reviewed the manuscript. K.J. conducted study surgeries, data acquisition, contributed to data analysis, and reviewed the manuscript. T.B. performed the statistical analysis and reviewed the manuscript. H.C.T. conducted study surgeries, data acquisition, contributed to data analysis, and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Each Investigator has obtained approval of the local Institutional Review Board or Ethical committee prior to the consent of the first subject. The trial has been registered under Trial Registration Number NCT03189303.
Consent for publication
All authors have consented for publication of the data.
Competing interests
G.M., L.Z., R.H.M.tB., K.J., and H.C.T. received funding support from DePuy Synthes for this study. G.M. is a on the education committee of the European Hip Society. L.Z. is a paid consultant for DePuy Synthes, Medacta, Stryker, and 3M. R.H.M.tB. is the President of the Dutch Hip Society. K.J. is a paid consultant for DePuy Synthes. H.C.T. is the President and board member for the Southern Orthopaedic Association. D.F. and T.B. are employees of DePuy Synthes. D.F. holds share of stock in Johnson & Johnson.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Meermans, G., Fawley, D., Zagra, L. et al. Accuracy of cup placement compared with preoperative surgeon targets in primary total hip arthroplasty using standard instrumentation and techniques: a global, multicenter study. J Orthop Traumatol 25, 25 (2024). https://doi.org/10.1186/s10195-024-00766-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10195-024-00766-2