Abstract
Background
Cardiovascular Disease (CVD) is a major cause of mortality worldwide. Control and reduction of cardiovascular risk factors such as elevated blood pressure, high cholesterol levels, excess of body weight, smoking and lack of exercise can contribute to a reduction of CVD mortality.
Methods
A standardized questionnaire was administered to all medical officers willing to participate in the study, who were working in the Cardiology Units all over Sri Lanka to assess the source of continuous medical education, attitudes on secondary prevention, barriers to secondary prevention and knowledge assessment of secondary prevention of cardiovascular diseases. Chi square was used to compare groups and p < 0.05 was considered significant.
Results
132 participants with equal numbers of males and female doctors participated. While 56 doctors have had no training in cardiology, 75 doctors have had some training in a cardiology unit. The barriers for secondary prevention were, poor knowledge/understanding of patients 3.82 (1.06), too many drugs 3.74 (0.98), presence of co-morbid conditions 3.68(0.97), cost of medications 3.69 (0.97) and poor adherence to prevention strategies by patients 3.44 (1.15). Routine clinic visits 85 (65%) and public awareness day seminars 30 (22.2%) were the most effective methods of secondary prevention. Guidelines were the most popular method of continuous medical education. Those who have had some training in cardiology did not differ in their knowledge from those who have never had training in cardiology. Knowledge about prevention with regard to diet was inadequate and exercise and lipids were adequate but not good. Rates of knowledge on smoking cessation were much higher than for other CVD risk factors.
Conclusion
There needs to be more adherences to clinical guidelines and attention paid to CVD prevention, in particular, the importance of dietary modifications, adequate exercise, and lipid control.
Similar content being viewed by others
Background
Cardiovascular Disease (CVD) is a major cause of mortality worldwide. Studies have proven that control and reduction of cardiovascular risk factors such as elevated blood pressure, high cholesterol levels, excess of body weight, smoking and lack of exercise can contribute to a reduction of CVD mortality of around 40-60% [1].
To optimally manage the risk factors for CVD, the risk factors must be identified. This will enable risk stratification of patients with CVD. There are different risk estimation scores: SCORE [2], Framingham [3] and ASSIGN–SCORE [4]. Risk factor estimations are important as atherosclerosis is a multifactorial disease. These risk estimation scores are built on the ideal target levels for each risk factor. The targets are values at which each risk factor control is started. A group of modestly deranged risk factors can result in a higher total risk than a single deranged risk factor as multiple risk factors give multipliable and additive risk [5]. A clinically useful CVD risk-estimation system should be methodologically robust, easy to use and should have a beneficial outcome [5]. Though risk factor estimation systems should theoretically improve outcomes, not many studies have proven the above [5]. Therefore as of now, until the actual benefits of risk-factor estimation systems can be proven, everyday clinical practice should involve the assessment of risk factors and control of them. In order to control risk factors one needs to be aware of the target level for each factor. Though at present there are no studies done to prove that knowing the targets for each risk factor is beneficial, knowing the targets for each risk factor would enable physicians to participate to secondary prevention in an active way. The concept of controlling each risk factor at a particular threshold is a controversial concept as CVD risk is a continuum [6]. Yet until further trials are available comparing the effects of controlling individual risk factors versus total risk factor control of a patient, it is wise to control a risk factor once identified.
The targets for risk factors control change from time to time. They are the result of extensive of clinical research. In an attempt to standardize and improve care, international health agencies have published guidelines for secondary prevention of cardiovascular risk factors. The European Society of Cardiology and American Heart Association [7], National High Blood Pressure Education Program committee (JNC 7) [8], and National Cholesterol Education Panel (ATP III) [9] are some of them.
Studies assessing the knowledge and efforts of doctors in secondary prevention have found that doctors do not stress enough on the role of secondary prevention to their patients [10]. Lack of awareness about prevention guidelines [11] and lack of motivation [12] could be possible reasons. The lack of adherence to guidelines leads to erroneous or suboptimal management of risk factors.
The objectives of this study were to assess the knowledge on secondary prevention among medical officers, to find out the methods of Continuous medical education (CME) among medical officers and to find out their perceived role in risk factor prevention.
CME is one powerful method of bridging the gap between evidence based medicine and clinical practice. Ongoing CME is an important area for the maintenance of good quality clinical care [13]. In most countries in South Asia, though there are various continuing medical education programs, there is no revalidation process and no established system of awarding credits for educational activities [14]. Sri Lanka is a developing country and there is no established compulsory continuous medical education program or revalidation process in Sri Lanka at present. There is a National Continuous Professional Development Program, which is voluntary [14, 15]. There is a dearth of data from Sri Lanka on the impact of continuing medical education programs in general. No studies have been done on knowledge assessment on secondary prevention of cardiovascular disease in Sri Lanka. This study hopes to fulfill the above objectives with the aim of better secondary prevention of cardiovascular risk factors in the country.
Methods
Ethical clearance was obtained from the Ethical Review Committee of the National Hospital of Sri Lanka (NHSL). A standardized questionnaire (Additional file 1: Questionnaire) was administered to all medical officers who were working in the Cardiology Units all over Sri Lanka and the medical officers working in the medical wards of the National Hospital of Sri Lanka. Informed consent was obtained. All participants who were willing to take part were administered the questionnaire.
Development of questionnaire
The questionnaire consisted of three parts.
Part 1 - Demographic details of the participants
Part 2 - Source of CME
Part 3 - Attitudes on secondary prevention. Barriers to secondary prevention were given and the participants were asked to rate on a 1–5 likert scale. 1 been not a significant barrier and 5 been very significant barrier.
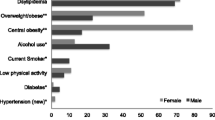
Part4 - Knowledge assessment of secondary prevention. This part was further subdivided in to prevention of smoking, blood pressure control, lipids, dietary management, alcohol use, physical activity, weight, management of diabetes, drugs therapy. This included questions regarding the targets for optimal control for each of the above and important questions on prevention. They were open ended questions.
The questionnaire was developed by the authors who included a Senior Consultant cardiologist. The targets expected were based on the present guidelines applicable at the time of study namely: AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients With Coronary and Other Atherosclerotic Vascular Disease: 2011 Update [7], National High Blood Pressure Education Program committee (JNC 7) [8], and National Cholesterol Education Panel (ATP III) [9] and ACCORD trial.
Statistical analysis was done using SPSS V.17.0 (SPSS inc. Chicago, IL). Chi square and t test was used for data analysis. The level of significance was <0.05.
Results
Participant characteristics
A total of 132 participants with equal numbers of male and female doctors responded to the questionnaire. The majority of the participants were in the age group of 30–40 years. The mean age was 33. The number of doctors in a post graduate training program (Registrars and Senior Registrars) was 41. While 56 doctors have had no training in cardiology, 75 doctors have had some training in a cardiology unit. The demographic details are given in Table 1.
Awareness about guidelines and barriers to adherence
Among the leading reasons the participants sighted as barriers for secondary prevention were, poor knowledge/understanding of patients 3.82 (1.06), too many drugs 3.74 (0.98), presence of co-morbid conditions 3.68(0.97), cost of medications 3.69 (0.97) and poor adherence to prevention strategies by patients 3.44 (1.15). The barriers to guideline adherence given by participants are listed in Table 2.
Routine clinic visits 85 (65%) and public awareness day seminars 30 (22.2%) were the most effective methods of secondary prevention. Guidelines were the most popular method of continuous medical education among the participants (Table 2).
Lifestyle, smoking recommendations and lipids, diabetes and blood pressure management
The knowledge and adherence to guideline recommendation on lifestyle modification, smoking prevention, lipid, blood pressure and diabetes management are given in Table 3.
A modest number of participants 40(29.6%) advised patients to engage in physical activity more than 5 times a week as recommended by the guidelines. The minimum duration of 30 minutes was also a well known factor among this group of doctors (58.5%).
A significant proportion of participants identified blood pressure targets set up by the AHA for general population, but the targets for patients with Diabetes and Kidney disease were not identified as frequently as the above.
About 40.7% participants identified the LDL target of 100 mg/dl as ideal but only 18% were able to give the correct dose of Atorvastatin for treatment. There was moderate understanding about triglyceride level management as only 21% were able to give the target at which treatment should be started before a statin.
Majority of doctors did not specify the exact targets for fat intake. The overall response rates for fat intake been all less than 10.4%. The recommended alcohol intake for men (36.3%) and women (37.8%) both were identified by a significant number of participants.
The waist circumference cut off specific for Asians were identified by a 24.5% and 20.7% of doctors. The goal of HBAIC of 7 was correctly identified by 62 (5.9%) of the participants.
The use of Aspirin and Clopidogrel was well known among the participants and there was a response over 80% about the correct dose and duration of Aspirin. The knowledge about the duration of Clopidogrel was only 29%.
When comparing the two groups of participants, those who have had some training in cardiology versus those who have never had training in cardiology, there was no difference in the level of knowledge.
Discussion
There are issues with regard to the generizability of studies done on knowledge assessment. This preliminary study on the knowledge on secondary prevention of cardiovascular diseases among medical officers is the first of its kind done in Sri Lanka and it reveals several important findings. The findings are relevant in three areas: the level of knowledge on secondary prevention among medical officers, strategies and obstacles to secondary prevention and methods of CME used by doctors.
Knowledge on secondary prevention
Counseling may be an effective tool in reducing behavioral risk factors for CVD. Yet, doctors do not counsel their patients aggressively about lifestyle changes to prevent CVD. In our study the knowledge about prevention with regard to diet was inadequate and exercise and lipids were adequate but not good. Rates of knowledge on smoking cessation was much higher than for other CVD risk factors, a finding which has been reported by others [16]. Only a handful of physicians knew about the exact dietary recommendations for fat and salt and the frequency of exercise needs. Over the past few decades there has been a consistent need for the change of dietary habits to prevent cardiovascular deaths. This has been addressed in many leading papers on the subject [17]. Yet the knowledge on the dietary recommendation still remains poor. This calls for a more vigorous shift in the attitudes and knowledge of doctors on dietary recommendations. Over 90% asked about tobacco use at the initial visit and over 50% advised on quitting smoking. The knowledge on secondary prevention of smoking was excellent.
Our study also indicated there is more education needed in blood sugar control targets and blood pressure targets as evidence by a similar study done in USA [18] Blood pressure control plays a vital role in the prevention of CVD. In a recent meta-analysis it was found that blood pressure reduction of 10 mmHg systolic or 5 mmHg diastolic reduced the rate of coronary heart disease by 22% [19].
Lower the serum LDL-cholesterol level, the better it is for cardiovascular disease prevention [20]. Yet not many doctors identified the importance of proper lipid control and they were not certain about the targets for lipid control. The kowledge on lipids was inadequate. This was also revealed by a study done by Freedman et al. In another study done in Germany the knowledge on lipid control was similar to our study [16]. There need to be more educational activities to ensure doctors practice the lipid control guidelines more accurately.
The benefit of Clopidogrel for secondary prevention after an episode of acute coronary syndrome had been shown by many multicentre clinical trials [21]. Yet the duration of Clopidogrel use is not very clear in literature and our respondents were doubtful about the appropriate duration of it. This shows that more emphasis needs to be made on the introduction of evidence based medicine to our setting.
The limited adherence shown to clinical guidelines has been termed clinical inertia. The reasons that could contribute to inertia are doctors overestimating the quality of the care they actually provide, lack of training, and use of “soft excuses” to avoid intervention [22]. In our study we found there was very little clinical inertia when it came to prescribing beta blockers and ACE inhibitors, two drug classes which have morbidity and mortality benefit cardiovascular disease prevention. In our study most doctors (>60%) knew the exact indications for beta blockers and ACE Inhibitors. It is therefore safe to assume they would be prescribing it to all patients who need both the classes of drugs.
This study also showed that awareness and incorporation of CVD prevention did not differ by the training doctors received. The doctors who have not received cardiology training were equally knowledgeable as those who hadn’t received training. Our study explored whether physician training level was predictive of adherence to guidelines. The data form Friedman et al. found that attending physicians and resident physicians did not differ in prevention counseling. The reasons given were that attending physicians did not believe in physician counseling and also were not very knowledgeable in the present guidelines [23].
Strategies of secondary prevention
There is gap in what is mentioned in clinical guidelines and what is practiced in the sphere of secondary prevention in CVD. The real issue in cardiovascular medicine is implementation of these recommendations into clinical practice [24]. In an attempt to bridge this gap, heath care providers and patients both need to take action [25]. Though there are several available methods of secondary prevention, not many are evidenced based. Until such time evidence becomes available it is wise to take in to account what the physicians think are the most appropriate methods and utilize them to educate patients. When asked from doctors in our study clinic visits were the best approach to educate patients. This is in contrast to the popular belief that a one to one consultation with a consultant or specialist is more useful. Regular clinic visits allowed a proper follow up plan to be implemented. The value of clinics in secondary prevention has been reported elsewhere in the world. A day clinic where patients are educated regarding secondary prevention has found to be very effective [26]. Yet the difference in these clinics done elsewhere in the world, they have less volume of patients, the clinic is primarily focused on secondary prevention and special lectures on atherogenesis and nutrition and an individualized care plan is made at the end of the day. To uplift the status of the secondary prevention in our country will be a difficult task only through clinics because our clinics cater to a massive number of patients, limited time available to devote for each patient and the clinics are mainly run by doctors with no involvement of nursing staff who could be useful in advising patients.
Therapeutic patient education [27] might be one method a country like Sri Lanka should try implementing. Sri Lanka has Cardiac Rehabilitation Programs in several leading hospitals. These have proven to be effective which indicates patients should be and can be used effectively for secondary prevention of CVD [28].
Barriers to secondary prevention
Over time, studies done all over the world have highlighted several obstacles for optimal cardiovascular disease prevention. The main obstacles identified were lack of time [23], lack of understanding of patients about the disease and adherence to life style modifications [18], the high cost of medication and inadequate time for counseling [29]. The main barriers to secondary preventions as seen by doctors in our study were: poor knowledge of the patients, too many drugs and high cost of medications and the fact that patient values acute care more than preventive care. These barriers were common to Europe as well as Asia as evident by the REACT study [23, 30]. Sri Lanka is still a developing country and the majority of patients who utilize the free health care system are not advanced enough to look up and read about their illnesses and learn about them. Poor knowledge of patients was considered a major problem by our respondents. Lack of knowledge is a significant barrier in developing nations [30]. Patients participation been crucial to CVD prevention has been highlighted by studies before [16, 18]. In order to overcome the barriers in our setting several important measures could be implemented. We can learn from studies which have proven the efficacy of these methods [30]. To educate patients, patent information leaflets can be utilized. Self care diary maintenance can be promoted. Sri Lanka at present does not have an official referral and counter referral system and any patient can seek treatment from any government or private sector health care facility as and when they wish. This leads to overcrowding of tertiary care centers which leads to less time spent on patients. An organized referral and counter referral system if implemented can bring a drastic improvement in the patient care system as duplication of work will be avoided and patients will be given more care which is continuous.
Continuous medical education
Practice guidelines were found to be the most common method of CME in our study. This is in contrast to some studies done previously [31]. CME resources are one of the second commonest sources of knowledge in our study population. CME was preferred over clinical practice guidelines in studies done elsewhere [20]. CME programs are always found to be useful to educate and keep the practicing medical officers up-to-date on the new developments in the field. This highlights the need for improvement in the CME programs in the country [32].
Limitations and future directions
Our study was small. The questionnaire was not subjected to validity tests. The results may not be generalizable to all physicians in the country. Our study also lacked the power to examine whether barriers to treatment varied by age, gender, or race/ethnicity of the physician. However, since our findings indicate a low level of adherence to guidelines, this adds weight to the concern that doctors may be under counseling for CVD prevention. Further larger studies should be carried out to follow up patient’s long term and determine the effect of risk factor control on morbidity and mortality of CVD.
Conclusion
Overall, this study highlights the need for more CME among doctors to improve secondary prevention of cardiovascular diseases. It also highlights the need for a more robust setup at state hospitals to incorporate nursing staff and other health professionals in running clinics. This might help provide a more qualitative service to patients. Passive dissemination of information is not enough for cardiovascular prevention. Logistically and financially there needs to be a system in place so physicians can exercise proper secondary prevention activities and as highlighted before by many studies more aggressive CME are needed and the mere existence of guidelines will never be enough.
In summary, our study adds to the growing body of literature there needs to be more adherences to clinical guidelines and attention paid to CVD prevention, and, in particular, the importance of diet, exercise, and lipid control. Most importantly, our study did not find any differences in counseling practices between those who have training in cardiology versus those who did not have training finding that highlights the need to create more educational activities to educate both groups.
Abbreviations
- CVD:
-
Cardiovascular disease
- CME:
-
Continuous medical education
- SBP:
-
Systolic blood pressure
- DM:
-
Diabetes mellitus
- CKD:
-
Chronic kidney disease
- LDL:
-
Low density lipoproteins.
References
Institute of Medicine (US) Committee on Preventing the Global Epidemic of Cardiovascular Disease: Meeting the Challenges in Developing Countries. Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health. Edited by: Fuster VKB. 2010, Washington (DC): National Academies Press (US), 2, Epidemiology of Cardiovascular Disease. Available from: http://www.ncbi.nlm.nih.gov/books/NBK45688/
Conroy RM, Pyorala K, Fitzgerald AP, Sans S, Menotti A, De Backer G, De Bacquer D, Ducimetiere P, Jousilahti P, Keil U, Njolstad I, Oganov RG, Thomsen T, Tunstall-Pedoe H, Tverdal A, Wedel H, Whincup P, Wilhelmsen L, Graham IM: Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003, 24: 987-1003. 10.1016/S0195-668X(03)00114-3.
D'Agostino RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB: General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008, 117: 743-753. 10.1161/CIRCULATIONAHA.107.699579.
Woodward M, Brindle P, Tunstall-Pedoe H: Adding social deprivation and family history to cardiovascular risk assessment: the ASSIGN score from the Scottish Heart Health Extended Cohort (SHHEC). Heart. 2007, 93: 172-176.
Lloyd-Jones DM: Cardiovascular risk prediction: basic concepts, current status, and future directions. Circulation. 2010, 121: 1768-1777. 10.1161/CIRCULATIONAHA.109.849166.
Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren WM, Albus C, Benlian P, Boysen G, Cifkova R, Deaton C, Ebrahim S, Fisher M, Germano G, Hobbs R, Hoes A, Karadeniz S, Mezzani A, Prescott E, Ryden L, Scherer M, Syvanne M, Scholte Op Reimer WJ, Vrints C, Wood D, Zamorano JL, Zannad F: European Guidelines on cardiovascular disease prevention in clinical practice (version 2012): The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Atherosclerosis. 2012, 223: 1-68. 10.1016/j.atherosclerosis.2012.05.007.
Smith SC, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, Gibbons RJ, Grundy SM, Hiratzka LF, Jones DW, Lloyd-Jones DM, Minissian M, Mosca L, Peterson ED, Sacco RL, Spertus J, Stein JH, Taubert KA: AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol. 2011, 58: 2432-2446. 10.1016/j.jacc.2011.10.824.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, Roccella EJ: The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003, 289 (19): 2560-2572. 10.1001/jama.289.19.2560.
National Cholesterol Education Program (NCEP) Expert Panel on Detection E, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III): Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002, 106 (25): 3143-3421.
Filippi A, Buda S, Brignoli O, Cricelli C, Degli Espositi E: Global cardiovascular risk evaluation in Italy: a cross-sectional survey in general practice. Ital Heart J Suppl. 2004, 5: 223-227.
Hyman DJ, Pavlik VN: Self-reported hypertension treatment practices among primary care physicians: blood pressure thresholds, drug choices, and the role of guidelines and evidence-based medicine. Arch Intern Med. 2000, 160: 2281-2286. 10.1001/archinte.160.15.2281.
Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, Rubin HR: Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999, 282: 1458-1465. 10.1001/jama.282.15.1458.
Peck C, McCall M, McLaren B, Rotem T: Continuing medical education and continuing professional development: international comparisons. Bmj. 2000, 320: 432-435. 10.1136/bmj.320.7232.432.
Mendis LABV, Adhikari RK, Muzaherul Huq M, Qureshi AF: Postgraduate medical education in South Asia: Time to move on from the postcolonial era. BMJ. 2004, 328 (7443): 779-10.1136/bmj.328.7443.779.
Epa SS: Revalidation of Sri Lankan doctors. Ceylon Med J. 2003, 48: 65-67.
Heidrich J, Behrens T, Raspe F, Keil U: Knowledge and perception of guidelines and secondary prevention of coronary heart disease among general practitioners and internists. Results from a physician survey in Germany. Eur J Cardiovasc Prev Rehabil. 2005, 12: 521-529.
Willett WC, Stampfer MJ: Rebuilding the food pyramid. Sci Am. 2003, 288: 64-71. 10.1038/scientificamerican0103-64.
Mosca L, Linfante AH, Benjamin EJ, Berra K, Hayes SN, Walsh BW, Fabunmi RP, Kwan J, Mills T, Simpson SL: National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation. 2005, 111: 499-510. 10.1161/01.CIR.0000154568.43333.82.
Law MR, Morris JK, Wald NJ: Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009, 338: b1665-10.1136/bmj.b1665.
Doroodchi H, Abdolrasulnia M, Foster JA, Foster E, Turakhia MP, Skelding KA, Sagar K, Casebeer LL: Knowledge and attitudes of primary care physicians in the management of patients at risk for cardiovascular events. BMC Family Practice. 2008, 9: 42-10.1186/1471-2296-9-42.
Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK: Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001, 345: 494-502.
Reinharth D: Clinical inertia. Ann Intern Med. 2002, 137: 547-548. 10.7326/0003-4819-137-6-200209170-00025. author reply 547–548
Hobbs FD, Erhardt L: Acceptance of guideline recommendations and perceived implementation of coronary heart disease prevention among primary care physicians in five European countries: the Reassessing European Attitudes about Cardiovascular Treatment (REACT) survey. Fam Pract. 2002, 19: 596-604. 10.1093/fampra/19.6.596.
Wood D: Guidelines and global risk: a European perspective. Eur Heart J. 2002, 4: F12-F18.
Kiessling A: Participatory learning: a Swedish perspective. Heart. 2004, 90 (1): 113-116. 10.1136/heart.90.1.113.
Timmerman MK, Rensing KL, Giral P, Cramer MJ, Bruckert E, Twickler TB: Lessons from france: the cardiovascular prevention clinic in the la pitie-salpetriere hospital in paris. Neth Heart J. 2007, 15: 22-26.
2014: Therapeutic Patient Education, Continuing Education Programmes for Health Care Providers in the Field of Prevention of Chronic Diseases, Report of a WHO Working Group. 1998, http://www.euro.who.int/__data/assets/pdf_file/0007/145294/E63674.pdf. Last accessed on 3rd of June 2014
Pinidiyapathirage MJ, Wickremasinghe AR, Mendis S: The Role of a Cardiac Rehabilitation Programme on Risk Modification in Patients with Established Coronary Heart Disease Department of Public Health, Faculty ofMedicine, University ofKelaniya, Institute of Cardiology, National Hospital of Sri Lanka, Colombo 10. University of Kelaniya: Proceedings of the Annual Research Symposium 2007- Faculty of Graduate Studies, http://www.kln.ac.lk/uokr/ARS2007/5.1.pdf. Last accessed on 3rd of June 2014
Doroodchi H, Abdolrasulnia M, Foster JA, Foster E, Turakhia MP, Skelding KA, Sagar K, Casebeer LL: Knowledge and attitudes of primary care physicians in the management of patients at risk for cardiovascular events. BMC Fam Pract. 2008, 9: 42-10.1186/1471-2296-9-42.
Ferrante D, Konfino J, Linetzky B, Tambussi A, Laspiur S: Barriers to prevention of cardiovascular disease in primary care settings in Argentina. Rev Panam Salud Publica. 2013, 33: 259-266. 10.1590/S1020-49892013000400004.
Grant A, Niyonsenga T, Isabelle D, Elisabeth D, Marianne X, Roch B: Physician attitudes toward prevention and treatment. Canadian Family Physician. 1998, 44: 780-788.
O'Keefe CE, Hahn DF, Betts NM: Physicians' perspectives on cholesterol and heart disease. J Am Diet Assoc. 1991, 91: 189-192.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-6920/14/113/prepub
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
All authors were involved in planning, data collection, analysis of data and writing the manuscript. All authors read and approved the final manuscript.
Electronic supplementary material
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Matthias, A.T., Lokunarangoda, N.C. & Ekanayaka, R. Knowledge assessment regarding secondary prevention of coronary heart disease- a multi centre survey. BMC Med Educ 14, 113 (2014). https://doi.org/10.1186/1472-6920-14-113
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1472-6920-14-113