Abstract
Several mitochondrial DNA (mtDNA) mutations of Leber's hereditary optic neuropathy (LHON) have been reported in patients with multiple sclerosis (MS) from different ethnicities. To further study the involvement of LHON mtDNA mutations in MS in the Arab population, we analyzed sequencing data of the entire mitochondrial genome from 47 unrelated Saudi individuals, 23 patients with relapse-remitting MS (RRMS) and 24 healthy controls. Ten LHON mutations/variants were detected in the patients but were absent in the controls. Of them, the common primary pathogenic mutation m.14484T>C and the rare mutation m.10237T>C were found in one patient, whereas the rare mutation m.9101T>C was found in another patient. The remaining were secondary single nucleotide variants (SNVs) found either in synergy with the primary/rare mutations or individually in other patients. Patients carrying LHON variants also exhibited distinct mtDNA variants throughout the mitochondrial genome, eight were previously reported in patients with LHON. Moreover, five other LHON-related SNVs differed significantly in their prevalence among patients and controls (P < 0.05). This study, the first to investigate LHON mtDNA mutations/variants in a Saudi cohort may suggest a role of these mutations/variants in the pathogenesis or genetic predisposition to MS, a possibility which needs to be explored further in a large-scale.
Similar content being viewed by others
Introduction
Multiple sclerosis (MS) is a progressive neurological disease characterized by autoimmune inflammation coupled with demyelination and neurodegeneration1,2. The disease which affects over two million people worldwide, is more common in females than in males2,3. The exact cause of MS is still unclear, but it is believed that genetic predisposition, epigenetic factors and various environmental factors such as infections, vitamin D deficiency, and smoking contribute significantly to the development of the disease4,5. These agents are able to trigger a cascade of events in the immune system including an accumulation of macrophages in microglia in the brain and lymphocytes in the white matter and the gray matter of the central nervous system (CNS), leading to demyelination and destruction of axons6.
In recent years, mitochondrial dysfunction has been shown to occur early in MS and plays an important role in the axonal degeneration and demyelination7,8,9. Abnormalities in the mitochondrial genome including defects in the mitochondrial DNA (mtDNA), altered mtDNA content and dysregulation of mitochondrial gene expression, which ultimately lead to increase production of free radical and oxidative damage, have all been reported in patients with MS9,10. The main role of mitochondria is to produce energy through oxidative phosphorylation (OXPHOS). The human mtDNA is a 16.6 kb circular double-stranded DNA molecule which encodes 13 OXPHOS proteins, 22 tRNA genes and 2 rRNA genes. The mtDNA-encoded genes include seven subunits of NADH dehydrogenase of complex I (ND 1, 2, 3, 4L, 4, 5 and 6); cytochrome b-c1 (CYB) of ubiquinol-cytochrome c reductase of complex III; three subunits of cytochrome c oxidase of complex IV (COI, II, III); and two subunits of mitochondrial ATP synthase of complex V (ATP6 and ATP8). Due to the multi-copy nature of the mitochondrial genome, some mutations affect all copies of the mtDNA (homoplasmic), whereas others only present in some copies of the mtDNA (heteroplasmic)11.
Multiple lines of evidence have suggested that mtDNA could play a role in MS. In this context, mutations and common polymorphisms in mtDNA have been reported in MS patients. For instance, variants in the ND2 gene and other mtDNA-encoded genes have been implicated in the susceptibility to MS12,13. Moreover, a previous study by our group identified four novel mutations in the mtDNA-encoded ND4 gene in patients with MS, which caused complex I dysfunction and could be implicated in the pathogenicity of MS14. Though the involvement of mtDNA in the pathogenesis of MS was initially proposed based on the observation of mother-to-child transmission in familial cases15,16, and the coexistence of symptoms of inflammatory demyelination similar to MS in Leber’s hereditary optic neuropathy (LHON), a maternally inherited mitochondrial blinding disorder caused by mtDNA mutations17.
One of three primary mutations m.3460G>A, m.11778G>A and m.14484T>C respectively affecting the MT-ND1, MT-ND4 and MT-ND6 subunit genes of NADH dehydrogenase (complex I) are present in more than 90% of all LHON cases18,19. Other mtDNA mutations that cause LHON appear to be relatively rare within the population and have been found in singleton cases or in a single family, and their strict pathogenicity awaiting further confirmation18,19. It has been shown that only about 50% of males and 10% of females who harbour pathogenic LHON mutations develop optic neuropathy20,21. This incomplete penetrance and gender bias of males being more affected than females imply that additional mitochondrial and nuclear genetic factors or environmental factors contribute to the phenotypic expression and severity of the disease18,19,20,21. On the other hand, a number of mtDNA variants known as “secondary mutations” have been shown to influence the penetrance and clinical expression of these primary mutations22,23,24. Secondary mutations have been also found at higher frequency in LHON patients than in controls and thus may play an additional role in the pathogenesis/risk of the disease22,23,24. In an early study to explore a possible connection between MS and LHON, Harding et al.17 described the primary mutation m.11778G>A in eight LHON women who developed neurological features compatible with a diagnosis of MS. This was followed by many other reports which verified the presence of primary LHON mutations in a sub-group of MS patients or patients with MS-like syndrome in the European and North American populations25,26,27,28. While a study by Vanopdenbosch et al.29 showed that the association of LHON primary mutations with MS is more than a coincidence and that carrying a primary mutation is a risk factor for developing MS, at least in Caucasian populations. In contrast, none of the most common LHON primary mutations were detected in Japanese or Korean patients with MS30,31. Additionally, certain sets of secondary LHON-related mDNA variants were found to contribute to the genetic susceptibility of MS in specific ethnic groups32,33. These observations suggest that the presence and relative frequencies of LHON variants vary among individuals of different ethnicities, possibly due to genetic, racial and other factors, which differ in different populations. Aside from these studies, no information is available on the incidence of LHON variants in MS patients in the Arab population. We recently sequenced the entire mitochondrial genome from unrelated Saudi Arab individuals including 23 patients with relapse-remitting MS (RRMS) and 24 healthy controls using next-generation sequencing (NGS), and we found several unique and common mtDNA mutations/variants34. In this study we analyzed the generated large-scale genomic sequence data of the entire mtDNA to investigate the presence of variants involved in or associated with LHON in this Saudi cohort. Knowledge about LHON-associated mtDNA variants can assist in the understanding of genetic contribution of LHON to the pathogenesis and genetic predisposition to MS.
Results
Characteristics of study subjects
The characteristics of 47 Saudi subjects including 23 patients diagnosed with RRMS according to McDonald diagnosis criteria35, and 24 healthy controls are illustrated in Table 1. The data are presented as number or mean ± standard deviation (SD). The patient group consisted of 5 males and 18 females. The mean age of the patient group was 28 ± 7.5 within a range between 18 and 44 years. The control group consisted of 5 males and 19 females. The mean age of the control group was 31 ± 7.5 within a range between 22 and 52 years. There were no significant differences between patients and controls in the mean age, sex distribution, mean BMI and mean blood pressure (P > 0.05). For patient group, the mean disease duration was 5.3 years ± 4 and ranged from 1 to 15 years, the mean EDSS was 3.9 ± 1.4 and ranged from 2 to 6.5. Most of the patients presented with numbness and visual problem (23 and 20 respectively). Eighteen patients had muscle spasticity, 13 patients had balance problem, 10 patients suffered from slurred speech and 14 patients suffered from a psychiatric condition, most commonly depression. The patients were under the following treatment: Avonex (n = 3), Betaferon (n = 8), Glienya (n = 3), Rebif (n = 5) and Tysabri (n = 4).
Analysis of mtDNA sequences in RRMS patients and healthy controls
We analyzed our recently generated large-scale genomic sequence data of the entire mitochondrial genome from 23 patients with RRMS and 24 healthy controls34. The mtDNA sequences from the patients and controls were compared to the revised rCRS and nucleotide variants recorded, and all mtDNA variants were submitted to the GenBank database34.
Identification of LHON mtDNA mutations/variants in RRMS patients
mtDNA variants were annotated using the MITOMAP database system for the human mitochondrial genome (http://www.mitomap.org/MITOMAP) and other databases, in which mtDNA variants are classified into three categories: Benign variants, unclassified variants or mutations36. Analysis of the entire mtDNA sequences in RRMS patients revealed ten single nucleotide variants (SNVs) described as missense mutations in protein-coding genes, which were detected in six patients. Details of these SNVs are shown in Table 2. All of the identified SNVs were previously reported in the MTOMAP and other databases to be associated with LHON. Of them, two pathogenic mutations were detected in one patient (P2) namely the primary homoplasmic mutation m.14484T>C in MT-ND6 gene and the rare heteroplasmic mutation m.10237T>C in MT-ND3 gene. Whereas one rare homoplasmic mutation namely m.9101T>C in MT-ATP6 gene was found in another patient (P15). Short reads mapped against mitochondrial genome of these mutations are shown in Fig. 1.
Seven other secondary variants, all in the homoplasmic state, were found either in synergy with the primary/rare mutations or individually in other patients. These include m.5442T>C in MT-ND2 gene and m.13105A>G in MT-ND5 gene, both were detected in patient P2; m.12358A>G in MT-ND5 gene was detected in patient P15. The remaining variants m.4695T>C in MT-ND2 gene, m.4917A>G in MT-ND2 gene, m.3316G>A in MT-ND1 gene and m.3533C>T in MT-ND1 were found in four other patients (P1, P16, P18 and P22) respectively. Bioinformatics analysis of the deleteriousness prediction of these variants using the PolyPhen2, SIFT, CADD, and Mutation Assessor models37 confirmed the pathogenicity of m.14484T>C and m.10237T>C mutations which were detected in patient P2, while all other variants were predicted as benign (Table 2).
Characteristics of RRMS patients carrying LHON mtDNA mutations/variants
Table 3 shows the characteristics of RRMS patients who harboured one of the LHON mutations/variants in mtDNA-encoding genes. Patient P2 was a 20 year-old male with a disease duration of 1 years and an EDSS of 3. He carried four variants; the primary mutation m.14484T>C in MT-ND6 gene, the rare mutation m.10237T>C in MT-ND3 gene, and the secondary variants m.5442T>C in MT-ND2 gene and m.13105A>G in MT-ND5 gene. Whereas patient P15 was a 27 year-old female with a disease duration of 3 years and an EDSS of 3. She carried the rare mutation m.9101T>C in MT-ATP6 gene and the secondary variant m.12358A>G in MT-ND5 gene. All other patients who carried secondary LHON-related variants were young adult females aged from 20 to 34 years old and had disease durations from 1 to 5 years and EDSS scales from 2.5 to 3.5. All of the patients were reported with numbness and visual problem along with other neurological dysfunctions.
Other variants in RRMS patients carrying LHON mtDNA mutations
We next investigated the presence of other variants in the six RRMS patients who carried one of the LHON mtDNA mutations. As shown in Table 4, the patients exhibited distinct SNVs in different regions of the mitochondrial genome. Of these, eight were previously reported in patients with LHON. Two variants namely the heteroplasmic m.189A>G and the homoplasmic m.236T>C in the D-loop region were found in patient P2. This patient also carried four homoplasmic silent variants namely m.10810T>C, m.10915T>C, m.11176G>A, and m.12007G>A in MT-ND4 gene. Additional homoplasmic silent variant in MT-ND4 gene namely m.10876A>G was found in another patient (P15). Finally, one homoplasmic variant namely m.15928G>A in MT-TT tRNA gene was found in patient P16.
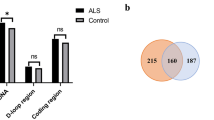
LHON-related mtDNA variants in RRMS patients and healthy controls
We also investigated the presence of mtDNA variants in RRMS patients and healthy controls. The results (Table 5) revealed a number of mtDNA SNVs in protein-coding genes, all were in the homoplasmic state and were previously reported in LHON patients. Comparison of the frequency of individual variant between patients and controls showed statistically significant differences in the prevalence of five variants (P < 0.05). The association of these variants with MS was confirmed by the Fisher's exact test and Bonferroni correction test.
Short reads mapped against mitochondrial genome of these variants are shown in Supplementary S1 Fig, S2 Fig, S3 Fig, S4 Fig and S5 Fig. Among them, three missense variants and one silent variant were more prevalent in the patient group: The missense variant m.4216T>C (referred as rs1599988 polymorphism) in MT-ND1 gene occurred in 39% of patients vs 13% of controls (OR 3.13, 95% CI 0.97–10.1). The missense variant m.13708G>A (refereed as rs28359178 polymorphism) in MT-ND5 gene occurred in 39% of patients vs 8% of controls (OR 4.69, 95% CI 1.13–19.5). The missense variant m.14766C>T (referred as rs193302980 polymorphism) in MT-CYB gene occurred in 96% of patients vs 50% of controls
(OR 1.91, 95% CI 1.27–2.88). The silent variant m.7028C>T (referred as rs2015062 polymorphism) in MT-CO1 gene occurred in 96% of patients vs 42% of controls (OR 2.30, 95% CI 1.42–3.72). However, according to ClinVar database, the variants m.4216T>C and m.13708G>A showed conflicting interpretations of pathogenicity, whereas m.14766C>T was classified as a benign variant. Only one missense variant namely m.10398A>G (referred as rs2853826 polymorphism) in MT-ND3 gene occurred less frequently in patients (30%) compared to controls (63%) (OR 0.49, 95% CI 0.24–0.97). This variant was classified as having a benign/protective effect according to ClinVar database.
Other variants showed no statistical significant differences in their prevalence among patients and controls, and represent simple polymorphisms with no pathological impact, thus they were not analyzed further.
Discussion
MS has long been known to be associated with LHON, a mitochondrial inherited form of vision loss caused by point mutations in mtDNA genes. Both primary and secondary LHON variants have been reported in MS17,25,26,27,28,29,30. However, the presence and relative frequencies of LHON variants in MS patients vary between populations, possibly due to genetic, racial and other factors, which differ in different ethnicities25,26,27,28,29,30,31,32,33. In the current study, we analyzed our recently generated large-scale genomic sequence data of the entire mtDNA from 47 unrelated Saudi Arab individuals, 23 patients diagnosed with RRMS and 24 healthy control subjects to investigate the presence of mutations/variants involved in or associated with LHON in those subjects. Our mutational analysis revealed ten LHON-related variants exclusively present in RRMS patients and not in healthy subjects (Table 2). Three of them were pathogenic/provisional pathogenic mutations and detected in two patients. The homoplasmic m.14484T>C mutation was found in patient P2. m.14484T>C mutation which causes an amino acid change from methionine to valine at position 64 (Met64Va) within the MT-ND6 gene is one of the well-known primary LHON-causing mutation and was also described in a young man with an MS-like illness26. While this mutation infrequently found in LHON patients in most countries17,38, it is the most common mutation detected among French-Canadians due to a founder effect39. The heteroplasmic m.10237T>C mutation was also found in patient P2. m.10237T>C mutation which causes an amino acid change from isoleucine to threonine at position 60 (Ile60Thr) within the MT-ND3 gene is a rare LHON mutation, reported in two Hungarian siblings with LHON patients lacking the three most common pathogenic DNA mutations40. It was also described in eleven patients with LHON of European ancestry harbouring the primary mutation m.14484T>C41. Based on predictive analysis of the impact on protein function (Table 2), both mutations were classified as deleterious, having probably damaging/damaging effects by the PolyPhen2, SIFT, CAAD, and Mutation Assessor models. In our previous study34, we also showed that these two mutations affect the structures of encoded-proteins. The homoplasmic m.9101T>C mutation was found in another patient (P15). This mutation which causes an amino acid change from isoleucine to threonine at position 192 (Ile192Thr) within the MT-ATP6 gene is a rare LHON mutation reported in a single affected patient42. Although the site of this mutation is not in the conserved region of the MT-ATP6 gene, it was linked with decreased coupling of proton flow with ATP production42, but without inhibition of respiration43. Highly conserved residues among homologous proteins are generally considered to be critical for protein stability, interaction and function. In our bioinformatics analysis, the effect of this mutation on encoded-protein was predicted to be benign, neutral and low by the PolyPhen2 SIFT, CAAD and Mutation Assessor models respectively (Table 2).
In addition, seven secondary LHON-related SNVs, all in the homoplasmic state, were also detected in the patient group (Table 2). Of them, three were found in two patients along with the primary/rare LHON mutations. These include m.5442T>C in MT-ND2 gene and m.13105A>G in MT-ND5 which were detected in patient P2 and m.12358A>G in MT-ND5 which was found in patient P15. The other four variants namely m.4695T>C in MT-ND2 gene, m.4917A>G in MT-ND2 gene, m.3316G>A in MT-ND1 gene and 3533C>T in MT-ND1 were individually found in different other patients (P1, P16, P18 and P22 respectively). In previous studies, these secondary variants were described in LHON or LHON-like cases from different ethnic backgrounds along with other LHON primary mutations, and suggested to modify the effect of primary mutations44,45,46. Interestingly, m.4659G>A was also reported as a benign variant associated with Parkinson’s disease, a progressive neurodegenerative disorder47. Our prediction analysis revealed that all these secondary variants have benign, neutral and low effects by the PolyPhen2 SIFT, CAAD and Mutation Assessor models respectively (Table 2).
In our study, most of the identified LHON mutations/variants in RRMS patients were located in NADH dehydrogenase subunit genes of complex I, except for one rare mutation in MT-ATP6 gene of complex V. Mutations in mtDNA-encoded genes of the mitochondrial electron transport chain complexes can lead to deficient function of OXPHOS, decrease in ATP synthesis, and increase in ROS production11,48. Importantly, defects in mitochondrial OXPHOS mainly affect tissues with a high energy demand such as brain, nerves, retina, skeletal and cardiac muscle. While earlier reports showed the co-occurrence of LHON mutations in a sub-group of MS patients or patients with MS-like illness17,25,26,27,28, the association of primary LHON mutations with MS was suggested to be more than a coincidence and individuals carrying primary LHON mutations are at risk of developing MS29. There is an overlap in the clinical and molecular features of MS and LHON. At the molecular level, the interaction between mtDNA mutations in LHON and MS has been suggested as converge on shared pathways of oxidative damage and cell death49. Particularly, complex I respiratory chain dysfunction caused by LHON mtDNA mutations has been shown to decrease energy production and increase ROS generation, leading to retinal ganglion cell defect and apoptosis48,49. These impairments are also seen in demyelination and neurodegeneration in MS whereby complex I dysfunction leads to mitochondrial dysfunction and energy failure7,8,9. Moreover, mtDNA mutations underlying LHON may contribute to presumably immunologically mediate involvement of other myelinated axons in the CNS in susceptible individuals28. The presence of primary/rare pathogenic LHON mutations in some patients with RRMS in this study may suggests a possible role for these mutation in the pathogenesis of MS. Secondary LHON-associated variants may have synergistic effects with the primary mutations or may be responsible for disease phenotype difference22,23,24. Therefore, secondary LHON variants with uncertain pathological significance may also play a role in MS. Further investigations are fundamental to verify the link between LHON-related variants and MS, because the etiology of MS is still unknown.
All patients reported here were first diagnosed as being affected with MS and had both clinical and MRI features of RRMS based on the McDonald diagnosis criteria35. Five out of the six patients who harboured LHON variants were females (P1, P15, P16, P18, P22) and one was a male patient (P2) (Table 3). They were all young adults with different disease durations and different disability scales as indicated by their EDSS. Along with other neurological dysfunctions such as weakness and balance problem, the patients were reported with numbness and visual problem. Visual problem is one of the most common symptoms of MS caused by inflammation in various parts of the optic nerve (optic neuritis) and the pathways from the brain to the eyes and eye muscles2. Unfortunately, we do not know if the family members of our patients are affected by LHON, as genetic testing for LHON is not routinely performed when the initial diagnosis of MS was considered. While there is no evidence to support screening for LHON mutations in all MS patients20, mtDNA analysis is appropriate in a sub-group of MS patients who harbour pathogenic LHON mutations27. Our observations of the presence of pathogenic/provisional pathogenic LHON mutations in two RRMS patients (P2 and P15) highlight the importance of performing molecular genetic analysis not only for patients, but for all relatives in the maternal line to seek guidance on whether they have affected family members and offspring. Molecular genetic testing can be also offered to exclude the possibility of de novo LHON mutations. De novo mutations in LHON are extremely rare, but have been reported for m.14484T>C mutation and other mutations18,19.
Although the penetrance of LHON pedigrees is determined primarily by a mutation in the mtDNA, other factors such as mitochondrial genetic background, nuclear genetic factors and environmental factors are also necessary for manifestation and severity of the disease18,19,20,21. Since our patients were initially diagnosed with MS, many factors need to be addressed to determine the penetrance of the pathogenic/rare mutations. Therefore, further studies are required to investigate the family members of the patients to determine the number of affected males to females, and to assess if they do or not develop features of LHON. Moreover haplogroup analysis is also important for the clustering of theses mutations in the Arab ethnic group. For instance, LHON m.11778G>A and m14484T>C mutations are clustered in haplogroup J in European populations, whereas these two mutations are not associated with haplogroups J but in the Asian haplogroups M and BM, suggesting that different sets of SNPs from the European LHON-related haplotype may contribute to the Asian LHON onset50.
When we investigated the presence of other mtDNA variants in the RRMS patients who carried one of the LHON-related variants, we found that these patients exhibited distinct sets of mtDNA SNVs in different regions of the mitochondrial genome (Table 4). Of them, eight were previously reported in patients with LHON. In the D-loop region, the variants m.189A>G and m.236T>C were found in one patient (P2). Both variants were previously reported in Chinese patients carrying other LHON mutations51. The D-loop is the non-coding region in mtDNA and contains essential transcription and replication elements, thus contributes to the proper functioning of mitochondria52. Variants, which are more frequently occur in the D-Loop region have been implicated in several diseases including neurological disorders53. Another variant namely m.15928G>A in MT-TT gene-encoding tRNAThr was found in one patient (P16). This variant was also described in Chinese subjects with LHON and was suggested to influence the phenotypic manifestation of LHON by affecting the function of MT-TT gene, leading to impairment of mitochondrial protein synthesis and deficient respiration54. Five more SNVs represented silent variants were found in MT-ND4 gene. Four of them namely m.10810T>C, m.10915T>C, m.11176G>A, and m.12007G>A were detected in patient P2 and m.10876A>G was found in patient P15. All of these silent variants were previously described in Chinese subjects carrying LHON mutations51,54. Although silent substitutions do not alter the amino acids and hence the protein sequence, they are suspected to have a potential involvement in human diseases by altering transcript splicing, mRNA stability, or even protein structure and function55,56. The presence of numerous mtDNA variants in RRMS patients who possess one of the LHON mutations might modify the effect of these mutations. The functional significances of these variants should be further examined, especially in patient P2 who was noticed to carry most of these variants along with the pathogenic/rare LHON mutations and secondary variants.
Our analysis of the entire mtDNA in patients and controls revealed a number of variants in protein-coding genes, all were in the homoplasmic state (Table 5) and were previously described as secondary LHON-related variants22,57,58. Five of these variants differed significantly in their prevalence among patients and controls (P < 0.05). Specifically, three missense variants and one silent variant were more prevalent in patients than in controls.
The missense variants include: m.4216T>C referred as rs1599988 polymorphism in MT-ND1 gene was observed in 39% of patients vs 13% of controls (OR 3.13, 95% CI 0.97–10.1), m.13708G>A refereed as rs28359178 polymorphism in MT-ND5 gene was observed in 39% of patients vs 8% of controls (OR 4.69, 95% CI 1.13–19.5), m.14766C>T referred as rs193302980 polymorphism in MT-CYB gene was found in 96% of patients vs 50% of controls (OR 1.91, 95% CI 1.27–2.88). One silent variant namely m.7028C>T referred as rs2015062 polymorphism in MT-CO1 gene was found in 96% of patients vs 42% of controls (OR 2.30, 95% CI 1.42–3.72). These variants were previously described in MS cases and healthy controls14,33,59. Particularly, m.4216T>C and m.13708G>A variants were considered as predisposing markers to MS33,59. Both of them were also suggested as contributing factors of optic neuritis in MS patients60,61. According to ClinVar database, the variants m.4216T>C and m.13708G>A showed conflicting interpretations of pathogenicity, whereas m.14766C>T was classified as a benign variant. Only one missense variant namely m.10398A>G referred as rs2853826 polymorphism in MT-ND3 gene was found less frequently in patients (30%) compared to controls (63%) (OR 0.49, 95% CI 0.24–0.97), suggesting a protective effect of this variant in MS. This variant was classified as having a benign/protective effect according to ClinVar database. It was found to be associated with the reduced risk of Parkinson disease, and its protective effect was proposed to increase the performance of complex I within the brain and other tissues in individuals belong to specific haplogroups62. A protective effect of mtDNA variants has been reported for several diseases such as for haplogroup M with reduced the risk of visual failure in European families with m.11778G>A LHON mutation58. Even though these results indicate that particular mtDNA SNVs differ in their prevalence among MS patients and controls, further validations are required to conclude their exact association with the risk of MS.
Results from the present study, the first to investigate LHON mtDNA mutations/variants in Saudi patients with RRMS and healthy controls, suggest a possible role of the primary/rare LHON mutations in the pathogenesis of MS and a potential association of secondary LHON-related variants with the genetic predisposing to MS. While our study provide important information on the occurrence and association of LHON mtDNA mutations/variants with MS in an Arab population, it has some limitations. The sample size was relatively small and further studies are needed in a large-scale. Moreover, genetic screening of a selected MS patients for pathogenic LHON mutations, pedigree analysis, and additional functional and structural investigations of LHON-related variants are required to provide a better insight into the involvement of these variants in MS.
Methods
Study subjects
The study included 47 unrelated Saudi Arab individuals, 23 patients with RRMS and 24 healthy controls. Patients were recruited from the Neurology Clinic at King Khalid Hospital, King Saud University, Saudi Arabia. Patients were classified as RRMS when they satisfied McDonald diagnosis criteria35, with at least two previous relapses in the central nervous system regions, confirmed by a neurological examination, magnetic resonance imaging (MRI) scans, and electrophysiological studies. Control subjects without neurological conditions or history of autoimmune and inflammatory disease were King Khalid hospital blood donors. Demographic data (Age at the onset of the first symptoms and gender) and clinical data (disease duration, disability status evaluated using the Kurtzke Expanded Disability Status Scale [EDSS], clinical features and medications) were reported for all patients. Other data including blood pressure and body mass index (BMI) were also recorded for both patients and controls. Written informed consents were obtained from all participants. The study was approved by the Scientific and Ethics Committee in King Saud University, College of Medicine (Saudi Arabia), and the Medical Research and Ethics Committee in the College of Medicine and Medical Sciences, Arabian Gulf University (Bahrain). All methods were performed in accordance with the relevant guidelines and regulations.
DNA extraction, next generation sequencing and analysis
DNA was extracted in our previous study34 from the blood of RRMS patients and healthy controls using the QIAMP DSP DNA kit (Qiagen, Hilden, Germany), and all extracted DNA samples were quantified and checked for purity using the NanoDrop ND-1000 ultraviolet–Visible light spectrophotometer (Thermo Fisher Scientific, Inc.). High-throughput sequencing of mitochondrial genomes was performed as described previously34. In brief, whole mtDNA was amplified using long-range PCR kit (Qiagen) PCR products were subsequently purified and quantified before proceeding to DNA library preparation for next-generation sequencing (NGS) using Illumina protocol and sequencing on HiSeq X instrument. For sequence analysis, paired end sequencing data were exported to FASTQ file. Then the sequence reads were trimmed using custom script to remove adapters and bases with low quality value. Alignment of the trimmed reads was performed to hg19 version of the genome available from UCSC genome browser. A sequencing coverage of 10,000 X of the mitochondrial genome was achieved, at such coverage heteroplasmy at 5% levels would be detectable. After alignment, the mtDNA variants were compared with the Revised Cambridge Reference Sequence (rCRS), (NCBI Reference Sequence: NC_012920). mtDNA variants were annotated using the MITOMAP database system for the human mitochondrial genome (http://www.mitomap.org/MITOMAP) and other databases. In general, mtDNA variants can be classified into three categories36:
-
(1)
Benign variant: If a variant has been reported in MITOMAP as a polymorphism, has not been associated with a disease in the population or family studies, and has been reported in mtDB at a frequency > 0.2%.
-
(2)
Unclassified variant: A novel variant, a rare variant that has been reported in MITOMAP as a polymorphism, or reported in mtDB at a frequency ≤ 0.2%, and a rare variant reported in the literature or MITOMAP as a mutation based on a single family study/single report with no functional studies for their pathogenicity. These variants must be further evaluated by protein structure prediction.
-
(3)
Mutation: a variant that has been listed in MITOMAP as confirmed mutation and has been reported in multiple unrelated patients/families with clinical correlation and or supporting functional prediction.
For the identification of LHON mutations/variants, extensive search was done through several databases including MITOMAP, HmtDB (Human Mitochondrial Genome Database), ClinVar and MEDLINE-listed publications on life sciences.
Bioinformatics analysis
We used four bioinformatics tools (PolyPhen2, SIFT, CADD and Mutation Assessor) to determine the deleteriousness of nonsynonymous mutations. These tools predict the impact of nonsynonymous mutations on protein function and structure based on sequence homology, evolutionary conservation, and protein structural information37. The prediction of PolyPhen (Polymorphism Phenotyping) is provided as benign, possibly damaging, and probably damaging with scores of < 0.446, > 0.446, and > 0.908 respectively. The prediction of SIFT (Sorting Intolerant From Tolerant) is provided as tolerated with a score of ≥ 0.05, whereas a score of < 0.05 is considered as damaging. The prediction of CADD (Combined Annotation Dependent Depletion) is provided as benign and deleterious with scores range from 1 to 99 (higher scores indicate more deleterious variants). The Mutation Assessor prediction is provided as neutral, low, medium, or high with scores ranging from 0 to 1 (higher scores indicate more deleterious variants).
Statistical analysis
Comparisons between patients and controls were evaluated using a Chi-square test for categorical variables or equivalent non-parametric Wilcoxon signed-rank test and Mann–Whitney test for normally distributed variables. Differences in the frequencies of variants among cases and controls were assessed using the Fischer exact test. The association of variants with MS was done using the Fisher's exact test, and the odds ratios (OD) and 95% confidence interval (95% CI) were reported. Moreover, multiple comparison correction was also done using the Bonferroni correction. A P value of < 0.05 was considered as statistically significant. All data were analysed using the SPSS software (version 23; IBM Corp., Armonk, NY, USA).
Data availability
The data sets of the entire mtDNA sequences were previously registered in the Sequence Read Archive Repository (ref. No. PRJNA781092)34.
References
Frohman, E. M., Racke, M. K. & Raine, C. S. Multiple sclerosis: The plaque and its pathogenesis. N. Engl. J. Med. 354, 942–955 (2006).
Reich, D. S., Lucchinetti, C. F. & Calabresi, P. A. Multiple sclerosis. N. Engl. J. Med. 11, 169–180 (2018).
Harbo, H. F., Gold, R. & Tintore, M. Sex and gender issues in multiple sclerosis. Ther. Adv. Neurol. Disord. 6, 237–248 (2013).
Waubant, E. et al. Environmental and genetic risk factors for MS: An integrated review. Ann. Clin. Transl. Neurol. 6, 1905–1922 (2019).
Koch, M. K., Metz, L. M. & Kovalchuk, O. Epigenetic changes in patients with multiple sclerosis. Nat. Rev. Neurol. 9, 35–43 (2013).
Ghasemi, N., Razavi, S. & Nikzad, E. Multiple sclerosis: Pathogenesis, symptoms, diagnoses and cell-based therapy. Cell J. 19, 1–10 (2017).
Mahad, D., Lassmann, H. & Turnbull, D. Review: Mitochondria and disease progression in multiple sclerosis. Neuropathol. Appl. Neurobiol. 34, 577–589 (2008).
Dutta, R. et al. Mitochondrial dysfunction as a cause of axonal degeneration in multiple sclerosis patients. Ann. Neurol. 59, 478–489 (2006).
Mao, P. & Reddy, P. H. Is multiple sclerosis a mitochondrial disease?. Biochim. Biophys. Acta. 1802, 66–79 (2010).
Al-Kafaji, G. et al. Mitochondrial DNA copy number in peripheral blood is a novel non-invasive biomarker for multiple sclerosis. Neuromol. Med. 22, 304–313 (2020).
Taylor, R. W. & Turnbull, D. M. Mitochondrial DNA mutations in human disease. Nat. Rev. Genet. 6, 389–402 (2005).
Vyshkina, T. et al. Association of common mitochondrial DNA variants with multiple sclerosis and systemic lupus erythematosus. Clin. Immunol. 129, 31–35 (2008).
Zonouzi, P. A., Ghorbian, S., Abkar, M., Zonouzi, P. A. & Azadi, A. Mitochondrial complex I gene variations as a potential risk factor in the pathogenesis of multiple sclerosis. J. Neurol. Sci. 345, 220–223 (2014).
Alharbi, M. A. et al. Four novel mutations in mitochondrial ND4 gene of complex I in Saudi patients with multiple sclerosis. Biomed. Rep. 11, 257–268 (2019).
Sadovnick, A. D., Bulman, D. & Ebers, G. C. Parent-child concordance in multiple sclerosis. Ann. Neurol. 29, 252–255 (1991).
Ebers, G. C. et al. Parent-of-origin effect in multiple sclerosis: Observations in half-siblings. Lancet 363, 1773–1774 (2004).
Harding, A. E. et al. Occurrence of a multiple sclerosis-like illness in women who have a Leber’s hereditary optic neuropathy mitochondrial DNA mutation. Brain 115, 979–989 (1992).
Yu-Wai-Man, P., Griffiths, P. G., Hudson, G. & Chinnery, P. F. Inherited mitochondrial optic neuropathies. J. Med. Genet. 46, 145–158 (2009).
Yu-Wai-Man, P. & Chinnery, P. F. Leber hereditary optic neuropathy: Therapeutic challenges and early promise. Taiwan J. Ophthalmol. 1, 12–15 (2011).
Harding, A. E., Sweeney, M. G., Govan, G. G. & Riordan-Eva, P. Pedigree analysis in Leber hereditary optic neuropathy families with a pathogenic mtDNA mutation. Am. J. Hum. Genet. 57, 77–86 (1995).
Riordan-Eva, P. & Harding, A. E. Leber’s hereditary optic neuropathy: The clinical relevance of different mitochondrial DNA mutations. J. Med. Genet. 32, 81–87 (1995).
Liang, M., Guan, M. & Zhao, F. Leber’s hereditary optic neuropathy is associated with mitochondrial ND1 T3394C mutation. Biochem. Biophys. Res. Commun. 383, 286–292 (2009).
Matsumoto, M., Hayasaka, S. & Kadoi, C. Secondary mutations of mitochondrial DNA in Japanese patients with Leber’s hereditary optic neuropathy. Ophthal. Genet. 20, 153–160 (1999).
Zhang, M., Zhou, X. & Li, C. Mitochondrial haplogroup M9a specific variant ND1 T3394C may have a modifying role in the phenotypic expression of the LHON-associated ND4 G11778A mutation. Mol. Genet. Metab. 101, 192–199 (2010).
Nikoskelainen, E. K. et al. Leber’s ‘plus’: Neurological abnormalities in patients with Leber’s hereditary optic neuropathy. J. Neurol. Neurosurg. Psychiatry. 59, 160–164 (1995).
Bhatti, M. T. & Newman, N. J. A multiple sclerosis-like illness in a man harboring the mtDNA 14484 mutation. J. Neuroophthalmol. 19, 28–33 (1999).
Kellar-Wood, H., Robertson, N., Govan, G. G., Compston, D. A. & Harding, A. E. Leber’s hereditary optic neuropathy mitochondrial DNA mutations in multiple sclerosis. Ann. Neurol. 36, 109–112 (1994).
Olsen, N. K. et al. Leber’s hereditary optic neuropathy associated with a disorder indistinguishable from multiple sclerosis in a male harbouring the mitochondrial DNA 11778 mutation. Acta Neurol. Scand. 91, 326–329 (1995).
Vanopdenbosch, L., Dubois, B., D’Hooghe, M. B., Meire, F. & Carton, H. Mitochondrial mutations of Leber’s hereditary optic neuropathy: A risk factor for multiple sclerosis. J. Neurol. 247, 535–543 (2000).
Nishimura, M. et al. No association of the 11778 mitochondrial DNA mutation and multiple sclerosis in Japan. Neurology 45, 1333–1334 (1995).
Hwang, J. M., Chang, B. L. & Park, S. S. Leber’s hereditary optic neuropathy mutations in Korean patients with multiple sclerosis. Ophthalmologica 215, 398–400 (2001).
Kalman, B., Lublin, F. D. & Alder, H. Mitochondrial DNA mutations in multiple sclerosis. Mult. Scler. 1, 32–36 (1995).
Mihailova, S. M., Ivanova, M. I., Quin, L. M. & Naumova, E. J. Mitochondrial DNA variants in Bulgarian patients affected by multiple sclerosis. Eur. J. Neurol. 14, 44–47 (2007).
Al-Kafaji, G. et al. Next-generation sequencing of the whole mitochondrial genome identifies functionally deleterious mutations in patients with multiple sclerosis. PLoS ONE 7, e0263606 (2022).
Polman, C. H. et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann. Neurol. 69, 292–302 (2011).
Wang, J. et al. An integrated approach for classifying mitochondrial DNA variants: One clinical diagnostic laboratory’s experience. Genet. Med. 14, 620–626 (2012).
Dong, C. et al. Comparison and integration of deleteriousness prediction methods for nonsynonymous SNVs in whole exome sequencing studies. Hum. Mol. Genet. 15, 2125–2137 (2015).
Mashima, Y. et al. Spectrum of pathogenic mitochondrial DNA mutations and clinical features in Japanese families with Leber’s hereditary optic neuropathy. Curr. Eye Res. 17, 403–408 (1998).
Macmillan, C., Johns, T. A., Fu, K. & Shoubridge, E. A. Predominance of the T14484C mutation in French-Canadian families with Leber hereditary optic neuropathy is due to a founder effect. Am. J. Hum. Genet. 66, 332–335 (2000).
Horvath, J., Horvath, R., Karcagi, V., Komoly, S. & Johns, D. R. Sequence analysis of Hungarian LHON patients not carrying the common primary mutations. J. Inherit Metab. Dis. 25, 323–324 (2002).
Carelli, V. et al. The landscape of mitogenomes from LHON patients carrying the m.14484T>C/MT-ND6 mutation. Invest. Ophthalmol. Vis. Sci. 60, 3601 (2019).
Lamminen, T. et al. A mitochondrial mutation at nt 9101 in the ATP synthase 6 gene associated with deficient oxidative phosphorylation in a family with Leber hereditary optic neuroretinopathy. Am. J. Hum. Genet. 56, 1238–1240 (1995).
Majander, A. et al. Mutations in subunit 6 of the F1Fo-ATP synthase cause two entirely different diseases. FEBS Lett. 412, 351–354 (1997).
Starikovskaya, E. et al. Mitochondrial DNA variation of Leber’s hereditary optic neuropathy in Western Siberia. Cells 8, 1574 (2019).
Khan, N. A. et al. Haplogroup heterogeneity of LHON patients carrying the m.14484T>C mutation in India. Invest. Ophthalmol. Vis. Sci. 54, 3999–4005 (2013).
Yu, D. et al. Molecular characterization of six Chinese families with m.3460G>A and Leber hereditary optic neuropathy. Neurogenetics 11, 349–356 (2010).
Khusnutdinova, E. et al. A mitochondrial etiology of neurodegenerative diseases: Evidence from Parkinson’s disease. Ann. N. Y. Acad. Sci. 1147, 1–20 (2008).
Szczepanowska, J., Malinska, D., Wieckowski, M. R. & Duszynski, J. Effect of mtDNA point mutations on cellular bioenergetics. Biochim. Biophys. Acta. 1817, 1740–1746 (2012).
Bargiela, D. & Chinney, P. F. Mitochondria in neuroinflammation: Multiple sclerosis (MS), leber hereditary optic neuropathy (LHON) and LHON-MS. Neurosci. Lett. 710, 132932 (2019).
Nishioka, T. et al. Leber’s hereditary optic neuropathy with 14484 mutation in Central Java, Indonesia. J. Hum. Genet. 48, 385–398 (2003).
Jiang, P. et al. Prevalence of mitochondrial ND4 mutations in 1281 Han Chinese subjects with Leber’s hereditary optic neuropathy. Invest. Ophthamol. Vis. Sci. 56, 4778–4788 (2015).
Suissa, S. et al. Ancient mtDNA genetic variants modulate mtDNA transcription and replication. PLoS Genet. 5, e1000474 (2009).
Cruz, A. C. P., Ferrasa, A., Muotri, A. R. & Herai, R. H. Frequency and association of mitochondrial genetic variants with neurological disorders. Mitochondrion 46, 345–360 (2019).
Lyu, Y. et al. Frequency and spectrum of MT-TT variants associated with Leber’s hereditary optic neuropathy in a Chinese cohort of subjects. Mitochondrial DNA B Resour. 4, 2266–2280 (2019).
Komar, A. A. SNPs, silent but not invisible. Science 315, 466–467 (2007).
Shabalina, S. A., Spiridonov, N. A. & Kashina, A. Sounds of silence: synonymous nucleotides as a key to biological regulation and complexity. Nucleic Acids Res. 41, 2073–2094 (2013).
Abu-Amero, K. K. & Bosley, T. M. Mitochondrial abnormalities in patients with LHON-like optic neuropathies. Invest. Ophthalmol. Vis. Sci. 47, 4211–4220 (2006).
Ji, Y. et al. Mitochondrial DNA haplogroups M7b1’2 and M8a affect clinical expression of leber hereditary optic neuropathy in Chinese families with the m.11778G>a mutation. Am. J. Hum. Genet. 83, 760–768 (2008).
Yu, X. et al. mtDNA nt13708A variant increases the risk of multiple sclerosis. PLoS ONE 3, e1530 (2008).
Mayr-Wohlfart, U., Paulus, C., Henneberg, A. & Rodel, G. Mitochondrial DNA mutations in multiple sclerosis patients with severe optic involvement. Acta Neurol. Scand. 94, 167–171 (1996).
Reynier, P. et al. mtDNA haplogroup J: A contributing factor of optic neuritis. Eur. J. Hum. Genet. 7, 404–406 (1999).
van der Walt, J. M. et al. Mitochondrial polymorphisms significantly reduce the risk of Parkinson disease. Am. J. Hum. Genet. 72, 804–811 (2003).
Author information
Authors and Affiliations
Contributions
G.A., M.B. and M.A. developed the project, collected and analyzed the data. H.A. and A.S. analyzed the data and prepared tables and figures. G.A. wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Al‐Kafaji, G., Alharbi, M.A., Alkandari, H. et al. Analysis of the entire mitochondrial genome reveals Leber’s hereditary optic neuropathy mitochondrial DNA mutations in an Arab cohort with multiple sclerosis. Sci Rep 12, 11099 (2022). https://doi.org/10.1038/s41598-022-15385-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-15385-2
- Springer Nature Limited