Abstract
Leber's hereditary optic neuropathy (LHON) is a maternally inherited late-onset form of blindness characterized by acute or subacute bilateral retinal degradation resulting in a permanent loss of central vision. G11778A, C3460A, and T14484C mutations on mitochondrial DNA (mtDNA) are specific for LHON and account for most, but not all, worldwide LHON cases. A six-generation Indonesian LHON family with the T14484C mutation was analyzed. Polymerase chain reaction/restriction fragment length polymorphism analysis showed that all of the maternal lineages had the T14484C mutation in a homoplasmic form. Penetrance of the disease (33.3%) and male predominance (3:1) was similar to other worldwide LHON with the T14484C mutation. The incidence of offspring born to affected mothers was no different from that of unaffected mothers, and the age distribution of cases was no higher than that of asymptomatic carriers. Eight secondary mutations were sought but not detected. The patients of this family belonged to haplogroup M. These findings support the idea that the mtDNA backgrounds involved in the expression of LHON mutations in southeast Asians are different from those of Europeans.
Similar content being viewed by others
Introduction
Leber's hereditary optic neuropathy (LHON) is a maternally inherited late-onset form of blindness characterized by acute or subacute bilateral retinal degradation resulting in a permanent loss of central vision. A typical feature of LHON is a peripapillary microangiopathy, which involves the presence of tortuous vessels in the central retina and telangiectatic capillaries (Newman 1998). Genetic studies of LHON families have shown incomplete penetrance of optic neuropathy and higher incidence in male offspring (Riordan-Eva et al. 1995; Sudoyo et al. 2002; Mashima et al. 1998). Therefore, genetic and/or environmental etiologic factors play roles in LHON development.
In the late 1980s, Wallace and colleagues initiated studies of the molecular basis of LHON and characterized a responsible mitochondrial DNA (mtDNA) mutation for LHON; the mutation, G11778A, which was located in the ND4 gene, was found in the majority of LHON cases with European origins (Wallace et al. 1988). Together with other two mutations, C3460A and T14484C, the G11778A mutation is one of the primary mutations that are specific for LHON and that account for most, but not all, worldwide LHON cases (Johns et al. 1992; Howell et al. 1991; Huoponen et al. 1991).
However, these primary mutations do not account for characteristics of LHON such as incomplete penetrance and male predominance, and so, many attempts have been made to determine other possible factors influencing LHON development. For the primary mutations, a homoplasmic status for the mutated allele is observed in most LHON patients. However, a small proportion of patients demonstrate a heteroplasmic status for wild and mutated alleles, and the relationship between heteroplasmy and onset of LHON is still not well understood (Newman et al. 1991; Smith et al. 1993; Howell 1994; Mashima et al. 1995; Chinnery et al. 2001).
Several mutations, such as those at nucleotide positions (np) 3394, 4216, 4917, 5244, 7444, 9438, 9804, 13708, 13730, 15257, and 15812, are considered to be related to LHON pathogenesis. They are called "secondary" mutations because (1) some of them are rarely found, and others are found not only in LHON patients and their maternal relatives, and (2) they contribute to LHON progression, if at all, in combination with other mutations (Oostra et al. 1994; Hofmann et al. 1997; Mashima et al. 1998).
MtDNA haplotype analyses of European LHON families have revealed that European and north American 11778 and 14484 mutations tend to associate with haplogroup J (Brown et al. 1997; Howell et al. 1995; Torroni et al. 1997). Recently, Sudoyo et al. (2002) have surveyed southeast Asian LHON patients and have shown that southeast Asian LHON 11778 is associated with haplogroups M and BM.
Although many genetic studies have been carried out on LHON in European and north American populations, few studies have been performed in southeast Asians. To understand the molecular mechanism of LHON development, investigations of Asian LHON cases and comparisons of them with European LHON cases are awaited. We report here an Indonesian family carrying the LHON T14484C mutation.
Subjects and methods
Subjects
A large family with inherited blindness in Banjarnegara, Central Java, Indonesia has been reported (Dyat 1989). They have a Javanese ethnic background. After informed consent was obtained, peripheral blood was collected from the members of the family. The total number of blood specimens was 43, including those from 12 blind individuals. Their sex, age, and case histories were recorded. One male aged 18 years recovered from blindness. The pedigree of this family is presented in Fig. 1.
Family tree of the Indonesian LHON family (filled symbols affected, open symbols unaffected, shaded symbols unaffected maternal relative). The numbered individuals were the subjects of this genetic study, and each number indicates the age of the individual at examination (? unknown age, asterisk recovered from blindness)
LHON mutation screening and haplotype analysis
DNA was extracted from blood specimens by the NaI method (Wang et al. 1994) and analyzed by the polymerase chain reaction (PCR)-restriction fragment length polymorphism (RFLP) technique. The primer sets and restriction enzymes used for LHON mutation screening are shown in Table 1. PCR amplifications were performed in 50 μl reaction mixture, consisting of 1× PCR buffer, 2 mM MgCl2, 20 pmol forward primer, 20 pmol reverse primer, 1 U Ampli Taq gold (Applied Biosystems, Tokyo, Japan), and 1 μl DNA. PCR cycling was initiated after a denature step of 95°C for 9 min, and 45 PCR cycles were preformed. Aliquots of 10 μl PCR products were used for restriction enzyme digestion. In total, 20 μl mixture (1× buffer, 1 U restriction enzyme, 10 μl PCR product) was incubated at the recommended temperature for more than 12 h. The restriction fragments were electrophoresed on 2% agarose gel and visualized by ethidium bromide staining.
To confirm the presence of 14484 mutants, PCR was performed by using a specific primer set (forward: 14393–14414, reverse: 14739–14758), and the nucleotide sequence of the PCR product was determined by using an ABI PRISM BigDye Terminator cycle sequencing FS kit and ABI PRISM 310 Genetic Analyzer (Applied Biosystems).
Primer sets for 10394 DdeI and 10397 AluI (forward: 10200–10217, reverse: 10678–10691) and 13708 BstNI (forward: 13462–13480, reverse: 13875–13894) were used in the PCR-RFLP analysis to identify the mtDNA haplogroup of the patients.
Results
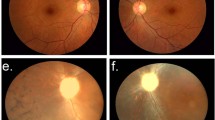
PCR-RFLP analyses to detect LHON primary mutations were performed in 12 patients of our Indonesian family and showed that all the patients had a T14484C mutation (Fig. 2a). This mutation was confirmed by direct sequencing (Fig. 2b). Other primary mutations, viz., G11778A and G3460A, were not found in the patients. The presence of the T14484C mutation was screened and was found exclusively in the maternal relatives of the patients (15 individuals). Heteroplasmy of this mutation was not observed in this family.
Penetrance in this family was 33.3%. The male to female ratio was 3:1, and the number of male cases was significantly greater than that of female cases (P=0.014, Fisher's exact test; Table 2).
The age of the youngest patient was 18 years in this family. In order to determine the factors responsible for LHON onset, we compared the incidence in offspring aged over 18 years born to affected and unaffected mothers, but this was not significantly different (P>0.05, Fisher's exact test; Table 3). Figure 3 shows the age distribution of the patients and asymptomatic carriers over 18 years of age; the age distribution of the patients and asymptomatic carriers was not different (P>0.05, Mann-Whitney U test).
We performed PCR-RFLP screening for np 4216, 4917, 5244, 9438, 9804, 13708, 15257, and 15812 substitutions to find secondary mutations. PCR-RFLP showed that none of the subjects had any substitutions. We then identified the mtDNA lineages of the LHON family as haplogroup M (gain of np 10394 DdeI and np 10397 AluI sites).
Discussion
The genetic backgrounds of southeast Asian LHON are poorly understood compared with those of European and north American LHON. We report here a six-generation LHON family with the T14484C mutation in Indonesia.
The penetrance of LHON in this family was 33.3%, and significant male predominance was observed in the LHON patients (male:female=3:1; P=0.014). These characteristics were similar to those of other worldwide LHON 14484 mutation carriers (Riordan-Eva et al. 1995; Sudoyo et al. 1998, 2002; Mashima et al. 1998).
A better visual prognosis of LHON patients with the 14484 mutation than those carrying the 11778 mutation has been universally observed (Riordan-Eva et al. 1995; Oostra et al. 1994; Johns et al. 1993; Mashima et al. 1998). One case who showed an amelioration in his eyesight indicates that the visual prognosis of LHON patients with the 14484 mutation is relatively good and provides us with a clue regarding the search for a treatment.
In order to find the factors influencing LHON progression, we studied the incidence of LHON patients born to affected mothers and the relationship between age and LHON development; however, we could not find any significant tendency relating to the development of LHON. More numbers of cases are thus required.
We performed PCR-RFLP screening to detect eight known secondary mutations, but none of the subjects had any of these substitutions. The present Indonesian LHON family with the 14484 mutation belongs to the large Asian haplogroup M, in comparison with the southeast Asian G11778A mutation, which belongs to haplogroups M and BM (Sudoyo et al. 2002).
The clustering of the European LHON 11778 and 14484 mutations in haplogroup J suggests that several sets of single-nucleotide polymorphisms in this haplogroup may have a relationship with the development of LHON; however, the finding that the Asian LHON 11778 and 14484 mutations are not associated with haplogroup J but with the Asian haplogroups M and BM indicates that different sets of sequence variants from the European LHON-related haplotype may contribute to the Asian LHON onset. Our result supports the idea that different DNA backgrounds are involved in the expression of LHON in southeast Asians and Europeans. A10398G is responsible for the DdeI recognition site at np 10394 and is common to haplogroups M, BM, and J. This substitution is considered to be one of the candidate sequence substitutions influencing the development of LHON; however, this region is also known to be variable, and the substitution is present in numerous haplogroups (Brown et al. 1992; Torroni et al. 1997; Finnilä and Majamaa 2001; Sudoyo et al. 2002). Comparing the DNA variants between European LHON patients and Asian patients is essential for understanding the effect of genetic background on LHON.
References
Anderson S, Bankier AT, Barrell BG, De Bruijin MHL, Coulson AR, Drouin J, Eperon IC, Nierlich DP, Roe BA, Sanger F, Schreier PH, Smith AJ, Staden R, Young IG (1981) Sequence and organization of the human mitochondrial genome. Nature 290:457–465
Brown MD, Voljavec AS, Lott MT, Torroni A, Yang C-C, Wallace DC (1992) Mitochondrial DNA complex I and III mutations associated with Leber's hereditary optic neuropathy. Genetics 130:163–173
Brown MD, Sun F, Wallace DC (1997) Clustering of Caucasian Leber hereditary optic neuropathy patients containing the 11778 or 14484 mutations on an mtDNA Linage. Am J Hum Genet 60:381–387
Chinnery PF, Andrews RM, Turnbull DM, Howell N (2001) Leber hereditary optic neuropathy: does heteroplasmy influence the inheritance and expression of the G11778A mitochondrial DNA mutation? Am J Med Genet 98:235–243
Dyat M (1989) Atrofi Nervus opticus herediter di kecamatan wanadari. Medika 10:911–912
Finnilä S, Majamaa K (2001) Phylogenetic analysis of mtDNA haplogroup TJ in a Finnish population. J Hum Genet 46:64–69
Hofmann S, Bezold R, Jaksch M, Kaufhold P, Obermaier-Kusser B, Gerbitz KD (1997) Disease relevance of the so-called secondary Leber hereditary optic neuropathy mutations. Am J Hum Genet 60:1539–1542
Howell N (1994) Primary LHON mutations: trying to separate "Fruyt" from "Chaf". Clin Neurosci 2:130–137
Howell N, Bindoff LA, McCullough DA, Kubacka I, Poulton J, Mackey D, Taylor L, Turnbull DM (1991) Leber hereditary optic neuropathy: identification of the same mitochondrial ND1 mutation in six pedigrees. Am J Hum Genet 49:939–950
Howell N, Kubacka I, Halvorson S, Howell B, McCullough DA, Mackey D (1995) Phylogenetic analysis of the mitochondrial genomes from Leber hereditary optic neuropathy pedigrees. Genetics 140:285–302
Huoponen K, Vilkki J, Aula P, Nikoskelainen EK, Savontaus M-L (1991) A new mtDNA mutation associated with Leber hereditary optic neuroretinopathy. Am J Hum Genet 48:1147–1153
Johns DR, Neufeld MJ (1993) Cytochrome c oxidase mutations in Leber hereditary optic neuropathy. Biochem Biophys Res Commun 196:810–815
Johns DR, Neufeld MJ, Park RD (1992) An ND-6 mitochondrial DNA mutation associated with Leber hereditary optic neuropathy. Biochem Biophys Res Commun 187:1551–1557
Johns DR, Heher KL, Miller NR, Smith KH (1993) Leber's hereditary optic neuropathy clinical manifestations of the 14484 mutation. Arch Ophthalmol 111:495–498
Mashima Y, Saga M, Hiida Y, Oguchi Y, Wakakura M, Kudoh J, Shimizu N (1995) Quantitative determination of heteroplasmy in Leber's hereditary optic neuropathy by single-strand conformation polymorphism. Invest Ophthalmol Vis Sci 36:1714–1720
Mashima Y, Yamada K, Wakakura M, Kigasawa K, Kudoh J, Shimizu N, Oguchi Y (1998) Spectrum of pathogenic mitochondrial DNA mutations and clinical features in Japanese families with Leber's hereditary optic neuropathy. Current Eye Res 17:403–408
Newman NJ (1998) Leber's optic neuropathy In: Miller NR, Newman NJ (eds) Walsh and Hoyt's clinical neuro-ophthalmology, 5th edn. Lippincott, Williams and Wilkins, Philadelphia, pp 742–753
Newman NJ, Lott MT, Wallace DC (1991) The clinical characteristics of pedigrees of Leber's hereditary optic neuropathy with the 11778 mutation. Am J Ophthalmol 111:750–762
Oostra RJ, Bolhuis PA, Wijburg FA, Zorn-Ende G, Bleeker-Wagemakers EM (1994) Leber's hereditary optic neuropathy: correlations between mitochondrial genotype and visual outcome. J Med Genet 31:280–286
Riordan-Eva P, Sanders MD, Govan GG, Sweeney MG, Da Costa J, Harding AE (1995) The clinical features of Leber's hereditary optic neuropathy defined by the presence of a pathogenic mitochondrial DNA mutation. Brain 118:319–337
Smith KH, Johns DR, Heher KL, Miller NR (1993) Heteroplasmy in Leber's hereditary optic neuropathy. Arch Ophthalmol 111:1486–1490
Sudoyo H, Sitepu M, Malik S, Poesponegoro HD, Marzuki S (1998) Leber's hereditary optic neuropathy in Indonesia: Two families with the mtDNA 11778G→A and 14484T→C mutations. Hum Mutat (Suppl) 1:s271–s274
Sudoyo H, Suryadi H, Lertrit P, Pramoonjago P, Lyrawati D, Marzuki S (2002) Asian-specific mtDNA backgrounds associated with the primary G11778A mutation of Leber's hereditary optic neuropathy. J Hum Genet 47:594–604
Torroni A, Petrozzi M, D'Urbano L, Sellitto D, Zeviani M, Carrara F, Carducci C, Leuzzi V, Carelli V, Barboni P (1997) Haplotype and phylogenetic analyses suggest that one European-specific mtDNA background plays a role in the expression of Leber hereditary optic neuropathy by increasing the penetrance of the primary mutations 11778 and 14484. Am J Hum Genet 60:1107–1121
Wallace DC, Singh G, Lott MT, Hodge JA, Schurr TG, Lezza AMS, Elsas II LJ, Nikoskelainen EK (1988) Mitochondrial DNA mutation associated with Leber's hereditary optic neuropathy. Science 242:1427–1430
Wang L, Hirayasu K, Ishizawa M, Kobayashi Y (1994) Purification of genomic DNA from human whole blood by isopropanol-fractionation with concentrated NaI and SDS. Nucleic Acids Res 22:1774–1775
Acknowledgements
We greatly appreciate the members and non-members of the present LHON family for their participation in this study. Blood sampling was carried out with the collaboration of Drs. Y. Sukri and M. Dyat. This work was partly supported by the Japan Society for the Promotion of Science and a grant-in-aid for the Scientific research from NEXT, Japan.
Author information
Authors and Affiliations
Corresponding author
Additional information
T. Nishioka and M. Tasaki contributed equally to this work
Rights and permissions
About this article
Cite this article
Nishioka, T., Tasaki, M., Soemantri, A. et al. Leber's hereditary optic neuropathy with 14484 mutation in Central Java, Indonesia. J Hum Genet 48, 385–389 (2003). https://doi.org/10.1007/s10038-003-0042-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10038-003-0042-2
Keywords
This article is cited by
-
Analysis of the entire mitochondrial genome reveals Leber’s hereditary optic neuropathy mitochondrial DNA mutations in an Arab cohort with multiple sclerosis
Scientific Reports (2022)
-
Molecular epidemiology of mtDNA mutations in 903 Chinese families suspected with Leber hereditary optic neuropathy
Journal of Human Genetics (2006)
-
mtDNA/nDNA ratio in 14484 LHON mitochondrial mutation carriers
Journal of Human Genetics (2004)