Abstract
Endothelial dysfunction is a key player in both the onset and development of atherosclerosis. No study has examined whether healthy dietary patterns can improve microvascular endothelial function in patients with coronary heart disease (CHD) in the long-term and whether this relationship can affect patient’s risk of CHD recurrence. In the CORDIOPREV study, a randomized, double-blind, controlled trial, dietary intervention with either the Mediterranean diet or a low-fat diet was implemented in 1,002 CHD patients. A laser-doppler flowmetry was performed at baseline and after 6 years of follow up in 664 patients, evaluating the effects of this dietary intervention on microvascular basal flow and reactive hyperaemia area, as well as on the risk of CHD recurrence, based on the TRS2P risk score. Basal flow (97.78 ± 2.79 vs. 179.31 ± 5.06 arbitrary perfusion units, 83.38% increase, p < 0.001) and reactive hyperaemia area (4233.3 ± 127.73 vs. 9695.9 ± 205.23 arbitrary perfusion units per time, 129.04% increase, p < 0.001) improved after the dietary intervention in the cohort, without finding differences due to the diet (p > 0.05 for the diet-effect). When patients were stratified to low, moderate or high-risk of recurrence, basal flow was similarly increased in all three groups. However, reactive hyperaemia area was improved to a greater extent in patients at the low-risk group compared with those at moderate or high-risk. No differences were observed between diets. Healthy dietary patterns can improve microvascular endothelial function and this improvement persists in the long-term. Patients with a low-risk of CHD recurrence show a greater improvement in reactive vasodilation to ischemia than patients in the moderate or high-risk groups.
Similar content being viewed by others
Introduction
Endothelial dysfunction is one of the key processes in the development and progression of atherosclerosis1. In this context, the endothelium malfunctions mainly due to a lack of bioavailability of nitric oxide (NO), which, in turn, encourages platelet adhesion and aggregation, smooth cell proliferation and migration of leukocytes in the vascular bed, leading to the establishment of a prooxidant, proinflammatory and procoagulant environment2. Furthermore, common comorbidities of atherosclerosis, including hypertension, diabetes mellitus, obesity and dyslipidemia enhance the production of reactive oxygen species, thus promoting atherothrombosis1. Therefore, endothelial dysfunction is currently identified as a key contributor to atherogenesis and the development of atherosclerotic plaque1,2.
Endothelial function (EF) can be evaluated at different blood vessel levels, i.e. at large, medium and microvascular sites. Different methodologies have been developed specifically for each site, as vascular biology in the different types of vessels responds differently to stimuli3. Several cardiovascular risk factors have been linked to an impaired EF4. Consumption of a healthy dietary pattern can modulate EF5,6,7. Indeed, previous studies have shown that the consumption of a Mediterranean diet (MedDiet), rich in extra virgin olive, improved EF in patients with obesity, hypercholesterolaemia, diabetes mellitus or metabolic syndrome in the short term5,8,9. In the CORDIOPREV study, we have previously found a favorable effect of the MedDiet on EF in the brachial artery, measured by flow-mediated dilation (FMD), in patients with coronary heart disease (CHD)10,11. This improvement in FMD correlated with a reduction in the concentration of endothelial microparticles and the intracellular production of reactive oxygen species, as well as an increase in endothelial progenitor cells11. Other healthy dietary patterns, such as a low-fat diet (LFD), have yielded divergent results in terms of their effect on EF7,12,13,14,15. Of note, among the different vascular beds used to evaluate EF, the brachial artery EF (assessed by FMD) has been the most studied. In this technique, echography of the brachial artery, before and after cuff-induced hypoxia, reveals the reactivity of medium-sized vessels16.
The microvascular system constitutes a special vascular site in human biology. The capillaries have certain structural characteristics that affect the regulation of their function, mainly their vasodilatory capacity, with circulating substances playing an important role in this process17. Microvascular EF (MEF) has been identified as a major homeostatic regulator, since most of the oxygen delivery to cells is carried out by blood capillaries17. The best-established method to evaluate MEF is laser-doppler flowmetry (LDF), an easy, fast, semi-automatic method to assess blood flow in capillaries in a similar way to pulsioxymetry18,19,20,21. The main factors usually assessed by LDF are: (1) basal flow (BF), i.e. the amount of blood flow that passes through the capillaries in a resting condition, and, (2) the reactive hyperaemia area (RHA), which expresses the capacity of the microvascular endothelium to vasodilate in the presence of an acute ischemia22.
MEF has been positively associated with the concentrations of phenol compounds23, NO24 and endothelial progenitor cells25. In this context, consumption of a MedDiet for 4 weeks increased the circulating levels of these substances and improved MEF23,24,25. However, up-to-date, there are no studies evaluating the long-term impact of healthy diets on the MEF in CHD patients, or whether this impact is linked to their risk of CHD recurrence. This risk may be assessed by the “Thrombolysis in Myocardial Infarction Risk (TIMI) Score for Secondary Prevention” (TRS2P), a tool that can categorize the risk of recurrence in patients with atherosclerotic cardiovascular disease (ASCVD)26.
The aim of the current study was to evaluate whether the consumption of healthy diets (MedDiet or LFD) influences the MEF of CHD patients in the long-term, and whether this influence may interrelate with the risk of CHD recurrence, assessed by the TRS2P score.
Patients and methods
Overall design and patient population
The CORDIOPREV study (Clinicaltrials.gov number NCT00924937) is a randomized, double-blind, controlled trial including 1,002 CHD patients. The study was conducted at the Instituto Maimonides de Investigacion Biomedica de Cordoba (IMIBIC), a scientific institute which carries out research into biomedical areas for the Reina Sofia University Hospital, and the University of Cordoba, Spain. The lipids and atherosclerosis unit, internal medicine unit, is also a member of the CIBER Fisiopatologia de la Obesidad y Nutrición (CIBERobn), a national research organization studying obesity and nutrition and their impact on health and disease.
Objectives and interventions
The aim of the CORDIOPREV study was to examine the efficacy of a MedDiet rich in olive oil, compared with a LFD, to prevent new, major cardiovascular clinical events. The baseline characteristics, inclusion and exclusion criteria have been published previously27 (See the Supplemental Materials). The aim of the current study was to evaluate whether the consumption of these two healthy diets influences the MEF of CHD patients in the long-term, and whether this influence may interrelate with the risk of CHD recurrence, assessed by the TRS2P. MEF was measured at baseline and during follow-up. The CORDIOPREV study protocol was approved by the local ethics committee, in line with the Helsinki declaration and good clinical practices, and all patients gave their informed consent to participate in the study.
The current study included only those patients who were active, following the study protocol and who had an LDF performed at 6 years of follow-up.
Assesment of MEF
LDF (Periflux 5000, Perimed SA) was used to assess MEF at baseline and after 6 years. LDF evaluates cutaneous microcirculation in real time through a laser probe situated on the second finger of the dominant hand22. This technique also assesses ischemia-induced effect in a specific site, as a stimulus for microvascular endothelial vasodilation. Ischemia is induced by inflating a blood pressure cuff over suprasystolic pressure (200 to 220 mmHg) for 4 min in the upper arm, 2–4 cm above the elbow bend. BF and RHA were measured. BF was expressed as arbitrary perfusion units (APU) and RHA as arbitrary perfusion units per time (APUT)22.
Patient classification based on their baseline risk of CHD recurrence as assessed by the TRS2P risk score
To assess whether the effect of dietary intervention on the MEF of CHD patients can be related to their risk of CHD recurrence, patients were classified according to the TRS2P score. This tool is used to predict the risk of recurrence in several populations, and is based on 9 clinical entities identified as independent factors of new atherothrombotic events (Fig. 1). Each item represents 1 point. Total score is the sum of all clinical comorbities present in each individual. According to previous findings28,29,30, patients were classified into three groups: low (0–1 points), moderate (2 points) and high atherothrombotic risk (> 2 points).

Source: Bohula et al.26.
TRS2P risk indicators. Self-production.
Statistical analysis
Continuous variables are expressed as mean ± standard error,whereas percentages were used to express dichotomous variables. Long-term changes in BF and RHA at 6 years were assessed with a T-test for related samples. Repeated-measures ANOVA and post-hoc multiple comparisons analysis with Bonferroni’s correction were used to investigate the effects of diets on BF and RHA and the differences between atherothrombotic risk groups. The chi-square and the Monte Carlo test were performed to evaluate the distribution of the TRS2P components among the three risk groups. All analyses were adjusted for gender and drug therapy (statins, beta-blockers, angiotensin-converting enzyme inhibitors and angiotensin receptor blockers) at baseline. A 2-sided p value < 0.05 was considered statistically significant. All statistical analyses were performed by the use of SPSS 23 (IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp).
Ethics approval and consent to participate
All the patients gave their written informed consent to participate in the study. Following institutional and Good Clinical Practice guidelines, the Human Investigation Review Committee (the local ethics committee “Comité de Ética de la Investigación de Córdoba (CEIC)”) approved the study protocol at Reina Sofia University Hospital.
Consent for publication
Not applicable.
Results
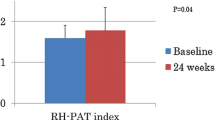
From the initial 1,002 CHD patients included in the CORDIOPREV study, a total of 664 patients were included in the study (See flow-chart included in the Supplemental Materials). Dietary intervention with either MedDiet or LFD improved both BF (97.78 ± 2.79 APU vs. 179.31 ± 5.06 APU, 83.38% increase, p < 0.001) and RHA (4233.3 ± 127.73 APUT vs. 9695.9 ± 205.23 APUT, 129.04% increase, p < 0.001). No differences were observed between the two diets (p = 0.69) (Fig. 2).
According to the TRS2P score, 298 patients were classified as low-risk, 243 as moderate-risk and 123 as high-risk. The clinical characteristics and TRS2P factor distribution for each risk group are shown in Table 1. At baseline, there were no differences in BF and RHA between risk groups and according to the dietary pattern (BF: 97.7 ± 6.3 vs. 87.7 ± 5.3 APU for MedDiet vs. LFD in the low-risk group; 100.4 ± 7.2 vs. 103.5 ± 6.1 APU for MedDiet vs. LFD in the moderate-risk group; 101.5 ± 8.1 vs. 98.9 ± 8.5 APU for MedDiet vs. LFD in the high-risk group, p > 0.05 all comparisons; RHA: 4251.96 ± 262.3 vs.4564.88 ± 300.3 APUT for MedDiet vs. LFD in the low-risk group; 4263.6 ± 256.7 vs. 3988.83 ± 306.7 APUT for MedDiet vs. LFD in the moderate-risk group; 3984.5 ± 389.5 vs. 4192.8 ± 470.8 APUT for MedDiet vs. LFD in the high-risk group, p > 0.05 all comparisons).
BF and RHA significantly improved in the total population after 6 years of follow-up in all risk groups (BF: 92.83 ± 4.2 vs. 186.62 ± 7.6 APU in the low-risk group; 102.2 ± 4.6 vs. 180.5 ± 8.4 APU in the moderate-risk group; 99.12 ± 6.6 vs. 161.46 ± 12 APU in the high-risk group; RHA: 4416.6 ± 193.2 vs. 10,424.59 ± 308.5 APUT in the low-risk group; 4120.28 ± 211.9 vs. 9133.16 ± 338.3 APUT in the moderate-risk group; 4073.02 ± 303.7 vs. 8995.58 ± 484.82 APUT in the high-risk group; p < 0.001 all comparisons) (Fig. 3). We didn´t find any effect of diet in these changes(Supplemental Material).
BF improvement was similar between the three atherothrombotic risk groups (p = 0.47), but RHA was greatly improved in the low-risk group compared with both the moderate and high-risk groups (p < 0.05) (Fig. 3).
Discussion
The current study found that the consumption a healthy dietary pattern (MedDiet or LFD) over 6 years can lead to a long-term improvement in MEF in patients with CHD. Indeed, both BF and RHA improved compared with baseline measurements, regardless of the type of healthy diet. Furthermore, although this benefit was evident in all patients, those at low-risk of CHD recurrence, according to the TRS2P score, showed an even greater improvement in their RHA, compared with the moderate and high-risk groups.
EF is impaired in patients with hypertension, diabetes mellitus and hypercholesterolemia17,31,32,33. Drug treatment of these conditions was shown to improve macro- and microvascular EF in the short-term3,31,32,33,34,35,36. On the other hand, different dietary patterns may modulate EF. In a previous report from our group, the long-term consumption of a MedDiet, rich in extra virgin olive oil, for 1.5 years improved FMD in the brachial artery in patients with diabetes and prediabetes, while the consumption of a LFD stabilized FMD10. A recent meta-analysis, including 7 randomized controlled trials using FMD, confirmed these results37. Regarding LFD, the evidence on its impact on EF is controversial with some authors reporting an improvement in EF after a few weeks of LFD consumption7,13, and others finding that EF remained stable after one year of follow-up12,15. Of note, the available studies focused on assessing the effect of LFD in obese or diabetic patients without ASCVD7,12,13,14,15. Up-to-date, it had not been clarified whether these effects of healthy diets on EF, especially in MEF, persisted or disappeared over time.
With regard to microcirculation, previous studies demonstrated that MedDiet increased MEF at 8 weeks in patients over 65 years, alone or in combination with exercise 25,38. This benefit was also observed in patients with hypercholesterolemia or metabolic syndrome, when evaluating postprandial MEF with LDF 23,24. There are varying underlying mechanisms that may account for the benefits of a MedDiet on MEF. On one hand, extra virgin olive oil is rich in monounsaturated fatty acids (MUFAs) and phenolic compounds, both of which reduce superoxide production and decrease the oxidation of low-density lipoprotein (LDL) particles, thus inhibiting the development of atherosclerotic plaque and endothelial dysfunction39,40. On the other hand, oily fish increases NO bioavailability, by upregulation of endothelial NO synthase, whereas green vegetables, grains and legumes are the provisions of inorganic nitrate and L-arginine, which are NO precursors37. Oxidative stress, inflammation and endothelial dysfunction are interrelated1. In fact, long-term consumption of a MedDiet rich in extra virgin olive oil was linked to a reduction in the plasma/serum concentration of pro-inflammatory markers such as interleukin-6, a C-reactive protein, adhesion molecules and in the chemokines in the PREDIMED (Prevención con Dieta Mediterránea) Study41,42, where the MedDiet reduced the relative risk of major cardiovascular events in patients without ASCVD. Most of the evidence about LFD derives from studies invovling vascular beds other than microcirculation. Therefore, the findings of the current study are the first to assess long-term impact of LFD on microcirculation with laser-doppler technology, and confirmed that both MedDiet and LFD can improve MEF in patients with CHD.
In the current study, patients were classified according to TRS2P to evaluate whether long-term changes in MEF after the implementation of a healthy dietary pattern were associated with individual’s risk of CHD recurrence. This hypothesis could help to implement diverse dietary approaches for patients with a different CHD severity, with a more personalized approach. We used the TRS2P score since this tool was also applied in the Examining Outcomes in Subjects With Acute Coronary Syndrome: Vytorin (Ezetimibe/Simvastatin) vs Simvastatin (IMPROVE-IT)28, The Saxagliptin assessment of vascular outcomes recorded in patients with diabetes mellitus-thrombolysis in myocardial infarction (SAVOR-TIMI)30 or the Further Cardiovascular Outcomes Research With PCSK9 Inhibition in Subjects With Elevated Risk (FOURIER)29 clinical trials which all evaluated the efficacy of pharmacological therapies to decrease atherothrombotic events and mortality in patients with established ASCVD or very high cardiovascular risk. The results from these clinical trials showed that patients classified as low-risk had a lower incidence of atherothrombotic events than the high-risk group in the following 24–36 months.
The aim of the current sub-study from the CORDIOPREV trial was not to evaluate the incidence of atherothrombotic events, but to compare the changes in MEF between risk categories according to TRS2P in the environment of a long-term dietary intervention. We found that both MedDiet and LFD improved MEF in a similar way in the low, moderate and high atherothrombotic risk groups. However, the low-risk TRS2P group showed a greater improvement in microvascular reactivity (assessed by the RHA) compared with the moderate and high-risk groups. These findings suggest that, although a healthy dietary pattern can beneficially affect BF in all patients in a similar way, microvascular reactivity to ischemia improves more in low-risk patients according to TRS2P. In previous studies, only patients classified as moderate or high-risk benefited from more intensive pharmacological treatment 28,29,30. However, in the current analysis, it seems that the low-risk patients benefited most from the dietary intervention. Therefore, although this improvement in MEF has not been correlated with a lower incidence of cardiovascular events yet, the role of dietary recommendations in all patients with cardiovascular disease should be highlighted, especially in low-risk groups who may not benefit from more intensive drug therapy and who may gain more from adherence to a healthy dietary pattern, according to the findings of the current study.
To our knowledge, this is the largest study up-to-date evaluating the long-term effects of two dietary healthy patterns on MEF (i.e., BF and RHA) in patients with CHD. However, there are certain limitations, including the lack of possibility of generalization to other populations without CVD, the fact that Mediterranean Diet was used in a country where it has a high acceptation and may not be extrapolated to other countries, or that we performed a high intensity dietary intervention which could be difficult to achieve in other settings.
In conclusion, a long-term healthy dietary intervention with MedDiet or LFD significantly improved microvascular BF in CHD patients, regardless of their baseline atherothrombotic risk (defined by the TRS2P). Microvascular reactivity to ischemia (as assessed by RHA) also improved in all CHD patients following a healthy dietary pattern, but this improvement was greater in patients at the low-risk category compared with those at the moderate and high-risk groups. Further research is needed to establish the long-term benefits of dietary intervensions in MEF in different patient populations.
Data availability
Data supporting the findings of this study may be requested to the corresponding author. Propierty of Data Policy from the Cordioprev Study apply to this article.
Abbreviations
- CHD:
-
Coronary heart disease
- NO:
-
Nitric oxide
- EF:
-
Endothelial function
- MedDiet:
-
Mediterranean diet
- FMD:
-
Flow-mediated dilation
- LFD:
-
Low-fat diet
- MEF:
-
Microvascular EF
- LDF:
-
Laser-doppler flowmetry
- BF:
-
Basal flow
- RHA:
-
Reactive hyperaemia area
- TIMI:
-
Thrombolysis in Myocardial Infarction Risk
- TRS2P:
-
TIMI Score for Secondary Prevention
- ASCVD:
-
Atherosclerotic cardiovascular disease
- APUT:
-
Arbitrary perfusion units per time
- MUFAs:
-
Monounsaturated fatty acids
- LDL:
-
Low-density lipoprotein
References
Deanfield, J. E., Halcox, J. P. & Rabelink, T. J. Endothelial function and dysfunction: Testing and clinical relevance. Circulation 115(10), 1285–1295. https://doi.org/10.1161/CIRCULATIONAHA.106.652859 (2007).
Hansson, G. K. Inflammation, atherosclerosis, and coronary artery disease. N. Engl. J. Med. 352(16), 1685–1695. https://doi.org/10.1056/nejmra043430 (2005).
Flammer, A. J. et al. The assessment of endothelial function: From research into clinical practice. Circulation 126(6), 753–767. https://doi.org/10.1161/CIRCULATIONAHA.112.093245 (2012).
Brunner, H. et al. Endothelial function and dysfunction. Part II: Association with cardiovascular risk factors and diseases. A statement by the Working Group on Endothelins and Endothelial Factors of the European Society of Hypertension. J. Hypertens. 23(2), 233–246. https://doi.org/10.1097/00004872-200502000-00001 (2005).
Torres-Peña, J. D., Rangel-Zuñiga, O. A., Alcala-Diaz, J. F., Lopez-Miranda, J. & Delgado-Lista, J. Mediterranean diet and endothelial function: A review of its effects at different vascular bed levels. Nutrients 12(8), 1–22. https://doi.org/10.3390/nu12082212 (2020).
Fuentes, F. et al. Chronic effects of a high-fat diet enriched with virgin olive oil and a low-fat diet enriched with α-linolenic acid on postprandial endothelial function in healthy men. Br. J. Nutr. 100(1), 159–165. https://doi.org/10.1017/S0007114508888708 (2008).
Phillips, S. A. et al. Benefit of low-fat over low-carbohydrate diet on endothelial health in obesity. Hypertension 51(2), 376–382. https://doi.org/10.1161/HYPERTENSIONAHA.107.101824 (2008).
Delgado-Lista, J. et al. Mediterranean diet and cardiovascular risk: beyond traditional risk factors. Crit. Rev. Food Sci. Nutr. 56(5), 788–801. https://doi.org/10.1080/10408398.2012.726660 (2016).
Schwingshackl, L. & Hoffmann, G. Mediterranean dietary pattern, inflammation and endothelial function: A systematic review and meta-analysis of intervention trials. Nutr. Metab. Cardiovasc. Dis. 24(9), 929–939. https://doi.org/10.1016/j.numecd.2014.03.003 (2014).
Torres-Peña, J. D. et al. Mediterranean diet improves endothelial function in patients with diabetes and prediabetes: A report from the CORDIOPREV study. Atherosclerosis 269, 50–56. https://doi.org/10.1016/j.atherosclerosis.2017.12.012 (2018).
Yubero-Serrano, E. M. et al. Mediterranean diet and endothelial function in patients with coronary heart disease: An analysis of the CORDIOPREV randomized controlled trial. PLoS Med. 17(9), e1003282. https://doi.org/10.1371/JOURNAL.PMED.1003282 (2020).
Mohler, E. R. et al. Endothelial function and weight loss: Comparison of low-carbohydrate and low-fat diets. Obesity 21(3), 504–509. https://doi.org/10.1002/oby.20055 (2013).
Barbosa-Yañez, R. L. et al. Acute endothelial benefits of fat restriction over carbohydrate restriction in type 2 diabetes mellitus: Beyond carbs and fats. Nutrients 10(12), 1859. https://doi.org/10.3390/nu10121859 (2018).
Seligman, B. G. S. et al. Intensive practical lifestyle intervention improves endothelial function in metabolic syndrome independent of weight loss: A randomized controlled trial. Metabolism 60(12), 1736–1740. https://doi.org/10.1016/j.metabol.2011.05.006 (2011).
Wycherley, T. P. et al. Long-term effects of weight loss with a very-low carbohydrate, low saturated fat diet on flow mediated dilatation in patients with type 2 diabetes: A randomised controlled trial. Atherosclerosis 252, 28–31. https://doi.org/10.1016/j.atherosclerosis.2016.07.908 (2016).
Corretti, M. C. et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: A report of the international brachial artery reactivity task force. J. Am. Coll. Cardiol. 39(2), 257–265. https://doi.org/10.1016/S0735-1097(01)01746-6 (2002).
Levy, B. I. et al. Impaired tissue perfusion a pathology common to hypertension, obesity, and diabetes mellitus. Circulation 118(9), 968–976. https://doi.org/10.1161/CIRCULATIONAHA.107.763730 (2008).
Ibrahimi, K. et al. Reproducibility and agreement of different non-invasive methods of endothelial function assessment. Microvasc. Res. 117, 50–56. https://doi.org/10.1016/j.mvr.2018.01.004 (2018).
Jekell, A., Kalani, M. & Kahan, T. The interrelation of endothelial function and microvascular reactivity in different vascular beds, and risk assessment in hypertension: Results from the Doxazosin–ramipril study. Heart Vessels 34(3), 484–495. https://doi.org/10.1007/s00380-018-1265-7 (2019).
Debbabi, H., Bonnin, P., Ducluzeau, P. H., Lefthériotis, G. & Levy, B. I. Noninvasive assessment of endothelial function in the skin microcirculation. Am. J. Hypertens. 23(5), 541–546. https://doi.org/10.1038/ajh.2010.10 (2010).
Agarwal, S. C., Allen, J., Murray, A. & Purcell, I. F. Laser Doppler assessment of dermal circulatory changes in people with coronary artery disease. Microvasc. Res. 84(1), 55–59. https://doi.org/10.1016/j.mvr.2012.02.002 (2012).
Cracowski, J. L., Minson, C. T., Salvat-Melis, M. & Halliwill, J. R. Methodological issues in the assessment of skin microvascular endothelial function in humans. Trends Pharmacol. Sci. 27(9), 503–508. https://doi.org/10.1016/j.tips.2006.07.008 (2006).
Ruano, J. et al. Phenolic content of virgin olive oil improves ischemic reactive hyperemia in hypercholesterolemic patients. J. Am. Coll. Cardiol. 46(10), 1864–1868. https://doi.org/10.1016/j.jacc.2005.06.078 (2005).
Jiménez-Morales, A. I. et al. NOS3 Glu298Asp polymorphism interacts with virgin olive oil phenols to determine the postprandial endothelial function in patients with the metabolic syndrome. J. Clin. Endocrinol. Metab. 96(10), E1694-702. https://doi.org/10.1210/jc.2011-1056 (2011).
Marin, C. et al. Mediterranean diet reduces endothelial damage and improves the regenerative capacity of endothelium. Am. J. Clin. Nutr. 93(2), 267–274. https://doi.org/10.3945/ajcn.110.006866 (2011).
Bohula, E. A. et al. Atherothrombotic risk stratification and the efficacy and safety of vorapaxar in patients with stable ischemic heart disease and previous myocardial infarction. Circulation 134(4), 304–313. https://doi.org/10.1161/CIRCULATIONAHA.115.019861 (2016).
Delgado-Lista, J. et al. CORonary Diet Intervention with Olive oil and cardiovascular PREVention study (the CORDIOPREV study): Rationale, methods, and baseline characteristics A clinical trial comparing the efficacy of a Mediterranean diet rich in olive oil versus a low-fat diet on cardiovascular disease in coronary patients. Am. Heart J. 177, 42–50. https://doi.org/10.1016/j.ahj.2016.04.011 (2016).
Bohula, E. A. et al. Atherothrombotic risk stratification and ezetimibe for secondary prevention. J. Am. Coll. Cardiol. 69(8), 911–921. https://doi.org/10.1016/j.jacc.2016.11.070 (2017).
Bohula, E. A. et al. Atherothrombotic risk stratification and magnitude of benefit of evolocumab in Fourier. Circulation 136(Supplement 1), A20183 (2017).
Bergmark, B. A. et al. Risk assessment in patients with diabetes with the TIMI risk score for atherothrombotic disease. Diabetes Care 41(3), 577–585. https://doi.org/10.2337/dc17-1736 (2018).
Rossi, R. et al. Flow-mediated vasodilation and the risk of developing hypertension in healthy postmenopausal women. J. Am. Coll. Cardiol. 44(8), 1636–1640. https://doi.org/10.1016/j.jacc.2004.07.027 (2004).
Mordi, I., Mordi, N., Delles, C. & Tzemos, N. Endothelial dysfunction in human essential hypertension. J. Hypertens. 34(8), 1464–1472. https://doi.org/10.1097/HJH.0000000000000965 (2016).
Serné, E. H. et al. Capillary recruitment is impaired in essential hypertension and relates to insulin’s metabolic and vascular actions. Cardiovasc. Res. 49(1), 161–168. https://doi.org/10.1016/S0008-6363(00)00198-X (2001).
Hellmann, M., Roustit, M. & Cracowski, J. L. Skin microvascular endothelial function as a biomarker in cardiovascular diseases?. Pharmacol. Rep. 67(4), 803–810. https://doi.org/10.1016/j.pharep.2015.05.008 (2015).
Settergren, M., Böhm, F., Rydén, L., Pernow, J. & Kalani, M. Lipid lowering versus pleiotropic effects of statins on skin microvascular function in patients with dysglycaemia and coronary artery disease. J. Intern. Med. 266(5), 492–498. https://doi.org/10.1111/j.1365-2796.2009.02128.x (2009).
Reriani, M. K. et al. Effects of statins on coronary and peripheral endothelial function in humans: A systematic review and metaanalysis of randomized controlled trials. Eur. J. Cardiovasc. Prev. Rehabil. 18(5), 704–716. https://doi.org/10.1177/1741826711398430 (2011).
Shannon, O. M. et al. Mediterranean diet increases endothelial function in adults: A systematic review and meta-analysis of randomized controlled trials. J. Nutr. 150(5), 1151–1159. https://doi.org/10.1093/jn/nxaa002 (2020).
Klonizakis, M., Alkhatib, A., Middleton, G. & Smith, M. F. Mediterranean diet- and exercise-induced improvement in age-dependent vascular activity. Clin. Sci. 124(9), 579–587. https://doi.org/10.1042/CS20120412 (2013).
Korakas, E., Dimitriadis, G., Raptis, A. & Lambadiari, V. Dietary composition and cardiovascular risk: A mediator or a Bystander?. Nutrients 10(12), 1912. https://doi.org/10.3390/nu10121912 (2018).
Yubero-Serrano, E. M., Lopez-Moreno, J., Gomez-Delgado, F. & Lopez-Miranda, J. Extra virgin olive oil: More than a healthy fat. Eur. J. Clin. Nutr. 72(Table 1), 8–17. https://doi.org/10.1038/s41430-018-0304-x (2019).
Estruch, R. et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 368(14), 1279–1290. https://doi.org/10.1056/NEJMoa1200303 (2013).
Estruch, R. Anti-inflammatory effects of the Mediterranean diet: The experience of the PREDIMED study. Proc. Nutr. Soc. 69, 333–340. https://doi.org/10.1017/S0029665110001539 (2010).
Funding
We received funding from CITOLIVA, CEAS, Junta de Andalucia (Consejeria de Salud, Consejeria de Agricultura y Pesca, Consejeria de Innovacion, Ciencia y Empresa), Diputaciones de Jaen y Cordoba, Centro de Excelencia en Investigacion sobre Aceite de Oliva y Salud and Ministerio de Medio Ambiente, Medio Rural y Marino and the Spanish Government. This work was also partly supported by research grants from the Ministerio de Ciencia e Innovacion (AGL2009-122270 to J L-M, FIS PI10/01041 to P P-M, FIS PI13/00023 to J D-L); Ministerio de Economia y Competitividad (AGL2012/39615 to J L-M); Consejeria de Salud, Junta de Andalucia (PI0193/09 to J L-M, PI-0252/09 to J D-L, and PI-0058/10 to P P-M, PI-0206-2013 to A G-R); Proyecto de Excelencia, Consejería de Economía, Innovación, Ciencia y Empleo (CVI-7450 to J L-M); Antonio Pablo Arenas-Larriva is supported by an ISCIII research contract (Programa Rio-Hortega). The study was also co-financed by the Fondo Europeo de Desarrollo Regional (FEDER). The CIBEROBN is an initiative of the Instituto de Salud Carlos III, Madrid, Spain. The funding bodies had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
J.L-M, P.P-M and J.D.-L. conceived the topic ; M.M-O, J.D.T-P and A.A-L drafted the manuscript; J.F.A-D and P.P-O formatted the bibliography; All authors reviewed the drafted manuscript; M.M-O, J.D.T-P, J.F.A-D, J.L-M, P.P-M, N.K and J.D.-L revised the final manuscript; All authors accepted the final manuscript; All authors made significant contributions to this article.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Millan-Orge, M., Torres-Peña, J.D., Arenas-Larriva, A. et al. Influence of dietary intervention on microvascular endothelial function in coronary patients and atherothrombotic risk of recurrence. Sci Rep 11, 20301 (2021). https://doi.org/10.1038/s41598-021-99514-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-99514-3
- Springer Nature Limited