Abstract
Nosocomial infections caused by enterococci are an ongoing global threat. Thus, finding therapeutic agents for the treatment of such infections are crucial. Some Enterococcus faecalis strains are able to produce antimicrobial peptides called bacteriocins. We analyzed 65 E. faecalis isolates from 43 food samples and 22 clinical samples in Egypt for 17 common bacteriocin-encoding genes of Enterococcus spp. These genes were absent in 11 isolates that showed antimicrobial activity putatively due to bacteriocins (three from food, including isolate OS13, and eight from clinical isolates). The food-isolated E. faecalis OS13 produced bacteriocin-like inhibitory substances (BLIS) named enterocin OS13, which comprised two peptides (enterocin OS13α OS13β) that inhibited the growth of antibiotic-resistant nosocomial E. faecalis and E. faecium isolates. The molecular weights of enterocin OS13α and OS13β were determined as 8079 Da and 7859 Da, respectively, and both were heat-labile. Enterocin OS13α was sensitive to proteinase K, while enterocin OS13β was resistant. Characterization of E. faecalis OS13 isolate revealed that it belonged to sequence type 116. It was non-hemolytic, bile salt hydrolase-negative, gelatinase-positive, and sensitive to ampicillin, penicillin, vancomycin, erythromycin, kanamycin, and gentamicin. In conclusion, BLIS as enterocin OS13α and OS13β represent antimicrobial agents with activities against antibiotic-resistant enterococcal isolates.
Similar content being viewed by others
Introduction
Lactic acid bacteria (LAB) are defined as aerotolerant Gram-positive cocci or bacilli that ferment sugars to produce lactic acid1,2. Enterococci are LAB, and they are found in the gastrointestinal tract of humans and animals as well as in feed, food, and healthcare units3. Most strains of Enterococcus faecalis are harmless commensals that may be beneficial to health (probiotics). In contrast, other strains are opportunistic pathogens, especially vancomycin-resistant enterococci (VRE) and multidrug-resistant enterococci (MDRE), causing nosocomial infections and acquiring antibiotic resistance determinants that become intrinsically resistant to commonly used antibiotics, leading to an increasingly serious problem in public health worldwide4. E. faecalis and E. faecium are recognized as the most common causes of nosocomial infections in their genus, causing urinary tract infection, postoperative wound infection, endocarditis, bacteremia, pneumonia, and meningitis5. The search for novel effective antimicrobial agents has become a global concern due to the increasing prevalence of MDRE and VRE. Over the past three decades, the rate of antibiotic discovery has slowed, and few antibiotics have been developed against VRE6. Furthermore, some enterococci have evolved resistance to the most recently-developed antimicrobial agents, such as quinupristin-dalfopristin, linezolid, daptomycin, and tigecycline7.
Antimicrobial peptides (AMPs) have drawn attention as alternatives to conventional antibiotics. Enterococci produce a variety of ribosomally-synthesized AMPs or bacteriocins8,9,10. There are three classes of bacteriocins. Briefly, class I consists of small, heat-stable, post-translationally modified peptides. Lantibiotics, due to the presence of the modified residues lanthionine and methyl-lanthionine, are a well-known example of that class. Some other bacteriocins are also considered members of class I, namely, those belonging to ribosomally-synthesized and post-translationally modified peptides that function as bacteriocins, such as circular bacteriocins, sactibiotics, and glycocins11. Class II consists of small, heat-stable peptides without modified residues. Class III consists of abundant, heat-labile proteins12,13.
Bacteriocins have been used in the food industry for over 50 years and are Generally Recognized As Safe (GRAS)14,15,16. The use of bacteriocins as a replacement for currently used antibiotics is promising15. Furthermore, resistance toward bacteriocins has rarely been observed17. Because enterococci are part of the healthy microbiota in humans, they are considered relatively safe but are not endowed with GRAS status18. However, some of them are used as probiotics19, and bacteriocin production adds an essential feature in their protection against pathogenic bacteria20.
Bacteriocins differ from antibiotics in that they are ribosomally synthesized and target bacteria closely related to the producing strain by different mechanisms of action12. These killing mechanisms include membranous pore formation, disruption of the cell wall or protein synthesis, and degradation of nucleic acids21. Narrow-spectrum antibacterials, such as bacteriocins, are an attractive approach in the battle against multidrug-resistant bacterial pathogens due to their limited resistance acquisition and trigger no significant disruption to the host microbiota. It worth mentioning that the use of traditional broad-spectrum antibiotics can disturb the host microbiota, affecting the crucial role that it plays in various functions, including nutrient and certain amino acids supply, vitamin production, and protection against pathogens22. Exposure to broad-spectrum antibiotics during infancy and early childhood is mostly unfavorable, as the early microbiota lacks diversity and stability, making it distinctively sensitive to disruption, besides the importance of the gut microbiota in the early development and education of the immune system23. Thus, if the infection's causative pathogen is well-known, the use of narrow-spectrum antimicrobials, such as bacteriocins, could potentially avoid these issues of hurting gut microbiota.
In these perspectives, the main objective of this study was to screen different E. faecalis isolates, obtained from food and clinical samples, for their ability to produce bacteriocins. Attempts were performed to purify and characterize BLIS with activity against nosocomial enterococci. One putative bacteriocinogenic isolate was studied in detail, and two BLIS were characterized from this isolate.
Materials and methods
Bacterial strains and culture conditions
The bacterial strains used in this study and their culture conditions are presented in Table 1. All strains were maintained in glycerol stock 40% (v/v) and stored at − 80 ºC.
Isolation and identification of E. faecalis
Different food samples (milk products; mozzarella cheese and buttermilk—pastries; commercial cakes and bread) and clinical samples (urine and stool) were collected in sterile plastic cups from Beni-Suef City, Egypt, and refrigerated for 24 h prior to processing. Urine sample precipitates (collected after centrifugation at 5000×g for 10 min) and 1 g of each of the food and stool samples were inoculated into tubes containing 5 mL of GM17 broth (Oxoid, Hampshire, UK) and incubated aerobically at 37 °C for 24 h.
Enterococci were isolated by selective culture on bile esculin agar (Oxoid), where they grow in the presence of 4% (w/v) bile and hydrolyze esculin to esculetin that reacts with Fe3+ to form a dark brown to black precipitate on the agar plate. The resultant black colonies were presumptively identified as Enterococcus sp. using the l-pyrrolidonyl-β-naphthylamide (PYR) test and then identified at species level using the API 50 CHL system (bioMérieux, Marcy l’Etoile, France) according to the manufacturer’s instructions.
Genomic DNA isolation
It was performed with some modifications of a previously described protocol24. Briefly, 1.5 ml of an overnight culture was centrifuged for 10 min at 3000×g, and the supernatant was discarded. The pellet was resuspended in 200 μL of spheroplast buffer (10% [w/v] sucrose, 25 mM Tris [pH 8.4], 25 mM EDTA [pH 8.0], 2 mg/mL lysozyme, 1 mg/mL proteinase K, and 0.4 mg/mL RNase A), vortexed, and incubated at 37 ºC for 10 min until cell lysis occurred. Then, 50 μL of each of 5% (w/v) sodium dodecyl sulfate (SDS) (lysis buffer 1) and 5 M NaCl (lysis buffer 2) were added, mixed, and incubated at 65 ºC for 5 min. Next, 100 μL of neutralizing buffer (60 mL 5 M potassium acetate, 11.5 mL glacial acetic acid, and 28.5 mL dH2O) was added. The sample was vortexed, placed on ice for 5 min, and centrifuged at 18,000×g at 4 ºC for 15 min. The supernatant (approximately 400 μL) was transferred to a new tube, mixed with an equal volume of isopropanol, left to stand for 5 min at room temperature, and centrifuged at 18,000×g at room temperature for 15 min to precipitate the DNA. The resultant pellet was washed with 70% (v/v) ethanol by centrifugation at 18,000×g at room temperature for 5 min and finally air-dried, resuspended in 50 μL 1× TE buffer [pH 8], and stored in a refrigerator at 4 ºC. The DNA purity and concentration were determined by optical density measurement using a NanoDrop ND1000 spectrophotometer (Thermo Scientific, Wilmington, DE, USA).
Polymerase chain reaction (PCR) amplification and sequencing of 16S rDNA gene
These were accomplished using primers 11F and 4R (Table S1). The PCR amplicon of interest was detected by agarose gel electrophoreses25 using 1% (w/v) agarose gels with reference to 1 kbp DNA ladder (Fermentas, Vantaa, Finland). Any impurities were removed from the PCR product using the QIAquick PCR purification kit (Qiagen, Hilden, Germany). Quantification of the PCR products was determined by optical density measurement using a NanoDrop ND1000 spectrophotometer (Thermo Scientific, Wilmington, DE, USA). The PCR product was sequenced and analyzed using an ABI Prism BigDye Terminator v3.1 Ready Reaction Cycle Sequencing Kit on an ABI Prism 3100 Genetic Analyzer, according to the manufacturer’s instructions. The sequences were assembled by BioEdit v7.0.9.0 software, and a homology search of the National Center for Biotechnology Information (NCBI) database was performed using BLAST. Multiple sequence alignment was performed, and molecular phylogenies were evaluated using MEGA7 software using the neighbor-joining method, and the evolutionary distances were computed using the Kimura two-parameter method26.
PCR screening for bacteriocin structural genes
The presence of genes encoding 17 known bacteriocins in Enterococcus spp. were determined by PCR amplification using specific primers purchased from Invitrogen (Carlsbad, CA, USA) (Table S1). DNA samples from different standard strains belonging to Laboratory of Microbiology, Department of Biochemistry and Microbiology, Faculty of Sciences of Ghent University, Ghent, Belgium, (LMG) culture collections with known bacteriocin genes were used as positive controls for the PCR reactions (Table 1). The PCR product of interest was detected by agarose gel electrophoreses25 using 1.5% (w/v) agarose gels with reference to a 100-bp DNA ladder (Fermentas).
Screening for antimicrobial activity production
The antimicrobial activity was detected using a deferred inhibition test27. Briefly, the colonies were overlaid with 5 mL of soft agar containing 70 µl of the indicator strains which were grown to late exponential phase (Table 1). A confirmatory test was established by adding aliquots of the pH-adjusted supernatant (50 µl) into 0.5-cm wells, made in the inoculated agar plates with indicator strain. Then, the plates were incubated overnight and checked for the presence of growth inhibition zones.
Quantitative estimation of BLIS in the cell-free culture supernatant was performed using a microtiter plate assay28, where 100× dilutions of the sensitive indicator strains were exposed to twofold serial dilutions of bacteriocin in growth media. The plates were incubated overnight, and the growth was measured spectrophotometrically at 620 nm using a microtiter plate reader (iEMS Reader; Labsystems, Helsinki, Finland). One arbitrary activity unit (AU) was defined as the reciprocal of the highest dilution of bacteriocin, causing 50% growth inhibition of the treated indicator strain by measuring growth turbidity inhibition at 620 nm in the microtiter plate reader compared to the untreated control29. The bacteriocin activity was calculated according to the following equation; Bacteriocin activity (AU/mL) = (d × 1/m), where “d”; is the used dilution factor and “m” is the highest dilution causing 50% growth inhibition.
Determination of virulence traits (hemolytic activity, proteolytic gelatinase activity, and bile salt hydrolase activity)
Hemolytic activity, being alpha, beta, or gamma, was determined by streaking putative bacteriocinogenic E. faecalis isolates onto a fresh plate of Columbia blood agar (Oxoid) containing 5% (v/v) defibrinated horse blood and incubating at 37 °C for 24 h. The formation of a clear zone around the colonies indicated beta complete hemolytic activity. In contrast, the formation of greenish discoloration surrounding the colonies indicated alpha partial hemolytic activity, and the absence of any hemolysis was referred to as gamma or no hemolysis. Proteolytic gelatinase activity was detected by inoculating E. faecalis isolates into tubes containing gelatin medium composed of 0.5% (w/v) peptone, 2% (w/v) gelatin, 0.3% (w/v) beef extract, 0.5% (w/v) NaCl and final pH was adjusted to 7.2. All tubes, including the control (uninoculated), were incubated at 37 °C for 24 h. Gelatin liquefaction observed after keeping the tubes at 4 °C for 3 h, indicated positive gelatinase activity. Putative bacteriocinogenic E. faecalis isolates were cultured on both control MRS agar and MRS agar containing 0.5% (w/v) thioglycolate and 0.5% (w/v) sodium glychodeoxycholate (bile salt) to investigate bile salt hydrolase activity. The formation of white precipitate around the colonies indicated bile salt hydrolase activity.
Antibiotic susceptibility testing and minimum inhibitory concentration (MIC) determination
In order to perform antibiotic susceptibility typing of the 11 putative bacteriocinogenic E. faecalis isolates to check whether they are relevant to each other or from different clones, and to overview their biosafety for further applications, the Clinical and Laboratory Standards Institute (CLSI) broth microdilution method in microtiter plates30 was used to determine the antibiotic resistance phenotype and MIC of these isolates against 13 antibiotics with different concentration ranges (Table S2), using Mueller–Hinton broth (Oxoid). The microtiter plates were incubated at 37 °C for 20 h before visually determining the MIC, which is the lowest drug concentration that causes complete inhibition of microorganism growth.
Multilocus sequence typing (MLST)
An MLST scheme based on seven housekeeping genes was performed to investigate the epidemiology and population structure of the 11 putative bacteriocinogenic E. faecalis isolates31. The PCR primers are listed in Table S1. The allelic profile or sequence type (ST) was determined, according to the E. faecalis MLST database (http://efaecalis.mlst.net/)31. The ST distribution among all putative bacteriocinogenic E. faecalis isolates, included in the MLST database, was evaluated using eBurst v332.
Purification of BLIS
The BLIS was purified as previously described33. Briefly, 2 L of E. faecalis OS13 cultivated in MRS broth at 30 °C for 18 h was used for further purification steps. After centrifugation at 14,500×g for 10 min at 4 °C (Sorvall RC-6; Kendro Laboratory Products, Asheville, NC, USA) and filtration (500 mL Steritop 0.22 µm filter system; Millipore, Dublin, Ireland), the supernatant was subjected to ammonium sulfate precipitation 50% (w/v) and shaken vigorously at 4 °C for 30 min. The protein pellet was harvested by centrifugation at 14,500×g for 10 min at 4 °C and then redissolved in 40 mL of distilled water to obtain a 50× concentrated crude BLIS solution. Whenever necessary, the pH was adjusted to 3.5 using 0.1 M HCl.
The crude BLIS solution underwent cation exchange chromatography using a 10-mL SP Sepharose Fast Flow column (GE Healthcare Bioscience, Uppsala, Sweden) pre-washed with 200 mL distilled water and equilibrated with 10 mL sodium acetate (10 mM, pH 5.0). After applying the crude BLIS, the column was washed with 50 mL sodium phosphate buffer (20 mM, pH 6.8) and finally eluted using 20 mL of 1 M NaCl. The BLIS was further purified by reverse-phase chromatography on an ÄKTA FPLC purifier system (Amersham Pharmacia Biotech, Amersham, UK). First, the sample was applied to a Resource RPC 1 mL column (Amersham Pharmacia Biotech) pre-equilibrated with 0.1% (v/v) trifluoroacetic acid (TFA) in water (Buffer A) and eluted using a 30 column volume (CV) linear gradient from 0 to 100% (v/v) isopropanol containing 0.1% (v/v) TFA (Buffer B). Fractions of 2 mL each were collected. The most active fraction (determined by microtiter plate assay) was further diluted in 20 mL 0.1% (v/v) TFA in water and applied to a Sephasil Peptide C8 5-µm ST 4.6/250 column (Amersham Pharmacia Biotech). Elution was performed using 0.5 CV (10% (v/v) Buffer B), 1 CV (10–30% (v/v) Buffer B), 5 CV (30–45% (v/v) Buffer B), and finally 2 CV (45–100% (v/v) Buffer B) at a flow rate of 0.4 mL/min. The peaks were monitored at 214, 254, and 280 nm, and fractions (1 mL each) were collected.
Sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) and mass spectrometry
After cation exchange chromatography, the partially purified BLIS was analyzed by one-dimensional SDS-PAGE (Mini-PROTEAN electrophoresis apparatus; Bio-Rad, Hercules, CA, USA) using a 4% (v/v) stacking gel and 15% (v/v) separating gel. A pre-stained molecular mass protein marker with a range of 7000–70,000 Da was used. The BLIS was separated at 180 V for 45 min, and the gel was divided into two identical vertical parts, one of which was stained and visualized using silver nitrate. The other part was used to identify antibacterial activity by first washing the gel three times with distilled water (40 min/wash) to remove excess SDS. Then, the gel was transferred to an MRS agar plate and overlaid with 10 mL of soft MRS agar containing the indicator microorganism (L. sakei LMG 2313) and incubated overnight at 30 °C. The molecular weight of the purified peptide after reverse-phase chromatography was further confirmed with matrix-assisted laser desorption ionization (MALDI)-TOF/MS (Voyager-DE RP; Applied Biosystems, Foster City, CA, USA), as described34,35. Briefly, 0.5 μL of the sample was mixed with 0.5 μL of the matrix mixed with 15 mg/mL alpha-cyano-4-hydroxycinnamic acid and deposited on a ground steel MALDI plate (Bruker Daltonics, Billerica, MA, USA). The mass window was adjusted between 4000 and 10,000 Da in the linear positive ion mode, with an acceleration voltage of 25 kV. A peptide mass similarity search was performed using ExPASy with the TagIdent tool (http://www.pdg.cnb.uam.es/cursos/Leon_2003/pages/visualizacion/programas_manuales/spdbv_userguide/us.expasy.org/tools/tagident.html).
Effect of heat and proteinase K enzyme
The thermal stability of both crude and purified BLIS was determined by heating the samples at 100 ºC for 30 min. Sensitivity toward proteinase K (Sigma-Aldrich, St. Louis, MO, USA) at a final concentration of 1 mg/mL was determined for both the crude and purified BLIS by incubating samples (pH 7.5) with or without enzyme at 37 °C for 60 min. Then, the activity of each sample was compared with the untreated sample using a microtiter plate assay with the indicator strain L. sakei LMG 2313.
Results
Isolation and identification of E. faecalis
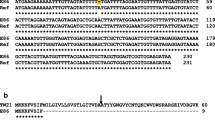
The 65 isolates (43 from food and 22 from clinical samples) that were collected from various food and healthcare units were positive for esculin hydrolysis on bile esculin agar and for l-pyroglutamic acid beta-naphthylamide hydrolysis on PYR discs (results not shown). They were identified at the species level as E. faecalis using an API 50 CHL carbohydrate fermentation kit and were positive for glycerol, ribose, galactose, glucose, fructose, mannose, mannitol, sorbitol, N-acetyl glucosamine, amygdalin, arbutin, esculin, salicin, cellobiose, maltose, saccharose, trehalose, melezitose, and tagatose. Furthermore, 16S rDNA sequence analysis confirmed their identity as E. faecalis. The obtained sequences of the bacteriocinogenic isolates were submitted to the NCBI GenBank database under specific accession numbers (Table S3). The partial 16S rRNA gene sequences were aligned to closely related species retrieved from the NCBI GenBank database and assembled in MEGA7 software to construct a phylogenetic tree (Fig. 1).
Screening for bacteriocin genes and spectrum of antimicrobial activity
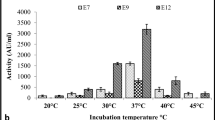
Interestingly, when the putative bacteriocinogenic E. faecalis isolates were screened by PCR for genes corresponding to any of 17 known bacteriocin genes, none of these genes were found in 11 of the isolates (three from food samples and eight from clinical samples). Of them, the food-isolated E. faecalis OS13 produced the most potent antimicrobial activity and was chosen for further study and purification of its biologically active antimicrobial substance. Some Gram-positive bacteria, such as L. sakei, L. plantarum, E. faecalis, and E. faecium were sensitive to the antimicrobial activity of the OS13 isolate. Still, other Gram-positive bacteria, such as Listeria, Bacillus, and Staphylococcus, and all tested Gram-negative bacteria were resistant. The most potent antimicrobial activity was shown against L. sakei LMG 2313, which was then used as the primary indicator microorganism during purification.
Characterization of the isolates producing antimicrobial activities at biosafety and epidemiology levels
All selected 11 isolates with antimicrobial activities demonstrated bile salt hydrolase activity except strains OS11, 13, 16, and 64. Furthermore, all strains were non-hemolytic and gelatinase-positive. They were sensitive to ampicillin and vancomycin (Table S2) but resistant to clindamycin, fusidic acid, apramycin, streptomycin, tetracycline, and polymyxin B (Table S2, Fig. S1). Other antibiotics sensitivities and resistance patterns are listed (Table S2). Clustering based on the resistance pattern of these isolates is presented in Fig. S1. Finally, the multilocus sequence typing (MLST) of seven housekeeping genes31 revealed that these isolates belonged to ST 6 and ST116 (Table S3). ST116, representing E. faecalis OS13, did not belong to clonal complex (CC) 6 or CC9, which are commonly spread in the hospital environment (Fig. S2).
Purification of BLIS from E. faecalis OS13
The BLIS produced from isolate OS13 was purified using successive purification steps (Table 2). The activity (AU/mL) was determined by microtiter plate assay using L. sakei LMG 2313 as the indicator strain. The final step of reverse-phase chromatography using a Sephasil Peptide C8 column allowed the separation of two peaks with antimicrobial activity, eluted at approximately 39.5% (v/v) and 40.5% (v/v) isopropanol, respectively (Fig. 2).
Second reversed-phase chromatography using the Sephasil peptide C8 column. This shows two peaks with antimicrobial activity eluted at approximately 39.5% and 40.5% (v/v) isopropanol. The solid line shows the absorbance at 214 nm, while the broken line shows the elution gradient of isopropanol. The antimicrobial activity (AU/mL) is shown as gray columns.
Sodium dodecyl sulfate (SDS)-polyacrylamide gel electrophoresis (PAGE) and mass spectrometry
The partially purified BLIS obtained by cation exchange chromatography were analyzed by one-dimensional SDS-PAGE. A single diffuse band with a molecular weight of 7–16.5 kDa was observed that produced a clear zone of inhibition against L. sakei LMG 2313 (Fig. 3A). The molecular weights of the purified agents were further determined by MALDI-time of flight mass spectrometry (TOF/MS) analysis. The two BLIS were designated enterocin OS13α and OS13β and showed a molecular weight of 8079.1 Da (Fig. 3B) and 7858.6 Da (Fig. 3C), respectively. A peptide mass similarity search using ExPASy revealed that there were no molecular weight similarities with any other AMPs except holotricin-2 (7858 Da)36.
SDS-PAGE (A) of protein marker (i) compared to partially purified BLIS after cation exchange chromatography (ii) and showed a single diffused band in the bioassay experiment (iii) with a molecular weight between 7 and 16.5 kDa. The full-length gels are presented in Supplementary Figure S3; (B) MALDI-TOV mass spectrometry analysis of enterocin OS13α obtained from second reversed-phase chromatography and (C) MALDI-TOV mass spectrometry analysis of enterocin OS13β obtained from second reversed-phase chromatography.
Effect of heat and proteinase K enzyme
When the crude BLIS with an initial activity of 10,240 AU/mL was heated to 100 °C, the activity was reduced to 640 AU/mL (6.25%). Also, the antimicrobial activity was decreased to 1280 AU/mL (12.5%) after proteinase K treatment. Repeating the same treatment with the concentrated purified enterocin OS13α with initial activity (1,024,000 AU/mL) and enterocin OS13β with initial activity (128,000 AU/mL) confirmed the sensitivity of both peptides to heat treatment, and their activities were entirely abolished. Proteinase K treatment reduced the activity of enterocin OS13α to 512,000 AU/mL (50%), but enterocin OS13β remained unaffected with an activity of 128,000 AU/mL.
Discussion
Enterococcus faecalis are widely spread in the environment and are commonly isolated from foodstuffs and clinical samples37. E. faecalis and other LAB have attracted more attention over the last few years due to the production of many useful AMPs or BLIS, with several safe applications in the food industry and medical treatments38,39. The identification of antimicrobial agents to treat antibiotic-resistant nosocomial enterococci is crucial because the treatment of such infections is becoming increasingly problematic. In addition, enterococci gained greater medical and public attention since the mid-1980s when vancomycin resistance was first present in clinical isolates (VRE)40. BLIS with the potential to inhibit the growth of such bacteria could remedy infections without affecting endogenous beneficial microbiota or risking dissemination of R-factors to non-enterococcal pathogens (e.g., vancomycin-intermediate Staphylococcus aureus).
Our study searched for suitable candidate BLIS in 65 E. faecalis isolates from Egypt of food and clinical origin. The 11 unknown putative bacteriocinogenic E. faecalis isolates were characterized epidemiologically by MLST and tested for antibiotic resistance, virulence traits, and antimicrobial activities. Our study showed that, E. faecalis OS13 produced highly active (> 106 AU/mL) BLIS designated enterocin OS13α and OS13β that had antimicrobial activity against some Gram-positive bacteria, such as L. sakei, L. plantarum, E. faecalis, and E. faecium, but not against Gram-negative bacteria. Generally, the bacteriocins produced from Gram-positive bacteria are active against closely related species and not directly active against Gram-negative bacteria. However, some other bacteriocins from LAB showed antagonistic activities against both Gram-positive and Gram-negative bacteria, like enterocin E76041, enterocin E50-5242, and salivaricin SMXD5143. Owing to the narrow-spectrum capabilities of enterocin OS13α and OS13β against target pathogens, they are favored when compared with conventional broad-spectrum antibiotics that can interfere with the host microbiota, affecting their crucial beneficial roles22. Especially during infancy and early childhood, exposure to broad-spectrum antibiotics is often unfavorable, as the early microbiota lacks diversity and stability, rendering it distinctly vulnerable to disturbance, in addition to the importance of intestinal microbiota in early development and education of the immune system23.
Noticeably, bacteriocins from isolate OS13 were active against multi-resistant nosocomial enterococci as Enterococcus faecalis V583, which was the first VRE Enterococcus isolated in the United States, and it was also resistant to high levels of aminoglycosides, macrolides, lincosamides, and streptogramin B44. Therefore, BLIS could represent a non-conventional alternative of interest to combat pathogens like enterococci, recognizing that the presence of natural resistance prevents a variety of modern drugs widely used, such as cephalosporins and quinolones, from working effectively against enterococcal infections45. Most VREs are also resistant to antibiotics as ampicillin, vancomycin, and aminoglycosides, widely used in the hospital environment. Therefore, only a few therapeutic options are commercially available to treat multidrug-resistant VRE infections, including linezolid, tedizolid, tigecycline, and daptomycin46,47. The increased use of these last-source antibiotics and the ability of enterococci to readily acquire new resistance determinants are currently raising the need to find alternative therapeutics and explore the effectiveness of natural antimicrobials such as bacteriocins.
In this study, purification of two BLIS, OS13α and OS13β, from strain OS13 and based on their chromatographic properties exposed that both BLIS were cationic and hydrophobic, which is in agreement with most bacteriocins purified from LAB48,49,50,51. At each purification level, the antimicrobial activity decreased, especially after reverse-phase chromatography, which was observed in other studies34,52. SDS-PAGE did not accurately determine the molecular weight of both BLIS and was unable to differentiate between them53,54.
Although both enterocin OS13α and OS13β were heat-labile, and their activity was wholly abolished after heating at 100 ºC for 30 min, their activity together as a crude BLIS in the supernatant was decreased to 6.25% following heat treatment. There are previous reports of many BLIS becoming less heat-stable during subsequent purification steps55,56. The larger size of enterocin OS13α and OS13β being 8079.1 Da and 7858.6 Da, respectively, could interpret the reasons behind their heat sensitivity39,57,58. Although the crude BLIS with an initial activity of 10,240 AU/mL was decreased to be 1,280 AU/mL (12.5%) after proteinase K treatment but the purified enterocin OS13α was sensitive to proteinase K (50% reduction in its activity), which strongly suggests its proteinaceous nature52,59. Also, enterocin OS13β was resistant to proteinase K, and this is probably not due to the absence of digestion sites but more likely due to a tightly folded structure, making it inaccessible to enzymatic digestion60,61. The variation in sensitivity of crude BLIS compared to purified ones to proteinase K could indicate that the OS13 isolate might also produce other BLIS besides OS13α and OS13β that is/are more sensitive to proteinase K but was/were not isolated and purified.
Generally, Enterococcus spp. found in food are presumed less virulent than clinical isolates62,63. Regarding the virulence traits of strain OS13, neither hemolytic activity nor bile salt hydrolase activity was demonstrated, while gelatinase activity was observed. Cytolysin (also called hemolysin) is a lantibiotic, but it differs from most lantibiotics because it is both antibacterial and hemolytic64. A higher incidence of cytolysin genes has been shown in clinical isolates (33%) compared with food isolates (6%)65. In our study, PCR analysis was used to confirm the absence of the cytolysin gene cluster (cyl). Although E. faecalis can be an opportunistic pathogen that possesses bile salt hydrolase activity66, such activity might be a desirable trait for a probiotic bacterium since it could maximize its ability to survive in the hostile environment of the gastrointestinal tract67. The gelatinase enzyme is involved in the virulence of Enterococcus sp. and hydrolyzes gelatin, casein, hemoglobin, and other bioactive peptides65. The primary role of gelatinase in enterococcal pathogenesis is to provide nutrients to the bacteria by degrading host tissue. However, it also appears to play a role in biofilm formation68.
The food chain is considered the primary transmission route of antibiotic-resistant bacteria between populations. Enterococcus sp. behave as opportunistic pathogens in nosocomial infections and spread antibiotic resistance through the food chain with potential risks to humans69. In biosafety evaluations of enterococci, their resistance to glycopeptides, such as vancomycin, should be considered70. In our study, the pathogenic potential of the food isolated E. faecalis OS13, and the spectrum of resistance to various antibiotics was determined. OS13 was sensitive to ampicillin, penicillin G, vancomycin, erythromycin, kanamycin, and gentamicin. It was resistant to chloramphenicol, streptomycin, tetracycline, clindamycin, fusidic acid, and polymyxin B. These results are in agreement with previous publications71,72, where all tested E. faecalis strains were sensitive to ampicillin, penicillin, and vancomycin. Resistance to chloramphenicol, tetracycline, erythromycin, gentamicin, and kanamycin is becoming common among enterococci from different sources due to the abuse of antibiotics in clinics, animal and fish farming, and agriculture. Thus, enterococcal antibiotic resistance is not exclusive to the clinical field and is also prevalent in the food industry71.
Although MLST is a tool for global epidemiological studies, the possible role of plasmids in transferring virulence between different strains should be considered73. MLST analysis of E. faecalis OS13 revealed that it belongs to ST116 and CC116. E. faecalis with ST116 has been reported as isolated twice from human clinical samples; vancomycin-resistant E. faecalis from a blood sample in Denmark and E. faecalis DQ287 from a catheter in Cuba74,75. To our knowledge, ours is the first report of the isolation of E. faecalis with ST116 from non-human samples.
The ability of CC116 to spread in hospitals and cause infection is unknown. However the most common clonal complexes that spread in the hospital environment are CC2, CC6, and CC931,76.
Conclusion
The food-isolated E. faecalis OS13 produced BLIS named enterocin OS13α (8079 Da) and OS13β (7859 Da), with activities against VRE and MDRE. MLST of E. faecalis OS13 revealed its belongings to ST116, being the first from non-human samples. E. faecalis OS13 was non-hemolytic, bile salt hydrolase-negative, and sensitive to ampicillin, penicillin, vancomycin, erythromycin, kanamycin, and gentamicin, suggesting several safe applications in the food industry and medical treatments. Although our BLIS showed sensitivity to heat treatments, they could be used for preservation of raw or minimally processed foods stored at low temperatures besides their likely role in the treatment of clinical infections with VRE and MDRE. Future works are still required to figure out the amino acid sequences, structures, encoding genes, and mode of actions of such BLIS.
References
Chun, W. & Hancock, R. E. Action of lysozyme and nisin mixtures against lactic acid bacteria. Int. J. Food Microbiol. 60, 25–32. https://doi.org/10.1016/s0168-1605(00)00330-5 (2000).
Parada, J. L., Caron, C. R., Medeiros, A. B. P. & Soccol, C. R. Bacteriocins from lactic acid bacteria: Purification, properties and use as biopreservatives. Braz. Arch. Biol. Technol. 50, 512–542 (2007).
Sánchez, J. et al. Cloning and heterologous production of Hiracin JM79, a Sec-dependent bacteriocin produced by Enterococcus hirae DCH5, in lactic acid bacteria and Pichia pastoris. Appl. Environ. Microbiol. 74, 2471–2479. https://doi.org/10.1128/aem.02559-07 (2008).
Aakra, A., Nyquist, O. L., Snipen, L., Reiersen, T. S. & Nes, I. F. Survey of genomic diversity among Enterococcus faecalis strains by microarray-based comparative genomic hybridization. Appl. Environ. Microbiol. 73, 2207–2217. https://doi.org/10.1128/aem.01599-06 (2007).
Baldassarri, L., Creti, R., Montanaro, L., Orefici, G. & Arciola, C. R. Pathogenesis of implant infections by enterococci. Int. J. Artif. Organs 28, 1101–1109. https://doi.org/10.1177/039139880502801107 (2005).
Coates, A. R. & Hu, Y. Novel approaches to developing new antibiotics for bacterial infections. Br. J. Pharmacol. 152, 1147–1154. https://doi.org/10.1038/sj.bjp.0707432 (2007).
Kristich, C. J., Rice, L. B. & Arias, C. A. In Enterococci: From Commensals to Leading Causes of Drug Resistant Infection (eds Gilmore, M. S. et al.) (Massachusetts Eye and Ear Infirmary, 2014).
Sánchez, J. et al. Antimicrobial and safety aspects, and biotechnological potential of bacteriocinogenic enterococci isolated from mallard ducks (Anas platyrhynchos). Int. J. Food Microbiol. 117, 295–305. https://doi.org/10.1016/j.ijfoodmicro.2007.04.012 (2007).
Nilsen, T., Nes, I. F. & Holo, H. Enterolysin A, a cell wall-degrading bacteriocin from Enterococcus faecalis LMG 2333. App. Environ. Microbiol. 69, 2975–2984. https://doi.org/10.1128/aem.69.5.2975-2984.2003 (2003).
Franz, C. M., van Belkum, M. J., Holzapfel, W. H., Abriouel, H. & Gálvez, A. Diversity of enterococcal bacteriocins and their grouping in a new classification scheme. FEMS Microbiol. Rev. 31, 293–310. https://doi.org/10.1111/j.1574-6976.2007.00064.x (2007).
Acedo, J. Z., Chiorean, S., Vederas, J. C. & van Belkum, M. J. The expanding structural variety among bacteriocins from Gram-positive bacteria. FEMS Microbiol. Rev. 42, 805–828. https://doi.org/10.1093/femsre/fuy033 (2018).
Nes, I. F., Diep, D. B. & Holo, H. Bacteriocin diversity in Streptococcus and Enterococcus. J. Bacteriol. 189, 1189–1198. https://doi.org/10.1128/jb.01254-06 (2007).
Cotter, P. D., Hill, C. & Ross, R. P. Bacteriocins: Developing innate immunity for food. Nat. Rev. Microbiol. 3, 777–788. https://doi.org/10.1038/nrmicro1273 (2005).
Cleveland, J., Montville, T. J., Nes, I. F. & Chikindas, M. L. Bacteriocins: Safe, natural antimicrobials for food preservation. Int. J. Food Microbiol. 71, 1–20. https://doi.org/10.1016/s0168-1605(01)00560-8 (2001).
Papagianni, M. Ribosomally synthesized peptides with antimicrobial properties: Biosynthesis, structure, function, and applications. Biotechnol. Adv. 21, 465–499. https://doi.org/10.1016/s0734-9750(03)00077-6 (2003).
De Martinis, E. C., Públio, M. R., Santarosa, P. R. & Freitas, F. Z. Antilisterial activity of lactic acid bacteria isolated from vacuum-packaged Brazilian meat and meat products. Braz. J. Microbiol. 32, 32–37 (2001).
Giuliani, A., Pirri, G. & Nicoletto, S. Antimicrobial peptides: An overview of a promising class of therapeutics. Open Life Sci. 2, 1–33 (2007).
Huys, G. et al. Microbial characterization of probiotics–advisory report of the Working Group “8651 Probiotics” of the Belgian Superior Health Council (SHC). Mol. Nutr. Food Res. 57, 1479–1504. https://doi.org/10.1002/mnfr.201300065 (2013).
Franz, C. M., Huch, M., Abriouel, H., Holzapfel, W. & Gálvez, A. Enterococci as probiotics and their implications in food safety. Int. J. Food Microbiol. 151, 125–140. https://doi.org/10.1016/j.ijfoodmicro.2011.08.014 (2011).
Nissen-Meyer, J., Oppegård, C., Rogne, P., Haugen, H. S. & Kristiansen, P. E. Structure and mode-of-action of the two-peptide (class-IIb) bacteriocins. Probiotics Antimicrob. Proteins 2, 52–60. https://doi.org/10.1007/s12602-009-9021-z (2010).
Riley, M. A. Molecular mechanisms of bacteriocin evolution. Annu. Rev. Genet. 32, 255–278. https://doi.org/10.1146/annurev.genet.32.1.255 (1998).
Langdon, A., Crook, N. & Dantas, G. The effects of antibiotics on the microbiome throughout development and alternative approaches for therapeutic modulation. Genome Med. 8, 39. https://doi.org/10.1186/s13073-016-0294-z (2016).
Schulfer, A. & Blaser, M. J. Risks of antibiotic exposures early in life on the developing microbiome. PLoS Pathog. 11, e1004903. https://doi.org/10.1371/journal.ppat.1004903 (2015).
Birri, D. J., Brede, D. A. & Nes, I. F. Salivaricin D, a novel intrinsically trypsin-resistant lantibiotic from Streptococcus salivarius 5M6c isolated from a healthy infant. Appl. Environ. Microbiol. 78, 402–410. https://doi.org/10.1128/aem.06588-11 (2012).
Sambrook, H. Molecular Cloning: A Laboratory Manual (Cold Spring Harbor, 1989).
Tamura, K., Dudley, J., Nei, M. & Kumar, S. MEGA4: Molecular Evolutionary Genetics Analysis (MEGA) software version 4.0. Mol. Biol. Evol. 24, 1596–1599. https://doi.org/10.1093/molbev/msm092 (2007).
De Vuyst, L., Callewaert, R. & Pot, B. Characterization of the antagonistic activity of Lactobacillus amylovorus DCE 471 and large scale isolation of its bacteriocin amylovorin L471. Syst. Appl. Microbiol. 19, 9–20 (1996).
Holo, H., Nilssen, O. & Nes, I. F. Lactococcin A, a new bacteriocin from Lactococcus lactis subsp. cremoris: Isolation and characterization of the protein and its gene. J. Bacteriol. 173, 3879–3887. https://doi.org/10.1128/jb.173.12.3879-3887.1991 (1991).
Chen, Y. S. et al. Leucocin C-607, a novel bacteriocin from the multiple-bacteriocin-producing Leuconostoc pseudomesenteroides 607 Isolated from Persimmon. Probiotics Antimicrob. Proteins 10, 148–156. https://doi.org/10.1007/s12602-017-9359-6 (2018).
Clinical & Institute, L. S. Vol. 32 (Clinical and Laboratory Standards Institute Wayne, PA, 2012).
Ruiz-Garbajosa, P. et al. Multilocus sequence typing scheme for Enterococcus faecalis reveals hospital-adapted genetic complexes in a background of high rates of recombination. J. Clin. Microbiol. 44, 2220–2228. https://doi.org/10.1128/jcm.02596-05 (2006).
Feil, E. J., Li, B. C., Aanensen, D. M., Hanage, W. P. & Spratt, B. G. eBURST: Inferring patterns of evolutionary descent among clusters of related bacterial genotypes from multilocus sequence typing data. J. Bacteriol. 186, 1518–1530. https://doi.org/10.1128/jb.186.5.1518-1530.2004 (2004).
Dündar, H., Atakay, M., Çelikbıçak, Ö., Salih, B. & Bozoğlu, F. Comparison of two methods for purification of enterocin B, a bacteriocin produced by Enterococcus faecium W3. Prep. Biochem. Biotechnol. 45, 796–809. https://doi.org/10.1080/10826068.2014.958165 (2015).
Birri, D. J., Brede, D. A., Forberg, T., Holo, H. & Nes, I. F. Molecular and genetic characterization of a novel bacteriocin locus in Enterococcus avium isolates from infants. Appl. Environ. Microbiol. 76, 483–492. https://doi.org/10.1128/aem.01597-09 (2010).
Mehmeti, I. et al. Transcriptome, proteome, and metabolite analyses of a lactate dehydrogenase-negative mutant of Enterococcus faecalis V583. Appl. Environ. Microbiol. 77, 2406–2413. https://doi.org/10.1128/aem.02485-10 (2011).
Lee, S. Y. et al. Purification and molecular cloning of cDNA for an inducible antibacterial protein of larvae of a coleopteran insect, Holotrichia diomphalia. J. Biochem. 115, 82–86. https://doi.org/10.1093/oxfordjournals.jbchem.a124309 (1994).
Farías, M. E., Farías, R. N., de Ruiz Holgado, A. P. & Sesma, F. Purification and N-terminal amino acid sequence of Enterocin CRL 35, a “pediocin-like” bacteriocin produced by Enterococcus faecium CRL 35. Lett. Appl. Microbiol. 22, 417–419. https://doi.org/10.1111/j.1472-765x.1996.tb01193.x (1996).
El-Gendy, A., Essam, T., Amin, M., Ahmed, S. & Nes, I. Clinical screening for bacteriocinogenic Enterococcus faecalis isolated from intensive care unit inpatient in Egypt. J. Microb. Biochem. Technol. 4, 161–167 (2013).
Nes, I. F. & Holo, H. Class II antimicrobial peptides from lactic acid bacteria. Biopolymers 55, 50–61. https://doi.org/10.1002/1097-0282(2000)55:1%3c50::aid-bip50%3e3.0.co;2-3 (2000).
Johnson, A. P., Uttley, A. H., Woodford, N. & George, R. C. Resistance to vancomycin and teicoplanin: An emerging clinical problem. Clin. Microbiol. Rev. 3, 280–291. https://doi.org/10.1128/cmr.3.3.280 (1990).
Line, J. E. et al. Isolation and purification of enterocin E-760 with broad antimicrobial activity against gram-positive and gram-negative bacteria. Antimicrob. Agents Chemother. 52, 1094–1100. https://doi.org/10.1128/aac.01569-06 (2008).
Svetoch, E. A. et al. Diverse antimicrobial killing by Enterococcus faecium E 50–52 bacteriocin. J. Agric. Food Chem. 56, 1942–1948. https://doi.org/10.1021/jf073284g (2008).
Messaoudi, S. et al. Purification and characterization of a new bacteriocin active against Campylobacter produced by Lactobacillus salivarius SMXD51. Food Microbiol. 32, 129–134. https://doi.org/10.1016/j.fm.2012.05.002 (2012).
Sahm, D. F. et al. In vitro susceptibility studies of vancomycin-resistant Enterococcus faecalis. Antimicrob. Agents Chemother. 33, 1588–1591. https://doi.org/10.1128/aac.33.9.1588 (1989).
Arias, C. A. & Murray, B. E. The rise of the Enterococcus: Beyond vancomycin resistance. Nat. Rev. Microbiol. 10, 266–278. https://doi.org/10.1038/nrmicro2761 (2012).
Barber, K. E., King, S. T., Stover, K. R. & Pogue, J. M. Therapeutic options for vancomycin-resistant enterococcal bacteremia. Expert Rev. Anti-infect. Ther. 13, 363–377. https://doi.org/10.1586/14787210.2015.1001839 (2015).
Mutters, N. T., Werner, G., Tacconelli, E. & Mischnik, A. Treatment options for serious infections caused by vancomycin-resistant enterococci. Dtsch. Med. Wochenschr. 1946(140), 42–45. https://doi.org/10.1055/s-0040-100428 (2015).
Holo, H., Jeknic, Z., Daeschel, M., Stevanovic, S. & Nes, I. F. Plantaricin W from Lactobacillus plantarum belongs to a new family of two-peptide lantibiotics. Microbiology 147, 643–651. https://doi.org/10.1099/00221287-147-3-643 (2001).
Maldonado, A., Ruiz-Barba, J. L. & Jiménez-Díaz, R. Purification and genetic characterization of plantaricin NC8, a novel coculture-inducible two-peptide bacteriocin from Lactobacillus plantarum NC8. Appl. Environ. Microbiol. 69, 383–389. https://doi.org/10.1128/aem.69.1.383-389.2003 (2003).
Morgan, S. M., O’Connor, P. M., Cotter, P. D., Ross, R. P. & Hill, C. Sequential actions of the two component peptides of the lantibiotic lacticin 3147 explain its antimicrobial activity at nanomolar concentrations. Antimicrob. Agents Chemother. 49, 2606–2611. https://doi.org/10.1128/aac.49.7.2606-2611.2005 (2005).
Yamazaki, K., Suzuki, M., Kawai, Y., Inoue, N. & Montville, T. J. Purification and characterization of a novel class IIa bacteriocin, piscicocin CS526, from surimi-associated Carnobacterium piscicola CS526. Appl. Environ. Microbiol. 71, 554–557. https://doi.org/10.1128/aem.71.1.554-557.2005 (2005).
Mareková, M., Lauková, A., Skaugen, M. & Nes, I. Isolation and characterization of a new bacteriocin, termed enterocin M, produced by environmental isolate Enterococcus faecium AL41. J. Ind. Microbiol. Biotechnol. 34, 533–537. https://doi.org/10.1007/s10295-007-0226-4 (2007).
Aymerich, T. et al. Biochemical and genetic characterization of enterocin A from Enterococcus faecium, a new antilisterial bacteriocin in the pediocin family of bacteriocins. Appl. Environ. Microbiol. 62, 1676–1682. https://doi.org/10.1128/aem.62.5.1676-1682.1996 (1996).
Cintas, L. M. et al. Isolation and characterization of pediocin L50, a new bacteriocin from Pediococcus acidilactici with a broad inhibitory spectrum. Appl. Environ. Microbiol. 61, 2643–2648. https://doi.org/10.1128/aem.61.7.2643-2648.1995 (1995).
Barefoot, S. F. & Klaenhammer, T. R. Detection and activity of lactacin B, a bacteriocin produced by Lactobacillus acidophilus. Appl. Environ. Microbiol. 45, 1808–1815. https://doi.org/10.1128/aem.45.6.1808-1815.1983 (1983).
Stoffels, G. et al. Purification and characterization of a new bacteriocin isolated from a Carnobacterium sp. Appl. Environ. Microbiol. 58, 1417–1422. https://doi.org/10.1128/aem.58.5.1417-1422.1992 (1992).
Hassan, M. U. et al. Characterisation of bacteriocins produced by Lactobacillus spp. isolated from the traditional Pakistani yoghurt and their antimicrobial activity against common foodborne pathogens. Biomed. Res. Int. 2020, 8281623. https://doi.org/10.1155/2020/8281623 (2020).
Martínez, B., Suárez, J. E. & Rodríguez, A. Lactococcin 972: A homodimeric lactococcal bacteriocin whose primary target is not the plasma membrane. Microbiology 142(Pt 9), 2393–2398. https://doi.org/10.1099/00221287-142-9-2393 (1996).
Tiwari, S. K. & Srivastava, S. Purification and characterization of plantaricin LR14: A novel bacteriocin produced by Lactobacillus plantarum LR/14. Appl. Microbiol. Biotechnol. 79, 759–767. https://doi.org/10.1007/s00253-008-1482-6 (2008).
Borrero, J. et al. Characterization of garvicin ML, a novel circular bacteriocin produced by Lactococcus garvieae DCC43, isolated from mallard ducks (Anas platyrhynchos). Appl. Environ. Microbiol. 77, 369–373. https://doi.org/10.1128/aem.01173-10 (2011).
Kemperman, R. et al. Identification and characterization of two novel clostridial bacteriocins, circularin A and closticin 574. Appl. Environ. Microbiol. 69, 1589–1597. https://doi.org/10.1128/aem.69.3.1589-1597.2003 (2003).
Busani, L. et al. Antimicrobial susceptibility of vancomycin-susceptible and -resistant enterococci isolated in Italy from raw meat products, farm animals, and human infections. Int. J. Food Microbiol. 97, 17–22. https://doi.org/10.1016/j.ijfoodmicro.2004.04.008 (2004).
Lepage, E. et al. Comparative genomic hybridization analysis of Enterococcus faecalis: Identification of genes absent from food strains. J. Bacteriol. 188, 6858–6868. https://doi.org/10.1128/jb.00421-06 (2006).
Koch, S., Hufnagel, M., Theilacker, C. & Huebner, J. Enterococcal infections: Host response, therapeutic, and prophylactic possibilities. Vaccine 22, 822–830. https://doi.org/10.1016/j.vaccine.2003.11.027 (2004).
Semedo, T. et al. Virulence factors in food, clinical and reference Enterococci: A common trait in the genus?. Syst. Appl. Microbiol. 26, 13–22. https://doi.org/10.1078/072320203322337263 (2003).
Shankar, N., Baghdayan, A. S. & Gilmore, M. S. Modulation of virulence within a pathogenicity island in vancomycin-resistant Enterococcus faecalis. Nature 417, 746–750. https://doi.org/10.1038/nature00802 (2002).
Begley, M., Hill, C. & Gahan, C. G. Bile salt hydrolase activity in probiotics. Appl. Environ. Microbiol. 72, 1729–1738. https://doi.org/10.1128/aem.72.3.1729-1738.2006 (2006).
Mohamed, J. A. & Huang, D. B. Biofilm formation by enterococci. J. Med. Microbiol. 56, 1581–1588. https://doi.org/10.1099/jmm.0.47331-0 (2007).
Franz, C. M., Stiles, M. E., Schleifer, K. H. & Holzapfel, W. H. Enterococci in foods—A conundrum for food safety. Int. J. Food Microbiol. 88, 105–122. https://doi.org/10.1016/s0168-1605(03)00174-0 (2003).
Klein, G. Taxonomy, ecology and antibiotic resistance of enterococci from food and the gastro-intestinal tract. Int. J. Food Microbiol. 88, 123–131. https://doi.org/10.1016/s0168-1605(03)00175-2 (2003).
Choho, G. et al. Characterization of a bacteriocin-producing strain of Enterococcus faecalis from cow’s milk used in the production of Moroccan traditional dairy foods. World J. Microbiol. Biotechnol. 24, 997–1001 (2008).
Hickey, R. M., Twomey, D. P., Ross, R. P. & Hill, C. Production of enterolysin A by a raw milk enterococcal isolate exhibiting multiple virulence factors. Microbiology 149, 655–664. https://doi.org/10.1099/mic.0.25949-0 (2003).
McBride, S. M. et al. Genetic variation and evolution of the pathogenicity island of Enterococcus faecalis. J. Bacteriol. 191, 3392–3402. https://doi.org/10.1128/jb.00031-09 (2009).
Agersø, Y. et al. Vancomycin-resistant Enterococcus faecalis isolates from a Danish patient and two healthy human volunteers are possibly related to isolates from imported turkey meat. J. Antimicrob. Chemother. 62, 844–845. https://doi.org/10.1093/jac/dkn271 (2008).
Quiñones, D., Kobayashi, N. & Nagashima, S. Molecular epidemiologic analysis of Enterococcus faecalis isolates in Cuba by multilocus sequence typing. Microb. Drug Resist. 15, 287–293. https://doi.org/10.1089/mdr.2009.0028 (2009).
Kawalec, M. et al. Clonal structure of Enterococcus faecalis isolated from Polish hospitals: Characterization of epidemic clones. J. Clin. Microbiol. 45, 147–153. https://doi.org/10.1128/jcm.01704-06 (2007).
Acknowledgements
Dzung Diep, Linda Godager, Zhian Salehian, Ibrahim Mehmeti, and Dagim Birri are specially acknowledged for their support and technical assistance. Special gratitude to Morten Skaugen for the MALDI-TOF analysis.
Author information
Authors and Affiliations
Contributions
I.F.N., H.H and D.A.B. designed all experiments. A.O.E., T.E, Y.I.S, M.A.A, and S.H.A performed the microbiology experiments, organized and analyzed data. A.O.E. wrote the initial draft of the manuscript. All authors revised the manuscript prior to its submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
El-Gendy, A.O., Brede, D.A., Essam, T.M. et al. Purification and characterization of bacteriocins-like inhibitory substances from food isolated Enterococcus faecalis OS13 with activity against nosocomial enterococci. Sci Rep 11, 3795 (2021). https://doi.org/10.1038/s41598-021-83357-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-83357-z
- Springer Nature Limited
This article is cited by
-
Untargeted metabolite profiling of Enterococcus villorum SB2, isolated from the vagina of pregnant women, by HR-LCMS
World Journal of Microbiology and Biotechnology (2022)
-
Novel pathways in bacteriocin synthesis by lactic acid bacteria with special reference to ethnic fermented foods
Food Science and Biotechnology (2022)