Abstract
Immune checkpoint inhibitors and BRAF-targeted therapy each improve survival in melanoma. Immune changes early during targeted therapy suggest the mechanisms of each drug class could work synergistically. In the non-comparative, randomized, phase 2 NeoTrio trial, we investigated whether targeted therapy could boost the proportion of patients achieving long-term recurrence-free survival with neoadjuvant immunotherapy in resectable stage III BRAFV600-mutant melanoma. Sixty patients (42% females) were randomized to pembrolizumab alone (n = 20), sequential therapy (dabrafenib plus trametinib followed by pembrolizumab; n = 20) or concurrent (triple) therapy (n = 20), followed by surgery and adjuvant therapy. The primary outcome was pathological response; secondary outcomes included radiographic response, recurrence-free survival, overall survival, surgical outcomes, peripheral blood and tumor analyses and safety. The pathological response rate was 55% (11/20; including six pathological complete responses (pCRs)) with pembrolizumab, 50% (10/20; three pCRs) with sequential therapy and 80% (16/20; ten pCRs) with concurrent therapy, which met the primary outcome in each arm. Treatment-related adverse events affected 75–100% of patients during neoadjuvant treatment, with seven early discontinuations (all in the concurrent arm). At 2 years, event-free survival was 60% with pembrolizumab, 80% with sequential therapy and 71% with concurrent therapy. Recurrences after major pathological response were more common in the targeted therapy arms, suggesting a reduction in response ‘quality’ when targeted therapy is added to neoadjuvant immunotherapy. Risking the curative potential of immunotherapy in melanoma cannot be justified. Pending longer follow-up, we suggest that immunotherapy and targeted therapy should not be combined in the neoadjuvant setting for melanoma. ClinicalTrials.gov registration: NCT02858921.
Similar content being viewed by others
Main
BRAF mutations are found in ~40% of cutaneous melanomas1 and are associated with more aggressive early-stage disease and a younger patient population2,3. BRAF and mitogen-activated protein kinase kinase (MEK)-targeted therapies and immune checkpoint inhibitor (ICI) immunotherapy have led to remarkable improvements in response and survival outcomes in the advanced (unresectable stage III or IV melanoma) setting4,5. Almost 70% of patients achieve an objective response with targeted therapy; however, most progress within 2 years5. While ICIs have a lower response rate, acquired resistance is much less common4.
Treatment with BRAF/MEK inhibitors has been shown to induce a favorable tumor immune microenvironment in melanoma6,7,8. In a study of metastatic melanomas, there was a substantial increase in tumor-infiltrating CD4+ and CD8+ T cells after 7 days of treatment with a BRAF inhibitor (vemurafenib or dabrafenib)6. The infiltrate persisted with the addition of a MEK inhibitor (trametinib) to dabrafenib, which was also associated with an increase in CD4+, CD8+ and PD-1+ T cells, as well as in programmed death-ligand 1 (PD-L1) expression on tumor cells8. In another study, treatment with 10–14 days of BRAF inhibitor alone (vemurafenib) or with concurrent MEK inhibition (dabrafenib plus trametinib) resulted in a marked increase in CD8+ T cells and an increase in PD-L1 expression7. In a melanoma model, MEK1/MEK2 inhibition was associated with the reprogramming of CD8+ T cells into a potent stemness state9. Anti-programmed cell death-protein 1 (PD-1) ICI treatment is most effective in patients where T cells can recognize the tumor, and the highest response rates are found in patients with a higher density of tumor-infiltrating lymphocytes10,11,12,13, suggesting that BRAF/MEK inhibitor treatment could amplify the antitumor activity of anti-PD-1. However, the most effective way to combine these treatments is unknown.
Different approaches to combining BRAF-targeted therapy and ICIs have been examined in the setting of advanced melanoma. Three trials (Keynote-022, COMBI-i and IMspire150) have tested the use of BRAF-targeted therapy with or without concurrent anti-PD-1 in advanced BRAF-mutant melanoma14,15,16. In all three studies, addition of anti-PD-1 prolonged progression-free survival but substantially increased toxicity14,15,16. Two additional trials (SECOMBIT and DREAMseq) have investigated sequencing options, identifying a combination of anti-PD-1 and anti-CTLA-4 to progression followed by BRAF-targeted therapy as the optimal regimen in a clinical trial-eligible population17,18.
For patients with resectable melanoma, presurgical or ‘neoadjuvant’ drug therapy is an area of active investigation. In a pooled analysis of neoadjuvant trials, a pathological complete response (pCR) was achieved by 47% of patients with neoadjuvant BRAF-targeted therapy19,20 and 33% with neoadjuvant ICI21,22,23,24 (20% with anti-PD-1 monotherapy and 43% with combination anti-PD-1 plus anti-CTLA-4)25. Interestingly, the 2-year recurrence-free survival (RFS) rate was only 79% in patients achieving a pCR to targeted therapy, compared with 96% for patients achieving any pathological response (pCR, near-pathological complete response (near-pCR) or pathological partial response (pPR)) to an ICI regimen25, suggesting (alongside 5-year outcomes from the NeoCombi trial26) that neoadjuvant targeted therapy has no benefit over adjuvant targeted therapy. This is in contrast to ICI, where in the phase II SWOG S1801 trial, the 2-year event-free survival (EFS) rate was 72% with neoadjuvant (plus adjuvant) anti-PD-1 versus 49% with adjuvant anti-PD-1 alone (the current standard of care)27. It is possible that combining neoadjuvant anti-PD-1 with targeted therapy could enhance the impressive, sometimes curative, gains made with neoadjuvant ICI even further.
The NeoTrio trial (ClinicalTrials.gov registration: NCT02858921) was designed to determine whether targeted therapy (dabrafenib plus trametinib) enhances the benefit of neoadjuvant anti-PD-1 (pembrolizumab) in stage III resectable BRAF-mutant melanoma. Specifically, we investigated pathological response and survival outcomes with sequential or concurrent BRAF-targeted therapy and anti-PD-1, or anti-PD-1 alone, in the 6 weeks before surgery. Here we present the primary endpoint of pathological response rate and key secondary endpoints, namely radiographic response, RFS, overall survival (OS), surgical outcomes and safety. Additional planned secondary endpoints not reported in this paper are peripheral blood and tumor analyses.
Results
Baseline patient characteristics and disposition
Between 8 November 2017 and 18 May 2021, 63 patients with resectable BRAFV600-mutant stage III melanoma were screened, of which 60 were enrolled. Patients were randomized to treatment with 6 weeks of neoadjuvant pembrolizumab monotherapy (n = 20), sequential therapy (1 week of dabrafenib plus trametinib followed by pembrolizumab; n = 20) or concurrent triple therapy (pembrolizumab with dabrafenib plus trametinib; n = 20; Fig. 1). At baseline, the median age was 53 (interquartile range (IQR) = 42–63), 25 (42%) patients were females and all patients had confirmed BRAFV600 mutations; 49 (82%) patients had V600E, 9 (15%) had V600K and 2 (3%) had V600R (Table 1). Nodal basins included the axilla (43%), ilioinguinal (32%) and neck (32%). As per the American Joint Committee on Cancer (AJCC) eighth edition staging manual28,29, patients had either clinical N1b nodal disease (1 macroscopic node; 63%), N2b nodal disease (2–3 macroscopic nodes; 20%) or N3b nodal disease (≥4 macroscopic nodes or matted nodes; 17%).
a, Overview of the non-comparative randomized phase 2, open-label, three-arm NeoTrio trial (ClinicalTrials.gov registration: NCT02858921), with pathological response-directed adjuvant therapy. Dosing regimen for D/T was dabrafenib 150 mg PO BID plus trametinib 2 mg PO QD. b, Patient flow diagram. BID, twice per day; D/T, dabrafenib plus trametinib; NT, neoadjuvant therapy; PO, per oral; QD, once per day; Q3W, every three weeks.
At data cut-off (26 October 2023), the median follow-up was 24.5 months (95% confidence interval (CI), 23.0–35.3). All 60 patients received at least one dose of neoadjuvant pembrolizumab and were included in the analysis. Of these, 51 (85%) patients completed neoadjuvant treatment and 9 (15%) patients discontinued early due to neoadjuvant treatment-related adverse events (TRAEs; 8 (40%) in the concurrent arm, none in the sequential arm and 1 (5%) in the pembrolizumab arm; Fig. 1 and Table 2). Following neoadjuvant treatment, 57 (95%) patients underwent surgery; 3 (5%) patients did not, due to distant progression. Following surgery, 45 (75%) patients received adjuvant pembrolizumab, 5 (8%) received adjuvant dabrafenib plus trametinib per investigator decision following pathological non-response (pNR) and 7 (12%) received no adjuvant therapy, either due to toxicity (n = 5), progression (n = 1) or poor quality of life following surgery due to pre-existing paraplegia (n = 1; Fig. 1).
Efficacy: response
Pathological, radiological and metabolic response rates are shown in Table 3. The primary endpoint was met in all three arms (pathological response rate of ≥5%). A pathological response was achieved in 55% (11/20; 95% CI, 36–83) of patients in the pembrolizumab arm, 50% (10/20; 95% CI, 27–73) in the sequential arm and 80% (16/20; 95% CI, 60–97) in the concurrent arm; a pCR was reported in 30% (6/20), 15% (3/20) and 50% (10/20) of patients, respectively (Table 3). A major pathological response (MPR; pCR or near-pCR) occurred in 40% (8/20) of patients with pembrolizumab monotherapy, 30% (6/20) of patients with sequential therapy and 55% (11/20) of patients with concurrent therapy. A pNR occurred in 35% (7/20) of patients treated with pembrolizumab, 50% (10/20) of patients with sequential therapy and 15% (3/20) of patients with concurrent therapy.
An objective radiological response (CR or PR) per Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1 (ref. 30) was observed in 30% (6/20) of patients treated with pembrolizumab, 50% (10/20) of patients treated with sequential treatment and 70% (14/20) of patients treated with concurrent treatment (Table 3). There were seven (12%) patients with RECIST progressive disease (PD; three distant and four locoregional lymph nodes; 5/20 patients (25%) in the pembrolizumab arm, 1/20 (5%) in the sequential arm and 1/20 (5%) in the concurrent arm). An MPR was found in 70% (7/10) of patients with RECIST CR, 55% (11/20) of patients with RECIST PR, 30% (7/23) of patients with RECIST stable disease (SD) and no patient with RECIST PD (Extended Data Table 1 and Extended Data Fig. 1). A pNR was found in 30% (6/20) and 52% (12/23) of patients with RECIST PR and SD, respectively. RECIST CR selected patients with an MPR with poor sensitivity (36%) and high specificity (92%). Similarly, RECIST PD selected patients with pNR with poor sensitivity (10%) and high specificity (95%).
A metabolic response (complete metabolic response (CMR) or partial metabolic response (PMR)) per the European Organization for Research and Treatment of Cancer (EORTC) positron emission tomography (PET) criteria31 was observed in 40% (8/20) of patients treated with pembrolizumab, 50% (10/20) of those treated with sequential therapy and 95% (19/20) of those treated with concurrent therapy, including five CMR in the concurrent arm and one CMR in each of the sequential and pembrolizumab monotherapy arms (Table 3). An MPR was found in 57% (4/7 had pCR) of patients with a CMR, 60% (18/30) of patients with a PMR, but no patient with stable metabolic disease and only two patients (25%) with progressive metabolic disease (PMD; Extended Data Table 2 and Extended Data Fig. 1). pNR was found in 23% (7/30) and 78% (7/9) of patients with partial or stable metabolic response, respectively. CMR selected patients with an MPR with poor sensitivity (22%) and high specificity (92%). Similarly, PMD selected patients with pNR with poor sensitivity (25%) and high specificity (91%).
Efficacy: recurrence and survival
At data cut-off, there were 18 patients (30%) with postsurgical recurrence, and nine (15%) patients had died. All deaths followed presurgical progression (2/9) or postsurgical recurrence (7/9) events, and all were attributed to melanoma.
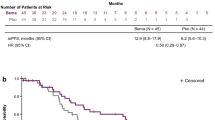
At data cut-off, there were nine (45%), nine (45%) and six (30%) defined events for the EFS in the pembrolizumab alone, sequential and concurrent arms, respectively (Table 4). The landmark EFS rates at 12 and 24 months were 80% and 60% with pembrolizumab alone, 80% and 80% with sequential treatment and 80% and 71% with concurrent treatment (Fig. 2 and Table 4).
Landmark survival rates were calculated at 12 and 24 months. a, EFS curve showing 12-month EFS rate was 80% in all arms; 24-month EFS was 60% with pembrolizumab monotherapy, 80% with sequential therapy and 71% with concurrent therapy. b, RFS curve showing 12-month RFS rate was 89% with pembrolizumab monotherapy, 80% with sequential therapy and 84% with concurrent therapy; 24-month RFS rate was 66%, 80% and 75%, respectively. c, OS curve showing 12-month OS rate was 94% with pembrolizumab monotherapy, 95% with sequential therapy and 95% with concurrent therapy; 24-month OS rate was 76%, 89% and 95%, respectively.
At data cut-off, there were six (30%), eight (40%) and five (25%) recurrence events or deaths in the pembrolizumab alone, sequential and concurrent arms, respectively (Table 4). The landmark RFS rates at 12 and 24 months were 89% and 66% with pembrolizumab alone, 80% and 80% with sequential treatment and 84% and 75% with concurrent treatment (Fig. 2 and Table 4).
The RFS rate was higher in patients with MPR versus those without MPR (Extended Data Figs. 2 and 3 and Extended Data Table 3). In the pembrolizumab monotherapy arm, no patient with MPR recurred. One patient with MPR recurred in each of the targeted therapy arms (a patient with near-pCR in the sequential therapy arm who recurred >2 years after surgery and a patient with pCR in the concurrent arm who recurred 10 months after surgery). Pathological response was a better predictor of RFS than imaging response measures, with landmark RFS rates at 12 and 24 months of—96% and 96% for MPR; 89% and 89%, respectively, for RECIST CR; 95% and 95% for RECIST PR; 100% and 33% for EORTC CMR; and 89% and 79% for EORTC PMR.
At data cut-off, there were four (20%), three (15%) and two (10%) deaths in the pembrolizumab alone, sequential and concurrent arms, respectively (Table 4). The landmark OS rates at 12 and 24 months were 95% and 76% with pembrolizumab alone, 95% and 89% with sequential treatment and 95% and 95% with concurrent treatment (Fig. 2 and Table 4).
Adverse events
Overall, TRAEs of any grade occurred in 85% (17/20) of patients treated with pembrolizumab monotherapy, 95% (19/20) of patients with sequential therapy and 100% (20/20) of patients with concurrent therapy (Extended Data Table 4). Most TRAEs occurred during neoadjuvant therapy; 75% (15/20) of patients were treated with pembrolizumab monotherapy, 80% (16/20) of patients were treated with sequential therapy and 100% (20/20) of patients were treated with concurrent therapy. Overall, grade 3/grade 4 TRAEs occurred in 5% (1), 25% (5) and 55% (11) of patients, respectively, with grade 3/grade 4 TRAEs during neoadjuvant therapy occurring only in the concurrent arm (40%; 8/20; Table 2). Pyrexia was the most common TRAE, occurring in 21 patients (17 in the concurrent arm), followed by fatigue, rash, pruritis, vitiligo, headache and nausea (Extended Data Table 4).
Twenty-two patients had interruptions to neoadjuvant dabrafenib/trametinib treatment due to TRAEs (19 (95%) in the concurrent arm and 3 (15%) in the sequential arm; Table 2); there were no interruptions to neoadjuvant pembrolizumab. Seven patients discontinued neoadjuvant therapy early due to TRAEs, all from the concurrent arm (six of whom ceased dabrafenib/trametinib and one who ceased both dabrafenib/trametinib and pembrolizumab). Four of the seven patients had ≥1 TRAE. TRAEs leading to early discontinuation of dabrafenib/trametinib ranged from grades 1–3 and included pyrexia (n = 3), chills (n = 2) and elevated alanine transferase and aspartate transferase (n = 1). The sole patient who ceased neoadjuvant pembrolizumab had grade 3 hepatitis and grade 3 drug-induced liver injury attributed to pembrolizumab, resulting in the cessation of all three agents. All patients who ceased neoadjuvant treatment fully recovered from toxicity. At data cut-off, two of the seven patients had recurred (one with pCR who recurred in the liver and one with pNR who recurred in the spleen), and both were on survival follow-up.
Twenty-six (59%) patients completed all planned doses of adjuvant pembrolizumab. TRAEs were the primary reason for early discontinuation of adjuvant pembrolizumab (one (5%) patient in the pembrolizumab arm, four (20%) in the sequential arm and four (30%) in the concurrent arm; Table 2). In the six patients who received adjuvant dabrafenib plus trametinib, five completed 12 months of treatment as planned and one received 9 months of treatment with discontinuation due to peripheral neuropathy.
Surgical complications occurred in 39 patients overall (68%; Extended Data Table 5). There were nine grade 3/grade 4 surgical adverse events (four with pembrolizumab monotherapy, three with sequential therapy and two with concurrent therapy), including five cases of wound infection requiring hospitalization.
The ease of upfront resection (estimated at baseline) was compared with the ease of resection after 6 weeks of neoadjuvant therapy (recorded within 24 h after surgery; Extended Data Table 6). There were ten patients for whom resection was more difficult than estimated at baseline, due to the presence of inflammatory tissue or immunotherapy-related changes in four of six patients for whom reasons were provided. Neoadjuvant therapy was associated with improved resectability in eight (47%) patients in the concurrent arm, four (21%) patients in the sequential arm and two (12%) patients in the pembrolizumab arm. For most patients (55%), there was no difference, although resectability was harder in five (29%) patients in the pembrolizumab arm (two with pNR and three with MPR). When analyzed by lymph node basin or pathological response, all eight patients with improved resectability in the concurrent arm had pCR or pPR; however, overall, there was no difference when assessed by the pathological response. Resections were harder in neck nodal basin resections (27% (4/15)) compared with axillary (14% (3/22)) and ilioinguinal (18% (3/17)) resections.
Protocol amendment
Eleven patients were enrolled before the protocol amendment, resulting in surgery at 7–12 weeks for ten patients (four from the pembrolizumab monotherapy arm and three each from the sequential and concurrent arms) rather than at 6 weeks. There was no increased incidence of presurgical progression, recurrence, death or toxicity events in this group.
Health-related quality of life (HRQOL)
Statistically significant deterioration in HRQOL was only reported in the perioperative period—week 6 (presurgery) for patients treated with concurrent therapy (Global Health Score (GHS) mean change: −10.83 (95% CI, −19.63 to −2.01), P < 0.05) and at week 12 (postsurgery) for patients treated with either pembrolizumab monotherapy (GHS mean change: −17.70 (95% CI, −25.10 to −10.30), P < 0.001) or sequential therapy (GHS mean change: −16.37 (95% CI, −23.83 to −8.92), P < 0.001; Extended Data Fig. 4). Patients treated with pembrolizumab monotherapy also had a statistically significant decline at week 30 (mean change: −11.95 (95% CI, −21.02 to −2.87), P < 0.05). However, the only deterioration deemed to be clinically significant was in the pembrolizumab monotherapy arm at week 12.
Discussion
The NeoTrio trial investigated combination BRAF-targeted therapy and ICI in the neoadjuvant setting for resectable melanoma, including an anti-PD-1 monotherapy comparator arm. All regimens elicited a substantial pathological response rate (≥50% of patients) and met the primary endpoint. Concurrent therapy induced the highest pathological response rate, similar to that observed in previous neoadjuvant studies of BRAF-targeted therapy alone (67%)25,26, but the durability is uncertain. Across all arms, patients with MPR had fewer recurrences than those without MPR; however, no patient with MPR in the pembrolizumab arm has recurred, compared with one each from the arms containing targeted therapy. Concurrent therapy was the most toxic, with 55% of patients experiencing grade 3/grade 4 adverse events and a 40% discontinuation rate during neoadjuvant therapy. This mirrors experience in the advanced setting, where triple therapy has induced high rates of grade 3/grade 4 adverse events, ranging from 55% to 79%14,15,16. Overall, pending longer survival follow-up, we do not endorse the addition of BRAF-targeted therapy to neoadjuvant ICI in melanoma.
In the NeoTrio trial, it was hypothesized that response to neoadjuvant anti-PD-1 treatment would be improved by a short course of BRAF/MEK inhibitor induction therapy. However, the pathological response rate with induction therapy in the sequential arm (50% (95% CI, 27–73)) was similar to pembrolizumab alone (55% (95% CI, 36–83)). Administering BRAF/MEK inhibitors and ICI in sequence has been previously examined in the metastatic setting. In SECOMBIT, 8 weeks of encorafenib plus binimetinib followed by nivolumab plus ipilimumab (and further encorafenib plus binimetinib if progression) was no more effective than nivolumab plus ipilimumab (and further encorafenib plus binimetinib if progression)17. This suggests that the T cells induced by BRAF/MEK inhibition in melanoma tumors are not conducive to a heightened anti-PD-1 response and may not be tumor-specific but rather a non-specific immune response to cell death induced by the BRAF-targeted therapy. Potential mechanisms of cross-resistance between the two treatment modalities have been explored, with several common pathways identified including mitogen-activated protein kinase (MAPK)32 and PTEN33. Further investigation is essential to understand the lack of synergy, and the translational analysis of tissue samples from NeoTrio is ongoing34.
Although the response rate was highest with concurrent therapy, the quality and duration of response must be observed carefully. In multiple settings for BRAF-mutant melanoma, targeted therapy has been associated with a good initial response rate, but a higher risk of treatment failure when compared with patients who respond to immunotherapy. In a pooled analysis, 37% of patients had a pCR to neoadjuvant immunotherapy. Two-year RFS for complete responders was excellent, at 96%; however, any pathological response was associated with excellent durability (for example, 2-year RFS of 94% for partial responders). In contrast, 47% of patients had a pCR to targeted therapy, but this afforded a substantially lower 2-year RFS of 79%; partial responders had a 2-year RFS of 18%25. Recurrences with targeted therapy tended to occur late (>12–18 months)25, but still within 2 years26. With a median follow-up of 24.5 months, the only recurrences in MPR patients in NeoTrio have occurred in targeted therapy arms. Long-term follow-up is required to monitor for further late recurrences in each of the arms. Despite the higher response rate, loss of prognostic certainty is an important consideration when balancing the advantages and disadvantages of adding targeted therapy to anti-PD-1.
There is a strong correlation between pathological response to neoadjuvant ICI and long-term survival25. In an updated analysis of the OpACIN and OpACIN-neo trials, 3-year RFS was 95% for patients with any pathological response versus 37% with pNR (P < 0.001)35. In a recent trial of neoadjuvant nivolumab plus relatlimab, 2-year RFS was 92% in patients with a pathological response and 55% with non-response (P = 0.005)36. Importantly, previous neoadjuvant trials have reported that pathological response outcomes are often better than anticipated by presurgical RECIST response22,25,36,37. In the NeoTrio trial, almost half (46%) of patients with no objective radiological response had a pathological response, including seven with MPR. Interestingly, fluorodeoxyglucose (FDG)-PET CMR was more specific for MPR than RECIST CR, yet both modalities had poor sensitivity. Pathological response is currently the best surrogate marker for survival following neoadjuvant therapy25,35, and our data showed that pathological response at week 6 predicted RFS better than RECIST or metabolic response at week 6. More data are required to evaluate the relationship between pathological response and metabolic response.
Around 35% of patients do not have a pathological response to neoadjuvant immunotherapy (pooled anti-PD-1 monotherapy and anti-PD-1 plus anti-CTLA-4) and are at high risk of postsurgical recurrence, with a 2-year RFS of 37%25. Future studies should focus on new immune approaches that target non-responders to provide a durable response. Pathological response to anti-PD-1, with and without anti-CTLA-4, has been shown to correlate with high interferon-γ expression and high tumor mutation burden, suggesting biomarker-driven treatment investigation may be appropriate38,39. The neoadjuvant platform is an ideal vehicle for testing new approaches due to the rapid readout and correlation of pathological responses with survival outcomes that allow quick and definitive ‘go’ or ‘no-go’ decisions on new agents, combinations or regimens. For example, in the DONIMI trial, a theoretically promising combination of the HDAC inhibitor domatinostat and anti-PD-1 was quickly discarded when 6 weeks of neoadjuvant combination therapy provided no pathological response benefit (and possibly a measurable detriment) compared with anti-PD-1 alone38. Investigation of alternative immune approaches in the neoadjuvant setting is ongoing, including with anti-LAG-3 antibody relatlimab, which was recently found to provide a 70% pathological response rate when combined with nivolumab36. Combination treatment with drugs such as Janus kinase (JAK) inhibitors to target therapeutic resistance to immunotherapy may also be explored40.
HRQOL was lowest following neoadjuvant treatment in the concurrent arm (week 6) and following surgery in the pembrolizumab monotherapy and sequential arms (week 12). High rates of toxicity in the concurrent arm correlated with a deterioration in HRQOL at week 6 before surgery. Substantial decrements in HRQOL were observed in the postoperative period with sequential and pembrolizumab monotherapy, but not with concurrent therapy, and can be attributed to a lower rate of surgical adverse events in the concurrent arm. Interestingly, resectability was more frequently assessed as being ‘easier’ compared with surgical expectations at baseline in the concurrent arm, and the pathological response rate was higher, which may explain the maintenance of HRQOL from weeks 6 through 12. Further analyses and correlation at the patient-specific level regarding drug and surgical adverse events are ongoing.
The study was limited in several ways. The NeoTrio trial was not powered to make statistical comparisons between the three arms, which limits the interpretation of the findings. The small sample size also makes it difficult for clear trends to emerge in long-term survival and HRQOL.
To conclude, the NeoTrio trial suggests that BRAF-targeted therapy should not be added to neoadjuvant ICI for BRAFV600-mutant patients, at risk of higher toxicity and loss of curative potential. Longer-term follow-up will be critical to determining the durability and quality of response, particularly in the targeted therapy arms.
Methods
Patients and study design
NeoTrio (ClinicalTrials.gov registration: NCT02858921) was a randomized, multi-arm, open-label, parallel phase II study of neoadjuvant pembrolizumab, dabrafenib and trametinib in patients with BRAFV600-mutant resectable stage III cutaneous or unknown primary melanoma. Patients were ≥18 years of age with histologically confirmed resectable AJCC eighth edition29 stage IIIB–D melanoma with nodal disease (no in-transits) and sufficient tissue to enable multiple core and excision biopsies. Unresected primary melanoma was allowed. Patients had measurable disease per RECIST version 1.1 (ref. 30; ≥15 mm shortest diameter for lymph nodes), BRAFV600 mutation positivity, adequate organ function and Eastern Cooperative Oncology Group (ECOG) performance status ≤1. Patients were enrolled at three sites in Australia (Westmead Hospital, Melanoma Institute Australia and Peter MacCallum Cancer Center). The study was performed in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines. Patients provided written informed consent. The study protocol was approved by the human research ethics committee at each participating institution. Key sections of the study protocol are given in Supplementary Information.
Treatment
Patients received neoadjuvant therapy for 6 weeks across the three parallel treatment arms. Patients were randomized in a 1:1:1 ratio via a web-based system in permuted blocks (block sizes 6 and 9) and stratified by BRAFV600E versus non-BRAFV600E (that is, V600K, V600R, V600D and V600M) mutation. Patients allocated to pembrolizumab monotherapy received pembrolizumab 200 mg intravenously (IV) on days 1 and 22. Patients allocated to sequential therapy received targeted therapy (dabrafenib 150 mg orally twice per day and trametinib 2 mg orally once per day) for 7 days, followed by pembrolizumab 200 mg IV on days 8 and 22. Patients allocated to concurrent therapy received targeted therapy as above for 6 weeks, with pembrolizumab 200 mg IV on days 1 and 22. Following neoadjuvant therapy, all patients underwent therapeutic lymph node dissection (between days 42 and 56). After surgery, patients received 42 weeks (16 doses) of adjuvant pembrolizumab administered every 3 weeks, with the first adjuvant dose given as soon as possible after surgery, until toxicity, withdrawn consent, disease recurrence or death. For patients with pNR to neoadjuvant therapy, investigators/patients had the choice to switch from adjuvant pembrolizumab to standard-of-care dabrafenib and trametinib outside of the protocol for 52 weeks duration.
Assessments and outcomes
Self-reported biological sex was recorded. BRAFV600 mutation status was confirmed before study enrollment by immunohistochemistry or local molecular testing (for example, Oncofocus). At baseline, all patients underwent computed tomography (CT), magnetic resonance imaging and FDG-PET scans. CT scans were conducted every 6 weeks until the surgery, and then every 12 weeks afterward. FDG-PET scans were repeated at weeks 6 and 48. Tumor samples were collected at baseline, day 8 and day 15, followed by complete resection at week 6. A proportion of patients underwent surgery at week 12, before a protocol amendment to align with International Neoadjuvant Melanoma Consortium (INMC) guidelines41. Samples of peripheral blood for biomarker analysis were collected at baseline, day 8, day 15 and day 42 (before surgery) and at disease progression or recurrence, if applicable. Stool samples for microbiome analysis were collected at baseline, within 2 weeks before surgery, week 24 and at disease progression or recurrence, if applicable. HRQOL was assessed every 6 weeks using the EORTC Quality of Life Questionnaire-C30 (ref. 42) and after surgery using FACT-M43 (questions M10–M17). Safety was monitored continuously throughout the trial. Surgical outcomes were assessed for 4 weeks after surgery. Resectability, as per INMC guidelines,44 was assessed at baseline and week 6 (within 24 h after surgery). Survival follow-up continued every 12 weeks for up to 10 years.
The primary endpoint was pathological response rate and pCR rate based on examination of the resected tumor at week 6 by central pathologist review (R.A.S.). Definitions of pathological response categories per the INMC45 are given in Supplementary Table 1 and Supplementary Information. Secondary endpoints included radiological response (RECIST version 1.1 (ref. 30)) at week 6 before surgery, RFS (defined as the time from surgery to recurrence or death), OS, surgical outcomes, safety, HRQOL and translational endpoints comparing immunological, proteomic and genetic biomarkers in tumor tissue and blood samples. Other endpoints were metabolic response (EORTC PET31) at week 6 before surgery and EFS (defined as the time from treatment start to progression, recurrence, or death).
Statistical methods
Each arm was designed as a single-arm study. The sample size of 20 patients per arm (n = 60) was calculated to determine whether the pathological response rate was ≤5% or ≥20%. If the number of pathological responses was three or more, the hypothesis that a pathological response rate ≤5% was rejected with a target error rate of 0.080 and an actual error rate of 0.075. If the number of pathological responses was two or less, the hypothesis that a pathological response rate ≥20% was rejected with a target error rate of 0.210 and an actual error rate of 0.206 (refs. 46,47). With the exception of HRQOL, outcomes were measured in the intention-to-treat population, which included all patients who received at least one dose of pembrolizumab. Patients who dropped out before the first dose were replaced, except in the case of disease progression or death.
Patient characteristics are summarized by arm using descriptive statistics. The primary and secondary response outcomes were summarized using frequency and proportion by arm along with the two-sided 95% Clopper–Pearson exact CIs. The secondary time-to-event outcomes (EFS, RFS and OS) were analyzed using the Kaplan–Meier method stratified by arm. Twelve-month landmark rates for each survival outcome were provided for up to 3 years. RFS curves stratified by MPR (pCR or near-pCR response versus pPR or pNR) were drawn within each arm. No formal statistical inference to compare arms was computed.
HRQOL outcomes were assessed in all patients who completed baseline and ≥1 follow-up questionnaire. Data were censored at 60 weeks due to a small number (<5) of patients. Mean change over time with respect to baseline and 95% CI were calculated using mixed linear modeling including cohort, time (as a categorical variable) and a random intercept effect. A two-sided P ≤ 0.05 was considered statistically significant, with mean changes assessed with respect to established minimal clinically important difference values48. All statistical analyses were performed using SAS (version 9.4) and R (version 4.1.3).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
De-identified data are available on reasonable request and after signing of a data transfer agreement with Melanoma Institute Australia. Requests for data sharing can be made to the corresponding author, G.V.L., including a research proposal that must be approved by the principal investigators of the three participating centers. The Background and Patient Information sections of the study protocol are provided in the Supplementary Information.
References
Long, G. V. et al. Prognostic and clinicopathologic associations of oncogenic BRAF in metastatic melanoma. J. Clin. Oncol. 29, 1239–1246 (2011).
Jakob, J. A. et al. NRAS mutation status is an independent prognostic factor in metastatic melanoma. Cancer 118, 4014–4023 (2012).
Van der Kooij, M. K. et al. Age does matter in adolescents and young adults versus older adults with advanced melanoma: a national cohort study comparing tumor characteristics, treatment pattern, toxicity and response. Cancers 12, 2072 (2020).
Larkin, J. et al. Five-year survival with combined nivolumab and ipilimumab in advanced melanoma. N. Engl. J. Med. 381, 1535–1546 (2019).
Robert, C. et al. Five-year outcomes with dabrafenib plus trametinib in metastatic melanoma. N. Engl. J. Med. 381, 626–636 (2019).
Wilmott, J. S. et al. Selective BRAF inhibitors induce marked T-cell infiltration into human metastatic melanoma. Clin. Cancer Res. 18, 1386–1394 (2012).
Frederick, D. T. et al. BRAF inhibition is associated with enhanced melanoma antigen expression and a more favorable tumor microenvironment in patients with metastatic melanoma. Clin. Cancer Res. 19, 1225–1231 (2013).
Kakavand, H. et al. PD-L1 expression and tumor-infiltrating lymphocytes define different subsets of MAPK inhibitor-treated melanoma patients. Clin. Cancer Res. 21, 3140–3148 (2015).
Verma, V. et al. MEK inhibition reprograms CD8+ T lymphocytes into memory stem cells with potent antitumor effects. Nat. Immunol. 22, 53–66 (2021).
Gide, T. N. et al. Close proximity of immune and tumor cells underlies response to anti-PD-1 based therapies in metastatic melanoma patients. Oncoimmunology 9, 1659093 (2020).
Tumeh, P. C. et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature 515, 568–571 (2014).
Vilain, R. E. et al. Dynamic changes in PD-L1 expression and immune infiltrates early during treatment predict response to PD-1 blockade in melanoma. Clin. Cancer Res. 23, 5024–5033 (2017).
Chen, P. L. et al. Analysis of immune signatures in longitudinal tumor samples yields insight into biomarkers of response and mechanisms of resistance to immune checkpoint blockade. Cancer Discov. 6, 827–837 (2016).
Dummer, R. et al. Randomized phase III trial evaluating spartalizumab plus dabrafenib and trametinib for BRAF V600-mutant unresectable or metastatic melanoma. J. Clin. Oncol. 40, 1428–1438 (2022).
Ferrucci, P. F. et al. KEYNOTE-022 part 3: a randomized, double-blind, phase 2 study of pembrolizumab, dabrafenib, and trametinib in BRAF-mutant melanoma. J. Immunother. Cancer 8, e001806 (2020).
Gutzmer, R. et al. Atezolizumab, vemurafenib, and cobimetinib as first-line treatment for unresectable advanced BRAF(V600) mutation-positive melanoma (IMspire150): primary analysis of the randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 395, 1835–1844 (2020).
Ascierto, P. A. et al. Sequencing of ipilimumab plus nivolumab and encorafenib plus binimetinib for untreated BRAF-mutated metastatic melanoma (SECOMBIT): a randomized, three-arm, open-label phase II trial. J. Clin. Oncol. 41, 212–221 (2023).
Atkins, M. B. et al. Combination dabrafenib and trametinib versus combination nivolumab and ipilimumab for patients with advanced BRAF-mutant melanoma: the DREAMseq Trial-ECOG-ACRIN EA6134. J. Clin. Oncol. 41, 186–197 (2023).
Amaria, R. N. et al. Neoadjuvant plus adjuvant dabrafenib and trametinib versus standard of care in patients with high-risk, surgically resectable melanoma: a single-centre, open-label, randomised, phase 2 trial. Lancet Oncol. 19, 181–193 (2018).
Long, G. V. et al. Neoadjuvant dabrafenib combined with trametinib for resectable, stage IIIB–C, BRAF(V600) mutation-positive melanoma (NeoCombi): a single-arm, open-label, single-centre, phase 2 trial. Lancet Oncol. 20, 961–971 (2019).
Amaria, R. N. et al. Neoadjuvant immune checkpoint blockade in high-risk resectable melanoma. Nat. Med. 24, 1649–1654 (2018).
Blank, C. U. et al. Neoadjuvant versus adjuvant ipilimumab plus nivolumab in macroscopic stage III melanoma. Nat. Med. 24, 1655–1661 (2018).
Huang, A. C. et al. A single dose of neoadjuvant PD-1 blockade predicts clinical outcomes in resectable melanoma. Nat. Med. 25, 454–461 (2019).
Rozeman, E. A. et al. Identification of the optimal combination dosing schedule of neoadjuvant ipilimumab plus nivolumab in macroscopic stage III melanoma (OpACIN-neo): a multicentre, phase 2, randomised, controlled trial. Lancet Oncol. 20, 948–960 (2019).
Menzies, A. M. et al. Pathological response and survival with neoadjuvant therapy in melanoma: a pooled analysis from the International Neoadjuvant Melanoma Consortium (INMC). Nat. Med. 27, 301–309 (2021).
Menzies, A. M. et al. Neoadjuvant dabrafenib and trametinib (D plus T) for stage III melanoma: long-term results from the NeoCombi trial. J. Clin. Oncol. 40, 9580 (2022).
Patel, S. P. et al. Neoadjuvant-adjuvant or adjuvant-only pembrolizumab in advanced melanoma. N. Engl. J. Med. 388, 813–823 (2023).
Gershenwald, J. E., Scolyer, R.A. & Hess, K. R. in Melanoma of the Skin (eds Amin, M. B. et al.) pp. 563–585 (Springer, 2017).
Gershenwald, J. E. et al. Melanoma staging: evidence-based changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J. Clin. 67, 472–492 (2017).
Eisenhauer, E. A. et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur. J. Cancer 45, 228–247 (2009).
Young, H. et al. Measurement of clinical and subclinical tumour response using [18F]-fluorodeoxyglucose and positron emission tomography: review and 1999 EORTC recommendations. Eur. J. Cancer 35, 1773–1782 (1999).
Kakavand, H. et al. PD-L1 expression and immune escape in melanoma resistance to MAPK inhibitors. Clin. Cancer Res. 23, 6054–6061 (2017).
Deken, M. A. et al. Targeting the MAPK and PI3K pathways in combination with PD1 blockade in melanoma. Oncoimmunology 5, e1238557 (2016).
Braden, J. et al. NeoTrio—optimal neoadjuvant (NAT) sequencing of anti-PD-1 and BRAF targeted therapy (TT) in BRAF mutant stage III melanoma: results of histopathological analysis. Ann. Oncol. 33, S909–S909 (2022).
Versluis, J. M. et al. Survival update of neoadjuvant ipilimumab plus nivolumab in macroscopic stage III melanoma in the OpACIN and OpACIN-neo trials. Ann. Oncol. 34, 420–430 (2023).
Amaria, R. N. et al. Neoadjuvant relatlimab and nivolumab in resectable melanoma. Nature 611, 155–160 (2022).
Forde, P. M. et al. Neoadjuvant PD-1 blockade in resectable lung cancer. N. Engl. J. Med. 378, 1976–1986 (2018).
Reijers, I. L. M. et al. Relapse-free survival (RFS) update and first translational analyses of DONIMI, a study testing personalized neoadjuvant domatinostat, nivolumab (NIVO) and ipilimumab (IPI) in stage III melanoma patients (pts) based on the interferon-γ signature (IFN-γ sign) algorithm. Ann. Oncol. 33, S908–S909 (2022).
Rozeman, E. A. et al. Survival and biomarker analyses from the OpACIN-neo and OpACIN neoadjuvant immunotherapy trials in stage III melanoma. Nat. Med. 27, 256–263 (2021).
Shen, H. et al. Selective suppression of melanoma lacking IFN-γ pathway by JAK inhibition depends on T cells and host TNF signaling. Nat. Commun. 13, 5013 (2022).
Amaria, R. N. et al. Neoadjuvant systemic therapy in melanoma: recommendations of the International Neoadjuvant Melanoma Consortium. Lancet Oncol. 20, e378–e389 (2019).
Aaronson, N. K. et al. The European Organisation for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J. Natl Cancer Inst. 85, 365–376 (1993).
Cormier, J. N., Davidson, L., Xing, Y., Webster, K. & Cella, D. Measuring quality of life in patients with melanoma: development of the FACT-melanoma subscale. J. Support. Oncol. 3, 139–145 (2005).
van Akkooi, A. C. J. et al. Neoadjuvant systemic therapy (NAST) in patients with melanoma: surgical considerations by the International Neoadjuvant Melanoma Consortium (INMC). Ann. Surg. Oncol. 29, 3694–3708 (2022).
Tetzlaff, M. T. et al. Pathological assessment of resection specimens after neoadjuvant therapy for metastatic melanoma. Ann. Oncol. 29, 1861–1868 (2018).
A’Hern, R. P. Sample size tables for exact single-stage phase II designs. Stat. Med. 20, 859–866 (2001).
Khan, I., Sarker, S. J. & Hackshaw, A. Smaller sample sizes for phase II trials based on exact tests with actual error rates by trading-off their nominal levels of significance and power. Br. J. Cancer 107, 1801–1809 (2012).
Musoro, J. Z. et al. Interpreting European Organisation for Research and Treatment for Cancer Quality of Life questionnaire core 30 scores as minimally importantly different for patients with malignant melanoma. Eur. J. Cancer 104, 169–181 (2018).
Acknowledgements
We thank all the patients and their families for participating in this trial. We thank our colleagues, including investigators and site personnel, at Melanoma Institute Australia, Peter MacCallum Cancer Center and Westmead Hospital. We acknowledge the work of the INMC in supporting the development of neoadjuvant treatment for melanoma. Funding support was provided by Melanoma Institute Australia and Merck Sharp & Dohme, a subsidiary of Merck & Co (Rahway, NJ, USA). Study drugs were supplied by Merck Sharp & Dohme (pembrolizumab) and Novartis (dabrafenib and trametinib). G.V.L. is supported by an NMHRC Investigator Grant and the University of Sydney Medical Foundation. A.M.M. is supported by an NMHRC Investigator Grant, Nicholas and Helen Moore and Melanoma Institute Australia. I.B. is supported by the Bill and Patricia Ritchie Foundation. R.P.M.S. is supported by Melanoma Institute Australia. R.A.S. is supported by an NHMRC Investigator Grant. Medical writing and editorial assistance were provided by Kristen A. Perry (BAdvSc Hons I), funded by G.V.L. and Melanoma Institute Australia.
Funding
Open access funding provided by the University of Sydney.
Author information
Authors and Affiliations
Contributions
G.V.L., M.S.C., R.A.S. and A.M.M conceptualized and designed the study. G.V.L., M.S.C., G.A.Y., A.J.S., K.F.S., D.E.G., E.H., R.K., J.H., S.C., M.G., R.P.M.S., T.E.P. and A.M.M collected the data. G.V.L., M.S.C., S.N.L., A.M.M., J.R.T., I.B. and R.A.S carried out analysis and interpretation of results. G.V.L. drafted the paper. All authors reviewed the results and approved the final version of the paper.
Corresponding author
Ethics declarations
Competing interests
G.V.L. is consultant advisor for Agenus, Amgen, Array Biopharma, AstraZeneca, BioNTech, Boehringer Ingelheim, Bristol Myers Squibb, Evaxion, Hexal AG (Sandoz Company), Highlight Therapeutics S.L., IOBiotech Immunocore, Innovent Biologics USA, Merck Sharpe & Dohme, Novartis, PHMR, Pierre Fabre and Regeneron. A.M.M. is a consultant advisor for Bristol Myers Squibb, Merck Sharpe & Dohme, Novartis, Pierre Fabre, QBiotics and Roche. M.S.C. has served on advisory boards or as a consultant for Amgen, Bristol Myers Squibb, Eisai, Ideaya, Merck Sharpe & Dohme, Nektar, Novartis, Oncosec, Pierre Fabre, Qbiotics, Regeneron, Roche, Merck and Sanofi, and received honoraria from Bristol Myers Squibb, Merck Sharpe & Dohme and Novartis. D.E.G. has served on the advisory board for Amgen and received honoraria from Bristol Myers Squibb and Merck Sharpe & Dohme. R.P.M.S. has received honoraria for advisory board participation from Merck Sharpe & Dohme, Novartis and Qbiotics and speaking honoraria from Bristol Myers Squibb and Novartis. R.A.S. has received fees for professional services from Amgen, Bristol Myers Squibb, Evaxion, GlaxoSmithKline, Merck Sharp & Dohme, MetaOptima Technology, Myriad Genetics, NeraCare, Novartis, Provectus, Qbiotics and Roche. All other authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Anita Giobbie-Hurder and Antoni Ribas for their contribution to the peer review of this work. Primary Handling Editor: Ulrike Harjes, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Waterfall plots of percentage change in tumor burden following neoadjuvant therapy by pathological response.
a, Percentage change from baseline in sum of CT target lesions. b, Percentage change from baseline in SUVmax. CT, computed tomography; SUV, standardized uptake value.
Extended Data Fig. 2 Recurrence-free survival by response outcomes.
Recurrence-free survival in all patients who underwent surgery by (a) pathological response, (b) radiographic (RECIST v1.1) response and (c) metabolic (EORTC PET) response. CMR, complete metabolic response; CR, complete response; MPR, major pathological response; PD, progressive disease; PMD, progressive metabolic disease; PMR, partial metabolic response; PR, partial response; RFS, recurrence-free survival; SD, stable disease; SMD, stable metabolic disease.
Extended Data Fig. 3 Recurrence-free survival by pathological response.
Recurrence-free survival by pathological response with (a) pembrolizumab monotherapy, (b) sequential therapy and (c) concurrent therapy. MPR, major pathological response; pCR, pathological complete response; pNR, pathological non-response; pPR, pathological partial response; RFS, recurrence-free survival.
Extended Data Fig. 4 Change in EORTC QLQ-C30 Global Health Score over time.
Patients were surveyed at 6-week intervals from baseline (censored at week 60 due to small number of responses (<5)). Data are presented as mean values ± 95% CI. Mean change from baseline was compared to established levels of MCID1 improvement or deterioration. A number of responses (n) at each timepoint are displayed in the data table (range per treatment arm, 6–20). CI, confidence interval; EORTC QLQ-C30, European Organization for Research and Treatment of Cancer’s Core Quality of Life Questionnaire; MCID, minimum clinically important difference.
Supplementary information
Supplementary Information
Supplementary Table 1 and Supplementary Note (NeoTrio Protocol V4.0 sections).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Long, G.V., Carlino, M.S., Au-Yeung, G. et al. Neoadjuvant pembrolizumab, dabrafenib and trametinib in BRAFV600-mutant resectable melanoma: the randomized phase 2 NeoTrio trial. Nat Med (2024). https://doi.org/10.1038/s41591-024-03077-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41591-024-03077-5
- Springer Nature America, Inc.