Abstract
Tumor spheroids are one of the well-characterized 3D culture systems bearing close resemblance to the physiological tissue organization and complexity of avascular solid tumor stage with hypoxic core. They hold a wide-spread application in the field of pharmaceutical science and anti-cancer drug research. However, the difficulty in determining optimal technique for the generation of spheroids with uniform size and shape, evaluation of experimental outputs, or mass production often limits their usage in anti-cancer research and in high-throughput drug screening. In recent times, several studies have demonstrated various simple techniques for generating uniform-size 3D spheroids, including the hanging drop (HD), liquid overlay technique (LOT), and microfluidic approaches. Morphological alterations apart from biochemical assays, and staining techniques are suitably employed for the evaluation of experimental outcomes within 3D spheroid models. Morphological alterations in response to effective anti-cancer drug treatment in 3D tumor spheroids such as reduced spheroid size, loss of spheroid compactness and integrity or smooth surface, are highly reliable. These alterations can significantly reduce the need for biochemical assays and staining techniques, resulting in both time and cost savings. The present article specifically covers a variety of available procedures in spheroid generation. For practical applicability, we have supplemented our review study with the generation of glioblastoma U87 spheroids using HD and LOT methods. Additionally, we have also incorporated the outcome of U87 spheroid treatment with doxorubicin on spheroid morphology.





Similar content being viewed by others
Data availability
The data sets used and or/analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- 2D:
-
Two-dimensional
- 3D:
-
Three-dimensional
- 5-FU:
-
5-Fluorouracil
- 5-FUChnps:
-
5-FU loaded chitosan nanoparticles
- CAR:
-
Cell adhesion recognition
- CPT:
-
Cisplatin
- D:
-
Diameter
- D2R:
-
Dopamine D2 receptor
- DAPI:
-
4′,6-Diamidino-2-phenylindole dihydrochloride
- DOX:
-
µ
- FBS:
-
Fetal bovine serum
- GBM:
-
Glioblastoma multiforme
- GFR:
-
Growth factor reduced
- H:
-
Hour
- HD:
-
Hanging drop
- IFF:
-
Interstitial fluid flow
- LOT:
-
Liquid overlay technique
- NA:
-
Not applicable
- N/A:
-
Data not available
- NCCS:
-
National Centre for Cell Science
- OGC:
-
N-octanoyl glycol chitosan
- PDAC:
-
Pancreatic ductal adenocarcinoma
- PDMS:
-
Polydimethylsiloxane
- PEGNIO:
-
Polyethylene glycolated niosomes
- PMX:
-
Pemetrexed
- PEGNIO:
-
Polyethylene glycolated niosomes
- PEGNIO/D–C/t-Lyp-1:
-
PEGNIO/D–C conjugated with t-Lyp-1 peptide
- PNIPAM-co-AA:
-
Poly(N-isopropylacrylamide-co-acrylic acid)
- PI:
-
Propidium iodide
- RPM:
-
Revolution per minute
- STP:
-
Stiripentol
- THPMs:
-
2-Oxo-1,2,3,4-tetrahydropyrimidines
- TMZ:
-
Temozolomide
- TPZ:
-
Tirapazamine
- TME:
-
Tumor microenvironment
- ULA:
-
Ultra low attachment
- ↓:
-
Decreased/reduced
References
Cooper GM, Hausman RE. The development and causes of cancer. The cell: A molecular approach. 2nd edition. Sunderland (MA): Sinauer Associates; 2000. Available from https://www.ncbi.nlm.nih.gov/books/NBK9963/.
Fontebasso Y, Dubinett SM. Drug development for metastasis prevention. Crit Rev Oncog. 2015;20(5–6):449–73.
Zanoni M, et al. 3D tumor spheroid models for in vitro therapeutic screening: a systematic approach to enhance the biological relevance of data obtained. Sci Rep. 2016;6:19103.
Cwikiel W, et al. Malignant esophageal strictures: treatment with a self-expanding nitinol stent. Radiology. 1993;187(3):661–5.
Jacobi N, et al. Organotypic three-dimensional cancer cell cultures mirror drug responses in vivo: lessons learned from the inhibition of EGFR signaling. Oncotarget. 2017;8(64):107423–40.
Mellor HR, Ferguson DJ, Callaghan R. A model of quiescent tumour microregions for evaluating multicellular resistance to chemotherapeutic drugs. Br J Cancer. 2005;93(3):302–9.
Ware MJ, et al. Generation of homogenous three-dimensional pancreatic cancer cell spheroids using an improved hanging drop technique. Tissue Eng Part C Methods. 2016;22(4):312–21.
Ma HL, et al. Multicellular tumor spheroids as an in vivo-like tumor model for three-dimensional imaging of chemotherapeutic and nano material cellular penetration. Mol Imaging. 2012;11(6):487–98.
Karlsson H, et al. Loss of cancer drug activity in colon cancer HCT-116 cells during spheroid formation in a new 3-D spheroid cell culture system. Exp Cell Res. 2012;318(13):1577–85.
Kang A, et al. Concave microwell array-mediated three-dimensional tumor model for screening anticancer drug-loaded nanoparticles. Nanomedicine. 2015;11(5):1153–61.
Filipiak-Duliban A, Brodaczewska K, Kajdasz A, Kieda C. Spheroid culture differentially affects cancer cell sensitivity to drugs in melanoma and rcc models. Int J Mol Sci. 2022;23(3):1166.
Nederman T, et al. Demonstration of an extracellular matrix in multicellular tumor spheroids. Cancer Res. 1984;44(7):3090–7.
Miyazaki T, et al. Formation of proteoglycan and collagen-rich scaffold-free stiff cartilaginous tissue using two-step culture methods with combinations of growth factors. Tissue Eng Part A. 2010;16(5):1575–84.
Liao W, et al. Therapeutic potential of CUDC-907 (Fimepinostat) for hepatocarcinoma treatment revealed by tumor spheroids-based drug screening. Front Pharmacol. 2021;12:658197.
Wanigasekara J, et al. Plasma induced reactive oxygen species-dependent cytotoxicity in glioblastoma 3D tumourspheres. Plasma Processes Polym. 2022;19(4):2100157.
Zraikat M, Alshelleh T. Comparison between different 3D spheroid tumor invasion models. Assay Drug Dev Technol. 2020;18(5):239–42.
Vinci M, et al. Tumor spheroid-based migration assays for evaluation of therapeutic agents. Methods Mol Biol. 2013;986:253–66.
Nunes AS, et al. 3D tumor spheroids as in vitro models to mimic in vivo human solid tumors resistance to therapeutic drugs. Biotechnol Bioeng. 2019;116(1):206–26.
Baranyai Z, et al. Cellular internalization and inhibition capacity of new anti-glioma peptide conjugates: physicochemical characterization and evaluation on various monolayer- and 3D-spheroid-based in vitro platforms. J Med Chem. 2021;64(6):2982–3005.
Chaddad H, et al. Combining 2D angiogenesis and 3D osteosarcoma microtissues to improve vascularization. Exp Cell Res. 2017;360(2):138–45.
Boucherit N, Gorvel L, Olive D. 3D tumor models and their use for the testing of immunotherapies. Front Immunol. 2020;11:603640.
Tchoryk A, et al. Penetration and uptake of nanoparticles in 3D tumor spheroids. Bioconjug Chem. 2019;30(5):1371–84.
Singh MS, et al. An ovarian spheroid based tumor model that represents vascularized tumors and enables the investigation of nanomedicine therapeutics. Nanoscale. 2020;12(3):1894–903.
Martinez-Pacheco S, O'Driscoll L. Pre-clinical in vitro models used in cancer research: results of a worldwide survey. Cancers (Basel). 2021;13(23):6033.
Han SJ, Kwon S, Kim KS. Challenges of applying multicellular tumor spheroids in preclinical phase. Cancer Cell Int. 2021;21(1):152.
Khan AQ. Animal Models in Cancer Drug Discovery || Role of 3D tissue engineering models for human cancer and drug development. Animal Models in Cancer Drug Discovery, pp 309–322.
Bartosh TJ, Ylostalo JH. Preparation of anti-inflammatory mesenchymal stem/precursor cells (MSCs) through sphere formation using hanging-drop culture technique. Curr Protoc Stem Cell Biol. 2014;28:2B 6 1-2B 6 23.
Sant S, Johnston PA. The production of 3D tumor spheroids for cancer drug discovery. Drug Discov Today Technol. 2017;23:27–36.
Gebhard C, Gabriel C, Walter I. Morphological and immunohistochemical characterization of canine osteosarcoma spheroid cell cultures. Anat Histol Embryol. 2016;45(3):219–30.
Amaral RLF, et al. Comparative analysis of 3D bladder tumor spheroids obtained by forced floating and hanging drop methods for drug screening. Front Physiol. 2017;8:605.
Bruningk SC, et al. 3D tumour spheroids for the prediction of the effects of radiation and hyperthermia treatments. Sci Rep. 2020;10(1):1653.
Sirenko O, et al. High-content assays for characterizing the viability and morphology of 3D cancer spheroid cultures. Assay Drug Dev Technol. 2015;13(7):402–14.
Kessel S, et al. High-throughput 3D tumor spheroid screening method for cancer drug discovery using celigo image cytometry. SLAS Technol. 2017;22(4):454–65.
Kwapiszewska K, et al. A microfluidic-based platform for tumour spheroid culture, monitoring and drug screening. Lab Chip. 2014;14(12):2096–104.
Nath S, Devi GR. Three-dimensional culture systems in cancer research: Focus on tumor spheroid model. Pharmacol Ther. 2016;163:94–108.
Rolver MG, Elingaard-Larsen LO, Pedersen SF. Assessing cell viability and death in 3D spheroid cultures of cancer cells. J Vis Exp. 2019;(148):e59714.
Hirschhaeuser F, et al. Multicellular tumor spheroids: an underestimated tool is catching up again. J Biotechnol. 2010;148(1):3–15.
Van Zundert I, Fortuni B, Rocha S. From 2D to 3D cancer cell models-the enigmas of drug delivery research. nanomaterials (Basel). 2020;10(11):2236.
Riffle S, Hegde RS. Modeling tumor cell adaptations to hypoxia in multicellular tumor spheroids. J Exp Clin Cancer Res. 2017;36(1):102.
Sutherland RM, et al. A multi-component radiation survival curve using an in vitro tumour model. Int J Radiat Biol Relat Stud Phys Chem Med. 1970;18(5):491–5.
Abolhassani H, et al. Rapid generation of homogenous tumor spheroid microtissues in a scaffold-free platform for high-throughput screening of a novel combination nanomedicine. PLoS ONE. 2023;18(2):e0282064.
Lazzari G, et al. Multicellular spheroid based on a triple co-culture: a novel 3D model to mimic pancreatic tumor complexity. Acta Biomater. 2018;78:296–307.
Moscona A, Moscona H. The dissociation and aggregation of cells from organ rudiments of the early chick embryo. J Anat. 1952;86(3):287–301.
Xu S, Gao J. Invasiveness and metastasis of tumor spheroid aggregates of human giant cell carcinoma (lung clone strain PLA801-95D) in vitro and in vivo. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 1991;13(5):353–8.
Browning AP, Sharp JA, Murphy RJ, Gunasingh G, Lawson B, Burrage K, et al. Quantitative analysis of tumour spheroid structure. Elife. 2021;10:10:e73020.
Crnogorac MD, et al. 3D HeLa spheroids as a model for investigating the anticancer activity of Biginelli-hybrids. Chem Biol Interact. 2021;345:109565.
Sermuksnyte A, Kantminiene K, Jonuskiene I, Tumosiene I, Petrikaite V. The effect of 1,2,4-Triazole-3-thiol derivatives bearing hydrazone moiety on cancer cell migration and growth of melanoma, breast, and pancreatic cancer spheroids. Pharmaceuticals (Basel). 2022;15(8):1026.
Gupta P, Miller A, Olayanju A, Madhuri TK, Velliou E. A systematic comparative assessment of the response of ovarian cancer cells to the chemotherapeutic cisplatin in 3D Models of various structural and biochemical configurations-does one model type fit all? Cancers (Basel). 2022;14(5):1274.
Varesano S, Zocchi MR, Poggi A. Zoledronate triggers Vdelta2 T cells to destroy and kill spheroids of colon carcinoma: quantitative image analysis of three-dimensional cultures. Front Immunol. 2018;9:998.
Quail DF, Joyce JA. Microenvironmental regulation of tumor progression and metastasis. Nat Med. 2013;19(11):1423–37.
Lee J, Shin D, Roh JL. Development of an in vitro cell-sheet cancer model for chemotherapeutic screening. Theranostics. 2018;8(14):3964–73.
Azzarito G et al. Mammary epithelial and endothelial cell spheroids as a potential functional in vitro model for breast cancer research. J Vis Exp. 2021;(173).
Dey M, et al. Studying tumor angiogenesis and cancer invasion in a three-dimensional vascularized breast cancer micro-environment. Adv Biol (Weinh). 2021;5(7):e2100090.
Vinci M, et al. Advances in establishment and analysis of three-dimensional tumor spheroid-based functional assays for target validation and drug evaluation. BMC Biol. 2012;10:29.
Mulholland T, et al. Drug screening of biopsy-derived spheroids using a self-generated microfluidic concentration gradient. Sci Rep. 2018;8(1):14672.
Singh SK, et al. Critical role of three-dimensional tumorsphere size on experimental outcome. Biotechniques. 2020;69(5):333–8.
Patra B, et al. Drug testing and flow cytometry analysis on a large number of uniform sized tumor spheroids using a microfluidic device. Sci Rep. 2016;6:21061.
Casey RC, et al. Beta 1-integrins regulate the formation and adhesion of ovarian carcinoma multicellular spheroids. Am J Pathol. 2001;159(6):2071–80.
Breslin S, O’Driscoll L. The relevance of using 3D cell cultures, in addition to 2D monolayer cultures, when evaluating breast cancer drug sensitivity and resistance. Oncotarget. 2016;7(29):45745–56.
Bae Y, et al. Preparation and characterization of 3D human glioblastoma spheroids using an N-octanoyl glycol chitosan hydrogel. Int J Biol Macromol. 2021;185:87–97.
Mirab F, Kang YJ, Majd S. Preparation and characterization of size-controlled glioma spheroids using agarose hydrogel microwells. PLoS ONE. 2019;14(1):e0211078.
Bresciani G, et al. Evaluation of spheroid 3D culture methods to study a pancreatic neuroendocrine neoplasm cell line. Front Endocrinol (Lausanne). 2019;10:682.
Xu X, et al. Recreating the tumor microenvironment in a bilayer, hyaluronic acid hydrogel construct for the growth of prostate cancer spheroids. Biomaterials. 2012;33(35):9049–60.
Li Q, et al. 3D models of epithelial-mesenchymal transition in breast cancer metastasis: high-throughput screening assay development, validation, and pilot screen. J Biomol Screen. 2011;16(2):141–54.
Ivascu A, Kubbies M. Rapid generation of single-tumor spheroids for high-throughput cell function and toxicity analysis. J Biomol Screen. 2006;11(8):922–32.
Howes AL, et al. 3-Dimensional culture systems for anti-cancer compound profiling and high-throughput screening reveal increases in EGFR inhibitor-mediated cytotoxicity compared to monolayer culture systems. PLoS ONE. 2014;9(9):e108283.
Edwards K, Yao S, Pisano S, Feltracco V, Brusehafer K, Samanta S, et al. Hyaluronic acid-functionalized nanomicelles enhance SAHA efficacy in 3D endometrial cancer models. Cancers (Basel). 2021;13(16):4032.
Sherman H, Rossi AE. A novel three-dimensional glioma blood-brain barrier model for high-throughput testing of tumoricidal capability. Front Oncol. 2019;9:351.
Wanigasekara J, et al. Three-dimensional (3D) in vitro cell culture protocols to enhance glioblastoma research. PLoS ONE. 2023;18(2):e0276248.
Alves SR, et al. Characterization of glioblastoma spheroid models for drug screening and phototherapy assays. OpenNano. 2023;9:100116.
Eilenberger C, et al. Effect of spheroidal age on sorafenib diffusivity and toxicity in a 3D HepG2 spheroid model. Sci Rep. 2019;9(1):4863.
Sarisozen C, Abouzeid AH, Torchilin VP. The effect of co-delivery of paclitaxel and curcumin by transferrin-targeted PEG-PE-based mixed micelles on resistant ovarian cancer in 3-D spheroids and in vivo tumors. Eur J Pharm Biopharm. 2014;88(2):539–50.
Yakavets I, Jenard S, Francois A, Maklygina Y, Loschenov V, Lassalle HP, et al. Stroma-rich co-culture multicellular tumor spheroids as a tool for photoactive drugs screening. J Clin Med. 2019;8(10):1686.
Hagemann J, et al. Spheroid-based 3D cell cultures enable personalized therapy testing and drug discovery in head and neck cancer. Anticancer Res. 2017;37(5):2201–10.
Raghavan S, et al. Comparative analysis of tumor spheroid generation techniques for differential in vitro drug toxicity. Oncotarget. 2016;7(13):16948–61.
Corning®1536-well. Corning® 1536-well black/clear round bottom ultra-low attachment spheroid microplate, with lid, sterile. [cited 2023 23rd July]; Available from: 4527 | Corning® 1536-well Black/Clear Round Bottom Ultra-low Attachment Spheroid Microplate, with Lid, Sterile | Corning.
PrimeSurface®3D-Culture-Spheroid-plates. PrimeSurface® 3D culture spheroid plates: ultra-low attachment (ULA) plates. [cited 2023 8th July]; Available from: 356257 | Corning® Matrigel® Matrix - 3D Plate, 384-well, White/Clear Square Bottom, Phenol Red-Free, Individually Wrapped, with Lid, 5/Cs | Corning.
Corning®384-well. Corning® 384-well Spheroid Microplates. [cited 2023 22nd July]; Available from: Corning® 384-well Spheroid Microplates | Corning.
Sun Y, Hu J, Zhu M. in Emerging molecular mechanisms of cell cycle regulation in cancer: functions and potential applications. 2022, Frontiers in Oncology and Frontiers in Cell and Developmental Biology, p 168.
Corning®96-well. Corning® 96-well black/clear round bottom ultra-low attachment spheroid microplate, with lid, sterile. 2023 [cited 2023 22nd July]; Available from: 4515 | Corning® 96-well Black/Clear Round Bottom Ultra-Low Attachment Spheroid Microplate, with Lid, Sterile | Corning.
Corning®Elplasia®24-well. Corning® Elplasia® 24-well black/clear round bottom ultra-low attachment, microcavity plate, with lid. [cited 2023 23rd July]; Available from: 4441 | Corning® Elplasia® 24-well Black/Clear Round Bottom Ultra-Low Attachment, Microcavity Plate, with Lid | Corning.
Corning®Elplasia®6-well. Corning® Elplasia® 6-well black/clear round bottom ultra-low attachment, microcavity plate, with lid. [cited 2023 24th July]; Available from: 4440 | Corning® Elplasia® 6-well Black/Clear Round Bottom Ultra-Low Attachment, Microcavity Plate, with Lid | Corning.
Corning®Elplasia®96-well. Corning® Elplasia® 96-well black/clear round bottom ultra-low attachment, microcavity microplate, with lid. [cited 2023 19th July]; Available from: 4442 | Corning® Elplasia® 96-well Black/Clear Round Bottom Ultra-Low Attachment, Microcavity Microplate, with Lid | Corning.
Corning®Elplasia®12KFlask. Corning® Elplasia® 12K flask. Available from: Corning® Elplasia® 12K Flask | Corning.
Sherman H, Shyu J, Kennebunk M. Corning® Matrigel® Matrix-3D Plates for High Throughput 3D Assays. Available from: https://www.corning.com/catalog/cls/documents/application-notes/CLS-AN-572-A4.pdf
Corning®Matrigel®Matrix-3D-Plate-384-well. Corning® Matrigel® Matrix - 3D plate, 384-well, black/clear square bottom, phenol red-free, individually wrapped, with lid, 5/Cs. [cited 2023 21st July]; Available from: 356256 | Corning® Matrigel® Matrix - 3D Plate, 384-well, Black/Clear Square Bottom, Phenol Red-Free, Individually Wrapped, with Lid, 5/Cs | Corning.
Plate-384-well, C.M.M.-D. Corning® Matrigel® Matrix - 3D Plate, 384-well, White/Clear Square Bottom, Phenol Red-Free, Individually Wrapped, with Lid, 5/Cs. [cited 2023 8th July]; Available from: 356257 | Corning® Matrigel® Matrix - 3D Plate, 384-well, White/Clear Square Bottom, Phenol Red-Free, Individually Wrapped, with Lid, 5/Cs | Corning.
Corning®Matrigel®Matrix-3D-Plate-96-well. Corning® Matrigel® Matrix - 3D plate, 96-well, phenol red-free, black/clear, individually wrapped, with lid, 1/Cs. [cited 2023 20th July]; Available from: 356259 | Corning® Matrigel® Matrix - 3D Plate, 96-well, Phenol Red-Free, Black/Clear, Individually Wrapped, with Lid, 1/Cs | Corning.
Nunclon™Sphera™96-Well. Nunclon™ Sphera™ 96-well, nunclon sphera-treated, U-shaped-bottom microplate. [cited 2023 19th July]; Available from: Nunclon™ Sphera™ 96-Well, Nunclon Sphera-Treated, U-Shaped-Bottom Microplate (thermofisher.com).
Hofmann S, et al. Patient-derived tumor spheroid cultures as a promising tool to assist personalized therapeutic decisions in breast cancer. Transl Cancer Res. 2022;11(1):134–47.
Gaarn L, Marwood T, Scott R, Carter S, Granchelli J, Neeley C. The Nunclon Sphera surface supports formation of three dimensional cancer spheroids in suspension. Available from: https://www.fishersci.com/content/dam/fishersci/en_US/documents/programs/scientific/technical-documents/application-notes/thermo-scientific-sphera-cancer-application-note.pdf
ThermoScientific™96-well. 96 well plate, sphera low-attachment surface, pack of 1. [cited 2023 19th July]; Available from: 96 Well Plate, Sphera Low-Attachment Surface, Pack of 1 (thermofisher.com)
Nunclon™Sphera™Dishes. Nunclon™ Sphera™ Dishes. [cited 2023 19th July]; Available from: https://www.thermofisher.com/order/catalog/product/174943.
Nunclon™Sphera™Flasks. Nunclon™ Sphera™ Flasks. [cited 2023 19th July]; Available from: Nunclon™ Sphera™ Flasks (thermofisher.com).
Wardwell-Swanson J, et al. A framework for optimizing high-content imaging of 3D models for drug discovery. SLAS Discov. 2020;25(7):709–22.
Akura™384-Spheroid-Microplate. Akura™ 384 spheroid microplate [cited 2023 8th July]; Available from: https://shop.insphero.com/products/akura-384-spheroid-microplate-10-pack?pr_prod_strat=copurchase_transfer_learning&pr_rec_id=847ff397b&pr_rec_pid=7645112139937&pr_ref_pid=6917606047905&pr_seq=uniform.
Akura™384-ImagePro. Akura™ 384 ImagePro. [cited 2023 8th July]; Available from: Akura™ 384 ImagePro (10/pack) – InSphero.
Akura™96-Spheroid-Microplate. Akura™ 96 spheroid microplate. [cited 2023 10th July]; Available from: Akura™ 96 Spheroid Microplate (20/pack) – InSphero.
Navis, A.R., Hanging drop tissue culture. Embryo Project Encyclopedia, 2012.
Gutierrez L, et al. A hanging drop culture method to study terminal erythroid differentiation. Exp Hematol. 2005;33(10):1083–91.
Liu X et al. A novel SimpleDrop chip for 3D spheroid formation and anti-cancer drug assay. Micromachines (Basel). 2021;12(6).
Zhang W, et al. Optimization of the formation of embedded multicellular spheroids of MCF-7 cells: how to reliably produce a biomimetic 3D model. Anal Biochem. 2016;515:47–54.
Shujaa Edin HY, et al. Recombinant human erythropoietin enhanced the cytotoxic effects of tamoxifen toward the spheroid MCF-7 breast cancer cells. Saudi J Biol Sci. 2021;28(9):5214–20.
Low LTHTLE et al. A reliable and affordable 3D tumor spheroid model for natural product drug discovery: a case study of curcumin Prog Drug Discov Biomed Sci. 2019;1(1).
Jeong Y, Tin A, Irudayaraj J. Flipped well-plate hanging-drop technique for growing three-dimensional tumors. Front Bioeng Biotechnol. 2022;10:898699.
Rodriguez CE, et al. Autophagy protects from trastuzumab-induced cytotoxicity in HER2 overexpressing breast tumor spheroids. PLoS ONE. 2015;10(9):e0137920.
Monico DA, et al. Melanoma spheroid-containing artificial dermis as an alternative approach to in vivo models. Exp Cell Res. 2022;417(1):113207.
Raghavan S, et al. Formation of stable small cell number three-dimensional ovarian cancer spheroids using hanging drop arrays for preclinical drug sensitivity assays. Gynecol Oncol. 2015;138(1):181–9.
Kelm JM, et al. Method for generation of homogeneous multicellular tumor spheroids applicable to a wide variety of cell types. Biotechnol Bioeng. 2003;83(2):173–80.
Li L, LaBarbera D. 3D high-content screening of organoids for drug discovery. Comprehensive Med Chem. 2017;III:2.
Akura™PLUS-Hanging-Drop-System. [cited 2023 25th July ]; Available from: https://shop.insphero.com/products/akura-plus-spheroid-hanging-drop-system.
Lee G, et al. Generation of uniform liver spheroids from human pluripotent stem cells for imaging-based drug toxicity analysis. Biomaterials. 2021;269:120529.
Rescigno F, Ceriotti L, Meloni M. Extra cellular matrix deposition and assembly in dermis spheroids. Clin Cosmet Investig Dermatol. 2021;14:935–43.
Mohan S, et al. Assessing the predictive response of a simple and sensitive blood-based biomarker between estrogen-negative solid tumors. Adv Med Sci. 2020;65(2):424–8.
Pawlik TM, et al. Amino acid uptake and regulation in multicellular hepatoma spheroids. J Surg Res. 2000;91(1):15–25.
Casciari JJ, Sotirchos SV, Sutherland RM. Glucose diffusivity in multicellular tumor spheroids. Cancer Res. 1988;48(14):3905–9.
Foster TH, et al. Fluence rate effects in photodynamic therapy of multicell tumor spheroids. Cancer Res. 1993;53(6):1249–54.
Wigle JC, Sutherland RM. Increased thermoresistance developed during growth of small multicellular spheroids. J Cell Physiol. 1985;122(2):281–9.
Ronen S, Degani H. Studies of the metabolism of human breast cancer spheroids by NMR. Magn Reson Med. 1989;12(2):274–81.
Erlichman C, Tannock IF. Growth and characterization of multicellular tumor spheroids of human bladder carcinoma origin. In Vitro Cell Dev Biol. 1986;22(8):449–56.
Mueller-Klieser RMSBSJBHGBBW. Oxygenation and differentiation in multicellular spheroids of human colon carcinoma. Cancer Res. 1986;46(10):5320–9.
Bauman GS, et al. Effects of radiation on a three-dimensional model of malignant glioma invasion. Int J Dev Neurosci. 1999;17(5–6):643–51.
Deen DF, et al. Development of a 9L rat brain tumor cell multicellular spheroid system and its response to 1,3-bis(2-chloroethyl)-1-nitrosourea and radiation. J Natl Cancer Inst. 1980;64(6):1373–82.
Rofstad EK, Sutherland RM. Growth and radiation sensitivity of the MLS human ovarian carcinoma cell line grown as multicellular spheroids and xenografted tumours. Br J Cancer. 1989;59(1):28–35.
Achilli TM, Meyer J, Morgan JR. Advances in the formation, use and understanding of multi-cellular spheroids. Expert Opin Biol Ther. 2012;12(10):1347–60.
Sakthivel K, Hoorfar M, Kim K. High-throughput three-dimensional cellular platforms for screening biophysical microenvironmental signals. In: Micro and Nano Systems for Biophysical Studies of Cells and Small Organisms. Elsevier; 2021. p. 125–52.
Santos JM, et al. Three-dimensional spheroid cell culture of umbilical cord tissue-derived mesenchymal stromal cells leads to enhanced paracrine induction of wound healing. Stem Cell Res Ther. 2015;6(1):90.
Pinto DS, da Silva CL, Cabral JM. Scalable expansion of mesenchymal stem/stromal cells in bioreactors. A Focus on Hydrodynamic Characterization. 2019:537.
Corning®Disposable-Spinner-Flasks. Corning® disposable spinner flasks. [cited 2023 1st August 2023]; Available from: https://ecatalog.corning.com/life-sciences/b2c/US/en/Bioprocess-and-Scale-up/Disposable-Spinner-Flasks/Corning%C2%AE-Disposable-Spinner-Flasks/p/corningDisposableSpinnerFlasks.
Teale M, et al. Chemically defined, xeno-free expansion of human mesenchymal stem cells (hMSCs) on benchtop-scale using a stirred single-use bioreactor. Methods Mol Biol. 2022;2436:83–111.
Moreira JL, et al. Effect of viscosity upon hydrodynamically controlled natural aggregates of animal cells grown in stirred vessels. Biotechnol Prog. 1995;11(5):575–83.
Jossen V, Eibl R, Kraume M, Eibl D. Growth behavior of human adipose tissue-derived stromal/stem cells at small scale: numerical and experimental investigations. Bioengineering (Basel). 2018;5(4):106.
Chiesa E, Dorati R, Pisani S, Conti B, Bergamini G, Modena T, et al. The microfluidic technique and the manufacturing of polysaccharide nanoparticles. Pharmaceutics. 2018;10(4):267.
Nielsen JB, et al. Microfluidics: innovations in materials and their fabrication and functionalization. Anal Chem. 2020;92(1):150–68.
Prince E, et al. Microfluidic arrays of breast tumor spheroids for drug screening and personalized cancer therapies. Adv Healthc Mater. 2022;11(1):e2101085.
Takeuchi T. Medical checking of the aged. 13. Orthopedic diseases (2). Hokenfu Zasshi. 1989;45(2):128–9.
Sabhachandani P, et al. Generation and functional assessment of 3D multicellular spheroids in droplet based microfluidics platform. Lab Chip. 2016;16(3):497–505.
Marimuthu M, et al. Multi-size spheroid formation using microfluidic funnels. Lab Chip. 2018;18(2):304–14.
Chen MC, Gupta M, Cheung KC. Alginate-based microfluidic system for tumor spheroid formation and anticancer agent screening. Biomed Microdevices. 2010;12(4):647–54.
Au Ieong K et al. Investigation of drug cocktail effects on cancer cell-spheroids using a microfluidic drug-screening assay. Micromachines. 2017;8(6).
Sun D, et al. A novel three-dimensional microfluidic platform for on chip multicellular tumor spheroid formation and culture. Microfluid Nanofluid. 2014;17(5):831–42.
Lim W, Park S. A microfluidic spheroid culture device with a concentration gradient generator for high-throughput screening of drug efficacy. Molecules. 2018;23(12).
Ziółkowska K, et al. Development of a three-dimensional microfluidic system for long-term tumor spheroid culture. Sens Actuators, B Chem. 2012;173:908–13.
Chen Y, et al. Drug cytotoxicity and signaling pathway analysis with three-dimensional tumor spheroids in a microwell-based microfluidic chip for drug screening. Anal Chim Acta. 2015;898:85–92.
Lim W, et al. Formation of size-controllable tumour spheroids using a microfluidic pillar array (muFPA) device. Analyst. 2018;143(23):5841–8.
Barisam M, Niavol FR, Kinj MA, Saidi MS, Ghanbarian H, Kashaninejad N. Enrichment of cancer stem-like cells by controlling oxygen, glucose and fluid shear stress in a microfluidic spheroid culture device. J Sci: Adv Mater Device. 2022;7(2):100439.
Huang YL, et al. Tumor spheroids under perfusion within a 3D microfluidic platform reveal critical roles of cell-cell adhesion in tumor invasion. Sci Rep. 2020;10(1):9648.
Lee SI, Choi YY, Kang SG, Kim TH, Choi JW, Kim YJ, et al. 3D Multicellular tumor spheroids in a microfluidic droplet system for investigation of drug resistance. Polymers (Basel). 2022;14(18):3752.
Lee JM, et al. Generation of tumor spheroids using a droplet-based microfluidic device for photothermal therapy. Microsyst Nanoeng. 2020;6:52.
Lee SR, et al. U-IMPACT: a universal 3D microfluidic cell culture platform. Microsyst Nanoeng. 2022;8:126.
Lee SW, et al. In vitro lung cancer multicellular tumor spheroid formation using a microfluidic device. Biotechnol Bioeng. 2019;116(11):3041–52.
Lunt SJ, et al. Interstitial fluid pressure in tumors: therapeutic barrier and biomarker of angiogenesis. Future Oncol. 2008;4(6):793–802.
Milosevic M, Fyles A, Hill R. Interstitial fluid pressure in cervical cancer: guide to targeted therapy. Am J Clin Oncol. 2001;24(5):516–21.
Yeo SG, et al. Interstitial fluid pressure as a prognostic factor in cervical cancer following radiation therapy. Clin Cancer Res. 2009;15(19):6201–7.
Boucher Y, et al. Interstitial fluid pressure in intracranial tumours in patients and in rodents. Br J Cancer. 1997;75(6):829–36.
Munson JM, Shieh AC. Interstitial fluid flow in cancer: implications for disease progression and treatment. Cancer Manag Res. 2014;6:317–28.
Aryasomayajula A, Bayat P, Rezai P, Selvaganapathy PR. Microfluidic devices and their applications. In: Bhushan B, edetor. Springer Handbook of Nanotechnology. Springer Handbooks. Berlin, Heidelberg: Springer; 2017. p.487–536.
Sun Q, et al. Microfluidic formation of coculture tumor spheroids with stromal cells as a novel 3D tumor model for drug testing. ACS Biomater Sci Eng. 2018;4(12):4425–33.
Tsai HF, Trubelja A, Shen AQ, Bao G. Tumour-on-a-chip: microfluidic models of tumour morphology, growth and microenvironment. J R Soc Interface. 2017;14(131):20170137.
Uhl CG, Liu Y. Microfluidic device for expedited tumor growth towards drug evaluation. Lab Chip. 2019;19(8):1458–70.
Alliedmarketresearch. Microfluidic devices market research, 2031. [cited 2023 20230812]; Available from: https://www.alliedmarketresearch.com/microfluidic-devices-market-A17085.
Fortunebusinessinsights. Medical device / microfluidic devices market. [cited 2023 20230812]; Available from: https://www.fortunebusinessinsights.com/industry-reports/microfluidic-devices-market-101098.
MERCK-MO4. CellASIC ONIX switching plate mammalian cells (4 chamber). [cited 2023 12th August]; Available from: https://www.sigmaaldrich.com/IN/en/product/mm/m04s035pk.
eNUVIO. microfluidics. [cited 2023 12th August]; Available from: https://enuvio.com/product-tag/microfluidics/.
Seleci DA, et al. Tumor homing and penetrating peptide-conjugated niosomes as multi-drug carriers for tumor-targeted drug delivery. RSC Adv. 2017;7(53):33378–84.
Sivakumar H, et al. Multi-cell type glioblastoma tumor spheroids for evaluating sub-population-specific drug response. Front Bioeng Biotechnol. 2020;8:538663.
Blandin AF, et al. Glioma cell dispersion is driven by alpha5 integrin-mediated cell-matrix and cell-cell interactions. Cancer Lett. 2016;376(2):328–38.
Casey RC, et al. β1-integrins regulate the formation and adhesion of ovarian carcinoma multicellular spheroids. Am J Pathol. 2001;159(6):2071–80.
Matsuda Y, et al. Morphological and cytoskeletal changes of pancreatic cancer cells in three-dimensional spheroidal culture. Med Mol Morphol. 2010;43(4):211–7.
Smyrek I et al. E-cadherin, actin, microtubules and FAK dominate different spheroid formation phases and important elements of tissue integrity. Biol Open. 2019;8(1).
Shimazui T, et al. Role of complex cadherins in cell-cell adhesion evaluated by.pdf. Oncol Rep. 2004;11:357–60.
Saias L, et al. Cell-cell adhesion and cytoskeleton tension oppose each other in regulating tumor cell aggregation. Cancer Res. 2015;75(12):2426–33.
Ivascu A, Kubbies M. Diversity of cell-mediated adhesions in breast cancer spheroids.pdf. Int J Oncol. 2007;31:1403–13.
Weissenrieder JS, et al. The dopamine D2 receptor contributes to the spheroid formation behavior of U87 glioblastoma cells. Pharmacology. 2020;105(1–2):19–27.
Marie PJ, et al. Cadherin-mediated cell-cell adhesion and signaling in the skeleton. Calcif Tissue Int. 2014;94(1):46–54.
Maitre JL, Heisenberg CP. Three functions of cadherins in cell adhesion. Curr Biol. 2013;23(14):R626–33.
Gumbiner BM. Cell adhesion: the molecular basis of tissue architecture and morphogenesis. Cell. 1996;84(3):345–57.
Ivascu A, Kubbies M. Diversity of cell-mediated adhesions in breast cancer spheroids. Int J Oncol. 2007;31(6):1403–13.
Schliwa M. Action of cytochalasin D on cytoskeletal networks. J Cell Biol. 1982;92(1):79–91.
Galateanu B, et al. Impact of multicellular tumor spheroids as an in vivolike tumor model on anticancer drug response. Int J Oncol. 2016;48(6):2295–302.
Gomes A, et al. Evaluation by quantitative image analysis of anticancer drug activity on multicellular spheroids grown in 3D matrices. Oncol Lett. 2016;12(6):4371–6.
Thakuri PS, et al. Quantitative size-based analysis of tumor spheroids and responses to therapeutics. Assay Drug Dev Technol. 2019;17(3):140–9.
Kulesza J, Pawłowska M, Augustin E. The influence of antitumor unsymmetrical bisacridines on 3D cancer spheroids growth and viability. Molecules. 2021;26(20):6262.
Smith T, Affram K, Bulumko E, Agyare E. Evaluation of in-vitro cytotoxic effect of 5-FU loaded-chitosan nanoparticles against spheroid models. J Nat Sci. 2018;4(10):e535.
Akasov R, et al. Formation of multicellular tumor spheroids induced by cyclic RGD-peptides and use for anticancer drug testing in vitro. Int J Pharm. 2016;506(1–2):148–57.
Yadav A, et al. Repurposing an antiepileptic drug for the treatment of glioblastoma. Pharm Res. 2022;39(11):2871–83.
Wang J, et al. Anti-gastric cancer activity in three-dimensional tumor spheroids of bufadienolides. Sci Rep. 2016;6:24772.
Kim CH, et al. Vertically coated graphene oxide micro-well arrays for highly efficient cancer spheroid formation and drug screening. Adv Healthc Mater. 2020;9(7):e1901751.
Ivanov DP, et al. Multiplexing spheroid volume, resazurin and acid phosphatase viability assays for high-throughput screening of tumour spheroids and stem cell neurospheres. PLoS ONE. 2014;9(8):e103817.
Gendre DAJ, et al. Optimization of tumor spheroid model in mesothelioma and lung cancers and anti-cancer drug testing in H2052/484 spheroids. Oncotarget. 2021;12(24):2375–87.
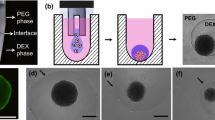
Lemmo S, et al. Optimization of aqueous biphasic tumor spheroid microtechnology for anti-cancer drug testing in 3D culture. Cell Mol Bioeng. 2014;7(3):344–54.
Ghosh S. Cisplatin: the first metal based anticancer drug. Bioorg Chem. 2019;88:102925.
Johnson-Arbor K, Dubey R. Doxorubicin. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459232/.
Carvalho C, et al. Doxorubicin: the good, the bad and the ugly effect. Curr Med Chem. 2009;16(25):3267–85.
Thorn CF, et al. Doxorubicin pathways: pharmacodynamics and adverse effects. Pharmacogenet Genomics. 2011;21(7):440–6.
Moriwaki T, et al. Cytotoxicity of tirapazamine (3-amino-1,2,4-benzotriazine-1,4-dioxide)-induced DNA damage in chicken DT40 cells. Chem Res Toxicol. 2017;30(2):699–704.
Massaro F, Molica M, Breccia M. Ponatinib: a review of efficacy and safety. Curr Cancer Drug Targets. 2018;18(9):847–56.
Tyagi A, et al. Cervical cancer stem cells manifest radioresistance: association with upregulated AP-1 activity. Sci Rep. 2017;7(1):4781.
Ganesh K, Massague J. Targeting metastatic cancer. Nat Med. 2021;27(1):34–44.
Martin TA, Ye L, Sanders AJ, Lane J, Jiang WG. Cancer invasion and metastasis: molecular and cellular perspective. In: Madame Curie Bioscience Database [Internet]. Austin (TX): Landes Bioscience; 2013. Available from: https://www.ncbi.nlm.nih.gov/books/NBK164700/.
Hunter KW, Crawford NP, Alsarraj J. Mechanisms of metastasis. Breast Cancer Res. 2008;10 Suppl 1(Suppl 1):S2.
Stoletov K, Beatty PH, Lewis JD. Novel therapeutic targets for cancer metastasis. Expert Rev Anticancer Ther. 2020;20(2):97–109.
Jones NP, et al. PLCgamma1 is essential for early events in integrin signalling required for cell motility. J Cell Sci. 2005;118(Pt 12):2695–706.
Tomas NM, et al. Akt and phospholipase Cgamma are involved in the regulation of growth and migration of MDA-MB-468 breast cancer and SW480 colon cancer cells when cultured with diabetogenic levels of glucose and insulin. BMC Res Notes. 2012;5:214.
Moser C, et al. Blocking heat shock protein-90 inhibits the invasive properties and hepatic growth of human colon cancer cells and improves the efficacy of oxaliplatin in p53-deficient colon cancer tumors in vivo. Mol Cancer Ther. 2007;6(11):2868–78.
Schmidt M, et al. The influence of Osmunda regalis root extract on head and neck cancer cell proliferation, invasion and gene expression. BMC Complement Altern Med. 2017;17(1):518.
Sharudin NA, et al. Invasion and metastasis suppression by anti-neonatal Nav1.5 antibodies in breast cancer. Asian Pac J Cancer Prev. 2022;23(9):2953–64.
Xu X, et al. ITGA5 promotes tumor angiogenesis in cervical cancer. Cancer Med. 2023;12(10):11983–99.
Laborda-Illanes A, et al. Development of in vitro and in vivo tools to evaluate the antiangiogenic potential of melatonin to neutralize the angiogenic effects of VEGF and breast cancer cells: CAM assay and 3D endothelial cell spheroids. Biomed Pharmacother. 2023;157:114041.
Bayat N, et al. The anti-angiogenic effect of atorvastatin in glioblastoma spheroids tumor cultured in fibrin gel: in 3D in vitro model. Asian Pac J Cancer Prev. 2018;19(9):2553–60.
Bhat SK, et al. P-I metalloproteinases and L-amino acid oxidases from Bothrops species inhibit angiogenesis. J Venom Anim Toxins Incl Trop Dis. 2021;27: e20200180.
Szade K, et al. Spheroid-plug model as a tool to study tumor development, angiogenesis, and heterogeneity in vivo. Tumour Biol. 2016;37(2):2481–96.
Han M, et al. Enhanced percolation and gene expression in tumor hypoxia by PEGylated polyplex micelles. Mol Ther. 2009;17(8):1404–10.
Wortzel I, Seger R. The ERK cascade: distinct functions within various subcellular organelles. Genes Cancer. 2011;2(3):195–209.
Nitulescu GM, et al. The Akt pathway in oncology therapy and beyond (Review). Int J Oncol. 2018;53(6):2319–31.
Ettrich TJ, Seufferlein T. Regorafenib. Recent Results Cancer Res. 2018;211:45–56.
Abdelgalil AA, Al-Kahtani HM, Al-Jenoobi FI. Erlotinib. Profiles Drug Subst Excip Relat Methodol. 2020;45:93–117.
Zoetemelk M, et al. Short-term 3D culture systems of various complexity for treatment optimization of colorectal carcinoma. Sci Rep. 2019;9(1):7103.
Organ SL, Tsao MS. An overview of the c-MET signaling pathway. Ther Adv Med Oncol. 2011;3(1 Suppl):S7–19.
Expasy. Cellosaurus U-87MG Uppsala (CVCL_GP63). 12-Jan-2021 [cited 2022 22nd November]; Available from: https://www.cellosaurus.org/CVCL_GP63.
Larjavaara S, et al. Incidence of gliomas by anatomic location. Neuro Oncol. 2007;9(3):319–25.
Belousov A, et al. The extracellular matrix and biocompatible materials in glioblastoma treatment. Front Bioeng Biotechnol. 2019;7:341.
Chen W, Wong C, Vosburgh E, Levine AJ, Foran DJ, Xu EY. High-throughput image analysis of tumor spheroids: a user-friendly software application to measure the size of spheroids automatically and accurately. J Vis Exp. 2014;(89):51639.
Wallberg F, Tenev T, Meier P. Analysis of apoptosis and necroptosis by fluorescence-activated cell sorting. Cold Spring Harb Protoc. 2016;2016(4):pdb prot087387.
Crowley LC, Marfell BJ, Waterhouse NJ. Analyzing cell death by nuclear staining with Hoechst 33342. Cold Spring Harb Protoc. 2016;2016(9). https://doi.org/10.1101/pdb.prot087205.
Crowley LC et al. Measuring cell death by propidium iodide uptake and flow cytometry. Cold Spring Harb Protoc. 2016;2016(7). https://doi.org/10.1101/pdb.prot087163.
Chen H, et al. Clinical significance of ALDH1 combined with DAPI expression in patients with esophageal carcinoma. Oncol Lett. 2017;14(4):4878–82.
Otto FJ. High-resolution analysis of nuclear DNA employing the fluorochrome DAPI. Methods Cell Biol. 1994;41:211–7.
Acknowledgements
We are thankful to Prof. Savita Roy, Principal, Daulat Ram College, University of Delhi, for providing constant support and lab facility throughout the investigation and Late Dr Amar Jyoti for the initial efforts to conceptualize.
Funding
The study was supported by research grants from Indian Council of Medical Research (ICMR-ICRC) to ACB (No.5/13/4/ACB/ICRC/2020/NCD-III), grant from Institution of Eminence University of Delhi (Ref. No./IoE/2021/12/FRP) to ACB, grant from CSIR-UGC to A. Chhokar [573(CSIR-UGC NET JUNE 2017)]; grant from CSIR to NA (09/045(1622)/2019-EMR-I); grant from CSIR to JY (09/045(1629)/2019-EMR-I); grant from CSIR-UGC to TT (764/(CSIR-UGC NET JUNE 2019); grant from CSIR to DJ (09/0045/(11635)/2021-EMR-1) and grant from CSIR to A. Chaudhary (09/0045(12901)/2022-EMR-1). This study was partly supported by the UGC-FRPS grant [Ref. F.30–400/2017(BSR F.D.Dy.No.5326] & SERB-ECR grant (Ref.ECR/2016/000897) to late Dr Amar Jyoti, Neuropharmacology and Drug Delivery Laboratory, Daulat Ram College, University of Delhi, Delhi.
Author information
Authors and Affiliations
Contributions
Conceptualization: ACB and AS. Data curation: AS and ACB. Formal analysis: AS, SL, JK, NG, DJ, TT, NA, AC, JY, and AC. Funding acquisition: ACB. Investigation: AS, SL, JK, NG, DJ, and ACB. Methodology: AS, SL, JK, NG, DJ, TT, NA, AC, JY, and AC. Project administration: ACB. Resources: ACB and AS. Supervision: ACB. Validation: ACB. Visualization: AS, DJ, TT, NA, and ACB. Writing original draft: AS and ACB. Review and editing: ACB.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
NA
Consent for publication
All authors have read the final manuscript and agreed to the publication.
Competing interests
The authors declare no competing interests.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Senrung, A., Lalwani, S., Janjua, D. et al. 3D tumor spheroids: morphological alterations a yardstick to anti-cancer drug response. In vitro models 2, 219–248 (2023). https://doi.org/10.1007/s44164-023-00059-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44164-023-00059-8