Abstract
Carbon materials have emerged as a rapidly advancing category of high-performance materials that have garnered significant attention across various scientific and technological disciplines. Their exceptional biochemical properties render them highly suitable for diverse biomedical applications, including implantation, artificial joints, bioimaging, tissue and bone engineering, and scaffold fabrication. However, a more systematic approach is required to fully exploit the potential of carbon-based materials in the biomedical realm, necessitating extensive and collaborative research to address the existing challenges, which comprehensive long-term stability studies, the surface properties and investigate the toxicity of biomedical materials. This review paper aims to provide a comprehensive overview of carbon materials, elucidating their inherent advantages and highlighting their increasingly prominent role in biomedical applications. After a brief introduction of carbonaceous materials, we discuss innovative deposition strategies that can be utilized to artificially replicate desired properties, such as biocompatibility and toxicology, within complex structures. Further, this paper serves as a valuable resource to harness the potential of carbon materials in the realm of biomedical applications. Last, we conclude with a discussion on the significance of continuous exploration in propelling further advancements within this captivating field.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
1 Introduction
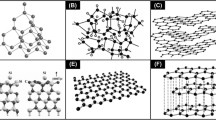
In recent years, significant progress has occurred in the field of biomedical materials and technologies, establishing a robust foundation for forthcoming advancements and practical applications [1, 2]. Within the expanding landscape of academic inquiry, carbon-based materials, including carbon dots, carbon nanotubes (CNTs), graphene, carbon nanofibers (CNFs), and MXenes, have emerged as key focal points, presenting themselves as promising candidates for future material design and utilization [3].
Carbon dots, characterized as zero-dimensional (0D) materials with singular domains of small size (typically 1 to 30 nm in diameter), have garnered significant attention due to their low toxicity, facile surface functionalization, diverse raw material sources, cost-effectiveness, excellent fluorescence stability, adjustable emission wavelength, and biocompatibility [4,5,6,7,8,9,10]. CNTs, classified as 1D materials based on the number of graphene layers comprising the tube, exhibit significant promise as optical tags (nanoprobe labels) or contrast agents in various biomedical imaging techniques. These include applications in Raman spectroscopy, near-infrared (NIR) fluorescence imaging, and photoacoustic imaging across a diverse range of biological specimens, predominantly observed in the case of single-walled nanotubes. Furthermore, the tubular architecture affords a versatile platform for drug encapsulation, thereby enabling precise control over drug release kinetics and targeted therapeutic interventions in the realm of medical treatments [11,12,13,14,15].
Graphene consists of single-atom-thick sheets of sp2-bonded carbon atoms closely packed into a 2D honeycomb lattice. Graphene and its derivatives, such as graphene oxide (GO) and reduced graphene oxide (rGO), exhibit unique properties including large surface area, strong laser absorption property, high elasticity, good charge-transfer ability, and ferromagnetic properties [16,17,18,19]. In addition, graphene’s excellent electrical conductivity makes it an ideal material for biosensors. Functionalized graphene can be employed to detect specific biomolecules with high sensitivity, enabling early diagnosis of diseases. GO also serves as contrast agents in various imaging techniques, including magnetic resonance imaging (MRI) and photoacoustic imaging, providing enhanced contrast for more accurate diagnostics [20, 21].
CNFs are nanoscale materials characterized by a fibrous structure primarily composed of carbon atoms. Their extensive application as reinforcing elements in tissue engineering scaffolds is attributed to their impressive mechanical strength, electrical conductivity, and structural integrity. This utilization enhances cell adhesion and contributes to the regeneration of tissues, exemplified in applications like artificial teeth and hip joints. In these contexts, CNFs are progressively supplanting metal materials, addressing concerns such as corrosion and diminished impact resistance associated with traditional metals [22,23,24,25,26,27,28].
MXenes are a unique class of 2D materials comprised of transition metal carbides, nitrides, or carbonitrides with a general formula of Mn+1Xn (n = 1–3), where “M” represents an early transition metal and “X” denotes carbon or nitrogen. This combination of complete metal atomic layers and abundant surface functional groups enables MXenes to possess both metallic conductivity and hydrophilic properties [29,30,31]. These materials exhibit a thickness of less than 1 nm due to their limited number of atomic layers. Their nanoscale size allows for prolonged circulation within biological systems while also introducing unique characteristics, such as enhanced molecular interactions and size-dependent luminescence [32,33,34]. MXenes present promising possibilities for highly sensitive disease diagnosis and efficient treatment.
Distinguished by their unique attributes, the burgeoning interest in carbon-based materials as reinforcements for biomedical applications has been rapidly growing, positioning them particularly well for pivotal roles in various biomedical applications. Notably, carbon materials display a reduced propensity for eliciting immune responses compared to alternative materials, such as metal nanoparticles—a critical feature for sustained biological interactions, especially in the realm of implantable organ devices [35,36,37,38].
Moreover, carbon-based materials and their hybrid metal/polymer/ceramic nanocomposites demonstrate significant potential across a broad spectrum of biomedical applications. The collaborative interaction among these constituents establishes a synergistic relationship, augmenting the overall strength of the produced nanocomposites. Carbon-based materials assume a pivotal role in enhancing the chemical and mechanical properties of the hybrid nanocomposites, capitalizing on their diminutive size, expansive surface area, and surface modification capabilities. The polymer matrix serves the crucial function of maintaining an optimal distance between the carbon materials, preventing agglomeration. Concurrently, the amalgamation of ceramics with carbon materials facilitates the concurrent existence of photoluminescence and magnetic properties, contributing to wear resistance and dispersion control. Simultaneously, metal nanoparticles enhance the mechanical properties, thermal stability, and electrical conductivity within the hybrid nanocomposites. This precise control at the nanoscale renders them versatile for specific and sophisticated biomedical applications, such as highly controlled drug delivery systems, tissue engineering, medical imaging, implant coatings, diagnostic tools, and biosensors [39, 40]. An exemplary illustration of their capabilities lies in advanced designs enabling precise drug transport to targeted areas within the body, thereby enhancing efficacy, minimizing side effects, and enabling controlled release—a transformative paradigm in disease treatment. These adaptable materials manifest in various formats, including films, nanofibers, hydrogels, and 3D porous structures, extending their utility across a diverse range of biomedical applications [41, 42].
However, certain nanoparticles, such as CNTs and MXenes, continue to pose challenges due to their inherent toxicity. Overcoming these challenges necessitates precise functionalization, sophisticated dispersion methods, or targeted modifications aligned with specific biomedical goals. Various techniques, such as electrospinning, microsphere fabrication, nanocomposite synthesis, hydrogel formulation, deposition coating, and 3D printing, have also been widely acknowledged for their potential in augmenting biomedical applications. Furthermore, strict adherence to preclinical safety pharmacology guidelines set forth by regulatory bodies such as the Food and Drug Administration (FDA), the International Conference on Harmonization (ICH), and the European Medicines Agency (EMA) is imperative [43,44,45,46,47,48,49,50,51]. Achieving enduring biocompatibility emerges as a pivotal milestone for the widespread acceptance and seamless integration of carbonaceous nanomaterials in biomedical applications.
This article presents a systematic and thorough analysis of carbon-based materials and deposition techniques used for biomedical applications, encompassing methods such as chemical vapor deposition (CVD), plasma-enhanced chemical vapor deposition (PECVD), ion-beam (IB), electrospinning, 3D printing, diamond-like carbon (DLC) coating, and hydrogel fabrication. Historically, the scientific literature has predominantly focused on either the investigation of carbon-based materials or the exploration of deposition methodologies in isolation. However, this paper aims to bridge this gap by providing comprehensive insights into both the materials and techniques, with a specific emphasis on their application in the biomedical field. By undertaking this study, our objective is to contribute to the existing knowledge base by offering valuable guidance on the selection of suitable carbon allotropes and deposition techniques for biomedical applications. The scope and structure of the review are shown in a schematic diagram in Fig. 1.
2 Carbon-based materials for biomedical applications
Carbon materials have expanded the horizons of research in biomedical applications, encompassing fields such as tissue engineering and bioimaging. Carbon materials inherently possess a diverse range of properties, which can be substantially amplified through nanostructure engineering and appropriate surface functionalization, further enhancing their contributions to these domains. The details of the different nanostructured carbon materials and the latest research are discussed in the subsequent sections of this review.
2.1 Carbon quantum dots (CQDs) and their composites
Carbon quantum dots (CQDs) have drawn great attraction and play a pivotal role in biomedical applications. CQDs are highly sensitive to changes in their local environment, making them ideal for biosensing applications. CQDs exhibit strong and tunable fluorescence properties, rendering them indispensable for use as imaging agents, particularly in live-cell imaging and the monitoring of cellular processes. Furthermore, they have the capability to transform absorbed light into thermal energy, a phenomenon referred to as photothermal conversion. This attribute is strategically utilized in photothermal therapy, where CQDs are employed to selectively eliminate cancer cells by delivering controlled heat upon laser irradiation [52,53,54]. CQDs are emerging as a promising alternative to semiconductor QDs known for stable fluorescence. Unlike semiconductor QDs with high toxicity due to heavy metals, CQDs offer biocompatible, cost-effective, and chemically inert fluorescent solutions for clinical applications [55].
Tian et al. introduced a one-pot strategy for the synthesis of targeting agent functionalized graphitic carbon nitride quantum dots (CNQDs), as shown in Fig. 2a−e [56]. The resulting FA-CNQDs exhibited several desirable characteristics, including intense fluorescence, stable colloidal properties, and biocompatibility in vitro and in vivo. Moreover, the FA-CNQDs demonstrated exceptional capabilities for targeted fluorescence imaging and penetration of multicellular spheroids that overexpress FA receptors. This strategy holds promise for extensive applications in diverse functionalized CNQDs, spanning device development, sensing, and bioimaging. Moreover, the study’s exploration of in vivo biocompatibility holds the potential to propel CNQDs further in the field of biomedicine. Wang et al. proposed a feasible atomic-hybridization strategy for attaching CQDs onto the surface of ZnO microspheres (Fig. 2f−k) [57]. By breaking the C = O bonds in the CQDs and subsequent orbital hybridization of Zn-3d orbital and C-2p, the researchers achieved efficient carrier recombination and the emergence of magnetism at room temperature. Also, the HEI-OC-1 cells are cultured in a medium containing varying concentrations of CQDs/ZnO (20, 40, 60, 80, and 100 ppm) for a duration of 24 h. The findings illustrated in Fig. 2j reveal that cellular viability can be sustained at a high level of bioactivity, irrespective of the concentration of CQDs/ZnO. The fluorescence image of cells colored with bioprobes in Fig. 2k also confirms that almost all the cells retain their activity after incubation with CQDs/ZnO sample at 100 ppm. Thus, the bioprobes proposed, comprising CQD/ZnO hybrid materials, can be evaluated to confirm the absence of cytotoxicity. This assessment underscores their enhanced biocompatibility and suitability for biological applications. These properties, including biocompatibility and electronic modulation, unveil exciting prospects for seamlessly integrating fluorescence optical imaging (FOI) and magnetic resonance imaging (MRI) technologies, thus enabling precise clinical diagnoses and surgical procedures with utmost accuracy.
A TEM image of FA-CNQDs. b Cell viabilities of HepG2 cells treated with different concentrations of FA-CNQDs and CNQDs, respectively, for 24 h, by CCK-8 assay. c H&E-stained major organs collected from mice post-intraperitoneal administration of 0.1 mL of 1 mg/mL nanomaterials every other day for 2 weeks. d Flow cytometry analysis of the apoptosis of HepG2 cells subjected to the treatments of CNQDs and FA-CNQDs with concentration of 200 µg/mL. e CLSM images of HepG2 cells after incubation with FA-CNQDs for 2 h. Excitation wavelength = 405 nm, scale bar = 100 µm. Reproduced with permission from [56], Copyright 2022, Elsevier. f Schematic of CQDs/ZNO. g FESEM image of CQDs/ZnO sample. h M − H curves of the ZnO and CQDs/ZnO at room temperature. i The orbital-resolved DOS for C element at CQDs/ZnO. j Cell viability of HEI-OC-1 cells treated with different concentrations of CQDs/ZnO. k Fluorescence image of cells stained with CQDs/ZnO sample. Reproduced with permission from [57], Copyright 2023, Wiley–VCH
2.2 Carbon nanotube (CNT) and their composites
CNTs are composed of three carbon atoms coordinated in a pyramidal fashion, transitioning from sp3 hybridization to sp2 hybridization [58]. Normally, CNTs are available in the form of SWCNTs (single layer, a diameter of smaller than 20 nm) and MWCNTs (multiple layer, a diameter greater than 30 nm) [59, 60]. MWCNTs and SWCNTs play complementary roles in biomedical applications, with MWCNTs providing structural support and controlled release, such as suppression of uncontrolled cell growth in the biomedicine, while SWCNTs excel in precision targeting and cellular imaging applications [61,62,63].
Zadeh et al. reported the electrospun polyurethane (PU)/MWCNT composites with varying amounts of CNTs but consistent fiber diameter for potential biomedical applications (Fig. 3a−c) [64]. The authors showed that adding CNTs caused an increase in crystallinity percentage, water absorption ratio, Young’s modulus, toughness, conductivity, degradation time in an accelerated medium, clotting time, and human umbilical vein endothelial cell adhesion. Moreover, no significant cytotoxicity was observed for 7-day extracts of all samples.
A Comparison of the integrity of different samples before and after 48 days of immersion in CoCl2. b HUVEC proliferation on the electrospun mats according to the content of CNTs and tissue culture plate as a control for 7 days. c Cell viability percentage after 7 days of culture. Reproduced with permission from [64], Copyright 2021, Elsevier. d Scaffold and SEM images of the 3D-printed CNT/CS/AL composite scaffold. e Cell viability and proliferation. Reproduced with permission from [65], Copyright 2023, Wiley–VCH. f SEM images of MG63 cells seeded on PHB-starch-1%MWNT electrospun scaffolds at days 1 and 7. g Remaining weight and h the pH of incubated PBS of PHB-S and PHB-S-1%MWCNT electrospun scaffolds (statistical difference with *p < 0.05). i Cell viability as indicated with MTT assay of MG-63 cells seeded on PHB-S, PHB-S-1%MWCNT electrospun scaffolds, and control group at days 1, 3, and 7 (statistical difference with **p < 0.01). Reproduced with permission from [66], Copyright 2022, Elsevier
Suo et al. prepared a MWCNT/chitosan/sodium alginate (CNT/CS/AL) ternary composite hydrogel via 3D printing technology for porous scaffolds (Fig. 3d, e) [65]. The study investigated its impact on human periodontal ligament cell (hPDLC) proliferation and its antibacterial properties against Porphyromonas gingivalis. The results demonstrated the successful fabrication of CNT/CS/AL porous composite scaffolds with uniform pores, and the scaffold’s degradation rate and swelling degree decreased as the CNT concentration increased. Additionally, the CNT/CS/AL scaffold exhibited excellent biocompatibility, promoting hPDLC proliferation, with the 0.5% CNT/CS/AL scaffold showing the highest biocompatibility among the tested concentrations Furthermore, in vitro antibacterial experiments revealed that the CNT/CS/AL scaffold exhibited bacteriostatic effects on P. gingivalis, with increased antimicrobial activity observed when the CNT concentration exceeded 0.5%, resulting in the inactivation of approximately 30% of the bacteria.
Asl et al. developed electrospun nanocomposite scaffolds using a combination of polyhydroxybutyrate (PHB), starch, and MWCNTs, as depicted in Fig. 3f and g [66]. The prepared scaffolds underwent comprehensive characterization, including assessments of their morphology, porosity, thermal and mechanical properties, biodegradability, bioactivity, and their impact on cell function. The results revealed that the scaffold incorporating 1 wt% MWCNTs exhibited the smallest fiber diameter (124 ± 44 nm), with a porosity exceeding 80% and the highest tensile strength (24.37 ± 0.22 MPa). The addition of MWNTs positively influenced surface roughness (Ra) and hydrophilicity. Scanning electron microscopy (SEM) revealed the formation of calcium phosphate deposits on scaffold surfaces after immersion in simulated body fluid (SBF), a finding confirmed by energy-dispersive spectrometry (EDS) and X-ray diffraction (XRD) analysis. Moreover, MG63 cells demonstrated robust growth on the MWCNT-containing scaffold, exhibiting increased cell viability, alkaline phosphatase (ALP) secretion, calcium deposition, and gene expression compared to scaffolds lacking MWCNTs.
2.3 Carbon nanofiber (CNF)-reinforced composites
Carbon fibers are strong and thin fibers made primarily of carbon atoms. Carbon fiber-reinforced composites are used in orthopedic implants, such as bone plates, screws, and artificial joints due to their exceptional strength-to-weight ratio [67,68,69]. These materials offer excellent strength and durability while being lightweight and biocompatible making them suitable for load-bearing applications, such as a support for dental crowns and bridges [70,71,72,73].
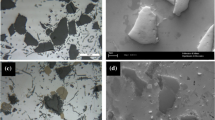
Feng et al. explored a composite material consisting of polyether ether ketone (PEEK), zinc oxide nanoparticles (ZnO), and short carbon fibers (SCFs) for an artificial joint material, as shown in Fig. 4a−c [23]. ZnO-modified short carbon fiber (SCF) powder was incorporated into PEEK through a melt-blending process, followed by injection molding. This approach aimed to enhance both the wear resistance and antibacterial characteristics of PEEK. The findings revealed that the resulting PEEK/ZnO-SCF composite exhibited a dense microstructure, with the addition of ZnO facilitating the integration of SCF and PEEK. The addition of SCF could improve the mechanical properties of the resultant composites. The PEEK/ZnO-SCF composite showed good antibacterial activity against Escherichia coli and Staphylococcus aureus and had good biocompatibility.
A Synthesis of ZnO-SCF: micromorphology of ZnO-SCF composite powder and EDS of ZnO-SCF composite powder. b Live/dead staining image: PEEK composite material and pure PEEK. c SEM images after XLPE wear: PEEK/ZnO-SCF. d PEEK/ZnO-SCF composites with different contents were cultured with E. coli and S. aureus for 24 h and e diameter of the inhibition zone. Reproduced with permission from [23], Copyright 2022, ACS. f PLA/CFRC specimen. g Prototype stem, PLA (layer, 1, 2, and 3), CFRC (layer, 2 and 4). h Percentage of cell viability (MTT) in peripheral blood mononuclear cells and L929 fibroblast cells. Both cells were exposed for 24 h to PLA, PLA/CFRC, and CFRC surfaces. All measurements were made in triplicate (average ± standard deviation). Reproduced with permission from [24], Copyright 2023, Elsevier
Paz-González et al. developed a structural composite using 3D printed-polylactic acid (PLA) and carbon fiber laminates (PLA/CFRC, Fig. 4d−f) with a potential application in implant prosthetics [24]. The composite showed good cytocompatibility with more than 80% cell viability, a tensile modulus of 19.3 ± 0.5 GPa, and tensile strength of 238.91 ± 25.95 MPa, with mechanical properties closely analogous to bone. The findings indicate that the suggested PLA/CFRC composite holds promise as a potential material for manufacturing femoral stem hip prostheses.
2.4 Graphene and their composites
Graphene, a single layer of carbon atoms arranged in a two-dimensional honeycomb lattice, possesses exceptional properties, including outstanding electrical and thermal conductivity, mechanical strength, and a substantial surface area [74,75,76]. The graphene family encompasses various materials, including few-layer graphene (2 − 5 layers), multilayer graphene (2 − 10 layers), and graphene oxide (GO), each exhibiting distinct lateral dimensions, thicknesses, and functionalities [77]. While ideally single-layer graphene presents limitations for widespread biomedical applications, such as challenges in scalable synthesis, poor dispersibility in aqueous solutions, and concerns about biocompatibility and toxicity [78,79,80], other members of the graphene family, particularly GO, have gained prominence as preferred materials in biomedical research [81,82,83,84,85].
Li et al. reported GO coated-sulfonated carbon fiber/polyetheretherketone (PEEK) composites for mechanical and biological properties, as shown in Fig. 5a−c [81]. The fabricated GO-sulfonated carbon fiber/PEEK composites exhibited a three-dimensional porous structure with a bioactive GO coating. Both in vitro and in vivo assessments, using the cell counting kit-8 (CCK-8) and histological examination of hematoxylin and eosin (H&E)-stained sections, respectively, demonstrated the biocompatibility and non-toxic nature of these composites In addition, the composites showed increased apatite deposition in the SBF test, upregulated expression of osteogenic genes by reverse transcription-PCR (RT-PCR), and better osseointegration by micro-computed tomography (micro-CT) analysis after surface modification, including ALP, Runt-related transcription factor 2 (Runx-2), Col-I, and OC. The results suggested that these materials hold promise for use in biomedical engineering applications, particularly as bone implants and tissue engineering scaffolds.
A Surface morphology of GO-SCF/PEEK composites before and after SBF immersion observed by SEM. b In vitro cytotoxicity of the PEEK and CF/PEEK composites with and without surface modification for 1 day, 4 days, and 7 days by CCK-8 assay, *p < 0.05. c Histological evaluation of viscera extracted from rats which are implanted with GO-SCF/PEEK composites including hearts, lungs, spleens, and kidneys. Reproduced with permission from [81], Copyright 2022, Elsevier. d Electrospun nanofiber mat (PU-GPCL). e In vitro degradation of electrospun nanofiber mats in PBS for 8 weeks. f Results of MTT assay after 3 and 10 days (a) and optical microscopy images of 3T3 fibroblast cells cultured in control and g PU-G0.5, PU-G1, PU-GPCL, and PU-GPCL1. Reproduced with permission from [84], Copyright 2021, Elsevier. h SEM of GCNT-HAP composites at different magnifications. i Cell viability analysis, the cells are incubated for 1, 3, and 5 days and comparison of all the fillers reinforced HAP composites. Reproduced with permission from [85], Copyright 2021, Elsevier
Razzaghi et al. examined the effect of graphene in electrospun PU nanocomposites mats grafted with polycaprolactone (PCL)-functionalized GO nanosheets, as shown in Fig. 5d−g [84]. The inclusion of graphene nanosheets in the nanocomposites improved electron signal diffusion, enhancing 3T3 fibroblast cell proliferation, attachment, and viability on PU-graphene and PU/reduced polycaprolactone-grafted graphene oxide (GPCL) nanofiber mats. Furthermore, GPCL nanosheets, being highly compatible with the PU matrix, bolstered the mechanical properties of the PU-GPCL nanofiber mats. Overall, graphene nanosheets increased the nanocomposites’ thermal stability, mechanical strength, and biocompatibility.
Jyoti et al. fabricated GO-CNT-hydroxyapatite (GCNT-HAP) hybrid composites for biomedical applications (Fig. 5h, i) [85]. The inclusion of GCNTs significantly improved the nanoindentation hardness and Young’s modulus of HAP composites compared to other carbon nanofillers and pristine HAP. In vitro cytotoxicity testing on MDCK cells indicated that GCNT-HAP composites with 2% GCNT filler exhibited enhanced cell viability, compatibility, and proliferation compared to other materials, suggesting their potential for implantable medical devices and tissue engineering scaffolds.
2.5 MXene and their composites
MXenes are emerging materials for biomedical applications due to their unique properties. Their 2D structure with high surface area allows for efficient drug delivery and biomolecule adsorption. MXenes possess not only excellent electrical conductivity, ideal for biosensors and bioelectrodes, but also tunable optical properties including photoluminescence and light absorption, making them suitable contrast agents for various imaging techniques [86, 87]. Their hydrophilic nature enables easy dispersion in aqueous solutions, essential for biomedical compatibility. Moreover, MXenes can be engineered to have antibacterial properties, making them promising candidates for infection-resistant coatings on medical devices and implants [88,89,90]. However, the long-term biosafety of MXenes has yet to be systematically assessed. Although several studies have demonstrated the general biocompatibility of currently available MXenes for biomedical applications, with some even showing in vivo biodegradability, most of these studies have been limited to cell experiments or short-term hematological assays [91,92,93].
Neubertova et al. functionalized Ti3C2T flakes with diethylenetriaminepentaacetic acid (DTPA) as a chelating agent and then further complexed with gadolinium (Gd3+) ions (Fig. 6a−c) [94]. This covalent functionalization process resulted in a paramagnetic response in the Ti3C2T flakes, which are intrinsically diamagnetic, rendering the flakes suitable for T1-MRI because Gd is the powerful contrast agent for this imaging modality. Additionally, this technique provided surface protection against oxidation when exposed to phosphate buffer saline and blood serum, enhancing cytocompatibility. The study showcased the high photothermal conversion efficiency of MXene-Gd composites, highlighting their potential in photothermal therapy. This research expanded the range of bioapplications for MXenes by introducing an MRI contrast agent and advancing covalent functionalization strategies for these materials.
A Schematic representation of MXene flake functionalization with DTPA and subsequent chelation with Gd3+ ions. b Cell viability, measured after the cultivation of MRC-5 cells and c the L929 cell line with different concentrations (and corresponding lateral flakes size measured by DLS) of “fresh” MXene previously stored in MXene and MXene-Gd flakes for 72 h (pristine MXene, unlike MXene-Gd, undergoes oxidation and is designated MXene (ox)). Reproduced with permission from [94], Copyright 2022, Elsevier. d Preparation of MXene/NSBS nanofibrous membranes. Biocompatibility evaluation: e fluorescence microscopy images of L929 cells on days 1, 3, and 5 for the control and MXene/NSBS sample. f Optical density values of CCK-8 assay. Reproduced with permission from [95], Copyright 2023, Elsevier. g Round membranes (Ø 5 mm) were glued onto adhesive paper and photographed in the daylight; zero corresponds to the as-spun PCL membrane, and 1, 2, 3, and 4 indicate the PCL–MX-1 to PCL–MX-4 samples, respectively. h Suggested positron interaction model with the PCL–MXene composite. i CCK-8 assay data on the proliferation of human dermal fibroblasts during the 7-day experiment. Reproduced with permission from [96], Copyright 2023, ACS
Chen et al. developed a versatile all-nanofiber sensor using MXene and modified styrene–butadiene–styrene (SBS) nanofibers (Fig. 6d−f) [95]. They functionalized SBS by introducing quaternary ammonium groups (NSBS) via thiol-ene click chemistry, improving hydrophilicity and mechanical properties. MXene nanosheets were then electrostatically adsorbed onto NSBS nanofibers. This MXene/NSBS sensor displayed a high sensitivity of 62,194 in the wide detection range of 300% and excellent stability of 3000 cycles and was applied for wireless detection of human joint motion, pulse, and electrocardiogram (ECG) signals. The MXene/NSBS electrodes also exhibited reliable temperature response and thermal management.
Diedkova et al. immobilized MXenes onto electrospun polycaprolactone (PCL) membranes (Fig. 6g−i) [96]. They utilized positron annihilation analysis and complementary techniques to study defect structure and porosity in the nanofiber scaffolds. The composite scaffolds displayed conductivity across a broad temperature range, indicating their potential as conductive biomaterials. They examined MXene’s electronic structure and layer defects, correlating these features with in vitro biological properties and bacterial adhesion tests. The results revealed that double and triple MXene coatings facilitated cell attachment and proliferation and showed mild antibacterial effects. Overall, the PCL-MXene composite exhibited distinct advantages in tissue engineering, underlining its potential as a conductive biomaterial.
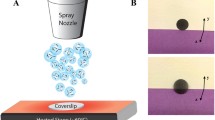
3 Deposition techniques for biomedical applications
The choice of coating techniques depends on factors, such as substrate material, intended applications, and desired coating layer thickness. The following sections offer a comprehensive overview of the diverse coating technologies employed, detailing their processes and the current research status in this field.
3.1 Chemical vapor deposition (CVD)
CVD has gained recognition as a promising technology in medical applications, particularly for enhancing medical device coatings and drug delivery systems [97,98,99]. Through the deposition of thin and uniform films onto implant surfaces, CVD improves biocompatibility and reduces the risk of rejection [100,101,102]. Additionally, CVD has been used in the development of drug delivery systems, where a thin film is deposited onto a substrate and loaded with therapeutic agents. This allows for the controlled release of medication over an extended period, enabling sustained drug delivery [103]. Over the years, CVD has been extensively employed to coat the surfaces of medical devices with diverse materials, including carbon-based materials, resulting in remarkable improvements in device performance [104,105,106]. While there are a few elements from the periodic table, such as noble gases, halogens, actinides, and alkali metals, that cannot be deposited using CVD, it remains a highly effective method for depositing multidirectional and assorted coatings [107,108,109].
Kheradmandfard et al. enhanced wear resistance of biomedical β-type titanium alloy by coating biocompatible multilayer silicon (Si)/DLC nanocomposites (Fig. 7a−c) [110]. When the coating was applied to titanium alloy surface, the wear resistance properties were improved exceptionally (6.2 × 10−10 mm3 N−1 mm−1). The wear track depth after 1 million wear cycles was only 220 nm, compared to the full coating thickness of 370 nm. Cell culture tests demonstrated that Si/DLC multilayer nanocomposite coating (MNC) samples exhibited better biocompatibility than the Ti–29Nb–13Ta‒4.6Zr (TNTZ) alloy samples. A quantitative analysis revealed that 60% of the Si/DLC MNC sample surface was covered by cells, approximately double that of the TNTZ alloy sample. In addition, no dead cells were observed in the Si/DLC MNC samples, indicating that the Si/DLC MNC samples exhibited no toxic effects against the MC3T3 cells. The findings indicate that the Si/DLC nanocomposite coating obtained through CVD significantly improved the wear resistance of the TNTZ alloy, establishing its potential as an ideal choice for biomedical applications demanding exceptional wear resistance.
A HR-TEM of the Si/DLC MNC. b Fluorescent microscopic images of live (green)/dead (red) staining of MC3T3 cells on the Si/DLC MNC on the TNTZ samples after 1 day and 4 days of culture. c MC3T3 cell proliferation on the TNTZ and Si/DLC MNC on the TNTZ samples (n = 3, **indicates p-value < 0.01). d Hardness and elastic modulus. Reproduced with permission from [110], Copyright 2022, Elsevier. e Schematic illustrations of iCVD-GNFs. f MTS assay for the iCVD-GNFs and TCP as control. g Weight loss percentage of the CVD-GNFs upon immersion in 37 °C PBS as a function of time. h FE-SEM image of hFC on the surface of the CVD-GNFs after 2 days of cell seeding. i Water uptake percentage of the CVD-GNFs versus time. Reproduced with permission from [111], Copyright 2020, Elsevier
Mansurnezhad et al. harnessed the initiated chemical vapor deposition (iCVD) technique to coat poly(ethylene glycol dimethacrylate) (pEGDMA) onto the surface of electrospun graphene nanofibers (GNFs) (Fig. 7d–f) [111]. This process resulted in the creation of an ultrathin layer, denoted as iCVD-GNFs, which established covalent bonds with gelatin chains. A comprehensive assessment of iCVD-GNF performance was undertaken, including morphological and chemical analyses that verified the existence of the ultrathin layer and its bonding to the nanofibers. In vitro biodegradability tests revealed that iCVD-GNFs maintained their morphology significantly even after 14 days of immersion and retained their structural integrity for 31 days, mitigating the typical problem of rapid dissolution in GNFs. Furthermore, cytocompatibility assessments using human fibroblast cells (hFC) in in vitro cell culture studies demonstrated that iCVD-GNFs were compatible with the cells and enhanced cell proliferation compared to a control group cultured on tissue culture plates (TCP). These results underscore the potential of iCVD-GNFs for applications in biomedicine, including tissue engineering scaffolds and wound dressings.
3.2 Plasma-enhanced chemical vapor deposition (PECVD)
PECVD, an advanced iteration of CVD, was developed to tackle the issue of elevated coating temperatures that could compromise the integrity of certain materials, rendering them unsuitable for conventional CVD processes [112,113,114]. In contrast to CVD, PECVD enables the deposition of thin films at significantly reduced temperatures, making it applicable to a broader range of materials, both organic and inorganic. This is achieved by harnessing electrical energy to create a plasma that ionizes natural gas, generating free radicals that polymerize to create the deposition layer [115, 116].
PECVD is frequently employed for coating biomedical implants, using precursor gases like silane (SiH4), methane (CH4), and phosphine (PH3) to deposit nitrogen (N)-doped hydrogenated amorphous SiC (a-SiC:H) coatings [117,118,119]. These PECVD coatings have been extensively researched and proven to be non-cytotoxic and biocompatible across various biomedical applications [120, 121]. In summary, PECVD is an effective technique for coating biomedical devices and implants, enabling improvements in their mechanical and biocompatibility properties, and holds great promise in advancing the field of biomedical materials research.
Zhang et al. introduced vertical graphene (VG) on medical-grade titanium (VG@Ti) surfaces by PECVD (Fig. 8a−c) [114]. The study conducted a comprehensive investigation into the physicochemical properties, photothermal effects, antibacterial activities, and biocompatibility of VG@Ti. The results revealed that the thickness of the VG film increased with higher reaction temperatures. Graphene films exhibited a vertical loading on medical-grade titanium, leading to improved corrosion resistance, hydrophobicity, and enhanced antibacterial performance against both Gram-positive S. aureus and Gram-negative E. coli when exposed to NIR light (808 nm at 0.8 W cm–2). Notably, under NIR light (808 nm) at 0.8 W cm–2 for 10 min. Furthermore, VG coatings on the titanium surface displayed no discernible cytotoxicity toward osteoblast cells. In vivo results confirmed the efficient antibacterial properties of VG under NIR light without any evident toxicity.
A Cross-section morphologies of VG@Ti-650 and VG@Ti-750. b Fluorescent images of live/dead cell staining of MC3T3-E1 cells cultured on various sample surfaces for 4 days. c Cell proliferation of MC3T3-E1 cells cultured on various samples. Reproduced with permission from [114], Copyright 2022, Elsevier. d Cross-sectional morphology of SiN-DLC film. e Fluorescence images of MC3T3-E1 mouse osteoblasts grown on SiN-DLC film and stained using the live/dead kit assay, showing viable (green) and dead (red) cells. f Results of cytotoxicity measurement by the enzyme-labeled method; compared to the control group: * indicates p < 0.05, ** indicates p < 0.01, and *** indicates p < 0.001. Reproduced with permission from [122], Copyright ACS, Elsevier. g PECVD system. h Effect of bare and DLC-coated SS304 samples on A172 human glioblastoma cell viability as assessed by the MTT reduction test and morphological aspect of the human glioblastoma cells grown on DLC-coated SS304. The results were calculated as percentages relative to the control (untreated cells), considering the mean and the standard error of the mean (n = 4 per group). Reproduced with permission from [123], Copyright 2019, IOP Science
Wei et al. deposited Si-incorporated diamond-like-carbon (Si-DLC) and Si/N-incorporated DLC (SiN-DLC) as a protective film for Ti6Al4V artificial implants via PECVD method (Fig. 8d−f) [122]. The study found that the as-deposited DLC film had a thickness of approximately 2 µm, and the SiN-DLC film exhibited the lowest surface roughness Ra (53.0 ± 3.6 nm) compared to Ti6Al4V and DLC films. SiN-DLC showed superior mechanical properties to Ti6Al4V, especially in terms of resistance to plastic deformation. It also displayed excellent adhesive strength(> 13 N) with Ti6Al4V, a critical requirement for use in liquid environments. In both simulated body fluid (SBF) and SBF containing bovine serum albumin (BSA), the SiN-DLC film exhibited significantly lower friction coefficients and wear rates compared to Ti6Al4V, demonstrating superior tribological properties (0.072 and 1.82 (× 10–7) mm3 N–1 m–1, respectively). Moreover, Si-DLC and SiN-DLC films possessed similar corrosion resistance but surpassing Ti6Al4V. The cytotoxicity tests revealed that the SiN-DLC film notably enhanced cell viability and promoted cell proliferation to a certain extent.
Oliveira et al. deposited a DLC film with 20% hydrogen and 80% carbon onto 304 stainless steel (SS304) surface using PECVD technique (Fig. 8g, h) [123]. Tribocorrosion tests were performed after immersion in SBF, demonstrating that the DLC film reduced SS304 corrosion susceptibility by 59-fold compared to the untreated surface, enhancing corrosion protection. Evaluations with A172 glial cells indicated that the DLC film did not exhibit genotoxicity or cytotoxicity. Moreover, A172 cells exposed to DLC-coated SS304 for 24 h did not show any cytotoxicity or genotoxicity compared to untreated cells. These findings shed light on the tribocorrosion behavior of the DLC film, encompassing wear rate, friction coefficient, and corrosion resistance in SBF, offering insights for the development of advanced DLC-coated implants in biomedical applications.
3.3 Ion-beam (IB)
The use of ion-beam (IB) deposition has arisen as a promising technology for improving biomedical coatings, primarily by enhancing surface selectivity and biocompatibility through precise surface modifications [124,125,126]. This growing interest in IB is driven by several key factors. Firstly, it addresses shortcomings in metallic orthopedic grafts used in the replacement of long bones and cartilage, such as high friction resistance and limited biocompatibility [127,128,129]. Secondly, as biomaterials expand beyond traditional metals, ceramics, and polymers to biological materials [36, 130, 131], IB offers a means to modify their properties effectively [132]. Lastly, IB in conjunction with plasma treatment enhances biomaterials by providing superior surface selectivity compared to conventional simple etching processes [133,134,135]. In summary, IB deposition is a powerful technique for creating biomedical coatings, offering substantial potential for advancing biomedical materials research.
Liu et al. employed a one-step IB method to create a highly biocompatible micropatterned surface on diamond-like carbon (DLC) to enhance surface properties at the nanoscale level (Fig. 9a−c) [136]. Increasing the dose of IB irradiation raised the sp3 C − N content on the DLC surface, positively impacting biocompatibility. The adhesion of MC3T3 osteoblasts increased from 32 to 86% at an irradiation dose of 8 × 1015 ions cm−2. However, the micropattern hindered osteoblast adhesion by physically constraining cell expansion and extension. The micropattern with a depth of 37 nm exhibited favorable friction properties, reducing the coefficient of friction by 21% at higher speeds. These findings underscore IB irradiation’s effectiveness in enhancing biotribological properties and biocompatibility of DLC coatings, making them more suitable for various biomedical applications, including orthopedic implants, cardiovascular devices, and dental materials. Penkov et al. utilized IB irradiation to enhance the biocompatibility of DLC-based nanocomposite coatings (Fig. 9d−f) [137]. Optimal irradiation conditions were determined through molecular dynamics simulations, and subsequent experiments validated these conditions, establishing a correlation between surface modifications and biomedical properties. The irradiation process resulted in the creation of a surface layer with low density and reduced DLC sp3 content, with these structural and chemical changes being largely independent of the initial sp3 content and irradiation energy. Importantly, IB irradiation significantly improved the biocompatibility of DLC-based nanocomposite coatings. When irradiated with 1 keV He ions at a dose of 4.2 × 1015 ions cm−2, the adhesion of MG63 cells increased dramatically from 10 to approximately 100%.
A Schematic illustration of the IB irradiation process. b Nanoindentation load displacement and c hardness and modulus for the DLC coatings under negative bias voltage of 0, –20, –40, –60, and –80 V, respectively. c Surface topographies of as-coated DLC and DLC coating after irradiation by N ions under irradiation dose of 2 × 1015, 4 × 1015, and 8 × 1015 ions/cm2. e Optical images of the MC3T3 cells on the IB-irradiated DLC under ion doses of 2 × 1015, 4 × 1015, and 8 × 1015 ions/cm2 and as-coated DLC. f Cell coverage for as-coated DLC, patterned DLC, and irradiated DLC as a function of irradiation dose. Reproduced with permission from [136], Copyright 2022, Springer. d Changes in diamond structure under irradiation at 1 keV with neutral He after different irradiation doses (side view). Red arrows indicate the initial direction of ions, and sp3 bonds are shown in red, and sp2 bonds in blue. e Si/DLC coating irradiated by 1 keV He ions at a dose of 4.2 × 1015 ions/cm2. f Cell coverage as a function of irradiation dose for 1 keV He ions. Reproduced with permission from [137], Copyright 2019, Elsevier
4 Industrial trend of carbon-based materials for biomedical applications
In the academic and industrial arenas, the increasing prominence of carbon-based composites in biomedical applications is indisputable. In recent years, there has been a promising industrial trend toward utilizing carbon-based composites in biomedical applications, aligning with the goal of advancing safer and more effective medical treatments and devices. The regulatory pathway for medical devices is a meticulous and varied process influenced by product characteristics and regulatory frameworks. This sequence outlines the progression from initial classification and preclinical testing to clinical trials, regulatory submissions, and post-market surveillance, ensuring that medical devices meet stringent standards for safety and efficacy. Particularly in the context of the USA and the US Food and Drug Administration (FDA), the process begins with classifying the medical device based on its intended use, potential risks, and indications for use, followed by preclinical testing. Subsequently, an Investigational Device Exemption (IDE) application is submitted for FDA permission to conduct clinical trials. The clinical trials progressively assess the safety and effectiveness of the medical device in human subjects. The premarket submission, incorporating data from preclinical testing and clinical trials, along with details regarding the device’s design and manufacturing, is then submitted to the FDA for regulatory review. After the FDA’s decision, post-market surveillance then ensures continuous monitoring of device performance, with ongoing data continuous monitoring of device performance, with ongoing data related to adverse events, malfunctions, and long-term outcomes, contributing to the ongoing evaluation and enhancement of the device’s overall reliability and safety profile [138]. This section provides several instances of commercial products incorporating carbon-based materials in various biomedical domains.
CarboFix Orthopedics Ltd., an industry trailblazer, has effectively brought carbon fiber-reinforced polymers to the market for use in orthopedic implants and devices [139]. These implants utilize continuous carbon fibers, arranged both in a unidirectional, longitudinal orientation and helical/diagonal configurations. Notably, the composite material closely approximates the modulus of elasticity of cortical bone, potentially expediting fracture healing and reducing the risk of stress risers and secondary fractures. Moreover, CarboFix implants offer the unique advantage of radiolucency, enhancing their utility during surgical procedures and follow-up assessments. This exceptional composite material allows for MRI and CT scans with minimal to no artifacts, improving soft tissue visualization and facilitating radiation therapy with minimal backscatter. CarboFix nails and plates also exhibit outstanding fatigue resistance, providing vital support to patients with delayed union and those undergoing oncological treatment. The CarboFix implants portfolio encompasses a diverse range of options, including intramedullary nails for the humerus, tibia, and femur, an ankle arthrodesis nail, and plates designed for the distal femur, proximal tibia, distal radius, proximal humerus, distal fibula, among other configurations (Fig. 10a).
The contemporary industrial focus on the advancement of carbon-based materials and their applications in the biomedical domain. a The CarboFix implants portfolio (CarboFix Orthopedics Ltd.). b Biopsy site identification and fiducial markers tailored for radiation therapy treatment (Carbon Medical Technologies Inc.). c Commercial product of carbon fibers wound dressings (Bio-medical Carbon Technology Ltd.). d Dental CNT X-ray Tube (Vatech Inc.). e Graphene-based neural probes and head stages for bio-signal amplification and acquisition systems (Guger technology medical engineering GmbH). Reproduced with permission from [139,140,141,142,143]
Carbon Medical Technologies Inc. has made significant contributions in academia and the professional sphere through its pioneering pyrolytic carbon-coating technology [140]. This innovation has resulted in various biomedical products, including injectable bulking agents, implantable tissue markers for biopsy site identification, and fiducial markers for radiation therapy treatment, as shown in Fig. 10b. Notably, Durasphere, one of their products, showcases the practical application of this technology. Durasphere is an injectable bulking agent containing pyrolytic carbon-coated graphite beads suspended in a water-based carrier gel with beta-glucan. It is used for conditions such as stress urinary incontinence, fecal incontinence, gastroesophageal reflux, and vesicoureteral reflux. Durasphere is highly biocompatible and can be administered in a simple office-based procedure, typically taking less than 30 min. These innovations illustrate the synergy between advanced technology and clinical practice, advancing the field of biomedical materials.
Bio-medical Carbon Technology Ltd. specializes in advanced wound care solutions, particularly carbon fiber wound dressings [141]. Notably, their recent innovation, KoCarbon®, represents a new generation of activated carbon fiber dressings, validated through clinical trials for their remarkable ability to absorb bacteria and endotoxins (Fig. 10c). The KoCarbon® Medical Bandage™, a product designed for post-surgical wounds, exhibits a sophisticated three-layer structure. The first layer, composed of PET non-woven fabric, serves as a porous medium, facilitating the exchange of air between the wound and the external environment. The second layer features carbon fiber fabric, functioning as an absorption layer capable of swiftly absorbing blood exudate and bacteria from the wound, thereby mitigating wound odors and creating an antimicrobial environment. The third layer consists of a PE that prevents wound adhesion and secondary injuries. Incorporating carbon fiber into wound dressings advances wound care technology, enhancing healing and infection control and reducing post-surgical complications. These innovations exemplify the synergy between materials science and healthcare, leading to improved patient outcomes and advancements in wound care.
Vatech Inc. has pioneered the integration of CNT technology into a dental digital X-ray generator for dental imaging sectors [142]. Traditionally, the X-ray market has relied on analog thermoelectric tubes made of metals. The conventional method involves applying high voltage exceeding 2300° to a metal wire filament, requiring a warm-up period and emitting radiation, leading to pre-image radiation exposure for patients and medical personnel. In contrast, CNT X-ray tubes, functioning as generators, are a paradigm shift with reduced dimensions and weight compared to analog counterparts using filaments. This characteristic facilitates their incorporation into ultra-lightweight X-ray equipment, thereby enabling the acquisition of high-resolution images. Notably, the X-ray dose is digitally adjustable down to microseconds, offering precise control and mitigating radiation exposure to the human body. The EzRay Air series, featuring CNT X-ray tubes (Fig. 10d), stands out by instantly managing X-rays through digital electrical signals, eliminating the need for unwarranted exposure during the X-ray preparation phase, and ensuring an efficient and streamlined imaging process. In addition to operational efficiency, the EzRay Air series delivers high-quality images. Its design enables miniaturization and weight reduction, making it more compact and lighter than conventional market products. This technological leap forward in dental radiography aligns with contemporary standards of precision, safety, and efficiency.
G.tec medical engineering GmbH leads in brain-computer interface (BCI) and bio-signal processing technologies, distinguished by its utilization of graphene transistors (Fig. 10e) [143]. Their offerings include bio-signal amplifiers, invasive/non-invasive stimulators, wearable Electroencephalogram (EEG) headsets, and Conformité Européenne (CE)-certified, FDA-cleared user-ready applications. Applied in hospital and rehabilitation settings, these applications aid in stroke rehabilitation, neurological assessment, communication facilitation for coma/locked-in patients, and pre- and intraoperative brain mapping in neurosurgical procedures. Their advancements encompass graphene-based neural probes and headstages designed for comprehensive amplification, recording, and analysis within living organisms or cellular environments. Ongoing research explores enhancing electrical stimulation to neuronal circuits using graphene, particularly for conditions like blindness or Parkinson’s disease.
5 Summary and future directions
Carbon-based materials and their composites hold remarkable promise across various biomedical domains, owing to their exceptional attributes. These include substantial specific surface areas, high hydrophilicity, adaptable layer thickness, modifiable structures, and a diverse range of compositions. Notably, carbon-based materials, such as graphene quantum dots, exhibit an impressive level of biocompatibility, minimizing undesirable reactions when interfacing with biological systems. Their noteworthy surface area-to-volume ratio facilitates efficient drug delivery, thus amplifying therapeutic effectiveness. Furthermore, the exceptional electrical conductivity inherent to carbon materials empowers the development of bioelectrodes and biosensors, enabling precise monitoring of physiological parameters. Additionally, the tunable mechanical properties of carbon-based materials render them highly suitable for an array of applications, including implants, artificial joints, bone engineering, and scaffold reinforcement.
Notwithstanding the advantages, it is crucial to recognize that the adoption of carbon materials in biomedical applications necessitates comprehensive long-term stability studies to ensure their reliability and safety—substantial research has been conducted but this field is still in its early stages. Looking ahead for these carbon-based materials and coating techniques in biomedical applications, the future direction encompasses a multifaceted approach. It begins with the imperative of conducting comprehensive, long-term, in vivo safety assessments to ensure the sustained well-being of patients. Simultaneously, the focus extends to innovation, with a goal to develop multifunctional materials, such as hybrid metal/polymer/ceramic nanocomposites, that transcend conventional roles and offer versatile solutions in diagnostics and therapeutics. In this context, a meticulous understanding of surface properties through detailed characterization is emphasized, aiming to tailor materials for specific biomedical applications, optimize performance, and predict biological responses accurately. Also, establishing industry standards emerges as a pivotal step, involving the definition and implementation of guidelines governing manufacturing processes, quality control, and safety protocols. Collectively, this comprehensive strategy seeks to advance the field, ensuring the responsible and effective utilization of carbon-based materials in the evolving landscape of biomedical science.
-
1.
Comprehensive long-term stability studies are urgently needed for emerging carbon-based materials. For instance, MXenes, which have garnered substantial attention for potential biomedical applications, exhibit initial signs of low toxicity. However, a systematic exploration of their toxicity, environmental impact, and effects on human health is lacking, leaving the underlying mechanisms unclear. To fully harness the potential of MXenes in biomedicine, addressing these challenges through further research is imperative.
-
2.
Although extensive research has probed the safety of carbon-based materials, it is essential to acknowledge that many biocompatibility studies have relatively short durations compared to human lifespans. To obtain a comprehensive understanding of long-term effects, in-depth and extended studies focusing on biocompatibility and toxicity are imperative for accurately evaluating the safety and potential risks associated with the biomedical use of carbon-based materials. From these, a robust assessment of long-term biocompatibility and toxicity profiles can be achieved, offering vital insights for the development of safe and effective biomedical materials and devices.
-
3.
The characterization and comprehension of surface properties in carbon-based materials remain domains necessitating extensive investigation. Specifically, there is a pressing requirement for a systematic exploration of how surface properties influence the stability of carbon-based materials in aqueous solutions and comprehensive studies on surface modification techniques. These inquiries are pivotal in facilitating the expansion of carbon-based materials’ applications by providing heightened control over their surface attributes. Notably, within the context of medical markers, proficient surface engineering holds the potential to significantly enhance their performance.
-
4.
Securing the effective functionality and stability of biomedical coatings mandates a thorough and prolonged biotribological evaluation. The substantial threat posed to the performance of coatings by wear and degradation, exacerbated by the absence of replenishment mechanisms, has constrained the range of applicable coatings. To address this challenge, the application of accelerated wear testing methods facilitates the simulation of extended usage within a condensed timeframe. Researchers employ multi-modal characterization techniques for a thorough assessment of coating surfaces over time, alongside long-term in vivo studies that allow the observation of materials’ performance within living organisms. Integration of smart sensors facilitates continuous monitoring of factors like friction and wear. Furthermore, real-time insights into the wear and degradation of biomedical coatings are gained through continuous monitoring and data collection systems. This multifaceted approach contributes to a nuanced understanding of the long-term behavior and performance of biomedical materials.
-
5.
The establishment of carbon-based materials for biomedical applications relevant to clinical and industry standards emerges as a pivotal imperative. The significance of this endeavor lies in its capacity to ensure consistency, safety, and efficacy across diverse applications. Standardization not only fosters regulatory compliance but also engenders a framework for rigorous evaluation, comparability, and interoperability within the realm of biomedical technologies. By delineating clear and comprehensive standards, the biomedical community can navigate the challenges associated with the integration of carbon-based materials, fostering advancements that are not only scientifically robust but also ethically and clinically sound. Standardization efforts are poised to facilitate the seamless translation of research innovations into clinical practice, thereby promoting the reliability and reproducibility of outcomes in the biomedical applications.
This review offers a comprehensive exploration of carbon materials, emphasizing their growing significance in biomedicine and innovative deposition techniques to attain specific properties. Additionally, we scrutinized various products employing carbon-based composites. While the widespread adoption of carbon materials in biomedical applications is still in its early commercial stages, noteworthy successes have been witnessed in products like carbon fiber wound dressings. Therefore, a profound understanding of the unique properties of diverse carbon materials and their strategic integration within the biomedical sector holds the potential to unlock further advancements in tailored biomedical solutions. These attributes underscore the diverse advantages of carbon materials in advancing biomedical technologies.
Data availability
All data included in this study are available from the corresponding author (Soo-Jin Park), upon reasonable request.
References
Woltman SJ, Jay GD, Crawford GP (2007) Liquid-crystal materials find a new order in biomedical applications. Nat Mater 6(12):929–938. https://doi.org/10.1038/nmat2010
Delplace V, Nicolas J (2015) Degradable vinyl polymers for biomedical applications. Nat Chem 7(10):771–784. https://doi.org/10.1038/Nchem.2343
Cha CY, Shin SR, Annabi N, Dokmeci MR, Khademhosseini A (2013) Carbon-based nanomaterials: multifunctional materials for biomedical engineering. ACS Nano 7(4):2891–2897. https://doi.org/10.1021/nn401196a
Molaei MJ (2019) Carbon quantum dots and their biomedical and therapeutic applications: a review. RSC Adv 9(12):6460–6481. https://doi.org/10.1039/c8ra08088g
Zhao DL, Chung TS (2018) Applications of carbon quantum dots (CQDs) in membrane technologies: a review. Water Res 147:43–49. https://doi.org/10.1016/j.watres.2018.09.040
Zhang LY, Yin LW, Wang CX, Lun N, Qi YX, Xiang D (2010) Origin of Visible Photoluminescence Of ZnO quantum dots: defect-dependent and size-dependent. J Phys Chem C 114(21):9651–9658. https://doi.org/10.1021/jp101324a
Han M, Zhu SJ, Lu SY, Song YB, Feng TL, Tao SY et al (2018) Recent progress on the photocatalysis of carbon dots: classification, mechanism and applications. Nano Today 19:201–218. https://doi.org/10.1016/j.nantod.2018.02.008
Das R, Bandyopadhyay R, Pramanik P (2018) Carbon quantum dots from natural resource: a review. Mater Today Chem 8:96–109. https://doi.org/10.1016/j.mtchem.2018.03.003
Wang R, Lu KQ, Tang ZR, Xu YJ (2017) Recent progress in carbon quantum dots: synthesis, properties and applications in photocatalysis. J Mater Chem A 5(8):3717–3734. https://doi.org/10.1039/c6ta08660h
Lim SY, Shen W, Gao ZQ (2015) Carbon quantum dots and their applications. Chem Soc Rev 44(1):362–381. https://doi.org/10.1039/c4cs00269e
Liang C, Diao S, Wang C, Gong H, Liu T, Hong G et al (2014) Tumor metastasis inhibition by imaging-guided photothermal therapy with single-walled carbon nanotubes. Adv Mater 26(32):5646–5652
Huang YY, Terentjev EM (2012) Dispersion of carbon nanotubes: mixing, sonication, stabilization, and composite properties. Polymers 4(1):275–295
Fujigaya T, Nakashima N (2015) Non-covalent polymer wrapping of carbon nanotubes and the role of wrapped polymers as functional dispersants. Sci Technol Adv Mater 16(2):024802
Antonucci A, Reggente M, Roullier C, Gillen AJ, Schuergers N, Zubkovs V et al (2022) Carbon nanotube uptake in cyanobacteria for near-infrared imaging and enhanced bioelectricity generation in living photovoltaics. Nat Nanotechnol 17(10):1111–1119
Negri V, Pacheco‑Torres J, Calle D, López‑Larrubia P (2020) Carbon nanotubes in biomedicine. Surf-Modified Nanobiomater Electrochem Biomed Appl 177–217
Lee J-H, Kim Y-S, Ru H-J, Lee S-Y, Park S-J (2022) Highly flexible fabrics/epoxy composites with hybrid carbon nanofillers for absorption-dominated electromagnetic interference shielding. Nano-Micro Lett 14(1):188
Heo Y-J, Lee J-H, Kim S-H, Mun S-J, Lee S-Y, Park S-J (2022) Derived millimeter-thick yarn supercapacitors enabling high volumetric energy density. ACS Appl Mater Interfaces 14(37):42671–42682
Jeong WY, Choi HE, Kim KS (2022) Graphene-based nanomaterials as drug delivery carriers. Multifaceted Biomed Appl Graphene 109–124
Lee J-H, Yang G, Kim C-H, Mahajan RL, Lee S-Y, Park S-J (2022) Flexible solid-state hybrid supercapacitors for the internet of everything (IoE). Energy Environ Sci 15(6):2233–2258
Mostafavi E, Iravani S (2022) Mxene-graphene composites: a perspective on biomedical potentials. Nano-Micro Lett 14(1):130
Iravani S, Varma RS (2020) Green synthesis, biomedical and biotechnological applications of carbon and graphene quantum dots. A review. Environ Chem Lett 18:703–727
Wilk S, Medina-Cruz D, Zambrzycki M, Szewczyk PK, Nocuń M, Menaszek E et al (2023) The addition of carbon nanotubes modifies the biological, physicochemical, and electrical properties of carbon nanofiber composites. Chem Eng J 455:140617
Feng C, Cen J, Wu T, Hou T, Chen K, Li X et al (2022) Preparation and properties of the poly (ether ether ketone)(PEEK)/nano-zinc oxide (ZnO)–short carbon fiber (SCF) artificial joint composites. ACS Appl Polym Mater 4(12):8869–8877
Paz-González JA, Velasco-Santos C, Villarreal-Gómez LJ, Alcudia-Zacarias E, Olivas-Sarabia A, Cota-Leal MA et al (2023) Structural composite based on 3D printing polylactic acid/carbon fiber laminates (PLA/CFRC) as an alternative material for femoral stem prosthesis. J Mech Behav Biomed Mater 138:105632
Sun L, Zhang L, Wang J, Liu Y, Guo Y (2023) Fabrication of novel multilayer core-shell structured nanofibers network reinforced carbon matrix composites for bone tissue engineering. Mater Lett 333:133634
Nandeshwar R, Illa MP, Khandelwal M, Tallur S (2022) Enzymatic degradation of bacterial cellulose derived carbon nanofibers (BC-CNF) by myeloperoxidase (MPO): performance evaluation for biosensing. Biosens Bioelectron: X 12:100252
Zheng H, Han X, Wei Q, Liu X, Li Y, Zhou J (2022) A green flexible and wearable biosensor based on carbon nanofibers for sensitive detection of uric acid in artificial urine. J Mater Chem B 10(41):8450–8461
Miao Z, Song Y, Dong Y, Ge D, Shui J, He X et al (2023) Intrinsic conductive cellulose nanofiber induce room-temperature reversible and robust polyvinyl alcohol hydrogel for multifunctional self-healable biosensors. Nano Res 16(2):3156–3167
Gogotsi Y, Anasori B (2019) The rise of MXenes. Acs Nano 13(8):8491–8494. https://doi.org/10.1021/acsnano.9b06394
Anasori B, Lukatskaya MR, Gogotsi Y (2017) 2D metal carbides and nitrides (MXenes) for energy storage. Nat Rev Mater 2(2):16098. https://doi.org/10.1038/natrevmats.2016.98
Mohammadi AV, Rosen J, Gogotsi Y (2021) The world of two-dimensional carbides and nitrides (MXenes). Science 372(6547):1165-abf1581. https://doi.org/10.1126/science.abf1581
Rasool K, Helal M, Ali A, Ren CE, Gogotsi Y, Mahmoud KA (2016) Antibacterial activity of Ti3C2Tx MXene. ACS Nano 10(3):3674–3684. https://doi.org/10.1021/acsnano.6b00181
Huang K, Li ZJ, Lin J, Han G, Huang P (2018) Two-dimensional transition metal carbides and nitrides (MXenes) for biomedical applications (vol 47, pg 5109, 2018). Chem Soc Rev 47(17):6889–6889. https://doi.org/10.1039/c8cs90090f
Huang HY, Jiang RM, Feng YL, Ouyang H, Zhou NG, Zhang XY et al (2020) Recent development and prospects of surface modification and biomedical applications of MXenes. Nanoscale 12(3):1325–1338. https://doi.org/10.1039/c9nr07616f
Egbedina AO, Bolade OP, Ewuzie U, Lima EC (2022) Emerging trends in the application of carbon-based materials: a review. J Environ Chem Eng 10(2):107260
Islam M, Lantada AD, Mager D, Korvink JG (2022) Carbon-based materials for articular tissue engineering: from innovative scaffolding materials toward engineered living carbon. Adv Healthcare Mater 11(1):2101834
Liu J, Chen C, Zhao Y (2019) Progress and prospects of graphdiyne-based materials in biomedical applications. Adv Mater 31(42):1804386
Abubakre OK, Medupin RO, Akintunde IB, Jimoh OT, Abdulkareem AS, Muriana RA, et al (2023) Carbon nanotube-reinforced polymer nanocomposites for sustainable biomedical applications: a review. J Sci: Adv Mater Devices 8(2):100557
Rivers TJ, Hudson TW, Schmidt CE (2002) Synthesis of a novel, biodegradable electrically conducting polymer for biomedical applications. Adv Func Mater 12(1):33–37. https://doi.org/10.1002/1616-3028(20020101)12:1%3c33::Aid-Adfm33%3e3.0.Co;2-E
Makvandi P, Wang CY, Zare EN, Borzacchiello A, Niu LN, Tay FR (2020) Metal-based nanomaterials in biomedical applications: antimicrobial activity and cytotoxicity aspects. Adv Funct Mater 30(22):1910021. https://doi.org/10.1002/adfm.201910021
Monge C, Almodovar J, Boudou T, Picart C (2015) Spatio-temporal control of LbL films for biomedical applications: from 2D to 3D. Adv Healthcare Mater 4(6):811–830. https://doi.org/10.1002/adhm.201400715
Lin X, Wang JL, Wu XY, Luo Y, Wang YA, Zhao YJ (2023) Marine-derived hydrogels for biomedical applications. Adv Funct Mater 33(6):2211323. https://doi.org/10.1002/adfm.202211323
Bennett AC, Bennett CL, Witherspoon BJ, Knopf KB (2019) An evaluation of reports of ciprofloxacin, levofloxacin, and moxifloxacin-association neuropsychiatric toxicities, long-term disability, and aortic aneurysms/dissections disseminated by the Food and Drug Administration and the European Medicines Agency. Expert Opin Drug Saf 18(11):1055–1063
Gazzi A, Fusco L, Orecchioni M, Ferrari S, Franzoni G, Yan JS et al (2020) Graphene, other carbon nanomaterials and the immune system: toward nanoimmunity-by-design. J Phys: Mater 3(3):034009
Sharma P, Jain V, Tailang M (2023) Advancement of nanocarrier-based engineering for specific drug delivery for cancer therapy. In Target Cancer Ther Biomed Eng 465–486 Springer
Ding X, Pu Y, Tang M, Zhang T (2023) Pulmonary hazard identifications of Graphene family nanomaterials: adverse outcome pathways framework based on toxicity mechanisms. Sci Total Environ 857:159329
Willenborg S, Sanin DE, Jais A, Ding X, Ulas T, Nüchel J et al (2021) Mitochondrial metabolism coordinates stage-specific repair processes in macrophages during wound healing. Cell Metabol 33(12):2398-2414. e2399
de Luna LAV, Loret T, Fordham A, Arshad A, Drummond M, Dodd A et al (2022) Lung recovery from DNA damage induced by graphene oxide is dependent on size, dose and inflammation profile. Part Fibre Toxicol 19(1):1–21
Xiao Y, Pang YX, Yan Y, Qian P, Zhao H, Manickam S et al (2023) Synthesis and functionalization of graphene materials for biomedical applications: recent advances, challenges, and perspectives. Adv Sci 10(9):2205292
Liao G, He F, Li Q, Zhong L, Zhao R, Che H et al (2020) Emerging graphitic carbon nitride-based materials for biomedical applications. Prog Mater Sci 112:100666
Su W, Wu H, Xu H, Zhang Y, Li Y, Li X et al (2020) Carbon dots: a booming material for biomedical applications. Mater Chem Front 4(3):821–836
Tan J, Zou R, Zhang J, Li W, Zhang LQ, Yue DM (2016) Large-scale synthesis of N-doped carbon quantum dots and their phosphorescence properties in a polyurethane matrix. Nanoscale 8(8):4742–4747. https://doi.org/10.1039/c5nr08516k
Kasinathan K, Samayanan S, Marimuthu K, Yim JH (2022) Green synthesis of multicolour fluorescence carbon quantum dots from sugarcane waste: investigation of mercury (II) ion sensing, and bio-imaging applications. Appl Surf Sci 601:154266. https://doi.org/10.1016/j.apsusc.2022.154266
Nekoueian K, Amiri M, Sillanpaa M, Marken F, Boukherroub R, Szunerits S (2019) Carbon-based quantum particles: an electroanalytical and biomedical perspective. Chem Soc Rev 48(15):4281–4316. https://doi.org/10.1039/c8cs00445e
Gidwani B, Sahu V, Shukla SS, Pandey R, Joshi V, Jain VK et al (2021) Quantum dots: prospectives, toxicity, advances and applications. J Drug Deliv Sci Technol 61:102308. https://doi.org/10.1016/j.jddst.2020.102308
Tian LB, Guo HZ, Bai YF, Zhong YT, Zhou SF, Chen LC (2022) One-pot preparation of biocompatible folate-functionalized graphitic carbon nitride quantum dots for targeted bioimaging. Chem Eng J 446:136932. https://doi.org/10.1016/j.cej.2022.136932
Wang LF, Li XH, Jin Y, Liu GQ, Shan Y (2023) Integrating photoluminescence and ferromagnetism in carbon quantum Dot/ZnO by interfacial orbital hybridization for multifunctional bioprobes. ChemPhysChem. https://doi.org/10.1002/cphc.202200766
Pirlot C, Willems I, Fonseca A, Nagy JB, Delhalle J (2002) Preparation and characterization of carbon nanotube/polyacrylonitrile composites. Adv Eng Mater 4(3):109–114. https://doi.org/10.1002/1527-2648(200203)4:3%3c109::Aid-Adem109%3e3.0.Co;2-5
Fan HJ, Knez M, Scholz R, Nielsch K, Pippel E, Hesse D et al (2006) Monocrystalline spinel nanotube fabrication based on the Kirkendall effect. Nat Mater 5(8):627–631. https://doi.org/10.1038/nmat1673
Sathish T, Saravanan R, Vijayan V, Kumar SD (2022) Investigations on influences of MWCNT composite membranes in oil refineries waste water treatment with Taguchi route. Chemosphere 298:134265. https://doi.org/10.1016/j.chemosphere.2022.134265
Park SY, Kang JH, Kim HS, Hwang JY, Shin US (2022) Electrical and thermal stimulus-responsive nanocarbon-based 3D hydrogel sponge for switchable drug delivery. Nanoscale. https://doi.org/10.1039/d1nr06074k
Dalili F, Aghdam RM, Soltani R, Saremi M (2022) Corrosion, mechanical and bioactivity properties of HA-CNT nanocomposite coating on anodized Ti6Al4V alloy. J Mater Sci-Mater Med 33(4):34. https://doi.org/10.1007/s10856-022-06655-6
Jha R, Singh A, Sharma PK, Fuloria NK (2020) Smart carbon nanotubes for drug delivery system: a comprehensive study. J Drug Deliv Sci Technol 58:101811. https://doi.org/10.1016/j.jddst.2020.101811
Zadeh ZE, Solouk A, Shafieian M, Nazarpak MH (2021) Electrospun polyurethane/carbon nanotube composites with different amounts of carbon nanotubes and almost the same fiber diameter for biomedical applications. Mater Sci Eng: C 118:111403
Suo L, Wu H, Wang P, Xue Z, Gao J, Shen J (2023) The improvement of periodontal tissue regeneration using a 3D-printed carbon nanotube/chitosan/sodium alginate composite scaffold. J Biomed Mater Res B Appl Biomater 111(1):73–84
Asl MA, Karbasi S, Beigi-Boroujeni S, Benisi SZ, Saeed M (2022) Polyhydroxybutyrate-starch/carbon nanotube electrospun nanocomposite: a highly potential scaffold for bone tissue engineering applications. Int J Biol Macromol 223:524–542
De Jong KP, Geus JW (2000) Carbon nanofibers: catalytic synthesis and applications. Catal Rev-Sci Eng 42(4):481–510. https://doi.org/10.1081/Cr-100101954
Ci LJ, Li YH, Wei BQ, Liang J, Xu CL, Wu DH (2000) Preparation of carbon nanofibers by the floating catalyst method. Carbon 38(14):1933–1937. https://doi.org/10.1016/S0008-6223(00)00030-0
Yue LC, Zhao HT, Wu ZG, Liang J, Lu SY, Chen G et al (2020) Recent advances in electrospun one-dimensional carbon nanofiber structures/heterostructures as anode materials for sodium ion batteries. J Mater Chem A 8(23):11493–11510. https://doi.org/10.1039/d0ta03963b
Abdo GG, Zagho MM, Al Moustafa AE, Khalil A, Elzatahry AA (2021) A comprehensive review summarizing the recent biomedical applications of functionalized carbon nanofibers. J Biomed Mater Res B-Appl Biomater 109(11):1893–1908. https://doi.org/10.1002/jbm.b.34828
Balasubramaniam B, Kumar SA, Singh KA, Bhunia S, Verma K, Tian LM et al (2022) Electrically conductive MoS2 reinforced polyacrylonitrile nanofibers for biomedical applications. Adv Nanobiomed Res 2(4):2100105. https://doi.org/10.1002/anbr.202100105
Choi S, Raja IS, Selvaraj AR, Kang MS, Park TE, Kim KS et al (2023) Activated carbon nanofiber nanoparticles incorporated electrospun polycaprolactone scaffolds to promote fibroblast behaviors for application to skin tissue engineering. Adv Compos Hybrid Mater 6(1):24. https://doi.org/10.1007/s42114-022-00608-x
Rana SMS, Salauddin M, Sharifuzzaman M, Lee SH, Shin YD, Song H et al (2022) Ultrahigh-output triboelectric and electromagnetic hybrid generator for self-powered smart electronics and biomedical applications. Adv Energy Mater 12(40):2202238. https://doi.org/10.1002/aenm.202202238
Jiang JW, Wang JS, Li BW (2009) Young’s modulus of graphene: a molecular dynamics study. Phys Rev B 80(11):113405. https://doi.org/10.1103/PhysRevB.80.113405
Zhou M, Liu Z, Ming WM, Wang ZF, Liu F (2014) sd(2) graphene: kagome band in a hexagonal lattice. Phys Rev Lett 113(23):236802. https://doi.org/10.1103/PhysRevLett.113.236802
Yin SY, Goldovsky Y, Herzberg M, Liu L, Sun H, Zhang YY et al (2013) Functional free-standing graphene honeycomb films. Adv Func Mater 23(23):2972–2978. https://doi.org/10.1002/adfm.201203491
Daneshmandi L, Barajaa M, Tahmasbi Rad A, Sydlik SA, Laurencin CT (2021) Graphene-based biomaterials for bone regenerative engineering: a comprehensive review of the field and considerations regarding biocompatibility and biodegradation. Adv Healthcare Mater 10(1):2001414
Pinto AM, Goncalves IC, Magalhaes FD (2013) Graphene-based materials biocompatibility: a review. Colloids Surf B-Biointerfaces 111:188–202. https://doi.org/10.1016/j.colsurfb.2013.05.022
Lin L, Peng HL, Liu ZF (2019) Synthesis challenges for graphene industry. Nat Mater 18(6):520–524. https://doi.org/10.1038/s41563-019-0341-4
Park D, Kim JH, Kim HJ, Lee D, Lee DS, Yoon DS et al (2020) Multiplexed femtomolar detection of Alzheimer’s disease biomarkers in biofluids using a reduced graphene oxide field-effect transistor. Biosens Bioelectron 167:112505. https://doi.org/10.1016/j.bios.2020.112505
Li Y, Jia H, Cui X, Qin W, Qin S, Wu Y et al (2022) Bending properties, compression properties, biocompatibility and bioactivity of sulfonated carbon fibers/PEEK composites with graphene oxide coating. Appl Surf Sci 575:151774
Joy A, Unnikrishnan G, Megha M, Haris M, Thomas J, Kolanthai E et al (2022) Design of biocompatible polycaprolactone-based nanocomposite loaded with graphene oxide/strontium nanohybrid for biomedical applications. Appl Nanosci. https://doi.org/10.1007/s13204-022-02721-1
Garren M, Ashcraft M, Crowley D, Brisbois EJ, Handa H (2023) Derivatization of graphene oxide nanosheets with tunable nitric oxide release for antibacterial biomaterials. J Biomed Mater Res A 111(4):451–464. https://doi.org/10.1002/jbm.a.37493
Razzaghi D, Rezaei M, Babaie A (2021) The effect of incorporating graphene and polycaprolactone-grafted graphene oxide nanosheets on thermal and physico-mechanical properties, microstructure and biocompatibility of electrospun polyurethane nanocomposite mats. Compos B: Eng 224:109210
Jyoti J, Kiran A, Sandhu M, Kumar A, Singh BP, Kumar N (2021) Improved nanomechanical and in-vitro biocompatibility of graphene oxide-carbon nanotube hydroxyapatite hybrid composites by synergistic effect. J Mech Behav Biomed Mater 117:104376
Gu MY, Dai ZQ, Yan X, Ma JF, Niu YC, Lan WJ et al (2021) Comparison of toxicity of Ti(3)C(2)and Nb2C Mxene quantum dots (QDs) to human umbilical vein endothelial cells. J Appl Toxicol 41(5):745–754. https://doi.org/10.1002/jat.4085
Xue Q, Zhang HJ, Zhu MS, Pei ZX, Li HF, Wang ZF et al (2017) Photoluminescent Ti3C2 MXene quantum dots for multicolor cellular imaging. Adv Mater 29(15):1604847. https://doi.org/10.1002/adma.201604847
Yang QH, Yin HH, Xu TM, Zhu DY, Yin JH, Chen YX et al (2020) Engineering 2D mesoporous Silica@MXene-integrated 3D-printing scaffolds for combinatory osteosarcoma therapy and NO-augmented bone regeneration. Small 16(14):1906814. https://doi.org/10.1002/smll.201906814
Sun LY, Fan L, Bian FK, Chen GP, Wang YT, Zhao YJ (2021) MXene-integrated microneedle patches with innate molecule encapsulation for wound healing. Research 2021:9838490. https://doi.org/10.34133/2021/9838490
He PP, Du XX, Cheng Y, Gao Q, Liu C, Wang XW et al (2022) Thermal-responsive MXene-DNA hydrogel for near-infrared light triggered localized photothermal-chemo synergistic cancer therapy. Small 18(40):2200263. https://doi.org/10.1002/smll.202200263
Lim GP, Soon CF, Ma NL, Morsin M, Nayan N, Ahmad MK et al (2021) Cytotoxicity of MXene-based nanomaterials for biomedical applications: a mini review. Environ Res 201:111592. https://doi.org/10.1016/j.envres.2021.111592
Zhao LJ, Wang LL, Zheng YQ, Zhao SF, Wei W, Zhang DW et al (2021) Highly-stable polymer-crosslinked 2D MXene-based flexible biocompatible electronic skins for in vivo biomonitoring. Nano Energy 84:105921. https://doi.org/10.1016/j.nanoen.2021.105921
Awasthi GP, Maharjan B, Shrestha S, Bhattarai DP, Yoon D, Park CH et al (2020) Synthesis, characterizations, and biocompatibility evaluation of polycaprolactone-MXene electrospun fibers. Colloids Surf A-Physicochem Eng Asp 586:124282. https://doi.org/10.1016/j.colsurfa.2019.124282
Neubertova V, Guselnikova O, Yamauchi Y, Olshtrem A, Rimpelova S, Cizmar E et al (2022) Covalent functionalization of Ti3C2T MXene flakes with Gd-DTPA complex for stable and biocompatible MRI contrast agent. Chem Eng J 446:136939. https://doi.org/10.1016/j.cej.2022.136939
Chen YX, Fu XL, Jiang Y, Feng WQ, Yu D, Wang W (2023) Highly sensitive and durable MXene/SBS nanofiber-based multifunctional sensors via thiol-ene click chemistry. Chem Eng J 467:143408. https://doi.org/10.1016/j.cej.2023.143408
Diedkova K, Pogrebnjak AD, Kyrylenko S, Smyrnova K, Buranich VV, Horodek P et al (2023) Polycaprolactone-MXene nanofibrous scaffolds for tissue engineering. ACS Appl Mater Interfaces 15(11):14033–14047. https://doi.org/10.1021/acsami.2c22780
Penkov OV, Khadem M, Lee JS, Kheradmandfard M, Kim CL, Cho SW et al (2018) Highly durable and biocompatible periodical Si/DLC nanocomposite coatings. Nanoscale 10(10):4852–4860. https://doi.org/10.1039/c7nr06762c
Dearnaley G, Arps JH (2005) Biomedical applications of diamond-like carbon (DLC) coatings: a review. Surf Coat Technol 200(7):2518–2524
Heinrich G, Grogler T, Rosiwal SM, Singer RF (1997) CVD diamond coated titanium alloys for biomedical and aerospace applications. Surf Coat Technol 94–5(1–3):514–520. https://doi.org/10.1016/S0257-8972(97)00459-3
Tang L, Tsai C, Gerberich WW, Kruckeberg L, Kania DR (1995) Biocompatibility of chemical-vapor-deposited diamond. Biomaterials 16(6):483–488. https://doi.org/10.1016/0142-9612(95)98822-V
Piszczek P, Lewandowska Z, Radtke A, Jedrzejewski T, Kozak W, Sadowska B et al (2017) Biocompatibility of titania nanotube coatings enriched with silver nanograins by chemical vapor deposition. Nanomaterials 7(9):274. https://doi.org/10.3390/nano7090274
Su CC, Hu YQ, Song Q, Ye YM, Gao LL, Li P et al (2020) Initiated chemical vapor deposition of graded polymer coatings enabling antibacterial, antifouling, and biocompatible surfaces. ACS Appl Mater Interfaces 12(16):18978–18986. https://doi.org/10.1021/acsami.9b22611
Coclite AM (2013) Smart surfaces by initiated chemical vapor deposition. Surf Innov 1(1):6–14. https://doi.org/10.1680/si.12.00019
Liu ZX, Jiang XY, Li ZY, Zheng YF, Nie JJ, Cui ZD et al (2022) Recent progress of photo-excited antibacterial materials via chemical vapor deposition. Chem Eng J 437:135401. https://doi.org/10.1016/j.cej.2022.135401
Hogg A, Uhl S, Feuvrier F, Girardet Y, Graf B, Aellen T et al (2014) Protective multilayer packaging for long-term implantable medical devices. Surf Coat Technol 255:124–129. https://doi.org/10.1016/j.surfcoat.2014.02.070
Spoiala A, Ilie CI, Ficai D, Ficai A, Andronescu E (2022) From biomedical applications of alginate towards CVD implications linked to COVID-19. Pharmaceuticals 15(3):318. https://doi.org/10.3390/ph15030318
Shirman T, Freeman D, Posner YD, Feldman I, Facchetti A, van der Boom ME (2008) Assembly of crystalline halogen-bonded materials by physical vapor deposition. J Am Chem Soc 130(26):8162. https://doi.org/10.1021/ja8029784
Selvakumar J, Sathiyamoorthy D (2012) Nanocrystalline silicon carbide thin films by fluidised/packed bed chemical vapor deposition using a halogen-free single source. J Mater Chem 22(15):7551–7558. https://doi.org/10.1039/c2jm15561c
Hwang NM, Cheong WS, Yoon DY, Kim DY (2000) Growth of silicon nanowires by chemical vapor deposition: approach by charged cluster model. J Cryst Growth 218(1):33–39. https://doi.org/10.1016/S0022-0248(00)00543-1
Kheradmandfard M, Penkov OV, Kashani-Bozorg SF, Lee JS, Kim C-L, Khadem M et al (2022) Exceptional improvement in the wear resistance of biomedical β-type titanium alloy with the use of a biocompatible multilayer Si/DLC nanocomposite coating. Ceram Int 48(12):17376–17384
Mansurnezhad R, Ghasemi-Mobarakeh L, Coclite AM, Beigi MH, Gharibi H, Werzer O et al (2020) Fabrication, characterization and cytocompatibility assessment of gelatin nanofibers coated with a polymer thin film by initiated chemical vapor deposition. Mater Sci Eng C-Mater Biol Appl 110:110623. https://doi.org/10.1016/j.msec.2019.110623
Meyyappan M, Delzeit L, Cassell A, Hash D (2003) Carbon nanotube growth by PECVD: a review. Plasma Sources Sci Technol 12(2):205–216. https://doi.org/10.1088/0963-0252/12/2/312. (Pii S0963-0252(03)60688-2)
Huang H, Winchester KJ, Suvorova A, Lawn BR, Liu Y, Hu XZ et al (2006) Effect of deposition conditions on mechanical properties of low-temperature PECVD silicon nitride films. Mater Sci Eng A-Struct Mater Prop Microstruct Process 435:453–459. https://doi.org/10.1016/j.msea.2006.07.015
Zhang XM, Qiu JJ, Tan J, Zhang DD, Wu L, Qiao YQ et al (2022) In-situ growth of vertical graphene on titanium by PECVD for rapid sterilization under near-infrared light. Carbon 192:209–218. https://doi.org/10.1016/j.carbon.2022.02.050
Chugh S, Mehta R, Lu N, Dios FD, Kim MJ, Chen ZH (2015) Comparison of graphene growth on arbitrary non-catalytic substrates using low-temperature PECVD. Carbon 93:393–399. https://doi.org/10.1016/j.carbon.2015.05.035
Li D, Bulou S, Gautier N, Elisabeth S, Goullet A, Richard-Plouet M et al (2019) Nanostructure and photocatalytic properties of TiO2 films deposited at low temperature by pulsed PECVD. Appl Surf Sci 466:63–69. https://doi.org/10.1016/j.apsusc.2018.09.230
Joshi P, Riley PR, Denning W, Shukla S, Khosla N, Narayan J et al (2022) Laser-patterned carbon coatings on flexible and optically transparent plastic substrates for advanced biomedical sensing and implant applications. J Mater Chem C 10(8):2965–2975. https://doi.org/10.1039/d1tc05176h
Euridice WA, Leite NB, Gelamo RV, Buranello PAD, da Silva MV, de Oliveira CJF et al (2020) a-C: H films produced by PECVD technique onto substrate of Ti6Al4V alloy: chemical and biological responses. Appl Surf Sci 503:144084. https://doi.org/10.1016/j.apsusc.2019.144084
Jagadeesh GV, Setti SG (2021) Bio-engineering and bio-design of new generation bioresorbable implants. Indian J Biochem Biophys 58(2):118–126
Cho YS, Liao LK, Hsu CH, Hsu YH, Wu WY, Liao SC et al (2019) Effect of substrate bias on biocompatibility of amorphous carbon coatings deposited on Ti6Al4V by PECVD. Surf Coat Technol 357:212–217. https://doi.org/10.1016/j.surfcoat.2018.09.070
Oliveira SMM, Barzotto ILM, Vieira L, Sene A, Radi PA, Fraga S et al (2019) Tribocorrosion studies on diamond-like carbon film deposited by PECVD on 304 stainless steel in simulated body fluid. Biomed Phys Eng Express 5(4):045012. https://doi.org/10.1088/2057-1976/ab18e9
Wei X, Zhang Y, Feng H, Cao X, Ding Q, Lu Z et al (2022) Bio-tribology and corrosion behaviors of a Si-and N-incorporated diamond-like carbon film: a new class of protective film for Ti6Al4V artificial implants. ACS Biomater Sci Eng 8(3):1166–1180
Oliveira S, Barzotto I, Vieira L, Sene A, Radi P, Fraga S et al (2019) Tribocorrosion studies on diamond-like carbon film deposited by PECVD on 304 stainless steel in simulated body fluid. Biomed Phys Eng Express 5(4):045012
Jagielski J, Turos A, Biefinski D, Abdul-Kader AM, Platkowska A (2007) Ion-beam modified polymers for biomedical applications. Nucl Inst Methods Phys Res Sect B-Beam Interact Mater Atoms 261(1–2):690–693. https://doi.org/10.1016/j.nimb.2007.03.021
Panin SV, Kornienko LA, Chaikina MV, Sergeev VP, Ivanova LR, Shilko SV (2014) Nano- and micro-structured UHMWPE composites filled with hydroxyapatite irradiated by nitrogen ion beams for bio-medical applications. Russ Phys J 56(10):1137–1143. https://doi.org/10.1007/s11182-014-0153-6
Asdi MH, Khan MUA, Hussain J, Arshad M, Karim MRA, Javed K et al (2022) Effect of phosphorous ion implantation on the surface, crystal structure, mechanical, and electrochemical properties of bioresorbable magnesium for biomedical applications. J Mater Eng Perform 31(9):7695–7704. https://doi.org/10.1007/s11665-022-06763-y
Kimmel DB, Vennin S, Desyatova A, Turner JA, Akhter MP, Lappe JM et al (2022) Bone architecture, bone material properties, and bone turnover in non-osteoporotic post-menopausal women with fragility fracture. Osteoporos Int 33(5):1125–1136. https://doi.org/10.1007/s00198-022-06308-y
Fada R, Babadi NF, Azimi R, Karimian M, Shahgholi M (2021) Mechanical properties improvement and bone regeneration of calcium phosphate bone cement, polymethyl methacrylate and glass ionomer. J Nanoanalysis 8(1):60–79. https://doi.org/10.22034/Jna.2021.681550
Barba D, Alabort E, Reed RC (2019) Synthetic bone: design by additive manufacturing. Acta Biomater 97:637–656. https://doi.org/10.1016/j.actbio.2019.07.049
Marques A, Miranda G, Silva F, Pinto P, Carvalho O (2021) Review on current limits and potentialities of technologies for biomedical ceramic scaffolds production. J Biomed Mater Res B-Appl Biomater 109(3):377–393. https://doi.org/10.1002/jbm.b.34706
Zhao YQ, Sun YJ, Zhang YD, Ding XK, Zhao NN, Yu BR et al (2020) Well-defined gold nanorod/polymer hybrid coating with inherent antifouling and photothermal bactericidal properties for treating an infected hernia. ACS Nano 14(2):2265–2275. https://doi.org/10.1021/acsnano.9b09282
Yao XY, Tang JC, Zhou YH, Atrens A, Dargusch MS, Wiese B et al (2021) Surface modification of biomedical Mg-Ca and Mg-Zn-Ca alloys using selective laser melting: corrosion behaviour, microhardness and biocompatibility. J Magnes Alloys 9(6):2155–2168. https://doi.org/10.1016/j.jma.2020.08.011
Huang R, Hao YF, Pan YS, Pan CL, Tang XL, Huang L et al (2022) Using a two-step method of surface mechanical attrition treatment and calcium ion implantation to promote the osteogenic activity of mesenchymal stem cells as well as biomineralization on a beta-titanium surface. RSC Adv 12(31):20037–20053. https://doi.org/10.1039/d2ra00032f
Lin X, Yang SF, Lai K, Yang HL, Webster TJ, Yang L (2017) Orthopedic implant biomaterials with both osteogenic and anti-infection capacities and associated in vivo evaluation methods. Nanomedicine-Nanotechnol Biol Med 13(1):123–142. https://doi.org/10.1016/j.nano.2016.08.003
Yu ZL, Deng JG, He JJ, Huo YP, Wu YJ, Wang XD et al (1991) Mutation breeding by ion-implantation. Nucl Inst Methods Phys Res Sect B-Beam Interact Mater Atoms 59:705–708. https://doi.org/10.1016/0168-583x(91)95307-Y
Liu Y, Zhang K, Han J-H, Hwang Y-H, Xu S, Kim D-E (2022) One-step method to enhance biotribological properties and biocompatibility of DLC coating by ion beam irradiation. Friction 10(7):1114–1126
Penkov OV, Kheradmandfard M, Khadem M, Kharaziha M, Mirzaamiri R, Seo K-J et al (2019) Ion-beam irradiation of DLC-based nanocomposite: creation of a highly biocompatible surface. Appl Surf Sci 469:896–903
Food and Drug Administration hompage. http:/fda.gov. Accessed on 29 Feb 2024
CARBOFIX orthopedics homepage. http://carbo-fix.com. Accessed on 29 Feb 2024
CARBON MEDICAL TECHNOLOGIES homepage. http://carbonmed.com. Accessed on 29 Feb 2024
Bio-medical Carbon Tecnology homepage. http://bm-carbon.com. Accessed on 29 Feb 2024
Vatech hompage. http://vatech.com. Accessed on 29 Feb 2024
G.tec medical enginerring GmbH. https://www.gtec.at/. Accessed on 29 Feb 2024
Funding
This research was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. 2022M3J7A1062940).
Author information
Authors and Affiliations
Contributions
Choong-Hee Kim: writing-original draft; Seul-Yi Lee: writing—review and editing; Kyong Yop Rhee: supervision, project administration; Soo-Jin Park: supervision, project administration, writing—review and editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, CH., Lee, SY., Rhee, K.Y. et al. Carbon-based composites in biomedical applications: a comprehensive review of properties, applications, and future directions. Adv Compos Hybrid Mater 7, 55 (2024). https://doi.org/10.1007/s42114-024-00846-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s42114-024-00846-1