Abstract
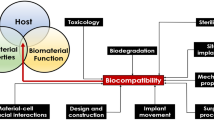
Carbon-based materials have emerged as an excellent class of biomedical materials due to their exceptional mechanical properties, lower surface friction, and resistance to wear, tear, and corrosion. Experimental studies have shown the promising results of carbon-based coatings in the field of biomedical implants. The reasons for their successful applications are their ability to suppress thrombo-inflammatory reactions which are evoked as an immune response due to foreign body object implantation. Different types of carbon coatings such as diamond-like carbon, pyrolytic carbon, silicon carbide, and graphene have been extensively studied and utilized in various fields of life including the biomedical industry. Their atomic arrangement and structural properties give rise to unique features which make them suitable for multiple applications. Due to the specificity and hardness of carbon-based precursors, only a specific type of coating technique may be utilized for nanostructure development and fabrication. In this paper, different coating techniques are discussed which were selected based on the substrate material, the type of implant, and the thickness of coating layer. Chemical vapor deposition-based techniques, thermal spray coating, pulsed laser deposition, and biomimetic coatings are some of the most common techniques that are used in the field of biomaterials to deposit a coating layer on the implant. Literature gathered in this review has significance in the field of biomedical implant industry to reduce its failure rate by making surfaces inert, decreasing corrosion related issues and enhancing biocompatibility.




Similar content being viewed by others
Data availability
All relevant data are included in the article and/or its supplementary information files.
References
Grainger DW et al (2013) Critical factors in the translation of improved antimicrobial strategies for medical implants and devices. Biomaterials 34:9237–9243
Arsiwala A, Desai P, Patravale V (2014) Recent advances in micro/nanoscale biomedical implants. J Controll Release 189:25–45
Hassija V, Chamola V, Bajpai BC, Naren, and S. Zeadally, (2021) Security issues in implantable medical devices: Fact or fiction? Sustaina Cities Soc 66:102552
Costa RC et al (2021) Microbial corrosion in titanium-based dental implants: how tiny bacteria can create a big problem? J Bio- Tribo-Corros 7:136
Guo T, Gulati K, Arora H, Han P, Fournier B, Ivanovski S (2021) Race to invade: understanding soft tissue integration at the transmucosal region of titanium dental implants. Dent Mater 37(5):816–831
Kelly CN et al (2021) High-strength, porous additively manufactured implants with optimized mechanical osseointegration. Biomaterials 279:121206
Zhang H, Li Z, Li W (2021) M2 macrophages serve as critical executor of innate immunity in chronic allograft rejection. Front Immunol 12:648539
Alhammadi SH, Burnside G, Milosevic A (2021) Clinical outcomes of single implant supported crowns versus 3-unit implant-supported fixed dental prostheses in Dubai Health Authority: a retrospective study. BMC Oral Health 21(1):171
Kheradmandfard M et al (2018) Significant improvement in cell adhesion and wear resistance of biomedical β-type titanium alloy through ultrasonic nanocrystal surface modification. J Alloy Compd 762:941–949
Abaricia JO, Farzad N, Heath TJ, Simmons J, Morandini L, Olivares-Navarrete RJ (2021) Control of innate immune response by biomaterial surface topography, energy, and stiffness. Acta Biomater 133:58–73
Hasan A et al (2020) Surface design for immobilization of an antimicrobial peptide mimic for efficient anti-biofouling. Chem A Eur J 26:5789–5793
Doloff JC et al (2021) The surface topography of silicone breast implants mediates the foreign body response in mice, rabbits and humans. Nat Biomed Eng 5(10):1115–1130
Apte G, Börke J, Rothe H, Liefeith K, Nguyen T-H (2020) Modulation of platelet-surface activation: current state and future perspectives. ACS Appl Bio Mater 3(9):5574–5589
Choi J et al (2022) Micro-textured silicone-based implant fabrication using electrospun fibers as a sacrificial template to suppress fibrous capsule formation. Biomater Adv 135:112687
Ratha I, Datta P, Balla VK, Nandi SK, Kundu B (2021) Effect of doping in hydroxyapatite as coating material on biomedical implants by plasma spraying method: a review. Ceram Int 47(4):4426–4445
Jiang P, Hou R, Zhu S, Guan S (2022) A robust calcium carbonate (CaCO3) coating on biomedical MgZnCa alloy for promising corrosion protection. Corros Sci 198:110–124
Quarterman JC, Geary SM, Salem AK (2021) Evolution of drug-eluting biomedical implants for sustained drug delivery. Eur J Pharma Biopharm 159:21–35
Quarterman JC, Geary SM, Salem AK (2021) Evolution of drug-eluting biomedical implants for sustained drug delivery. Eur J Pharm Biopharm 159:21–35
Manabe K, Nara H (2021) Construction of stable biological albumin/heparin multilayers for elastic coatings on hydrophobic antithrombogenic artificial blood vessels. Tribol Int 156:106843
Zhang B, Su Y, Zhou J, Zheng Y, Zhu D (2021) Toward a better regeneration through implant-mediated immunomodulation: harnessing the immune responses. Adv Sci 8(16):2100446
Srimaneepong V, Skallevold HE, Khurshid Z, Zafar MS, Rokaya D, Sapkota J (2022) Graphene for antimicrobial and coating application. Int J Mol Sci 23(1):499
Gaur M et al (2021) Biomedical applications of carbon nanomaterials: fullerenes, quantum dots, nanotubes, nanofibers, and graphene. Materials 14(20):5978
Cumont A, Pitt AR, Lambert PA, Oggioni MR, Ye H (2022) Properties, mechanism and applications of diamond as an antibacterial material. Funct Diam 1(1):1–28
Rothammer B et al (2021) Amorphous carbon coatings for total knee replacements—part i: deposition, Cytocompatibility, chemical and mechanical properties. Polymers 13(12):1952
Hassan S, Ali MN, Mir M, Ahmed A, Arshad M (2021) Development and evaluation of drug delivery patch for topical wound healing application. SN Appl Sci 3(10):825
Blyweert P, Nicolas V, Fierro V, Celzard A (2021) 3D printing of carbon-based materials: a review. Carbon 183:449–485
Ying B, Park S, Chen L, Dong X, Young EW, Liu X (2020) NanoPADs and nanoFACEs: an optically transparent nanopaper-based device for biomedical applications. Lab Chip 20(18):3322–3333
Maleki H, Azimi B, Ismaeilimoghadam S, Danti S (2022) Poly (lactic acid)-based electrospun fibrous structures for biomedical applications. Appl Sci 12(6):3192
Efe GÇ, Yenilmez E, Altinsoy İ, Türk S, Bindal C (2021) Characterization of UHMWPE-HAp coating produced by dip coating method on Ti6Al4V alloy. Surf Coat Technol 418:127091
Falcao EH, Wudl F (2007) Carbon allotropes: beyond graphite and diamond. J Chem Technol Biotechnol 82(6):524–531
Hirsch A (2010) The era of carbon allotropes. Nat Mater 9(11):868–871
Rajak DK, Kumar A, Behera A, Menezes PL (2021) Diamond-like carbon (DLC) coatings: classification, properties, and applications. Appl Sci 11(10):4445
M. E. Arslan et al. (2022) Structural, biocompatibility, and antibacterial properties of Ge–DLC nanocomposite for biomedical applications. Journal of Biomedical Materials Research n/a, no. n/a
Love CA, Cook RB, Harvey TJ, Dearnley PA, Wood RJK (2013) Diamond like carbon coatings for potential application in biological implants—a review. Tribol Int 63:141–150
Li C, Huang L, Yuan J (2020) Effect of sp3 content on adhesion and tribological properties of non-hydrogenated DLC films. Materials 13(8):1911
Paul R (2017) Diamond-like-carbon coatings for advanced biomedical applications. Global J Nanomed 2(5):555598
Hasebe T et al (2007) Fluorine doping into diamond-like carbon coatings inhibits protein adsorption and platelet activation. J Biomed Mater Res 83A(4):1192–1199
Gutensohn K et al (2000) In vitro analyses of diamond-like carbon coated stents: reduction of metal ion release, platelet activation, and thrombogenicity. Thromb Res 99(6):577–585
Maguire P et al (2005) Mechanical stability, corrosion performance and bioresponse of amorphous diamond-like carbon for medical stents and guidewires. Diam Relat mater 14(8):1277–1288
Polukhina A et al (2022) Cellular and molecular issues of hemo-and biocompatibility of diamond-like carbon films. a brief critical review. Cell Tissue Biol 16(1):1–14
Zhang M, Xie T, Qian X, Zhu Y, Liu X (2020) Mechanical properties and biocompatibility of Ti-doped diamond-like carbon films. ACS Omega 5(36):22772–22777
Ando K et al (2016) Prospective multi-center registry to evaluate efficacy and safety of the newly developed diamond-like carbon-coated cobalt–chromium coronary stent system. Cardiovasc Interv Ther 32:225–232
Gorzelanny C et al (2016) Silver nanoparticle-enriched diamond-like carbon implant modification as a mammalian cell compatible surface with antimicrobial properties. Sci Rep 6(1):22849
Ban M, Tobe S, Takeuchi L (2018) Effects of diamond-like carbon thin film and wrinkle microstructure on cell proliferation. Diam Relat Mater 90:194–201
Zhu W et al (2022) Preparation and characterization of diamond-like carbon (DLC) film on 316L stainless steel by microwave plasma chemical vapor deposition (MPCVD). Diam Relat Mater 122:108820
Zhang X et al (2019) Theoretical strength and rubber-like behaviour in micro-sized pyrolytic carbon. Nat Nanotechnol 14(8):762–769
Wang M, Guo L, Sun H (2019) Manufacture of Biomaterials. In: Narayan R (ed) Encyclopedia of biomedical engineering. Elsevier, Oxford, pp 116–134
Liu F, Shirasu K, Hashida T (2021) Epitaxial pyrolytic carbon coatings templated with defective carbon nanotube cores for structural annealing and tensile property improvement. J Mater Sci 56(34):19015–19028
Stanley J, Klawitter J, More R (2008) 26 - Replacing joints with pyrolytic carbon. In: Revell PA (ed) Joint replacement technology. Woodhead Publishing, pp 631–656
Salkeld SL, Patron LP, Lien JC, Cook SD, Jones DG (2016) Biological and functional evaluation of a novel pyrolytic carbon implant for the treatment of focal osteochondral defects in the medial femoral condyle: assessment in a canine model. J Orthop Surg Res 11(1):155
Bokros J, Gott V, La Grange L, Fadall A, Vos K, Ramos M (1969) Correlations between blood compatibility and heparin adsorptivity for an impermeable isotropic pyrolytic carbon. J Biomed Mater Res 3(3):497–528
Serino G, Gusmini M, Audenino AL, Bergamasco G, Ieropoli O, Bignardi C (2021) Multiscale characterization of isotropic pyrolytic carbon used for mechanical heart valve production. Processes 9(2):338
Mountfort K et al (2014) Cre8™ Unique Technology in Challenging Daily Practice: proceedings of a satellite symposium held at EuroPCR on 20th - 23rd May 2014 in Paris, (in eng). Interv Cardiol (London, England) 9(3):180–183
Carrié D et al (2012) A multicenter randomized trial comparing amphilimus-with paclitaxel-eluting stents in de novo native coronary artery lesions. J Am Coll Cardiol 59(15):1371–1376
Pivato CA, Leone PP, Petriello G, Sanz-Sanchez J, Chiarito M, Stefanini GG (2020) The Cre8 amphilimus-eluting stent for the treatment of coronary artery disease: safety and efficacy profile. Expert Rev Med Devices 17(4):267–275
Goodman SL, Tweden KS, Albrecht RM (1996) Platelet interaction with pyrolytic carbon heart-valve leaflets. J Biomed Mater Res: Off J Soc Biomater Jpn Soc Biomater 32(2):249–258
Ogwu AA, Okpalugo TIT, Ali N, Maguire PD, McLaughlin JAD (2008) Endothelial cell growth on silicon modified hydrogenated amorphous carbon thin films. J Biomed Mater Res 85B(1):105–113
Okpalugo TIT, Ogwu AA, Maguire PD, McLaughlin JAD (2004) Platelet adhesion on silicon modified hydrogenated amorphous carbon films. Biomaterials 25(2):239–245
Li M, Cheng Y, Zheng YF, Zhang X, Xi TF, Wei SC (2012) Surface characteristics and corrosion behaviour of WE43 magnesium alloy coated by SiC film. Appl Surf Sci 258(7):3074–3081
Forrestal BJ, Case BC, Yerasi C, Garcia-Garcia HM, Waksman R (2020) The Orsiro Ultrathin, bioresorbable-polymer sirolimus-eluting stent: a review of current evidence. Cardiovasc Revasc Med 21(4):540–548
Ploumen EH et al (2021) Acute myocardial infarction treated with novel Resolute Onyx and Orsiro stents in the randomized BIONYX trial. Catheter Cardiovasc Interv 98(2):E188–E196
Saito S et al (2019) BIOFLOW-IV, a randomised, intercontinental, multicentre study to assess the safety and effectiveness of the Orsiro sirolimus-eluting stent in the treatment of subjects with de novo coronary artery lesions: primary outcome target vessel failure at 12 months. EuroIntervention 15(11):e1006–e1013
Wang J, Ma F, Sun M (2017) Graphene, hexagonal boron nitride, and their heterostructures: properties and applications. RSC Adv 7(27):16801–16822
Zhao C et al (2020) Synthesis of graphene quantum dots and their applications in drug delivery. J Nanobiotechnol 18(1):142
Jiříčková A, Jankovský O, Sofer Z, Sedmidubský D (2022) Synthesis and applications of graphene Oxide, (in eng). Materials (Basel) 15(3):920
Podila R, Moore T, Alexis F, Rao A (2013) Graphene coatings for biomedical implants, (in eng). J Vis Exp. https://doi.org/10.3791/50276
Reina G, González-Domínguez JM, Criado A, Vázquez E, Bianco A, Prato M (2017) Promises, facts and challenges for graphene in biomedical applications. Chem Soc Rev 46(15):4400–4416
Yang M-C et al (2019) Electrochemical polymerization of PEDOT–Graphene Oxide-heparin composite coating for anti-fouling and anti-clotting of cardiovascular stents. Polymers 11(9):1520
Ge S et al (2019) Inhibition of in-stent restenosis after graphene oxide double-layer drug coating with good biocompatibility. Regen Biomater 6(5):299–309
Shen H, Zhang L, Liu M, Zhang Z (2012) “Biomedical applications of graphene,” (in eng). Theranostics 2(3):283–294
Wu L, Yang H, Cheng J, Hu C, Wu Z, Feng Y (2021) Review in preparation and application of nickel-coated graphite composite powder. J Alloy Compd 862:158014
Kozbial A et al (2014) Understanding the intrinsic water wettability of graphite. Carbon 74:218–225
Shahriarinour M, Rahimi F, Siahbani E, Kochakinejad R, Kaki S (2022) A new electrochemical modified graphite pencil electrode developed for cholesterol assessing. J Irani Chem Soc 19(1):159–171
Tang X, Yang A, Li L (2022) Optimization of Nanofiber Wearable Heart Rate Sensor Module for Human Motion Detection," Computational Mathematical Methods in Medicine 2022
de Lima LF, de Freitas ADS, Ferreira AL, Maciel CC, Ferreira M, WR de, (2022) Enzymeless glucose sensor based on disposable Ecoflex®/graphite thermoplastic composite substrate modified with Au@ GQDs. Sens Actuators Rep 4:100102
Knoell A, Maxwell H, Bechtol C (1975) Graphite fiber reinforced bone cement. Ann Biomed Eng 3(2):225–229
Hung W-C, Wu K-H, Lyu D-Y, Cheng K-F, Huang W-C (2017) Preparation and characterization of expanded graphite/metal oxides for antimicrobial application. Mater Sci Eng: C 75:1019–1025
Oveissi F, Naficy S, Lee A, Winlaw D, Dehghani F (2020) Materials and manufacturing perspectives in engineering heart valves: a review. Materials Today Bio 5:100038
Kharlamova MV, Kramberger C (2021) Applications of filled single-walled carbon nanotubes: progress, challenges, and perspectives, (in eng). Nanomaterials (Basel) 11(11):2863
Yang Z et al (2010) Pharmacological and toxicological target organelles and safe use of single-walled carbon nanotubes as drug carriers in treating Alzheimer disease. Nanomed Nanotechnol Biol Med 6(3):427–441
Chen J, Chen S, Zhao X, Kuznetsova LV, Wong SS, Ojima I (2008) Functionalized single-walled carbon nanotubes as rationally designed vehicles for tumor-targeted drug delivery. J Am Chem Soc 130(49):16778–16785
Yola ML, Atar N (2021) Novel voltammetric tumor necrosis factor-alpha (TNF-α) immunosensor based on gold nanoparticles involved in thiol-functionalized multi-walled carbon nanotubes and bimetallic Ni/Cu-MOFs. Anal Bioanal Chem 413(9):2481–2492
Serafín V et al (2019) Graphene quantum dots-functionalized multi-walled carbon nanotubes as nanocarriers in electrochemical immunosensing. Determination of IL-13 receptor α2 in colorectal cells and tumor tissues with different metastatic potential. Sens Actuators B: Chem 284:711–722
Morais RP et al (2020) Naringenin-functionalized multi-walled carbon nanotubes: a potential approach for site-specific remote-controlled anticancer delivery for the treatment of lung cancer cells. Int J Mol Sci 21(12):4557
Ozgen PSO, Atasoy S, Kurt BZ, Durmus Z, Yigit G, Dag A (2020) Glycopolymer decorated multiwalled carbon nanotubes for dual targeted breast cancer therapy. J Mater Chem B 8(15):3123–3137
Sivaraj D, Vijayalakshmi K (2019) Novel synthesis of bioactive hydroxyapatite/f-multiwalled carbon nanotube composite coating on 316L SS implant for substantial corrosion resistance and antibacterial activity. J Alloy Compd 777:1340–1346
Xavier SA, Vijayalakshmi U (2018) Electrochemically grown functionalized-Multi-walled carbon nanotubes/hydroxyapatite hybrids on surgical grade 316L SS with enhanced corrosion resistance and bioactivity. Colloids Surf B: Biointerfaces 171:186–196
Vardharajula S et al (2012) “Functionalized carbon nanotubes: biomedical applications,” (in eng). Int J Nanomed 7:5361–5374
Murugesan R, Raman S (2022) Recent trends in carbon nanotubes based prostate cancer therapy: a biomedical hybrid for diagnosis and treatment. Curr Drug Deliv 19(2):229–237
Wee Y, Park S, Kwon YH, Ju Y, Yeon K-M, Kim J (2019) Tyrosinase-immobilized CNT based biosensor for highly-sensitive detection of phenolic compounds. Biosensors Bioelectronics 132:279–285
Kaur J, Gill GSS, Jeet K (2019) Applications of carbon nanotubes in drug delivery: A comprehensive review. Characterization biology of nanomaterials for drug delivery 113-135
Kiran AR, Kumari GK, Krishnamurthy PT (2020) Carbon nanotubes in drug delivery: focus on anticancer therapies. J Drug Deliv Sci Technol 59:101892
Simon J, Flahaut E, Golzio M (2019) Overview of carbon nanotubes for biomedical applications. Materials 12(4):624
Pahlevanzadeh F et al (2021) CNT and rGO reinforced PMMA based bone cement for fixation of load bearing implants: mechanical property and biological response. J Mech Behav Biomed Mater 116:104320
Francis AA, Abdel-Gawad SA, Shoeib MA (2021) Toward CNT-reinforced chitosan-based ceramic composite coatings on biodegradable magnesium for surgical implants. J Coat Technol Res 18(4):971–988
Mondal T et al (2022) Thin films of functionalized carbon nanotubes support long-term maintenance and cardio-neuronal differentiation of canine induced pluripotent stem cells. Nanomed Nanotechnol Biol Med 40:102487
Li T, Dorn HC (2017) Biomedical applications of metal-encapsulated fullerene nanoparticles. Small 13(8):1603152
Zhang Q et al (2009) Autophagy-mediated chemosensitization in cancer cells by fullerene C60 nanocrystal. Autophagy 5(8):1107–1117
Bhakta P, Barthunia B (2020) Fullerene and its applications: a review. J Indian Acad Oral Med Radiol 32(2):159
Buschbeck EK, Le Duc A, Kelley C, Hoque MA, Alvarez NT (2021) Functionalized carbon nanotube microfibers for chronic neural implants. J Neurosci Methods 364:109370
Bronner C (2018) Bottom-up synthesis and electronic structure of graphene nanoribbons on surfaces. In: Wandelt K (ed) Encyclopedia of interfacial chemistry. Elsevier, Oxford, pp 210–225
Burdanova MG, Kharlamova MV, Kramberger C, Nikitin MP (2021) Applications of pristine and functionalized carbon nanotubes, graphene, and graphene nanoribbons in biomedicine. Nanomaterials 11(11):3020
Zakharova OV, Mastalygina EE, Golokhvast KS, Gusev AA (2021) Graphene nanoribbons: prospects of application in biomedicine and toxicity. Nanomaterials 11:2425
Barui AK et al (2012) Zinc oxide nanoflowers make new blood vessels. Nanoscale 4(24):7861–7869. https://doi.org/10.1039/C2NR32369A
Negahdary M, Heli H (2018) Applications of nanoflowers in biomedicine. Recent Pat Nanotechnol 12(1):22–33
Fatima SW, Imtiyaz K, Alam Rizvi MM, Khare SK (2021) Microbial transglutaminase nanoflowers as an alternative nanomedicine for breast cancer theranostics," (in eng). RSC Adv 11(55):34613–34630
Fang Y, Wang S, Liu Y, Xu Z, Zhang K, Guo Y (2018) Development of Cu nanoflowers modified the flexible needle-type microelectrode and its application in continuous monitoring glucose in vivo. Biosens Bioelectron 110:44–51
Madannejad R, Shoaie N, Jahanpeyma F, Darvishi MH, Azimzadeh M, Javadi H (2019) Toxicity of carbon-based nanomaterials: reviewing recent reports in medical and biological systems. Chemico-Biol Interact 307:206–222
Fedel M, Wong TT, Speranza G, Lohberger B, Nogler M, Awaja F (2019) Hybrid graphene oxide/amorphous carbon coatings and their effect on the viability and toxicity of different cell types. Surf Coat Technol 374:95–102
Delorme MP et al (2012) Ninety-day inhalation toxicity study with a vapor grown carbon nanofiber in rats). Toxicol Sci 128(2):449–460
Pauluhn J (2010) Subchronic 13-week inhalation exposure of rats to multiwalled carbon nanotubes: toxic effects are determined by density of agglomerate structures, not fibrillar structure. Toxicol Sci 113(1):226–242
Holmannova D, Borsky P, Svadlakova T, Borska L, Fiala Z (2022) Carbon nanoparticles and their biomedical applications. Appl Sci 12(15):7865
Maiti D, Tong X, Mou X, Yang K (2019) Carbon-based nanomaterials for biomedical applications: a recent study. Front Pharmacol. https://doi.org/10.3389/fphar.2018.01401
Creighton J, Ho P (2001) Introduction to chemical vapor deposition (CVD). Chem Vap Depos 2:1–22
Kheradmandfard M et al (2022) Exceptional improvement in the wear resistance of biomedical β-type titanium alloy with the use of a biocompatible multilayer Si/DLC nanocomposite coating. Ceram Int 48(12):17376–17384
Song SH, Min BK, Hong M-H, Kwon T-Y (2020) Application of a novel CVD TiN coating on a Biomedical Co–Cr alloy: an evaluation of coating layer and substrate characteristics. Materials 13(5):1145
Anisur MR, Chakraborty Banerjee P, Easton CD, Singh Raman RK (2018) Controlling hydrogen environment and cooling during CVD graphene growth on nickel for improved corrosion resistance. Carbon 127:131–140
Johnson AP, Gangadharappa H, Pramod K (2020) Graphene nanoribbons: a promising nanomaterial for biomedical applications. J Control Release 325:141–162
Zhang Q et al (2021) Fabrication of a gradient hydrophobic surface with parallel ridges on pyrolytic carbon for artificial heart valves. Colloids Surf B: Biointerfaces 205:111894
Li H, Zhang LL, Li K-Z, He YG, Zhao XN, Zhao H (2009) Response of MG63 osteoblast-like cells on pyrolytic carbon coated carbon/carbon composites. Mater Sci Forum 620–622:579–582
Hassan S, Ali MN, Ghafoor B (2022) Evolutionary perspective of drug eluting stents: from thick polymer to polymer free approach. J Cardiothorac Surg 17:65
Chowdhury MSI et al (2020) Wear performance investigation of PVD coated and uncoated carbide tools during high-speed machining of TiAl6V4 aerospace alloy. Wear 446–447:203168
Vega J, Scheerer H, Andersohn G, Oechsner M (2018) Experimental studies of the effect of Ti interlayers on the corrosion resistance of TiN PVD coatings by using electrochemical methods. Corros Sci 133:240–250
Krella AK (2021) Cavitation erosion of monolayer PVD coatings – An influence of deposition technique on the degradation process. Wear 478–479:203762
Velusamy R, Ramakrishna S (2021) An in-vitro evaluation study on the effects of surface modification via physical vapor deposition on the degradation rates of magnesium-based biomaterials. Surf Coat Technol 411:126972
Bahi R, Nouveau C, Beliardouh NE, Ramoul CE, Meddah S, Ghelloudj O (2020) Surface performances of Ti-6Al-4V substrates coated PVD multilayered films in biological environments. Surf Coat Technol 385:125412
Nißen S, Heeg J, Wienecke M, Behrend D, Warkentin M (2018) Enhancing adhesion strength of a-C:H: Cu composite coatings on Ti6Al4V by graded copper deposition in a rf-PVD/PECVD hybrid process. Surf Coat Technol 350:659–671
Christy RW (1960) Formation of thin polymer films by electron bombardment. J Appl Phys 31(9):1680–1683
Baker AG, Morris WC (1961) Deposition of metallic films by electron impact decomposition of organometallic vapors. Rev Sci Instrum 32(4):458–458
Alt LL, Ing SW Jr, Laendle KW (1963) Low-temperature deposition of silicon oxide films. J Electrochem Soc 110(5):465
Mattox DM (2020) Handbook of physical vapor deposition (PVD) processing. Elsevier, pp 287–300
Eurídice WA et al (2020) a-C: H films produced by PECVD technique onto substrate of Ti6Al4V alloy: chemical and biological responses. Appl Surf Sci 503:144084
Fares C et al (2020) Demonstration of a SiC protective coating for titanium implants. Materials 13(15):3321
Huran J, Hrubcin L, Kobzev A, Liday J (1996) Properties of amorphous silicon carbide films prepared by PECVD. Vacuum 47(10):1223–1225
Bolz A, Amon M, Ozbek C, Heublein B, Schaldach M (1996) Coating of cardiovascular stents with a semiconductor to improve their hemocompatibility. Tex Heart Inst J 23(2):162
Frewin CL, Coletti C, Register JJ, Nezafati M, Thomas S, Saddow SE (2015) Silicon carbide materials for biomedical applications. In: Demarchi D, Tagliaferro A (eds) Carbon for Sensing Devices. Springer International Publishing, Cham, pp 153–207
Saddow SE, Frewin C, Reyes M, Register J, Nezafati M, Thomas S (2014) 3C-SiC on Si: a biocompatible material for advanced bioelectronic devices. ECS Trans 61:101–111
Fraga M, Pessoa R, Maciel H, Massi M (2011) Recent Developments on Silicon Carbide Thin Films for Piezoresistive Sensors Applications. M. Mukherjee, Ed.: Intech, pp. 369-388
Lan P, Nunez E, Polycarpou A (2019) “Advanced polymeric coatings and their applications: green tribology,” in Reference Module in Materials Science and Materials Engineering, 2019
Gu Y, Khor K, Pan D, Cheang P (2004) Activity of plasma sprayed yttria stabilized zirconia reinforced hydroxyapatite/Ti–6Al–4V composite coatings in simulated body fluid. Biomaterials 25(16):3177–3185
Zheng X, Huang M, Ding C (2000) Bond strength of plasma-sprayed hydroxyapatite/Ti composite coatings. Biomaterials 21(8):841–849
Yang Y, Ong JL, Tian J (2003) Deposition of highly adhesive ZrO2 coating on Ti and CoCrMo implant materials using plasma spraying. Biomaterials 24(4):619–627
Gérard B (2006) Application of thermal spraying in the automobile industry. Surf Coat Technol 201(5):2028–2031
Kumar S, Handa A, Chawla V, Grover NK, Kumar R (2021) Performance of thermal-sprayed coatings to combat hot corrosion of coal-fired boiler tube and effect of process parameters and post-coating heat treatment on coating performance: a review. Surf Eng 37(7):833–860
Kumar S, Kumar R (2021) Influence of processing conditions on the properties of thermal sprayed coating: a review. Surf Eng 37(11):1339–1372
Gadow R, Killinger A, Stiegler N (2010) Hydroxyapatite coatings for biomedical applications deposited by different thermal spray techniques. Surf Coat Technol 205:1157–1164
Prashar G, Vasudev H (2020) Thermal sprayed composite coatings for biomedical implants: a brief review. J Therm Spray Eng 2(1):50–55
Vilardell AM et al (2020) In-vitro comparison of hydroxyapatite coatings obtained by cold spray and conventional thermal spray technologies. Mater Sci Eng C 107:110306
Jagadeeshanayaka N, Awasthi S, Jambagi SC, Srivastava C (2022) Bioactive surface modifications through thermally sprayed hydroxyapatite composite coatings: a review of selective reinforcements. Biomater Sci 10:2484–2523. https://doi.org/10.1039/D2BM00039C
Prashar G, Vasudev H, Thakur L, Bansal A. Performance of thermally sprayed Hydroxyapatite coatings for biomedical implants: A comprehensive review 0, no. ja, p. null.
Arias JL, Mayor MB, Pou J, Leng Y, León B, Pérez-Amor M (2003) Micro-and nano-testing of calcium phosphate coatings produced by pulsed laser deposition. Biomaterials 24(20):3403–3408
Dailey OBLKB, Jordan L (2005) Characterization of hydroxyapatite films obtained by pulsed-laser deposition on Ti and Ti-6Al-4V. Dent Mater 21:1017–1024
Hidalgo-Robatto BM et al (2018) Pulsed laser deposition of copper and zinc doped hydroxyapatite coatings for biomedical applications. Sur Coat Technol 333:168–177
Pradhaban G, Kaliaraj GS, Vishwakarma V (2014) Antibacterial effects of silver–zirconia composite coatings using pulsed laser deposition onto 316L SS for bio implants. Prog Biomater 3(2):123–130
Chen L, Komasa S, Hashimoto Y, Hontsu S, Okazaki J (2018) In vitro and in vivo osteogenic activity of titanium implants coated by pulsed laser deposition with a thin film of fluoridated hydroxyapatite. Int J Mol Sci 19(4):1127
Li M, Komasa S, Hontsu S, Hashimoto Y, Okazaki J (2022) Structural characterization and osseointegrative properties of pulsed laser-deposited fluorinated hydroxyapatite films on nano-zirconia for implant applications. Int J Mol Sci 23(5):2416
Teghil R, Curcio M, De Bonis A (2021) Substituted hydroxyapatite, glass, and glass-ceramic thin films deposited by nanosecond pulsed laser deposition (PLD) for biomedical applications: a systematic review. Coatings 11(7):811
Joshi P et al (2022) Laser-patterned carbon coatings on flexible and optically transparent plastic substrates for advanced biomedical sensing and implant applications. J Mater Chem C 10(8):2965–2975
Vanalakar SA, Galal A, Singh VN, Min H (2018) A review of nanostructured thin films for gas sensing and corrosion protection. Mediterr J Chem 7:433–451
Acknowledgements
The authors acknowledge Bakhtawar Gafoor and Dr Mariam Mir for their valuable feedback and support during data collection and manuscript preparation.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, S.H. and H.Q.; data curation, S.H. and A.Y.N; writing, original draft preparation, S.H, H.Q. A.N.Y. and K. K.; writing, review and editing, S.H., K.K. A.A, A.S.K. and A.A.; supervision, A.S.K. and A.A. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hassan, S., Nadeem, A.Y., Qaiser, H. et al. A review of carbon-based materials and their coating techniques for biomedical implants applications. Carbon Lett. 33, 1171–1188 (2023). https://doi.org/10.1007/s42823-023-00496-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42823-023-00496-1