Abstract
Objectives
The potential role of neuroinflammation in adult attention deficit hyperactivity disorder (ADHD) patients has been investigated with peripheral hemogram-related inflammatory markers. Systemic immune inflammation index (SII) is defined as a new index that has been developed for the balance of inflammatory and immune status.
Methods
Our study was based on a prospective routine complete blood count(CBC) analysis of 74 Adult ADHD patients and 70 healthy participants. The DSM-5-Clinician version and Barratt impulsivity scale-11 were used to evaluate the participants.
Results
There was no statistical difference in the comparison of the SII ratios, platelet distribution width (PDW), and plateretritis (PCT) (p>0.05 for each) in a group of a young adults with ADHD and in a comparison control group. These inflammatory indicators were found to be similar between patients newly diagnosed with ADHD (n=40) and patients using methylphenidate (n=34) (p>0.05 for each). The relationship between ADHD clinical symptoms and severity and inflammation was evaluated. A significant negative correlation was observed between attention deficit scores and PCT (r=−0.301, p=0.009). A positive significant correlation was found between hyperactivity scores and SII (r=0.247, p=0.034). A significant positive correlation was found between Barrat motor scores and PDW(r=241, p=0.038). In the regression analysis, the PCT variable changed the attention deficit variable (β=.33, t(70)= −2.703, p=.009, pr2= .094) predicted negatively and significantly.
Conclusions
We demonstrated the association of SII, which is independently associated with adverse outcomes in many diseases, and the severity of hyperactivity symptoms in adult ADHD. The fact that PCT predicts attention deficit negatively and decisively shows the importance of inflammatory assessments specific to clinical presentations. The critical importance of platelets in inflammatory processes in ADHD has been demonstrated once again with inflammatory markers such as SII, PLT, and PDW, which can be accessed by an easily applicable complete blood count method.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder that is defined by the age-inappropriate symptoms of attention deficit, hyperactivity, and impulsivity that appear before the age of twelve, interfere with social or academic functioning (Association, 2013). Although ADHD is often considered as a childhood disorder, it is reported that 50% of the symptoms continue during adolescence and 30–60% extend into adulthood and continue to meet the diagnostic criteria in adulthood (Ahmed et al., 2014). It has been suggested that the number of adults with ADHD has increased over the past 20 years, and some of this increase is explained by the persistence of ADHD symptoms in adulthood (Núñez-Jaramillo et al., 2021). As developmental brain processes alleviate some of the consequences of ADHD with neural normalization, the symptoms of hyperactivity disappear wherever they are in adulthood, but the persistence of the symptoms of inattention from childhood to adulthood is emphasized (Duan et al., 2021). As well as changes in ADHD symptoms throughout life, the variable and complex interaction of genetic and environmental factors is believed to play a role in the continuity of the disorder (Caye, et al., 2016).
In the etiology of ADHD, it is thought that neuroinflammation may affect neurodevelopment in the immune system with changes in normal microglia, astrocytes, cytokines, chemokines, oxidative stress, and related molecular processes in the first months or years of life (Corona, 2020). An increased profile of ADHD risk is reported in children of mothers with inflammatory and immune system diseases (Instanes et al., 2017). The first study, which provides forward-looking human evidence that inflammation is an intermediary mechanism for brain development and behavior, suggests that maternal levels of interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and monocyte chemoattractant protein-1 (MCP-1) are a possible marker of ADHD risk (Gustafsson et al., 2020).
In addition to epidemiological and clinical studies, mechanistic evidence has been obtained from animal models consistent with the behavioral and neural consequences of maternal immune activation with ADHD (Dunn et al., 2019). It has been reported that neurodevelopmental high inflammatory responses by a number of mechanisms such as exposure to heavy metals, preterm birth, and perinatal problems such as nutrition or environmental factors may increase the risk of ADHD by conditional triggering evidence during perinatal development (Núñez-Jaramillo et al., 2021).
Peripheral pro-inflammatory cytokines, whose concentrations change with increased inflammatory response and decaying the balance between inflammatory anti-inflammatory mechanisms, can access the brain through humoral and neural pathways and maintain inflammatory responses through neuroimmune mechanisms. Changes in pro-inflammatory and anti-inflammatory cytokines have been shown to cause neurotransmission changes in tryptophan metabolism and dopaminergic pathways in the brain similar to those seen in ADHD (Kozłowska et al., 2019). . By activating multiple signaling pathways such as macrophages activated by the activation of microglia, chemokines are proposed to be able to induce the expression of a wide range of natural immune and inflammatory genes by the activation of many different transcription factors (Gustafsson et al., 2020).
It is thought that prenatal exposure to inflammation may hinder brain development, cause structural changes in the volume of gray matter and brain regions such as the prefrontal cortex, anterior cingulate cortex, and corpus callosum, cause permanent neural circuits to fail to mature, or cause neuroendocrine changes and increase the risk of ADHD in children (Buske-Kirschbaum et al., 2013). It is also known that hypothalamic pituitary adrenal (HPA) axis interactions with the chronic increase of immune system cytokine signals in developmental processes are involved in the pathogenesis of ADHD (Chen et al., 2009).
Various cytokines were found not only in the cerebrospinal fluid of children with ADHD but also in peripheral blood samples. Pro-inflammatory activity such as significantly higher IL-6 serum levels has been shown in children with ADHD (Donfrancesco et al., 2020). It supports an increased inflammatory response in adults as well as children with ADHD; levels of pro-inflammatory cytokines and inflammation-related proteins in serum, the presence of infections, and some acquired autoantibodies afterward have been reported (Toto et al., 2015; Oliva et al., 2020). Although the hypothesis that inflammation plays an important role in the pathophysiology of ADHD is supported, it is not enough alone to make a clear comment. A small number of small-sample clinical studies that evaluated different inflammatory variables investigating the role of the immune system in the pathophysiology of ADHD have yielded conflicting results. In addition to consistent findings, there are also studies in the literature that do not report changes in inflammatory parameters (Binici & Kutlu, 2019; Elsadek et al., 2020).
At the same time, although inflammatory cytokines are useful biomarkers, the high costs and limited availability disadvantages of requiring complex processes such as immunoassays to determine their level limit the feasibility of the research. On the other hand, leukocytes and platelets, which can be evaluated from complete blood count parameters, are low cost and widely used markers that play a central role in mediating inflammation, reflecting the dynamic response of the immune system. In the context of inflammation, neutrophils are triggered by the secretion of cytokines and chemokines, such as interleukin-6 (IL-6), tumor necrosis factor (TNF), and myeloid growth factors.
They have key functions in the inflammatory response and neutrophil-lymphocyte ratio (NLR) reflects the balance between innate and adaptive immune responses in many diseases and medical disciplines and chronic low-grade inflammation has been accepted as a standard to evaluate the use in routine clinical practice(Zahorec, 2017). NLR has been elevated in a number of psychiatric disorders, including schizophrenia, depression, and bipolar disorder (Zulfic et al., 2020). White blood cell (WBC), platelet count (PLT), platelet/lymphocyte ratio (PLR), monocyte/lymphocyte ratio (MLR), basophils/lymphocyte ratio (BLR), percentage of monocytes, and red blood cell distribution width (RDW) rates evaluated from peripheral blood are other indicators of inflammation.
Circulating platelets have been proposed as an accessible peripheral biomarker for neuropsychiatric disorders as an alternative model for investigating neuronal dysfunctions (Canobbio, 2019). Shared by neurons and platelets in neuropsychiatric disorders; changes in the metabolism of reelin, amyloid peptides, serotonin, and other proteins and biochemical properties may also be reflected in abnormalities in circulating platelets. Platelets play a critical role in inflammatory and proliferative events by producing and secreting internal membrane proteins, coagulation, and growth factors during the activation process (Ghoshal & Bhattacharyya, 2014).
Platelet/lymphocyte ratio (PLR) is calculated as the ratio of the platelet-lymphocyte count. PLR is a widely used simple marker associated with chronic diseases and infections as well as psychiatric disorders (Mazza et al., 2018). An increase in average platelet volume (MPV) with the activation of platelets was positively associated with more metabolic and enzymatic activity, more pronounced thrombogenic properties, coronary artery disease, and inflammation parameters of CRP (Citirik et al., 2015). MPW platelet volume is determined by the number of megakaryocytes present during platelet production and is associated with platelet function and activation. Normally, the size and number of platelets are inversely proportional.
Platerethritis (PCT) in platelet indices is a measure of the total platelet mass per unit volume of blood. It is determined by the combination of PLT and MPV (PLT × MPV), thus providing more accurate information than PLT or MPV alone (Sahbaz et al., 2016). PCT is a new, simple, inexpensive, and also easily obtainable biomarker of the inflammatory response of change in PLT and MPV levels (Qian et al., 2021).
Although various inflammation and immune-based prognostic scores have been developed using traditional clinicopathological indices, it is known that these scores alone do not comprehensively reflect the balance of inflammatory and immune status. Therefore, a novel index, defined as the systemic immune inflammation index (SII), was developed based on the balance of inflammatory and immune status. SII=P × N/L based on platelet, neutrophil, and lymphocyte counts. (Hu et al., 2014). A high SII appears to be associated with subclinical low-grade inflammation. The importance of the systemic immune inflammation index as an inflammation parameter in prognostic prediction has been demonstrated by meta-analyses in patients with coronary artery disease, patients with acute pulmonary embolism, and patients with solid tumors or multiple cancers (Yang et al., 2020; Gok & Kurtul, 2021; Yang et al., 2018). The low cost, easy determination, and reproducibility of CBC have made SII a promising tool for treatment strategy decisions in clinical practice today.
Confirming the potential role of neuroinflammation in the pathophysiology of ADHD may also be important in opening up new intervention pathways that involve the inflammatory system in treatment. A small number of studies examining the relationship between psychiatric symptomatic and inflammation in children and adolescents have revealed conflicting data on ADHD. As far as we know, routine complete blood count parameters and rates in studies previously conducted to confirm the presence of lifelong subclinical inflammation in adult ADHD; PDW, PCT, and SII have not been evaluated as inflammatory markers. The aim of this study for routine use in adult ADHD patients with new, easy, and peripheral hemogram parameters, which is a cheap option; WBC, NLR, PLR, MLR, BLR, monocyte percentage, RDW, PLT, PDW, PCT, and MPV are associated with increased inflammatory response and ADHD by evaluating whether to investigate. Second, the relationship between different ADHD appearances, variability in symptom severity, impulsivity in particular, and ADHD treatment with systemic inflammatory response levels will be evaluated.
Methods
Participants
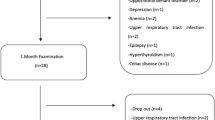
The sample size was calculated as 80% effect size, 5% alfa error, and 20% beta error with the G*power (version 3.1.9.7) program determined power analysis. The subjects included two samples of 74 adults with ADHD (45 men and 29 women) and of 70 healthy controls (36 men and 34 women). The first group which was consisted of 74 adults with ADHD was recruited from outpatients who were admitted to the Psychiatry Clinics of Atatürk University Faculty of Medicine Mental Health and Diseases in December April 2020–September 2021. The control group was formed from individuals who had not been diagnosed with any active psychiatric diagnosis who had been admitted to our outpatient clinic for the purpose of consulting or reporting the situation. The mean age of these two samples were 25.22 years (SD=6.75) and 27.13 years (SD=7.06), respectively. There was no significant difference in mean age (p = 0.099), gender (p= 0.257), or BMI (p= 0.803) decoupling between the groups. The demographic characteristics of the subjects are summarized in Table 1.
Procedure
Our study is focused on prospective and cross-sectional routine CBC analyses of 144 participants. The research protocol of the current observational study was approved by the Research Ethics Committee of Ataturk University (Erzurum, Turkey) and conducted in accordance with the Declaration of Helsinki. Prior to their initial assessment, all subjects gave their written informed consent.
ADHD diagnosis and sub-appearance were determined by the presence of pre-12 age symptoms confirmed by him and his relatives along with a structured clinical interview for the DSM-5-clinician version (SCID-5/CV) by the same psychiatrist. From patients receiving treatment with a diagnosis of ADHD, those who still had symptoms at the diagnostic level were enrolled in the study, and patients who showed partial remission were excluded from the study. Patients who met the diagnostic criteria in the clinical interview, but had active comorbid psychiatric diagnoses, acute and/ or chronic medical or inflammatory disease, and healthy controls were not included in the study. In addition to methylphenidate, ADHD patients receiving treatment were among the criteria for inclusion of newly diagnosed ADHD patients and healthy controls without simultaneous use of any medications. No changes were made to the treatment of patients who were enrolled in the study and did not want to participate in the study.
Obesity (body mass index-BMI>30 kg/m2), hypercholesterolemia, the presence of abnormal vital signs (e.g., fire), the results of a complete blood count abnormal (e.g., anemia, leukopenia), a history of the family immunological disease, and active alcohol, drug, and cigarette use which may affect inflammatory parameters were excluded subjects with. The exclusion of acute conditions was made according to the testimony and symptomatic status of the participants, as well as medical records.
Those who had volunteered their evaluation as a result of research informed written consent were received with similar inclusion criteria for adult ADHD patients without psychiatric or physical illness and the age and gender of the group of 77 and 75 healthy controls formed the study sample.
Blood Samples
The presence of inflammatory disease was re-evaluated by performing physical examinations and vital signs of all participants before blood intake. Blood samples were taken using a vacutainer in the morning after 12 hours of starvation by experienced people from the antecubital area after healthy checks and ADHD patients were provided with a sitting position.
Complete Blood Count Measurement
All blood analyses were performed using an automatic hematological analyzer (Sysmex XN-1000) in the biochemistry Central Laboratory of Ataturk University Hospital. Patients with a Normal hemoglobin value of 12–16 g/dl were evaluated. Normal reference ranges: leukocyte 4.8–10.8 103/mm3, neutrophils 2.06–7.02 103/mm3, lymphocytes 1.3–3.5 103/mm3, platelet 150–450 103/mm3, monocytes 0.3–0.8 103/mm3, eosinophils <0.42 103/mm3, and basophils <0.2 103/mm3 were. Normal NLR values were the following: median 1.8–2.2 (1.00–2.39) in adult population and subclinical inflammation 2.4–2.99% (Zahorec, 2017). Monocyte, RDW, PLT, PDW, PCT, and MPV wer calculated by automatic hematological analyzer. From Hemogram results, SII values were obtained with the formula NLR, PLR, MLR, BLR, and P × N/L by dividing the absolute numbers of the related cells.
Patients with anemia or polycythemia, lymphopenia or lymphocytosis, neutropenia or neutrophilia, and thrombocytopenia or thrombocytosis were also excluded from the study in a complete blood count analysis. A total of 74 adult ADHD patients and 70 healthy controls evaluated at normal limits after assessments and measurements were completed with CBC values.
Measures
Socio-demographic and Clinical Data Form
In the study, a form prepared by the researcher in the light of the literature was used to determine individual characteristics, life routines and clinical characteristics of patients.
DSM-5-Clinician Version (SCID-5/CV) Structured Clinical İnterview for the Structured İnterview
Including questions with detailed diagnostic criteria and diagnostic categories diagnostic category includes only the discovery 32 17 (Osório et al., 2019). Turkish SCID-5/CV validity and reliability study found that Kappa coefficients between 0.65 and 1.00 among interviewers (Elbir et al., 2019). In diagnostic interviews, the patient himself, his family and relatives, his medical records/documents, and the medical team were considered as sources of information. Adult ADHD diagnosis met the DSM-5 diagnostic criterion with five or more symptoms of inattention or hyperactivity/impulsivity resulting in impaired functionality in two or more environments in the clinician’s interview. Adult ADHD is divided into presentations as a combined appearance, an appearance dominated by inattention, and an appearance dominated by excessive mobility and impulsivity. The clinical severity of ADHD was assessed as non-severe, moderate, and severe.
Barratt İmpulsivity Scale-11 (Barratt İmpulse Scale-11, BIS-11)
This is a patient-filled scale used to evaluate impulsivity. It consists of thirty items and has three subscales: attention (inattention and cognitive disorders), motor (motor impulsivity, impatience), and plan (inability to control, cognitive confusion, intolerance). In the BIS-11 evaluation, four different sub-scores are obtained: total score, lack of planning, attention and motor impulsivity. The higher the total BIS-11 score, the higher the person’s level of impulsivity. The Turkish validity and reliability study of BIS-11 was conducted by Güleç et al. (Tamam, Güleç, & Karataş, 2013). Cronbach’s alpha reported for internal consistency in the Turkish version of the scale was 0.81 (patients). The reliability analysis of the entire scale in our study was repeated and it was found to be 0.798 for the patient group.
Data Analyses
Analysis IBM SPSS 20 (version 20, IBM, New York, USA) statistical analysis program software package was used. Data were presented as mean, standard deviation, median, minimum, maximum, percentage, and number. The normal distribution of continuous variables was looked at using the Kolmogorov Smirnov test. Chi-square test was used to evaluate the relationships between categorical variables and student’s t-test was used to compare group means. In the comparisons between two independent groups, the ındependent samples t-test was used when the normal distribution condition was met, and the Mann Whitney u test was used if it was not. Correlation analysis for variables with normal distribution was performed using the Pearson test. A Spearman correlation analysis was performed for variables that did not show a normal distribution. Multiple linear regression analysis was performed to investigate the effect of SII, PCT, and BIS-11 total score independent variables on the clinical severity of attention deficit. The statistical significance level was considered p<0.05.
Results
No statistical difference was found in comparing WBC, NLR, PLR, MLR, BLR, and SII ratios, % monocyte, RDW, PLT, PDW, PCT, and MPV values of ADHD group with healthy controls (p>0.05 for each, see Table 2). There were 6 subjects with NLR>2.39 in adult ADHD and 4 subjects from healthy controls, and there was no statistical significance between the groups for subclinical inflammation (p=0.571).
In the ADHD group, 34 people were receiving methylphenidate treatment, while 40 were newly diagnosed. The combined subtypes was 79.7% (n=59), while 20.3% (n= 15) had predominantly inattentive subtypes. Patients with predominantly hyperactive/impulsively dominant subtype were not included in the study. ADHD clinic, 35.1% (n=26) were non-severe, 39.2% (n=29) were moderate, and 25.7% (n=19) were severe.
The appearance groups in which combined and inattention predominated were similar in terms of gender (p=0.266). Subtype compared (independent samples t test, age (p=0.891), BMI (p=0.484), and token inflammatory blood parameters (WBC, NLR, PLR, MLR, monocyte percentage, RDW, PLT, PDW, PCT, MPV, BLR, and SII for each p>0.05), and there was not a significant difference. In the comparison between newly diagnosed ADHD patients (n=40) and patients receiving methylphenidate (n=34), the mean inflammatory blood parameters were statistically similar (p>0.05 for each, see Table 3).
Socio-demographic characteristics, age, gender, and BMI were evaluated for correlations with inflammatory markers; The age variable showed significant positive correlations with RDW values (r=0.264, p=0.023). Male sex showed significant positive correlations with PCT, MPW, and PLR (r=0.229, p=0.05, r=0.350, p=0.002, r=0.347, p=0.002, respectively). BMI showed a positive correlation with RDW (r=237, p=0.042) and a negative correlation with PRL (r=−292, p=0.012).
The relationship between ADHD clinical symptoms and severity and inflammation was evaluated. A significant negative correlation was observed between attention deficit scores and PCT (r=−0.301**, p=0.009). A positive significant correlation was found between hyperactivity scores and SII (r=0.247*, p=0.034). A significant positive correlation was found between Barrat motor scores and PDW(r=241*, p=0.038). (See Fig. 1a–c). No correlation between attention deficit and impulsivity values and other blood parameters was detected.
A multivariate linear regression analysis was performed to procedural the attention deficit variable using SII, PCT, and BIS-11 total score variables. A meaningful regression model as a result of the analysis F (3.70)= 3.31, p=0.025 and 9% of the variance in the dependent variable (R2 adjusted=.087) was found to be explained by arguments. Accordingly, from the independent variables, the PCT predicts the dependent variable as negative and significant: 33, t (70)= −2.703, p=0.009, pr2=0.094. It was observed that the SII and BIS-11 total score variables did not provide statistical significance in predicting the dependent variable attention deficit (respectively, p=0.322, p=0.164) (see Fig. 2)
Discussion
In this study, we found the averages of WBC, NLR, PLR, MLR, BLR, % monocyte, RDW, PLT, PDW, PCT, MPV, and SII among the adult ADHD group and healthy controls to be similar, but alone it does not support the role of inflammation in ADHD etiology.
Routine Complete Blood Count Analysis in ADHD
According to our reviews in the literature on this childhood-onset disorder, there are no studies conducted in the adult sample. Different from our results in the literature; in the first study investigating peripheral inflammatory markers that can be calculated from routine CBC analysis in children with ADHD, Avcıl et al. reported that the ADHD group’s NLR, PLR, MLR, and neutrophil numbers were significantly higher than those of healthy controls when 82 children with ADHD who did not receive treatment compared with 70 healthy controls (Avcil, 2018). Following Önder et al. in a study conducted by 100 children and adolescents diagnosed with ADHD (85 of whom received treatment) and 99 physically and mentally healthy children, they supported the finding of significantly higher average NLR and PLR rates in patients compared to controls (Önder et al., 2021). Pro-inflammatory and anti-inflammatory cytokines and cytokine neurotrophy were associated with ADHD in children and adolescents compared to the control group in the evaluation of a higher pro-inflammatory L-6, and anti-inflammatory activity which IL-10 cytokine levels revealed (Donfrancesco et al., 2016).
It is not surprising that changes in pro-inflammatory balance obtained due to the variability of individual characteristics of children cannot be shown in adults with ADHD. Again, in the mentioned child and adolescent atudies, comorbid diagnoses were reported at high rates of ADHD in general (Paucke et al., 2018), and neuropsychiatric disorders that have been shown to act in an inflammatory way may also have different results as an artifact of comorbidities. Due to a retrospective model of some studies, the history of acute-chronic infection and autoimmune disease that may affect inflammatory markers may not be clearly evaluated and excluded.
High comorbidity of ADHD is reported in the literature on immune conditions such as recurrent infections, asthma, and type 1 diabetes in both childhood and adulthood (Cortese et al., 2018; Nielsen et al., 2017; Oliva et al., 2020). At the same time, it can be assumed that causes such as daily life routines and the possible confounding effects of BMI may be effective in statistical difference when intra-individual variability is adequately taken into account. Obesity, known to be comorbid with ADHD, has been shown to have moderately elevated SII levels associated with low-grade chronic inflammation (Furuncuoglu et al., 2016). In our study, it was found that RDW and PRL were affected by BMI status, although BMI similarities were found between groups by decimating obesity.
The literature is evaluated in the light of each of these factors. With a methodology similar to our study by Bilici et al. in the study, 65 newly diagnosed children with ADHD aged 6–11 and 65 healthy control groups reported similar NLR and PLR values, supporting our results (Binici & Kutlu, 2019). Although our ADHD group in our study was consistent with the literature in terms of appearance distribution (Wilens et al., 2009), the lack of a patient in our sample and the lack of subjects with increased inflammation may have been instrumental in the change in our results in the appearance of hyperactivity/impulsivity in childhood ADHD presentations.
Blood Parameters and Methylphenidate
In our study, blood parameters did not change decidedly between those who received a new diagnosis in ADHD patients and those who had not yet started medication therapy, and those who took methylphenidate. In the literature on pro- and anti-inflammatory cytokines and cytokine associated with that neurotrophy evaluated in previous studies, such methylphenidate (Mph) psychostimulants, there is some evidence that cytokine levels are lower than in patients who received the drug (Oades et al., 2010). Both low-measured pro-inflammatory and anti-inflammatory cytokine values have been interpreted as the effect of treatment or improved symptomatic on well-controlled cytokine levels.
In human and animal studies, neurodegenerative effects of chronic use of Mph at doses such as 2, 3, and 5 mg/kg have been reported in the literature, in which inflammatory changes in brain cells such as the hippocampus induce apoptosis, oxidative damage, and DNA degradation (Sekine et al., 2008). Mph again, toxic at high doses (10 and 20 mg/kg) for 21 days in acute and chronic animal experiments in brain cells use oxidative and IL-1-β, IL-6, and TNF-α, have been shown to induce the expression of pro-inflammatory cytokines, such as increases and the neurodegeneration (Motaghinejad et al., 2017).
Our study results do not reflect the potential role of Mph therapy as a trigger for the expected inflammatory response. Similar to our results, Önder et al. could not decipher the relationship between psychopharmacological treatment status for ADHD and NLR and PLR rates, which are indicators of inflammation (Önder et al., 2021). Similar rates in the inflammatory parameters in our study results may be associated with the lack of statistical significance of Mph’s role as a trigger for the inflammatory response. Oades et al. (Oades, 2011) considering that the tendency of drug therapy to normalize slight changes in cytokine levels in children with ADHD correlates with clinical well-being; our group receiving drug therapy consists of patients whose clinical improvement has not been achieved while still meeting the diagnostic criteria, which may be effective in the difference in results. At the same time, it should be taken into account that The Mph used in patients does not exceed 1 mg/kg, and the level of peripheral inflammation does not fully reflect the central nervous system.
Blood Parameters and Clinical Symptom Severity or Presentation of ADHD
The effects on the corticosteroid-striatal-cortical network that contribute to the regulation of motor, cognitive, and emotional functions are known in the pathogenesis of ADHD. Within this network, immune-related dysfunction is also thought to exist, and differences in neurophysiological processes can be expressed clinically by different phenotypes (Bluschke et al., 2017). In the literature, no inflammatory changes specific to the clinical severity and presentation of ADHD have been reported to this day (Elsadek et al., 2020). NLR and PLR rates in ADHD patients and the lack of association between platelet marker and total ADHD symptom severity suggested that none of the clinical features had an adequate neurobiological effect on inflammatory markers (Metin et al., 2018; Önder et al., 2021).
Hyperactivity and Systemic Immune Inflammation İndex
This study correlates with clinical symptom severity and different levels of variability in the systemic inflammatory response are considered views; with systemic immune inflammation index (SII), there is a positive correlation between the severity of hyperactivity with weak statistically significance. In the literature, an association has been established between the increase of IL-16, a cytokine with pro-inflammatory activity, and hyperactivity(Oades, 2011). High levels of IL-6 and TNF-α have been associated with the intensity of hyperactivity and inattention, triggering increased levels of norepinephrine as well as decreased levels of dopamine (Oades et al., 2010). In the context of inflammation, neutrophils are triggered by the secretion of cytokines and chemokines, such as interleukin-6 (IL-6), tumor necrosis factor (TNF), and myeloid growth factors. SII was developed based on platelet count and NLR (SII, platelet count × neutrophil/lymphocyte ratio) to simultaneously assess patients’ inflammatory and immune status.
SII’s prognostic significance has been proven in various types of cancer and COVİD infection, superior to inflammation-based indices of different cell counts such as NLR, PLR, or MLR, but similar to CRP. Chronic heart failure is reported to be independently associated with adverse outcomes associated with many diseases, including cancer, metabolic disorders, and cardiovascular disease (Yang et al., 2020). Higher SII before treatment has a high prognostic value, especially for the poorer prognosis of hepatocellular carcinoma patients, and helps to develop clinical treatment strategies (Wang et al., 2020). With increased levels of SII, neutrophils can release large amounts of nitric oxide, arginase, and reactive oxygen species and, as inhibitors of activated T cells, may contribute to the increased apoptosis found in ADHD brains, a hallmark of ADHD (Yun et al., 2014).
It is known that increased inflammation may be associated with the development of psychopathology or resistance to treatment. It is noted that the etiology of ADHD may be very different from patient to patient and that the underlying physiological changes may possibly explain the variation in effect at the point of ADHD treatment effectiveness and treatment resistance (Miller & Raison, 2016; Núñez-Jaramillo et al., 2021). Non-invasive prognostic marker and as a low-cost SIIs the development of psychopathology, as well as on the clinical management of ADHD at the point of treatment response in ADHD symptoms as a marker of effective use, could be considered.
Attention Deficit and Platelets
In our study, there was no significant increase in PLT, MPV, and PCT values in ADHD patients. Abnormal (very low or very high) levels of platelet counts and MPV parameters have also been reported in the literature on psychiatric disorders such as schizophrenia, unipolar depression, and bipolar disorder (Yu et al., 2020; Wysokiński & Szczepocka, 2016). Significantly higher MPV values were also reported in children with ADHD than in the healthy control group (Yorbik et al., 2014). MPV levels have been reported to be significantly higher in Alzheimer’s disease with advanced and moderate cognitive impairment than in early-stage patients (Güzel et al., 2017). MPV levels are based on the fact that young erythrocytes released from the bone marrow during inflammation are volumetric larger than older ones. Metabolic and enzymatic as being activated platelets with a mean platelet volume (MPV) can give information about the course, the increase of inflammation; but with the relationship of CRP levels, the higher volume of low platelets also shrunk in physiologically older MPV has been shown (Sun et al., 2014).
We have not found a statistically significant difference in MPV values; it can be caused by the severity of inflammation and the inability to spend enough time in peripheral blood to cause changes in platelet volumes as a result of Tuesday’s release from the bone marrow or the rate of destruction in the periphery. But our determination of a significant negative relationship between PCT values and the attention deficit variable, and the fact that PCT predicts attention deficit negatively and decisively, shows the importance of inflammatory assessments specific to clinical presentations.
Clinically, adults with ADHD are known to have pronounced symptoms of inattention (LeRoy et al., 2019). Although it is not strong enough to meet the levels of sensitivity and specificity required for routine ADHD diagnosis, our finding suggests that PCT is a largely underestimated parameter in ADHD, a heterogeneous disorder. Low PCT may also indicate increased platelet consumption by coagulation, impaired platelet production, decreased platelet survival time, decreased vascular endothelial growth factor secretion, and impaired serotonergic neurotransmission (Mathew et al., 2018). In ADHD pathogenesis, both serotonin and inflammation hypotheses are platelet-containing hypotheses. This relationship can be evaluated as the active role of platelets in modulation between immune system cells, as in all inflammatory processes, ADHD decays.
According to our reviews in the literature, there has been no publication on PCT change in ADHD. In recent publications evaluating the relationship between diabetic neuropathy and PCT, the correlation of a lower PCT level with a slower nerve conduction rate and a higher rate of diabetic neuropathy has been reported(Qian et al., 2021). Our finding suggests that thrombocytcrit (PCT) has effects on attention and may indicate high expression of subunits that are majorly expressed in α 3 GABA A receptors, and monoaminergic and cholinergic basal forebrain cells, with GABAergic, acetylcholinergic, or any mechanical connection (Mohler, 2007). Genetic studies showing the potential role of inflammation in ADHD suggest that polymorphisms in many small-acting genes associated with inflammatory pathways may provide a genetic predisposition to adult and childhood ADHD (Leffa et al., 2018; Tylee et al., 2018). Considering that platelet-derived growth factor regulates oligodendrocyte progenitor numbers in the adult central nervous system, GABAergic signaling expressed by oligodendrocytes, ADHD may point to the possibility of having a common genetic basis for cognitive changes, including immunological conditions and attention deficit symptoms.
Similar to our results in previous studies, adult ADHD peripheral pro-inflammatory markers, IL-6 and TNF-α primary growth were not seen, although IL-6 and TNF-α, cortisol awakening response, with differences of presentation in the relationship between ADHD and careless of the presence of low basal cortisol levels and HPA activation in response to stress changing the dysfunction of circadian rhythms with different neurobiological profiles that can be united with important conclusions were reached from the presentation (Corominas-Roso et al., 2017). Further research is therefore needed to examine the underlying mechanism and examine refined phenotypes that can reduce heterogeneity, focusing on ADHD presentations, to confirm the association between PCT and attentional deficity.
Impulsivity and PDW
Barrat motor scores with PDW were significantly less positively correlated when the relationship of impulsivity to systemic inflammatory response levels was evaluated. PDW values were significantly higher in a large sample of children and adolescents with ADHD than in the control group (Akıncı & Uzun, 2021). PDW, as a simple and widely used platelet activation index, reflects platelet activation’s change in platelet sizes with morphological changes, including both spherical shape and pseudopodia formation. PDW has been used as a useful marker associated with a high risk of thromboembolic events for autoimmune and inflammatory diseases as well as cardiovascular diseases (Mehrpouri & Satlsar 2020). The critical importance of impulsivity and platelets can be used to identify more effective early intervention programs in the evaluation of candidates for early detection of risky behaviors such as accidents, criminal cases, suicide attempts, and alcohol-substance abuse for affected individuals in ADHD patients.
Evidence that increased immune system activation may be a common pathway in neuroimmune responses to critical effects in neurodegeneration and behavior should be considered with the dimensions of development, treatment, and prevention of ADHD. It is now known that inflammatory changes in the central nervous system are triggered in individuals affected by the severe acute respiratory syndrome coronavirus (COVID-19) pandemic. At the point of preventing psychiatric sequelae of the epidemic and providing anti-inflammatory effects with neuroprotective mechanisms against the risk of ADHD in the next generation, dietary and dietary content of D-vitamin, zinc, iron, magnesium and N-3 PUFA, such as ADHD, such as low rates of elements may be effective (LaChance et al., 2016; Chang et al., 2018). At the same time, do not respond to pharmacological treatments, or for those who suffer the negative effects of this medicine for ADHD patients, the inflammatory system in the path of the opening of a new intervention is more effective with higher response rates and the fewer negative results will help identify new targets for therapeutic development.
The strengths of this study are that ADHD diagnosis is always carried out with a semi-structured interview and supported by a family interview. The study group included a highly selected sample of adults with no psychiatric or acute or chronic organic-inflammatory and autoimmune diseases other than ADHD. As eating lifestyle, the presence of obesity, or habits such as exercise, alcohol, and smoking can also inhibit the expression of inflammatory markers, detailed assessment was provided, risky conditions were excluded in our study, and the similarity of BKI, sports, and heavy exercise situations was achieved. The fact that some of the patient group received new diagnoses and were not treated with ADHD medications provided an advantage for studying the natural course of ADHD. On the other hand, our results from a sample of ADHD with a better trend may not fully reflect the nature of ADHD by excluding psychiatric comorbidities that pose a higher risk of ADHD persistence in adulthood with a structured clinical interview in our study.
Limitations and Future Studies
Our study is not without limitations. The use of possible vitamins and dietary supplements has not been specifically controlled, is cross-sectional, and cannot assess causality. While our exclusion criteria have contributed to the reliability of the current findings, ıt should be taken into account that published studies are still very few and in a small sample to allow for definitive conclusions. Future research in larger samples and focusing on ADHD presentations, using the main biomarkers IL6, IL8, IL10, IL12, TNF, and CRP in parallel with SII and PCT, are needed to draw firm conclusions. Additional studies will therefore be required that take October into account existing limitations on whether the inflammatory markers SII, PLT, and PDW obtained by an easily accessible and feasible method such as CBC can be used as a diagnostic and treatment evaluation parameter in ADHD. We think that it will be possible to increase the level of functionality and quality of life in ADHD patients by revealing inflammatory evaluations specific to ADHD clinical presentations and developing strategies for necessary inflammatory and immune conditions. At the same time, we expect the benefit of increasing our knowledge of inflammatory and immune conditions in terms of preventing life-threatening behavioral problems and comorbidities in the clinical course.
We demonstrated the association of SII, which is independently associated with adverse outcomes in many diseases, and the severity of hyperactivity symptoms in adult ADHD. The fact that PCT predicts attention deficit negatively and decisively shows the importance of inflammatory assessments specific to clinical presentations. The critical importance of platelets in inflammatory processes in ADHD has been demonstrated once again with inflammatory markers such as SII, PLT, and PDW, which can be accessed by an easily applicable complete blood count method.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Ahmed, R., Borst, J. M., Yong, C. W., & Aslani, P. (2014). Do parents of children with attention-deficit/hyperactivity disorder (ADHD) receive adequate information about the disorder and its treatments? A qualitative investigation. Patient Preference and Adherence, 8, 661.
Akıncı, M. A., & Uzun, N. (2021). Evaluation of hematological inflammatory markers in children and adolescents with attentiondeficit/hyperactivity disorder. Clinical Study, 122(4), 256–262.
Association, A. P. (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5®): American Psychiatric Publication.
Avcil, S. (2018). Evaluation of the neutrophil/lymphocyte ratio, platelet/lymphocyte ratio, and mean platelet volume as inflammatory markers in children with attention-deficit hyperactivity disorder. Psychiatry and Clinical Neurosciences, 72(7), 522–530.
Binici, N. C., & Kutlu, A. (2019). Is ADHD an inflammation-related disorder?/DEHB inflamasyonla iliskili bir bozukluk olabilir mi? Anatolian Journal of Psychiatry, 20(3), 313–321.
Bluschke, A., Chmielewski, W. X., Mückschel, M., Roessner, V., & Beste, C. (2017). Neuronal intra-individual variability masks response selection differences between ADHD subtypes—A need to change perspectives. Frontiers in Human Neuroscience, 11, 329.
Buske-Kirschbaum, A., Schmitt, J., Plessow, F., Romanos, M., Weidinger, S., & Roessner, V. (2013). Psychoendocrine and psychoneuroimmunological mechanisms in the comorbidity of atopic eczema and attention deficit/hyperactivity disorder. Psychoneuroendocrinology, 38(1), 12–23.
Canobbio, I. (2019). Blood platelets: Circulating mirrors of neurons? Research and Practice in Thrombosis and Haemostasis, 3(4), 564–565. https://doi.org/10.1002/rth2.12254
Caye, A., Spadini, A. V., Karam, R. G., Grevet, E. H., Rovaris, D. L., Bau, C. H., Rohde, L. A., & Kieling, C. (2016). Predictors of persistence of ADHD into adulthood: A systematic review of the literature and meta-analysis. European Child & Adolescent Psychiatry, 25(11), 1151–1159.
Chang, J. P.-C., Su, K.-P., Mondelli, V., & Pariante, C. M. (2018). Omega-3 polyunsaturated fatty acids in youths with attention deficit hyperactivity disorder: a systematic review and meta-analysis of clinical trials and biological studies. Neuropsychopharmacology, 43(3), 534–545.
Chen, Y.-H., Chen, H., Liu, Y.-Y., Lin, G.-X., Wei, L.-X., & Chen, D.-L. (2009). Function of the hypothalamus-pituitary-adrenal axis in children with attention deficit hyperactivity disorder. (Zhongguo Dang dai er ke za zhi) Chinese Journal of Contemporary Pediatrics, 11(12), 992–995.
Citirik, M., Beyazyildiz, E., Simsek, M., Beyazyildiz, O., & Haznedaroglu, I. (2015). MPV may reflect subcinical platelet activation in diabetic patients with and without diabetic retinopathy. Eye, 29(3), 376–379.
Corominas-Roso, M., Armario, A., Palomar, G., Corrales, M., Carrasco, J., Richarte, V., Ferrer, R., Casas, M., & Ramos-Quiroga, J. A. (2017). IL-6 and TNF-α in unmedicated adults with ADHD: Relationship to cortisol awakening response. Psychoneuroendocrinology, 79, 67–73.
Corona, J. C. (2020). Role of oxidative stress and neuroinflammation in attention-deficit/hyperactivity disorder. Antioxidants (Basel, Switzerland), 9(11), 1039. https://doi.org/10.3390/antiox9111039
Cortese, S., Sun, S., Zhang, J., Sharma, E., Chang, Z., Kuja-Halkola, R., Almqvist, C., Larsson, H., & Faraone, S. V. (2018). Association between attention deficit hyperactivity disorder and asthma: A systematic review and meta-analysis and a Swedish population-based study. The Lancet Psychiatry, 5(9), 717–726.
Donfrancesco, R., Nativio, P., Borrelli, E., Giua, E., Andriola, E., Villa, M. P., & M, D. I. T. (2016). Serum cytokines in paediatric neuropsychiatric syndromes: Focus on Attention Deficit Hyperactivity Disorder. Minerva Pediatrica, 73(5),398–404.
Donfrancesco, R., Nativio, P., Di Benedetto, A., Villa, M. P., Andriola, E., Melegari, M. G., Cipriano, E., & Di Trani, M. (2020). Anti-Yo antibodies in children with ADHD: first results about serum cytokines. Journal of Attention Disorders, 24(11), 1497–1502. https://doi.org/10.1177/1087054716643387
Duan, K., Jiang, W., Rootes-Murdy, K., Schoenmacker, G. H., Arias-Vasquez, A., Buitelaar, J. K., et al. (2021). Gray matter networks associated with attention and working memory deficit in ADHD across adolescence and adulthood. Translational Psychiatry, 11(1), 184. https://doi.org/10.1038/s41398-021-01301-1
Dunn, G. A., Nigg, J. T., & Sullivan, E. L. (2019). Neuroinflammation as a risk factor for attention deficit hyperactivity disorder. Pharmacology, Biochemistry, and Behavior, 182, 22–34. https://doi.org/10.1016/j.pbb.2019.05.005
Elbir, M., Alp Topbaş, O., Bayad, S., Kocabaş, T., Topak, Z., Çetin, Ş., Özdel, O., Ateşçi, F., & Aydemir, Ö. (2019). Adaptation and reliability of the structured clinical interview for DSM-5-disorders-clinician version (SCID-5/CV) to the Turkish language. Türk Psikiyatri Dergisi, 30(1), 1–5.
Elsadek, A. E., Al-Shokary, A. H., Abdelghani, W. E., Kamal, N. M., Ibrahim, A. O., El-Shorbagy, H. H., Suliman, H. A., Barseem, N. F., Abdel Maksoud, Y. H., Azab, S. M., & Nour El Din, D. M. N. (2020). Serum levels of interleukin-6 and tumor necrosis factor alpha in children with attention-deficit hyperactivity disorder. Journal of Pediatric Neurosciences, 15(4), 402–408. https://doi.org/10.4103/jpn.Jpn_1_20
Furuncuoğlu, Y., Tulgar, S., Dogan, A. N., Cakar, S., Tulgar, Y. K., & Cakiroglu, B. (2016). How obesity affects the neutrophil/lymphocyte and platelet/lymphocyte ratio, systemic immune-inflammatory index and platelet indices: A retrospective study. European Review for Medical and Pharmacological Sciences, 20(7), 1300–1306.
Ghoshal, K., & Bhattacharyya, M. (2014). Overview of platelet physiology: İts hemostatic and nonhemostatic role in disease pathogenesis. The Scientific World Journal, 781857. https://doi.org/10.1155/2014/781857
Gok, M., & Kurtul, A. (2021). A novel marker for predicting severity of acute pulmonary embolism: Systemic immune-inflammation index. Scandinavian Cardiovascular Journal, 55(2), 91–96.
Gustafsson, H. C., Sullivan, E. L., Battison, E. A. J., Holton, K. F., Graham, A. M., Karalunas, S. L., Fair, D,A,, Loftis, J.M., Nigg, J. T. (2020). Evaluation of maternal inflammation as a marker of future offspring ADHD symptoms: A prospective investigation. Brain, Behavior, and Immunity, 89, 350-356. doi:https://doi.org/https://doi.org/10.1016/j.bbi.2020.07.019
Güzel, S., Ünal, A., Yıldız, Ö., Oğuz, K., Küçükyalçın, V., Güzel, E. Ç., & Bakkal, E. (2017). Alzheimer Hastalığında Ortalama Trombosit Hacmi Düzeyleri Vasküler Risk Göstergesi Olabilir mi? International Anatolia Academic Online Journal Health Sciences, 1(2).
Hu, B., Yang, X.-R., Xu, Y., Sun, Y.-F., Sun, C., Guo, W., Zhang, X., Wang, W. M., Qiu, S. J., Zhou, J., & Fan, J. (2014). Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clinical Cancer Research, 20(23), 6212–6222.
Instanes, J. T., Halmøy, A., Engeland, A., Haavik, J., Furu, K., & Klungsøyr, K. (2017). Attention-deficit/hyperactivity disorder in offspring of mothers with ınflammatory and Immune system diseases. Biological Psychiatry, 81(5), 452–459. https://doi.org/10.1016/j.biopsych.2015.11.024
Kozłowska, A., Wojtacha, P., Równiak, M., Kolenkiewicz, M., & Huang, A. C. W. (2019). ADHD pathogenesis in the immune, endocrine and nervous systems of juvenile and maturating SHR and WKY rats. Psychopharmacology, 236(10), 2937–2958. https://doi.org/10.1007/s00213-019-5180-0
LaChance, L., McKenzie, K., Taylor, V. H., & Vigod, S. N. (2016). Omega-6 to omega-3 fatty acid ratio in patients with ADHD: a meta-analysis. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 25(2), 87–96.
Leffa, D. T., Torres, I. L. S., & Rohde, L. A. (2018). A review on the role of ınflammation in attention-deficit/hyperactivity disorder. Neuroimmunomodulation, 25(5-6), 328–333. https://doi.org/10.1159/000489635
LeRoy, A., Jacova, C., & Young, C. (2019). Neuropsychological performance patterns of adult ADHD subtypes. Journal of Attention Disorders, 23(10), 1136–1147.
Mathew, B., Srinivasan, K., Pradeep, J., Thomas, T., & Mandal, A. K. (2018). Suicidal behaviour is associated with decreased esterified cholesterol in plasma and membrane fluidity of platelets. Asian Journal of Psychiatry, 32, 105–109. https://doi.org/10.1016/j.ajp.2017.11.023
Mazza, M. G., Lucchi, S., Tringali, A. G. M., Rossetti, A., Botti, E. R., & Clerici, M. (2018). Neutrophil/lymphocyte ratio and platelet/lymphocyte ratio in mood disorders: A meta-analysis. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 84, 229–236.
Mehrpouri, M., & Satlsar, E. S. (2020). Evaluation of platelet parameters in patients with coronary artery disease. Acta Medica Iranica, 58(9), 419–423.
Metin, Ö., Ray, P. C., Shamkhalova, U., Karci, C. K., Tahiroglu, A. Y., & Kaypakli, G. Y. (2018). The Relationship between platelet activation markers and anxiety symptoms in ADHD. Klinik Psikofarmakoloji Bulteni, 28, 113–113.
Miller, A. H., & Raison, C. L. (2016). The role of inflammation in depression: From evolutionary imperative to modern treatment target. Nature Reviews Immunology, 16(1), 22–34.
Möhler, H. (2007). Molecular regulation of cognitive functions and developmental plasticity: İmpact of GABAA receptors. Journal of Neurochemistry, 102(1), 1–12.
Motaghinejad, M., Motevalian, M., Shabab, B., & Fatima, S. (2017). Effects of acute doses of methylphenidate on inflammation and oxidative stress in isolated hippocampus and cerebral cortex of adult rats. Journal of Neural Transmission, 124(1), 121–131.
Nielsen, P. R., Benros, M. E., & Dalsgaard, S. (2017). Associations between autoimmune diseases and attention-deficit/hyperactivity disorder: A nationwide study. Journal of the American Academy of Child & Adolescent Psychiatry, 56(3), 234–240 e231.
Núñez-Jaramillo, L., Herrera-Solís, A., & Herrera-Morales, W. V. (2021). ADHD: Reviewing the causes and evaluating solutions. Journal of Personalized Medicine, 11(3), 166. https://doi.org/10.3390/jpm11030166
Oades, R. D. (2011). An exploration of the associations of pregnancy and perinatal features with cytokines and tryptophan/kynurenine metabolism in children with attention-deficit hyperactivity disorder (ADHD). ADHD Attention Deficit and Hyperactivity Disorders, 3(4), 301–318.
Oades, R. D., Dauvermann, M. R., Schimmelmann, B. G., Schwarz, M. J., & Myint, A.-M. (2010). Attention-deficit hyperactivity disorder (ADHD) and glial integrity: S100B, cytokines and kynurenine metabolism - effects of medication. Behavioral and Brain Functions, 6(1), 29. https://doi.org/10.1186/1744-9081-6-29
Oliva, F., di Girolamo, G., Malandrone, F., Iaia, N., Biasi, F., & Maina, G. (2020). Early childhood infections, antistreptococcal and basal ganglia antibodies in adult ADHD: A preliminary study. BMC Psychiatry, 20(1), 6. https://doi.org/10.1186/s12888-020-02946-w
Önder, A., Gizli Çoban, Ö., & Sürer Adanır, A. (2021). Elevated neutrophil-to-lymphocyte ratio in children and adolescents with attention-deficit/hyperactivity disorder. International Journal of Psychiatry in Clinical Practice, 25(1), 43–48. https://doi.org/10.1080/13651501.2020.1804940
Osório, F. L., Loureiro, S. R., Hallak, J. E. C., Machado-de-Sousa, J. P., Ushirohira, J. M., Baes, C. V. W., Apolinario, T. D., Donadon, M. F., Bolsoni, L. M., Guimarães, T., Fracon, V. S., Silva-Rodrigues, A. P. C., Pizeta, F. A., Souza, R. M., Sanches, R. F., Dos Santos, R. G., Martin-Santos, R., & Crippa, J. A. S. (2019). Clinical validity and intrarater and test–retest reliability of the structured clinical ınterview for DSM-5–Clinician Version (SCID-5-CV). Psychiatry and Clinical Neurosciences, 73(12), 754–760.
Paucke, M., Stark, T., Exner, C., Kallweit, C., Hegerl, U., & Strauß, M. (2018). Attention deficit-hyperactivity disorder (ADHD) and comorbid mental disorders : ADHD-specific self-rating scales in differential diagnostics. Der Nervenarzt, 89(11), 1287–1293. https://doi.org/10.1007/s00115-018-0553-x
Qian, Y., Zeng, Y., Lin, Q., Huang, H., Zhang, W., Yu, H., & Deng, B. (2021). Association of platelet count and plateletcrit with nerve conduction function and peripheral neuropathy in patients with type 2 diabetes mellitus. Journal of Diabetes Investigation, 12(10), 1835–1844. https://doi.org/10.1111/jdi.13535
Sahbaz, A., Cicekler, H., Aynioglu, O., Isik, H., & Ozmen, U. (2016). Comparison of the predictive value of plateletcrit with various other blood parameters in gestational diabetes development. Journal of Obstetrics and Gynaecology, 36(5), 589–593.
Sekine, Y., Ouchi, Y., Sugihara, G., Takei, N., Yoshikawa, E., Nakamura, K., Iwata, Y., Tsuchiya, K. J., Suda, S., Suzuki, K., Kawai, M., Takebayashi, K., Yamamoto, S., Matsuzaki, H., Ueki, T., Mori, N., Gold, M. S., & Cadet, J. L. (2008). Methamphetamine causes microglial activation in the brains of human abusers. Journal of Neuroscience, 28(22), 5756–5761.
Sun, W.-X., Zhang, J.-R., Cao, Z.-g., Li, Y., & Wang, R.-t. (2014). A decreased mean platelet volume is associated with stable and exacerbated asthma. Respiration, 88(1), 31–37.
Tamam, L., Güleç, H., & Karataş, G. (2013). Short form of Barratt ımpulsiveness scale (BIS-11-SF) turkish adaptation study. Archives of Neuropsychiatry, 50(2), 130–134.
Toto, M., Margari, F., Simone, M., Craig, F., Petruzzelli, M. G., Tafuri, S., & Margari, L. (2015). Antibasal ganglia antibodies and antistreptolysin O in noncomorbid ADHD. Journal of Attention Disorders, 19(11), 965–970.
Tylee, D. S., Sun, J., Hess, J. L., Tahir, M. A., Sharma, E., Malik, R., Worrall, B.B., Levine, A.J., Martinson, J.J., Nejentsev, S., Speed, D., Fischer, A., Mick, E., Walker, B.R., Crawford, A., Grant, S.F.A., Polychronakos, C., Bradfield, J.P., Sleiman, P.M.A. . . Glatt, S.J. (2018). Genetic correlations among psychiatric and immune-related phenotypes based on genome-wide association data. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, 177(7), 641-657.
Wang, B., Huang, Y., & Lin, T. (2020). Prognostic impact of elevated pre-treatment systemic immune-inflammation index (SII) in hepatocellular carcinoma: A meta-analysis. Medicine, 99(1), e18571. https://doi.org/10.1097/MD.0000000000018571
Wilens, T. E., Biederman, J., Faraone, S. V., Martelon, M., Westerberg, D., & Spencer, T. J. (2009). Presenting ADHD symptoms, subtypes, and comorbid disorders in clinically referred adults with ADHD. The Journal of Clinical Psychiatry, 70(11), 1557–1562. https://doi.org/10.4088/JCP.08m04785pur
Wysokiński, A., & Szczepocka, E. (2016). Platelet parameters (PLT, MPV, P-LCR) in patients with schizophrenia, unipolar depression and bipolar disorder. Psychiatry Research, 237, 238–245.
Yang, R., Chang, Q., Meng, X., Gao, N., & Wang, W. (2018). Prognostic value of systemic immune-inflammation index in cancer: A meta-analysis. Journal of Cancer, 9(18), 3295–3302. https://doi.org/10.7150/jca.25691
Yang, Y. L., Wu, C. H., Hsu, P. F., Chen, S. C., Huang, S. S., Chan, W. L., Lin, S. J., Chou, C. Y., Chen, J. W., Pan, J. P., Charng, M. J., Chen, Y. H., Wu, T. C., Lu, T. M., Huang, P. H., Cheng, H. M., Huang, C. C., Sung, S. H., Lin, Y. J., & Leu, H. B. (2020). Systemic immune-inflammation index (SII) predicted clinical outcome in patients with coronary artery disease. European Journal of Clinical Investigation, 50(5), e13230.
Yorbik, O., Mutlu, C., Tanju, I. A., Celik, D., & Ozcan, O. (2014). Mean platelet volume in children with attention deficit hyperactivity disorder. Medical Hypotheses, 82(3), 341–345.
Yu, Q., Weng, W., Zhou, H., Tang, Y., Ding, S., Huang, K., & Liu, Y. (2020). elevated platelet parameter in first-episode schizophrenia patients: A cross-sectional study. Journal of Interferon & Cytokine Research, 40(11), 524–529.
Yun, H. S., Park, M. S., Ji, E. S., Kim, T. W., Ko, I. G., Kim, H. B., & Kim, H. (2014). Treadmill exercise ameliorates symptoms of attention deficit/hyperactivity disorder through reducing Purkinje cell loss and astrocytic reaction in spontaneous hypertensive rats. Journal of Exercise Rehabilitation, 10(1), 22–30. https://doi.org/10.12965/jer.140092
Zahorec, R. (2017). Neutrophil-to-lymphocyte ratio. Sixteen-year-long history since publication of our article in Bratislava Medical Journal. Bratislavské Lekárske Listy, 118(6), 321–323. https://doi.org/10.4149/bll_2017_062
Zulfic, Z., Weickert, C. S., Weickert, T. W., Liu, D., Myles, N., & Galletly, C. (2020). Neutrophil–lymphocyte ratio–A simple, accessible measure of inflammation, morbidity and prognosis in psychiatric disorders? Australasian Psychiatry, 28(4), 454–458.
Author information
Authors and Affiliations
Contributions
HAC: designed and executed the study, conducted the data analysis, and wrote the paper. NG: conceptualization of the study and collaboration with the writing of the paper. Both authors collaborated in the writing and editing of the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethical approval was obtained from Ataturk University (Erzurum, Turkey), research ethics committee.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The author delare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ceyhun, H.A., Gürbüzer, N. New Hematological Parameters as Inflammatory Biomarkers: Systemic Immune Inflammation Index, Platerethritis, and Platelet Distribution Width in Patients with Adult Attention Deficit Hyperactivity Disorder. Adv Neurodev Disord 6, 211–223 (2022). https://doi.org/10.1007/s41252-022-00258-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41252-022-00258-6