Abstract
Purpose
Lumbar posterior instrumentation for facet stabilization has become popular for the treatment of lumbar instability. The present study investigated and compared facet stabilization following lumbar posterior instrumentation with facet spacers and facet screws using porcine lumbar spines.
Methods
Eighteen L5–L6 lumbar motion units (LMUs) of the porcine spines were randomly divided into three groups (un-instrumented, facet-spacer and facet-screw). In the un-instrumented group (control), all ligamentous structures were preserved. In the facet-spacer group, two facet spacers were inserted into the joint spaces of the bilateral upper and lower facets. In the facet-screw group, two cannulated screws were used to transfix the bilateral upper and lower facets. With the use of a material testing machine, a gradually increasing moment of up to 6000 N-mm was generated in flexion, extension, lateral bending and torsion motions to compare facet stabilization among the groups.
Results
The facet-spacer group was significantly stiffer than the facet-screw group in extension (p = 0.013), whereas the facet-screw group was significantly stiffer than the facet-spacer group in axial rotation (p = 0.004). No statistically significant differences were observed between the two fixation techniques in flexion (p = 0.284) and lateral bending (p = 0.085).
Conclusion
Both facet-spacer and facet-screw fixation techniques significantly improve stability in a single LMU. Facet-spacer fixation provided better stabilization in extension, while facet-screw fixation provided better stabilization in axial rotation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The pedicle screw fixation technique has been widely accepted in spinal posterior stabilization since the late 1980s [1]. The longevity of pedicle screw fixation as a surgical method has shown clear evidence regarding the efficacy of its application. However, the safety, insertion facility, and subsequent complications of pedicle screw fixation have been debated since its early use. For the adequate placement of pedicle screws, excessive lateral paraspinal muscle retraction has been questioned regarding injury to these muscles and an increase in the extent of devitalized tissue, which may cause an increased incidence of infection and other related complications [2,3,4,5]. Additionally, the possibility of screw malalignment, with the related risks of vascular and neurologic injury and inadequate fixation, has been reported in an extensive body of literature [3, 6,7,8].
The facet screw is one of the alternative techniques for intervertebral stabilization of the lumbar spine, which originates from the early years of spine instrumentation. Facet screws for vertebral fixation were first introduced by Boucher [9]. The facet screw is designed to constrain relative motion at the facet joint using cannulated screws that transfix the bilateral superior and inferior facets. To achieve a rigid spinal construct, two cortical screws are inserted bilaterally from the spinal process of the superior vertebra and passed through the facet joints until they reach the lower vertebra. Following screw insertion, a bone graft is set posteriorly on the bone construction to achieve a rigid bone structure [10,11,12]. In addition to the facet screw, an interfacet allograft spacer capable of packing bone growth-promoting substances such as grafts and synthetic materials into the articular space is a technique that is gaining interest and can lead to an increase in foraminal height by facet distraction [13]. The application of an interfacet spacer not only provides indirect neuroforaminal decompression, but also simultaneously raises the potential for fusion due to a large osteoconductive area and large compressive forces acting on the bone grafts. Consequently, the facet spacer has become an attractive alternative in the treatment of spine disorders due to the aforementioned potential benefits along with the relative ease of surgical procedures [14].
The use of a minimally invasive fixation technique is of substantial interest to the orthopedics field. For degenerative facet joint disease, facet stabilization using facet spacers or facet screws has become popular for the treatment of lumbar instability. The guideline for facet stabilization is to fuse the superior and inferior facets with intra-articular spacers (facet spacers) or to transfix the facet joint with cannulated screws (facet screws). Unlike traditional pedicle screw fixation requiring excessive lateral paraspinal muscle retraction, both facet spacer and facet screw techniques are conducted in a minimally invasive manner.
To the best of the authors’ knowledge, previous reports using in vitro experiments to compare the biomechanical performance of facet spacer and facet screw techniques are lacking. The present biomechanical laboratory study directly evaluated the relative mechanical performance of the facet spacer and facet screw fixation techniques using the LMU porcine lumbar model. The effects of nondestructive static loading involving flexion, extension, lateral bending and axial rotation on lumbar motion segments instrumented with facet spacer fixation were compared with those on lumbar motion segments instrumented with facet screw fixation.
2 Materials and Methods
2.1 Specimen Preparation
This study was approved by the committee of Chang Gung Memorial Hospital of Taiwan. All experiments conformed to the regulations for the care and use of animals.
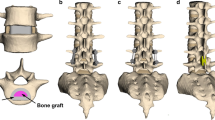
Eighteen (18) fresh lumbar spines from adult pigs (6 months old) were included in the current in vitro study. The specimens were stored at 20 °C until the day of testing. After thawing for 24 h, individual lumbar spines from L5 to L6 were freshly dissected, yielding 18 lumbar motion units (LMUs) (Note that a porcine spine has 7 lumbar vertebrae, and there were 5 in a human spine). Each LMU had two neighboring vertebrae and one intervertebral disc. For each L5–L6 specimen, the surrounding musculature was removed, leaving all ligamentous and bony structures intact, which yielded 18 un-instrumented LMUs. The 18 LMUs were randomly divided into three groups (un-instrumented, facet-spacer and facet-screw). In the un-instrumented group (control, n = 6), all ligamentous structures were preserved. The remaining 12 specimens were then randomly assigned to be instrumented with either a facet spacer (I-Lock, Paonan Corp., Taiwan, top of Fig. 1a) fixation construct (facet spacer group, n = 6) or a facet screw (diameter: 4 mm, length: 40 mm, Paonan Corp., Taiwan, bottom of Fig. 1a) fixation construct (facet screw group, n = 6). In the facet-spacer group (facet spacer fixation: ipsilateral facet fixation from the site of insertion), the facet joint was disrupted, and two facet spacers were inserted into the joint spaces of the bilateral superior and inferior facets (top of Fig. 1b and c, respectively). In the facet-screw group (facet screw fixation: contralateral facet fixation from the site of insertion), two cannulated screws were used to transfix the bilateral superior and inferior facets (bottom of Fig. 1b and c, respectively).
Photographs showing a two fixation devices, b instrumented LMUs and c X-ray images: (top) facet spacer and (bottom) facet screw. In facet-spacer fixation, two facet spacers were inserted into the joint spaces of the bilateral upper and lower facets. In facet-screw fixation, two cannulated screws were used to transfix the bilateral upper and lower facets
2.2 Biomechanical Evaluation
Each LMU was mounted in a customized grip using acrylic resin (AcryliMet, South Bay Technology Inc., San Clemente, CA, USA) along the longitudinal axis. For each LMU, fixation screws were placed in the superior and inferior vertebrae to prevent the specimen from loosening in the acrylic resin. Both the upper and the lower vertebrae were embedded into the acrylic resin to their midbodies. The disc and facet joints were free of acrylic resin and accessible for the application of instrumentation. The lower pot was firmly fixed to the platform of the testing machine. This experimental setup resulted in a compressive preload of 20 N due to the weight of the upper fixation pot. Moments were continuously applied to a maximum of 6000 N-mm [15, 16].
With use of an MTS material testing system (Binix 858, MTS corp., MN, US), each LMU was nondestructively tested without a preload in four sequential modes: flexion, extension, lateral bending and torsion [17]. For all four loading modes, a pure moment of up to 6000 N-mm generated through the MTS actuator was continuously applied to each specimen to achieve the flexion, extension, lateral bending and rotational motions. The grip was designed with a horizontal rotational pin across the upper plate, and the pin was perpendicular to the motion plane of the specimen. The horizontal pin and vertical motion path of the specimen resulted in a 3-D configuration that ensured the specimen achieved a vertical motion as the spinal construct was flexed or extended. In addition, because the specimen used is a porcine lumbar spine with one motion segment, malalignment of LMU motion with the extensometer is less of a concern with the current specimen than with a spinal construct with multilevel segments. The experimental setup of the various loading modes is shown in Fig. 2. For each specimen, the global stiffness of the vertebral constructs was calculated using the moment (torque for axial rotation) versus displacement (angle for axial rotation) curve in all four loading modes. Global stiffness was defined as the slope of the curve at the initial linear phase. For flexion and extension, an additional measurement of intervertebral displacement across the disc was conducted using an MTS extensometer (Model 632-12F-20, MTS Corp. MN, US). The two straight edges of the extensometer crossing the intervertebral disc were anteriorly attached on the upper and lower vertebrae, respectively, to measure anterior intervertebral displacement as the spinal construct was flexed or extended (Fig. 3). The gauge length and resolution of the extensometer were 25.4 and 0.0127 mm, respectively. Using MTS Testar II software, intervertebral displacement values were simultaneously recorded during testing.
Schematic showing the experimental setup of a flexion, b extension, c lateral bending and d axial rotation. For all four loading modes, a pure moment of up to 6000 N-mm generated through the MTS actuator was applied to each specimen to achieve flexion, extension, lateral bending and rotational motions
2.3 Statistical Analysis
All of the measurements were collected and expressed as the mean ± standard deviation (SD). Statistical software (SPSS for Windows version 12.0, SPSS Inc., Chicago, IL) was used to analyze the global stiffness and intervertebral displacement values of all specimens. In the beginning, normal distribution of the sample was examined. ANOVA test with post hoc LSD analysis was performed to evaluate the differences between groups if the data is normally distributed; whereas the Kruskal–Wallis test (Nonparametric statistics) was used to compare the differences between groups if the data is not normally distributed. A significant difference was reported at p < 0.05.
3 Results
3.1 Global Stiffness of the Spinal Constructs
The average global stiffness values of the spinal constructs of the un-instrumented, facet-spacer and facet-screw groups under various motions are shown in Table 1 and Fig. 4. The results demonstrate that both fixation techniques had significantly larger stiffness values in a single lumbar motion unit than in an un-instrumented state under various motions. The facet-spacer group (3034.62 ± 459.28 N-mm/mm) was significantly stiffer than the facet-screw group (2475.31 ± 199.84 N-mm/mm) in extension (p = 0.013), whereas the facet-screw group (5296.77 ± 919.55 N-mm/degree) was significantly stiffer than the facet-spacer group (3750.25 ± 887.72 N-mm/degree) in axial rotation (p = 0.004). No differences were observed between the two fixation techniques in flexion (p = 0.284) and lateral bending (p = 0.085).
Average global stiffness of LMU with an un-instrumented LMU and LMUs with facet-spacer fixation, and facet-screw fixation under various motions (*p < 0.05; +p > 0.05). Both fixation techniques yielded significantly greater stiffness compared with the un-instrumented state. The facet-spacer group was significantly stiffer than the facet-screw group in extension, whereas the facet-screw group was significantly stiffer than the facet-spacer group in axial rotation. No differences in flexion and lateral bending were observed between the two fixation techniques
3.2 Intervertebral Displacements of the Spinal Constructs
The maximal intervertebral displacements under 6000 N-mm were recorded for comparison. Table 2 and Fig. 5 display the intervertebral displacements for the un-instrumented, facet-spacer and facet-screw groups, under the flexion and extension motions. A positive intervertebral displacement value represents an increase in disc height, while a negative value represents a decrease in disc height. Theoretically, a lower absolute value of change in disc height (either positive or negative), corresponds to a more rigid LMU construct, which indicates a more stable overall spinal construct. Under the extension motion, the results reveal that the facet-spacer group exhibited the smallest amount of intervertebral displacement (0.36 ± 0.13 mm) compared with the un-instrumented (0.92 ± 0.23 mm; p < 0.001) and facet-screw groups (0.60 ± 0.11 mm; p = 0.022), whereas the un-instrumented group exhibited the largest amount of displacement (0.92 ± 0.23 mm). Under the flexion motion, however, the absolute value of the intervertebral displacement of the un-instrumented group (− 0.84 ± 0.35 mm) was significantly larger than that of both groups with facet spacers (− 0.19 ± 0.09 mm; p = 0.005) and facet screws (− 0.25 ± 0.21 mm; p = 0.011). Moreover, no differences were found between the groups with facet spacers and facet screws (p = 0.787).
Average intervertebral displacement under 6000 N-mm moment for an un-instrumented LMU and LMUs with facet-spacer fixation and facet-screw fixation under extension and flexion motions (*p < 0.05; +p > 0.05). Under the extension motion, the facet-spacer group exhibited the smallest amount of intervertebral displacement, whereas the un-instrumented group exhibited the largest amount of intervertebral displacement. Under the flexion motion, however, the intervertebral displacement of the un-instrumented group was statistically significantly larger than those of facet-spacer and facet-screw groups. No significant difference was found between the facet-spacer and facet-screw groups (p > 0.05)
4 Discussion
The spinal column is a highly complex and flexible structure that is capable of a large degree of motion in almost all directions. Because of injury, disease or degeneration, vertebral elements such as the laminae, pedicles, spinous process, or facets of one or more vertebrae may become damaged, which prevents the vertebrae from articulating and achieving proper alignment. With vertebral articular surface degeneration, facet joints may show a reduction in cartilage thickness which may degenerate further, leading to complete articular cartilage erosion [18, 19]. One traditional treatment method for facet joint damage is intervertebral stabilization. The aim of intervertebral stabilization is to prevent relative motion between the vertebrae. Inserting an intervertebral device, such as those used in posterior and transforaminal lumbar interbody fusion, may increase the risk for nerve injury, risk for nerve adhesion and the amount of intraoperative bleeding. Consequently, there is a need for spinal implants such as a facet spacer or facet screw that permits greater mobility in individuals with of spinal problems involving only the facet joints. These spinal implants are gaining popularity for lumbar posterior stability because they possess features that allow the packing of bone growth-promoting substances such as grafts and synthetic materials, minimally invasive procedures and easy operations.
Numerous spinal models have been used to study spinal biomechanics. Generally, the application of long segment spinal columns to investigate the biomechanical performance of spinal implants is labor extensive and time-consuming. Consequently, a motion unit of the spinal construct was used in the present study. With regard to the fixation stability of spinal implants, numerous biomechanical reports have been conducted to compare the stabilization performance of the pedicle screw, facet screw and translaminar screw [15, 20, 21]. Kandziora et al. [15] investigated the biomechanical properties of lumbar facet screws using human lumbar spines. Four stabilization techniques were tested: a “stand-alone” cage, a cage with translaminar screws, a cage with facet screws and a cage with pedicle screws. Their results indicate that the facet screw yields initial spinal stability that is similar to that produced by the translaminar screw, but inferior to that produced by the pedicle screw. Ferrara et al. [20] conducted a biomechanical comparison of cyclic loading on lumbar motion segments instrumented with either transfacet pedicle screws or pedicle screws. Their results demonstrated that lumbar motion segments instrumented with transfacet pedicle screws achieved biomechanical stability similar to that of traditional pedicle screws. Deguchi et al. [21] used sheep lumbar spines to biomechanically compare the spinal stability of the translaminar facet joint fixation technique with that of cortical screws and bioabsorbable poly-l-lactide pins and with that of conventional pedicle screw fixation. They concluded that translaminar facet joint fixation with cortical screws shows similar biomechanical performance to that of pedicle screw fixation. Translaminar facet joint fixation with poly-l-lactide pins is significantly less stiff than either type of screw fixation. To our knowledge, although an extensive number of studies have focused on the biomechanical performance of pedicle screws, facet screws and translaminar screws, previous reports addressing the stability performance of facet spacers are lacking.
The extensometer has been widely used as an effective tool to measure relative motion across discs after spinal implant fixation [22,23,24]. In previous studies, Mihara et al. [22] used four extensometers to biomechanically examine whether complete spondylolysis leads to the pathology of the upper adjacent motion segment to the pars defect. Their results show that bilateral pars interarticularis defects increase intervertebral mobility, not only at the involved level but also at the upper level adjacent to the lysis. In 2006, Chen et al. [23] investigated the effect of the absence of interspinous ligament on postoperative spinal stability. Porcine lumbar spines with varying extents of laminectomies (partial laminectomy and complete laminectomy) were investigated. In their study, an extensometer was used to measure intervertebral motion under extension and flexion. The results demonstrate that the intervertebral motion on the adjacent disc is significantly larger with complete laminectomy than with partial laminectomy. An instrumented spine with destructed anchoring point of the interspinous ligament is vulnerable in developing adjacent instability. In 2008, Tai et al. [24] used an extensometer to compare lumbar spine stability between laminectomy and bilateral laminotomy. The results indicate that intervertebral displacements of laminectomy specimens are statistically greater than those of bilateral laminotomy specimens. The authors concluded that a lumbar spine without a supraspinous ligament is more likely to develop segment instability than is a lumbar spine with posterior complex integrity.
In the present study, an extensometer was used to directly measure the intervertebral displacements only in the flexion and extension tests. The extensometer was not applied in the axial rotation and lateral bending tests because the extensometer was limited to measuring linear changes in the length of an object with its special clip-on design. Consequently, only the global displacement of the entire spinal construct can be measured in the axial rotation and lateral bending tests. In these cases, the rigidity of the spinal construct was calculated by the initial slope of the curve of global displacement versus the applied moment. The results from the calculation of the global stiffness indicate that there is no significant difference between the facet-spacer and facet-screw groups in flexion. However, the facet-spacer group was significantly stiffer than the facet-screw group in extension (Fig. 4). These results are consistent with those from the intervertebral displacement measurements (i.e., a smaller intervertebral displacement corresponds to a stiffer spinal construct, Fig. 5). Although both experimental methods (i.e., intervertebral and global displacements) demonstrated that the facet-spacer group presented a higher stiffness than the facet-screw group in extension, the facet-spacer group was significantly less stiff than the facet-screw group in axial rotation (Fig. 4). In extension, the high stiffness of the facet-spacer group may be attributable to a more kyphotic alignment of the spine construct following implantation of facet spacers. From a biomechanics perspective, a more kyphotic alignment of the spine construct might make it more difficult to achieve extension motions. In summary, our results demonstrate that both fixation techniques lead to significantly higher stiffness in a single lumbar motion unit. No statistically significant differences were observed between the facet-spacer and facet-screw groups in flexion and lateral bending. The facet-spacer group had significantly higher stiffness than the facet-screw group in extension but lower stiffness in axial rotation. Placement of the facet spacer can decrease intervertebral displacement, thereby indirectly decompressing the existing nerve roots.
Our work has certain limitations. First, in utilizing a laboratory setting, porcine spines were used as substitutes for human cadaveric spines in this in vitro experimental study. Although the porcine lumbar spine constructs, such as the vertebral posterior elements and the facet joints, are not completely identical to those of actual cadaveric spines, substantial research [23,24,25] has been performed to investigate the biomechanical performance of spinal constructs using porcine lumbar spines as a model for the human spine. Porcine spines may be the most appropriate alternative in conducting biomechanical experiments when human spines are not available. Second, our study is restricted to static loading (flexion, extension, rotation and lateral bending), and other physiological loading conditions were not considered. In daily activities, the entire spinal column involving the screw/bone and spacer/bone interfaces is subjected to complex, dynamic multidirectional loading conditions, and the choice between a facet screw and a facet spacer should be decided with caution. Further investigation into the effects of other loading methods such as dynamic fatigue testing, might be necessary in the future.
5 Conclusion
Both facet-spacer and facet-screw fixation techniques significantly improve stability in a single LMU. Facet-spacer fixation provided better stabilization in extension, while facet-screw fixation provided better stabilization in axial rotation. In addition, placement of the facet spacer significantly decreases intervertebral displacement, particularly in extension, which may be beneficial for spinal decompression.
References
Roy-Camille, R., Saillant, G., & Mazel, C. (1986). Internal fixation of the lumbar spine with 375 pedicle screw plating. Clinical Orthopaedics and Related Research,203, 7–17.
Sanpera, I., Jr., Piza-Vallespir, G., & Burgos-Flores, J. (2014). Upper thoracic pedicle screws loss of fixation causing spinal cord injury. Journal of Pediatric Orthopedics,34(6), e39.
Okuyama, K., Abe, E., Suzuki, T., Tamura, Y., Chiba, M., & Sato, K. (1999). Posterior lumbar interbody fusion: A retrospective study of complications after facet joint excision andpedicle screw fixation in 148 cases. Acta Orthopaedica Scandinavica,70(4), 329–334.
Mehta, S. S., Modi, H. N., Srinivasalu, S., Suh, S. W., Yi, J. W., Cho, J. W., et al. (2009). Pedicle screw-only constructs with lumbar or pelvic fixation for spinal stabilization in patients with Duchenne muscular dystrophy. Journal of Spinal Disorders & Techniques,22(6), 428–433.
Weinstein, J. N., Spratt, K. F., Spengler, D., Brick, C., & Reid, S. (1988). Spinal pedicle fixation: Reliability and validity of roentgenogram-based assessment and surgical factors on successful screw placement. Spine,13, 1012–1018.
Hicks, J. M., Singla, A., Shen, F. H., & Arlet, V. (2010). Complications of pedicle screw fixation in scoliosis surgery: A systematic review. Spine,35(11), E465–E470.
Jutte, P. C., & Castelein, R. M. (2002). Complications of pedicle screws in lumbar and lumbosacral fusions in 105 consecutive primary operations. European Spine Journal,11(6), 594–598.
Lonstein, J. E., Denis, F., Perra, J. H., Pinto, M. R., Smith, M. D., & Winter, R. B. (1999). Complications associated with pedicle screws. Journal of Bone and Joint Surgery American Volume,81, 1519–1528.
Boucher, H. H. (1959). A method of spinal fusion. The Journal of Bone and Joint Surgery,41B, 248–259.
Humke, T., Grob, D., Dvorak, J., & Messikommer, A. (1998). Translaminar screw fixation of the lumbar and lumbosacral spine: A 5-year follow-up. Spine,23, 1180–1184.
Aepli, M., Mannion, A. F., & Grob, D. (2009). Translaminar screw fixation of the lumbar spine: Long-term outcome. Spine,34(14), 1492–1498.
Best, N. M., & Sasso, R. C. (2006). Efficacy of translaminar facet screw fixation in circumferential interbody fusions as compared to pedicle screw fixation. Journal of Spinal Disorders & Techniques,19(2), 98–103.
Tan, L. A., Gerard, C. S., Anderson, P. A., & Traynelis, V. C. (2014). Effect of machined interfacet allograft spacers on cervical foraminal height and area. Journal of Neurosurgery Spine,20(2), 178–182.
Tan, L. A., Straus, D. C., & Traynelis, V. C. (2015). Cervical interfacet spacers and maintenance of cervical lordosis. Journal of Neurosurgery Spine,22(5), 466–469.
Kandziora, F., Schleicher, P., Scholz, M., Pflugmacher, R., Eindorf, T., Haas, N. P., et al. (2005). Biomechanical testing of the lumbar facet interference screw. Spine,30(2), E34–E39.
Serhan, H. A., Varnavas, G., Dooris, A. P., Patwadhan, A., & Tzermiadianos, M. (2007). Biomechanics of the posterior lumbar articulating elements. Neurosurgical Focus,22(1), E1.
Wilke, H. J., Geppert, J., & Kienle, A. (2011). Biomechanical in vitro evaluation of the complete porcine spine in comparison with data of the human spine. European Spine Journal,20(11), 1859–1868.
Fujiwara, A., Tamai, K., An, H. S., Kurihashi, T., Lim, T. H., Yoshida, H., et al. (2000). The relationship between disc degeneration, facet joint osteoarthritis, and stability of the degenerative lumbar spine. Journal of Spinal Disorders,13(5), 444–500.
Park, Y. K., Kim, J. H., Oh, J. I., Kwon, T. H., Chung, H. S., & Lee, K. C. (2002). Facet fusion in the lumbosacral spine: A 2-year follow-up study. Neurosurgery,51(1), 88–95.
Ferrara, L. A., Secor, J. L., Jin, B. H., Wakefield, A., Inceoglu, S., & Benzel, E. C. (2003). A biomechanical comparison of facet screw fixation and pedicle screw fixation: Effects of short-term and long-term repetitive cycling. Spine,28(12), 1226–1234.
Deguchi, M., Cheng, B. C., Sato, K., Matsuyama, Y., & Zdeblick, T. A. (1998). Biomechanical evaluation of translaminar facet joint fixation. A comparative study of poly-l-lactide pins, screws, and pedicle fixation. Spine,23(12), 1307–1312.
Mihara, H., Onari, K., Cheng, B. C., David, S. M., & Zdeblick, T. A. (2003). The biomechanical effects of spondylolysis and its treatment. Spine,28(3), 235–238.
Chen, L. H., Lai, P. L., Tai, C. L., Niu, C. C., Fu, T. S., & Chen, W. J. (2006). The effect of interspinous ligament integrity on adjacent segment instability after lumbar instrumentation and laminectomy—An experimental study in porcine model. Bio-Medical Materials and Engineering,16(4), 261–267.
Tai, C. L., Hsieh, P. H., Chen, W. P., Chen, L. H., Chen, W. J., & Lai, P. L. (2008). Biomechanical comparison of lumbar spine instability between laminectomy and bilateral laminotomy for spinal stenosis syndrome—An experimental study in porcine model. BMC Musculoskeletal Disorders,9(1), 84.
Smit, T. H. (2002). The use of a quadruped as an in vivo model for the study of the spine—Biomechanical considerations. European Spine Journal,11(2), 137–144.
Acknowledgements
This study was supported by the Financial Grant (CMRPD2D0141, CMRPD2D0142) from Chang Gung Memorial Hospital, Taiwan. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors would like to thank the statistical assistance from Shu-Ting Gan, Maintenance Project of the Center for Big Data Analytics and Statistics (Grant No. CLRPG3D0046) at Chang Gung Memorial Hospital.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Liu, MY., Tsai, TT., Chen, LH. et al. Biomechanical Comparison of Lumbar Motion Unit Stability Following Posterior Instrumentation with Facet Spacers and Facet Screws. J. Med. Biol. Eng. 40, 220–229 (2020). https://doi.org/10.1007/s40846-019-00501-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40846-019-00501-x