Abstract
Background
The association of lumbar spine instability between laminectomy and laminotomy has been clinically studied, but the corresponding in vitro biomechanical studies have not been reported. We investigated the hypothesis that the integrity of the posterior complex (spinous process-interspinous ligament-spinous process) plays an important role on the postoperative spinal stability in decompressive surgery.
Methods
Eight porcine lumbar spine specimens were studied. Each specimen was tested intact and after two decompression procedures. All posterior components were preserved in Group A (Intact). In Group B (Bilateral laminotomy), the inferior margin of L4 lamina and superior margin of L5 lamina were removed, but the L4–L5 supraspinous ligament was preserved. Fenestrations were made on both sides. In Group C (Laminectomy) the lamina and spinous processes of lower L4 and upper L5 were removed. Ligamentum flavum and supraspinous ligament of L4–L5 were removed. A hydraulic testing machine was used to generate an increasing moment up to 8400 N-mm in flexion and extension. Intervertebral displacement at decompressive level L4–L5 was measured by extensometer
Results
The results indicated that, under extension motion, intervertebral displacement between the specimen in intact form and at two different decompression levels did not significantly differ (P > 0.05). However, under flexion motion, intervertebral displacement of the laminectomy specimens at decompression level L4–L5 was statistically greater than in intact or bilateral laminotomy specimens (P = 0.0000963 and P = 0.000418, respectively). No difference was found between intact and bilateral laminotomy groups. (P > 0.05).
Conclusion
We concluded that a lumbar spine with posterior complex integrity is less likely to develop segment instability than a lumbar spine with a destroyed anchoring point for supraspinous ligament.
Similar content being viewed by others
Background
Decompression of the spinal canal is currently the standard treatment for degenerative lumbar spinal stenosis. However, studies have shown that total laminectomy increases segmental instability unless fusion is performed [1–4]. Various studies have proposed technical modifications of the standard laminectomy procedure, applicable to the cervical, thoracic and lumbar spines [5–7]. These techniques have evolved from attempts to adequately decompress spinal stenosis in patients while preserving spinal integrity. Technical variations of decompression for lumbar spinal stenosis include unilateral laminotomy, bilateral laminotomy, open-door type laminoplasty and laminectomy.
Clinical studies indicate that neurologic compression occurs most frequently at the level of the interlaminar window. Accordingly, this window has been used to afford adequate decompression by excision of ligamentum flavum, resection of laminar margins and trumpeted "undercutting" techniques of partial facetectomy while maintaining residual lamina, pars and facet joint stability. Neorological decompressions by bilateral laminotomy attempts to maintain spinal columnar stability by preserving the midline structures (spinous process, supraspinous and interspinous ligaments). However, if the midline structures are not partially removed, the trajectory for lateral decompression may be compromised [7, 8]. Therefore, decompressing the ipsilateral foramen and lateral recess requires further facet joint resection, which compromises spinal stability.
A modified technique characterized by bilateral laminotomy and contralateral foraminotomy was described by Weiner [7]. To address the lateral recess osteophyte and ligamentum flavum, the trajectory of Kerrison rongeur crosses the midline under the well-preserved supraspinous ligament. By this procedure, the hypertrophy of the ligamentum flavum and osteophyte formations on the articular facets can then be removed without jeopardizing the integrity of the supraspinous ligament complex and facet joints. Although the clinical result of the Weiner technique is satisfactory, no previous studies have reported the advantages of this modified bilateral laminotomy from a biomechanical perspective. A detailed description of the biomechanical performance of this modified bilateral laminotomy may be helpful in clinical practice. Based on the clinical superiority of the modified bilateral laminotomy in the current study, a further biomechanical examination was performed to evaluate the mechanical behavior of the treated lumbar spine.
Methods
Specimen preparation
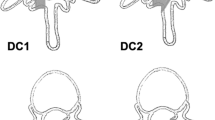
Eight adult porcine lumbar spines (L1–S1) were enrolled in this study. The paraspinal muscles of each specimen were completely excised, and all the ligamentous components, including the supraspinous ligaments, were carefully preserved. Each of the eight porcine lumbar spines was tested in intact form, after bilateral laminotomy and after laminectomy at different levels of decompressive surgery (Fig. 1 and Fig. 2). All posterior components were preserved in the intact group. In the bilateral laminotomy group, fenestration was made on both sides. The inferior margin of L4 lamina and superior margin of L5 lamina were removed by burr, and the L4–L5 ligamentum flavum was undercut. The L4–L5 supraspinous ligament was preserved in all specimens. Finally, in the laminectomy group, the lamina and spinous processes of lower L4 and upper L5 were removed by rongeur and Kerrison clamp. The ligamentum flavum and supraspinous ligament of L4–L5 were also removed. Preservation of bilateral L4–l5 facet joints was confirmed in all specimens.
Lateral View and posterior view of lumbar spine after (A) laminectomy and (B) bilateral laminotomy. In laminectomy, the lamina and spinous processes of lower L4 and upper L5 are removed by rongeur and Kerrison clamp. The ligamentum flavum and supraspinous ligament of L4–L5 are removed. In laminotomy, fenestration is made on both sides. The inferior margin of L4 lamina and superior margin of L5 lamina are removed by burr. The L4–L5 ligamentum flavum is removed.
Biomechanical Test
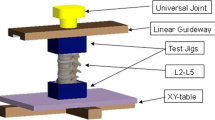
The specimens were mounted for biomechanical testing by MTS (Bionix 858, MTS Corp., MN, USA). A specially designed fixture used to increase moment up to 8400 N-mm generated through the axial movement of the MTS actuator was applied to each specimen to achieve the flexion and extension motions. During testing, intervertebral displacement at decompression levels L4–L5 was recorded continuously by MTS extensometer (Model 632-12F-20, MTS Corp., US). Gauge length and resolution of the extensometer was 25.4 mm and 0.0127 mm, respectively. During testing, intervertebral displacement data were simultaneously recorded by MTS Testar II software. Six intervertebral displacement measurements of L4–L5 lumbar segment were performed in each porcine specimen. 1) Intact under flexion; 2) Intact under extension; 3) Bilateral laminotomy under flexion; 4) Bilateral laminotomy under extension; 5) Laminectomy under flexion; 6) Laminectomy under extension. For specimens with bilateral laminotomy, following the measurements of intact, bilateral laminotomy was performed by fenestration on both sides of lamina. The inferior margin of L4 lamina, superior margin of L5 lamina and the L4–L5 ligamentum flavum were removed. For specimens with laminectomy, following the measurements of bilateral laminotomy, laminectomy was performed by removal of the lamina and spinous processes of lower L4 and upper L5. The ligamentum flavum and supraspinous ligament of L4–L5 were also removed. All measurements were carried out using identical testing procedures. The stability of the lumbar spine in intact form, after bilateral laminotomy and after laminectomy were evaluated by comparing data for intervertebral displacement between L4–L5. Fig. 3 illustrates the experimental setup.
Photograph of the (A) experimental setup for measuring intervertebral displacement and (B) flexion motion of intact lumbar spine. By using a specially designed fixture, an 8,400 N-mm constant moment generated through the axial movement of the MTS actuator was applied to the spine specimen to achieve flexion and extension motions. Intervertebral displacement at L4–L5 adjacent to the fusion level was recorded continuously using an MTS extensometer.
Results
Fig. 4 illustrates the typical intervertebral displacement versus applied moment on decompressive segment under flexion motion. The curve pattern demonstrates that the intervertebral displacement of the decompressive segment decreased significantly with the increasing flexion moment in the early period. However, the decreasing rate (slope) decreased gradually with increasing flexion moment.
A diagram of a typical intervertebral displacement versus applied moment on the decompressive segment under flexion motion. The curve pattern demonstrates a significant decrease in intervertebral displacement of the decompressive segment as flexion moment increases in the early period. However, the rate (slope) gradually decreased as flexion moment increased.
The maximal intervertebral displacement under conditions of 8400 N-mm were recorded for analysis. Table 1 and Fig. 5 display intervertebral displacements in decompression segment (L4–L5) for each of the three decompressive procedures under flexion and extension motions. The positive value represents the increased intervertebral displacement, while the negative value represents the decreased displacement. Theoretically, the higher the absolute value of change in disc height (either positive or negative), the less rigid the system, indicating a less stable overall spinal construct. Under extension motion, the facet joints locked and prevented posterior vertebral displacement. The moment increased rapidly to the end point of 8400 N-mm. The experimental results revealed no statistical difference in intervertebral displacement among the three different decompressive procedures (P > 0.05).
Under flexion motion, however, the intervertebral displacement of the decompression segment (L4–L5) with complete laminectomy was statistically greater than those of intact or bilateral laminotomy (P = 0.0000963 and P = 0.000418, respectively). Moreover, no difference was found between groups with intact and bilateral laminotomy (P > 0.05).
Discussion
Spinal stenosis is a common disease, and several decompressive procedures for this condition are becoming more common in the practice of spinal surgery. Pathologic changes include bony spurs on the vertebral bodies, posterior protrusion of the intervertebral discs, hypertrophy of the ligamentum flavum and osteophyte formation on the articular facets [9–11]. Total laminectomy is currently the standard approach for degenerative lumbar spinal stenosis with a success rate reportedly as high as 85% to 90% [9, 12]. However, the clinical effectiveness of laminectomy diminishes over time [13]. Many studies have shown that total laminectomy produces segmental instability unless fusion is performed [1–4]. Postacchini et al [12] compared multiple laminotomy and total laminectomy in sixty-seven clinical cases. Postoperative vertebral instability was rare in patients undergoing multiple laminotomy as compared with those who underwent total laminectomy. As the frequency of decompressive surgery for this condition increases, the ideal procedure will be one combining maximum canal and foraminal decompression with minimal resection of critical bony structures and supporting ligaments.
Intervertebral displacement of L3–L4 segment under flexion and extension motions (8400 N-mm). Intervertebral displacement between three different decompressive procedures under extension motion did not significantly differ (P > 0.05). However, under flexion motion, intervertebral displacement in the laminectomy group was statistically higher than in the intact or bilateral laminotomy groups (P < 0.05).
Most surgical approaches to decompression involve excision of the interspinous or supraspinous ligament complexes, altering an already pathologic biomechanical milieu. Goel et al [14, 15] found that, under normal conditions, the supraspinous ligament received the greatest force when exposed to an external flexion moment across an anatomic segment. Kanayama et al [16] observed similar findings and suggested that, in regions lacking this ligamentous support, the paraspinal musculature provides compensatory stability. Resection of portions or all of the spinous processes, interspinous ligaments and supraspinous ligaments as well as iatrogenic damage to the paraspinal musculature excessively increases the volume of dead space [17]. Dead space and its consequent risks are significantly decreased using bilateral laminotomy instead of laminectomy. Preservation of the spinous processes and inter-/supraspinous ligamentous complex maintains the normal posterior median furrow, which would be lost using other more invasive techniques.
Numerous investigations have used the extensometer as an in vitro tool to test motion across discs after pedicle screw fixation [18–20]. Gurr et al [18] simulated spinal instability after anterior corpectomy for treatment of a fracture in a calf-spine model, and four types of posterior instrumentation were compared by measurement of intervertebral displacement across the corpectomy using an anterior extensometer. Shono et al [19] performed an in vitro biomechanical analysis of three anterior instability patterns on calf lumbosacral spines. Stiffness of the constructs and segment motion were compared by extensometer. Shono concluded that as segmental spinal instrumentation progresses from one level to three levels, overall rigidity of the system increases. Recently, Chen et al [20, 21] investigated the effect of sagittal alignment on adjacent joint mobility after lumbar instrumentation in a porcine model. An anterior extensometer was used to compare the difference in intervertebral displacement of adjacent segments among instrumented lumbar spines in intact, lordotic and kyphotic alignment. The experimental results demonstrated that an instrumented spine in lordosis is less likely to develop adjacent instability than a kyphotic spine. In the present study, differences in intervertebral displacement between intact, bilateral laminotomy and laminectomy groups were compared by extensometer, and the relative differences of segmental instability after different decompressive procedures were thus examined.
In this study, the applied moment increased as applied loading increased. The maximal moment was preset at 8400 N-mm, which stopped the motion of flexion or extension when the moment reached the preset value of 8400 N-mm. Under extension motion, the facet joints locked and prevented posterior vertebral displacement, which caused the moment to increase rapidly to the end point of 8400 N-mm. This phenomenon was observed in all three groups. Under flexion motion, however, intervertebral displacement of the decompressive segment (L4–L5) in the laminectomy group was statistically greater than in the intact or bilateral laminotomy groups. Theoretically, this induces the greatest stress on the decompressive segment and leads to the degenerative acceleration of the decompressive segment following laminectomy despite preservation of the facet joint. The present results indicate that deconstruction of the anchor point for the supraspinous ligament might cause severe segmental instability after a decompressive procedure. The results also suggest that bilateral laminotomy is generally effective in lumbar spine decompressive surgery.
Although efforts have been made to simulate the clinical conditions, there are certain limitations to this study. First, under laboratory environment, this experimental study use porcine lumbar spine instead of human cadaveric spines. Although physiological structures such as spinal alignment, number of lumbar segments of the porcine spines are somewhat different from those of human cadaveric spines, however, animal spines are the most convenient choice to perform the experiment with long spinal segments on circumstance that human cadaveric spines can not be accessed. Numerous researches [22–28] have been done to evaluate the biomechanical behaviors of spinal column with use of porcine lumbar spines as a model for the human spine. Smit's report [22] had shown similarity in the mechanics of quadruped and human. He concluded that a quadruped can be a valuable model for the study of the spine in spite of its horizontal position. An important point of difference is the higher axial compression stress in quadrupeds, which leads to higher bone densities in the vertebrae. Second, unlike a constant bending moment across the spinal levels performed by Smith et al, who investigated the effects of surgical modification upon the canine lumbosacral spine using four-point bending [29], this study use an eccentrically applied compressive force to spinal segments, which results in a different load state at each spinal level as described in Kostuik and Smith [30]. From a biomechanical point of view, an applied eccentric load will lead to different loads at each spinal level since the load at an individual spinal level depend on the flexibility of the spine. For example, the applied moment will be proportional to the applied load and the moment arm, and this moment arm increases as the specimen flexibility increases. Therefore, the eccentrically applied moment will vary due to the change of specimen stiffness resulted from different surgical reconstruction procedures. Nevertheless, although the loading mode does not necessarily represent the actual physiological loading condition and may have great impact on the clinical relevance, the specimens in this study were all prepared and tested in a uniform and reproducible manner and we believe that these results provide useful information to orthopedic surgeons in performing decompressive surgery for lumbar spinal stenosis. Third, the loading conditions considered were only motion in saggital plane (flexion and extension). Further investigation on the effects of other loading conditions such as lateral bending and axial rotation might be necessary in the future.
Conclusion
In this study, intervertebral displacement of the lumbar spine following laminectomy was significantly greater than that of the lumbar spine in intact form or following bilateral laminotomy. The abnormal stress on the decompressive segment causes spinal instability treated with laminectomy. Therefore, the integrity of posterior complex (spinous process-supraspinous ligament-spinous process) acts as a tension band in flexion and helps stabilize the decompressive spine. Destruction of the supraspinous ligament may jeopardize this stability of the decompression segment. If the integrity of the posterior complex is completely destroyed by the decompression approach, it is more likely to develop segmental instability. To conclude, bilateral laminotomy presents a more stable performance as compared to the traditional laminectomy in decompressive surgery.
References
Hopp E, Tsou PM: Postdecompression lumbar instability. Clin Orthop. 1988, 227: 143-151.
Johnsson KE, Willner S, Johnsson K: Postoperative instability after decompression for lumbar spinal stenosis. Spine. 1986, 11 (2): 107-110. 10.1097/00007632-198603000-00001.
Katz JN, Lipson SJ, Larson MG: The outcome of decompressive laminectomy for degenerative lumbar stenosis. J Bone Joint Surg Am. 1991, 73 (6): 809-816.
Lu WW, Luk KD, Ruan DK, Fei ZQ, Leong JC: Stability of the whole lumbar spine after multilevel fenestration and discectomy. Spine. 1999, 24 (13): 1277-1282. 10.1097/00007632-199907010-00002.
Herron LD, Pheasant HC: Bilateral laminotomy and discectomy for segmental lumbar disk disease. Decompression with stability. Spine. 1983, 8 (1): 86-97. 10.1097/00007632-198301000-00015.
Lee TT, Manzano GR, Green BA: Modified open-door cervical expansive laminoplasty for spondylotic myelopathy: Operative technique, outcome, and predictors for gait improvement. J Neurosurg. 1997, 86 (1): 64-68.
Weiner BK, Walker M, Brower RS, McCulloch JA: Microdecompression for lumbar spinal canal stenosis. Spine. 1999, 24 (21): 2268-2281. 10.1097/00007632-199911010-00016.
Sharma M, Langrana NA, Rodriguez J: Role of ligaments and facets in lumbar spinal stability. Spine. 1995, 20 (8): 887-900. 10.1097/00007632-199504150-00003.
Fox MW, Onofrio BM, Hanssen AD: Clinical outcomes and radiological instability following decompressive lumbar laminectomy for degenerative spinal stenosis: A comparison of patients undergoing concomitant arthrodesis versus decompression alone. J Neurosurg. 1996, 85 (5): 793-802.
Grob D, Humke T, Dvorak J: Degenerative lumbar spinal stenosis: Decompression with and without arthrodesis. J Bone Joint Surg Am. 1995, 77 (7): 1036-1041.
Mayer RS, Chen IH, Lavender SA, Trafimow JH, Andersson GB: Variance in the measurement of sagittal lumbar spine range of motion among examiners, subjects, and instruments. Spine. 1995, 20 (13): 1489-1493. 10.1097/00007632-199507000-00008.
Postacchini F, Cinotti G, Perugia D, Gumina S: The surgical treatment of central lumber stenosis. Multiple laminotomy compared with total laminectomy. J Bone Joint Surg Br. 1993, 75 (3): 386-392.
Ensink FB, Saur PM, Frese K, Seeger D, Hildebrandt J: Lumbar range of motion: influence of time of day and individual factors on measurements. Spine. 1996, 21 (11): 1339-1343. 10.1097/00007632-199606010-00012.
Goel VK, Fromknecht SJ, Nishiyama K, Weinstein J, Liu YK: The role of the lumbar spinal elements in flexion. Spine. 1985, 10 (6): 516-523. 10.1097/00007632-198507000-00005.
Goel VK, Goyal S, Clark C, Nishiyama K, Nye T: Kinematics of the whole lumbar spine: Effect of discectomy. Spine. 1985, 10 (6): 543-554. 10.1097/00007632-198507000-00008.
Kanayama M, Abumi K, Kaneda K, Tadano S, Ukai T: Phase lag of the intersegmental motion in flexion-extension of the lumbar and lumbosacral spine: an in vivo study. Spine. 1996, 21 (12): 1416-1422. 10.1097/00007632-199606150-00004.
Mayer TG, Vanharanta H, Gatchel RJ, Mooney V, Barnes D, Judge L, Smith S, Terry A: Comparison of CT scan muscle measurements and isokinetic trunk strength in postoperative patients. Spine. 1989, 14 (1): 33-36. 10.1097/00007632-198901000-00006.
Gurr KR, McAfee PC, Shih CM: Biomechanical analysis of anterior and posterior instrumentation systems after corpectomy. J Bone Joint Surg Am. 1988, 70 (8): 1182-1191.
Shono Y, Kaneda K, Abumi K, McAfee PC, Cunningham BW: Stability of posterior spinal instrumentation and its effects on adjacent motion segments in the lumbosacral spine. Spine. 1998, 23 (14): 1550-1558. 10.1097/00007632-199807150-00009.
Chen WJ, Lai PL, Tai CL, Chen LH, Niu CC: The Effect of sagittal alignment on adjacent joint mobility after lumbar instrumentation – a biomechanical study of lumbar vertebrae in a porcine model. Clin Biomech. 2004, 19 (8): 763-768. 10.1016/j.clinbiomech.2004.05.010.
Chen LH, Lai PL, Tai CL, Niu CC, Fu TS, Chen WJ: The effect of interspinous ligament integrity on adjacent segment instability after lumbar instrumentation and laminectomy – an experimental study in porcine model. Biomed Mater Eng. 2006, 16 (4): 261-267.
Smit TH: The use of a quadruped as an in vivo model for the study of the spine – biomechanical considerations. Eur Spine J. 2002, 11 (2): 137-144. 10.1007/s005860100346.
Asazuma T, Stokes IAF, Moreland MS, Suzuki N: Intersegmental spinal flexibility with lumbosacral instrumentation – an in vitro biomechanical investigation. Spine. 1990, 15 (11): 1153-1158. 10.1097/00007632-199011010-00013.
Gillespie KA, Dickey JP: Biomechanical role of lumbar spine ligaments in flexion and extension: determination using a parallel linkage robot and a porcine model. Spine. 2004, 29 (11): 1208-1216. 10.1097/00007632-200406010-00010.
Gurwitz GS, Dawson JM, McNamara MJ, Federspiel CF, Spengler DM: Biomechanical analysis of three surgical approaches for lumbar burst fractures using short-segment instrumentation. Spine. 1993, 18 (8): 977-982. 10.1097/00007632-199306150-00005.
Kaigle A, Ekstrom L, Holm S, Rostedt M, Hansson T: In vivo dynamic stiffness of the porcine lumbar spine exposed to cyclic loading: influence of load and degeneration. J Spinal Disord. 1998, 11 (1): 65-70. 10.1097/00002517-199802000-00010.
Kostuik JP, Munting E, Valdevit A: Biomechanical analysis of screw load sharing in pedicle fixation of the lumbar spine. J Spinal Disord. 1994, 7 (5): 394-401. 10.1097/00002517-199410000-00005.
Russell GR, Lavoie G, Evenson R, Moreau M, Budney D, Raso VJ: A reproducible porcine vertebral fracture for biomechanical testing of spinal fixation devices. Clin Orthop. 1992, 284: 267-272.
Smith MEH, Bebchuk TN, Shmon CL, Watson LG, Steinmetz H: An in vitro biomechanical study of the effects of surgical modification upon the canine lumbosacral spine. Vet Comp Orthop Traumatol. 2004, 17 (1): 17-24.
Kostuik JP, Smith TJ: Pitfalls of biomechanical testing. Spine. 1991, 16 (10): 1233-5. 10.1097/00007632-199110000-00017.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2474/9/84/prepub
Acknowledgements
The authors would like to thank the National Science Council of the Republic of China for the financially supporting this research under Contract No. NSC93-2213-E-182A-002.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
C–LT participated in the study design, in collecting the data, the statistically analyses and drafting of the manuscript. P–HH, W–PC, L–HC and W–JC participated in the study design. P–LL advised and assisted drafting of the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Tai, CL., Hsieh, PH., Chen, WP. et al. Biomechanical comparison of lumbar spine instability between laminectomy and bilateral laminotomy for spinal stenosis syndrome – an experimental study in porcine model. BMC Musculoskelet Disord 9, 84 (2008). https://doi.org/10.1186/1471-2474-9-84
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2474-9-84