Abstract
Introduction
To compare the efficacy of abatacept and tumor necrosis factor inhibitor (TNFi) in patients with anti-citrullinated protein antibody (ACPA)-positive rheumatoid arthritis (RA) and identify those who benefit most from abatacept over TNFi.
Methods
This observational study identified RA patients who were ACPA-positive and initiated abatacept or TNFi from the Korean College of Rheumatology Biologics and Targeted therapy registry. Propensity score (PS) matching was performed to balance baseline confounding in abatacept- or TNFi-treated patients. The major endpoints were changes in Clinical Disease Activity Index (CDAI) and achievement of CDAI remission/low disease activity after 1 year of treatment. Subgroup analysis was mainly performed stratified by prior biologics use.
Results
A total of 291 PS-matched, ACPA-positive RA patients who initiated abatacept (n = 97) and TNFi (n = 194) were included. From baseline CDAI scores of 26.52 in the abatacept group and 26.38 in the TNFi group, the mean changes after 1 year were − 16.78 and − 13.61, respectively (difference − 3.17, p = 0.020). The proportion of patients achieving CDAI remission/low disease activity was 68.0% with abatacept and 52.6% with TNFi (p = 0.013). In the subgroup analysis, patients that were biologics-naïve had better improvement in CDAI after treatment with abatacept than TNFi (difference − 3.35, p = 0.021).
Conclusions
This real-world study suggests that abatacept may have better clinical response compared to TNFi in patients with established ACPA-positive RA, especially in those that were biologics-naïve.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Patients with rheumatoid arthritis (RA) who are anti-citrullinated protein antibody (ACPA)-positive have been shown to respond better to abatacept and rituximab than patients who are ACPA-negative. Yet, the evidence regarding comparative efficacy of biologic agents stratified by patient’s ACPA serostatus is very limited in Asian patients with RA. |
What was learned from the study? |
This real-world study, based on the Korean nationwide biologic registry, reveals that abatacept-treated ACPA-positive patients may have better clinical outcomes at 1 year than those treated with a TNF inhibitor, especially in biologics-naïve patients. These findings suggest that ACPA serostatus could guide treatment decisions in selecting biologic therapy for Asian RA patients with active disease. |
Introduction
Rheumatoid arthritis (RA) is a chronic immune-mediated disease characterized by synovial inflammation that leads to joint damage [1]. Over the past two decades, the advent of biological disease-modifying antirheumatic drugs (bDMARDs) and Janus kinase (JAK) inhibitor has improved the outlook for treatment of RA [2]. Although both classes of drugs have been approved for the treatment of active RA after unsuccessful treatment with conventional synthetic DMARD (csDMARD), determining the optimal drug for a particular patient remains a challenge. Due to the limited differences in overall efficacy between bDMARDs [3, 4], the current American College of Rheumatology (ACR) or European League Against Rheumatism (EULAR) guidelines for the treatment of RA still do not specify which patients should receive which bDMARD treatment at the start or switch [5, 6]. Furthermore, classical clinical trials of RA have shown common limits of therapeutic response that are difficult to overcome, regardless of drugs [7]. In this regard, it is necessary to compare the efficacy of bDMARD after stratifying patients according to specific predictors of therapeutic response and non-response to establish the optimal strategy for RA. A recent randomized controlled trial has shown different treatment response to rituximab compared to tocilizumab, depending on subgroups stratified by synovial tissue-based biomarkers [8].
Abatacept, a fusion protein of cytotoxic T-lymphocyte antigen-4 (CTLA-4) and Fc portion of an immunoglobulin (Ig) G molecule, binds to the costimulatory ligands CD80 and CD86 and blocks their interaction with CD28 expressed by T cells, resulting in inhibition of T cell co-stimulation [9]. In addition to inhibitory effect on cytokine production by macrophage [10], abatacept interferes with the stimulation of T follicular helper cells, thereby blocking the T cell–B cell interaction for autoantibody production [11]. Notably, some patients with early RA became autoantibody-negative after treatment with abatacept in clinical trials [12]. In line with the mode of action of abatacept, previous studies showed that anti-citrullinated protein antibody (ACPA)-positive patients responded significantly better to abatacept [13, 14] and had improved drug retention compared to ACPA-negative patients [15, 16]. Similar to abatacept, a meta-analysis found that seropositive patients responded significantly better to rituximab than seronegative patients [17]. On the other hand, no association between ACPA serostatus and clinical outcomes with tumor necrosis factor inhibitor (TNFi) has been identified [18, 19]. Nevertheless, the comparative efficacy between bDMARDs in patients stratified by ACPA serostatus remains unclear. Previous data from the United States (US) Corrona registry showed similar clinical outcomes between abatacept and TNFi in patients with ACPA-positive RA [20]. Post hoc analysis of the AMPLE trial indicated that abatacept tended to respond better than adalimumab in bDMARD-naïve patients with early, seropositive, erosive RA [21]. However, due to the observational nature of the studies, different study population, and limited data on ACPA titers, it is still difficult to draw clear conclusions about groups in which abatacept is preferable to other drugs.
Thus, the aim of this study was to compare the efficacy of abatacept and TNFi in patients with ACPA-positive RA and identify factors associated with the patients who most benefit from abatacept over TNFi, using a large nationwide registry.
Methods
Patients
The analysis of this observational cohort study was conducted using the Korean College of Rheumatology Biologics and Targeted therapy (KOBIO) registry database (NCT01965132). The KOBIO registry was established in Dec 2012 and contains nationwide, multicenter data on patients with RA, ankylosing spondylitis, and psoriatic arthritis who are receiving bDMARD with the aim of providing a long-term safety profile of bDMARD in Korean patients. Biologic agents included rituximab, abatacept, tocilizumab, etanercept, infliximab, adalimumab, and golimumab. The registry has enrolled new bDMARD users at initiation regardless of their previous exposure to bDMARD. Demographic, clinical, laboratory, and functional data of enrolled patients were prospectively recorded at baseline (at the time of new bDMARD initiation) and annual visits [22]. Besides, data were collected when the patients switched or discontinued bDMARD during the follow-up period.
Among the patients enrolled in the KOBIO registry, those aged 18 years or older who were diagnosed as RA, positive for ACPA, and started abatacept or TNFi treatment between Dec 2012 and Oct 2017 were included in this study. All patients met the 2010 ACR-EULAR classification criteria for RA [23]. ACPA positivity was defined according to the result of the anti-cyclic citrullinated peptide (anti-CCP) assay performed at each center. For example, ACPA titer levels were considered positive at greater than 5.0 U/ml at the Boramae Medical Center (BMC). Patients were excluded if they had a history of ankylosing spondylitis or psoriatic arthritis, or had no 1-year follow-up data. This study was conducted in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice guidelines. All included patients provided written informed consent upon enrolment into the KOBIO registry. The study protocol was approved by the institutional review boards at BMC (26-2012-34).
Study Design and Data Collection
The ACPA-positive RA patients were assigned to two treatment groups based on the type of bDMARD initiated; the abatacept group and the TNFi group. Abatacept-treated patients with prior exposure to a TNFi were excluded from the TNFi group. Due to the heterogeneity of baseline characteristics between the two groups, therapeutic efficacy was compared in a propensity score (PS)-matched population. Baseline was defined as the start date of each bDMARD (abatacept or TNFi). No dose reduction or increase in dose interval of abatacept or TNFi was observed during the first year of treatment. Both intravenous infusion and subcutaneous injection form of abatacept were included. The concomitant use of csDMARD, corticosteroids, and non-steroidal anti-inflammatory drugs was determined by the attending rheumatologist of each center.
Data were extracted from the KOBIO registry database at baseline and after 1 year of treatment. Baseline data included age, sex, disease duration, education level, smoking status, body mass index, swollen and tender joint counts, physician’s global assessment, patient’s global assessment, C-reactive protein (CRP) level, erythrocyte sedimentation rate (ESR), and the titers of ACPA and rheumatoid factor (RF). The Disease Activity Score of 28 joint count (DAS28) with ESR and CRP, clinical disease activity index (CDAI), simplified disease activity index (SDAI), and routine assessment of patient index data 3 (RAPID3) were collected. We also collected data on the presence of erosion in plain radiograph and concomitant medications.
Study Outcomes
The primary endpoint was the change from baseline in CDAI score after 1 year of treatment with abatacept or TNFi. Additionally, we stratified patients according to the baseline ACPA titer levels and previous exposure to bDMARD (bDMARD-naïve or not), and compared the changes in CDAI score after 1-year treatment for each subgroup. ACPA titer level was divided into three groups (low, > upper limit of normal and ≤ 100 U/ml; moderate, > 100 and ≤ 200 U/ml; high, > 200 U/ml) [24]. Secondary endpoint was the proportion of patient achieving CDAI remission or low disease activity (LDA) at 1 year. The level of CDAI score was categorized as follows: a CDAI of ≤ 2.8 indicated remission; 2.9 to 10.0, low disease activity; 10.1 to 22.0, moderate disease activity; and more than 22.0, high disease activity [25]. As a sensitivity analysis, we examined the change of DAS28-ESR as well as the remission rate based on DAS28-ESR (cut-off value < 2.6).
Statistical Analysis
Values were expressed as mean (standard deviation, SD) or number (percentage, %). Baseline characteristics of crude population were compared using Chi-square or Fisher’s exact tests for categorical variables and Student’s t test for continuous variables. Patients were matched using 1:2 PS matching method to adjust baseline confounders between treatment groups. For PS matching, the caliper was set to 0.2, then abatacept and TNFi users were matched by nearest-neighbor matching with multiple variables including age, sex, baseline CDAI score and the proportion of bDMARD-naïve users. The primary endpoint was analyzed using the analysis-of-covariance model with treatment group as the fixed factor and with the baseline CDAI score as a covariate. Subgroup analysis for primary endpoint was conducted using the generalized estimating equation. For secondary endpoint, treatment groups were compared with the generalized estimating equation with ordinal responses. Odds ratio (OR) and 95% confidence intervals (CI) for achieving CDAI remission or LDA after 1-year treatment with abatacept were determined through univariable and multivariable logistic regression analyses with TNFi as the reference in both the crude and PS-matched populations. Three multivariable regression models were constructed. Model 1 was adjusted for age, sex, baseline CDAI, disease duration, concomitant use of corticosteroids and methotrexate (MTX). Additional adjustments were performed to assess whether the association was independent of ACPA titers (low, moderate, and high) and line of bDMARD use (model 2 and 3, respectively). All statistical analysis was performed using R software version 3.5.1. A p value < 0.05 was considered statistically significant.
Results
Patients
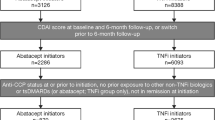
We identified 912 patients with RA who initiated abatacept or TNFi from the KOBIO registry, and 27 patients were lost to follow-up within a year and therefore excluded. Of the remaining 885 patients, a total of 138 abatacept and 487 TNFi initiators were ACPA-positive (crude population), 104 patients were ACPA-negative (22 abatacept initiators, 82 TNFi initiators), and 156 patients were unavailable for ACPA serostatus. After PS matching, 97 abatacept initiators and 194 TNFi initiators remained in the PS-matched population and were analyzed in this study (Fig. 1). Baseline data for PS-matched and crude population are presented in Table 1. In the crude population, TNFi group were younger (mean (SD), 53.3 (12.5) vs. 57.0 (13.5) years, p = 0.003), had a shorter disease duration (mean (SD), 7.1 (7.3) vs. 8.7 (8.0) years, p = 0.02), had higher disease activity at baseline (mean (SD) 27.5 (11.6) vs. 24.6 (10.4) in CDAI score, p = 0.01), and had a higher proportion of bDMARD-naïve patients (84.8 vs. 74.6%, p = 0.01) than abatacept group. Approximately, 90% of both groups were RF- and ACPA-positive. This discrepancy in the crude population was well balanced in the PS-matched population (Table 1).
Concomitant use of RA-related medication at baseline did not differ substantially across the PS-matched groups. Most patients (~ 97%) used csDMARD in both groups, however, the TNFi group used MTX more frequently while the abatacept group used leflunomide more frequently (Table 1). Notably, use of corticosteroids was prevalent in both groups (90.7% for abatacept and 85.1% for TNFi group). Most patients were bDMARD-naïve in both groups (86.6% for abatacept and 87.1% for TNFi group). Over half of the patients in each group had more than one radiographic erosion at baseline.
Changes in Clinical Outcomes After 1 Year of Treatment
At baseline, the mean (SD) CDAI score was 26.52 (9.77) in the abatacept group and 26.38 (9.11) in the TNFi group. The mean change in CDAI from baseline after 1-year treatment was − 16.78 (95% CI, − 19.55 to − 14.01) and − 13.61 (95% CI, − 15.61 to − 11.61), respectively (difference, − 3.17 points, p = 0.020) (Fig. 2A). The proportion of patients achieving CDAI remission or low disease activity after 1-year treatment was 68% with abatacept and 52.6% with TNFi (p = 0.013) (Fig. 2B). Univariable logistic regression analysis showed that achieving CDAI remission or LDA was associated with abatacept treatment (Table 2). In the multivariable logistic regression analysis, CDAI remission or LDA was again significantly associated with abatacept treatment in both the crude and PS-matched populations (adjusted OR 4.01, 95% CI, 1.46 to 11.00 in PS-matched population); abatacept treatment showed a significant association with CDAI remission or LDA even after adjusting for ACPA titers or line of bDMARD use (Table 2).
The results were similar in terms of comparison of DAS28-ESR changes at 1 year (− 2.28 (95% CI, − 2.59 to − 1.97) vs. − 1.80 (95% CI, − 2.05 to − 1.55), abatacept vs. TNFi group, p = 0.008). In addition, the abatacept group had a higher DAS28-ESR remission rate than the TNFi group (60.8 vs. 45.3%, p = 0.023).
Subgroup Analysis
Subgroup analysis stratified by baseline ACPA titer levels and previous exposure to bDMARD in the PS-matched population showed similar results for primary outcome. In a subgroup analysis of bDMARD-naïve or failure patients, the mean changes from baseline in CDAI for the abatacept and TNFi groups were − 16.85 (95% CI, − 18.97 to − 14.73) and − 13.50 (95% CI, − 15.49 to − 11.51), respectively, in the bDMARD-naïve patients (difference, − 3.35, p = 0.021). For bDMARD-failure patients, there was no significant difference in CDAI improvement between the abatacept and TNFi groups (difference, − 2.03, p = 0.793) (Fig. 3).
In a separate subgroup analysis for the ACPA titer levels, baseline characteristics including disease activity were generally comparable between the treatment groups, although a few differences were noted (e.g. corticosteroid dose; Table S1). At 1 year, mean changes from baseline in CDAI for the abatacept and TNFi group were − 18.13 (95% CI, − 20.14 to − 16.12) and − 12.56 (95% CI − 14.60 to − 10.52), in the low ACPA titer group, respectively (difference, − 5.57, p = 0.010). In contrast, moderate and high ACPA titer groups showed no significant differences in CDAI improvement between the abatacept and TNFi groups (p = 0.414 and p = 0.719, respectively) (Figure S1)).
Discussion
The relationship between ACPA serostatus and therapeutic response of bDMARD in patients with RA is still unclear. In this real-world study using data from the KOBIO registry, we found that the change of CDAI score was significantly greater in established ACPA-positive RA patients who started treatment with abatacept compared to TNFi. Furthermore, more patients in the abatacept group achieved CDAI remission or low disease activity at 1 year than in the TNFi group. Among ACPA-positive RA patients, patients with bDMARD naïve or ACPA titer levels of ≤ 100 U/ml had a greater improvement in CDAI when treated with abatacept compared to TNFi.
Autoantibody-positive and autoantibody-negative RA are considered to be distinct disease subtypes that might be associated with different pathogenic mechanisms [26, 27]. ACPA positivity is associated with poor prognosis such as radiographic joint damage and increased mortality [28,29,30,31]. Therefore, it is important to determine the optimal patient-centric strategy for the choice of bDMARD for patient with RA, especially those with poor prognostic factors. Positive autoantibody status is associated with a good response to rituximab and abatacept, which target B cells and T cells, respectively [17]. Although RF positivity did not predict a response to abatacept [32], previous studies have shown that ACPA positivity is associated with improved clinical response and drug retention of abatacept [13, 16, 19]. One meta-analysis showed a significant positive association between ACPA positivity and EULAR response to abatacept (Relative risk (RR) 1.18 [95% CI 1.03 to 1.35]), but for TNFi there was no association with ACPA positivity and EULAR response (RR 0.97 [0.86 to 1.10]) [33].
Nevertheless, evidence for comparative efficacy of abatacept and TNFi in RA patients stratified by ACPA serostatus is still scarce. An observational study using US Corrona registry found that patients with ACPA-positive RA showed similar clinical outcomes at 6 months between the abatacept and TNFi groups of the overall population [20]. This study compared the treatment groups after PS matching and had similar disease duration (9.6–9.8 years) to our study. However, short-term follow-up period and low proportions of concomitant use of MTX (59.7–62.4%) and corticosteroid (37.0–38.5%) may affect the outcomes, resulting in a less pronounced improvement of CDAI (− 9.85 for abatacept and − 8.53 for TNFi) compared to our study. The longitudinal CDAI changes reported in another study for abatacept in ACPA-positive patients were similar to our study; −8.53 and −19.01 at 6 and 12 months, respectively [34].
In our study, CDAI after 1 year was significantly reduced in abatacept treated patients compared with those treated with TNFi who were bDMARD-naïve, while there was no difference between the two groups among patients who had been exposed to a bDMARD. Previous studies showed that there was no difference in disease activity and patient-reported outcomes between the abatacept and TNFi treated patients regardless of prior exposure to a bDMARD, yet the subjects were not stratified by ACPA status [35,36,37,38]. Since most of the head-to-head trials were conducted using a non-inferiority study design, it remains at times a challenge to select the proper bDMARD for patients in daily clinical practice. On the other hand, Frisell et al. showed superior effectiveness of non-TNFi bDMARDs compared with TNFi in patients with RA from the Swedish Rheumatology Register [39]. Furthermore, a recent post hoc analysis of the AMPLE study found that abatacept was more effective than adalimumab after 1 and 2 years of treatment in patients with bDMARD-naïve, seropositive, erosive, early RA [21]. Another comparative study showed similar improvements in disease activity of abatacept and TNFi among bDMARD-naïve, ACPA-positive patients; this might be due to a less erosive disease than our study (proportion of abatacept-treated patients with radiographic erosion, 37.3 versus 58.9%) [20]. Indeed, erosions have been shown to be a poor prognostic factor for patients with RA, and hence, they might also be a factor associated with the lack of response to different treatment [40]. Therefore, this finding suggests that abatacept may be a treatment option for difficult-to-treat patients with poor prognostic factors. On the other hand, the small sample size after PS matching may limit the comparison of abatacept with TNFi in patients who failed to one bDMARD in this study. In addition, response to a particular drug can be affected differently depending on previous treatment. Failure to one or more bDMARD may also be related to non-inflammatory mechanisms or other molecular mechanisms that elude common pathways targeted by current bDMARDs treatment [27].
Interestingly, better improvement in CDAI with abatacept over TNFi treatment was seen in patients with low ACPA titers (> upper limit of normal and ≤ 100 U/ml) in our study. Furthermore, the difference in CDAI changes between the treatment groups tended to increase with lower ACPA titer levels across the three subgroups stratified by ACPA titer levels. On the other hand, Sokolove et al. demonstrated a better clinical response with abatacept in patients with the highest quartiles of ACPA titer than patients with lower levels among ACPA-positive, bDMARD-naïve RA patients [14]. However, ACPA-positive patients treated with adalimumab showed no association between ACPA titer levels and treatment response. One plausible explanation for this different trend is that the disease duration in our study (~ 8 years) was greater than in the previous study (~ 2 years). Over half of patients in our study already had radiographic erosions at baseline, suggesting long-standing established RA. Meanwhile, in terms of high ACPA titer being a poor prognostic factor, differences in efficacy between treatment groups can be attenuated in patients with high ACPA titer, as most drugs are often ineffective in high ACPA titers. Another plausible reason for the treatment response according to ACPA titers is the different drivers that promote inflammation in patients with RA. Among active ACPA-positive patients who initiated bDMARD, inflammation in patients with high ACPA titers could be primarily mediated by increased ACPA-citrullinated protein immune complex formation, which results in production of pro-inflammatory cytokines (e.g., TNF-alpha) by its binding to Fc receptors on monocytes/macrophages [9]. Therefore, this effector function of ACPA could be effectively neutralized by TNFi. On the other hand, aberrant T cell activation due to autoimmunity may be the main factor associated with inflammation in patients with low ACPA titers [9]. Thus, abatacept may be more effective than TNFi in RA patients with low ACPA titers whose inflammation is characterized by pathological T cell activation.
To the best of our knowledge, this is the first study from an Asian population comparing the efficacy between abatacept and TNFi in patients with ACPA-positive RA. It is important to conduct studies with patients of different ethnic backgrounds, as therapeutic responses to drugs can vary by race due to a its genetic background. For instance, CD84 expression is associated with response to etanercept in RA patients of European ancestry, but not in Portuguese or Japanese [41]. The limitations of this study should be considered. First, physicians prescribe medication based on the patient’s profile and treatment selection is not random due to the nature of the observational study. To overcome this bias, we matched by PS method, however, this method also does not address unknown confounding factors. Second, each subgroup contained a relatively limited number of patients, which may have compounded the ability to detect differences in therapeutic response. Third, our study used CDAI as a key clinical outcome rather than DAS28 and/or other indices. However, CDAI has been validated in RA and has shown significant correlations with the SDAI and the DAS28 [42]. Furthermore, CDAI has been utilized as the primary outcome in studies comparing the efficacy of bDMARDs [35, 38]. Fourth, it should also be noted that there was no centralized laboratory evaluation of ACPA serostatus, which may have led to some misclassification. Lastly, this is 1-year data and requires long-term follow-up.
Conclusions
This study, based on data from this nationwide biologic registry, suggests that abatacept may show a significant improvement in clinical outcomes compared to TNFi in patients with established ACPA-positive RA. Abatacept may be particularly beneficial over TNFi in patients with ACPA-positive RA who are bDMARD-naïve or have an ACPA titer of 100 U/ml or less. These findings suggest that stratification of patients by ACPA serostatus, along with disease duration and previous biologic treatment, is important in predicting treatment response of abatacept, thereby improving the clinical response by selecting a suitable biological treatment option for the right patient.
References
McInnes IB, Schett G. The pathogenesis of rheumatoid arthritis. N Engl J Med. 2011;365:2205–19.
Kerschbaumer A, Sepriano A, Smolen JS, et al. Efficacy of pharmacological treatment in rheumatoid arthritis: a systematic literature research informing the 2019 update of the EULAR recommendations for management of rheumatoid arthritis. Ann Rheum Dis. 2020;79:744–59.
Jansen JP, Buckley F, Dejonckheere F, Ogale S. Comparative efficacy of biologics as monotherapy and in combination with methotrexate on patient reported outcomes (PROs) in rheumatoid arthritis patients with an inadequate response to conventional DMARDs—a systematic review and network meta-analysis. Health Qual Life Outcomes. 2014;12:102.
Buckley F, Finckh A, Huizinga TW, Dejonckheere F, Jansen JP. Comparative efficacy of novel DMARDs as monotherapy and in combination with methotrexate in rheumatoid arthritis patients with inadequate response to conventional DMARDs: a network meta-analysis. J Manag Care Spec Pharm. 2015;21:409–23.
Smolen JS, Landewé RBM, Bijlsma JWJ, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis. 2020;79:685–99.
Singh JA, Saag KG, Bridges SL Jr, et al. 2015 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Rheumatol. 2016;68:1–26.
Pitzalis C, Choy EHS, Buch MH. Transforming clinical trials in rheumatology: towards patient-centric precision medicine. Nat Rev Rheumatol. 2020;16:590–9.
Humby F, Durez P, Buch MH, et al. Rituximab versus tocilizumab in anti-TNF inadequate responder patients with rheumatoid arthritis (R4RA): 16-week outcomes of a stratified, biopsy-driven, multicentre, open-label, phase 4 randomised controlled trial. Lancet. 2021;397:305–17.
Schett G, Tanaka Y, Isaacs JD. Why remission is not enough: underlying disease mechanisms in RA that prevent cure. Nat Rev Rheumatol. 2021;17:135–44.
Bozec A, Luo Y, Engdahl C, Figueiredo C, Bang H, Schett G. Abatacept blocks anti-citrullinated protein antibody and rheumatoid factor mediated cytokine production in human macrophages in IDO-dependent manner. Arthritis Res Ther. 2018;20:24.
Iwata S, Nakayamada S, Fukuyo S, et al. Activation of Syk in peripheral blood B cells in patients with rheumatoid arthritis: a potential target for abatacept therapy. Arthritis Rheumatol. 2015;67:63–73.
Jansen D, Emery P, Smolen JS, et al. Conversion to seronegative status after abatacept treatment in patients with early and poor prognostic rheumatoid arthritis is associated with better radiographic outcomes and sustained remission: post hoc analysis of the AGREE study. RMD Open. 2018;4: e000564.
Gottenberg JE, Ravaud P, Cantagrel A, et al. Positivity for anti-cyclic citrullinated peptide is associated with a better response to abatacept: data from the “Orencia and Rheumatoid Arthritis” registry. Ann Rheum Dis. 2012;71:1815–9.
Sokolove J, Schiff M, Fleischmann R, et al. Impact of baseline anti-cyclic citrullinated peptide-2 antibody concentration on efficacy outcomes following treatment with subcutaneous abatacept or adalimumab: 2-year results from the AMPLE trial. Ann Rheum Dis. 2016;75:709–14.
Nüßlein H, Alten R, Galeazzi M, et al. Real-world effectiveness of abatacept for rheumatoid arthritis treatment in European and Canadian populations: a 6-month interim analysis of the 2-year, observational, prospective ACTION study. BMC Musculoskelet Disord. 2014;15:14.
Nüßlein HG, Alten R, Galeazzi M, et al. Prognostic factors for abatacept retention in patients who received at least one prior biologic agent: an interim analysis from the observational, prospective ACTION study. BMC Musculoskelet Disord. 2015;16:176.
Isaacs JD, Cohen SB, Emery P, et al. Effect of baseline rheumatoid factor and anticitrullinated peptide antibody serotype on rituximab clinical response: a meta-analysis. Ann Rheum Dis. 2013;72:329–36.
Lv Q, Yin Y, Li X, et al. The status of rheumatoid factor and anti-cyclic citrullinated peptide antibody are not associated with the effect of anti-TNFα agent treatment in patients with rheumatoid arthritis: a meta-analysis. PLoS ONE. 2014;9: e89442.
Harrold LR, Litman HJ, Connolly SE, et al. Effect of anticitrullinated protein antibody status on response to abatacept or antitumor necrosis factor-α therapy in patients with rheumatoid arthritis: a US national observational study. J Rheumatol. 2018;45:32–9.
Harrold LR, Litman HJ, Connolly SE, et al. Comparative effectiveness of abatacept versus tumor necrosis factor inhibitors in patients with rheumatoid arthritis who are anti-CCP positive in the United States Corona Registry. Rheumatol Ther. 2019;6:217–30.
Fleischmann R, Weinblatt M, Ahmad H, et al. Efficacy of abatacept and adalimumab in patients with early rheumatoid arthritis with multiple poor prognostic factors: post hoc analysis of a randomized controlled clinical trial (AMPLE). Rheumatol Ther. 2019;6:559–71.
Kim J, Koh JS, Choi SJ, et al. KOBIO, the first web-based Korean biologics registry operated with a unified platform among distinct disease entities. J Rheum Dis. 2021;28:176–82.
Aletaha D, Neogi T, Silman AJ, et al. Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010;62:2569–81.
Shiozawa K, Kawasaki Y, Yamane T, et al. Anticitrullinated protein antibody, but not its titer, is a predictor of radiographic progression and disease activity in rheumatoid arthritis. J Rheumatol. 2012;39:694–700.
Aletaha D, Ward MM, Machold KP, Nell VP, Stamm T, Smolen JS. Remission and active disease in rheumatoid arthritis: defining criteria for disease activity states. Arthritis Rheum. 2005;52:2625–36.
van der Helm-van Mil AH, Huizinga TW. Advances in the genetics of rheumatoid arthritis point to subclassification into distinct disease subsets. Arthritis Res Ther. 2008;10(2):205.
Buch MH, Eyre S, McGonagle D. Persistent inflammatory and non-inflammatory mechanisms in refractory rheumatoid arthritis. Nat Rev Rheumatol. 2021;17:17–33.
van Gaalen FA, van Aken J, Huizinga TW, et al. Association between HLA class II genes and autoantibodies to cyclic citrullinated peptides (CCPs) influences the severity of rheumatoid arthritis. Arthritis Rheum. 2004;50(7):2113–21.
Gonzalez A, Icen M, Kremers HM, et al. Mortality trends in rheumatoid arthritis: the role of rheumatoid factor. J Rheumatol. 2008;35:1009–14.
Aletaha D, Alasti F, Smolen JS. Rheumatoid factor, not antibodies against citrullinated proteins, is associated with baseline disease activity in rheumatoid arthritis clinical trials. Arthritis Res Ther. 2015;17:229.
Meyer O, Labarre C, Dougados M, et al. Anticitrullinated protein/peptide antibody assays in early rheumatoid arthritis for predicting five year radiographic damage. Ann Rheum Dis. 2003;62:120–6.
Maneiro RJ, Salgado E, Carmona L, Gomez-Reino JJ. Rheumatoid factor as predictor of response to abatacept, rituximab and tocilizumab in rheumatoid arthritis: systematic review and meta-analysis. Semin Arthritis Rheum. 2013;43:9–17.
Alemao E, Postema R, Elbez Y, Mamane C, Finckh A. Presence of anti-cyclic citrullinated peptide antibodies is associated with better treatment response to abatacept but not to TNF inhibitors in patients with rheumatoid arthritis: a meta-analysis. Clin Exp Rheumatol. 2020;38:455–66.
Tymms K, Butcher B, Smith T, Littlejohn G. Impact of anti-citrullinated protein antibody on tumor necrosis factor inhibitor or abatacept response in patients with rheumatoid arthritis. Eur J Rheumatol. 2020;8:67–72.
Pappas DA, St John G, Etzel CJ, et al. Comparative effectiveness of first-line tumour necrosis factor inhibitor versus non-tumour necrosis factor inhibitor biologics and targeted synthetic agents in patients with rheumatoid arthritis: results from a large US registry study. Ann Rheum Dis. 2021;80:96–102.
Schiff M, Weinblatt ME, Valente R, et al. Head-to-head comparison of subcutaneous abatacept versus adalimumab for rheumatoid arthritis: two-year efficacy and safety findings from AMPLE trial. Ann Rheum Dis. 2014;73:86–94.
Kubo S, Nakayamada S, Nakano K, et al. Comparison of efficacy of TNF inhibitors and abatacept in patients with rheumatoid arthritis; adjusted with propensity score matching. Clin Immunol. 2018;191:67–74.
Harrold LR, Reed GW, Kremer JM, et al. The comparative effectiveness of abatacept versus anti-tumour necrosis factor switching for rheumatoid arthritis patients previously treated with an anti-tumour necrosis factor. Ann Rheum Dis. 2015;74:430–6.
Frisell T, Dehlin M, Di Giuseppe D, Feltelius N, Turesson C, Askling J. Comparative effectiveness of abatacept, rituximab, tocilizumab and TNFi biologics in RA: results from the nationwide Swedish register. Rheumatology. 2019;58:1367–77.
Novella-Navarro M, Plasencia C, Tornero C, et al. Clinical predictors of multiple failure to biological therapy in patients with rheumatoid arthritis. Arthritis Res Ther. 2020;22:284.
Cui J, Stahl EA, Saevarsdottir S, et al. Genome-wide association study and gene expression analysis identifies CD84 as a predictor of response to etanercept therapy in rheumatoid arthritis. PLoS Genet. 2013;9: e1003394.
Aletaha D, Smolen J. The Simplified Disease Activity Index (SDAI) and the Clinical Disease Activity Index (CDAI): a review of their usefulness and validity in rheumatoid arthritis. Clin Exp Rheumatol. 2005;23:S100–8.
Acknowledgements
We would like to thank Evo Alemao and Song-Wha Chae for sharing their insights for this study.
Funding
The study was sponsored by Bristol-Myers Squibb. This funding source had no role in the design of this study nor did it have any role during its execution, analysis, interpretation of the data, or decision to submit results. The journal’s Rapid Service Fee was funded by the authors.
Medical Writing and Editorial Assistance
Professional medical writing and editorial assistance was provided by Lola Parfitt, MRes, at Caudex, and was funded by Bristol-Myers Squibb.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Conceptualization, KS; data curation, S-KL and SO; formal analysis, S-KL, SO and KS; funding acquisition, KS; writing—original draft, MJK and KS; writing—review and editing, H-AK, Y-BP, S-SL, and KS
Disclosures
Min Jung Kim, Sun-Kyung Lee, Sohee Oh, Hyoun-Ah Kim, Yong-Beom Park, Shin-Seok Lee and Kichul Shin have nothing to disclose. They do not have any commercial benefits or financial interests in the study reported, or any other financial interests, which could create a potential conflict of interest or the appearance of a conflict of interest.
Compliance with Ethics Guidelines
This study was performed in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice guidelines. All subjects provided written informed consent upon enrolment into the KOBIO registry. The study protocol was approved by the institutional review boards at BMC (26-2012-34).
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Prior Presentation
This work was presented as a poster communication in the Annual European Congress of Rheumatology (ARD, June 2018, Volume: 77, Pages 331).
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kim, M.J., Lee, SK., Oh, S. et al. Efficacy of Abatacept Versus Tumor Necrosis Factor Inhibitors in Anti-citrullinated Protein Antibody-Positive Patients with Rheumatoid Arthritis: Results from a Korean Nationwide Biologics Registry. Rheumatol Ther 9, 1143–1155 (2022). https://doi.org/10.1007/s40744-022-00467-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-022-00467-4